Abstract
Migraine is one of the most frequent causes of primary headache and 9% of children suffer from migraines. Most children will continue to experience migraine attacks as adults, therefore it is imperative that we have a thorough understanding of this major health issue. This article considers the so-called abdominal variants of migraine, which are more commonly seen in children rather than adults: abdominal migraine, cyclic vomiting syndrome, and infantile colic. Other functional abdominal pain disorders such as irritable bowel syndrome and functional dyspepsia have also been linked to migraine in clinical studies. The common pathophysiological root of these diseases seems to be the gut-brain axis mechanism. Abdominal variants of migraine are considered pediatric precursors of migraine whereas the functional abdominal pain disorders related to migraine seem to share a pathophysiological root with no temporarily link as for today. In this review we aim to describe the epidemiological background, the current pathophysiological theories and the relationship of each disease to migraine. This review is the first to compile abdominal variants of migraine and functional abdominal pain disorders associated with migraine and we endeavor to elucidate the broad spectrum of migraine-related episodes in children.
Keywords: Abdominal pain, Child, Gastrointestinal microbiome, Migraine disorders
Introduction
Migraine is one of the most frequent types of primary headache. In 2015, the Global Burden of Disease Study ranked it third as a cause of disability for men and women under 50 years of age.1 In 2017, the European prevalence of migraine was 20%, which was a 6% increase compared to 1997.2
In the pediatric population, the most recent epidemiological study3 estimated the prevalence of migraine to be 9.1%, and cross-sectional studies underline a constant increase of incidence of migraine with and without aura.4 Understanding the epidemiology and the prognosis of migraines in children and adolescents is important since the majority will continue to suffer into adulthood.3,5
Pediatric migraines differ from those experienced by adults, thus, their diagnosis can be challenging. Firstly, the diagnostic criteria are different:6 episodes are commonly bilateral (whereas they are typically unilateral for adults) and shorter (sometimes less than one hour, especially for young children).7 Secondly, we now acknowledge a broad spectrum of migraine-related episodes which are more frequently seen in children: abdominal migraine (AM), cyclic vomiting syndrome (CVS), and infantile colic.8 These episodes can have a great impact on the child’s and parent’s quality of life,9 particularly since migraineur children are frequently afflicted with other comorbidities. Obesity,10 atopy, or allergic disease,11 a dysfunctional family situation, a low level of physical activity and physical or emotional abuse have all been associated with migraine and to its onset or progression.12 The relationship between migraine and functional abdominal pain has been discussed at length among adults13-15 and identifies a connection between migraine and irritable bowel syndrome (IBS) and functional dyspepsia (FD), but further research is required among the pediatric population.16
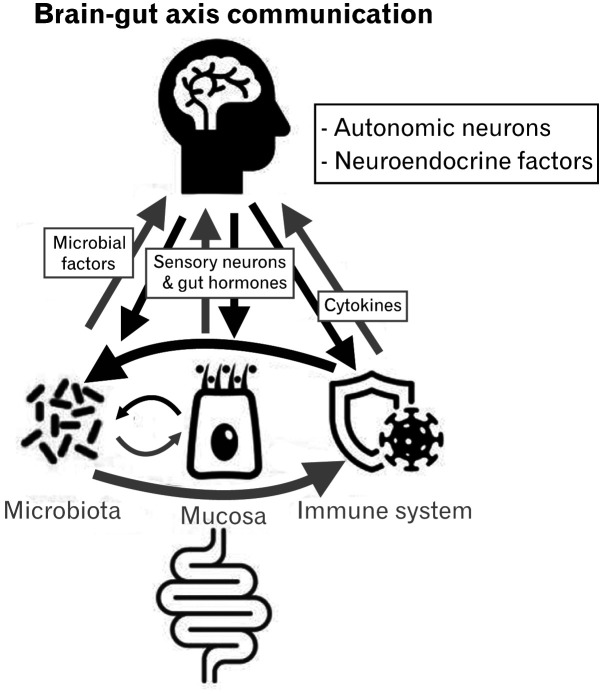
These studies are evidence for the scholarly interest in understanding the pathophysiology behind migraines. The pathophysiology of migraine is a multifactorial phenomenon,17 dependent on genetic factors (more than thirty migraine-associated gene polymorphisms have been discovered),18 environmental factors (such as medication, diet, and stress) and metabolic factors (examples include neuroendocrine function, the menstrual cycle, and pregnancy). The activation of the hypothalamus results in an alteration in thalamo-cortical circuits and brain connectivity, which subsequently leads to calcitonin gene-related peptide (CGRP) and pituitary adenylate cyclase-activating polypeptide (PACAP) release. The release of PACAP triggers intra-cerebral vasodilatation, ultimately causing the symptoms of migraine. Today, the role of CGRP in the gut-brain axis bidirectional communication is well recognized: CGRP has an antimicrobial action on gut bacterial strains (for instance, Escherichia coli, Enterococcus faecalis, and Lactobacillus acidophilus) and dysbiosis can increase the secretion of CGRP.19 The communication of the gut immune system, mucosa, and microbiota with the brain has been recently explored in great depth within the field of migraine research, particularly the association between functional abdominal pain disorders and migraine.19,20 The main communication pathways of the gut-brain axis are represented in Figure.
Figure.
Gut-brain axis communication. Brain-gut communication describes the bidirectional messages from brain to gut microbiota, mucosa and immune system and vice versa, as well as the communication of the microbiota with the mucosa and the gut immune system. Microbial factors, gut hormones, sensory neurons, and cytokines can modify cerebral function. Autonomic neurons and neuroendocrine factors can modify the gut behavior in return.
The diagnosis of migraine, its abdominal variants and functional abdominal pain can be challenging as they are often associated with each other. Early diagnosis is a good prognostic indicator of recovery for children and adolescents suffering from functional abdominal pain21 and migraines,5 thus the recognition of those conditions can have a great impact on children’s quality of life.
To date, reviews have studied either the association of abdominal variants or the functional abdominal pain disorders with migraine (Table 1).13,22-30 In this review, we aim to define the different abdominal variants of migraine (AM, CVS, and infantile colic) and the functional abdominal pain disorders associated with migraine (IBS and dyspepsia) (Table 2), to describe their relation to migraine (Table 3), their epidemiology and their evolution within the pediatric population, and finally to discuss current therapeutic management.
Table 1.
Previous Reviews on Abdominal Variants of Migraine and Functional Abdominal Pain Disorders’ Association to Migraine
| Subject of study | Study | Authors | Year of publication |
|---|---|---|---|
| Abdominal variants of migraine | Migraine and childhood periodic syndromes in children and adolescents | Gelfand22 | 2013 |
| Pediatric migraine and episodic syndromes that may be associated with migraine | Spiri et al23 | 2014 | |
| Migraine equivalents as part of migraine syndrome in childhood | Tarantino et al 24 | 2014 | |
| Migraine variants or episodic syndromes that may be associated with migraine and other unusual pediatric headache syndromes | Rothner and Parikh25 | 2016 | |
| Recurrent gastrointestinal disturbance: abdominal migraine and cyclic vomiting syndrome | Irwin et al26 | 2017 | |
| Cyclic vomiting syndrome | Cyclic vomiting syndrome and migraine in children | Lin et al27 | 2011 |
| Infantile colic | The relation between migraine and infantile colic: a systematic review and meta-analysis | Gelfand et al28 | 2015 |
| The link between infantile colic and migraine | Qubty and Gelfand29 | 2016 | |
| Relation between infantile colic and migraine as well as tension-type headache: a meta-analysis | Zhang et al30 | 2019 | |
| Functional gastrointestinal disorders | Migraine associated with gastrointestinal disorders: review of the literature and clinical implications | van Hemert et al13 | 2014 |
Table 2.
Abdominal Variants of Migraine and Functional Abdominal Pain Disorders Associated to Migraine
| Pathology | Clinical definition | Source |
|---|---|---|
| Abdominal migraine | Episodic central abdominal pain, usually lasting > 1 hour | Adapted from ICHD-3ba and Rome IV classification |
| Episodes interfere with normal activity | ||
| Episodes occur with one or more of pallor, anorexia, nausea, vomiting, photophobia, and headache, or are associated with other episodic syndromes (particularly cyclic vomiting syndrome and migraine limb pain) | ||
| The person is well between episodes and has a normal physical and developmental examination | ||
| Cyclic vomiting syndrome | Recurrent episodic attacks of intense nausea and vomiting, usually stereotypical in the individual and with predictable timing of episodes | ICHD-3ba criteria |
| Attacks may be associated with pallor and lethargy | ||
| There is a complete resolution of symptoms between attacks | ||
| The diagnostic criteria include all of the following: | ||
| Nausea and vomiting occurring at least 4 times per hour | ||
| Attacks lasting from 1 hour up to 10 days | ||
| Attacks occurring 1 week apart | ||
| Infantile colic | A. Recurrent episodes of irritability, fussing, or crying from birth to 4 months of age, fulfilling criterion B: | ICHD-3ba criteria |
| B. Both of the following: | ||
| Episodes last for 3 hours per day | ||
| Episodes occur on 3 days per week for 3 weeks | ||
| Not attributed to another disorder | ||
| Irritable bowel syndrome | Abdominal pain at least 4 days per month associated with one or more of the following: | Rome IV classification |
| Related to defecation | ||
| A change in frequency of stool | ||
| A change in form (appearance) of stool | ||
| In children with constipation, the pain does not resolve with resolution of the constipation (in this case, the child has functional constipation) | ||
| After appropriate evaluation, the symptoms cannot be fully explained by another medical condition | ||
| Functional dyspepsia | One or more of the following symptoms at least 4 days per month: | Rome IV classification |
| Postprandial fullness | ||
| Early satiation | ||
| Epigastric pain or burning not associated with defecation | ||
| After appropriate evaluation the symptoms cannot be fully explained by another medical condition |
aInternational classification of headache disorders (ICHD)-3 (beta version).
Table 3.
Pathophysiological, Clinical, and Temporal Relation of Abdominal Migraine, Cyclic Vomiting Syndrome, Infantile Colic, Irritable Bowel Syndrome, and Functional Dyspepsia With Migraine
| Pathology | Common physiopathology | Common clinical features | Temporal course |
|---|---|---|---|
| Abdominal migraine | Gastric motility alteration | Triggering/relieving factors | Precursor of migraine in adulthood |
| Increased gut permeability | Family history of migraine | ||
| Cyclic vomiting syndrome | Neuronal hyperexcitation | Anxiety/depression in personal or family history | Precursor of migraine in adulthood |
| Gastric motility alteration | |||
| Infantile colic | Microbiota modification | Anxiety/depression in personal or family history | Precursor of migraine in adulthood |
| Increased gut inflammation and permeability | Family history of migraine | ||
| Irritable bowel syndrome | Visceral hyperalgesia | Amelioration of symptoms with FODMAPs exclusive regime | Co-occurrence with migraine |
| Increased gut permeability and immune-allergic response | Anxiety/depression in personal or family history | ||
| Functional dyspepsia | Gastric motility alteration | Anxiety/depression in personal history | Co-occurrence with migraine |
| Visceral hyperalgesia | |||
| Increased immune-allergic response |
FODMAPs, fermentable oligosaccharides, disaccharides, monosaccharides, and polyols.
Abdominal Variants of Migraine
AM, CVS, and infantile colic are gastrointestinal episodic syndromes classified as variants of migraine by the international classification of headache disorders (ICHD)-3 (beta version).8 Among the episodic syndromes, we also acknowledge benign paroxysmal vertigo and benign paroxysmal torticollis, but these 2 conditions will not be discussed here as they do not involve the gastrointestinal tract.
Abdominal Migraine
AM has been described in children since 1984 by Symon and Russel31 and is now part of both the ICHD classification, and the Rome IV classification.32 The diagnosis of AM can be challenging as it is at the crossroads of multiple organ’s symptomatology. A positive clinical diagnosis of AM avoids unnecessary treatments and investigations.
A pragmatic clinical definition of AM in children is given by Angus-Leppan et al33 in 2018, adapted from definitions of Symon and Russel,31 ICHD-3 beta,8 and Rome IV32: (1) episodic central abdominal pain, usually lasting > 1 hour, (2) episodes interfere with normal activity, (3) episodes occur with one or more of pallor, anorexia, nausea, vomiting, photophobia, headache, or are associated with other episodic syndromes (particularly CVS well between episodes), and (4) normal physical and developmental examination.
Children with AM report similar triggers (stress and fatigue) and relieving factors (rest and sleep) to migraineurs.34 One key to the diagnosis is the absence of headache during episodes. Vomiting symptoms are also less severe than in CVS. The prevalence of AM is generally reported to be around 5% to 9% of the pediatric population34,35 but increases in children with a family history of migraine or depression.34-37 It is also higher among girls, with a reported sex ratio around 1.6/1 in Abu-Arafeh‘s first prevalence study in 1995.34
In the adult population, the diagnosis of AM remains very uncommon and few case reports have been published to date.38 Roberts and deShazo39 reported a cohort of 13 patients (11 from the medical literature and 2 from their clinic) and analyzed their symptoms by the IHCD-2 and the Rome III classifications of pediatric AM: 10 of their patients met some criteria for AM. Ninety percent of them had a family history of migraine.39 Their findings suggest considering AM in the differential diagnosis of recurrent abdominal pain in adults, especially if a family history of migraine is observed.
With respect to the pathophysiology hypothesis, in 2016, Devanarayana et al40 studied gastric motility of AM patients compared with control patients and showed that gastric and antral motility parameters were significantly lower in children with AM. They also noticed a significant correlation between symptom severity and gastric motility, a field of study within gut-brain axis diseases since it aids our understanding of the central innervation of the gut. Moreover, alteration of gut permeability has been proven in AM patients. In a study of 11 AM patients and 9 control children, Bentley et al37 showed that the mucosal permiability of small intestine was increased in AM patients. Furthermore, they longitudinally followed 3 AM patients and noticed a decrease in gut permeability correlated to the improvement of the AM symptoms. In some patients, the mucosal response to food allergens evidently seemed to trigger AM.37 The communication between the enteric and the central nervous system (CNS), best known as the gut-brain axis, helps us to understand how these intestinal changes are related to migraine.41
Children with AM have an excellent prognosis, with a majority demonstrating complete resolution of symptoms. It is unclear what causes AM to persist into adulthood since there are few case reports and small sample sizes.39 Although AM symptoms ultimately tend to evanesce, almost 70% of children will go on to develop classic migraine or recurrent abdominal pain syndrome.42,43
AM is now considered to be a pediatric precursor of migraine, consequently experts tend to extrapolate the usual migraine treatment to AM. However, to date, only 1 randomized control trial has been published within the field of pediatrics: pizotifen (a serotonin agonist) reduces the duration and the severity of AM when used as a preventive treatment44 Retrospective data on propranolol (a b blocker), cyproheptadine (an antihistamine), and flunarizine (a calcium channel blocker) as preventive therapies also seem to show a reduction in the frequency and severity of AM episodes.33 Lifestyle modifications are also recommended to prevent migraine crises.
Cyclic Vomiting Syndrome
CVS is part of the episodic syndromes associated with migraine as defined by the ICHD-3b classification.8 The symptoms of CVS are very typical and have been recently defined as8: (1) recurrent episodic attacks of intense nausea and vomiting, usually stereotypical to the individual and with predictable timing of episodes, (2) attacks may be associated with pallor and lethargy, and (3) there is a complete resolution of symptoms between attacks.
The diagnostic criteria include all of the following: (1) nausea and vomiting occurring at least 4 times per hour, (2) attacks lasting from 1 hour up to 10 days, and (3) attacks occurring 1 week apart.
The prodromal phase is characterized by intense nausea, pallor, tiredness, and abdominal pain. The vomiting phase is very intense within the first hour with a median frequency of 6 vomiting episodes per hour, declining during the next 4 hours to 8 hours. The recovery phase begins with the remission of nausea, continuing until recovery of appetite and strength. In 75% of children, the attacks begin between midnight and early morning.45
The prevalence of CVS is estimated between 0.3%46 and 6.1%47 making it less frequent in the pediatric population than migraine or AM. The pathophysiology of CVS remains unclear but different possibilities have been researched recently. Mitochondrial abnormalities have been explored as a maternal inheritance of CVS and 2 mitochondrial polymorphisms have been found to be highly associated with migrainous headaches and CVS.48 As with the migrainous pathophysiology, hypothalamic function is also influential in CVS as the control center of the CNS. In 2016, Ellingsen et al49 published the first functional MRI study to characterize altered brain connectivity in the insular cortex, the region of the brain involved in disease mechanisms responsible for both CVS and adult migraine. Autonomic dysfunction studies show a strong correlation between CVS, postural orthostatic tachycardia and an aberrant heart rate variability.50 Gastric motility has been explored in pediatric and adult patients suffering from CVS or migraine and mostly shows acceleration of gastric emptying, which implies altered autonomic function.
In comparison to AM, CVS has also been explored in the adult population and it is interesting to compare these cohorts. As children mature, their symptoms generally ameliorate or resolve; attacks become less intense and shorter in duration. In a Taiwanese pediatric study,51 9 out of 24 patients were symptom-free 4 years after diagnosis. On the other hand, newly diagnosed adult patients tend to have longer and more intense episodes than children52 but the vomiting pattern previously described remains consistent.53 Time to diagnosis is around 2 years for children whereas it is around 8 years for adults. The quality of life of CVS school-age children is often significantly affected; 85% had absences from school in the previous year due to their condition.45 An early diagnosis improves the quality of life of children suffering from CVS.54 Considering these data, the psychiatric profile of CVS patients has also been explored,55 with 1 study finding that 47% of children with CVS suffer from anxiety disorders. It is important to note that in this study parents reported significantly more psychiatric symptoms in their children than the children themselves. The hypothesis of anxiety transmission has also been explored for migraine and infantile colic.
The treatment of CVS in children is the same as for migraine: lifestyle modifications, plus medical management such as propranolol, flunarizine or mirtazapine, or anticonvulsants such as topiramate, phenobarbital, or levetiracetam. Antiemetic treatment such as aprepitant can also be used as a preventive treatment in CVS.56
Prognostically, it has been demonstrated that between 30% and 50% of CVS patients will develop migraines,57 with children diagnosed at an early age and those with more severe symptoms being the most likely to become migraineurs. Moreover, the clinical features (nausea, vomiting, and phono-photo-phobia), the periodicity, the triggers (stress and sleep deprivation) allow us to consider CVS as an equivalent and a precursor of migraine in children.
Infantile Colic
Infantile colic has recently been added to the ICHD classification, first appearing in the 2013 ICHD-3b.8 Infantile colic was first described and characterized by Wessel et al58 in 1954 to describe the “paroxysmal fussing” of infants under 4 months of age. It describes “paroxysmal fussing” or “infantile colic” as “possibly one of the earliest somatic responses to the presence of tension in the environment” leading to years of understanding infantile colic as a type of psychosomatic disorder. The ICHD classification’s diagnosis criteria are as follows: (1) A. Recurrent episodes of irritability, fussing, or crying from birth to 4 months of age, fulfilling criterion B; (2) B. Both of the following: episodes last for 3 hours per day and episodes occur on 3 days per week for 3 weeks; and (3) not attributed to another disorder.
A systematic review and meta-analysis of 2017 by Wolke et al59 studied the prevalence and crying duration of infantile colic and reported a high prevalence, 17-25%, of infantile colic under 6 weeks, decreasing shortly after 6 weeks to 11% and to 0.6% by 10-12 weeks.
The pathophysiology of infantile colic is also a good model of the gut-brain axis mechanism. The influence of microbiota on infantile colic has been investigated by means of stool studies60 and on the effect of intrapartum61 or neonatal antibiotic treatment.62 These studies show an increased risk of infantile colic for children who were administered antibiotics at birth or in the first week. It is widely recognized that antibiotic treatment modifies the gut and vaginal microbiota, and a review by Zeevenhooven et al63 studying children with colic identified a lower diversity in their intestinal microbiota, an abundance of microorganisms such as Escherichia, Enterobacter, and Klebsiella and a delayed or altered colonization by Lactobacillus spp. It has been demonstrated that Lactobacillus spp. has a protective effect against gas production bacteria such as Escherichia, Enterobacter, and Klebsiella.64 Recently, studies have also highlighted the presence of fecal calprotectin in stool samples from children suffering from infantile colic.60 Fecal calprotectin is a biochemical marker that indicates the presence of inflammation in the intestinal tract. Higher levels of IL-8, MCP-1, and MIP-1b have also been found in blood samples of colicky children, suggesting low grade systemic inflammation.65
Factors influencing the microbiota of children and their mothers have thus been widely explored by researchers, with particular attention paid to maternal medical and psychological status. Maternal health conditions such as obesity,66 migraine,66 tobacco consumption,67 anxiety,68 and depression represent risk factors for infantile colic. Paternal support to the expectant mothers,69 familial support and a couple’s level of happiness have also been linked to a lower risk of infantile colic. Moreover, paternal depression has been linked to infantile colic.70
The complexity of infantile colic is also influenced by an immature CNS. Indeed, the prevalence and the intensity of infantile colic decreases at around 8 weeks of age, which corresponds to the transition from reflex mechanisms to behavior controlled by the cerebral cortex.63 A perfect example of the effects of CNS immaturity is the preterm population where the risk of infantile colic is increased, and some studies have shown that increased prevalence corresponds with the degree of prematurity.71 Similarly, newborns with a lower birth weight tend to suffer more with colic.72 The immature enteric nervous system may contribute to infantile colic by way of gut dysmotility, which leads to altered mucus secretion and modification of microbial composition.
Although the pathophysiology of infantile colic is complex, there is a better understanding of the outlook for children with colic. In follow-up studies of children between 5 years old73 and 10 years old,74 an increase in sleep disorders, aggression or anger, and ADHD have been observed.75 Concerning somatic health problems, infantile colic has now been linked to recurrent abdominal pain74 and migraine29,30,76,77 in numerous studies. The first case report linking migraine to infantile colic was published by Katerji and Painter78 in 1994 and describes an infantile migraine presenting as colic. In 2013, a case-control study of 679 patients showed that children with migraine were more likely to have experienced infantile colic (OR, 6.61; CI 95%, 4.38-10.00; P < 0.001)77 and other study has reached the same conclusion.76 This hypothesis has been strengthened by studies linking parental migraine to infantile colic,79 allowing us to consider the possibility that these phenomena are symptoms on the same spectrum.29,80
Concerning the treatment of infantile colic, it has been at an impasse for many years. A recent systematic review from Hjern et al81 found moderate evidence to support the efficacy of Lactobacillus reuteri DSM 17 938 in the treatment of infantile colic (favorable outcome in 3 out of 4 randomized control trials). On the other hand, Hjern et al81 reported that dietary modification (formula enriched with Lactobacillus) failed to show improvement of symptoms.
Functional Abdominal Pain Disorders Associated With Migraine
The Rome IV classification categorizes the functional gastrointestinal disorders (FGID) in children into 3 subtypes: (1) functional abdominal pain disorders, (2) functional nausea and vomiting disorders, and (3) functional defecation disorders.32
There are 3 subtypes of functional abdominal pain disorders: IBS, FD, and AM. Here we are interested in IBS and FD as they are the only 2 that studies have shown as being linked to migraine.13,14,16 They are not considered as abdominal variants of migraine, in comparison to AM, in the ICHD-3b as, so far as is known, they coexist with migraine, without being temporarily linked to it. The most frequent FGID identified in toddlers is functional constipation82 which is part of the functional defecation disorders, but again with no link to migraine proven to date.
Irritable Bowel Syndrome
The Rome IV classification32 defines IBS in children as: (1) abdominal pain in at least 4 days per month associated with 1 or more of the following: (a) related to defecation, (b) a change in frequency of stool, and (c) a change in form (appearance) of stool; (2) in children with constipation, the pain does not resolve with resolution of the constipation (in this case, the child has functional constipation); and (3) after appropriate evaluation, the symptoms cannot be fully explained by other medical conditions.
IBS can be divided into subtypes reflecting the predominant stool pattern: IBS with constipation, IBS with diarrhea, IBS with constipation and diarrhea, and unspecified IBS.
According to a meta-analysis of 16 studies on the prevalence of IBS in Asian children, the prevalence ranges from 2.8% to 25.7% with a pooled prevalence of 12.4%.83 The prevalence risk ratio for girls to boys is 1.39. The prevalence of IBS in children from the Mediterranean region of Europe is evaluated at 4.0%.84
IBS etiology is most likely multi-factorial involving biological, psychological, and social factors.85 Visceral hyperalgesia (or hypersensitivity) and visceral hypervigilance are key concepts in current research on pathophysiological mechanisms of IBS.86 Brain imaging studies show that the neural processing of visceral stimuli is altered in IBS.85 There is also growing evidence to suggest that peripheral immune mechanisms and disturbed neuro-immune communication could play a role in the pathophysiology of visceral hyperalgesia. The contribution of both stress and negative emotions on symptom frequency and severity has been studied for some time now amongst children.87 As a gut-brain axis disorder, the influence of microbiota has also been studied in IBS and Hollister et al88 observed a significant difference in bacterial species (Flavonifractor plautii and Lachnospiraceae bacterium 7_1_58FAA) in IBS cases compared to control patients. Using artificial intelligence programming, Hollister et al88 manage to distinguish stool features that could help diagnose IBS. The neuroimmune system, an element of the gut-brain axis, has also been explored and found to be activated in children suffering from IBS. Increased fecal granins in the stool,89 increased gut permeability,90,91 and increased serum brain-derived neurotrophic factor (BDNF) and proBDNF have been highlighted recently in pediatric studies.
The relationship between food allergies and recurrent abdominal pain, IBS in particular, has also been widely explored.92 Some studies have shown an improvement in the severity and the frequency of pain in pediatric patients under fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) exclusive-regime.93 In addition, the role of food on their symptoms is often expressed by IBS patients, whether they are adults or children.94
The role of personal beliefs and psychological factors is proven to impact the severity of symptoms. The transmission of somatic symptoms inside the family nucleus is part of the difficulty in acknowledging the symptoms of IBS patients, as shown by van Tilburg et al95 with mothers and fathers of IBS patients also tending to report more symptoms concerning themselves.96 The presence of adverse life events, inducing fear, increases the risk of IBS symptoms presenting in children.97 Thus, anxiety and depression are predictors of abdominal pain severity in IBS patients.87 In some families, the secondary benefit of having abdominal pain, such as providing an excuse to avoid household tasks, increases the risk of IBS in low-birth-weight children.98 These studies show the difficulties in understanding the underlying causes of such a multi-factorial syndrome.
The treatment of IBS in children is still mostly dominated by non-pharmaceutical interventions such as parental education, diet (FODMAP exclusion, gluten free or increase of fiber consumption) or behavioral therapy. Unfortunately, most of the trials regarding pharmaceutical therapies study children suffering from functional abdominal pain and not IBS or FD alone.98-100 A lack of clear evidence makes it very difficult to prioritize 1 treatment over another among: antiemetics (domperidone), antidepressants (tricyclic or selective serotonin reuptake inhibitors), acid suppressing agents, antispasmodics, and antihistamines. However, probiotics seem to be effective in treating IBS in children with an estimated number need to treat of 4 according to a meta-analysis of 19 randomized control trials (RCTs).101
Regarding the evolution of IBS in children, the majority (60%) will observe the disappearance of their symptoms over 2 years following the diagnosis, regardless of age, sex, and impact of symptoms.102,103 As exposed previously for abdominal variants of migraine, the initial diagnosis of IBS increases the chance of a symptom’s resolution, which makes the positive diagnosis a very important step in the support of IBS patients.21 Le Gal et al16 showed a 3.47 OR (95% CI, 1.81-6.62; P = 0.0002) of IBS in child migraineurs in a retrospective case-control study of 1072 patients. Retrospective and prevalence studies that were interested in the prevalence of IBS and FGID in adult and children migraineurs show an important correlation between these 2 disorders.13-16,104 In a large United States IBS cohort of 97 000 patients a 60% higher odds of migraine was demonstrated in the IBS population compared to control patients in an adult population.15 In the adult population, the symptoms are the same as defined for children in the Rome IV classification. In a recent review on the prevalence of IBS in adults, the Rome Foundation refuses to give a pooled percentage for IBS since the mean prevalence in individual countries ranged from 1.1% (France and Iran) to 35.5% (Mexico).105 To shed light on the pathophysiology of IBS studies focusing on regional and cross-cultural differences are needed.
Functional Dyspepsia
The diagnosis criteria for FD in children, as defined by the Rome IV classification,32 must include one or more of the following symptoms at least 4 days per month: (1) postprandial fullness, (2) early satiation, (3) epigastric pain or burning not associated with defecation, and (4) after appropriate evaluation the symptoms cannot be fully explained by other medical conditions.
Within FD, we describe 2 subtypes32: postprandial distress syndrome and epigastric pain syndrome. The postprandial distress syndrome includes bothersome postprandial fullness or early satiation that prevents finishing a regular meal, which can be associated with abdominal bloating, postprandial nausea, or excessive belching. The epigastric pain syndrome is defined as bothersome pain or burning localized to the epigastrium, without a retrosternal component and the ingestion of a meal being a trigger or an improvement factor. As for previous exposed syndromes, the diagnosis of FD requires clinical examination and history only. However, FD and gastroesophageal reflux can be difficult to distinguish, so the requirement of esophagogastroduodenoscopy in the diagnosis of FD has been debated.106 The Rome IV classification considers there is no compelling evidence to require an esophagogastroduodenoscopy in order to make a diagnosis of FD in the pediatric population.32
The prevalence of FD is described around 7.6%107 of children, using the Rome IV diagnostic criteria.
Concerning FD in the adult population, a recent review by Wauters et al108 consider it as the most common functional upper gastrointestinal disorder affecting 15% of the general population. Its symptoms do not differ in the Rome IV classification for either adults or children.
The pathophysiology of FD still remains unclear. It is a complex combination of physiologic, genetic, environmental, and psychological factors.109 We can distinguish 2 major mechanisms: gastric motility abnormalities and impaired gastric accommodation and visceral hypersensitivity.110 Gastric accommodation is defined by the ability of the stomach to distend appropriately during a meal with an increase in gastric volume in the absence of increased gastric pressure. Gastric motility can be explored by a number of different methods (sodium acetate breath tests,111 gastric emptying scintigraphy,112 or electrogastrography113 for example) and can be compared in FD and control patients in the pediatric and adult populations. Studies have shown delayed gastric emptying,111,112 antral hypomotility,113 and a negative correlation between gastric emptying rate and severity of abdominal pain114 among dyspeptic patients. This impaired accommodation may be linked to abnormalities of the vagal reflex and intrinsic inhibitory innervation.115 Studies on adults and children highlighted abnormal gastric sensorimotor function.116 The visceral hypersensitivity to gastric distention in FD can be considered as a model of a gut-brain axis disorder. The presence of inflammatory cells (eosinophilia and high mast cell density) can be found in the stomach and duodenum of children suffering from FD,117 especially if they are also suffering from headaches.118 An altered intestinal permeability, as observed in IBS or AM, was not observed in FD patients.119 The role of Helicobacter pylori on FD and migraine has also been studied. In 2016, a meta-analysis of 25 RCT and 5555 adult patients with FD showed a 1.23-fold improvement of symptoms after H. Pylori’s eradication at long-term follow-up.120 Moreover, a cohort of 305 adult dyspeptic patients showed a significantly positive association between H. Pylori and migraine and family history of headache.121 Concerning treatment, in the pediatric population, a systematic review of three RCTs studying pharmaceutical options to treat FD found no evidence to support the use of pharmacological drugs.122
An important intrinsic role for psychosocial factors and psychiatric disorders, especially anxiety and depression, has been described in the etiopathogenesis of FD, in addition to their putative influence on health care-seeking behavior. Around 50% of FD patients show high anxiety score responses.119
Finally, for a few years, studies have underlined a link between FD (postprandial distress syndrome or epigastric pain syndrome) and migraine in the pediatric population. Di Stefano et al123 were interested in the prevalence and pathophysiology of migraine in functional dyspeptic adult patients and demonstrated 54% of epigastric pain syndrome patients and 76% of postprandial distress syndrome patients also suffered from migraine. Among the postprandial distress syndrome patients, the severity of fullness and early satiation correlated to the severity of migraine.123 Cohort studies also showed an association between primary headache and FD: 25% of FD children declared having headache more than 3 times a month on an internet questionnaire survey,124 60% of adults migraineurs suffer from FD in a prevalence study,125 and Lankarani et al14 found a 1.68 OR (P < 0.001) for FD among 1038 adults migraineurs in Iran. Le Gal et al16 calculated an odds ratio of 10 for FD among children suffering from migraine.
Conclusion
The aim of this review is to summarize the recent knowledge on abdominal variants of migraine and functional abdominal pain disorders associated to migraine, as they appear to be part of a wider spectrum of diseases now being explored as brain-gut disorders (Table 2). Migraine and related syndromes have a great impact on the quality of life of children and their future as adults. The understanding of pathophysiological mechanisms underlying these conditions is crucial in order to improve diagnosis, treatment, and follow-up in these children.
In this review, we discussed whether the inflammatory mediators, gut microbiota profile, neuropeptides, serotonin pathway, stress hormones, and nutritional substances which are related with brain-gut axis could be a pathophysiology of abdominal variants of migraine and functional abdominal pain disorders associated to migraine. AM, CVS, infantile colic, and IBS appear to be mediated by neuroinflammatory and neuroimmune patterns that can also be found in migraine. For FD, alterations in motility and gastric accommodation are among the main hypotheses. Therefore, it is possible that alterations of the gut-brain axis could be involved in the underlying mechanism for all of the abdominal syndromes associated with migraine.
Footnotes
Financial support: None.
Conflicts of interest: None.
Author contributions: Léa LenglarT and Luigi Titomanlio: concept and design, drafting the paper, and revising the paper; Léa LenglarT, Delphine Wohrer, and Caroline Caula: collecting articles and revising the paper; and Thomas Moulding and Annabel Lyles: English revision of the paper.
References
- 1.Steiner TJ, Stovner LJ, Vos T. GBD 2015: migraine is the third cause of disability in under 50s. J Headache Pain. 2016;17:104. doi: 10.1186/s10194-016-0699-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Deuschl G, Beghi E, Fazekas F, et al. The burden of neurological diseases in Europe: an analysis for the Global Burden of Disease Study 2017. Lancet Public Health. 2020;5:e551–e567. doi: 10.1016/S2468-2667(20)30190-0. [DOI] [PubMed] [Google Scholar]
- 3.Wöber-Bingöl Ç. Epidemiology of migraine and headache in children and adolescents. Curr Pain Headache Rep. 2013;17:341. doi: 10.1007/s11916-013-0341-z. [DOI] [PubMed] [Google Scholar]
- 4.Anttila P. Long-term trends in the incidence of headache in finnish schoolchildren. Pediatrics. 2006;117:e1197–e1201. doi: 10.1542/peds.2005-2274. [DOI] [PubMed] [Google Scholar]
- 5.Kienbacher C, Wöber C, Zesch H, et al. Clinical features, classification and prognosis of migraine and tension-type headache in children and adolescents: a long-term follow-up study. Cephalalgia. 2006;26:820–830. doi: 10.1111/j.1468-2982.2006.01108.x. [DOI] [PubMed] [Google Scholar]
- 6.McAbee GN, Morse AM, Assadi M. Pediatric aspects of headache classification in the international classification of headache disorders-3 (ICHD-3 beta version) Curr Pain Headache Rep. 2016;20:7. doi: 10.1007/s11916-015-0537-5. [DOI] [PubMed] [Google Scholar]
- 7.Abu-Arafeh I, Callaghan M. Short migraine attacks of less than 2 h duration in children and adolescents. Cephalalgia. 2004;24:333–338. doi: 10.1111/j.1468-2982.2004.00670.x. [DOI] [PubMed] [Google Scholar]
- 8.Headache Classification Committee of the International Headache Society (IHS), author The international classification of headache disorders, 3rd edition (beta version) Cephalalgia. 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 9.Koller LS, Diesner SC, Voitl P. Quality of life in children and adolescents with migraine: an Austrian monocentric, cross-sectional questionnaire study. BMC Pediatr. 2019;19:164. doi: 10.1186/s12887-019-1537-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eidlitz Markus T, Toldo I. Obesity and migraine in childhood. Curr Pain Headache Rep. 2018;22:42. doi: 10.1007/s11916-018-0696-2. [DOI] [PubMed] [Google Scholar]
- 11.Özge A, Uluduz D, Bolay H. Co-occurrence of migraine and atopy in children and adolescents: myth or a casual relationship? Curr Opin Neurol. 2017;30:287–291. doi: 10.1097/WCO.0000000000000439. [DOI] [PubMed] [Google Scholar]
- 12.Russo A, Bruno A, Trojsi F, Tessitore A, Tedeschi G. Lifestyle factors and migraine in childhood. Curr Pain Headache Rep. 2016;20:9. doi: 10.1007/s11916-016-0539-y. [DOI] [PubMed] [Google Scholar]
- 13.van Hemert S, Breedveld AC, Rovers JMP, et al. Migraine associated with gastrointestinal disorders: review of the literature and clinical implications. Front Neurol. 2014;5:214. doi: 10.3389/fneur.2014.00241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lankarani KB, Akbari M, Tabrizi R. Association of gastrointestinal functional disorders and migraine headache: a population base study. Middle East J Dig Dis. 2017;9:139–145. doi: 10.15171/mejdd.2017.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole JA, Rothman KJ, Cabral HJ, Zhang Y, Farraye FA. Migraine, fibromyalgia, and depression among people with IBS: a prevalence study. BMC Gastroenterol. 2006;6:26. doi: 10.1186/1471-230X-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Le Gal J, Michel JF, Rinaldi VE, et al. Association between functional gastrointestinal disorders and migraine in children and adolescents: a case-control study. Lancet Gastroenterol Hepatol. 2016;1:114–121. doi: 10.1016/S2468-1253(16)30038-3. [DOI] [PubMed] [Google Scholar]
- 17.Charles A. The pathophysiology of migraine: implications for clinical management. Lancet Neurol. 2018;17:174–182. doi: 10.1016/S1474-4422(17)30435-0. [DOI] [PubMed] [Google Scholar]
- 18.Gormley P, Anttila V, Winsvold BS, et al. Meta-analysis of 375,000 individuals identifies 38 susceptibility loci for migraine. Nat Genet. 2016;48:856–866. doi: 10.1038/ng.3598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arzani M, Jahromi SR, Ghorbani Z, et al. Gut-brain axis and migraine headache: a comprehensive review. J Headache Pain. 2020;21:15. doi: 10.1186/s10194-020-1078-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mesa MD, Loureiro B, Iglesia I, et al. The evolving microbiome from pregnancy to early infancy: a comprehensive review. Nutrients. 2020;12:133. doi: 10.3390/nu12010133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trivić I, Hojsak I. Initial diagnosis of functional gastrointestinal disorders in children increases a chance for resolution of symptoms. Pediatr Gastroenterol Hepatol Nutr. 2018;21:264–270. doi: 10.5223/pghn.2018.21.4.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gelfand AA. Migraine and childhood periodic syndromes in children and adolescents. Curr Opin Neurol. 2013;26:262–268. doi: 10.1097/WCO.0b013e32836085c7. [DOI] [PubMed] [Google Scholar]
- 23.Spiri D, Rinaldi VE, Titomanlio L. Pediatric migraine and episodic syndromes that may be associated with migraine. Ital J Pediatr. 2014;40:92. doi: 10.1186/s13052-014-0092-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tarantino S, Capuano A, Torriero R, et al. Migraine equivalents as part of migraine syndrome in childhood. Pediatr Neurol. 2014;51:645–649. doi: 10.1016/j.pediatrneurol.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 25.Rothner AD, Parikh S. Migraine variants or episodic syndromes that may be associated with migraine and other unusual pediatric headache syndromes. Headache. 2016;56:206–214. doi: 10.1111/head.12750. [DOI] [PubMed] [Google Scholar]
- 26.Irwin S, Barmherzig R, Gelfand A. Recurrent gastrointestinal disturbance: abdominal migraine and cyclic vomiting syndrome. Curr Neurol Neurosci Rep. 2017;17:21. doi: 10.1007/s11910-017-0731-4. [DOI] [PubMed] [Google Scholar]
- 27.Lin YP, Ni YH, Weng WC, Lee WT. Cyclic vomiting syndrome and migraine in children. J Formos Med Assoc. 2011;110:382–387. doi: 10.1016/S0929-6646(11)60056-9. [DOI] [PubMed] [Google Scholar]
- 28.Gelfand AA, Goadsby PJ, Allen IE. The relationship between migraine and infant colic: a systematic review and meta-analysis. Cephalalgia. 2015;35:63–72. doi: 10.1177/0333102414534326. [DOI] [PubMed] [Google Scholar]
- 29.Qubty W, Gelfand AA. The link between infantile colic and migraine. Curr Pain Headache Rep. 2016;20:31. doi: 10.1007/s11916-016-0558-8. [DOI] [PubMed] [Google Scholar]
- 30.Zhang D, Zhang Y, Sang Y, Zheng N, Liu X. The relationship between infant Colic and migraine as well as tension-type headache: a meta-analysis. Pain Res Manag. 2019;2019:8307982. doi: 10.1155/2019/8307982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Symon DN, Russell G. Abdominal migraine: a childhood syndrome defined. Cephalalgia. 1986;6:223–228. doi: 10.1046/j.1468-2982.1986.0604223.x. [DOI] [PubMed] [Google Scholar]
- 32.Hyams JS, Di Lorenzo C, Saps M, Shulman R, Staiano A, van Tilburg M. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology. 2016;150:1456–1468. e2. doi: 10.1053/j.gastro.2016.02.015. [DOI] [PubMed] [Google Scholar]
- 33.Angus-Leppan H, Saatci D, Sutcliffe A, Guiloff RJ. Abdominal migraine. BMJ. 2018;360:k179. doi: 10.1136/bmj.k179. [DOI] [PubMed] [Google Scholar]
- 34.Abu-Arafeh I, Russell G. Prevalence and clinical features of abdominal migraine compared with those of migraine headache. Arch Dis Child. 1995;72:413–417. doi: 10.1136/adc.72.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mortimer MJ, Kay J, Jaron A. Clinocal epidemiology of childhood abdominal migraine in an urban general practice. Dev Med Child Neurol. 2008;35:243–248. doi: 10.1111/j.1469-8749.1993.tb11629.x. [DOI] [PubMed] [Google Scholar]
- 36.Mortimer MJ, Kay J, Jaron A, Good PA. Does a history of maternal migraine or depression predispose children to headache and stomach-ache? Headache. 1992;32:353–355. doi: 10.1111/j.1526-4610.1992.hed3207353.x. [DOI] [PubMed] [Google Scholar]
- 37.Bentley D, Kehely A, Michie CA al-Bayaty M, author. Abdominal migraine as a cause of vomiting in children: a clinican's view. J Pediatr Gastroenterol Nutr. 1995;21(suppl 1):S49–S51. doi: 10.1097/00005176-199501001-00014. [DOI] [PubMed] [Google Scholar]
- 38.Kunishi Y, Iwata Y, Ota M, et al. Abdominal migraine in a middle-aged woman. Intern Med. 2016;55:2793–2798. doi: 10.2169/internalmedicine.55.6626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Roberts JE, deShazo RD. Abdominal migraine, another cause of abdominal pain in adults. Am J Med. 2012;125:1135–1139. doi: 10.1016/j.amjmed.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 40.Devanarayana NM, Rajindrajith S, Benninga MA. Abdominal migraine in children: association between gastric motility parameters and clinical characteristics. BMC Gastroenterol. 2016;16:26. doi: 10.1186/s12876-016-0435-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mani J, Madani S. Pediatric abdominal migraine: current perspectives on a lesser known entity. Pediatric Health Med Ther. 2018;9:47–58. doi: 10.2147/PHMT.S127210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Albers L, von Kries R, Straube A, Heinen F, Obermeier V, Landgraf MN. Do pre-school episodic syndromes predict migraine in primary school children? A retrospective cohort study on health care data. Cephalalgia. 2019;39:497–503. doi: 10.1177/0333102418791820. [DOI] [PubMed] [Google Scholar]
- 43.Gelfand AA. Episodic syndromes that may be associated with migraine: A.K.A. 'the childhood periodic syndromes'. Headache. 2015;55:1358–1364. doi: 10.1111/head.12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Symon DN, Russell G. Double blind placebo controlled trial of pizotifen syrup in the treatment of abdominal migraine. Arch Dis Child. 1995;72:48–50. doi: 10.1136/adc.72.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Donnet A, Redon S. Cyclic vomiting syndrome in children. Curr Pain Headache Rep. 2018;22:30. doi: 10.1007/s11916-018-0684-6. [DOI] [PubMed] [Google Scholar]
- 46.Lu PL, Saps M, Chanis RA, Velasco-Benítez CA. The prevalence of functional gastrointestinal disorders in children in Panama: a school-based study. Acta Paediatr. 2016;105:e232–e236. doi: 10.1111/apa.13379. [DOI] [PubMed] [Google Scholar]
- 47.Chogle A, Velasco-Benitez CA, Koppen IJ, Moreno JE, Ramírez Hernández CR, Saps M. A population-based study on the epidemiology of functional gastrointestinal disorders in young children. J Pediatr. 2016;179:139–143. e1. doi: 10.1016/j.jpeds.2016.08.095. [DOI] [PubMed] [Google Scholar]
- 48.Zaki EA, Freilinger T, Klopstock T, et al. Two common mitochondrial DNA polymorphisms are highly associated with migraine headache and cyclic vomiting syndrome. Cephalalgia. 2009;29:719–728. doi: 10.1111/j.1468-2982.2008.01793.x. [DOI] [PubMed] [Google Scholar]
- 49.Ellingsen DM, Garcia RG, Lee J, et al. Cyclic vomiting syndrome is characterized by altered functional brain connectivity of the insular cortex: a cross-comparison with migraine and healthy adults. Neurogastroenterol Motil. 2017;29:e13004. doi: 10.1111/nmo.13004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chelimsky TC, Chelimsky GG. Autonomic abnormalities in cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2007;44:326–330. doi: 10.1097/MPG.0b013e31802bddb7. [DOI] [PubMed] [Google Scholar]
- 51.Liao KY, Chang FY, Wu LT, Wu TC. Cyclic vomiting syndrome in Taiwanese children. J Formos Med Assoc. 2011;110:14–18. doi: 10.1016/S0929-6646(11)60003-X. [DOI] [PubMed] [Google Scholar]
- 52.Prakash C, Staiano A, Rothbaum RJ, Clouse RE. Similarities in cyclic vomiting syndrome across age groups. Am J Gastroenterol. 2001;96:684–688. doi: 10.1111/j.1572-0241.2001.03606.x. [DOI] [PubMed] [Google Scholar]
- 53.Kovacic K, Sood M, Venkatesan T. Cyclic vomiting syndrome in children and adults: what is new in 2018? Curr Gastroenterol Rep. 2018;20:46. doi: 10.1007/s11894-018-0654-5. [DOI] [PubMed] [Google Scholar]
- 54.Tarbell SE, Li BU. Health-related quality of life in children and adolescents with cyclic vomiting syndrome: a comparison with published data on youth with irritable bowel syndrome and organic gastrointestinal disorders. J Pediatr. 2013;163:493–497. doi: 10.1016/j.jpeds.2013.01.025. [DOI] [PubMed] [Google Scholar]
- 55.Tarbell S, Li BU. Psychiatric symptoms in children and adolescents with cyclic vomiting syndrome and their parents. Headache. 2008;48:259–266. doi: 10.1111/j.1526-4610.2007.00997.x. [DOI] [PubMed] [Google Scholar]
- 56.Li BU. Managing cyclic vomiting syndrome in children: beyond the guidelines. Eur J Pediatr. 2018;177:1435–1442. doi: 10.1007/s00431-018-3218-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hikita T, Kodama H, Ogita K, Kaneko S, Nakamoto N, Mimaki M. Cyclic vomiting syndrome in infants and children: a clinical follow-up study. Pediatr Neurol. 2016;57:29–33. doi: 10.1016/j.pediatrneurol.2016.01.001. [DOI] [PubMed] [Google Scholar]
- 58.Wessel MA, Cobb JC, Jackson EB, Harris GS, Jr, Detwiler AC. Paroxysmal fussing in infancy, sometimes called colic. Pediatrics. 1954;14:421–435. [PubMed] [Google Scholar]
- 59.Wolke D, Bilgin A, Samara M. Systematic review and meta-analysis: fussing and crying durations and prevalence of colic in infants. J Pediatr. 2017;185:55–61. e4. doi: 10.1016/j.jpeds.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 60.Rhoads JM, Fatheree NY, Norori J, et al. Altered fecal microflora and increased fecal calprotectin in infants with colic. J Pediatr. 2009;155:823–828. e1. doi: 10.1016/j.jpeds.2009.05.012. [DOI] [PubMed] [Google Scholar]
- 61.Leppälehto E, Pärtty A, Kalliomäki M, Löyttyniemi E, Isolauri E, Rautava S. Maternal intrapartum antibiotic administration and infantile colic: is there a connection? Neonatology. 2018;114:226–229. doi: 10.1159/000489991. [DOI] [PubMed] [Google Scholar]
- 62.Oosterloo BC, van Elburg RM, Rutten NB, et al. Wheezing and infantile colic are associated with neonatal antibiotic treatment. Pediatr Allergy Immunol. 2018;29:151–158. doi: 10.1111/pai.12857. [DOI] [PubMed] [Google Scholar]
- 63.Zeevenhooven J, Browne PD, L'Hoir MP, de Weerth C, Benninga MA. Infant colic: mechanisms and management. Nat Rev Gastroenterol Hepatol. 2018;15:479–496. doi: 10.1038/s41575-018-0008-7. [DOI] [PubMed] [Google Scholar]
- 64.Savino F, Cordisco L, Tarasco V, et al. Antagonistic effect of Lactobacillus strains against gas-producing coliforms isolated from colicky infants. BMC Microbiol. 2011;11:157. doi: 10.1186/1471-2180-11-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pärtty A, Kalliomäki M, Salminen S, Isolauri E. Infantile colic is associated with low-grade systemic inflammation. J Pediatr Gastroenterol Nutr. 2017;64:691–695. doi: 10.1097/MPG.0000000000001340. [DOI] [PubMed] [Google Scholar]
- 66.Kaymaz N, Yıldırım Ş, Topaloğlu N, et al. Prenatal maternal risk factors for infantile colic. Nurs Child Young People. 2015;27:32–38. doi: 10.7748/ncyp.27.10.32.s28. [DOI] [PubMed] [Google Scholar]
- 67.Canivet CA, Ostergren PO, Jakobsson IL, Dejin-Kaelsson E, Hagander BM. Infantile colic, maternal smoking and infant feeding at 5 weeks of age. Scand J Public Health. 2008;36:284–291. doi: 10.1177/1403494807086981. [DOI] [PubMed] [Google Scholar]
- 68.Paradise JL. Maternal and other factors in the etiology of infantile colic: report of a prospective study of 146 infants. JAMA. 1966;197:191–199. doi: 10.1001/jama.1966.03110030085031. [DOI] [PubMed] [Google Scholar]
- 69.Alexander CP, Zhu J, Paul IM, Kjerulff KH. Fathers make a difference: positive relationships with mother and baby in relation to infant colic. Child Care Health Dev. 2017;43:687–696. doi: 10.1111/cch.12445. [DOI] [PubMed] [Google Scholar]
- 70.van den Berg MP, van der Ende J, Crijnen AA, et al. Paternal depressive symptoms during pregnancy are related to excessive infant crying. Pediatrics. 2009;124:e96–e103. doi: 10.1542/peds.2008-3100. [DOI] [PubMed] [Google Scholar]
- 71.Milidou I, Søndergaard C, Jensen MS, Olsen J, Henriksen TB. Gestational age, small for gestational age, and infantile colic. Paediatr Perinat Epidemiol. 2014;28:138–145. doi: 10.1111/ppe.12095. [DOI] [PubMed] [Google Scholar]
- 72.Søndergaard C. Fetal growth and infantile colic. Arch Dis Child Fetal Neonatal Ed. 2000;83:F44–F47. doi: 10.1136/fn.83.1.F44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Smarius LJ, Strieder TG, Loomans EM, et al. Excessive infant crying doubles the risk of mood and behavioral problems at age 5: evidence for mediation by maternal characteristics. Eur Child Adolesc Psychiatry. 2017;26:293–302. doi: 10.1007/s00787-016-0888-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Savino F, Castagno E, Bretto R, Brondello C, Palumeri E, Oggero R. A prospective 10-year study on children who had severe infantile colic. Acta Paediatr Suppl. 2005;94:129–132. doi: 10.1111/j.1651-2227.2005.tb02169.x. [DOI] [PubMed] [Google Scholar]
- 75.Hemmi MH, Wolke D, Schneider S. Associations between problems with crying, sleeping and/or feeding in infancy and long-term behavioural outcomes in childhood: a meta-analysis. Arch Dis Child. 2011;96:622–629. doi: 10.1136/adc.2010.191312. [DOI] [PubMed] [Google Scholar]
- 76.Levinsky Y, Eidlitz-Markus T. Comparison of the prevalence of infantile colic between pediatric migraine and other types of pediatric headache. J Child Neurol. 2020;35:607–611. doi: 10.1177/0883073820924264. [DOI] [PubMed] [Google Scholar]
- 77.Romanello S, Spiri D, Marcuzzi E, et al. Association between childhood migraine and history of infantile colic. JAMA. 2013;309:1607–1612. doi: 10.1001/jama.2013.747. [DOI] [PubMed] [Google Scholar]
- 78.Katerji MA, Painter MJ. Infantile migraine presenting as colic. J Child Neurol. 1994;9:336–337. doi: 10.1177/088307389400900325. [DOI] [PubMed] [Google Scholar]
- 79.Gelfand AA, Buse DC, Cabana MD, Grimes B, Goadsby PJ, Allen IE. The association between parental migraine and infant colic: a cross-sectional, web-based, U.S. survey study. Headache. 2019;59:988–1001. doi: 10.1111/head.13575. [DOI] [PubMed] [Google Scholar]
- 80.Gelfand AA, Thomas KC, Goadsby PJ. Before the headache: infant colic as an early life expression of migraine. Neurology. 2012;79:1392–1396. doi: 10.1212/WNL.0b013e31826c1b7b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Hjern A, Lindblom K, Reuter A, Silfverdal SA. A systematic review of prevention and treatment of infantile colic. Acta Paediatr. 2020;109:1733–1744. doi: 10.1111/apa.15247. [DOI] [PubMed] [Google Scholar]
- 82.Steutel NF, Zeevenhooven J, Scarpato E, et al. Prevalence of functional gastrointestinal disorders in european infants and toddlers. J Pediatr. 2020;221:107–114. doi: 10.1016/j.jpeds.2020.02.076. [DOI] [PubMed] [Google Scholar]
- 83.Devanarayana NM, Rajindrajith S, Pathmeswaran A, Abegunasekara C, Gunawardena NK, Benninga MA. Epidemiology of irritable bowel syndrome in children and adolescents in Asia. J Pediatr Gastroenterol Nutr. 2015;60:792–798. doi: 10.1097/MPG.0000000000000714. [DOI] [PubMed] [Google Scholar]
- 84.Scarpato E, Kolacek S, Jojkic-Pavkov D, et al. Prevalence of functional gastrointestinal disorders in children and adolescents in the Mediterranean region of Europe. Clin Gastroenterol Hepatol. 2018;16:870–876. doi: 10.1016/j.cgh.2017.11.005. [DOI] [PubMed] [Google Scholar]
- 85.Elsenbruch S. Abdominal pain in irritable bowel syndrome: a review of putative psychological, neural and neuro-immune mechanisms. Brain Behav Immun. 2011;25:386–394. doi: 10.1016/j.bbi.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 86.Di Lorenzo C, Youssef NN, Sigurdsson L, Scharff L, Griffiths J, Wald A. Visceral hyperalgesia in children with functional abdominal pain. J Pediatr. 2001;139:838–843. doi: 10.1067/mpd.2001.118883. [DOI] [PubMed] [Google Scholar]
- 87.Hollier JM, van Tilburg MAL, Liu Y, et al. Multiple psychological factors predict abdominal pain severity in children with irritable bowel syndrome. Neurogastroenterol Motil. 2019;31:e13509. doi: 10.1111/nmo.13509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Hollister EB, Oezguen N, Chumpitazi BP, et al. Leveraging human microbiome features to diagnose and stratify children with irritable bowel syndrome. J Mol Diagn. 2019;21:449–461. doi: 10.1016/j.jmoldx.2019.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Shulman RJ, Öhman L, Stridsberg M, Cain K, Simén M, Heitkemper M. Evidence of increased fecal granins in children with irritable bowel syndrome and correlates with symptoms. Neurogastroenterol Motil. 2019;31:e13486. doi: 10.1111/nmo.13486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shulman RJ, Devaraj S, Heitkemper M. Gut permeability is affected by sex and increased in children with irritable bowel syndrome but not in functional abdominal pain. Neurogastroenterol Motil. 2020;32:e13765. doi: 10.1111/nmo.13765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Di Nardo G, Barbara G, Cucchiara S, et al. Neuroimmune interactions at different intestinal sites are related to abdominal pain symptoms in children with IBS. Neurogastroenterol Motil. 2014;26:196–204. doi: 10.1111/nmo.12250. [DOI] [PubMed] [Google Scholar]
- 92.Loo EXL, Wang Y, Siah KTH. Association between irritable bowel syndrome and allergic diseases: to make a case for aeroallergen. Int Arch Allergy Immunol. 2020;181:31–42. doi: 10.1159/000503629. [DOI] [PubMed] [Google Scholar]
- 93.Brown SC, Whelan K, Gearry RB, Day AS. Low FODMAP diet in children and adolescents with functional bowel disorder: a clinical case note review. JGH Open. 2020;4:153–159. doi: 10.1002/jgh3.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chumpitazi BP, Weidler EM, Lu DY, Tsai CM, Chulman RJ. Self-perceived food intolerances are common and associated with clinical severity in childhood irritable bowel syndrome. J Acad Nutr Diet. 2016;116:1458–1464. doi: 10.1016/j.jand.2016.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.van Tilburg MA, Levy RL, Walker LS, et al. Psychosocial mechanisms for the transmission of somatic symptoms from parents to children. World J Gastroenterol. 2015;21:5532–5541. doi: 10.3748/wjg.v21.i18.5532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zeevenhooven J, Rutten JMTM, van Dijk M, Peeters B, Benninga MA. Parental factors in pediatric functional abdominal pain disorders: a cross-sectional cohort study. J Pediatr Gastroenterol Nutr. 2019;68:e20–e26. doi: 10.1097/MPG.0000000000002163. [DOI] [PubMed] [Google Scholar]
- 97.Rahal H, Videlock EJ, Icenhour A, et al. Importance of trauma-related fear in patients with irritable bowel syndrome and early adverse life events. Neurogastroenterol Motil. 2020;32:e13896. doi: 10.1111/nmo.13896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Harvey PR, Theron B, Smith SCL, et al. The association between low birth weight, childhood recollections of parental response to illness, and irritable bowel syndrome: a twin study. Neurogastroenterol Motil. 2020;32:e13939. doi: 10.1111/nmo.13939. [DOI] [PubMed] [Google Scholar]
- 99.Scarpato E, Auricchio R, Penagini F, Campanozzi A, Zuccotti GV, Troncone R. Efficacy of the gluten free diet in the management of functional gastrointestinal disorders: a systematic review on behalf of the Italian society of paediatrics. Ital J Pediatr. 2019;45:9. doi: 10.1186/s13052-019-0606-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Devanarayana NM, Rajindrajith S. Irritable bowel syndrome in children: current knowledge, challenges and opportunities. World J Gastroenterol. 2018;24:2211–2235. doi: 10.3748/wjg.v24.i21.2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Newlove-Delgado TV, Martin AE, Abbott RA, et al. Dietary interventions for recurrent abdominal pain in childhood. Cochrane Database Syst Rev. 2017;3:CD010972. doi: 10.1002/14651858.CD010972.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Giannetti E, Maglione M, Sciorio E, Coppola V, Miele E, Staiano A. Do children just grow out of irritable bowel syndrome? J Pediatr. 2017;183:122–126. e1. doi: 10.1016/j.jpeds.2016.12.036. [DOI] [PubMed] [Google Scholar]
- 103.Rawlley B, Shah D, Narang M, Pandey M. Long-term outcome of children with recurrent abdominal pain. Indian Pediatr. 2020;57:465–466. doi: 10.1007/s13312-020-1823-9. [DOI] [PubMed] [Google Scholar]
- 104.Lau CI, Lin CC, Chen WH, Wang HC, Kao CH. Association between migraine and irritable bowel syndrome: a population-based retrospective cohort study. Eur J Neurol. 2014;21:1198–1204. doi: 10.1111/ene.12468. [DOI] [PubMed] [Google Scholar]
- 105.Sperber AD, Dumitrascu D, Fukudo S, et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a rome foundation working team literature review. Gut. 2017;66:1075–1082. doi: 10.1136/gutjnl-2015-311240. [DOI] [PubMed] [Google Scholar]
- 106.Guariso G, Meneghel A, Dalla Pozza LV, et al. Indications to upper gastrointestinal endoscopy in children with dyspepsia. J Pediatr Gastroenterol Nutr. 2010;50:493–499. doi: 10.1097/MPG.0b013e3181bb3362. [DOI] [PubMed] [Google Scholar]
- 107.Robin SG, Keller C, Zwiener R, et al. Prevalence of pediatric functional gastrointestinal disorders utilizing the rome IV criteria. J Pediatr. 2018;195:134–139. doi: 10.1016/j.jpeds.2017.12.012. [DOI] [PubMed] [Google Scholar]
- 108.Wauters L, Talley NJ, Walker MM, Tack J, Vanuytsel T. Novel concepts in the pathophysiology and treatment of functional dyspepsia. Gut. 2020;69:591–600. doi: 10.1136/gutjnl-2019-318536. [DOI] [PubMed] [Google Scholar]
- 109.Romano C, Valenti S, Cardile S, Benninga MA. Functional dyspepsia: an enigma in a conundrum. J Pediatr Gastroenterol Nutr. 2016;63:579–584. doi: 10.1097/MPG.0000000000001344. [DOI] [PubMed] [Google Scholar]
- 110.Tack J, Talley NJ. Functional dyspepsia-symptoms, definitions and validity of the rome III criteria. Nat Rev Gastroenterol Hepatol. 2013;10:134–141. doi: 10.1038/nrgastro.2013.14. [DOI] [PubMed] [Google Scholar]
- 111.Hijaz NM, Friesen CA, Schurman JV, Pearce RE, Abdel-Rahman SM. Plasma ghrelin and liquid gastric emptying in children with functional dyspepsia consistent with post-prandial distress syndrome. Neurogastroenterol Motil. 2015;27:1120–1126. doi: 10.1111/nmo.12591. [DOI] [PubMed] [Google Scholar]
- 112.Yu YH, Jo Y, Jung JY, Kim BK, Seok JW. Gastric emptying in migraine: a comparison with functional dyspepsia. J Neurogastroenterol Motil. 2012;18:412–418. doi: 10.5056/jnm.2012.18.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Leung MW, Wong BP, Chao NS, Chung KW, Kwon WK, Liu KK. Electrogastrography in the management of pediatric functional dyspepsia and motility disorder. J Pediatr Surg. 2006;41:2069–2072. doi: 10.1016/j.jpedsurg.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 114.Devanarayana NM, Rajindrajith S, Perera MS, Nishanthanie SW, Benninga MA. Gastric emptying and antral motility parameters in children with functional dyspepsia: association with symptom severity. J Gastroenterol Hepatol. 2013;28:1161–1166. doi: 10.1111/jgh.12205. [DOI] [PubMed] [Google Scholar]
- 115.Vargas-Luna FM, Huerta-Franco MR, Schurman JV, et al. Heart rate variability and gastric electrical response to a cold pressor task in youth with functional dyspepsia. Dig Dis Sci. 2020;65:1074–1081. doi: 10.1007/s10620-019-05848-4. [DOI] [PubMed] [Google Scholar]
- 116.Pucci E, Di Stefano M, Miceli E, Corazza GR, Sandrini G, Nappi G. Patients with headache and functional dyspepsia present meal-induced hypersensitivity of the stomach. J Headache Pain. 2005;6:223–226. doi: 10.1007/s10194-005-0191-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Singh V, Singh M, Schurman JV, Friesen CA. Histopathological changes in the gastroduodenal mucosa of children with functional dyspepsia. Pathol Res Pract. 2018;214:1173–1178. doi: 10.1016/j.prp.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 118.Yeom JS, Choi MB, Seo JH, et al. Relationship between headache and mucosal mast cells in pediatric Helicobacter pylori-negative functional dyspepsia. Cephalalgia. 2013;33:323–329. doi: 10.1177/0333102412472070. [DOI] [PubMed] [Google Scholar]
- 119.Neilan NA, Garg UC, Schurman JV, Friesen CA. Intestinal permeability in children/adolescents with functional dyspepsia. BMC Res Notes. 2014;7:275. doi: 10.1186/1756-0500-7-275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Du LJ, Chen BR, Kim JJ, Kim S, Shen JH, Dai N. Helicobacter pylori eradication therapy for functional dyspepsia: systematic review and meta-analysis. World J Gastroenterol. 2016;22:3486–3495. doi: 10.3748/wjg.v22.i12.3486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Akbari N, Hormati A, Sharifipour E, et al. Migraine, dyspepsia, and Helicobacter pylori: zeroing in on the culprit. Iran J Neurol. 2019;18:19–24. doi: 10.18502/ijnl.v18i1.942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Browne PD, Nagelkerke SCJ, van Etten-Jamaludin FS, Benninga MA, Tabbers MM. Pharmacological treatments for functional nausea and functional dyspepsia in children: a systematic review. Expert Rev Clin Pharmacol. 2018;11:1195–1208. doi: 10.1080/17512433.2018.1540298. [DOI] [PubMed] [Google Scholar]
- 123.Di Stefano M, Pucci E, Miceli E, et al. Prevalence and pathophysiology of post-prandial migraine in patients with functional dyspepsia. Cephalalgia. 2019;39:1560–1568. doi: 10.1177/0333102419857596. [DOI] [PubMed] [Google Scholar]
- 124.Kumagai H, Yokoyama K, Imagawa T, Yamagata T. Functional dyspepsia and irritable bowel syndrome in teenagers: internet survey. Pediatr Int. 2016;58:714–720. doi: 10.1111/ped.12884. [DOI] [PubMed] [Google Scholar]
- 125.Kurth T, Holtmann G, Neufang-Hüber J, Gerken G, Diener HC. Prevalence of unexplained upper abdominal symptoms in patients with migraine. Cephalalgia. 2006;26:506–510. doi: 10.1111/j.1468-2982.2005.01076.x. [DOI] [PubMed] [Google Scholar]