Abstract
Objectives
In the wake of recent widespread interest in telemedicine during the COVID-19 era, many orthopaedic surgeons may be unfamiliar with clinical examination skills, patients’ safety, data security, and implementation-related concerns in telemedicine. We present a bibliometric analysis and review of the telemedicine-related publications concerning orthopaedics care during the COVID-19 pandemic. Such analysis can help orthopaedic surgeons become acquainted with the recent developments in telemedicine and its usage in regular orthopaedics practice.
Methods
We systematically searched the database of Thomson Reuters Web of Science for telemedicine-related articles in orthopaedics published during the COVID-19 pandemic. The selected articles were analysed for their source journals, corresponding authors, investigating institutions, countries of the corresponding authors, number of citations, study types, levels of evidence, and a qualitative review.
Results
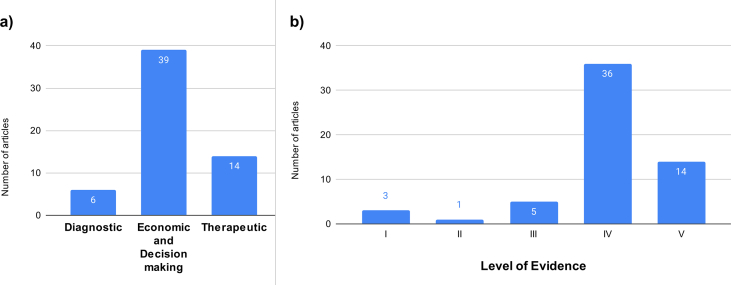
Fifty-nine articles meeting the inclusion criteria were published in 28 journals. Three hundred forty-two authors contributed to these research papers. The United States (US) contributed the most number of articles to the telemedicine-related orthopaedics research during the COVID-19 era. All articles combined had a total of 383 citations and 66.1% were related to the Economic and Decision-making Analyses of telemedicine implementation. By and large, level IV evidence was predominant in our review.
Conclusion
Telemedicine can satisfactorily cover a major proportion of patients' visits to outpatient departments, thus limiting hospitals’ physical workload. Telemedicine has a potential future role in emergency orthopaedics and inpatient care through virtual aids. The issues related to patient privacy, data security, medicolegal, and reimbursement-related aspects need to be addressed through precise national or regional guidelines. Lastly, the orthopaedic physical examination is a weak link in telemedicine and needs to be strengthened.
Keywords: Bibliometric analysis, COVID-19, Orthopaedics, Telemedicine, Trends
الملخص
أهداف البحث
في أعقاب الاهتمام الواسع النطاق مؤخرا بالتطبيب عن بُعد خلال حقبة كوفيد-١٩، قد لا يكون الكثير من جراحي العظام على دراية بمهارات الفحص السريري، وسلامة المرضى، وأمن البيانات، والمخاوف المتعلقة بالتنفيذ في التطبيب عن بُعد. نقدم تحليلا ببليومتريا ومراجعة للمنشورات المتعلقة بالتطبيب عن بُعد بشأن رعاية جراحة العظام أثناء جائحة كوفيد-١٩. يمكن أن يساعد هذا التحليل جراحي العظام على التعرف على التطورات الأخيرة في الطب عن بعد واستخدامه في ممارسة جراحة العظام العادية.
طرق البحث
بحثنا بشكل منهجي في قاعدة بيانات ثومسون رويترز ويب أوف ساينس عن المقالات المتعلقة بالتطبيب عن بعد في جراحة العظام التي نُشرت أثناء جائحة كوفيد-١٩. وتم تحليل المقالات المختارة لمجلات المصدر الخاصة بهم، والمؤلفين المراسلين، ومؤسسات البحث، ودول المؤلفين المراسلين، وعدد الاستشهادات، وأنواع الدراسة. كما تم عمل مراجعة نوعية وملخص لمستويات الأدلة.
النتائج
تم نشر ٥٩ مقالة تلبي معايير التضمين في ٢٨ مجلة. وأسهم ٣٤٢ مؤلفا في هذه الأوراق البحثية. ساهمت الولايات المتحدة بأكبر قدر في أبحاث جراحة العظام المتعلقة بالتطبيب عن بعد خلال حقبة كوفيد-١٩. واحتوت جميع المقالات على مجموع ٣٨٣ اقتباسا. وكان ٦٦.١٪ من الأوراق البحثية متعلقة بالتحليلات الاقتصادية وتحليلات القرار الخاصة بتطبيق التطبيب عن بعد. بشكل عام، كانت أدلة المستوى الرابع هي السائدة في مراجعتنا.
الاستنتاجات
يمكن أن يغطي التطبيب عن بعد بشكل مرض نسبة كبيرة من زيارات المرضى لأقسام العيادات الخارجية، وبالتالي يحد من عبء العمل البدني للمستشفيات. هناك دور محتمل للتطبيب عن بعد في رعاية جراحة العظام في حالات الطوارئ ورعاية المرضى الداخليين من خلال الوسائل الافتراضية. كما يجب معالجة القضايا المتعلقة بخصوصية المريض وأمن البيانات والطب القانوني والجوانب المتعلقة بالسداد من خلال الإرشادات الوطنية أو الإقليمية الدقيقة. أخيرا، الفحص البدني لجراحة العظام هو حلقة ضعيفة في التطبيب عن بعد ويحتاج إلى تعزيز.
الكلمات المفتاحية: التحليل الببليومتري, كوفيد-١٩, جراحة العظام, التطبيب عن بعد, الاتجاهات
Introduction
Telemedicine has emerged as a blessing in disguise during the ongoing COVID-19 pandemic.1,2 With the outburst of COVID-19 worldwide, the routine patient care of non-COVID-19 patients was bound to get affected. The majority of healthcare resources were channelised in managing COVID-19 affected patients who posed a national emergency in almost every country in the world. Most of the centres around the world had completely halted outpatient services and elective surgeries for an indefinite period.3 Furthermore, complete lockdowns as a part of the infection control strategy further reduced the non-COVID-19 patients’ access to healthcare services. As the nations started controlling the number of cases, the outpatient services gradually resumed in a controlled manner.4 However, several nations were gripped by the second wave of the pandemic, and the healthcare facilities were never restored to normal.5 The COVID-19 pandemic is the new normal, and we need to find ways to maintain quality patient care while exercising extreme caution against this unpredictable biohazard. The vaccination strategy can bring down the disease severity, but that does not provide absolute protection from getting infected and infecting others.
Telemedicine has been used as an alternative for outpatient care, rehabilitation, and even emergency room visits to reduce the physical interaction between patients and caregivers. The World Health Organization (WHO) defines telemedicine as the delivery of healthcare services by healthcare professionals using information and communication technologies for the exchange of valid information in which distance is a critical factor for the diagnosis, treatment, and prevention of disease and injuries, research, and evaluation as well as for accessing continuing education, all in the interests of advancing the health of individuals and their communities. Telemedicine has received a mostly positive response from patients as well as health caregivers. Currently, telemedicine is the need of the hour, even if the outpatient and elective surgeries have resumed to some extent.6 The norms of physical distancing and other infection control measures incur additional costs and time. The number of patients that a centre can cater to will automatically reduce with the requirement of more space and resources. Moreover, uncertainty regarding COVID-19 resurges remain, which might bring back all the restrictions again. Telemedicine appears to be a backup solution and an alternative plan for patient care during such scenarios.
In orthopaedics, bone and joint care include symptom evaluation, medical management, and specialised examination, reassessment, and rehabilitative measures. Further, decision-making regarding operative and nonoperative management is required through special assessment tools. Telemedicine is new for most orthopaedists, and thus, difficulties in patient evaluation and management may arise, especially when implemented on a large scale. Up-to-date knowledge about the trends and recent developments pertaining to telemedicine-based care during the COVID-19 pandemic can help orthopaedists improve their methods and skills in managing orthopaedic diseases. A bibliometric analysis helps explore the available evidence and prospects for future research by identifying the published contributions among authors, journals, institutions, and countries. We present a bibliometric analysis of the telemedicine-related publications concerning orthopaedic care during the COVID-19 pandemic.
Material and methods
We searched through the Thomson Reuters Web of Science database in May 2021 for the following specific keywords separated by the specified Boolean operators: (‘telemedicine’ or ‘telehealth’ or ‘mobile health’ or ‘mhealth’ or ‘electronic health’ or ‘ehealth’ or ‘electronic medicine’ or ‘emedicine’ or ‘virtual consultation’ or ‘remote consultation’ or ‘virtual clinic’) and (‘orthopaedics’ or ‘orthopaedic’ or ‘orthopedic’ or ‘orthopedics’ or ‘fracture’ or ‘fractures’ or ‘trauma’ or ‘bone’ or ‘joint’) under the ‘topic’ section without any language restriction. The ‘topic’ section covers wider results compared to the ‘all fields’ section. The search results were refined by placing them under the following broad categories: ‘orthopedics’ or ‘surgery’ or ‘rehabilitation’ or ‘sport sciences’, and the time frame was restricted to the years 2020 and 2021 considering the period during which the COVID-19 pandemic has been active. We then screened the titles and abstracts of the search results for articles discussing telemedicine within orthopaedics. Full texts of the publications where the abstract and titles did not specify telemedicine or its synonyms were checked for any telemedicine-related information. We excluded case reports, abstracts-only publications, letters, editorials, and the original articles and reviews not discussing telemedicine.
We used Bibliometrix R-package software for the data analysis.7 The included articles were analysed for their source journal, corresponding authorship, investigating institution, country of the corresponding author, and the number of citations. The articles were then categorised according to the type of study: a) Therapeutic Studies, b) Prognostic Studies, c) Diagnostic Studies, and d) Economic and Decision-making Analyses. Therapeutic Studies investigated the results of one or more treatment(s), prognostic studies investigated the outcomes of one or more disease(s), diagnostic studies investigated one or more diagnostic test(s), and economic and decision-making analyses dealt with developing economic or decision models.8 The level of evidence was assigned for all clinical articles using the Journal of Bone and Joint Surgery ranking system, updated in early 2015.8 Two senior authors then reviewed all the included articles for a qualitative review.
Results
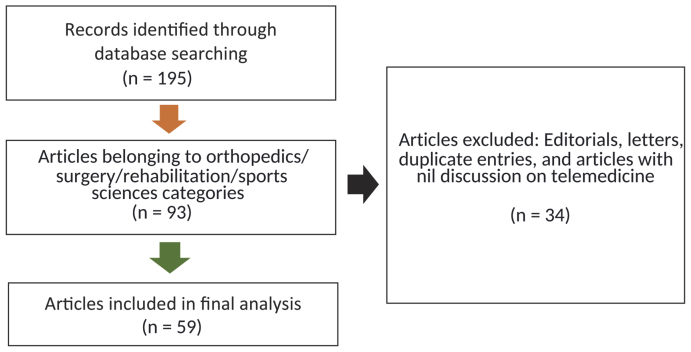
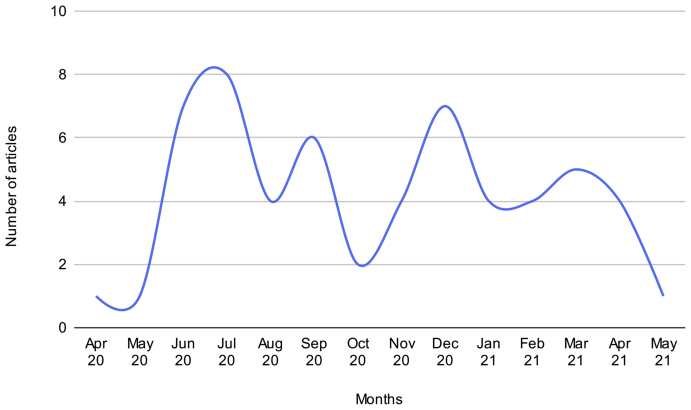
The search strategy yielded a total of 195 results, out of which 93 entries belonged to the predefined categories (orthopaedics/surgery/rehabilitation/sport sciences) and the time frame of 2020–2021. Fifty-nine articles met the inclusion criteria and were considered for the analysis.9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67 The excluded thirty-four papers were editorials, letters, duplicate entries, and articles with no discussion on telemedicine even in the full text (Figure 1). The monthly contributions trend of the orthopaedic telemedicine-related articles is shown in Figure 2.
Figure 1.
Modified PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram detailing the selection of the papers on telemedicine application in orthopaedics during the COVID-19 pandemic.
Figure 2.
The monthly number of orthopaedic telemedicine-related publications during the COVID-19 era.
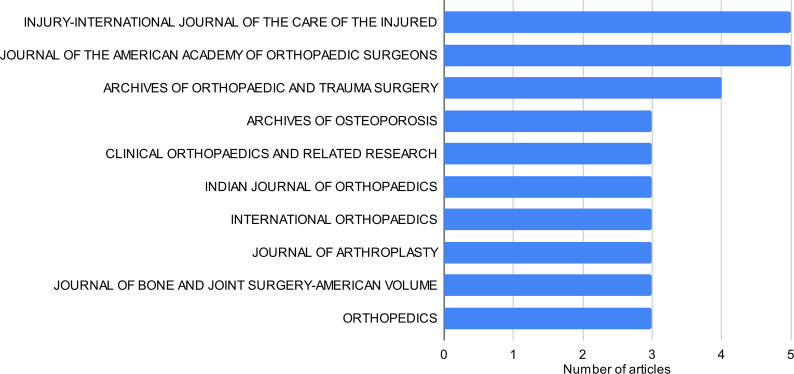
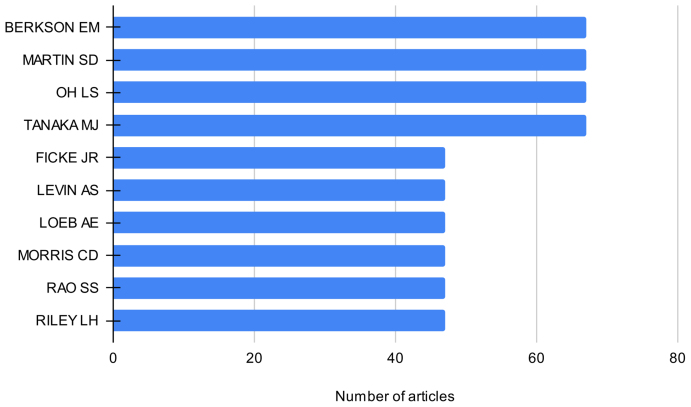
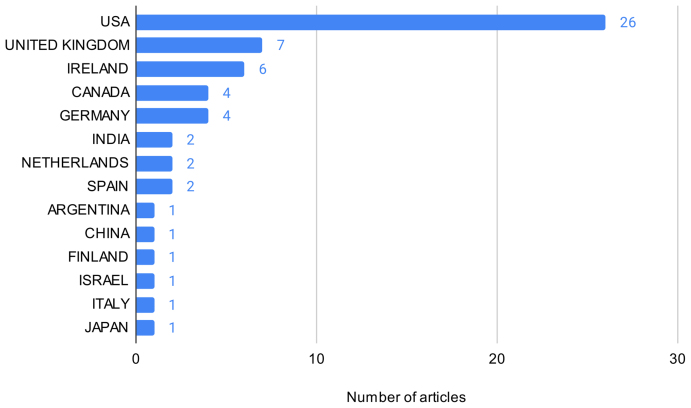
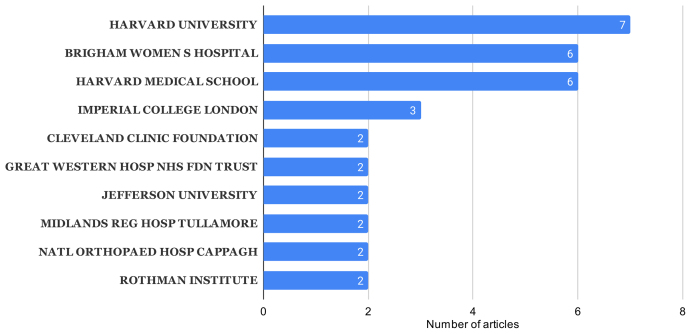
The articles discussing orthopaedic telemedicine were published in 28 journals. The top ten contributing journals are shown in Figure 3. The journals, Injury and Journal of the American Academy of Orthopaedic Surgeons carried the most number of orthopaedic telemedicine-related articles. Three hundred forty-two authors contributed, with 21 authors having two publications related to orthopaedic telemedicine. Figure 4 shows the top ten cited authors with orthopaedic telemedicine-related publications during the COVID-19 period. The United States (US) contributed the most number of articles to the orthopaedic telemedicine-related research with 26 articles (Figure 5). Among the top contributing institutions, Harvard University, Massachusetts (US) published the highest number of articles on orthopaedic telemedicine (Figure 6). The 59 published articles had a total of 383 citations, equivalent to 6.49 citations per article. The top ten cited articles are listed in Table 1. The majority of the research papers (66.1%) were related to the Economic and Decision Analyses of telemedicine implementation. The remaining papers belonged to therapeutic and diagnostic interventions (Figure 7a). The level of evidence of the research was predominantly level IV (Figure 7b).
Figure 3.
Top ten journals contributing to the papers on orthopaedic telemedicine during the COVID-19 pandemic.
Figure 4.
Top ten cited authors contributing to the papers on orthopaedic telemedicine during the COVID-19 pandemic.
Figure 5.
Top ten countries contributing to the papers on orthopaedic telemedicine during the COVID-19 pandemic.
Figure 6.
Top ten institutions/universities contributing to the papers on orthopaedic telemedicine during the COVID-19 pandemic.
Table 1.
Characteristics of the top ten cited papers on telemedicine application in orthopaedics during the COVID-19 pandemic.
| S. No. | Author (year) | Total citations | Study type | Number of patients reported | Key observations |
|---|---|---|---|---|---|
| 1. | Tanaka et al.64 (2020) | 66 | Expert opinion | Not provided | The authors highlighted the importance of proper camera positioning, audio-visual aids, and patient posture during telemedicine delivery. |
| 2. | Loeb et al.34 (2020) | 46 | Expert opinion | Not provided | The authors highlighted the importance of patient triage, technological resources, credentialing, education of providers and patients, scheduling, and regulatory considerations in telemedicine delivery. |
| 3. | Parisien et al.11 (2020) | 32 | Survey of residency programs | Not provided | Authors in a survey of orthopaedic residency programs found that 63.1% of them were providing telemedicine services. The authors stressed the need for telemedicine in academic orthopaedic institutions owing to the permanent pandemic-like situation. |
| 4. | Massey et al.41 (2020) | 30 | Expert opinion | Not provided | The authors observed telemedicine to be effective in the care of orthopaedic outpatients. Surgical priority, physical distancing, online clinical communications, and physician wellness governed inpatient care. |
| 5. | Awad et al.36 (2020) | 27 | Expert opinion | Not provided | In their evidence-based guidelines, authors recommended telemedicine and regarded it as virtual personal protective equipment. They emphasised preparation, practice, and following telemedicine start-up checklists to ensure effective implementation of telemedicine. |
| 6. | Kane et al.18 (2020) | 26 | Randomised controlled trial | 58 patients | Patients undergoing arthroscopic rotator cuff surgery could receive safe and effective early postoperative follow-up care using telemedicine. In addition, the preference for telehealth increased for both surgeons and patients following the first-hand experience. |
| 7. | O'Connor et al.42 (2020) | 23 | Expert opinion | Not provided | Authors found telemedicine to be an effective alternative even after the resumption of routine services. However, concerns regarding patient privacy and the need for further development and technological advances in telemedicine were also raised. |
| 8. | Makhni et al.43 (2020) | 16 | Expert opinion | Not provided | The authors discussed the factors that hindered the prior implementation of the telemedicine, which included lack of awareness, implementation costs, inefficiencies introduced, difficulty in performing physical examinations, overall lack of perceived benefit of virtual care, negative financial implications, concern for medicolegal liability, and regulatory restrictions. |
| 9. | Chhabra et al.44 (2020) | 9 | Expert opinion | Not provided | The authors found the role of telemedicine to be effective and encouraging. However, the limitations in developing countries due to connectivity issues and lack of awareness were highlighted. |
| 10. | Sultan et al.19 (2020) | 9 | Survey of patients with paediatric spinal deformity | 189 patients | Authors found that teleconsultations were a fast mode and satisfactory of care for paediatric spinal deformity patients comparable to physical visits. |
Figure 7.
a) Types of orthopaedic telemedicine-related research during COVID-19 pandemic. b) The level of evidence of the included research articles.
Discussion
Telemedicine is a hot topic in current orthopaedic practice in the COVID-19 era. It fulfils the need for patient care when physical visits can't be concluded due to the risk of infection spread. Telemedicine involves using electronic means (audio or visual) to provide clinical services to patients without a physical visit. Currently, telemedicine is frequently used for follow-up visits, management of chronic conditions, old age patients care, care of patients with difficult transportation needs, medication management, and remote patient care. The current analysis suggests that orthopaedic telemedicine has gained importance during the COVID-19 pandemic, as was evident from the consistent monthly contribution from May 2020 onwards. The contributed research appears to originate from different regions of the world, including American, European, and Asian countries, suggesting the need for telemedicine due to the rise in COVID-19 cases worldwide. However, most of the research papers have originated from the United States and some European nations. Previous familiarity with telemedicine, availability of resources, patient literacy, knowledge of operating telecommunication devices, patient awareness, healthcare infrastructure, and manpower, can all affect the implementation of telemedicine and could be the probable reasons behind its effective implementation in these countries. The articles were published in well-known journals, implying the importance of telemedicine during the COVID-19 pandemic as a topic of interest. The diversity of authors and institutes contributing to orthopaedic telemedicine research suggests the large-scale involvement of orthopaedists. The citations of the published papers also showed an increasing trend, indicating further ongoing research pertaining to orthopaedic telemedicine. Even though the interest in orthopaedic telemedicine is increasing, the current analysis suggests that it is yet to evolve. The current phase of widespread application of orthopaedic telemedicine is in its initial phase. Most of the evidence in the aforementioned period belonged to level 4 studies, and more than half of the studies belonged to the ‘economic and decision-making analyses’ category. Such studies deal with the effectiveness, feasibility, policies, feedback, decision making, resource allocation for implementation, and analysis of established and planned healthcare strategies.9 Thus, most clinical research deals with the effectiveness, feasibility, and patients'/doctors' perception of telemedicine.
Qualitative analysis
The evidence projected in the orthopaedic telemedicine related research during the COVID-19 era can be discussed under the following heads:
Implementation of telemedicine
The studies discussing the implementation of telemedicine in orthopaedics mainly discussed the application of audio-visual technology-based virtual care in orthopaedic out-patients, rehabilitation, fracture care, postoperative care, and health education. The main target of telemedicine implementation should be reducing the physical patient load without affecting patient care. The concept of virtual screening/E-triage/virtual fracture clinics addresses this target. Most of the studies presented the institutional experiences and surveys related to telemedicine implementation during the COVID-19 pandemic. The implementational studies addressed the following aspects of telemedicine-based care in orthopaedics:
Safety, feasibility, and effectiveness
Telemedicine is the necessary solution for patient care during the COVID-19 pandemic. Many studies and reviews mainly focused on analysing telemedicine's safety, feasibility, and effectiveness in orthopaedics. Most surveys reported widespread adoption of telemedicine as the main patient care modality.10, 11, 12, 13, 14, 15, 16, 17 Telemedicine can address the general and specialised needs of osteoporotic patients, paediatric deformities, fracture patients, and sports injuries.18, 19, 20, 21, 22, 23, 24, 25 High patient and doctor satisfaction has been recorded with telemedicine.26 It is found to be helpful in decision-making and telephone-based follow-up care.27,28
Screening tool
Several studies have found that a major proportion of orthopaedic injury patients visiting outpatient clinics and emergency rooms only require basic care and are discharged without the need for specialist consultation arising.29, 30, 31 Telemedicine-based care saves both cost and time in managing such patients. Telemedicine has emerged as an effective screening tool to categorise patients who require virtual consultation only and those who require physical evaluation. These services are required in high-volume centres where it is difficult to limit patient attendance due to the nature of disorders. Osteoporosis and its related morbidities and fracture care are two such fields. Lindsay et al.32 highlighted the importance of the E-triage system in osteoporotic patient care centres. These centres are usually overloaded due to the high volume of elderly osteoporotic patients. Secondly, these patients belong to the ‘at-risk’ population group. Therefore, they need appropriate assessment and management. Only 73.3% of patients needed the physical visit for a detailed evaluation. The remaining patients only needed investigative workup or direct discharge without the need for a physical visit. Direct discharge refers to the practice of discharging patients directly from the screening clinic without any expert consultation.31,32 Geerdink et al.31 advocated for a direct discharge approach via virtual fracture clinics where simple-stable injuries were discharged directly and managed with self-assisted splints or braces and phone-based health care.
Limitations in telemedicine implementation in orthopaedic care
While telemedicine is a convenient mode of patient care during the ongoing pandemic situation, it has some limitations and shortcomings. Medico-legal concerns, patient privacy, and secure patient data storage need to be streamlined to strengthen patients' and doctors’ trust in telemedicine. Gilbert et al.33 observed that teleconsultations had been rapidly deployed since the onset of the COVID-19 pandemic, often without clear guidance or consensus on many important issues. They identified legal and security issues in telemedicine implementation. Therefore, there is an urgent need to address these and develop local and national guidelines to facilitate telemedicine beyond the COVID-19 era. Zhang et al.,20 while supporting the effectiveness of telemedicine in orthopaedic patient management, highlighted the issues of missed or incomplete diagnosis and the absence of detailed patient counselling and monitoring as the main limitations of telemedicine. Guiroy et al.10 surveyed spine surgeons and observed that almost half of them were using telemedicine. However, the main concerns with telemedicine were the lack of physical examination that posed limitations in the management of their patients.
Review papers on the implementation of telemedicine in orthopaedics
A major chunk of the orthopaedic telemedicine-related papers published during the COVID-19 pandemic were review articles. The review articles touch on various aspects of telemedicine implementation, its advantages, and its limitations. Most of the reviews were narrative and were based on the authors' personal experiences and limited COVID-19-related literature. These review articles supported telemedicine as an alternative mode of patient care to physical outpatient visits.34, 35, 36, 37, 38, 39, 40 Most review articles critically analysed the available evidence to point out the limitations and ways to improve telemedicine. Loeb et al.34 suggested the need for proper utilisation of resources for telemedicine to be effective. The authors stressed strengthening telemedicine using patient triage, technological resources, credentialing, education of providers and patients, scheduling, and regulatory considerations during the pandemic. Massey et al.41 stressed the need for inpatient telemedicine as well, considering the limited workforce for specialities due to the COVID-19 pandemic. Awad et al.36 and O'Connor et al.42 advocated for strengthening telemedicine by adding more secured modalities to protect patients' confidentiality and keeping their medical records away from any anticipated breaches. A few authors discussed the factors limiting the implementation of telemedicine. These included lack of awareness, implementation costs, difficulty performing physical examinations, negative financial implications, concern for medicolegal liability, and regulatory restrictions.43,44 Hinckley et al.45 emphasised the need for regulatory mechanisms to keep the data secure and code the services to make telemedicine simpler and convenient for patients. Juhra et al.46 stressed on the legal considerations and reimbursement requirements before telemedicine consultations and the use of only certified software products for telemedicine conduction. Jansson et al.47 highlighted the need for higher-level evidence, technological innovation, and specialised patient-specific care for the at-risk population.
Therapeutic role of telemedicine in orthopaedics
These studies analysed the impact of telemedicine on the treatment of orthopaedic patients.
Clinical studies
Telemedicine was satisfactorily utilised in the care, decision making, and rehabilitation of general orthopaedic disorders, including fracture care, osteoporosis, spine disorders, sports injuries, arthroplasty patients, and post-operative care of patients.48, 49, 50, 51, 52, 53, 54 The common trends observed by the investigators were a significant reduction in inpatient visits, high patient satisfaction rates, and most importantly, timely care and referral of the patients requiring in-person evaluation.44,52,55 Hendrickson et al.56 observed better follow-up compliance among patients receiving post-discharge telemedicine-based care. The issues witnessed with orthopaedic telemedicine included limited physical examination and the need for a detailed in-person evaluation of patients with multiple comorbidities, advanced age, or obesity.57,58
Reviews articles
Similar to the reviews analysing telemedicine implementation in orthopaedics, the reviews on therapeutic aspects focused on the advantages and shortcomings of offering patient management through telemedicine in orthopaedics. The reviews supported the idea of telemedicine, considering it to be a cost-effective method of timely delivery of healthcare advice. At the same time, the authors raised concerns regarding inadequate physical examination, lack of proper supervised fracture care, improper brace application, deviation from treatment protocol and resulting complications, and limited application in moderate to severe disease patterns.59, 60, 61
Diagnostic studies
The diagnostic studies concerning telemedicine in orthopaedics mainly focused on the betterment of the physical examination which was highlighted by several studies as the main limitation.62,63 Tanaka et al.64 reported their experience of virtual examination through standardised manoeuvres for patients. The importance of proper camera positioning, audio-visual aids, and posture was emphasised. The authors found virtual video-based teleconsultations as an effective mode of treatment delivery for common outpatient orthopaedic conditions. Eble et al.65 presented a comprehensive virtual foot and ankle examination for telehealth visits, including instructions about patient convenient language. Goyal et al.66 recognised that assessment of motor, sensory, and special tests performed with telemedicine had similar observations to the traditional in-person examination. However, the authors stressed that the assessment needs to be administered by an experienced clinician. Rabin et al.67 observed that video examination of patients with shoulder disorders might present a valid alternative to face-to-face examination. However, the authors stressed that the video-based physical examination content might need to be modified to detect indications for specific interventions or diagnostic tests. The primary limitation of these studies is that the assessment tools need further validation.
Based on the above-stated qualitative analysis, it can be ascertained that telemedicine is the need of the hour and it has emerged as an effective alternative to conventional physical outpatient care. The main role of telemedicine lies in timely patient care and, at the same time, reducing the physical burden on hospitals. The virtual screening clinics can help differentiate patients requiring telemedicine-based care and those requiring in-person assessment. Therefore, the patients' and the hospitals’ time, cost, and resources are saved and channelised to patients requiring priority attention. The future scope of telemedicine lies in expanding telemedicine to various other health aspects such as inpatient care, rehabilitation, and remote aids to assist clinical assessment. In orthopaedics, the major limitations in telemedicine-based care are the lack of precise physical examination and inadequate assessment of at-risk populations such as old age patients, cases of osteoporotic fractures, and those with comorbidities. Measures to strengthen telemedicine skills and develop new technologies providing detailed objective assessment will help assist these patients. The studies concerning the physical examination of orthopaedic patients through telemedicine were very few. This deficiency highlights the need for more evidence that would enable appropriate physical examination of orthopaedic patients. Lastly, the orthopaedic assessment needs visual information and that too with details. Therefore, infrastructure development to provide high-speed patient to doctor connectivity, visual devices for clear picture and video transmission, and artificial intelligence-assisted examination will need to be set up in the future. Although based on our analysis, even though it is evident that telemedicine has a wide reach in developed and developing nations, the quality of telemedicine might need to be strengthened considering the limited orthopaedic evidence. Most of the studies were level IV studies, and very few addressed the therapeutic and diagnostic aspects. Therefore, more evidence is required for a sound recommendation of telemedicine use in orthopaedics.
There are some limitations in the current analysis. First, it is a cross-sectional study analysing evidence from the period when COVID-19 was active. Therefore, the past developments in orthopaedic telemedicine were not considered. Second, the bibliometric analysis is based on the results of one major scientific database. Therefore, there might be variations in the results of other databases. The data regarding citations were taken from the database statistics and minor variations from the actual citations counts may occur. Also, the database did not provide self-citation counts, which can affect the overall citation numbers. Third, the analysis is based on common keywords used for telemedicine, and the studies not covered under those keywords might have been missed. Lastly, the analysed articles were covered under orthopaedics, surgery, rehabilitation, and sport sciences-related journals. Therefore, studies outside these categories would have been missed. Nevertheless, the analysis fulfils the aim of studying the trend in orthopaedic telemedicine during the COVID-19 era, considering similar interests and concerns of the studies included.
Conclusions
The publication trends during the COVID-19 era suggest that telemedicine forms an integral model of outpatient care in orthopaedics considering the prolonged pandemic-like situation. Telemedicine can satisfactorily cover the major proportion of patients' visits to outpatient departments, thus limiting hospitals’ physical burden. Telemedicine has a potential future role in emergency orthopaedic care and inpatient care through virtual aids. The issues related to patient privacy, data security, medicolegal, and reimbursement-related aspects need to be addressed through precise national or regional guidelines. Lastly, the orthopaedic physical examination is the weak link in telemedicine and needs to be strengthened.
Recommendations
Based on the findings of the current analysis, we recommend the use of telemedicine in orthopaedics. However, efforts must be made to minimise the risk of a breach in patient privacy, data security, and patient mismanagements. Besides this, orthopaedists should follow appropriate national or regional guidelines to avoid medicolegal issues.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interests to declare.
Ethical approval
The authors confirm that this study was prepared in accordance with COPE rules and regulations. Given the nature of the study, the IRB review was not required.
Authors contributions
AK conceived and designed the study, conducted research, provided research materials, and collected and organised data. AK and SS performed the data acquisition and literature review. JJ and SK make relevant inferences based on the available data and formulated the discussion and conclusions. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Kumar S., Kumar A., Kumar M., Kumar A., Arora R., Sehrawat R. Feasibility of telemedicine in maintaining follow-up of orthopaedic patients and their satisfaction: a preliminary study. J Clin Orthop Trauma. 2020;11(Suppl 5):S704–S710. doi: 10.1016/j.jcot.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Valentino L.A., Skinner M.W., Pipe S.W. The role of telemedicine in the delivery of health care in the COVID-19 pandemic. Haemophilia. 2020;26(5):e230–e231. doi: 10.1111/hae.14044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moynihan R., Sanders S., Michaleff Z.A., Scott A.M., Clark J., To E.J., et al. Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open. 2021;11(3) doi: 10.1136/bmjopen-2020-045343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar A., Das S., Arora R., Kumar M., Kumar S., Jameel J. Resuming orthopaedic outpatient services in the current COVID-19 pandemic: an Indian perspective. J Bone Joint Dis. 2021;36(1):46–48. [Google Scholar]
- 5.Hafeez S., Din M., Zia F., Ali M., Shinwari Z.K. Emerging concerns regarding COVID-19; second wave and new variant. J Med Virol. 2021;93(7):4108–4110. doi: 10.1002/jmv.26979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jazieh A.R., Kozlakidis Z. Healthcare transformation in the post-coronavirus pandemic era. Front Med (Lausanne) 2020;7:429. doi: 10.3389/fmed.2020.00429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aria M., Cuccurullo C. Bibliometrix: an R-tool for comprehensive science mapping analysis. J Informetr. 2017;11(4):959–975. doi: 10.1016/j.joi.2017.08.007. [DOI] [Google Scholar]
- 8.Wright J.G., Swiontkowski M.F., Heckman J.D. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3. [PubMed] [Google Scholar]
- 9.Goeree R., Diaby V. Introduction to health economics and decision-making: is economics relevant for the frontline clinician? Best Pract Res Clin Gastroenterol. 2013;27(6):831–844. doi: 10.1016/j.bpg.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 10.Guiroy A., Gagliardi M., Coombes N., Landriel F., Zanardi C., Willhuber G.C., et al. COVID-19 impact among spine surgeons in Latin America. Global Spine J. 2020 doi: 10.1177/2192568220928032. 2192568220928032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Parisien R.L., Shin M., Constant M., Saltzman B.M., Li X., Levine W.N., et al. Telehealth utilization in response to the novel coronavirus (COVID-19) pandemic in orthopaedic surgery. J Am Acad Orthop Surg. 2020;28(11):e487–e492. doi: 10.5435/JAAOS-D-20-00339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lezak B.A., Cole P.A., Jr., Schroder L.K., Cole P.A. Global experience of orthopaedic trauma surgeons facing COVID-19: a survey highlighting the global orthopaedic response. Int Orthop. 2020;44(8):1519–1529. doi: 10.1007/s00264-020-04644-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peiro-Garcia A., Corominas L., Coelho A., DeSena-DeCabo L., Torner-Rubies F., Fontecha C.G. How the COVID-19 pandemic is affecting paediatric orthopaedics practice: a preliminary report. J Child Orthop. 2020;14(3):154–160. doi: 10.1302/1863-2548.14.200099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Earp B.E., Zhang D., Benavent K.A., Byrne L., Blazar P.E. The early effect of COVID-19 restrictions on an academic orthopedic surgery department. Orthopedics. 2020;43(4):228–232. doi: 10.3928/01477447-20200624-03. [DOI] [PubMed] [Google Scholar]
- 15.Luengo-Alonso G., Pérez-Tabernero F.G., Tovar-Bazaga M., Arguello-Cuenca J.M., Calvo E. Critical adjustments in a department of orthopaedics through the COVID-19 pandemic. Int Orthop. 2020;44(8):1557–1564. doi: 10.1007/s00264-020-04647-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Parnes N., Tousant C., Perrine J., DeFranco M.J. Outpatient orthopedic rehabilitation in New York state during the COVID-19 pandemic: therapist perspectives. Orthopedics. 2020;43(5):292–294. doi: 10.3928/01477447-20200721-16. [DOI] [PubMed] [Google Scholar]
- 17.Simon M.J.K., Regan W.D. COVID-19 pandemic effects on orthopaedic surgeons in British Columbia. J Orthop Surg Res. 2021;16(1):161. doi: 10.1186/s13018-021-02283-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kane L.T., Thakar O., Jamgochian G., Lazarus M.D., Abboud J.A., Namdari S., et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: a prospective, randomized controlled trial. J Shoulder Elbow Surg. 2020;29(4):775–783. doi: 10.1016/j.jse.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Sultan A.A., Acuña A.J., Samuel L.T., Rabin J.M., Grits D., Gurd D.P., et al. Utilization of telemedicine virtual visits in pediatric spinal deformity patients: a comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop. 2020;40(8):e712–e715. doi: 10.1097/BPO.0000000000001553. [DOI] [PubMed] [Google Scholar]
- 20.Zhang D., Blazar P., Benavent K., Earp B.E. The efficacy of orthopedic telemedicine encounters during the COVID-19 crisis. Orthopedics. 2021;44(2):e211–e214. doi: 10.3928/01477447-20210216-01. [DOI] [PubMed] [Google Scholar]
- 21.Rizzi A.M., Polachek W.S., Dulas M., Strelzow J.A., Hynes K.K. The new 'normal': rapid adoption of telemedicine in orthopaedics during the COVID-19 pandemic. Injury. 2020;51(12):2816–2821. doi: 10.1016/j.injury.2020.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manz W.J., Goel R., Fakunle O.P., Labib S.A., Bariteau J.T. Feasibility of rapid development and deployment of a telemedicine program in a foot and ankle orthopedic practice. Foot Ankle Int. 2021;42(3):320–328. doi: 10.1177/1071100720963059. [DOI] [PubMed] [Google Scholar]
- 23.Hughes A.J., Moloney D.P., Fraser C., Dembo J., O'Brien L., Corcoran M., et al. Remote delivery of the satellite virtual fracture clinic - a pilot report of the first 500 cases. Injury. 2021;52(4):782–786. doi: 10.1016/j.injury.2020.11.055. [DOI] [PubMed] [Google Scholar]
- 24.Dunkerley S., Thelwall C., Omiawele J., Smith A., Deo S., Lowdon I. Patient care modifications and hospital regulations during the COVID-19 crisis created inequality and functional hazard for patients with orthopaedic trauma. Int Orthop. 2020;44(12):2481–2485. doi: 10.1007/s00264-020-04764-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dunkerley S., Kurar L., Butler K., James M., Lowdon I. The success of virtual clinics during COVID-19: a closed loop audit of the British orthopaedic association (BOAST) guidelines of outpatient orthopaedic fracture management. Injury. 2020;51(12):2822–2826. doi: 10.1016/j.injury.2020.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Peeters J.J.M., van den Berg P., van den Bergh J.P., Emmelot-Vonk M.H., de Klerk G., Lems W.F., et al. Osteoporosis care during the COVID-19 pandemic in The Netherlands: a national survey. Arch Osteoporos. 2021;16(1):11. doi: 10.1007/s11657-020-00856-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murphy E.P., Fenelon C., Kennedy J.F., O’Sullivan M.D., Noel J., Kelly P.M., et al. Establishing a virtual clinic for developmental dysplasia of the hip: a prospective study. J Pediatr Orthop. 2021;41(4):209–215. doi: 10.1097/BPO.0000000000001755. [DOI] [PubMed] [Google Scholar]
- 28.Jella T.K., Samuel L.T., Acuña A.J., Emara A.K., Kamath A.F. Rapid decline in online search queries for hip and knee arthroplasties concurrent with the COVID-19 pandemic. J Arthroplasty. 2020;35(10):2813–2819. doi: 10.1016/j.arth.2020.05.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smithson K.B., Parham S.G., Mears S.C., Siegel E.R., Crawley L., Sachleben B.C. Transfers of pediatric patients with isolated injuries to a rural Level 1 Orthopedic Trauma Center in the United States: are they all necessary? Arch Orthop Trauma Surg. 2021 doi: 10.1007/s00402-020-03679-x. [DOI] [PubMed] [Google Scholar]
- 30.Siow M.Y., Walker J.T., Britt E., Kozy J.P., Zanzucchi A., Girard P.J., et al. What was the change in telehealth usage and proportion of No-show visits for an orthopaedic trauma clinic during the COVID-19 pandemic? Clin Orthop Relat Res. 2020;478(10):2257–2263. doi: 10.1097/CORR.0000000000001396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Geerdink T.H., Uijterwijk B.A., Meijer D.T., Sierevelt I.N., Mallee W.H., van Veen R.N., et al. Adoption of direct discharge of simple stable injuries amongst (orthopaedic) trauma surgeons. Injury. 2021;52(4):774–779. doi: 10.1016/j.injury.2020.11.026. [DOI] [PubMed] [Google Scholar]
- 32.Lindsay J.R., Lawrenson G., English S. A service evaluation of e-triage in the osteoporosis outpatient clinic-an effective tool to improve patient access? Arch Osteoporos. 2020;15(1):53. doi: 10.1007/s11657-020-0703-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gilbert A.W., Booth G., Betts T., Goldberg A. A mixed-methods survey to explore issues with virtual consultations for musculoskeletal care during the COVID-19 pandemic. BMC Musculoskelet Disord. 2021;22(1):245. doi: 10.1186/s12891-021-04113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Loeb A.E., Rao S.S., Ficke J.R., Morris C.D., Riley L.H., 3rd, Levin A.S. Departmental experience and lessons learned with accelerated introduction of telemedicine during the COVID-19 crisis. J Am Acad Orthop Surg. 2020;28(11):e469–e476. doi: 10.5435/JAAOS-D-20-00380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.D'Ambrosi R. Orthopedics and COVID-19: scientific publications rush. Indian J Orthop. 2020;54(Suppl 2):1–7. doi: 10.1007/s43465-020-00141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Awad M.E., Rumley J.C.L., Vazquez J.A., Devine J.G. Perioperative considerations in urgent surgical care of suspected and confirmed COVID-19 orthopaedic patients: operating room protocols and recommendations in the current COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):451–463. doi: 10.5435/JAAOS-D-20-00227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y., Zeng L., Yao S., Zhu F., Liu C., Di Laura A., et al. Recommendations of protective measures for orthopedic surgeons during COVID-19 pandemic. Knee Surg Sports Traumatol Arthrosc. 2020;28(7):2027–2035. doi: 10.1007/s00167-020-06092-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chatterji G., Patel Y., Jain V., Geevarughese N.M., Haq R.U. Impact of COVID-19 on orthopaedic care and practice: a rapid review. Indian J Orthop. 2021:1–14. doi: 10.1007/s43465-021-00354-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chaudhry H., Nadeem S., Mundi R. How satisfied are patients and surgeons with telemedicine in orthopaedic care during the COVID-19 pandemic? A systematic review and meta-analysis. Clin Orthop Relat Res. 2021;479(1):47–56. doi: 10.1097/CORR.0000000000001494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keshet D., Bernstein M., Dahan-Oliel N., Ouellet J., Pauyo T., Rabau O., et al. Management of common elective paediatric orthopaedic conditions during the COVID-19 pandemic: the Montreal experience. J Child Orthop. 2020;14(3):161–166. doi: 10.1302/1863-2548.14.200107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Massey P.A., McClary K., Zhang A.S., Savoie F.H., Barton R.S. Orthopaedic surgical selection and inpatient paradigms during the coronavirus (COVID-19) pandemic. J Am Acad Orthop Surg. 2020;28(11):436–450. doi: 10.5435/JAAOS-D-20-00360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.O'Connor C.M., Anoushiravani A.A., DiCaprio M.R., Healy W.L., Iorio R. Economic recovery after the COVID-19 pandemic: resuming elective orthopedic surgery and total joint arthroplasty. J Arthroplasty. 2020;35(7S):S32–S36. doi: 10.1016/j.arth.2020.04.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Makhni M.C., Riew G.J., Sumathipala M.G. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. 2020 Jul 1;102(13):1109–1115. doi: 10.2106/JBJS.20.00452. [DOI] [PubMed] [Google Scholar]
- 44.Chhabra H.S., Bagaraia V., Keny S., Kalidindi K., Mallepally A., Dhillon M.S., et al. COVID-19: current knowledge and best practices for orthopaedic surgeons. Indian J Orthop. 2020;54(4):1–15. doi: 10.1007/s43465-020-00135-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hinckley N.B., Henley M.B., McIntyre L., Stiefel E., Davidson J., Chhabra A. Orthopaedic documentation and coding primer for telemedicine and electronic patient communication for the COVID-19 pandemic. J Bone Joint Surg Am. 2020;102(13):1105–1108. doi: 10.2106/JBJS.20.00649. [DOI] [PubMed] [Google Scholar]
- 46.Juhra C., Ansorg J., Back D.A., John D., Kuckuck-Winkelmann A., Raschke M., et al. Online patient consultation. Z für Orthop Unfallchirurgie. 2020;158(4):345–350. doi: 10.1055/a-1192-7800. [DOI] [PubMed] [Google Scholar]
- 47.Jansson M.M., Hyvämäki P., Pikkarainen M. Computer- and telephone-delivered interventions on patient outcomes and resource utilization in patients with orthopaedic conditions: a systematic review and narrative synthesis. Orthop Nurs. 2020;39(5):340–352. doi: 10.1097/NOR.0000000000000699. [DOI] [PubMed] [Google Scholar]
- 48.Little M., Huntley D., Morris J., Jozsa F., Hardman J., Anakwe R.E. The virtual fracture clinic improves quality of care for patients with hand and wrist injuries: an assessment of 3709 patients. J Hand Surg Eur. 2020;45(7):748–753. doi: 10.1177/1753193420930610. [DOI] [PubMed] [Google Scholar]
- 49.Higgins J., Chang J., Hoit G., Chahal J., Dwyer T., Theodoropoulos J. Conventional follow-up versus mobile application home monitoring for postoperative anterior cruciate ligament reconstruction patients: a randomized controlled trial. Arthroscopy. 2020;36(7):1906–1916. doi: 10.1016/j.arthro.2020.02.045. [DOI] [PubMed] [Google Scholar]
- 50.El Ashmawy A.H., Dowson K., El-Bakoury A., Hosny H.A.H., Yarlagadda R., Keenan J. Effectiveness, patient satisfaction, and cost reduction of virtual joint replacement clinic follow-up of hip and knee arthroplasty. J Arthroplasty. 2021;36(3):816–822.e1. doi: 10.1016/j.arth.2020.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Crawford A.M., Lightsey H.M., Xiong G.X., Striano B.M., Schoenfeld A.J., Simpson A.K. Telemedicine visits generate accurate surgical plans across orthopaedic subspecialties. Arch Orthop Trauma Surg. 2021:1–8. doi: 10.1007/s00402-021-03903-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hughes A.J., Feeley I.H., Crowley M., Conlon B., Merghani K., Sheehan E.C. Upscaling virtual fracture clinic use is a safe, effective measure in the delivery of trauma care. J Orthop Trauma. 2020;34(9):e349–e352. doi: 10.1097/BOT.0000000000001894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Miller K.L., Steffen M.J., McCoy K.D., Cannon G., Seaman A.T., Anderson Z.L., et al. Delivering fracture prevention services to rural US veterans through telemedicine: a process evaluation. Arch Osteoporos. 2021;16(1):27. doi: 10.1007/s11657-021-00882-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Seward M.W., Antonelli B.J., Giunta N., Iorio R., Fitz W., Lange J.K., et al. Weight loss before total joint arthroplasty using a remote dietitian and mobile app: study protocol for a multicenter randomized, controlled trial. J Orthop Surg Res. 2020 Dec;15(1):1–8. doi: 10.1186/s13018-020-02059-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sugand K., Park C., Morgan C., Dyke R., Aframian A., Hulme A., et al. Impact of the COVID-19 pandemic on paediatric orthopaedic trauma workload in central London: a multi-centre longitudinal observational study over the “golden weeks”. Acta Orthop. 2020;91(6):633–638. doi: 10.1080/17453674.2020.1807092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hendrickson S.B., Simske N.M., DaSilva K.A., Vallier H.A. Improvement in outpatient follow-up with a postdischarge phone call intervention. J Am Acad Orthop Surg. 2020;28(18):e815–e822. doi: 10.5435/JAAOS-D-19-00132. [DOI] [PubMed] [Google Scholar]
- 57.Jaenisch M., Kohlhof H., Touet A., Kehrer M., Cucchi D., Burger C., et al. Evaluation of the feasibility of a telemedical examination of the hip and pelvis - early lessons from the COVID-19 pandemic. Z Orthop Unfall. 2021;159(1):39–46. doi: 10.1055/a-1289-0779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Takahashi T., Ae R., Minami K., Shibata M., Kubo T., Kosami K., et al. Willingness of patients with knee osteoarthritis to use telemedicine amid Sars-CoV-2 outbreak. Geriatr Orthop Surg Rehabil. 2020;11 doi: 10.1177/2151459320979974. 2151459320979974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Murphy E.P., Fenelon C., Murphy R.P., O’Sullivan M.D., Pomeroy E., Sheehan E., et al. Are virtual fracture clinics during the COVID-19 pandemic a potential alternative for delivering fracture care? A systematic review. Clin Orthop Relat Res. 2020 Nov;478(11):2610–2621. doi: 10.1097/CORR.0000000000001388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Davey M.S., Coveney E., Rowan F., Cassidy J.T., Cleary M.S. Virtual fracture clinics in orthopaedic surgery - a systematic review of current evidence. Injury. 2020;51(12):2757–2762. doi: 10.1016/j.injury.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 61.Petersen W., Karpinski K., Backhaus L., Bierke S., Häner M. A systematic review about telemedicine in orthopedics. Arch Orthop Trauma Surg. 2021:1–9. doi: 10.1007/s00402-021-03788-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Phuphanich M.E., Sinha K.R., Truong M., Pham Q.G. Telemedicine for musculoskeletal rehabilitation and orthopedic postoperative rehabilitation. Phys Med Rehabil Clin N Am. 2021;32(2):319–353. doi: 10.1016/j.pmr.2020.12.004. [DOI] [PubMed] [Google Scholar]
- 63.Scheidt S., Kehrer M., Jaenisch M., Goost H., Wirtz D.C., Burger C., et al. A feasibility pilot study on the use of telemedicine for the examination of the knee joint. Z Orthop Unfall. 2020 doi: 10.1055/a-1246-3615. [DOI] [PubMed] [Google Scholar]
- 64.Tanaka M.J., Oh L.S., Martin S.D., Berkson E.M. Telemedicine in the era of COVID-19: the virtual orthopaedic examination. J Bone Joint Surg Am. 2020 Jun 17;102(12):e57. doi: 10.2106/JBJS.20.00609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Eble S.K., Hansen O.B., Ellis S.J., Drakos M.C. The virtual foot and ankle physical examination. Foot Ankle Int. 2020;41(8):1017–1026. doi: 10.1177/1071100720941020. [DOI] [PubMed] [Google Scholar]
- 66.Goyal D.K.C., Divi S.N., Schroeder G.D., Pfeifer R., Canseco J.A., Bowles D.R., et al. Development of a telemedicine neurological examination for spine surgery: a pilot trial. Clin Spine Surg. 2020;33(9):355–369. doi: 10.1097/BSD.0000000000001066. [DOI] [PubMed] [Google Scholar]
- 67.Rabin A., Dolkart O., Kazum E., Wengier R., Goldstein Y., Maman E., et al. Shoulder assessment by smartphone: a valid alternative for times of social distancing. Arch Orthop Trauma Surg. 2021:1–7. doi: 10.1007/s00402-021-03762-x. [DOI] [PMC free article] [PubMed] [Google Scholar]