Abstract
Introduction and importance
Anterior column plate combined with posterior column screws have been effectively used for treatment of displaced transverse acetabular fractures. This article presents the use of 3D-printed technology for customising a guide template to appropriately place posterior column screw.
Case presentation
A 50-year-old female suffered displaced juxtatectal fracture of the right acetabulum. A personalised guide for antegrade posterior column screw placement was designed based on the data of her pelvic CT-scan. This guide and a prototype of her right acetabulum - created by mirroring the intact left acetabulum - were 3D-printed for preoperative evaluation and pre-contouring of reconstruction plate. Modified Stoppa approach and additional lateral window were used for direct reduction, anterior column plate and posterior column lag screw fixation. Post-operative CT-scan showed good reduction and nearly ideal screw position.
Clinical discussion
Anterior column plate and antegrade posterior column screw could provide joint stability and early mobilisation for displaced transverse acetabular fractures. However, determination of optimal entry point, direction and length for screw insertion is still technically demanding. The 3-D reconstruction images of hemipelvic specimen allowed us to identify the safe bone corridor, design a drill guide to put the proper guide pin and conduct preoperative trial. All those resulted in appropriate real screw fixation with reduction of soft tissue damage, X-ray exposure and time of operation.
Conclusion
The use of 3D-printed personalised guide for posterior column screw fixation is a promising alternative option for treatment of displaced transverse acetabular fracture where 3D-navigation system is not available.
Keywords: Case report, Transverse acetabular fracture, 3D-printed personalised drill guide, Posterior column screw fixation
Highlights
-
•
3D-printed personalised drill guide is a potential tool for minimally invasive techniques.
-
•
Anatomical reduction is required to optimise the precision of 3D-printed personalised guide.
-
•
Iliac tubercle can be used as a landmark for defining the entry point of posterior column lag screw.
-
•
Intraoperative fluoroscopic control is still needed to confirm the screw placement.
1. Introduction and importance
Acetabular fractures often require experienced surgeons to treat, especially in the type of fractures involving both columns, such as transverse fractures, T-type fractures, anterior column with posterior hemitransverse fractures and two-column fractures. Although being classified as one of five elementary fractures [1], transverse acetabular fractures may lead to osteoarthritis and poor clinical outcome if not reduced anatomically [2], [3], [4]. Recently, Jang et al. [5] have identified risks factors for poor outcomes in surgically treating transverse acetabular fractures, including dome impaction, residual gaps of more than 3 mm and step of more than 1 mm. Therefore, anatomical reduction and stable fixation are essential requirements for avoiding post-traumatic arthritis in management of transverse acetabular fracture, especially in the juxtatectal and transtectal subtypes [3]. Various strategies for stabilising these types of fractures have been proposed. Some authors preferred open reduction and plate fixation for the anterior column and minimally invasive lag screw fixation for the posterior column under guidance of intraoperative fluoroscopy [6], [7], [8]. There were also reports [9], [10] using 3D navigation system for percutaneous screw fixation of the acetabular and pelvic fractures. While the results from these reports of 3D navigation system were demonstrated to reduce the rate of screw malposition, the system is not widely available. In this report, we present an application of 3D-printed technology to customise an individual guide for minimally invasive screw fixation of the posterior column in a patient with displaced transverse acetabular fracture.
This case report has been reported in line with the SCARE 2020 criteria [11].
2. Case presentation
A 50-year-old female with no past medical history was admitted to our hospital due to motor vehicle accident. She was diagnosed with subarachnoid haemorrhage and right acetabular fracture. While she was receiving supplemental support as the conservative treatment of subarachnoid haemorrhage, her right acetabulum was planned to operate on. Initially, the right tibial traction was applied to facilitate later acetabular reduction. Her pelvic CT-scan showed that she had 62B1.2 type fracture according to AO/OTA classification [12] (Fig. 1).
Fig. 1.
The reconstruction images from CT-scan data illustrated juxtatectal type fracture of the right acetabulum. A) Anterior – posterior view; B) Intrapelvic view of the right acetabulum; C) Posterior – anterior view.
The CT-scan DICOM data was exported to STL model using Invesalius (CTI, Brazil). The mirrored model of the right hemipelvis from the left-sided one was created and 3D-printed. The prototype was used as a template for pre-contouring 14-holes reconstruction plate. A drill guide for posterior column screw fixation was designed based on the 3D data of the right hemipelvis. This drill guide includes two parts; each part took specific anatomic landmarks for positioning (Fig. 2): iliac tubercle, anterior superior iliac spine (ASIS) and anterior inferior iliac spine (AIIS). The estimated length of posterior cannulated screw was 90 mm based on the planed screw's trajectory. Subsequently, this 3D-printed drill guide was tested with the prototype (Fig. 2D).
Fig. 2.
(colour): The 3D model of the patient's pelvis with virtual reduction of the right acetabular fracture. A) The drill guide including two parts: the brighter one used iliac tubercle as the anatomical landmark and the darker one used the ASIS and anterior inferior iliac spine (AIIS) as the anatomical landmarks. Two parts could be joined together by two rectangular mortise. Each part had K-wire guides for its stabilisation (1,2 and 3). The red pin illustrates planned K-wire trajectory (4). B) The planned entry point of the 2.0 mm K-wire was illustrated by removing the drill guide. C) The posterior – anterior view of the pelvis with the planned exit's position of K-wire. D) The 3D-printed prototype of the mirrored left-sided pelvis to use as an reduced right acetabulum. The drill guide was designed to fit the right iliac tubercle and right ASIS but it also fit the mirrored left-sided pelvis. The K-wire trajectory was also in good position with this prototype.
After 14 days of the conservative treatment for subarachnoid haemorrhage, the patient underwent surgery for fixation of the acetabular fracture. The senior author (H.D·P) performed the procedure. Modified Stoppa approach was used to directly reduce and temporarily maintain the fragments with two 2.0 mm K-wires. The lateral window was opened for placing the pre-contoured reconstruction plate and the drill guide (Fig. 3).
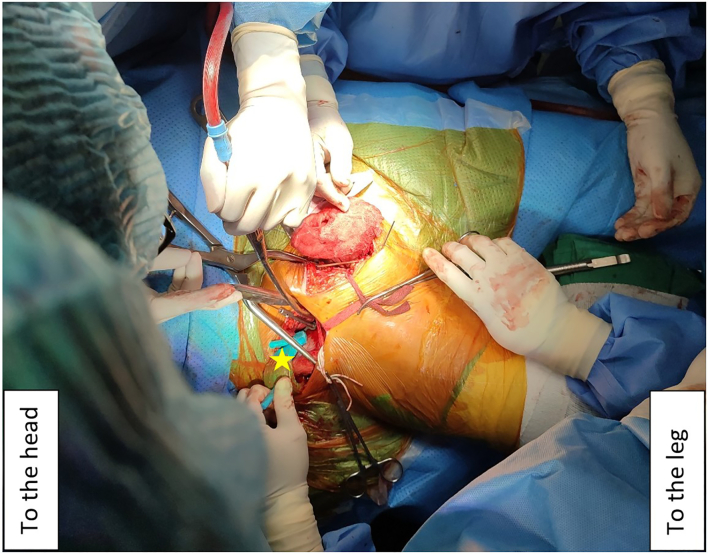
Fig. 3.
(colour): Patient was in supine position. Intraoperative placement of first part of the drill guide (yellow star) using iliac tubercle as the anatomical landmark. The modified Stoppa approach was used together with the lateral window.
However, we found the iliac tubercle part of the drill guide was sufficient for defining the entry point and the direction of the screw due to the fitting of the guide and the bony landmark. A 2.0 mm K-wire was used for pre-drilling the screw trajectory. After checking the position of this trajectory in three planes of fluoroscopy (plain anterior – posterior view, obturator oblique view and iliac oblique view), the screw was inserted to fix the posterior column (Fig. 4). The total blood loss and surgery time were 280 ml and 135 mins, respectively.
Fig. 4.
Intraoperative fluoroscopy with three views – (A): AP view, (B): iliac oblique view, (C): obturator oblique view – illustrated the 6.5 mm cannulated screw's position.
Fig. 5 showed postoperative CT-scan of the patient, and the screw position was also illustrated. The real screw entry point was medially deviated 3.75 mm in comparison with the estimated point (Fig. 5B). On post-operative day (POD) 1, the patient was satisfied with the result as she was able to sit in upright position and start passive range of motion of her right hip joint. The drain was removed on POD 2 and the patient was discharged on POD 5 with the allowance of toe touch weight bearing supported by crutches. During the post-operative period, there was neither sign of infection nor the requirement of blood transfusion. The total hospitalisation time was 20 days including 14 days of conservative treatment due to subarachnoid haemorrhage.
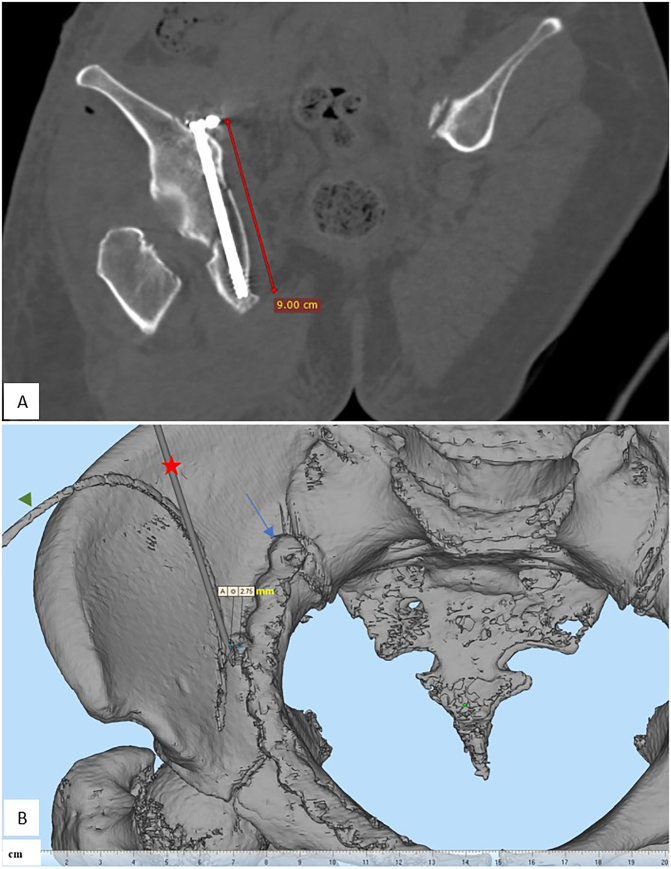
Fig. 5.
A) The postoperative CT-scan slice illustrates the screw with two reduced fragments of the right acetabulum. B) By superimposing the preoperative and postoperative CT-scan data, we measured the real entry point and the planned one (the planned 2.0 mm K-wire was marked with red star). There was a 3.75 mm (2.75 mm as illustrated and 1.0 mm from the radius of the 2.0 mm K-wire) medial displacement of the real screw's entry point. The green arrowhead and the blue arrow illustrated the drain tube and the reconstruction plate, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Clinical discussion
Open reduction and internal fixation remain the gold-standard for treatment of displaced acetabular fractures [13]. Lag screw fixation has been proved to achieve inter-fragmentary compression, maintenance of reduction with good clinical outcome [14]. In our presented case, plate fixation of the anterior column combined with a lag screw fixation of the posterior column was planned. The lag screw placement in the posterior column of the acetabulum has a narrow corridor of safety due to its close vicinity to the hip joint, neurovascular and visceral structures. Therefore, the anatomical reduction of fragments is prerequisite to optimise precision of the drill guide as the virtually planned fixation. In this case, we used modified Stoppa approach for direct visualisation and reduction of two main fragments. As in a systematic review, Meena et al. [15] found that modified Stoppa approach had better reduction and lower complication rates with less operative time when compared to ilioinguinal approach.
It is essential to preoperatively identify the safe corridor for screw placement because it would determine not only the screw entry point and its direction but also the screw size as well. Previous studies showed differences of reference points. Pierannunzii et al. [16] proposed the drill entry point is about 2.5 cm above the pelvic brim and 1 cm anterior to the coronal plane passing through the anterior aspect of the sacrum. The drill should point to the midpoint between the ischial spine and the posterior profile of the obturator foramen. In Stöckle's study [14] with 51 cases of acetabular fractures, the stabilising screws for the posterior column were inserted from the inner aspect of the ilium towards the ischium under visual and X-ray control. Feng et al. [17] analysed the 3D pelvic data of fifty-nine Chinese human subjects and found that while the safe zone and the direction of antegrade lag screw fixation were determined, it was not easy to directly use the results intra-operatively. Because the range and standard deviation of the results are relatively large, it is recommended that individual preoperative planning be implemented for each patient.
In our design, the iliac tubercle (first part) together with the ASIS and AIIS (second part) were used as anatomical landmarks for positioning this drill guide template. Intraoperatively, when applying the first part through the lateral window, however, we found that this part fitted well with the iliac tubercle and there was no need to dissect more soft tissue to insert the second part. Chen et al. [18] introduced an adult universal guide template for the placement of posterior column lag screw, using the quadrilateral surface and iliac fossa as the anatomical landmarks for its placement. This template requires deeper soft tissue dissection and more technical demanding for the surgeon to hold the template before stabilising it by adjacent K-wires.
The patient's postoperative CT-scan showed that the anatomical reduction was achieved, and the lag screw was in good position. However, there was a 3.75 mm medial deviation of the real 6.5 mm cannulated screw entry point when comparing to the planned one. It could be caused by the interference of residual soft tissue. Meesters et al. [19] conducted a cadaveric study with 3D-printed drill guides for 4.5 mm posterior column screw. He found that the deviation of its entry point is ranging from 2 mm to 5 mm. Chui et al. [9] reported the mean deviation of 1.91 mm with 3D-navigation system. The advantages of our method are to individualise plan of treatment in detail, reduce X-ray exposure while identifying screw entry point, its direction and result in less soft-tissue damage. The total blood loss and operative time were significantly reduced when comparing to the similar cases we treated previously with conventional methods using anatomical reference points to define the screw insertion and its trajectory. It may be a good alternative to conventional methods while there has been a widely unavailable of 3D-navigation system. And these results suggested that even after accurately positioning the drill guide, intraoperative fluoroscopic control is still needed to confirm the screw placement.
The method showed in this report is feasible for future clinical settings. However, it took us 4 days for preoperative planning, designing, and 3D-printing of all the needed models. Therefore, the available time should be considered from patient admission to surgery before this method could be widely applied.
4. Conclusion
The application of 3D-printed personalised drill guide for insertion of posterior column lag screw allows to simplify the complex traditional technique. It is a promising alternative option in the treatment of transverse acetabular fractures. However, it should be noted that intraoperative fluoroscopic control is still needed to confirm the screw position even when the accurate placement of the drill guide is achieved.
Sources of funding
This report did not receive any specific grant from any funding agencies in the public, commercial, or not-for-profit sectors.
Ethical approval
This report was conducted in accordance with the World Medical Association Declaration of Helsinki.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Research registration
Research Registry was not required.
Guarantor
Associate Professor Hung Do Phuoc MD, PhD.
Provenance and peer review
Not commissioned, externally peer-reviewed.
CRediT authorship contribution statement
Hung Do Phuoc: conceptualising the plan for surgery, performing the surgery, writing the literature review for case report, reviewing the manuscript.
Huong Cao Ba: Assisting the surgery, designing the drill guide template.
Phu Nguyen Hoang: Designing the drill guide template, assisting the surgery, writing the draft for case report.
Declaration of competing interest
The authors declare no conflicts of interest in this work.
Contributor Information
Hung Do Phuoc, Email: dphungcr@ump.edu.vn.
Phu Nguyen Hoang, Email: nguyenhoangphu@ump.edu.vn.
Huong Cao Ba, Email: cbh177@ump.edu.vn.
References
- 1.Letournel E., Judet R. Fractures of the acetabulum. 2nd ed. Springer-Verlag Berlin Heidelberg; Berlin, Heidelberg: 1993. pp. 63–66. [Google Scholar]
- 2.Oh C.W., Kim P.T., Park B.C., Kim S.Y., Kyung H.S., Jeon I.H. Results after operative treatment of transverse acetabular fractures. 2006;11(5):478–484. doi: 10.1007/s00776-006-1045-6. Epub 2006/10/03. [DOI] [PubMed] [Google Scholar]
- 3.Hak D.J., Hamel A.J., Bay B.K., Sharkey N.A., Olson S.A. Consequences of transverse acetabular fracture malreduction on load transmission across the hip joint. J. Orthop. Trauma. 1998;12(2):90–100. doi: 10.1097/00005131-199802000-00005. Epub 1998/03/21. [DOI] [PubMed] [Google Scholar]
- 4.Malkani A.L., Voor MJ Rennirt G., Helfet D., Pedersen D., Brown T. Increased peak contact stress after incongruent reduction of transverse acetabular fractures: a cadaveric model. J. Trauma. 2001;51(4):704–709. doi: 10.1097/00005373-200110000-00013. Epub 2006/10/03. [DOI] [PubMed] [Google Scholar]
- 5.Jang J.H., Moon N.H., Rhee S.J., Jung S.J., Ahn T.Y. Surgical outcomes of transverse acetabular fractures and risk factors for poor outcomes. BMC Musculoskelet. Disord. 2021;22(1):222. doi: 10.1186/s12891-021-04082-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shahulhameed A., Roberts C.S., Pomeroy C.L., Acland R.D., Giannoudis P.V. Mapping the columns of the acetabulum--implications for percutaneous fixation. Injury. 2010;41(4):339–342. doi: 10.1016/j.injury.2009.08.004. Epub 2009/09/08. [DOI] [PubMed] [Google Scholar]
- 7.Chen W., Zhang Z., Lu Y., Li J., Zhang Y., Shen Y. Fluoroscopic views for safe insertion of lag screws into the posterior column of the acetabulum. BMC Musculoskelet. Disord. 2014;15(1):303. doi: 10.1186/1471-2474-15-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Osterhoff G., Amiri S., Unno F., Dodd A., Guy P., O’Brien P.J. The "Down the PC" view – a new tool to assess screw positioning in the posterior column of the acetabulum. Injury. 2015;46(8):1625–1628. doi: 10.1016/j.injury.2015.04.042. [DOI] [PubMed] [Google Scholar]
- 9.Chui K.H., CCD Chan, Ip K.C., Lee K.B., Li W. Three-dimensional navigation-guided percutaneous screw fixation for nondisplaced and displaced pelvi-acetabular fractures in a major trauma centre. Int. Orthop. 2018;42(6):1387–1395. doi: 10.1007/s00264-017-3659-z. Epub 2017/10/25. [DOI] [PubMed] [Google Scholar]
- 10.Wong J.S.Y., Lau J.C.K., Chui K.H., Tiu K.L., Lee K.B., Li W. Three-dimensional-guided navigation percutaneous screw fixation of fragility fractures of the pelvis. J. Orthop. Surg. 2019;27(1) doi: 10.1177/2309499019833897. [DOI] [PubMed] [Google Scholar]
- 11.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. (Lond. Engl.) 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. Epub 2020/11/13. [DOI] [PubMed] [Google Scholar]
- 12.Tile M., Helfet D.L., Kellam J.F., Vrahas M. Fractures of the Pelvis and Acetabulum - Principles and Methods of Management. 4th ed. Vol. 2. Thieme; 2015. pp. 447–470. [Google Scholar]
- 13.Briffa N., Pearce R., Hill A.M., Bircher M. Outcomes of acetabular fracture fixation with ten years' follow-up. 2011;93(2):229–236. doi: 10.1302/0301-620x.93b2.24056. Epub 2011/02/02. [DOI] [PubMed] [Google Scholar]
- 14.Stöckle U., Hoffmann R., Nittinger M., Südkamp N.P., Haas N.P. Screw fixation of acetabular fractures. Int. Orthop. 2000;24(3):143–147. doi: 10.1007/s002640000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meena S., Sharma P.K., Mittal S., Sharma J., Chowdhury B. Modified stoppa approach versus ilioinguinal approach for anterior acetabular fractures; a systematic review and meta-analysis. Bull. Emerg. Trauma. 2017;5(1):6–12. [PMC free article] [PubMed] [Google Scholar]
- 16.Pierannunzii L., Fischer F., Tagliabue L., Calori G.M., d'Imporzano M. Acetabular both-column fractures: essentials of operative management. Injury. 2010;41(11):1145–1149. doi: 10.1016/j.injury.2010.08.011. Epub 2010/09/11. [DOI] [PubMed] [Google Scholar]
- 17.Feng X., Zhang S., Luo Q., Fang J., Lin C., Leung F. Definition of a safe zone for antegrade lag screw fixation of fracture of posterior column of the acetabulum by 3D technology. Injury. 2016;47(3):702–706. doi: 10.1016/j.injury.2016.01.026. Epub 2016/02/13. [DOI] [PubMed] [Google Scholar]
- 18.Chen H., Wang G., Li R., Sun Y., Wang F., Zhao H. A novel navigation template for fixation of acetabular posterior column fractures with antegrade lag screws: design and application. Int. Orthop. 2016;40(4):827–834. doi: 10.1007/s00264-015-2813-8. Epub 2015/06/27. [DOI] [PubMed] [Google Scholar]
- 19.AML Meesters, Assink N., Ten Duis K., Fennema E.M., Kraeima J., MJH Witjes. Accuracy of patient-specific drilling guides in acetabular fracture surgery: a human cadaver study. J. Personalized Med. 2021;11(8) doi: 10.3390/jpm11080763. Epub 2021/08/28. [DOI] [PMC free article] [PubMed] [Google Scholar]