Abstract
Introduction:
Prophylactic administration of doxycycline is regarded as a potential new public health strategy to combat the rising rates of Chlamydial trachomatis infections and syphilis among men who have sex with men (MSM). We conducted a survey-based study to evaluate how community members and healthcare providers in Southern California would perceive doxycycline pre-exposure/post-exposure prophylaxis (PrEP/PEP) to predict its acceptability and identify potential areas of concern.
Methods:
We conducted an online cross-sectional survey among community members who identify as MSM and healthcare providers with prescribing authority in Southern California to investigate the current attitudes toward doxycycline PrEP/PEP, including their willingness to accept. We analyzed the data using descriptive statistics and binary logistic regression.
Results:
Among 212 enrolled community member participants, 67.5% indicated they would take doxycycline PrEP/PEP if offered by their provider. Higher acceptability was significantly associated with several characteristics, including recent history of bacterial sexually transmitted infection diagnosis and current use of HIV PrEP. For healthcare providers, 89.5% of 76 enrolled participants expressed willingness to prescribe doxycycline PrEP/PEP to their patients if recommended by the Centers for Disease Control and Prevention, but only 43.4% were willing if not. Both community members and healthcare providers demonstrated high levels of concern toward possible drug resistance.
Conclusion:
Doxycycline PrEP/PEP as a preventive strategy against chlamydial infections and syphilis would likely be accepted among community members and healthcare providers. Clear guidelines from public health officials and further clarification on the strategy’s potential impact on developing drug resistance may be necessary to ensure successful implementation.
Keywords: Doxycycline, prophylaxis, chlamydia, syphilis, men who have sex with men
Short Summary
A survey-based study found that community members who identify as MSM and healthcare providers in Southern California are likely to accept doxycycline pre-exposure/post-exposure prophylaxis to prevent chlamydial infections and syphilis.
Introduction
In Southern California and nationwide, rates of sexually transmitted infections (STIs) caused by bacterial pathogens are increasing, particularly among men who have sex with men (MSM).1–3 In 2018, 10.8 cases per 100,000 population of primary and secondary syphilis were reported in the United States, a marked increase from just 4.4 reported back in 2008.1 Among the total 35,063 cases reported in 2018, MSM accounted for 53.5%.1 The disproportionately elevated STI burden among MSM can be attributed to several factors, but emerging evidence suggests that increased frequency of condomless sex may be one of the leading causes. This phenomenon appears to be closely connected to the recent advancement of antiretroviral therapy and use of human immunodeficiency virus pre-exposure prophylaxis (HIV PrEP), which may have decreased the perceived risk associated with condomless sexual acts (i.e. risk compensation). 4–7
Current STI prevention strategies focused on promoting regular condom use and frequent testing appear to be inadequate for controlling the disease burden among MSM, as evidenced by the consistently worsening state of the epidemic.8 In recent years, prophylactic use of antibiotics, specifically doxycycline, has shown potential to serve as an efficacious strategy for preventing chlamydial infections and syphilis in this population.9–11 The current suggested regimen for doxycycline pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) is 100mg of doxycycline monohydrate/hyclate a day throughout the duration of risk exposure or 200mg within 72 hours of exposure event (maximum of six pills a week), respectively.9,12 Preliminary randomized controlled trials found that those taking doxycycline PrEP/PEP showed about 70% of risk reduction in acquiring a chlamydial infection or syphilis compared to their respective control groups.11,12
Doxycycline is a widely available second-generation tetracycline associated with good tolerability and low risk for severe side effects.13 In fact, clinicians have routinely utilized long-term administration of doxycycline for malaria prophylaxis and acne management.10,14 There are limited studies investigating the effects of long-term doxycycline exposure with variable findings. Few reports of concurrent adverse effects (e.g. irritable mood, suicidality, esophagitis, esophageal ulceration, diarrhea, intracranial hypertension) exist.14 The majority of such cases have resolved or improved upon discontinuation.14 However, recent studies on the impact of long-term antibiotic exposure on the human intestinal microbiota have shown that effects may persist for months after discontinuation.15,16
Assessing the community’s willingness to accept doxycycline PrEP/PEP, in addition to evaluating potential sources of concern, is necessary to gauge demand, predict uptake, and better inform the direction toward successful implementation. In this study, we conducted a survey among community members and healthcare providers in Southern California to evaluate their interest and attitudes regarding doxycycline PrEP/PEP.
Methods
Study Population
We conducted a cross-sectional online study using two standardized surveys, one for community members and another for healthcare providers. Responses were collected anonymously between June and September 2020.
We recruited community members using various methods, including recruitment posts on social networking websites, banner ads on a mobile dating application (i.e., Grindr), and direct recruitment through local clinics and community-based organizations. Participants were offered to enter a raffle for a chance to win a $200 value prize. Anyone over the age of 18 years residing in Southern California who self-identified as MSM was eligible to participate. For the purpose of this study, “Southern California” was geographically defined as any of ten counties surrounding major cities of focus including Los Angeles, Palm Springs, San Diego, and Riverside. The cities of focus were chosen based on their reputation for high population of MSM and the presence of relevant community-based organizations.
Healthcare providers were recruited by purposive sampling through established networks of individual providers and local community-based clinics. Clinics yielding at least four responses were offered gift certificates ranging from $15 to $25. Any medical professional with prescribing authority practicing in Southern California was eligible to participate, namely physicians, physician assistants and nurse practitioners.
Survey Methods
For community member-targeted surveys, we collected self-reported demographics and information about their past and current experience with STIs and HIV PrEP/PEP. Participants were asked to read a brief text outlining the concept of prophylactic antibiotics for chlamydia and syphilis prevention, suggested regimen, possible side effects, and preliminary data on efficacy. Questions regarding their willingness to take doxycycline PrEP/PEP and level of concern regarding different aspects of the strategy were asked.
For healthcare provider-targeted surveys, we collected occupational information including job title, years in profession, and area of practice. A brief text outlining the concept of doxycycline PrEP/PEP, suggested dosage, possible side effects, and preliminary data on efficacy were provided. The participants’ level of agreement regarding different statements about the strategy were asked, including their willingness to prescribe doxycycline prophylactically to their patients who are MSM either with or without Centers for Disease Control and Prevention’s recommendation.
Both questionnaires primarily utilized 5-point Likert scales for opinion-based questions. Surveys were administered exclusively online on QualtricsXM and designed to take less than 3 minutes for completion. Full versions of the questionnaires are available in the appendix.
Sample Size Consideration
A previous study showed that the acceptability of pharmacological intervention in preventing bacterial STIs was 52.7% among 2,095 MSM surveyed.17 Assuming the acceptability of the intervention in this study target population is 50%, we calculated that the necessary sample size for a precision of 10% and a confidence level of 95% would be 97 participants for community members.
Data Analysis
All statistical analyses were performed using IBM SPSS Statistics V25. We used descriptive statistics to describe the study population by analyzing the demographic, behavioral, and sexual health characteristics of community members and occupational information of healthcare providers. We analyzed acceptability by converting the 5-point Likert scale to a binary variable (i.e., “Definitely not/disagree,” “Probably not/disagree” and “Neutral/I don’t know” vs. “Probably yes/agree” and “Definitely yes/agree”). In order to assess statistical differences on acceptability among various characteristic variables, we performed Pearson’s χ2 analysis based on the converted binary variable. When significant, we conducted a binary logistic regression analysis. Responses given on uni-directional 5-point Likert scale were analyzed by assigning a numerical value to each ascending level of response (i.e. “Not concerned at all”=1, “Very concerned”=5) and computing the average.
Ethical Approval and Study Funding
The University of California, Los Angeles (UCLA) Institutional Review Board granted approval for this study (IRB#20–000532). The Department of Medicine at David Geffen School of Medicine at UCLA, Team Klausner Saving Lives, and UCLA Center for AIDS Research National Institutes of Health grant number 5P30 AI028697 provided the funding.
Results
A total of 312 community members participated in the survey, of which 232 were considered eligible. Ineligible participants included non-transgender women, heterosexual cisgender men, those under age 18 years, and those with residence outside Southern California. After excluding 20 incomplete responses, we included 212 responses in the final analysis. For healthcare providers, a total of 97 participated, 85 were eligible (ineligible participants included those without prescription authority and providers outside Southern California), and 76 complete responses were included in the analysis.
Characteristics of Study Population
The median age of community members surveyed was 31 years (range: 18–76 years) with nearly all identifying as male (96.2%) (Table 1). Nearly all identified as gay (84.4%) or bisexual (12.7%). Most participants were white (48.1%), black (17.0%), or Asian (17.0%) [Table 1].
Table 1.
Demographic, behavioral, and sexual health characteristics of community members associated with willingness to use doxycycline PrEP/PEP (n=212) – Southern California, 2020
| Study population |
Willing to use doxycycline PrEP/PEP |
||||
|---|---|---|---|---|---|
| n | % | n | % | p-value* | |
|
| |||||
| Age (years) | Median: 31, Range: 18–76 | ||||
| Gender | |||||
| Male | 204 | 96.2 | 136 | 66.7 | 0.45 |
| Trans women | 1 | 0.5 | 1 | 100.0 | |
| Other/Unknown ** | 7 | 3.3 | 6 | 85.7 | |
| Sexual Orientation | |||||
| Gay or homosexual | 179 | 84.4 | 117 | 65.4 | 0.15 |
| Bisexual | 27 | 12.7 | 20 | 74.1 | |
| Other/Unknown *** | 6 | 2.8 | 6 | 100.0 | |
| Ethnicity | |||||
| Hispanic or Latino/Latina/Latinx | 81 | 38.2 | 61 | 75.3 | 0.06 |
| Not Hispanic or Latino/Latina/Latinx | 130 | 61.3 | 82 | 63.1 | |
| Other/Unknown | 1 | 0.5 | 0 | 0.0 | |
| Race | |||||
| African American/Black American | 27 | 12.7 | 20 | 74.1 | 0.03 |
| American Indian/Alaskan Native | 1 | 0.5 | 1 | 100.0 | |
| Asian | 30 | 14.2 | 15 | 50.0 | |
| Caucasian/White | 84 | 39.6 | 62 | 73.8 | |
| Multiracial **** | 24 | 11.3 | 11 | 45.8 | |
| Other/Unknown | 46 | 21.7 | 34 | 73.9 | |
| County of Residence | |||||
| Los Angeles County | 133 | 62.7 | 90 | 67.7 | 0.55 |
| Riverside County | 31 | 14.6 | 23 | 74.2 | |
| Orange County | 21 | 9.9 | 11 | 52.4 | |
| San Diego County | 15 | 7.1 | 11 | 73.3 | |
| Other/Unknown | 12 | 5.7 | 8 | 66.7 | |
| Concerns about contracting STI | |||||
| Not at all concerned | 28 | 13.2 | 15 | 53.6 | <0.01 |
| Slightly concerned | 40 | 18.9 | 22 | 55.0 | |
| Somewhat concerned | 29 | 13.7 | 19 | 65.5 | |
| Moderately concerned | 57 | 26.9 | 40 | 70.2 | |
| Very concerned | 57 | 26.9 | 46 | 80.7 | |
| Did not answer | 1 | 0.5 | 1 | 100.0 | |
| Bacterial STI diagnosis in the last 12 months (n=211) | 73 | 34.4 | 62 | 84.9 | <0.01 |
| Frequency of condom use during anal sex | |||||
| Never | 66 | 31.1 | 42 | 63.6 | 0.55 |
| Sometimes | 94 | 44.3 | 67 | 71.3 | |
| Always | 33 | 15.6 | 20 | 60.6 | |
| No history of anal sex in the past 12 months | 19 | 9.0 | 14 | 73.7 | |
| HIV-infected ***** | 34 | 16.0 | 25 | 73.5 | 0.41 |
| Currently on HIV PrEP (n=178) | 70 | 33.0 | 57 | 81.4 | <0.01 |
| History of HIV PEP use (n=179) | 43 | 20.3 | 33 | 76.7 | 0.14 |
Based on Pearson’s χ2 test.
Includes non-binary, genderqueer, and unspecified.
Includes pansexual, queer, and unspecified.
Defined as participants who report two or more races.
Categorization is based on responses regarding current HIV PrEP use.
STI, sexual transmitted infections; HIV, human immunodeficiency virus; PrEP, pre-exposure prophylaxis; PEP, post-exposure prophylaxis
Most healthcare provider participants were physicians, either Doctors of Medicine (MD, 67.1%) or Doctors of Osteopathic Medicine (DO, 5.3%) (Table 2). Nurse practitioners (17.1%) and physician assistants (8%) comprised more than a quarter of the sample population. Years of practice varied among participants, but 57.9% had more than 10 years of clinical practice [Table 2]. Los Angeles County represented about 60% of participants in each sample population.
Table 2.
Occupational characteristics of healthcare providers (n=76) - Southern California, 2020
| n | % | |
|---|---|---|
|
| ||
| Job title | ||
| MD | 51 | 67.1 |
| DO | 4 | 5.3 |
| PA | 8 | 10.5 |
| APRN | 13 | 17.1 |
| Years of practice | ||
| 0–10 years | 32 | 42.1 |
| 11–20 years | 19 | 25 |
| 21+ years | 25 | 32.9 |
| Location of practice (county) | ||
| Los Angeles County | 46 | 60.5 |
| San Diego County | 16 | 21.1 |
| Riverside County | 7 | 9.2 |
| San Bernardino County | 4 | 5.3 |
| Orange County | 1 | 1.3 |
| Other/Unknown | 2 | 2.6 |
MD, Medical Doctor; DO, Doctor of Osteopathy; PA, Physician Assistant; APRN, Advanced Practice Registered Nurse
Willingness to Take or Prescribe Doxycycline PrEP/PEP
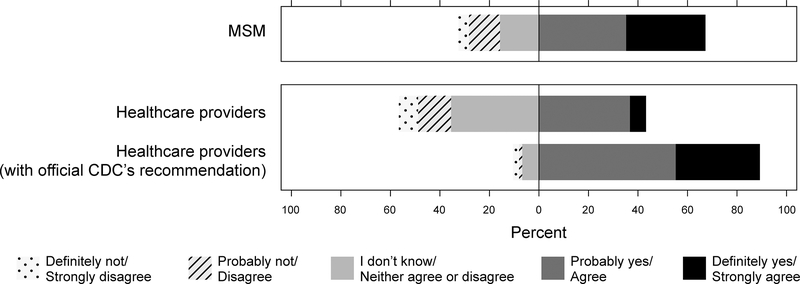
About two-thirds of community members (67.5%) responded either “Probably yes” or “Definitely yes” to taking doxycycline PrEP/PEP if offered by their provider [Figure 1]. For healthcare providers, less than half (43.4%) responded either “Agree” or “Strongly Agree” when asked if they would be willing to prescribe doxycycline PrEP/PEP to their patients who are MSM. However, when providers were again asked the identical question but under the hypothetical condition that CDC has recommended the strategies, acceptability increased to 89.5%.
Figure 1.
Willingness to take or prescribe doxycycline prophylactically for chlamydial infection and syphilis among community members (n=212) and healthcare providers (n=76) – Southern California, 2020
Preference of Drug Regimen
With regard to regimen, 52.4% of community members preferred one-time dosing required by doxycycline PEP, while 40.1% chose daily dosing demanded by PrEP.
Concerns Toward Doxycycline PrEP/PEP
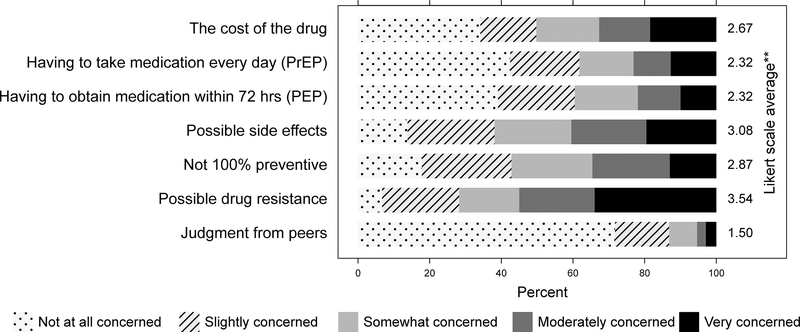
On a scale from “Not concerned at all=1” to “Very concerned=5”, community members reported the highest level of concern for “possible drug resistance” (Likert average=3.54) and “possible side effects” (Likert average=3.08) [Figure 2]. Concerns associated with “judgment from peers” were lowest (Likert average=1.50). Similarly, 80.3% of healthcare providers claimed they were concerned about drug resistance regarding prophylactic use of antibiotics.
Figure 2. Concerns regarding various aspects of doxycycline PrEP/PEP among community members (n=205–212*).
*Sample size varies for each question due to incomplete responses.
**Determined by assigning a numerical value to each level of response (i.e. “Not concerned at all”=1, “Very concerned”=5) and computing the average.
Factors Associated with Acceptability of Doxycycline PrEP/PEP
We identified several factors associated with acceptability among community members: race, concerns about contracting STIs, recent history of bacterial STI diagnosis, and current use of HIV PrEP. The odds of agreeing to doxycycline PrEP/PEP was lower for participants who self-identified as Asian (OR=0.289, 95%CI: 0.098–0.850, p=0.02) or multiracial (OR=0.146, 95%CI: 0.043–0.496, p=<0.01) compared to who identified as Caucasian/White. Linear-by-linear association test also revealed a trend of higher acceptability of doxycycline PrEP/PEP with increasing levels of concern regarding STIs. Those with history of bacterial STI diagnosis within the past 12 months had 2.8 times the odds of accepting doxycycline PrEP/PEP than those without (OR=2.803, 95%CI: 1.218–6.448, p=0.02), and those who are currently on HIV PrEP had 3.7 times the odds than those who are not (OR=3.679, 95%CI: 1.642–8.243, p=<0.01). Other demographic factors and sexual behavior characteristics, like patterns of condom use, showed no statistically significant associations with acceptability.
Discussion
We surveyed community members and healthcare providers in Southern California recruited from social media outlets, health clinics, and community-based organizations to assess the public’s attitudes and perspectives toward a new pharmacological strategy designed to prevent chlamydial infections and syphilis among MSM. Our data suggest that doxycycline PrEP/PEP will largely be accepted, especially among those who are currently on HIV PrEP or have a recent diagnosis of bacterial STI. We also found that most healthcare providers will also accept doxycycline PrEP/PEP if recommended by the CDC. In addition, we found that one of the most common concerns expressed by community members and healthcare providers alike was regarding the strategy’s impact on antimicrobial resistance.
Our findings on acceptability among community members are generally consistent with prior studies, which have reported acceptability rates ranging from 40% to 80%.17–19 However, our findings on decreased acceptability among Asians when compared to Caucasian/Whites seem to contradict results reported in a recent multi-city study conducted in Canada, which indicated Asians were about twice as likely to be accepting.18 Increased acceptability associated with high levels of personal STI-related concerns, history of STI diagnosis, and current HIV PrEP use was a predictable outcome, however. These variables reflect the participants’ heightened baseline awareness and vigilance toward STIs, which would reasonably lead to increased acceptability. The association between acceptability and current HIV PrEP use is especially noteworthy when considering the potential synergistic effect these two prophylactic strategies can bring to both individual wellness and public health, in particular among those at high risk for both infections (e.g. core groups).
In addition to acceptability, we also attempted to evaluate potential sources of concern that many may have regarding the strategy. We found that risks associated with antimicrobial resistance appear to be a significant concern among community members and providers alike. Currently, despite decades-long history of clinical use, there is no clear and direct evidence on the existence of tetracycline resistance among Chlamydia trachomatis or Treponema pallidum strains (doxycycline is not indicated for prevention or treatment of Neisseria gonorrhoeae, which has developed resistance to multiple antimicrobials).20–22 This lack of evidence on resistance must be emphasized if doxycycline PrEP/PEP becomes standard. Furthermore, empirical data on the effect of doxycycline PrEP/PEP specifically on the gut microbiome are expected to be available in the near future as several clinical trials are currently underway.23,24
Our findings also suggest that most healthcare providers will accept doxycycline PrEP/PEP, but under the important distinction that the strategy has been recommended by the CDC. Prophylactic use of doxycycline for STI prevention is not mentioned in the latest edition of STD Treatment Guidelines released by the CDC at this time.25 However, providers may still prescribe it based on their own clinical judgment. As such, anecdotal evidence and preliminary survey data suggest that some members of the community in the U.S. had already initiated or experienced doxycycline PrEP/PEP, though prevalence is uncertain.26 It appears that clear guidelines and accurate messaging from public health officials regarding doxycycline PrEP/PEP may already be needed.
Several limitations exist in this study. First, our survey-based methodology introduces potential for several biases. Because recruitment primarily occurred through convenience sampling at online communities and local clinics, there is potential for recruitment bias. Social desirability bias and recall bias may also be present since responses were self-reported. However, it is noteworthy that high acceptability for doxycycline PEP was also demonstrated in a recent non-survey study conducted in Philadelphia, where clinicians offered free supplies of doxycycline PEP to visitors at an HIV PrEP clinic.27 Although it is not direct evidence, the high uptake observed in this study (78.7%, n=237) may suggest that those who expressed willingness on the survey are also likely to accept the strategy if offered in an actual clinical setting. Second, the survey may not have been comprehensive in addressing or capturing all potential concerns, as the questionnaire only provided a list of preselected choices without an opportunity for participants to enter in their own subjective response.
New approaches to curbing the incidence of bacterial STIs are urgently needed. Our study demonstrates that doxycycline PrEP/PEP is potentially acceptable among both the targeted population and prescribers. While we may have to wait until more robust data on the safety profile of doxycycline PrEP/PEP and its effect on the gut microbiome to emerge before widespread implementation, it is clear that many will readily accept the strategy.
Supplementary Material
Footnotes
The authors have no conflict of interest to declare.
Contributor Information
Justin J. Park, Department of Medicine at the David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA.
Chrysovalantis Stafylis, Department of Medicine at the David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA.
Daniel D. Pearce, Borrego Community Health Foundation, Riverside, CA and Department of Medicine at Loma Linda University School of Medicine, Loma Linda, CA.
Jeff Taylor, HIV+Aging Research Project-Palm Springs, Palm Springs, CA.
Susan J. Little, Department of Medicine at the University of California, San Diego School of Medicine, La Jolla, CA.
Noah Kojima, Department of Medicine at the David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA.
Aleksandr M. Gorin, Department of Medicine at the David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA.
Jeffrey D. Klausner, Department of Medicine at the David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA.
References
- 1.Center for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2018; 2019. [Google Scholar]
- 2.Werner RN, Gaskins M, Nast A, Dressler C. Incidence of sexually transmitted infections in men who have sex with men and who are at substantial risk of HIV infection – A meta-analysis of data from trials and observational studies of HIV pre-exposure prophylaxis. PLoS One. 2018; 13(12): 1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.California Department of Public Health. Sexually Transmitted Diseases in California - 2018 Executive Summary. Available at: http://www.cdph.ca.gov/data/statistics/Documents/STD-Data-2013-Report.pdf.
- 4.Traeger MW, Schroeder SE, Wright EJ, et al. Effects of Pre-exposure Prophylaxis for the Prevention of Human Immunodeficiency Virus Infection on Sexual Risk Behavior in Men Who Have Sex with Men: A Systematic Review and Meta-analysis. Clin Infect Dis. 2018; 67(5): 676–686. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen VK, Greenwald ZR, Trottier H, et al. Incidence of sexually transmitted infections before and after preexposure prophylaxis for HIV. AIDS. 2018; 32(4): 523–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Traeger MW, Cornelisse VJ, Asselin J, et al. Association of HIV Preexposure Prophylaxis With Incidence of Sexually Transmitted Infections Among Individuals at High Risk of HIV Infection. JAMA. 2019; 321(14): 1380–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Montaño MA, Dombrowski JC, Dasgupta S, et al. Changes in Sexual Behavior and STI Diagnoses Among MSM Initiating PrEP in a Clinic Setting. AIDS Behav. 2019; 23(2): 548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerani RP, Handsfield HH, Stenger MS, et al. Rising rates of syphilis in the era of syphilis elimination. Sex Transm Dis. 2007; 34(3): 154–161. [DOI] [PubMed] [Google Scholar]
- 9.Grant JS, Stafylis C, Celum C, et al. Doxycycline Prophylaxis for Bacterial Sexually Transmitted Infections. Clin Infect Dis. 2020; 70(6): 1247–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Siguier M, Molina JM. Doxycycline Prophylaxis for Bacterial Sexually Transmitted Infections: Promises and Perils. ACS Infect Dis. 2018; 4(5): 660–663. [DOI] [PubMed] [Google Scholar]
- 11.Bolan RK, Beymer MR, Weiss RE, Flynn RP, Leibowitz AA, Klausner JD. Doxycycline Prophylaxis to Reduce Incident Syphilis among HIV-Infected Men Who Have Sex With Men Who Continue to Engage in High-Risk Sex. Sex Transm Dis. 2015; 42(2): 98–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Molina JM, Charreau I, Chidiac C, et al. Post-exposure prophylaxis with doxycycline to prevent sexually transmitted infections in men who have sex with men: an open-label randomised substudy of the ANRS IPERGAY trial. Lancet Infect Dis. 2018; 18(3): 308–317. [DOI] [PubMed] [Google Scholar]
- 13.Peyriere H, Makinson A, Marchandin H, Reynes J. Doxycycline in the management of sexually transmitted infections. J Antimicrob Chemoth. 2018; 73(3): 553–563. [DOI] [PubMed] [Google Scholar]
- 14.National Academies of Sciences, Engineering, and Medicine. Doxycycline. In: Savitz DA, Styka AN, eds. Assessment of Long-Term Health Effects of Antimalarial Drugs When Used for Prophylaxis. Washington, DC: The National Academies Press; 2020: 247–290. [PubMed] [Google Scholar]
- 15.Rashid MU, Zaura E, Buijs MJ, et al. Determining the long-term effect of antibiotic administration on the human normal intestinal microbiota using culture and pyrosequencing methods. Clin Infect Dis. 2015; 60(Suppl 2): S77–S84. [DOI] [PubMed] [Google Scholar]
- 16.Jernberg C, Löfmark S, Edlund C, Jansson JK. Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology. 2010; 156(11): 3216–3223. [DOI] [PubMed] [Google Scholar]
- 17.Wilson DP, Prestage GP, Gray RT, et al. Chemoprophylaxis is likely to be acceptable and could mitigate syphilis epidemics among populations of gay men. Sex Transm Dis. 2011; 38(7): 573–579. [DOI] [PubMed] [Google Scholar]
- 18.Fusca L, Hull M, Ross P, et al. High Interest in Syphilis Pre-exposure and Post-exposure Prophylaxis among Gay, Bisexual and Other Men Who Have Sex with Men in Vancouver and Toronto. Sex Transm Dis. 2020; 47(4): 224–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spinelli MA, Scott HM, Vittinghoff E, Liu AY, Coleman K, Buchbinder SP. High Interest in Doxycycline for Sexually Transmitted Infection Postexposure Prophylaxis in a Multicity Survey of Men Who Have Sex with Men Using a Social Networking Application. Sex Transm Dis. 2019; 46(4): e32–e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stamm L V Global challenge of antibiotic-resistant Treponema pallidum. Antimicrob Agents Ch. 2010; 54(2): 583–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.O’Neill CE, Seth-Smith HMB, Van Der Pol B, et al. Chlamydia trachomatis clinical isolates identified as tetracycline resistant do not exhibit resistance in vitro: Whole-genome sequencing reveals a mutation in porB but no evidence for tetracycline resistance genes. Microbiol (United Kingdom). 2013; 159(4): 748–756. [DOI] [PubMed] [Google Scholar]
- 22.Fox KK, Knapp JS, Holmes KK, et al. Antimicrobial resistance in Neisseria gonorrhoeae in the United States, 1988–1994: The emergence of decreased susceptibility to the fluoroquinolones. J Infect Dis. 1997; 175(6): 1396–1403. [DOI] [PubMed] [Google Scholar]
- 23.Evaluation of Doxycycline Post-exposure Prophylaxis to Reduce Sexually Transmitted Infections in PrEP Users and HIV-infected Men Who Have Sex With Men (U.S. National Library of Medicine - ClinicalTrials.gov Website). Available at: http://clinicaltrials.gov/ct2/show/NCT03980223. Accessed November 1, 2020.
- 24.Impact of the Daily Doxycycline Pre-exposure Prophylaxis (PrEP) on the Incidence of Syphilis, Gonorrhoea and Chlamydia (Syphilaxis). (U.S. National Library of Medicine - ClinicalTrials.gov Website). Available at: https://clinicaltrials.gov/ct2/show/NCT03709459. Accessed November 1, 2020. [Google Scholar]
- 25.Center for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2015. MMWR Recomm Rep 2015. 2015; 64(3). [PMC free article] [PubMed] [Google Scholar]
- 26.Dombrowski J, Whitney H, Golden M, et al. Doxycycline prophylaxis use among cisgender men and transgender persons who have sex with men in Seattle. Presented at: 2020 STD Prevention Conference; 2020. [Google Scholar]
- 27.Joseph S, Lewis F, Jensen S, et al. Initiation of doxycycline post-exposure prophylaxis in patients attending an HIV PrEP clinic – Philadelphia, 2019. Presented at: 2020 STD Prevention Conference; 2020. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.