Abstract
Background:
In hip arthroscopy, the best capsular closure technique to prevent microinstability in some patients while preventing overconstraints in other patients has yet to be determined.
Purpose:
To evaluate the biomechanical effects of capsular repair, capsular shift, and combination capsular shift and capsular plication for closure of the hip capsule.
Study Design:
Controlled laboratory study.
Methods:
Eight cadaveric hips (4 male and 4 female hips; mean age, 55.7 years) were evaluated in 7 conditions: intact, vented, capsulotomy, side-to-side repair, side-to-side repair with capsular plication (interval closure between iliofemoral and ischiofemoral ligaments), capsular shift repair, and capsular shift repair with plication. Measurements, via a 360° goniometer, included internal and external rotation with 1.5 N·m of torque at 5° of extension and 0°, 30°, 60°, and 90° of flexion. In addition, the degree of maximum extension with 5 N·m of torque and the amount of femoral distraction with 40 N and 80 N of force were obtained. Repeated-measures analysis of variance and Tukey post hoc analyses were used to analyze differences between capsular conditions.
Results:
At lower hip positions (5° of extension, 0° and 30° of flexion), there was a significant increase in external rotation and total rotation after capsulotomy versus the intact state (P < .05). At all hip flexion angles, there was a significant increase in external rotation, internal rotation, and total rotation as well as a significant increase in maximum extension after capsulotomy versus capsular shift with plication (P < .05 for all). At all flexion angles, both capsular closure with side-to-side repair (with or without plication) and capsular shift without capsular plication were able to restore rotation, with no significant differences compared with the intact capsule (P > .05). Among repair constructs, there were significant differences in range of motion between side-to-side repair and combined capsular shift with plication (P < .05).
Conclusion:
At all positions, significantly increased rotational motion was seen after capsulotomy. Capsular closure was able to restore rotation similar to an intact capsule. Combined capsular shift and plication may provide more restrained rotation for conditions of hip microinstability but may overconstrain hips without laxity.
Clinical Relevance:
More advanced closure techniques or a combination of techniques may be needed for patients with hip laxity and microinstability. At the same time, simple repair may suffice for patients without these conditions.
Keywords: hip capsule, capsular repair, capsular shift, capsular plication, biomechanics
As consensus grows in use of hip arthroscopy as a procedure for hip preservation surgery, controversy still exists over management of the hip capsule. 4,6,10,14 During hip arthroscopy, a capsulotomy is often performed to help gain access to the central compartment. By piercing through the iliofemoral ligament, a capsulotomy connecting the portals penetrates through the strongest component of the hip capsule that is responsible for resisting anterior translation and external rotation of the hip. 8,9 In biomechanical studies, hip capsulotomy in comparison with an intact hip capsule has been shown to significantly increase internal rotation, external rotation, and total rotation. 7,12 Clinical studies are consistent with the laboratory data in that outcomes appear to be inferior if the capsulotomy is not closed. 10 Subluxation of the hip and dislocation of the hip after hip arthroscopy without capsular closure have been reported. 4,14 At the same time, partial repair of the hip capsule, in comparison with complete closure, has shown significantly inferior outcomes after hip arthroscopy. 6
Simple closure of the hip capsule, with a side-to-side repair, has been reported along with more advanced techniques of capsular management, including capsular shift and capsular plication. 10 Safran et al 11 described a capsular plication technique that involves an interval closure technique between the iliofemoral and ischiofemoral ligaments. Domb et al 5 described a capsular shift technique that involves advancing the lateral aspect of the hip capsule with respect to the medial edge. Advanced management of the hip capsule has been recommended for patients undergoing hip arthroscopy for borderline dysplasia or microinstability. Jackson et al 7 demonstrated, through a biomechanical model, that a capsular shift repair can be used to treat capsular laxity. However, the biomechanical effect of these advanced capsular management techniques has not been directly compared as a combination of different hip capsular closure techniques used in unison.
The importance behind these different capsular management techniques is underscored in patients with hip microinstability, as seen in borderline hip dysplasia or hip hypermobility with connective tissue disorders, where instability may become more pronounced after iatrogenic injury to the hip capsule during hip arthroscopy. The purpose of this study was to evaluate the biomechanical properties of a side-to-side capsular repair compared with a capsular shift, with or without the addition of a capsular plication, and how these procedures affect hip motion and hip distraction. The hypotheses were that (1) there will be no difference in hip motion or hip distraction between a side-to-side capsular repair or a capsular shift repair with or without a capsular plication and (2) the addition of a capsular plication will have no difference in hip motion and hip distraction compared with an intact capsular state.
Methods
Specimen Preparation
Four fresh-frozen cadaveric pelvises (8 hips) were used for the study. The specimens were procured from the University of California Willed Body Program. The mean donor age was 55.7 years (range, 42-73 years), and there were 4 male and 4 female hips. From each specimen, all tissues except the hip capsule were carefully dissected without violation of the capsule. Each femur was cut 13 cm from the top of the greater trochanter to allow adequate space for insertion of the intramedullary femoral rod. The pelvis was aligned in the hip testing system (Figure 1) with the anterior superior iliac spine (ASIS) and the pubic symphysis parallel with the superior-inferior axis. Similarly, the right and left ASIS were parallel with the medial-lateral axis. The defining local coordinate systems were based on 3 screws that were positioned on the lateral ilium and the anterior femur; these 3 screws were positioned on both the lateral ilium and anterior femur to show the proximal, distal, and medial orientation. During femoral distraction, these coordinate screws were used to determine the femoroacetabular position with a 3-dimensional digitizing system (Microscribe 3DLX; Revware Inc). The accuracy of the Microscribe system was 0.3 mm. After preparation of the specimens and between testing sessions, the specimens were kept moist and properly wrapped before storage. Once testing was completed, all specimens were completely dissected to evaluate for signs of arthritis in the femoroacetabular compartment.
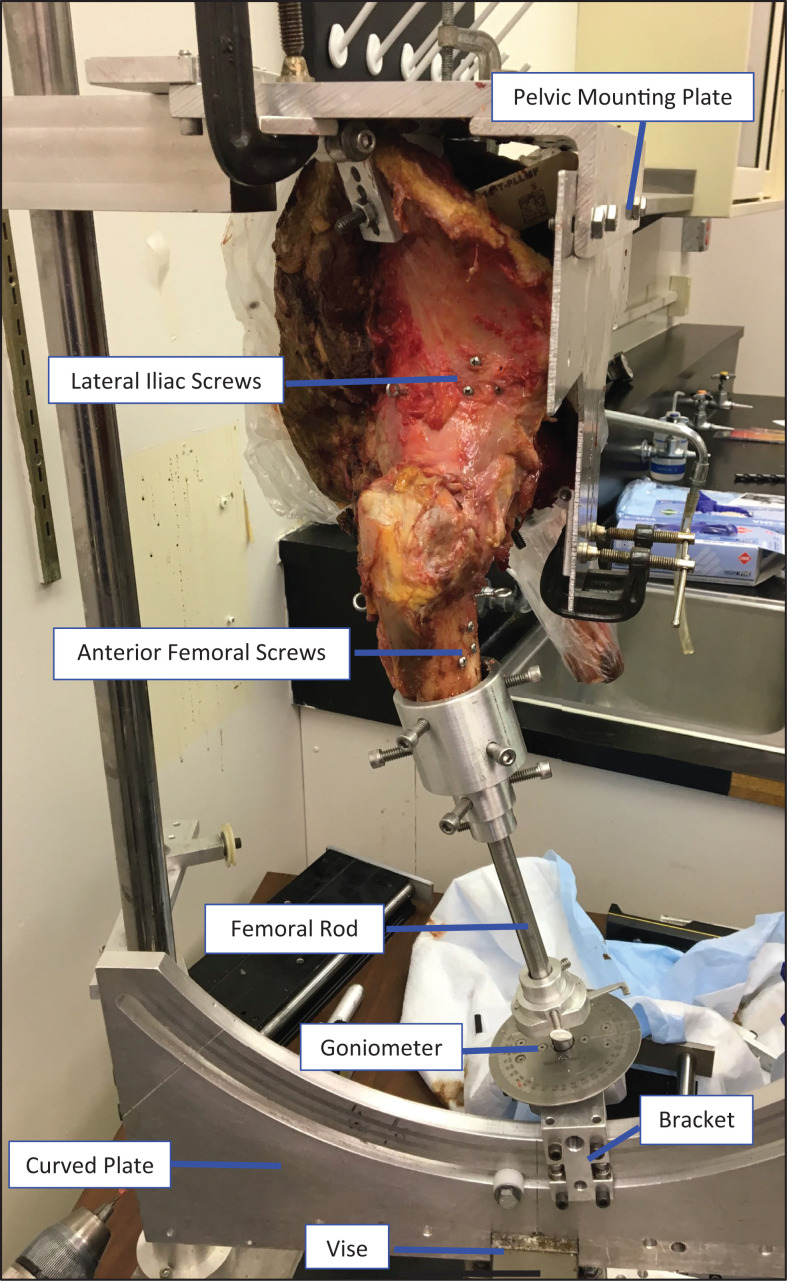
Figure 1.
Hip testing apparatus from lateral view of a right hip.
Testing Apparatus
A hip testing system, as previously described by Jackson et al, 7 was used to perform all biomechanical testing of each hip. In brief, the pelvis was mounted with the ASIS and pubic symphysis parallel with the superior-inferior axis. The right and left ASIS were parallel with the medial-lateral axis. Each femur was secured distally with an intramedullary rod that allowed 6 degrees of freedom. A curved plate and bracket were connected with the femoral intramedullary rod to allow free hip flexion and extension, internal and external rotation, and distraction in the proximal-distal axes of the femur. The arced plate was connected to 2 translating base plates; 1 translating plate allowed anteroposterior translation, the other translating plate allowed mediolateral translation. Each specimen, through use of the translating base plates, was uniquely adjusted to the specifications of each hip. At baseline, the femur was placed under 20 N of compressive loading with 10 N on the anterior femur and 10 N on the posterior femur.
Hip Rotation
Before testing, each specimen was preconditioned in internal rotation and external rotation by applying 1.5 N·m via a digital torque wrench. Measurements of rotation were made along the flexion and extension arc of the hip. Positions along this arc included 5° of extension and 0°, 30°, 60°, and 90° of flexion. Femoral rotational range of motion was measured with a 360° goniometer attached to the bracket on the arced plate, with 1.5 N·m applied to the distal rod via a digital torque wrench. A reference pin, positioned proximally to the goniometer, was placed in each intramedullary rod running through the femur. The relaxed position of each hip, 0°, was used to determine the neutral rotation of each specimen to ensure that the hip capsule was not under observable tension from external sources. Rotation of each hip, including maximum external and internal rotation, was measured by the position of the reference pin on the goniometer. Each testing condition and measurement was conducted on 2 trials, with a third trial performed if there was a difference of 1.0 mm or 2° between subsequent measurements.
Hip Distraction
The Microscribe 3-dimensional digitizing system was used to measure femoral distraction. With the femur in 15° of flexion, based on the hip testing jig, 0, 40, and 80 N of distraction were applied to the distal end of the femur, using the coordinate screws to measure distance between the femur and pelvis.
Testing Conditions
Each hip specimen underwent 7 testing conditions: intact state, vented capsule, capsulotomy, side-to-side repair, side-to-side repair with capsular plication, capsular shift repair, and capsular shift repair with capsular plication. Venting of the capsule was performed to control for effects seen with the loss of negative pressure.
The intact hip capsule was first tested for rotation (maximum internal rotation and maximum external rotation) with measurements conducted in increments of hip flexion (5° of extension, and 0°, 30°, 60°, and 90° of flexion), then it was tested for femoral distraction at both 40 and 80 N. Next, the vented capsule state was tested, with venting performed by entering a 22-gauge needle into the posterosuperior aspect of the hip capsule between the iliofemoral and ischiofemoral ligament. After venting and before testing subsequent conditions, markers were placed along the capsule using 3-0 nylon, to be used as guides to follow for the capsular repair techniques. This was done to determine the normal anatomically matched sides of the hip capsule before creating a hip capsulotomy. The third testing state consisted of a hip capsulotomy to replicate the capsulotomy typically performed during hip arthroscopy; the portal sites were connected using an incision starting 5 mm distal to the acetabular labrum and extending distally to the 4-o’clock position for a right hip and the 8-o’clock position for a left hip.
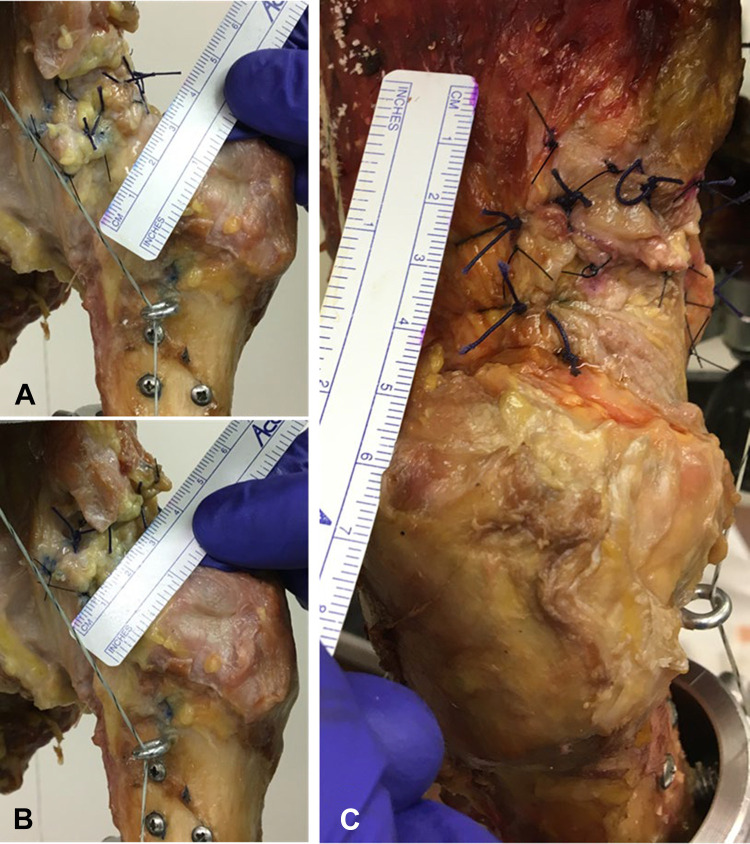
The fourth through seventh testing conditions had a randomized order of capsular closure techniques conducted between matched hip specimens. These subsequent testing conditions consisted of a side-to-side capsular repair with and without a capsular plication, and a capsular shift repair with and without a capsular plication. The intent behind these additional testing conditions was to reduce capsular redundancy and volume. Three techniques were tested in repair of the hip capsule (Figure 2). The first technique involved a simple side-to-side repair of the hip capsule using 1-0 Vicryl suture (Ethicon Inc), for a total of 5 knots with 3 separate suture constructs (Figure 2A). The second technique involved a capsular shift as described by Domb et al, 5 in which a suture was passed from the edge of the medial flap of the capsule then advanced 1 cm through the lateral aspect of the hip capsule. As a result, the advancement along the lateral aspect of the hip capsule allowed a superior shift of the iliofemoral ligament. Similar to the simple repair, a total of 5 knots using 1-0 Vicryl suture were used to create the capsular shift, with 3 separate suture constructs (Figure 2B). For the third technique of capsular closure, a capsular plication along the superior interval between the iliofemoral and ischiofemoral ligament, as described by Safran et al, 11 was performed. In reference to a left hip, this capsular plication was started at the 1-o’clock position and advanced, counterclockwise, to the 10-o’clock position. This distance spanned 2 cm, using 1-0 Vicryl suture, for a total of 5 knots with 2 separate suture constructs (Figure 2C).
Figure 2.
(A) Hip side-to-side capsular repair. (B) Hip capsular shift repair. (C) Hip plication.
Statistical Analysis
A repeated-measures analysis of variance was performed to compare rotational range of motion and femoral distraction between the different hip capsular repair constructs. Tukey post hoc analyses were performed to identify differences between intact, vented, capsulotomy, side-to-side repair, capsular shift repair, side-to-side repair with capsular plication, and capsular shift repair with capsular plication.
Results
Rotational motion of the hip between the intact state and after capsulotomy was significantly different at low hip flexion angles but not at high hip flexion angles. Specifically, under all hip flexion angles, maximum internal rotation was not found to be significantly different between the intact capsule and after capsulotomy. On the other hand, maximum external rotation was found to be significantly different between the intact state and capsulotomy state, with capsulotomy demonstrating significantly increased external rotation at 5° of extension and 0° and 30° of flexion (P < .05 for all) but not at 60° and 90° of flexion. For femoral distraction, there was no significant difference between the intact and capsulotomy conditions at both 40 and 80 N.
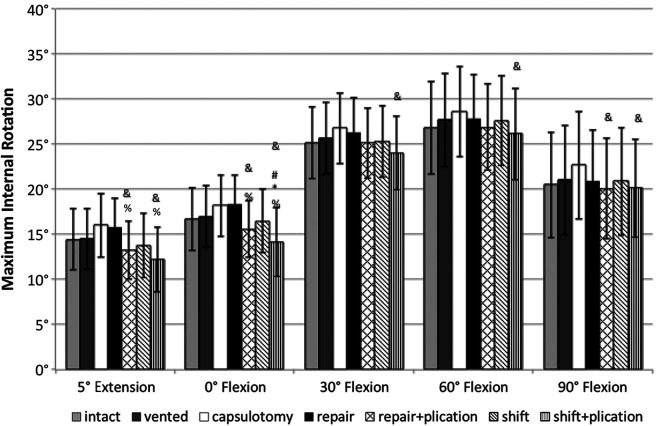
In evaluation of the different capsular repair techniques, maximum internal rotation was found to be significantly less for the side-to-side repair with capsular plication and the capsular shift repair with plication compared with the capsulotomy state at both 5° of extension and 0° of flexion (Figure 3). At higher hip flexion angles (30°, 60°, and 90°), maximum internal rotation was found to be significantly different only between capsulotomy and capsular shift repair with plication, with less internal rotation noted with the capsular closure technique. The addition of a capsular plication to a side-to-side repair was found to result in significantly less internal rotation compared with a side-to-side repair alone with the hip in 5° of extension and 0° of flexion.
Figure 3.
Comparison of internal rotation for the testing conditions. Statistically significant difference (P < .05): *versus intact; #versus vented; &versus capsulotomy; and %versus repair.
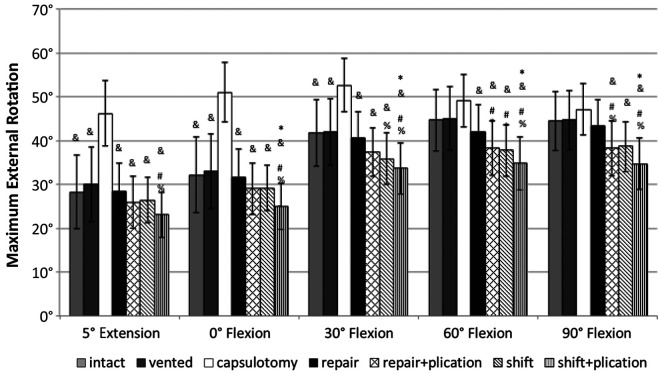
At all flexion angles, external rotation was found to be significantly different between side-to-side repair and capsular shift repair with plication, with less external rotation seen in the combined capsular closure technique (Figure 4). Compared with the intact hip capsule, only the capsular shift repair with the additional plication demonstrated a significant difference in external rotation at hip flexion angles of 0°, 30°, 60°, and 90°. This corresponds to a 22% decrease in external rotation at 0° and 30° of flexion and a 20% decrease in external rotation at 60° and 90° of flexion when capsular shift repair with plication is performed in comparison with the intact condition. When comparing capsular side-to-side repair without versus with capsular plication, a significant difference was found only in external rotation at 90° of flexion. There was no difference in external rotation at any hip flexion angle between capsular shift repair with versus without capsular plication.
Figure 4.
Comparison of external rotation for the testing conditions. Statistically significant difference (P < .05): *versus intact; #versus vented; &versus capsulotomy; and %versus repair.
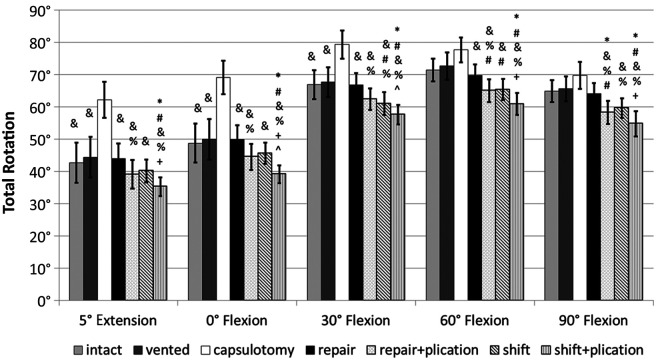
Compared with the intact hip capsule, total rotation (a summation of internal and external rotation) was found to be significantly different in only the capsular shift repair with plication condition at 5° of hip extension and all hip flexion angles (Figure 5). In comparison with the intact condition, capsular shift with plication resulted in lower hip rotation. This corresponds to an 18% decrease in total rotation at 5° of extension and 0° of flexion, and a 16% decrease in total rotation at hip flexion angles of 30°, 60°, and 90° when a capsular shift repair with additional plication is performed in comparison with the intact hip. Total rotation was found to be significantly different between capsular side-to-side repair with versus without capsular plication at all hip flexion angles. Similarly, total rotation was found to be significantly different between capsular shift repair with versus without capsular plication at 5° hip extension and hip flexion angles of 0°, 60°, and 90°. In both scenarios, the addition of capsular plication to either the side-to-side repair or capsular shift repair resulted in decreased total rotation.
Figure 5.
Comparison of total rotation for the testing conditions. Statistically significant difference (P < .05): *versus intact; #versus vented; &versus capsulotomy; %versus repair; +versus shift; and ^versus repair and plication.
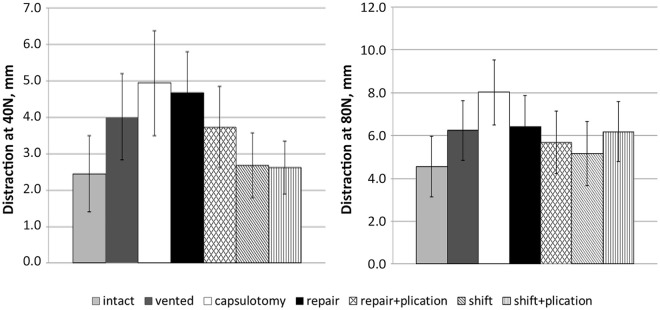
Femoroacetabular distraction, measured under both 40 and 80 N, was not found to be significantly different among any of the hip capsular closure techniques (Figure 6). At the conclusion of testing, dissection performed into the femoroacetabular joint did not find any significant arthritis changes, labral tears, or injury to the ligamentum teres. Equally important, no pathologic deformities of femoroacetabular impingement or hip dysplasia were identified.
Figure 6.
Comparison of distraction under 40 and 80 N for the testing conditions. No significant differences were detected.
Discussion
This biomechanical cadaveric study was performed to evaluate the effects of different capsular closure techniques on hip rotation and hip distraction in different hip joint positions. With attention to hip range of motion, no differences in internal rotation were found between the intact hip capsule and any of the hip capsular closure techniques. On the other hand, the side-to-side repair with or without plication and the capsular shift repair without capsular plication restored external rotation to the intact hip capsular state. At the same time, the only hip capsular closure technique that limits hip external rotation, compared with an intact hip capsule, was a capsular shift repair with capsular plication. A capsular shift repair with a capsular plication, also, was the only technique that had a significant difference in total rotation compared with the intact hip capsule. Most importantly, the addition of a capsular plication to either a side-to-side repair or a capsular shift repair demonstrated differences in total rotation for most hip flexion positions. Although there were no significant differences for femoroacetabular joint distraction, results for the capsular techniques involving a capsular shift repair more closely resembled that of the native intact hip capsule.
Our results on hip rotation were similar to those of previous cadaveric studies. In a study by Abrams et al, 1 total hip rotation increased after both an interportal capsulotomy and a T-shaped capsulotomy, with restoration of normal hip external rotation motion after capsular repair. In a similar fashion, Wuerz et al 13 revealed that larger capsulotomies resulted in greater increases in hip joint mobility; yet, complete closure of the hip capsule was able to restore motion in a comparable state to an intact hip capsule. Similarly, our results demonstrated that capsulotomy resulted in increased hip total motion, especially external rotation, with restoration of similar motion parameters after any of the capsular closure techniques. In a recent study by Baha et al, 2 hip kinematics at higher hip flexion angles (60° and 90°) were evaluated after either an interportal or T-capsulotomy. The T-capsulotomy showed a greater increase in motion and similarly, the repair of either capsulotomy reestablished the normal kinematics of an intact hip capsule. 2 In our study, higher degrees of hip flexion (60° and 90°) were evaluated with similar restoration of native hip kinematics after each of the hip capsular closure techniques. To emphasize, all of the capsular closure techniques evaluated in this study were tested with 2- to 3-suture constructs. Chahla et al 3 found that 2- and 3-suture constructs resulted in comparable biomechanical failure torques to external rotation after capsular repair from a hip capsulotomy.
In a study by Jackson et al, 7 a side-to-side repair was compared with a capsular shift repair for both an intact hip capsule and a hip instability model. In comparison of the 2 repair constructs, the only significant difference was noted for internal rotation at 5° of extension and 0° and 15° of flexion; however, there was no significant difference in external rotation. Likewise, there was no significant difference between the capsular shift repair and the capsular side-to-side repair constructs at both 40 and 80 N of distraction. This is important, as distraction testing during hip arthroscopy confirms hip instability, and patients with capsular laxity need less force for distraction. Along similar lines, during the late swing phase of walking, distractive forces place strain on the labrum, and a properly repaired capsule after hip arthroscopy may help minimize labral strain. In our study, we found a significant difference in internal rotation with the hip at 5° of extension and 0° of flexion when plication was added to either a side-to-side repair or capsular shift repair; however, there was no significant difference between a side-to-side repair and capsular shift when plication was not added to the repair construct. As seen in the study by Jackson et al, we also demonstrated that both a side-to-side repair and capsular shift repair were able to restore normal external rotation as seen in the native intact hip capsule. In contrast, the capsular shift repair with plication was the only construct that significantly reduced external rotation at all hip flexion angles and total rotation at all hip positions compared with intact hip capsule. Although not reaching statistical significance, a side-to-side repair with an additional capsular plication trended toward less total rotation in comparison with an intact hip capsule and demonstrated a significant difference in comparison with a side-to-side repair alone without additional plication.
The novelty of this study is the focus on a combination of capsular repair constructs used in tandem to repair a capsule after an interportal capsulotomy. Before this study, a capsule was repaired with only 1 type of repair construct and tested against another single repair construct. This study also adds the testing of advanced capsular repair constructs at higher degrees of hip flexion. Previous studies have focused testing of the advanced repair constructs at low levels of hip flexion (0°-45°), whereas this study augments testing of the constructs at hip flexion angles of 60° and 90°. Testing at this level provides information about potential implications to those patients undergoing capsular closure after hip arthroscopy who wish to return to sports participation that requires a high degree of hip flexion. Likewise, the results of this study have possible implications for capsular management following a capsulotomy conducted during hip arthroscopy. Specifically, the combination of capsular closure techniques may be beneficial for patients with microinstability from capsular laxity or borderline dysplasia. These advanced combination capsular closure techniques may have potential in those with impaired neuromuscular function or supraphysiologic laxity as indicated by an advanced Beighton score. Consideration for a combination closure of the hip capsule may be decided upon intraoperatively with identification of capsular redundancy, a thin capsule, or associated tear of the ligamentum teres. On the other hand, a combination capsular closure, especially a capsular shift repair with addition of a plication, may not be wanted for those without signs of capsular insufficiency, as this procedure would likely overconstrain motion of the hip. Further clinical studies evaluating these advanced capsular closure techniques on hip function and patient outcomes are needed.
Limitations
This study was affected by limitations of cadaveric biomechanical testing. To begin with, results are interpreted at time zero, which does not take into account potential physiologic loading and healing. This limited physiologic loading can limit the generalizability of the outcomes of this study, as the loading of the cadaveric hips does not approach the physiologic loading experienced during functional activities of the hip. The mean donor age of the specimens was 55.7 years, which is an older age for patients identified as potential candidates for hip preservation surgery. During testing, the hip was held in a neutral position, and different positions of hip abduction or adduction were not tested, thus limiting the application of these results to other possible positions of physiologic loading to the hip. Along these lines, translation of the hip, which could be a presentation of microinstability of the hip, was not able to be measured in this study. Additionally, all the capsular repair constructs were performed in an open environment, and not arthroscopically, thus limiting the potential feasibility of performing the combination of capsular closure techniques during hip arthroscopy. Finally, since our study was performed on 8 hips from 4 cadaveric pelvises, the study may have been underpowered. The limited number of specimens could lead to a bias.
Conclusion
The results of this study show that hip capsular closure was able to restore hip rotation and hip distraction similar to an intact hip capsule. An advanced combination of capsular closure techniques might provide more restrained rotation for conditions of hip microinstability but may overconstrain hips without laxity. Therefore, routine advanced combination closure of the hip capsule may not be the correct approach for all patients. Nevertheless, further clinical studies are required to evaluate the effects of advanced capsular management on hip function and patient-reported outcomes.
Footnotes
Final revision submitted March 21, 2021; accepted May 4, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.B. has received education payments from Arthrex, consulting fees from Stryker and Vericel, and nonconsulting fees from Arthrex, Smith & Nephew, and Vericel. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Abrams GD, Hart MA, Takami K, et al. Biomechanical evaluation of capsulotomy, capsulectomy, and capsular repair on hip rotation. Arthroscopy. 2015;31:1511–1517. [DOI] [PubMed] [Google Scholar]
- 2. Baha P, Burkhart TA, Getgood A, Degen RM. Complete capsular repair restores native kinematics after interportal and T-capsulotomy. Am J Sports Med. 2019;47(6):1451–1458. [DOI] [PubMed] [Google Scholar]
- 3. Chahla J, Mikula JD, Schon JM, et al. Hip capsular closure: a biomechanical analysis of failure torque. Am J Sports Med. 2016;45(2):434–439. [DOI] [PubMed] [Google Scholar]
- 4. Dierckman BD, Guanche CA. Anterior hip capsuloligamentous reconstruction for recurrent instability after hip arthroscopy. Am J Orthop (Belle Mead NJ). 2014;43:e319–e323. [PubMed] [Google Scholar]
- 5. Domb BG, Stake CE, Lindner D, et al. Arthrsocopic capsular plication and labral preservation in borderline hip dysplasia: two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41(11):2591–2598. [DOI] [PubMed] [Google Scholar]
- 6. Frank RM, Lee S, Bush-Joseph CA, et al. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoracetabular impingement: a comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. [DOI] [PubMed] [Google Scholar]
- 7. Jackson TJ, Peterson AB, Akeda M, et al. Biomechanical effects of capsular shift in the treatment of hip microinstability: creation and testing of a novel hip instability model. Am J Sports Med. 2015;44(3):689–695. [DOI] [PubMed] [Google Scholar]
- 8. Martin HD, Savage A, Braly BA, et al. The function of the hip capsular ligaments: a quantitative report. Arthroscopy. 2008;24:188–195. [DOI] [PubMed] [Google Scholar]
- 9. Myers CA, Register BC, Lertwanich P, et al. Role of the acetabular labrum and the iliofemoral ligament in hip stability: an in vitro biplane fluoroscopy study. Am J Sports Med. 2011;39:85S–91S. [DOI] [PubMed] [Google Scholar]
- 10. Ortiz-Declet V, Mu B, Chen AW, et al. Should the capsule be repaired or plicated after hip arthroscopy for labral tears associated with femoroacetabular impingement or instability? A systematic review. Arthroscopy. 2018;34(1):303–318. [DOI] [PubMed] [Google Scholar]
- 11. Safran MR, Giodano G, Lindsey DP, et al. Strains across the acetabular labrum during hip motion: a cadaveric model. Am J Sports Med. 2011;39(suppl):92S–102S. [DOI] [PubMed] [Google Scholar]
- 12. Stewart KJ, Edmonds-Wilson RH, Brand RA, Brown TD. Spatial distribution of hip capsule structural and material properties. J Biomech. 2002;35:1491–1498. [DOI] [PubMed] [Google Scholar]
- 13. Wuerz TH, Song SH, Grzybowki JS, et al. Capsulotomy size affects hip joint kinematic stability. Arthroscopy. 2016;32:1571–1588. [DOI] [PubMed] [Google Scholar]
- 14. Wylie JD, Beckmann JT, Aoki SK. Dislocation after hip arthroscopy for cam-type femoroacetabular impingement leading to progressive arthritis. JBJS Case Connect. 2015;5:e80. [DOI] [PubMed] [Google Scholar]