Abstract
Objective:
In 2017, the U.S. Food and Drug Administration (FDA) announced a proposed regulation to lower nicotine in cigarettes to minimally addictive levels to help smokers quit. We sought to explore effective message strategies communicating about nicotine reduction in cigarettes across the different key audiences that the regulation is most likely to influence.
Methods:
We designed four types of messages: efficacy messages, risk messages, a message about alternative sources of nicotine, and a compensation message. Sixteen virtual focus groups were conducted in Atlanta and San Francisco in April-May 2020. Data were analyzed in NVivo 12.0 using a thematic analysis approach.
Findings:
Exclusive smokers were receptive to both efficacy messages and risk messages. Dual users were the only group that was open to resorting to alternative sources of nicotine. Former smokers were critical of these messages as promoting the new kinds of cigarettes and potentially encouraging initiation and relapse of smoking. Nonsmokers felt that efficacy messages downplayed the risks of smoking and did not scare people away from smoking. Presenting information that very low nicotine cigarettes (VLNCs) still contain harmful chemicals made smokers question continued smoking in the absence of nicotine and view VLNCs as harmful.
Conclusions:
Messages communicating about nicotine reduction in cigarettes might help to motivate smokers to quit and can correct the misperceptions that VLNCs are less harmful. The FDA should consider specific target audiences and use different messages that complement each other in communicating about this regulation.
Introduction
Tobacco use remains a global public health challenge.1 While all tobacco products are harmful, combusted cigarettes have the biggest impact and are responsible for nearly half a million premature deaths each year in the United States.2 Quitting cigarettes is difficult because the nicotine in cigarettes makes them addictive.3 Reducing nicotine in cigarettes, therefore, aims to help smokers quit. It has been estimated that reducing nicotine in cigarettes can save millions of lives.4 In 2017, the U.S. Food and Drug Administration (FDA) proposed an unprecedented regulation to lower nicotine in cigarettes to minimally addictive levels while spurring innovation in lower-risk nicotine products, so that smokers who cannot otherwise quit all nicotine products have viable less harmful alternatives.5 No other country has adopted such a policy. One key to successful policy implementation is to effectively communicate this regulation and its objectives to diverse consumers. However, such communication is challenging.
The main goal of reducing nicotine in cigarettes to non-addictive levels is to help smokers quit. However, very low nicotine cigarettes (VLNCs) could be perceived as harmless, which can discourage quitting.6,7,8 While nicotine is not the main cancer-causing ingredient in cigarettes, around 80% of US adults believe that nicotine causes serious smoking-related harms.9 VLNCs may be misunderstood by adolescents and young adults, resulting in smoking initiation among individuals who may not have initiated smoking with traditional cigarettes. There is evidence that adolescents perceive VLNCs as less harmful than other tobacco products9 and have limited understanding of the mechanisms of nicotine addiction,10,11 which may result in misperceptions of the VLNC policy. Additionally, former smokers could relapse because they might think that VLNCs are less harmful than traditional cigarettes, or that they would be less likely to become addicted to smoking again. Furthermore, smokers believe that they would need to compensate for the low amount of nicotine by consuming more cigarettes or inhaling more intensely,12 although existing evidence does not support of this belief.13,14,15 Thus, messages communicating about VLNCs not only need to inform people of the regulation and its purpose, but also effectively dispel misperceptions.
To date, little research has investigated ways to communicate about VLNCs.16 Thus, this study aimed to explore effective message strategies to communicate about VLNCs across the different key audiences that the regulation is most likely to influence. This study provides the FDA with evidence to identify and evaluate ways to communicate about VLNCs to the public.
Methods
Message Design
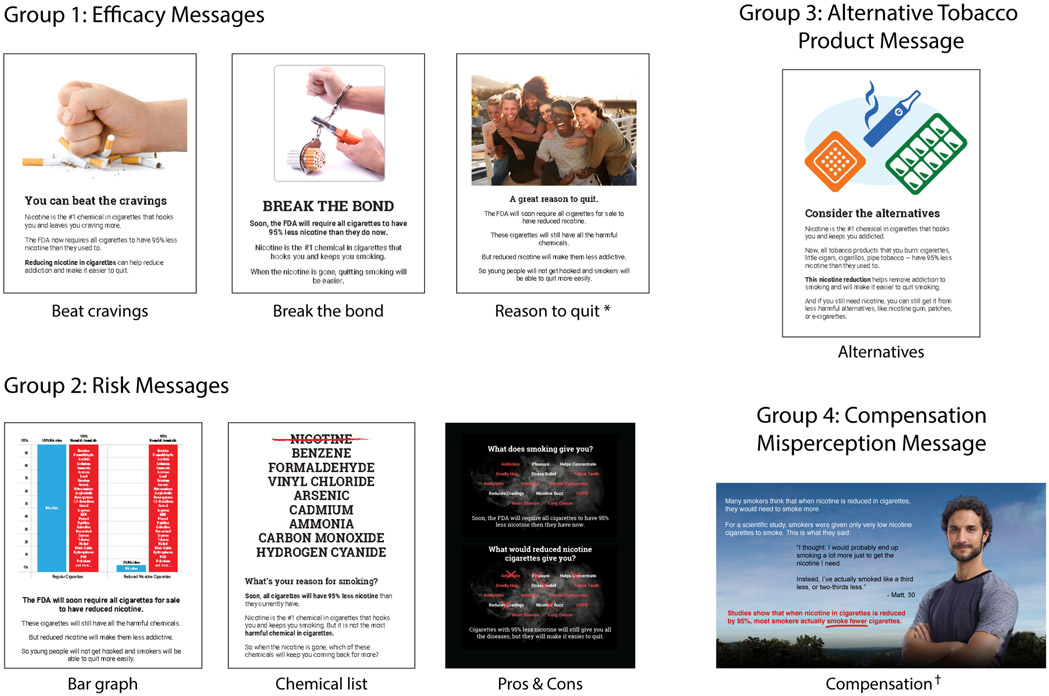
We tested four types of the messages (Fig. 1):
Figure 1.
Four Message Groups
*. The Reason to quit message shown in focus groups included a slightly different image with the same theme, which we are not displaying here for copyright reasons.
†. Image source: FDA “Every try counts” campaign, https://everytrycounts.betobaccofree.hhs.gov/
Three efficacy messages (Beat cravings, Break the bond, and Reason to quit) focused on empowering smokers and increasing their self-efficacy. The messages were positively framed, suggesting that quitting smoking would be easier when the nicotine is gone and featured positive imagery, showing smokers taking control and prevailing over cigarettes (e.g., by smashing them with a fist).
Three risk messages (Bar graph, Chemical list, Pros & Cons) addressed the misunderstanding that VLNCs are less harmful than regular cigarettes. Two messages showed specific chemicals in VLNCs, such as arsenic and formaldehyde, communicating that the harmful chemicals in cigarettes will remain after removing nicotine. The third message stated that when nicotine is reduced, some positive outcomes from smoking (e.g., pleasure, stress relief) will also be gone, and only harmful consequences will remain (e.g., lung cancer, erectile dysfunction).
The Alternatives message was aimed at smokers who find it hard to quit nicotine altogether, communicating that nicotine would still be available in alternative, potentially safer, products, such as nicotine patches or e-cigarettes. We mentioned that the policy would apply to all combusted tobacco products in the Alternatives message because we wanted to convey that the alternatives to VLNCs would not include other combusted products (such as cigarillos).
The Compensation message addressed the possible issue of smokers compensating for reduced nicotine by smoking more cigarettes. It cited a study in which smokers given VLNCs reported smoking not more but fewer cigarettes.17 Because our goal was to minimize potential reactance to the policy and narrative persuasive messages (like testimonials) reduce reactance, the message included a testimonial from a smoker on his personal experience with VLNCs.18,19,20
Participants
A marketing research company, The Research Associates, recruited participants from a consumer database of over 100 million US respondents. Participants are recruited into this database using a variety of online (social media advertising) and offline (face-to-face recruiting at large events) outreach efforts. Participants were contacted and screened through phone calls to assess age and tobacco use status. Participants were recruited from Atlanta and San Francisco, cities with contrasting tobacco control environments. In each city, participants were grouped into four smoking status groups, each of which could have different experiences in response to the nicotine reduction policy: 1) exclusive smokers had smoked at least 100 cigarettes in their lifetime and were currently smoking every day or some days (n = 27); 2) dual users both smoked and used e-cigarettes in the past 30 days (n = 25); 3) former smokers had smoked 100 cigarettes in their lives but no longer smoked (n = 32); and 4) young adult nonsmokers were aged 18-30 and had not smoked 100 cigarettes (n = 31). We excluded nonsmokers older than 30 because initiation of tobacco use is extremely low in this population.2 We ran 2 focus groups per smoking status in each city, for a total of 16 focus groups with 115 adults, 73 from Atlanta and 62 from San Francisco. Participants provided informed consent and received $50 for their time.
Procedures
Focus groups took place in April-May 2020 online due to the COVID-19 outbreak. The moderator used a semi-structured guide developed by our team based on the issues important for communicating about VLNCs, beginning with questions to gauge participants’ perceptions of nicotine. Then, participants viewed 8 messages in randomized order. Upon viewing each message, participants completed a brief online evaluation of the messages on perceived message effectiveness (see supplementary material). Next, the moderator facilitated a discussion about the messages, asking about cognitive, affective, and behavioral responses to the messages (e.g., “What is your impression of this message?”; “What do you think this message is trying to tell you?”; “Would this message make you switch from cigarettes to e-cigarettes?”). The moderator specifically called on participants who were not participating to encourage them to engage in the conversation. Focus groups lasted between 75 and 90 minutes. The number of participants per group ranged from 4 to 9 (median = 7.5). Discussions were audio-recorded and transcribed.
Data Analysis
Data were analyzed inductively in NVivo version 12.0, using a thematic analysis approach.21 The first two authors read all the transcripts and developed the initial codes, which were then discussed by the research team. Using the drafted codebook, the first two authors independently coded two randomly selected transcripts and met with the last author to discuss and resolve discrepancies in coding and to revise the codebook. After a master codebook had been developed, the two coders coded the remaining transcripts. Next, the extracted codes from the transcripts were divided among research team members to do in-depth reading and write memos on key themes. The first author then read all the memos and corresponding transcripts and synthesized the results.
Results
Participants were 50% female, 58% White, 22% Black, and 46% had college degrees (Table 1).
Table 1.
Demographics of each smoking status group
| Exclusive smokers |
Dual users | Former smokers |
Nonsmokers | |
|---|---|---|---|---|
| Female | 15 (55.6%) | 13 (52%) | 14 (43.8%) | 13 (41.9%) |
| Race | ||||
| White | 14 (56%) | 17 (68%) | 21 (67.7%) | 12 (42.9%) |
| Black | 7 (28%) | 4 (16%) | 4 (12.9%) | 11 (39.3%) |
| Asian | 1 (4%) | 2 (8%) | 4 (12.9%) | 2 (7.1%) |
| Hispanic/Latino | 0 | 1 (4%) | 1 (3.2%) | 1 (3.6%) |
| Other | 3 (12%) | 1 (4%) | 1 (3.2%) | 2 (7.1%) |
| Education | ||||
| Less than high school | 0 | 0 | 1 (3.1%) | 0 |
| High school | 2 (7.4%) | 2 (8%) | 3 (9.4%) | 2 (6.5%) |
| Some college | 11 (40.7%) | 5 (20%) | 10 (31.3%) | 12 (38.7%) |
| College graduate | 12 (44.4%) | 15 (60%) | 12 (37.5%) | 13 (41.9%) |
| Graduate degree | 2 (7.4%) | 3 (12%) | 6 (18.8%) | 4 (12.9%) |
| Age | ||||
| 18-29 | 5 (18.5%) | 10 (40%) | 2 (6.3%) | 29 (93.5%) |
| 30-44 | 9 (33.3%) | 11 (44%) | 13 (40.6%) | 2 (6.5%) |
| 45-64 | 12 (44.4%) | 4 (16%) | 12 (37.5%) | 0 |
| 65+ | 1 (3.7%) | 0 | 5 (15.6%) | 0 |
Exclusive Smokers’ Reactions
Exclusive smokers said that the Beat cravings and Break the bond efficacy messages moved them toward quitting smoking: “It’s telling me that I can kick the habit.” Some felt hopeful that VLNCs might eventually enable them to quit. One participant said, “If they legitimately lower the levels of nicotine, that's going to bring a lot of hope to people having trouble letting go of the cigarettes.” However, for some exclusive smokers, quitting was not a priority, “I know, it’s not the time. And it’s never going to be time because I don’t have that watch.” The Reason to quit efficacy message, however, was generally viewed by exclusive smokers as ineffective because the image (depicting happy people) did not match the serious message about cigarettes and addiction.
Risk messages received mixed responses from exclusive smokers. The Bar graph risk message prompted some to imagine that they would increase smoking frequency to get enough nicotine. However, the Chemical list risk message elicited several promising responses regarding quitting smoking. For example, one participant said, “This one makes me think about what I'm putting in my mouth. It's very to the point but it’s not condescending. It's just asking you: Is that what you want?” Moreover, exclusive smokers said that this message made them feel scared, “It's scary. It's just not something that comes to mind when you are smoking. So, it brings light to what you really put into your body.” As exclusive smokers talked about their fear of consuming these harmful chemicals, they also suggested that these risk messages might make them want to quit smoking.
Only one exclusive smoker said that the Alternatives message would make them consider switching. Some exclusive smokers explained that people smoked because they liked the taste of cigarettes, and thus, alternative tobacco products would not be satisfying. One exclusive smoker commented:
You know, it doesn't make a difference if that could help me with my nicotine. I just actually want to have a physical cigarette that is going to give me the same relief or satisfaction that I'm looking for that I know I'm going to get from a cigarette. It just feels like nothing else is going to be adequate enough.
The Compensation message referenced a scientific finding that smokers smoked fewer, not more VLNCs. This message was intended to clarify that the nicotine reduction was possible and that smokers do not simply smoke more to get the nicotine they crave. Exclusive smokers did not argue against the idea but focused on whether the evidence presented in the message was credible. A few said they wanted more information about who conducted and funded the study. Many discussed that the brief evidence in the message was not enough and suggested adding the statistic of how many of smokers actually smoked fewer cigarettes, such as “one of 10 or something like that.”
Dual Users’ Reactions
Dual users were mixed in their responses to efficacy messages. Some said that these messages made sense and “hit home.” They found the efficacy messages made smokers “believe that you can take the next steps and cut your cravings.” Others said that the Break the bond efficacy message downplayed the harms of smoking and, therefore, they wanted to smoke more. The majority of dual users, however, said that they would use e-cigarettes instead of quitting tobacco altogether. One participant said, “I would vape more if they come down to this. What's the point paying for cigarettes if they're not going to do anything?” Similar to exclusive smokers, dual users said that the Reason to quit efficacy message had an incongruency between the image and the text.
Several dual users said that viewing the risk messages encouraged them to use only e-cigarettes. Many also talked about quitting cigarettes and only consuming e-cigarettes because they felt that “the good stuff” (i.e., nicotine) was taken away. One dual user said, “I would probably just switch to e-cigarettes if I'm not getting the good things out of cigarettes.” The risk messages also encouraged some dual users to want more information about the chemicals mentioned in the messages.
Many dual users viewed the Alternatives message positively and said that it motivated them to switch completely to e-cigarettes. They commented that it could help reduce smokers’ anger toward VLNCs policy. Yet, many did not believe that this message would encourage other smokers to quit smoking.
The Compensation message elicited little reaction from dual users; a few said that it was relatable but some commented that when the nicotine is reduced, they would want to smoke more.
Former Smokers’ Reactions
Former smokers agreed that the efficacy messages might encourage smokers to quit smoking. However, many were also concerned that they may encourage young people to experiment with VLNCs, akin to saying to young people: “Go ahead, try these.” Former smokers also felt that telling smokers that VLNCs would make it easier to quit might actually reduce the urgency they feel to quit. While some former smokers remarked that these messages were relatable and positive, several commented that the messages minimized the harms of smoking.
When viewing the risk messages, several former smokers expressed strong emotional reaction. One of them commented: “You hear cyanide and like, oh wow! That'll definitely kill you.” But several focused on the non-addictive nature of VLNCs, arguing that these messages minimized smoking-related harms, suggesting that these messages would lead to young people initiating smoking.
Some former smokers said the Alternatives message would lead to smoking relapse. For example, one former smoker said, “It made me think, wow, maybe I can have an occasional cigarette because I won't get addicted to nicotine again.” Several former smokers concluded that this message promoted e-cigarettes, which they viewed negatively. Additionally, they argued that this message was illogical because while it said nicotine in cigarettes was bad, it still advised people to consume nicotine in other products.
Former smokers did not argue against the compensation idea in the Compensation message. Some of them said that the message was relatable. Similar to exclusive smokers, former smokers said that they wanted more information about how the study was conducted.
Nonsmokers' Reactions
The young adult nonsmokers generally said that the efficacy messages merely told young people that they would not get hooked if they start smoking. Although some discussed that the messages were positive and encouraging, many argued that the messages downplayed the risks of smoking and did not scare people away from smoking. Nonsmokers were particularly vocal about the Reason to quit efficacy message, arguing that it would not be effective because the image did not make people see the dangers of smoking.
In response to the risk message group, nonsmokers mostly commented about the effects of these messages on smokers and not on themselves. Nonsmokers argued that the Alternatives message seemed like a commercial produced by the tobacco industry to sell their harmful products. They argued that although replacing VLNCs with alternative tobacco products could work to help smokers to switch, such products were still harmful. They stated that the message may make smokers falsely believe that these products were harmless. In response to the Compensation message, many nonsmokers discussed that they liked this message, but argued that this message should provide some representative statistics. They also discussed that a reference to the cited research should be included in the message so that people knew who conducted the study.
Discussion
This study shows that the FDA’s proposed regulation to reduce nicotine has the potential to be well-received, but that people interpret messages about this regulation from the vantage of their tobacco use experience.
Exclusive smokers
viewed the risk messages and efficacy messages as the most effective. In particular, messages about harmful chemicals in VLNCs generated strong emotions (e.g., fear) and were considered powerful. This is in line with findings that cigarette warnings are most effective when they elicit negative emotions 22,23,24,25 and that mentioning chemicals increases perceived harm of tobacco products.26,27 Many smokers try to quit, but few succeed.28 Exclusive smokers viewed the efficacy messages as encouraging and believed that VLNCs could help them quit. However, the messages appeared less effective for those who did not intend to quit. This is consistent with past research, which has found that efficacy messages would be most likely to have an impact on those wanting to quit.29,30
Dual users
were the only group that was receptive to the message about alternative sources of nicotine. They also indicated that they would switch to e-cigarettes in response to all other types of messages. For dual users, switching to e-cigarettes appears to be a relatively convenient and agreeable option for consuming nicotine in response to the FDA’s proposed nicotine regulation for combustible tobacco.
Former smokers
in the general population know how hard it is to quit31 and likely interpreted messages about nicotine in the context of this experience. Perhaps because former smokers had experienced the struggle to quit, they were critical of messages on “the new kind of cigarettes,” which they perceived could encourage relapse for former smokers or smoking initiation among youth.
Nonsmokers
were concerned about messages focusing on discouraging nonsmokers, including youths. They argued that messages describing the lower harms of alternative tobacco products, particularly e-cigarettes, could make consumers falsely believe that such products were harmless. Overall, nonsmokers’ reactions to our messages indicated that they wanted messages to emphasize a serious loss to people so that the messages would deter nonsmokers from initiating smoking.
Implications
The divergent reactions to different types of messages across various tobacco use groups suggest a continued need to consider these groups in message development. While further research is needed on whether separate targeted campaigns or a single campaign addressing potential pitfalls for each group would be more appropriate, we can make some preliminary recommendations based on the theory and findings from previous research and our study. Rather than creating distinct campaigns for different groups, a single campaign comprising various messages and addressing potential shortfalls of some messages for some groups may be more appropriate. The evidence from this study suggests a campaign that focuses on communicating that VLNCs are still harmful (like the Chemicals message), combined with a message that conveys that VLNCs can make it easier for smokers to quit may be effective.9,10,11,12 We expand on this rationale below.
According to the Extended Parallel Process Model, risk messages that arouse fear and also show a way to avert the risk while raising people’s self-efficacy are effective at motivating protective behaviors.32,33,34 In this study, risk messages evoked some fear with several participants responding with strong reactions, such as “Oh my God” and “That's scary!”, particularly to the Chemical list message. Additionally, our efficacy messages seemed to motivate smokers, particularly those who intend to quit, and made them feel like they are able to do it.
One particular element of the Chemicals message may have contributed to the positive responses to this message among exclusive smokers. Risk messages can sometimes backfire. The communication literature suggests that when message viewers perceive that a message threatens their freedom, they are more likely to reject the message.35 By ending the Chemical list message with a question, the message aimed to avoid controlling language.36 This may have helped reduce perceptions that the message was pressuring participants to accept a persuasive intent by allowing them to answer the question for themselves.
Limited research on messages communicating nicotine reduction in cigarettes found that messages that effectively communicate reduction in addictiveness also reduced perceived risks of VLNCs.37 Our results suggest that explicitly talking about VLNCs as still containing the same amounts of harmful chemicals and causing the same diseases would be a way to address this problem. Thus, messages should combine information on severe risk (that VLNCs still contain the harmful chemicals and cause disease) and an efficacy component (“you can quit”) to ensure that they promote quitting behavior among smokers and do not encourage initiation among nonsmokers and relapse among former smokers.
It is important to highlight the reactions to the message that advised smokers to switch from combusted cigarettes to alternative tobacco products. Only dual users were receptive to this message, likely because they already exhibited preferences for these alternative products and, therefore, may have had relatively high efficacy to switch. This finding is in line with an earlier study showing that only 5.8% of US smokers reported they would switch to non-combusted tobacco product as a result of nicotine reduction.37 Additionally, several participants in our focus groups misperceived the intent of this message, as they viewed the message as promoting smoking initiation and continuation. Nonsmokers were particularly vocal against this strategy because they did not view the alternatives as less harmful and thus would not discourage nonsmokers from initiating smoking. Rather, they considered all types of tobacco products as detrimental. Hence, promoting any of these products seemed illogical to them. As these participants did not differentiate between the various alternatives to cigarettes (e.g., e-cigarettes versus NRT), this finding provided additional evidence of the importance of nuanced messaging around the continuum of risk for nicotine delivery products. Thus, although this message strategy might work with dual users, it should be considered with caution for other groups. Because dual users responded to other messages with intentions to switch to e-cigarettes, using messages that explicitly communicate about the alternative sources of nicotine might not be needed.
Our findings suggest that more research is needed regarding how to counter the incorrect belief that smokers would compensate for reduced nicotine by smoking more cigarettes.13 One potential approach to dispel misperceptions related to unhealthy behaviors is to report scientific research that can correct such misperceptions.38 Our study employed this approach and showed that participants did not argue against the content of the message, but focused on whether the message was believable. Using exemplar evidence from scientific studies (e.g., testimonials) might not be sufficient to change misperceptions about compensatory responses. Indeed, participants stated that statistical evidence was needed because testimony from one smoker was not representative of all smokers. Therefore, if this message strategy is considered, inclusion of representative statistics and trusted research institutions may be important to lend credibility to the message.39 Correcting misinformation is difficult because corrections sometimes reinforce misinformation.40,41 Future research should examine ways to correct this misperception and evaluate whether this misperception would lead to actual compensatory behavior. Initial research shows that even when smokers believe they would need to compensate, they end up not smoking more when VLNCs are the only cigarettes available.17 It is likely that the compensation misperception will not have an effect on smokers’ behavior, but it might result in less support for the policy.
This study is limited by the purposive sample from two cities with diverse demographics, tobacco control regulations, and use rates. The online platform might have restricted group interactions because of the lack of communicative cues (e.g., turn taking, eye contact). Alternatively, this platform might reduce perceived normative pressures that may lead to participants complying with opinion leaders. An online platform also has the potential for selection bias, as participants must have adequate internet connectivity and technology to participate. Yet, during the COVID-19 outbreak, the online platform was the only viable option for this study. The Alternatives message combined e-cigarettes and NRT, and future studies should evaluate messages about e-cigarettes and NRT as substitutes for VLNCs separately. Finally, findings related to the Compensation message showed that comparative effectiveness of testimonial and statistical messages varies dependent on context and individual characteristics. Thus, future studies should evaluate messages focusing on statistical arguments.
In conclusion, communication campaigns on reduced nicotine policy should consider specific target audiences. There might not be a “one-size fits all” message for the public, but campaigns typically include multiple messages which together can address the potential pitfalls of a single message type. In our study, messages highlighting the harmful chemicals in VLNCs seemed to be perceived as effective across all groups. They should be combined with efficacy messages that might be particularly helpful for exclusive smokers thinking about quitting because such messages were perceived by these smokers as giving them hope to give up. However, attention should be paid to the congruency between images and text for this message type, and positively framed efficacy messages should not be shown alone to nonsmokers and former smokers because they perceived them as promoting VLNCs. Messages focusing on alternative sources of nicotine might not be necessary as dual users indicated willingness to switch to e-cigarettes in response to all types of messages and other groups were not interested in alternative sources of nicotine. These results should be considered in future messages designed to communicate about VLNCs.
Supplementary Material
What this paper adds?
The FDA is considering lowering the nicotine in cigarettes to non-addictive levels to help smokers quit and save lives. How to communication about this regulation remains a challenge.
In a study with 16 focus groups that included exclusive smokers, dual users, former smokers, and nonsmokers, we found that different message strategies might be needed to communicate to each target audience group.
Efficacy and risk messages were well-received by exclusive smokers. All types of messages encouraged dual users to switch to e-cigarettes. Former smokers were concerned that these messages might encourage experimentation among youth. Only messages emphasizing a serious loss to smokers’ health were perceived as effective by nonsmokers.
Our divergent findings across groups suggest a continued need to consider these groups in message development and incorporate diverse messages into a communication campaign about reduced nicotine policy.
Acknowledgments
Funding: Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health and the Food and Drug Administration Center for Tobacco Products (R01CA239308). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Food and Drug Administration.
References
- 1.World Health Organization. WHO global report on trends in prevalence of tobacco smoking, 2015. July 20, 2020. https://apps.who.int/iris/bitstream/handle/10665/156262/9789241564922_eng.pdf?sequence=1
- 2.U.S. Department of Health and Human Services. The health consequences of smoking: 50 years of progress: a report of the Surgeon General, 2014. July 20, 2020. https://www.ncbi.nlm.nih.gov/books/NBK179276/pdf/Bookshelf_NBK179276.pdf
- 3.Benowitz NL. Nicotine addiction. N Engl J Med. 2010;362(24):2295–2303. doi: 10.1056/NEJMra0809890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Apelberg BJ, Feirman SP, Salazar E, et al. Potential public health effects of reducing nicotine levels in cigarettes in the United States. N Engl J Med. 2018;378(18):1725–1733. doi: 10.1056/NEJMsr1714617 [DOI] [PubMed] [Google Scholar]
- 5.Gottlieb S, Zeller M. A nicotine-focused framework for public health. N Engl J Med. 2017;377(12):1111–1114. doi: 10.1056/NEJMp1707409 [DOI] [PubMed] [Google Scholar]
- 6.O’Brien EK, Nguyen AB, Persoskie A, et al. U.S. adults’ addiction and harm beliefs about nicotine and low nicotine cigarettes. Prev Med. 2017;96:94–100. doi: 10.1016/j.ypmed.2016.12.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Denlinger-Apte RL, Joel DL, Strasser AA, et al. Low nicotine content descriptors reduce perceived health risks and positive cigarette ratings in participants using very low nicotine content cigarettes. Nicotine Tob Res. 2017;19(10):1149–1154. doi: 10.1093/ntr/ntw320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Byron MJ, Jeong M, Abrams DB, et al. Public misperception that very low nicotine cigarettes are less carcinogenic. Tob Control. 2018;27(6):712–714. doi: 10.1136/tobaccocontrol-2017-054124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Denlinger-Apte RL, Cassidy RN, Colby SM, et al. Effects of Cigarette Nicotine Content and Menthol Preference on Perceived Health Risks, Subjective Ratings, and Carbon Monoxide Exposure Among Adolescent Smokers. Nicotine & Tobacco Res. 2019;21(Supplement1), 56–62. 10.1093/ntr/ntz127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bottorff JL, Johnson JL, Moffat B, et al. Adolescent constructions of nicotine addiction. The Canadian Journal of Nursing Research, 2004;36(1), 22–39. [PubMed] [Google Scholar]
- 11.O’Loughlin J, Kishchuk N, DiFranza J, et al. The hardest thing is the habit: A qualitative investigation of adolescent smokers’ experience of nicotine dependence. Nicotine & Tobacco Re, 2002;4(2), 201–209. 10.1080/14622200210123000 [DOI] [PubMed] [Google Scholar]
- 12.Mumford EA, Pearson JL, Villanti AC, et al. Nicotine and e-cigarette beliefs and policy support among US smokers and nonsmokers. Tob Regul Sci. 2017;3(3):293–305. [Google Scholar]
- 13.Benowitz NL, Donny EC, Edwards KC, et al. The role of compensation in nicotine reduction. Nicotine Tob Res. 2019. Dec 23;21(Suppl 1):S16–S18. doi: 10.1093/ntr/ntz120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith TT, Koopmeiners JS, White CM, et al. The impact of exclusive use of very low nicotine cigarettes on compensatory smoking: an inpatient crossover clinical trial. Cancer Epidemiol Biomarkers Prev. 2020;29(4):880–886. doi: 10.1158/1055-9965.EPI-19-0963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith TT, Koopmeiners JS, Hatsukami DK, et al. Mouth-level nicotine intake estimates from discarded filter butts to examine compensatory smoking in low nicotine cigarettes. Cancer Epidemiol Biomarkers Prev. 2020;29(3):643–649. doi: 10.1158/1055-9965.EPI-19-0905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Byron MJ, Hall MG, King JL, et al. Reducing nicotine without misleading the public: descriptions of cigarette nicotine level and accuracy of perceptions about nicotine content, addictiveness, and risk. Nicotine Tob Res. 2019;21(Supplement_1):S101–S107. doi: 10.1093/ntr/ntz161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Denlinger-Apte RL, White CM, Donny EC, et al. “I actually finally feel like the cigarettes aren’t controlling me.”–Interviews with participants smoking very low nicotine content cigarettes during a residential study. Drug and Alcohol Dep, 2020.108465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Braddock K, & Dillard JP Meta-analytic evidence for the persuasive effect of narratives on beliefs, attitudes, intentions, and behaviors. Communication Monographs, 2016;83(4), 446–467. doi: 10.1080/03637751.2015.1128555 [DOI] [Google Scholar]
- 19.Moyer-Gusé E, & Nabi RL Explaining the effects of narrative in an entertainment television program: Overcoming resistance to persuasion. Human Comm Res, 2010;36(1), 26–52. Doi: 10.1111/j.1468-2958.2009.01367.x [DOI] [Google Scholar]
- 20.Ratcliff CL, & Sun Y (2020). Overcoming resistance through narratives: Findings from meta-analytic review. Human Comm Res, 2020. Doi: 10.1093/hcr/hqz017 [DOI] [Google Scholar]
- 21.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 22.Anshari D, Yong H-H, Borland R, et al. Which type of tobacco product warning imagery is more effective and sustainable over time? A longitudinal assessment of smokers in Canada, Australia and Mexico. BMJ Open. 2018;8(7):e021983. doi: 10.1136/bmjopen-2018-021983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cho YJ, Thrasher JF, Yong H-H, et al. Path analysis of warning label effects on negative emotions and quit attempts: a longitudinal study of smokers in Australia, Canada, Mexico, and the US. Soc Sci Med. 2018;197:226–234. doi: 10.1016/j.socscimed.2017.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thrasher JF, Brewer NT, Niederdeppe J, et al. Advancing tobacco product warning labels research methods and theory: a summary of a grantee meeting held by the US National Cancer Institute. Nicotine Tob Res. 2019;21(7):855–862. doi: 10.1093/ntr/nty017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hall MG, Sheeran P, Noar SM, et al. Negative affect, message reactance and perceived risk: how do pictorial cigarette pack warnings change quit intentions? Tob Control. 2018;27(e2):e136–e142. doi: 10.1136/tobaccocontrol-2017-053972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Owusu D, Lawley R, Yang B, et al. ‘The lesser devil you don’t know’: a qualitative study of smokers’ responses to messages communicating comparative risk of electronic and combusted cigarettes. Tob Control. 2020;29:217–223. doi: 10.1136/tobaccocontrol-2018-054883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Popova L, McDonald EA, Sidhu S, et al. Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: implications for health education and research. Addiction. 2017;(10):1821–1829. doi: 10.1111/add.13854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Walton K, Wang TW, Schauer GL, et al. State-specific prevalence of quit attempts among adult cigarette smokers - United States, 2011-2017. Morb Mortal Wkly Rep. 68(28):621–626. doi: 10.15585/mmwr.mm6828a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Moodie C Adult smokers’ perceptions of cigarette pack inserts promoting cessation: a focus group study. Tob Control. 2018;27(1):72–77. doi: 10.1136/tobaccocontrol-2016-053372 [DOI] [PubMed] [Google Scholar]
- 30.Thrasher JF, Islam F, Davis RE, et al. Testing cessation messages for cigarette package inserts: findings from a best/worst discrete choice experiment. Int J Environ Res Public Health. 2018;15(2):1–21. doi: 10.3390/ijerph15020282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults - United States, 2018. Morb Mortal Wkly Rep. 68(45):1013–1019. doi: 10.15585/mmwr.mm6845a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Witte K Putting the fear back into fear appeals: the extended parallel process model. Commun Monogr. 1992;59(4):329–349. doi: 10.1080/03637759209376276 [DOI] [Google Scholar]
- 33.Popova L Scaring the snus out of smokers: testing effects of fear, threat, and efficacy on smokers’ acceptance of novel smokeless tobacco products. Health Commun. 2014;29(9):924–936. doi: 10.1080/10410236.2013.824063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Popova L The extended parallel process model: illuminating the gaps in research. Health Educ Behav. 2012;39(4):455–473. doi: 10.1177/1090198111418108 [DOI] [PubMed] [Google Scholar]
- 35.Brehm SS, Brehm JW. Psychological reactance: a theory of freedom and control. Academic Press; 2013. [Google Scholar]
- 36.Miller CH, Lane LT, Deatrick LM, et al. Psychological reactance and promotional health messages: the effects of controlling language, lexical concreteness, and the restoration of freedom. Hum Commun Res. 2007;33(2):219–240. Doi: 10.1111/j.1468-2958.2007.00297.x [DOI] [Google Scholar]
- 37.Popova L, Owusu D, Nyman AL, et al. Effects of framing nicotine reduction in cigarettes on anticipated tobacco product use intentions and risk perceptions among us adult smokers. Nicotine Tob Res. 2019;21(Supplement_1):S108–S116. doi: 10.1093/ntr/ntz146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shi R, Feldman R, Liu J, et al. The dilemma of correcting nicotine misperceptions: nicotine replacement therapy versus electronic cigarettes. Health Commun. 2020:1–11. doi: 10.1080/10410236.2020.1800288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weaver SR, Jazwa A, Popova L, et al. Worldviews and trust of sources for health information on electronic nicotine delivery systems: effects on risk perceptions and use. SSM - Popul Health. 2017;3:787–794. doi: 10.1016/j.ssmph.2017.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lewandowsky S, Ecker UK, Seifert CM, et al. Misinformation and its correction: Continued influence and successful debiasing. Psychological science in the public interest. 2012;13(3): 106–131. [DOI] [PubMed] [Google Scholar]
- 41.Walter N, Tukachinsky R. A meta-analytic examination of the continued influence of misinformation in the face of correction: How powerful is it, why does it happen, and how to stop it? Communication Res. 2020;47(2):155–177. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.