Abstract
In 2021, many countries have begun distribution of COVID-19 vaccines but are hampered by significant levels of vaccine hesitancy or apathy. Experts recommend that standard health communication campaigns be expanded to include a more holistic approach of behaviourally oriented strategies. We constructed a large-scale Delphi panel of marketing and behavioural science university faculty to assess 12 previously reported US vaccination promotion strategies, asking respondents to assess applicability of the strategy in their country, how efficacy might compare to the USA and recommendations for local adaptations necessary to successful implementation. Separately, we sought to determine whether strategies based on cognitive mechanisms (eg, ‘nudges’) are more readily generalisable than strategies based on social identity. Ninety-two marketing and behavioural science faculty from universities worldwide participated. Globally, all 12 behavioural strategies were validated; a majority of respondents reported that they would or could work well in their country. While all strategies were strongly validated at a global level, specific need for regional adaptation was identified. Also, open-ended responses suggested the addition of three emergent strategies to a global effort. Finally, we see that strategies based on some types of cognitive mechanisms are more readily generalisable across regions than mechanisms based on social identity, however, this is not always true of ‘nudge’ strategies. All 12 strategies are robust to global use and consensus exists on adaptation for optimal efficacy in different regions; specific strategy recommendations are posited. Use of these strategies can accelerate individual country efforts to achieve desired vaccination rates to protect global public health.
Keywords: COVID-19, health education and promotion, prevention strategies, vaccines
Summary box.
Vaccine hesitancy continues to undermine the necessary vaccine uptake to herd immunity levels worldwide.
Twelve behaviourally oriented strategies, adapted from marketplace theories commonly used to spur innovation adoption, have been recommended to augment standard US vaccination promotion campaigns.
Because these strategies were developed for the USA and because they reflected different types of behavioural approaches (eg, social affiliation tactics, implicit ‘nudges’), it was not recommended that they be used for global vaccination promotion without validation.
We undertook to validate all 12 strategies for use in the 7 major world regions (as categorised by the World Bank) using a large-scale Delphi method with expert marketing and behavioural science faculty from each world region.
Experts independently assessed (1) whether the strategies could be applied in their region, (2) how efficacy would likely compare to the USA and (3) how strategies should be adapted for cultural context. Analysis yielded strong validation and a pattern of necessary adaptations.
Experts agree that use of these practices can confidently accelerate worldwide efforts to achieve desired vaccination rates.
All 12 behavioural strategies are recommended for use, but vary in the need for region-based adaptation to fit local contexts.
The use of behaviourally oriented persuasion techniques, that go beyond standard health communication practices, will also benefit future healthcare initiatives and campaigns.
The rapid development of multiple SARS-CoV-2 vaccines has been a staggering global achievement. Yet, while the scientific community focused on the clinical research, manufacture and distribution of vaccines, there was not a similar effort developing strategies to globally promote vaccine uptake. Unfortunately, merely sharing scientific data about vaccine efficacy and safety does not comprise a marketing strategy. To address this gap, we developed 12 promotion strategies—based on robust marketing and behavioural science theories—to augment standard US health communication practices.1 Because any single behavioural change approach is insufficient for reaching diverse communities and contexts, the strategies ranged across a behavioural spectrum, from small ‘nudges’ to large social identity motivations. When adapted and implemented, these strategies can constitute a multifaceted vaccine-promotion campaign.2 3
This research, and subsequent recommendations, focused on one country, the USA. As global firms know, to move successfully from one country to another, marketing strategies must carefully consider local cultures, contexts and constraints. All strategies may not be equally generalisable to new places. Thus, in this healthcare context, it is critical to validate and potentially adapt strategies for COVID-19 vaccination promotion campaigns from one global region to the next.
Fortunately, a wealth of worldwide expertise exists for consultation on the global validation and adaptation of these strategies—academic faculty who study consumer behaviour in universities around the world. To accelerate the translation of this vaccine promotion framework to seven world regions, we engaged in an unprecedented large-scale global validation effort using a diverse academic Delphi panel of consumer behaviour experts.
Expanding the toolbox for global COVID-19 vaccination campaigns
Given the urgency and size of the national COVID-19 vaccination initiative, 12 novel behavioural strategies were developed for use within, or in addition to, traditional US health communications (for descriptions of the 12 strategies, see table 1; for more detail about strategy methodologies and examples please see the original source.1 These strategies were developed using consumer behaviour and behavioural economics research, and were based, as identified by the academic literature, on either cognitive mechanisms or social mechanisms. Strategies with cognitive mechanisms rely primarily on underlying mental functions. Strategies with social mechanisms rely primarily on interpersonal effects.
Table 1.
Global validation of 12 behavioural strategies
| Behavioural strategy* | Definition | Phase | Mechanism type | Global validation, % |
Variance in global adaptation |
Efficacy versus US (sig <0.05) |
| Identity segments | Attitude towards vaccine is influenced by a person’s self-identity or membership in a group. Target messages towards different identities and use group leaders or celebrities. | 2 | Social mechanism: affiliation/affect | 83.3 | High | Similar |
| Common enemy | Unite highly polarised groups by framing vaccination as defeating a common enemy that both strongly dislike. | 3 | Social mechanism: affiliation/affect | 82.4 | High | Similar |
| Analogy | Explain processes (how the vaccine works) and risks (the odds of getting sick) with accurate analogies. | 1 | Cognitive mechanism: net benefits | 94.2 | Moderate | More |
| Observability | Make vaccinated persons a walking advertisement for vaccine popularity by making the # of vaccinated observable. | 2 | Social mechanism: affiliation/affect | 87.2 | Minimal | More |
| Leverage scarcity | Use the natural scarcity of the vaccine to frame it as highly precious. | 1 | Cognitive mechanism: implicit nudge | 83.5 | High | Similar |
| Negative attributions | Monitor and directly address incorrect negative attributions made about the vaccine or its delivery. | 1 | Cognitive mechanism: net benefits | 92.9 | Minimal | More |
| Anticipated regret | Ask people to consider what would happen and how they would feel if they or someone they loved were to get sick. | 3 | Social mechanism: affiliation/affect | 84.9 | High | More |
| Piecemeal risk info | Be aware that people see greater risk when information trickles out over time and thus changing info about vaccine roll-out may logically increase anxiety. | 3 | Cognitive mechanism: net benefits | 84.7 | Minimal | Similar |
| Compromise effect | When uncertain, people feel more confident about compromise options, so frame their vaccination ‘choice’ as the middle of three options. | 2 | Cognitive mechanism: implicit nudge | 74.7 | High | Similar |
| FOMO incentives | Trigger loss aversion by mentioning incentives that people may miss out on by not vaccinating now. | 2 | Social mechanism: affiliation/affect | 85.2 | Moderate | Similar |
| Uniqueness neglect | Look for hesitant people who see the vaccine as a ‘one-size-fits-all’ solution but see themselves as ‘not average’ and offer small special accommodations to them. | 3 | Cognitive mechanism: implicit nudge | 73.8 | High | Less |
| Base-rate fallacy | People are more persuaded by stories than statistics, so counter a hesitant person’s fear of unlikely bad outcomes with positive stories first and statistics second (if at all). | 1 | Cognitive mechanism: net benefits | 96.5 | Minimal | More |
*Behavioural strategies as described previously. (1) Promotion phase suggests when the strategy may be most effective. Phase 1: strategies that build understanding of a vaccine’s net benefits and are considered for early communication. Phase 2: strategies that prompt follow-through are considered for communication around vaccination campaigns. Phase 3: those that address populations that remain resistant. Mechanism is categorisation based on the underlying psychological mechanism of the strategy. Global validation is the proportion of the panel that responded yes or maybe to question of ‘whether the strategy would be helpful in your region.’ Variance in global adaptation reflects the diversity observed in recommendations of the Delphi Panel for local adaptation (as observed in open-ended responses). Efficacy compared with USA is rating (seven-point semantic differential scale item where 1=less, 7=more than USA); one sample t-test compared with midpoint).
†
FOMO, fear of missing out.
Methodology
For the Delphi panel, we recruited global university faculty, with doctoral degrees in marketing or behavioural science, to participate via emailed surveys (open 16 February 2021–11 March 2021). Delphi methods harness the power of expert groups to assess unknown entities like innovations or trends.4 5 Descriptions of this Delphi panel, from seven global regions (Latin America and the Caribbean, Middle-East and North Africa, Europe and Central Asia, sub-Saharan Africa, South Asia, East Asia and Pacific, and North America), are shown in figure 1. While heterogeneity exists within global regions, and even within countries or communities, this analysis of seven regions provides a practical and foundational effort to outline global strategy validation and adaptation. We used snow-balling recruitment, sending an initial recruitment email to 250 professors who serve on the Editorial Review Board for a premier international consumer research journal. This email asked recipients to respond to an anonymous survey (hosted on the Qualtrics online survey platform) and to forward the request to marketing professors they knew at universities in the seven world regions named. We received 189 responses from the initial email invitation of 250 professors (75.6%). Of the 189 responses, 103 completed the extensive 84-question survey (54.5%). The survey asked respondents to self-identify by academic degree (ie, Ph.D. vs other) and area (marketing/behavioural science or other). Marketing is an interdisciplinary academic field with roots in psychology and sociology and, thus, universities describe the field with different designations; ‘marketing’ is by far the most common term but some use ‘behavioural economics’ or ‘behavioural science.’ We filtered out respondents who were not a professor of marketing or behavioural science or not fully credentialed faculty (eg, doctoral students or marketing practitioners); this resulted in a final panel of 92 faculty. Typical Delphi panels consist of 10–20 experts; the panel here represents an extraordinary global effort. We implemented only one round of assessments from the full panel (given high levels of regional consensus), and sent a second round of inquiry into specific exemplars to a subset of the panel. The questions submitted to the panel can be seen in box 1.
Figure 1.

Description of Delphi panel (n=92).
Box 1. Questions from Online Survey of Delphi panel.
INSTRUCTIONS: For the next section, please consider the 12 strategies for Covid-19 vaccination promotion that were published last month in the New England Journal of Medicine. Each strategy is listed and described. For each one, please indicate your opinion about how this strategy would work in the country/region you indicated previously. (The strategies will be presented in random order, but you will see all 12.)
(DESCRIPTION OF STRATEGY INSERTED for each block; 12 blocks randomised)
Q1. Would the practice of (strategy inserted) be helpful in your region?
Yes (score 1)
Maybe (score 2)
No (score 3)
Q2. How would the practice of (strategy inserted) work in your region compared to the USA?
Work much worse than in the USA (score 1).
Work worse than in the USA (score 2).
Work a little worse than in the USA (score 3).
Work the same as in the USA (score 4).
Work a little better than in the USA (score 5).
Work better than in the USA (score 6).
Work much better than in the USA (score 7).
Q3. Can you suggest ways to modify or adapt this strategy to work in your region? (open- ended response)
Q4. Is there a reason why this strategy should be used with caution in your region or might backfire? (open-ended response)
Q5. Have you seen an example of this strategy in action in this region/country that you felt worked well? (open-ended response)
Validation results of behavioural strategies by global region
The results of the Delphi panel are described below; added details can be seen in the accompanying tables as noted. The global validation results (table 1) show that all strategies are validated (in this paper, we consider a strategy to be validated when a majority of experts agreed the strategy would or could be effective in their country), but that the need for regional adaptation varied greatly. Experts also predicted variance in efficacy, due in part to potential cultural differences; for example, increased efficacy of observability and decreased efficacy of uniqueness neglect between regions could be a function of differences in characteristics anthropologists define as individualism/collectivism.6
To understand why some strategies are more easily applicable to cross-national use, we categorised the original 12 into three categories based on mechanism: cognitive mechanisms to increase perceived net benefits, cognitive mechanisms to leverage implicit ‘nudges,’ and social mechanisms to increased perceived affiliation or affect (see table 2). Taken together, the data suggest that mechanism matters. Strategies that use cognitive mechanisms to promote net benefits are highly transferable and need only superficial adaptation. Strategies that use social mechanisms to promote affiliation and emotional appeal are highly transferable, but need careful adaptation to local culture. Finally, and importantly, strategies that use cognitive mechanism to prompt implicit nudges are not as easily transferable and also need significant adaptation regionally; thus, health organisations must be careful with how ‘nudges’ are used across global contexts.
Table 2.
Regional adaptations of behavioural vaccination promotion
| Validation of strategy | Latin America and Caribbean (n=20) | Middle East and North Africa (n=5) | Europe and Central Asia (n=20) | Sub-Saharan Africa (n=7) | South Asia (n=8) | East Asia and Pacific (n=23) | North America (n=9) | |||||||
| Identity segments | 68.5% | Recommended segmentation by: the intersection of religious/spiritual belief and attitudes towards modern science. Segmenting by political party is highly variable; effective in some countries and to be avoided in others. | 100% | Recommended segmentation by: generational identity (age) and urban/rural lifestyle. Political identity should be avoided and religious identity should only be used with great care. | 94.7% | Recommended segmentation by: positive identities like sports, affiliations, and national pride. Political identity is not effective due to greater trust in government or distaste for disunity. Can segment based on risk-aversion. Religious segmentation may work in some countries. | 86.5% | Recommended segmentation by: followers of aspirational leaders or celebrities (entertainment/sports). Segmenting based on politics is largely ineffective because of low trust, consistency, and commitment across all parties. | 85.8% | Recommended segmentation by: the intersection of affluence and health/strength. Segmenting may also be based on the followers of aspirational leaders or celebrities(entertainment/sports). Do not segment on ‘anti-vax’ as the need for vaccines is largely accepted. | 76.2% | Recommended segmentation by: reasons for lack of speed in vaccination rather than ‘choice’ of vaccination; that is, why would people see less personal urgency for their own vaccination. Effective segmentation groups may include work/profession or education level. | 100% | Recommended segmentation by: the intersection of political or religious identity and attitudes about science/pharmaceuticals. Other segmentation identity may include personal strength/health or risk-aversion. |
| Common enemy | 84.2% | Common enemy: Economic distress. Avoid use of warfare language. | 100% | Reframe as common goal: Health/Welfare of Islamic Nation or citizens | 90% | Reframe as common goal: High variance across countries. Includes health, economic recovery, freedom of movement, cultural connections (cafes, sports) | 85.5% | Common enemy: Health apathy or fatalism. May also use common goal of provincial pride. | 85.7% | Common enemy: Health apathy or fatalism. If COVID-19 is the enemy, link to mythology antagonists. | 68.2% | Common enemy: COVID-19. Use positive language and focus on unity. | 83.4% | Common enemy: COVID-19 and economic distress. Can use warfare language, national pride and anthropomorphize the virus. |
| Analogy | 94.7% | High use. Especially analogies that are pictoral. | 100% | High use. Especially analogies with emotion or tied to local proverbs. | 100% | High-moderate use. Target analogies by age group to avoid perception of “dumbing down” information | 100% | High use. Especially analogies with emotion or tied to local proverbs. | 100% | High use. Especially analogies tied to positive emotion and local mythology or to past successes with disease. | 90.9% | High use. Especially with analogies tied to local mythology or to past successes with disease. | 71.4% | High use. Target analogies by region or identity segment. |
| Observability | 94.8% | Mix of community and individual. Individual can be digital (social media) or wearables (stickers). | 80% | Community only. | 70% | Mix of community and individual. Individual should be primarily digital and beware virtue-signalling. | 85.7% | Community only. | 100% | Mix of community and individual. Individual should be primarily digital. | 95.5% | Community only. | 85.7% | Individual only. Individual can be digital or wearables. |
| Leverage scarcity | 83.4% | Scarcity=precious/taking care. Beware inflation/poverty triggers. | 80% | Scarcity=precious/taking care. Beware status triggers. | 78.9% | Scarcity=precious/taking care. Beware inequity triggers. | 100% | Scarcity=precious/taking care. Beware inequity and poverty triggers. | 85.7% | Scarcity=precious/taking care. Beware inequity and poverty triggers. | 81.8% | Scarcity=precious/taking care. Beware status triggers. | 85.7% | Scarcity=precious/taking care. Beware inequity triggers. |
| Address Negative Attributions | 94.7% | Source credibility/trust: Use partnerships, build trust. Counter misinformation: Social media campaigning | 100% | Source credibility/trust: Use governments, regional medical agencies. Counter misinformation: Social media campaigning | 100% | Source credibility/trust: Use government and global agencies. Counter misinformation: Social media regulation; Transparency via fully shared data | 100% | Source credibility/trust: Use partnerships, build trust. Counter misinformation: Social media campaigning | 85.8% | Source credibility/trust: Use government, national and global agencies. Counter misinformation: Social media campaigning; Transparency via fully shared data. | 81.8% | Source credibility/trust: Use governments, national medical agencies. Counter misinformation: Social media campaigning; Transparency via fully shared data | 100% | Source credibility/trust: Use partnerships, government, and global agencies. Counter misinformation: Social media regulation; Transparency via fully shared data |
| Anticipated regret | 79% | Regret about others, not self; Use cautiously to avoid guilt | 75% | Regret about others, not self; Use cautiously to avoid fear and guilt | 85% | Regret about others and self; Use cautiously to avoid reactance | 85.7% | Regret about others, not self; Use cautiously to avoid fear and guilt | 85.7% | Regret about others, not self; Use cautiously to avoid fear and reactance | 95.5% | Regret about others, not self; Use cautiously to avoid fear and guilt | 71.4% | Regret about others and self; Use cautiously to avoid reactance |
| Piecemeal info | 73.7% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ | 75% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ | 89.4% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ | 85.8% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ | 100% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ | 81.8% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ | 84.7% | Frame changes in advice from trusted sources as continual improvement not ‘corrections’ |
| Compromise effect | 57.9% | Choice of vaccination is common. However, use with extreme caution as compromise options can be seen as weak or ambivalent | 75% | Choice of vaccination is mixed. Use compromise options in peripheral decisions (eg, timing) | 75% | Choice of vaccination is common. | 85.7% | Choice of vaccination is common. | 85.7% | Choice of vaccination is common. | 82.6% | Choice of vaccination is less common. Use compromise options in peripheral decisions (eg, timing) | 85.8% | Choice of vaccination is common. |
| FOMO motivations | 90% | Incentives effective; offer utilitarian family-oriented goods (school supplies, bus tickets, food coupons); don't trigger fear of loss | 100% | Incentives effective; offer utilitarian family-oriented goods (school supplies, bus tickets, food coupons); don't trigger fear of loss | 75% | Incentives less effective; offer safety/travel options (event attendance; ‘fast lane’ for flight check-in; skip temperature checks); don't trigger ‘bought behaviour’ | 71.5 | Incentives effective; offer utilitarian family-oriented goods (school supplies, transportation compensation, food coupons); don't trigger fear of loss | 85.7% | Incentives effective; offer utilitarian family-oriented goods (school supplies, transportation compensation, food coupons); don't trigger fear of loss | 90.9% | Incentives less effective; offer safety/travel options (event attendance; ‘fast lane’ for flight check-in; skip temperature checks); don't trigger ‘bought behaviour’ | 87.5% | Incentives effective; offer monetary incentives and safety/travel options (event attendance; ‘fast lane’ for flight check-in; skip temperature checks) |
| Uniqueness neglect | 77.8% | Less common: Special information or accomodation may be by affluence or religion | 50% | Less common: Special information or accomodation may be by affluence or religion | 84.2% | More common: Special information or accomodation may be by medical condition or religion | 85.7% | Less common: Special information or accomodation unlikely | 71.4% | Less common: Special information or accomodation may be by religion | 63.6% | Less common: Special information or accomodation may be by medical condition | 71.4% | More common: Special information or accomodation may be by medical condition or religion |
| Base-rate fallacy | 95% | High use. Use stories specific to region, dialect. Use only positive ‘happy ending’ stories. | 100% | High use. Use stories specific to region, dialect. Use mainly positive ‘happy ending’ stories. Always follow stories with stats. | 100% | High use. Use stories specific to region, dialect. Use both positive and negative stories. Always follow stories with stats. | 100% | High use. Use stories specific to region, dialect. Use only positive ‘happy ending’ stories. | 100% | High use. Use stories specific to region, dialect. Use mainly positive ‘happy ending’ stories. Always follow stories with stats. | 90.9% | High use. Use stories specific to region, dialect. Use only positive ‘happy ending’ stories. | 100% | High use. Use stories specific to region, dialect. Use both positive and negative stories. Always follow stories with stats. |
Proportions reflect validation by region (the proportion of each region’s panel members who responded Yes or Maybe to question of ‘whether the strategy would be helpful in your region’). Mechanism is categorisation based on the underlying psychological mechanism of the strategy, and color-coding is based on mechanism. Recommended adaptations are shown by region and reflect consensus opinions in panel members’ open-ended responses.
FOMO, fear of missing out.
Strategy adaptations by global region
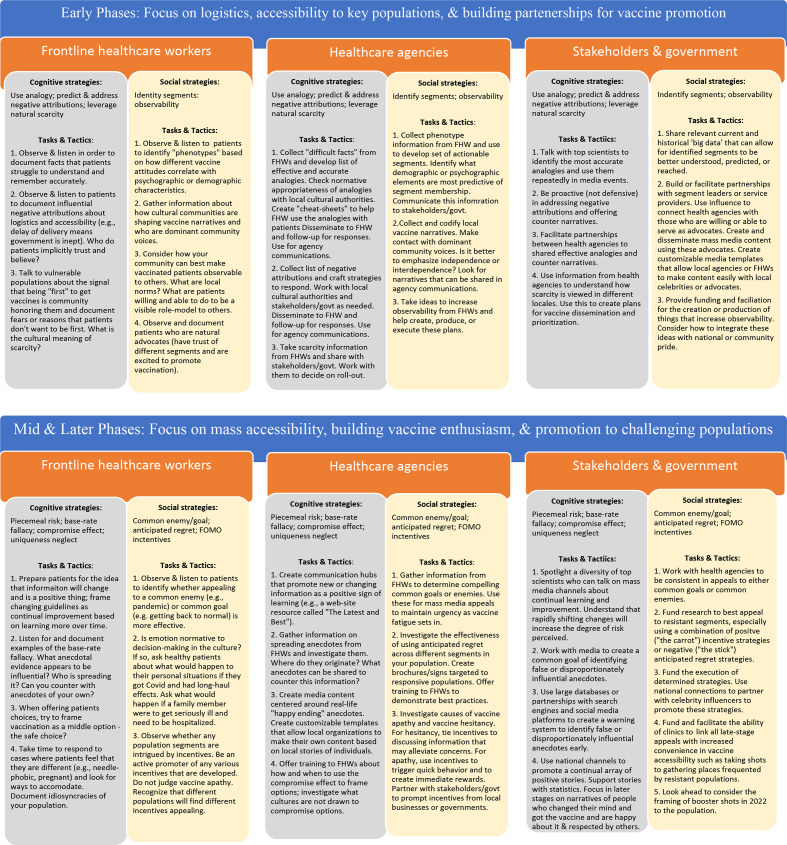
The open-ended responses provided by the Delphi panel described many concrete suggestions and examples for adapted use of the 12 strategies globally (validation percentages are reported by global region and summarised in table 2; examples of how the panellists agree these might be applied for selected countries—especially for high variance strategies—are shown for illustrative purposes (table 3). Finally, we outline a phased framework by healthcare role to deploy applicable strategies and combinations of strategies into local environments (figure 2).
Table 3.
Adaptation exemplars for high variance strategies
| Strategy | ||
| Identity segmentation |
Germany | Target sport-minded young adults with team affiliation (eg, ‘Top Shots’ campaigns for football fans; ‘Bundesliga has the highest average attendance on any football league in the world; we get our shot and we get back to it.’) |
| Brazil | Target indigenous tribes with in-group identity (eg, ‘Outsiders like miners are bringing COVID-19; this medicine will keep your village safe from other peoples’ diseases; ‘You must act to protect your village by getting these shots; the miners don’t care if you get sick.’) | |
| China | Target taxi drivers and transportation workers with professional pride (eg, taxi campaign fronted by Han Han, famous racecar driver; ‘You keep our city moving. Protect yourself and our city by moving fast to get your vaccine.’) | |
| Common enemy |
Jamaica | Economic distress as common enemy (eg, campaign ‘Poverty is our Enemy. Vaccination=Visitors’ by emphasising cruise company selections of ports of call will depend on island vaccination rates.) |
| Saudi Arabia | Health of religious community as common goal (eg, communicate ‘Our duty is to the health of the Islamic Nation; we must act in unity to stop COVID-19 now.’) | |
| Leverage scarcity |
Chile | Frame vaccine as precious and describe scarcity globally (ie, Chile is doing better than other countries at getting vaccines, so don’t waste them.) |
| Switzerland | Frame vaccine as precious and emphasise natural scarcity (ie, slow ramping up of production and distribution is to be expected) to avoid blaming of government for inability to procure vaccines. | |
| Australia | Frame vaccine as precious and emphasise limited opportunities to gain mobility or go to certain places (ie, travel freely or with ease). | |
| Mali, Niger | Frame vaccine as precious and offer first to traditional leaders (eg, chiefs, kings, and emirs) or religious leaders. | |
| Uganda | Frame vaccine as precious and emphasise it is above corruption and therefore will be distributed equitably to all as it is available. | |
| Prompt anticipated regret |
Sweden | Use less emotional language and non-health situations (eg, ‘Take a little care now to avoid missing out on something special later’ with images of weddings, graduations, travel) |
| Nepal | Use emotional appeal to get shot to avoid bringing disease to the family, especially elders and schoolchildren. | |
| Compromise effect |
India | Do not use compromise effect by offering a range of choices of getting the vaccine but rather by emphasising how most other people who were unsure thought it safest to go ahead and get the vaccine when available (ie, the modal response). Frame non-vaccination as a very extreme choice. |
| Canada | Use compromise effect by approaching hesitant populations with choice of vaccinate now, sign up for next month, or don’t sign up now. | |
| Israel | Wait to use compromise effect until there are choices among available vaccines so that a middle option could be a one-dose shot or a (future) nasal spray. | |
| Uniqueness neglect |
Ecuador | Allow the wealthy to access vaccines through their doctors rather than mass clinics even if that means they must pay for the vaccine. |
| Greece | In online registration let people enter personal health notes they feel are important to be known (eg, pregnant, allergies, chronic conditions); entering them in will give reassurance that the vaccine is ok for them specifically. | |
| South Africa | Avoid public communication of uniqueness neglect sentiments as perceived consistency is critical to trust; special accommodations for health conditions should be handled privately. |
Suggestions provided by Delphi panel members for local adaptation during second round of expert input. The strategies in this table represent those with high levels of variance between global regions and thus require the most local adaptation for effective use.
Figure 2.
Coordinating a locally adapted COVID-19 communication strategy across different roles.
Segment by identity barriers (panel validation: 83.3%)
Our identity, especially as a member of a group, often impacts our health behaviours. Thus, this strategy works to target behavioural ‘segments’ (or subpopulations) by personal or group identity—both to address the hurdles faced by that group and to frame vaccine adoption as a congruent component of that identity. Panellists see this as widely applicable, adapting the characteristic by which populations are segmented. While North American panellists see North America as often, and perhaps effectively, segmented by political identity, panellists in other global regions view politics to be a risky characteristic to target. Identity is clearly multifaceted and other facets of identity may be more effective. Panellists recommended that the best facets for each region are: affiliative groups based on sports, entertainment and social activities (Europe and Central Asia; sub-Saharan Africa), urban versus rural residence and age groups (Middle East and North Africa), professions (East Asia and the Pacific), religion and attitudes toward modern medicine (Latin America), and the intersection of affluence and perceived health (South Asia).
Identify a common enemy (panel validation: 82.4%)
This strategy works to unite polarised groups by focusing on a third, more hated common enemy, such as battling the economic impact of the pandemic.7 Panellists saw this strategy as effective in most regions. However, there were important suggestions for local adaptations. While common enemies can be used to unite a highly polarised area, for more homogeneous or collective communities, it is beneficial to reframe this strategy as a common goal. If a common enemy is used in collective communities, the enemy should be clearly related to something outside of individual control. The virus can be anthropomorphised to create an embodied (though ultimately defeatable) enemy. Some areas, preferring a common goal approach, can create an anthropomorphised goal-oriented mascot such as Brazil’s readapted Zé Gotinha (Droplet Joe) mascot, originally created to promote polio vaccination campaigns in the 1980s and 1990s as a way to make events more attractive to children.8
Several panellists identified pandemic fatigue as an evocative common enemy. Panellists (sub-Saharan Africa, South Asia) described the danger of health apathy in general, or for COVID-19 specifically. Recent research demonstrates that communications aimed at vaccine hesitancy will not be effective for vaccine apathy.9 In such cases, because apathy can breed fatalism about health, (decreasing the likelihood of vaccination), it is important not to identity people as apathetic, but rather set a campaign around a common goal to fight the concept of apathy (‘pandemic fatigue’) and help all citizens take good care of themselves.
Use analogy (panel validation 94.2%)
Analogies harness understanding of a familiar concept to elucidate a complex new concept.10 The Delphi panel saw this as highly applicable and effective globally; it is one of the most highly rated strategies for worldwide use. Minimal adaptation is necessary; panellists recommend checking that analogies are relevant and sensitive to different cultures. Many regions benefit from the use of emotion-based analogies (eg, the vaccination protects you like a mother’s loving arms), based on local proverbs, or tied to local mythologies (Latin America, sub-Saharan Africa, Middle East and North Africa, South Asia and East Asia and the Pacific). The panel suggest caution, however, in that any populations highly involved in vaccine decisions may experience overly simplistic analogies as authorities unnecessarily ‘dumbing down’ information.
Increase observability (panel validation: 87.2%)
Innovation observability suggests that consumers’ ability to physically see others’ choices can increase an innovation’s rate of adoption.11 The Delphi panel reported this strategy as effective in most regions, but with an important adaptation to shift the framing from the individual focus to the community. Making vaccinated individuals observable may be non-normative in collective communities, may cause unwarranted attention where vaccination is viewed with suspicion, or where it might trigger perceptions of status/corruption.
Here, the preference would be to make community numbers more visible. For example, a billboard with an electronic counter can both thank community members who have been vaccinated while updating the number of vaccinated daily. This increases communal ‘perceived’ popularity or a sense of momentum.12 Two simple ways to do this in communications are to highlight turnout for mass vaccination events as successes, and to use plural amplifications (eg, ‘people say…’).
Leverage natural scarcity (panel validation: 83.5%)
In consumer markets, scarcity often signals exclusivity and prompts greater interest or desirability.13 Again, this strategy was seen by the panel to be effective in most regions. Suggested adaptations are to focus communications about scarcity on the precious nature of the vaccine and the care taken of its handling and distribution. Importantly, scarcity can also trigger negative thoughts, particularly where communities have memory of other times of scarcity. For example, triggers to be avoided are inflation/poverty (Latin America, sub-Saharan Africa, South Asia), status (Middle East and North Africa, East Asia and Pacific) and inequity (Europe and Central Asia, sub-Saharan Africa, South Asia, North America). This strategy can prompt different patterns of vaccine distribution. For example, in Mali, it may be best to offer scarce vaccines first to the highest status members of a community because associating vaccinations with power emphasises their value. In Uganda, it may be best to offer scarce vaccines equitably to citizens and immigrants alike, where associating the shots with strict fairness emphasises their value.
Predict and address negative attributions (panel validation: 92.9%)
‘Attribution theory,’ from social psychology, describes how people confronted with something unexpected or troublesome develop explanations for it.14 This strategy recommends proactively finding and countering false negative attributions that people make about the vaccine. Panellists see it as highly applicable and effective globally. Negative attributions are so widespread that collective action and local adaptation were suggested by panellists.
The first step in adaptation of this strategy is determining the channel of misinformation most damaging in the community. The Delphi panel consistently named social media as dangerous due to its speed. Thus, at national levels, health leaders must determine how to monitor social media for misinformation and develop means to stop its spread. In some regions, social media regulation is seen as a critical tool (Europe and Central Asia, North America). In other regions, social media counter-campaigning was seen as more practical and effective. Other suggestions include partnering with social media influencers to both report misinformation they receive and to encourage them to post true information. To determine if a rumour is worth countering, Online scraping tools, like Google Trends’ Interest Score, can determine if a rumour is growing or declining in interest.
Panellists noted that the foundational challenge in implementing this strategy is the need to build trust. Widespread lack of trust in institutions and information is sadly ubiquitous, as was experienced in East Africa with Ebola.15 Trust is a prerequisite for any strategy to be effective, but is clearly critical in addressing misinformation. One common suggestion is to find, educate, empower and incentivise trusted local community-influencers since trust in health agents can differ regionally; this mirrors excellent existing work on building trust through a community-oriented approach (eg, https://www.weforum.org/agenda/2019/08/important-tool-in-healthcare-is-trust-vaccines-africa/). Additionally, trust can be established by: (1) noting common ground, (2) providing credentials or authority, (3) affiliative mimicry and (4) consistency.12
Prompt anticipated regret (panel validation: 84.9%)
Imagining the practical and emotional consequences of a bad thing that may happen (anticipated regret) prompts people to take action to prevent that thing, even if it is very rare. Emotions, such as regret, are such powerful motivators of decisions that they can motivate us even before they are experienced.16 However, panellists expressed less support for this strategy, recommending it only be used where the vaccine is widely available or when the patient can get vaccinated at that moment so that guilt and fear may be avoided. Also, they note that in more communal regions, focusing on the possible illness of a loved one (not oneself) will be more effective. Finally, some subpopulations may feel that such a question is too emotionally manipulative (Europe and Central Asia) and, in such instances, this strategy is not recommended.
Beware the danger of piecemeal risk information (panel validation: 84.7%)
This strategy notes that the ‘trickling out’ or piecemeal delivery of vaccine-related information may increase the perceived risk of taking the vaccine. This is not something that can be changed, but is a danger that should be understood by everyone involved in vaccine communication efforts. For patients, changing risk information is frequently perceived as increasing the frequency of side effects.17 The massive regulatory response across Europe to several reports of rare thrombotic side effects with the Astra-Zeneca vaccine is an example of this phenomena.18
Here, health advocates can emphasise how the new information is a positive sign and indicates that scientists/doctors are not just resting on their laurels after developing the vaccine. The Delphi panel largely acknowledged that the effect of piecemeal risk information can impact most regions, but saw different potential to address this issue, especially when clinical data are coming from outside the region. Overall, this was seen as the least easily applicable strategy of the 12.
Promote compromise options (panel validation: 74.7%)
In the US consumer marketplace, three choices are often offered to consumers (eg, small, medium and large drink sizes, ‘gold, silver or bronze’ level services); when consumers are uncertain, choosing the middle option feels most reasonable or logical. This strategy was largely validated by the panel, but there was additional concern about local adaptation of this strategy. For many regions, the ‘illusion’ of choice does not exist; people may be required to be vaccinated. Similarly, even if they can choose, the idea of having an array of options may feel false or suspicious in communities where this is not often the case. Finally, in some cultures, choosing a middle option may be attractive because it is seen as polite, but in others it can be a very negative signal of ambivalence or weakness. While this strategy is often extremely effective in the behavioural sciences literature, it is more challenging to apply globally and should only to be used in limited situations for COVID-19 communication according to the panel.
Create fear of missing out motivations (panel validation: 85.2%)
Fear of missing out (FOMO) refers to the fear people have of missing out on something others are doing. In this strategy, vaccination is linked to some other positive attribute such as a day-off from work, a direct payment or gift, or some other reward that will be ‘missed’ if the person does not get vaccinated. The panellists also agree the FOMO concept can explain the efficacy of vaccination conferring preferential access, such as vaccine-passports for travel or special benefits for the vaccinated in workplaces or schools. The Delphi panel saw strong applicability of this strategy globally, but did caution that in areas with rampant economic, health or security crises, the ‘fear’ should be taken out of FOMO so that a positive tone is employed. The panel further expressed that it is critical that promises be fulfilled if this strategy is implemented.
Combat uniqueness neglect (panel validation: 73.8%)
Uniqueness neglect is an individual patient’s dislike of being treated as the average case or with a ‘one-size-fits-all’ treatment recommendation. To counter uniqueness neglect, healthcare advocates can provide special accommodations for some vaccines (eg, the vaccine has been blessed or is certified to be halal, or to have had a religiously permissible technology development pathway),19 or can provide special accommodations to some patients (eg, provide longer postshot observation times for patients with allergies). While the overall strategy was validated by the panel, it felt to be not as locally applicable as the other strategies. Some regions may be more attracted by the sameness of the treatment and be suspicious of inconsistencies (South Asia, sub-Saharan Africa).
Neutralise the case versus base-rate heuristic (panel validation: 96.5%)
Healthcare often emphasises communication using facts and statistics, and yet robust data show that people often underweight base-rate statistics and overweight anecdotal cases—stories—in judging probability, a decision heuristic known as the base-rate fallacy or case versus base-rate effect.20 To neutralise this perception bias, healthcare advocates should use more stories in both their educational and persuasive communications. This approach can be especially powerful in countering negative stories which are shared on social media.
The Delphi panel strongly validated this strategy and emphasised its efficacy. They reported that across cultures, people communicate using stories which are memorable, emotionally evocative and compelling. Some respondents noted the importance of following up stories with statistics, especially in regions where people may be more numerate. Another overarching recommendation was that healthcare workers should learn to use narrative stories before reporting scientific findings. Finally, in all regions, many positive vaccine stories should be shared in order to overcome the fewer but more attention-grabbing negative vaccine side effect stories.
Additional emergent strategies available for global use
This research also uncovered several strategies suggested by the Delphi panel that had not been previously identified for US use; some may be better suited to different global regions.
Behaviour coupling
One emergent strategy is the need to use ‘coupling’ strategies that encourage people to achieve multiple prohealth behaviours. Because of global attention and financial support for COVID-19 efforts, existing efforts to provide vaccinations for measles, malaria and polio have been overshadowed. Other non-COVID health efforts, which have a disproportionate benefit for children, may be compromised or curtailed. One solution is to couple or link together multiple health behaviours (COVID-19 vaccination plus other treatments/protections, especially those that occur regularly like annual check-ups, influenza vaccines or cancer screenings), thereby increasing the likelihood of achieving both rather than by raising the likelihood of one at the expense of the other. It is important to note that more ‘all-encompassing’ messaging around COVID-19 and other health threats should only be done in areas where it is necessary. Panellists noted it is challenging but important to coordinate across multiple health agencies and/or multiple vertical donors in implementing a strategy where multiple well-being behaviours (both vaccinations and other kinds of unmet needs) are addressed in one effort.15
Focus on recent ‘wins’
Another emergent strategy is to focus on past wins, even small ones. Around the world, individual countries or regions emerged in 2020 as leaders in controlling COVID-19 outbreaks. For example, Uruguay was noted for their rapid, scientifically grounded response to COVID-19.21 Similarly, Chile has experienced great momentum around vaccination from successful political negotiations to buy large supplies of vaccine from Sinovac, Pfizer and AstraZeneca.22 Even when ‘success’ is relative to other more catastrophically hit areas, a basis of pride can prompt new efforts in an effort to avoid losing that pride. This strategy is powerful because it is positive and encouraging, but also subtly prompts loss aversion. Loss aversion describes the asymmetric attention to and motivation for avoiding losses compared with achieving gains; where countries already have a point of pride in their COVID-19 response, it will be especially motivating to make sure that this pride is not lost.
Vaccine as ritual artifact
Ritual artifacts are products that are symbolic or important to cultural rituals, such as traditional wedding garments. When ritual traditions are important to group identity, vaccination offers a unique opportunity to build from what is most cherished in that tradition. Thus, vaccination can be a chance to reflect those values at a highly symbolic moment in time. This can be done by timing (eg, the Navaho Nation decided to first vaccinate their members who can fluently speak Navaho—the famed ‘Code Talkers’ —irrespective of age), or by ceremony (eg, first vaccinating leaders in ceremonial dress at a community event).23 As is true with many ritualised behaviours, the meaning stems from or is greatly enhanced by the symbolic narratives promoted by community leaders such as religious elders or matriarchs/patriarchs; the ritual meaning of vaccines must evolve naturally but can be shared to inspire other communities.
Putting it into practice
The global healthcare community is facing the challenge of developing diverse communication strategies for COVID-19 vaccination efforts across many populations and cultures.24–26 By providing a validated global framework for communication efforts, we can better develop promotional campaigns that ‘travel’ across regions, and know which efforts require local adaptations before being implemented. Importantly, strategies which are based on explicit cognitive mechanisms (those that aid learning or the perception of net benefits) are judged inherently more generalisable, while strategies which rely on cognitive ‘nudges’ or underlying social mechanisms require more careful adaptation.
The tables contain additional material that can be disseminated to communication stakeholders; table 1 defines the strategies and their characteristics; table 2 describes the necessary adaptations by global region; Table highlights strategies with high levels of variance and offers examples of how this changes the strategy execution. Finally, in figure 2, we organise the strategies best suited to different stakeholder roles and necessary to construct a multifaceted vaccination promotion campaign.
It is important to note that while these COVID-19 strategies originate from a set of behavioural theories originally developed for US use, the marketing literature they are based on is international, though skewed towards North American and European sources. In light of a growing desire to remove the consequences of colonialisation from public health research, we note it would have been equally appropriate to first develop theories from the extant marketing literature for any region and to subsequently adapt them for US use. Additionally, while our Delphi panel included experts from all the regions we studied, we were able to recruit fewer experts from some regions. Finally, even at a regional level, it is important to note that some recommendations may still be overgeneralised for particularly heterogeneous populations. Unfortunately, the examples described here cannot speak to every country or community in detail and require local expertise to aid in adaptation.
Finally, it is critical to note that successful campaigns will use a combination of many strategies in the effort to reach the heterogeneity of vaccine attitudes even within the same community, such as those who are vaccine hesitant versus those that are vaccine apathetic. Ultimately, whether carefully coordinated or more organically evolved, the 12 globally validated strategies here can accelerate local country efforts to confidently develop vaccine promotion at a time when both speed and care are critical.
Acknowledgments
Dr Vicki Morwitz (Columbia University) and Dr Angela Lee (Northwestern University); Delphi panel members participation was anonymous; however, panelists could voluntarily share their names in order to be recognised in this global effort against the Covid-19 pandemic. Our gratitude goes to: Professor Carolyn Yoon, University of Michigan, USA; Professor Eric Arnould, Aalto University, Finland; Professor Sharon Ng, Nanyang Technological University, Singapore; Professor Eduardo B. Andrade, FGV-EBAPE, Rio de Janeiro, Brazil; Professor Bernardo Figueiredo, RMIT University – Australia; Professor Lucia Barros, FGV-EAESP, Brazil; Professor Andrés Barrios, Universidad de Los Andes; Professor Prakash Satyavageeswaran, Indian Institute of Management Udaipur, India; Professor Kathleen Adams, RMIT University, Australia; Professor Anthony Tibaingana, Makerere University, Uganda; Professor Stav Rosenzweig, Ben-Gurion University, Israel; Professor Jayant Nasa, Indian Institute of Management Udaipur, India; Professor Cathy Ikiror Mbidde, Makerere University, Uganda; Professor Enav Friedmann, Ben Gurion University, Israel; Professor Vicki Morwitz, Columbia University, USA; Professor Liyin Jin, Fudan University, China; Professor Yaxuan Ran, Zhongnan University of Economics and Law, China; Professor Soniya Billore, School of Business and Economics, Linnaeus University, Sweden; Professor Lucia Malär, University of Bern, Switzerland; Professor Gianluca Scheidegger, University of St.Gallen, Switzerland; Professor Sabrina Stöckli, University of Bern, Switzerland; Professor Steffen Jahn, University of Oregon, USA; Professor Giana Eckhardt, King's College London, UK; Professor Arobindu Dash, International University of Business Agriculture & Technology (IUBAT), Bangladesh; Professor Luk Warlop, BI Norwegian Business School, Oslo, Norway; Professor Marie-Agnès Parmentier, HEC Montréal, Canada; Professor Eric Cohen, State University of Campinas, Brazil; Professor Bernadette Kamleitner, WU Vienna University of Economics and Business, Austria; Professor Antonios Stamatogiannakis, IE University, Spain; Professor Daiane Scaraboto, The University of Melbourne, Australia; Professor Debbie Human-Van Eck, Stellenbosch University, South Africa; Professor Karin Usach-Franck Phd(c), Universidad Adolfo Ibañez, Chile; Professor Manuel Moyano, University of Cordoba, Spain; Professor Klaus Wertenbroch, INSEAD, Singapore; Professor Flavia Cardoso, Universidad Adolfo Ibáñez, Chile; Professor Alfredo Hoffmann, UPC Universidad Peruana de Ciencias Aplicadas, Perú; Professor Nidhi Agrawal, University of Washington, USA; Professor Gustavo Lembcke, Universidad Peruana de Ciencias, Lima; Professor Claire Tsai, University of Toronto, Canada; Professor Teniza da Silveira, Associate Professor at UFRGS, Brazil; Professor Marc Linzmajer, University of St. Gallen, Switzerland; Professor Caroline Graebin, University of São Paulo, Brazil; Professor Maria Fernanda Jaramillo, MBA, Universidad San Francisco de Quito USFQ, Ecuador; Professor Paola Valencia, MBA, Universidad San Francisco de Quito, Ecuador; Professor Heyla A Selim King Saud University, Saudi Arabia, Riyadh; Professor Georgios Abakoumkin, University of Thessaly, Greece; Professor Irene Consiglio and Sofia Kousi, Nova SBE, Portugal; Professor Pooja Haldea, Centre for Social and Behaviour Change, Ashoka University, India.
Footnotes
Handling editor: Seye Abimbola
Contributors: All authors provided substantial contributions to the conception of the work. SW provided the first draft of the manuscript, and KS and MAP provided critical input into revising the draft. All coauthors provided final approval of the manuscript and are accountable for the content.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: MAP is employed by the World Bank.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This project was found to exempt by the Institution Review Board at NC State University.
References
- 1.Wood S, Schulman K. Beyond politics — promoting Covid-19 vaccination in the United States. N Engl J Med Overseas Ed 2021;384:NEJMms2033790. 10.1056/NEJMms2033790 [DOI] [PubMed] [Google Scholar]
- 2.Wood S. A case for marketing in medicine: using consumer theory to understand patient choice and improve patient care. Health Management Policy and Innovation 2018;3. [Google Scholar]
- 3.Moorman C. Consumer health under the scope. J Consum Res 2002;29:10.1086/339928:152–8. 10.1086/339928 [DOI] [Google Scholar]
- 4.Mannes AE, Soll JB, Larrick RP. The wisdom of select crowds. J Pers Soc Psychol 2014;107:299 10.1037/a0036677 [DOI] [PubMed] [Google Scholar]
- 5.Duboff RS. The wisdom of (expert) crowds. 85. Harvard Business Review, 2007: 1–28. [Google Scholar]
- 6.Hofstede GH. Culture’s consequences, comparing values, behaviors, institutions, and organizations across nations. Thousand Oaks, CA: Sage Publications, 2003. [Google Scholar]
- 7.Bierwiaczonek K, Kunst JR, Pich O. Belief in COVID‐19 conspiracy theories reduces social distancing over time. Applied Psychology: Health and Well‐Being 2020;12:1270–85. [DOI] [PubMed] [Google Scholar]
- 8.Vaccination of Indigenous children and women starts in Brazil. Available: https://www.paho.org/english/DD/PIN/vw05_brasil.htm [Accessed 07 Jun 2021].
- 9.Wood S, Schulman K. When vaccine apathy, not hesitancy, drives vaccine disinterest. JAMA 2021;325:10.1001/jama.2021.7707:2435–6. 10.1001/jama.2021.7707 [DOI] [PubMed] [Google Scholar]
- 10.Goode MR, Dahl DW, Moreau CP. The effect of experiential analogies on consumer perceptions and attitudes. Journal of Marketing Research 2010;47:274–86. 10.1509/jmkr.47.2.274 [DOI] [Google Scholar]
- 11.Hayes KJ, Eljiz K, Dadich A, et al. Trialability, observability and risk reduction accelerating individual innovation adoption decisions. J Health Organ Manag 2015;29:271–94. 10.1108/JHOM-08-2013-0171 [DOI] [PubMed] [Google Scholar]
- 12.Cialdini RB. Influence: science and practice. 5th edn. Boston: Pearson Education, 2009. [Google Scholar]
- 13.Hamilton R, Thompson D, Bone S, et al. The effects of scarcity on consumer decision journeys. J Acad Mark Sci 2019;47:532–50. 10.1007/s11747-018-0604-7 [DOI] [Google Scholar]
- 14.Heider F. The psychology of interpersonal relations. New York: Wiley, 1958. [Google Scholar]
- 15.Skrip LA, Bedson J, Abramowitz S, et al. Unmet needs and behaviour during the Ebola response in Sierra Leone: a retrospective, mixed-methods analysis of community feedback from the social mobilization action Consortium. Lancet Planet Health 2020;4:e74–85. 10.1016/S2542-5196(20)30008-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sandberg T, Conner M. A mere measurement effect for anticipated regret: impacts on cervical screening attendance. Br J Soc Psychol 2009;48:221–36. 10.1348/014466608X347001 [DOI] [PubMed] [Google Scholar]
- 17.Wood S. The dangers of piecemeal risk: how do people respond when health risk information trickles out over time? working paper. North Carolina State University, 2020. [Google Scholar]
- 18.Jordans F. Major European nations suspend use of AstraZeneca vaccine. AP news, 2021. Available: https://apnews.com/article/germany-suspends-astrazeneca-vaccine-blood-clotting-0ab2c4fe13370c96c873e896387eb92f [Accessed 15 Mar 2021].
- 19.Wamsley L. Vatican OKS receiving COVID-19 vaccines, even if research involved fetal tissue. National public radio (US), 2020. Available: https://www.npr.org/sections/coronavirus-live-updates/2020/12/21/948806643/vatican-oks-receiving-COVID-19-vaccines-even-if-research-involved-fetal-tissue [Accessed 21 Dec 2021].
- 20.Lynch JG, Ofir C. Effects of cue consistency and value on base-rate utilization. J Pers Soc Psychol 1989;56:170–81. 10.1037/0022-3514.56.2.170 [DOI] [Google Scholar]
- 21.Taylor L. Uruguay is winning against covid-19. this is how. BMJ 2020;370:m3575. 10.1136/bmj.m3575 [DOI] [PubMed] [Google Scholar]
- 22.Oppenheimer A. There’s a good reason why Chile is winning COVID vaccine race —and Mexico and Venezuela are not. Miami Herald, 2021. Available: https://www.miamiherald.com/news/local/news-columns-blogs/andres-oppenheimer/article249160835.html [Accessed 12 Feb 2021].
- 23.Roberts L. The art of eradicating polio. Science 2013;342:28–35. 10.1126/science.342.6154.28 [DOI] [PubMed] [Google Scholar]
- 24.IFRC, Unicef . Building trust within and across communities for health emergency response, 2020. Available: https://apps.who.int/gpmb/assets/thematic_papers_2020/tp_2020_3.pdf [Accessed 07 Jun 2021].
- 25.Unicef . Minimum standards and indicators for community engagement. Available: https://www.unicef.org/mena/reports/community-engagement-standards [Accessed 07 Jun 2021].
- 26.IFRC . Words to action: towards a community centered approach to preparedness and response in health emergencies, 2019. Available: https://apps.who.int/gpmb/assets/thematic_papers/tr-5.pdf [Accessed 07 Jun 2021].