Abstract
Objectives
To examine whether racial/ethnic differences in mortality rates have changed in recent years among adults in late midlife, and if so, how.
Methods
We analyze Health and Retirement Study data on non-Hispanic Whites (Whites), non-Hispanic Blacks (Blacks), and English- and Spanish-speaking Hispanics (Hispanic-English and Hispanic-Spanish), aged 50–64 from 2 periods: 1998–2004 (Period 1, n = 8,920) and 2004–2010 (Period 2, n = 7,224). Using survey-generalized linear regression techniques, we model death-by-end-of-period as a function of race/ethnicity and sequentially adjust for a series of period-specific baseline risk factors including demographics, health status, health insurance, health behaviors, and social networks. Regression decomposition techniques are used to assess the contribution of these factors to observed racial/ethnic differences in mortality rates.
Results
The odds ratio for death (ORD) was not statistically different for Blacks (vs. Whites) in Period 1 but was 33% higher in Period 2 (OR = 1.33; 95% confidence interval [CI] = 1.05–1.69). The adjusted ORD among Hispanic-English (vs. Whites) was not statistically different in both periods. The adjusted ORD among Hispanic-Spanish (vs. Whites) was lower (ORD = 0.36; 95% CI = 0.22–0.59) in Period 1 but indistinguishable in Period 2. In Period 1, 50.1% of the disparity in mortality rates among Blacks was explained by baseline health status, 53.1% was explained by financial factors. In Period 2, 55.8% of the disparity in mortality rates was explained by health status, 40.0% by financial factors, and 16.2% by health insurance status.
Discussion
Mortality rates among Blacks and Hispanic-Spanish have risen since the mid-1990s. Hispanic-Spanish may be losing their advantageous lower risk of mortality, long known as the “Hispanic Paradox.”
Keywords: Death rates, Disparities, Minorities
Research has documented longstanding differences in mortality rates among non-Hispanic Whites (hereafter, Whites), non-Hispanic Blacks (hereafter, Blacks), and Hispanics in the United States (McBean et al., 2004; Miller, 1997; National Center for Health Statistics, 2002, 2011; Sudano & Baker, 2006). Life expectancy at birth is highest for Hispanics (81.8 years) and lowest for Blacks (74.8 years), with Whites falling roughly in between 78.5 years as of 2016 estimates (National Center for Health Statistics, 2018). Most work, however, has approached the question of mortality by looking at life expectancy at birth or age 65, and less work has focused on middle-age death that conjures important and distinct socioeconomic and health mechanisms contributing to “early” mortality. Fewer studies still have investigated racial/ethnic differences in mortality among adults in late midlife, and if they are shrinking over time. This study contributes to the critical debate on premature deaths in late midlife and analyzes how socioeconomic and demographic factors contribute to them. We update published findings from the work of Sudano and Baker (2006) for the period 1992–1998 by examining two more recent periods, 1998–2004 and 2004–2010, using data from the Health and Retirement Study (HRS). Over these periods, two important economic shocks took place in the United States, the recession of the early 2000s and the Great Recession of 2007–2009.
Existing research points to disproportionate mortality rates among Blacks in the United States. Socioeconomic inequalities, lower social status, systemic discrimination, and endemic life course constraints present multiple jeopardies to Black individuals in the United States (Quiñones et al., 2011). Black Americans have earlier onsets of disease, show higher levels of comorbidities by midlife (e.g., more hypertension and diabetes), and present a greater prevalence of risky health behaviors such as smoking and drinking (Mokdad et al., 2004; Wong et al., 2002), particularly among males (Ho & Elo, 2013; Witbrodt et al., 2014). The combination of these factors triggers biological mechanisms (e.g., inflammation) starting in midlife and is likely to cause accelerated cardiovascular aging and heart disease leading to premature death among Blacks. Prior studies have also attributed differences in mortality rates between Blacks and Whites to Blacks’ lower socioeconomic status (SES), reduced access to health care, and lower quality health care (Baker et al., 2001; Kahn et al., 1994; Schulz et al., 2002).
Until recently, existing evidence has pointed to an epidemiological paradox among Hispanics—“an oversimplified idiom” according to some (Brown & Tucker-Seeley, 2018)—who present comparable mortality rates, as well as parity in certain health outcomes, compared to Whites, despite economic and social status profiles that are comparable to Black Americans (Ruiz et al., 2013). Several explanations have been proposed for this paradox: (a) the “healthy migrant effect” resulting from positive health selection into migration, (b) the protective “enclave effect” that provides a social buffer against health shocks in the host country, (c) the “salmon bias” whereby sicker individuals migrate back to their home countries and get excluded from morbidity and mortality estimates, as well as, until recently, (d) relatively weak data on Hispanics which lead to poor ascertainment of Hispanic origin and increase imprecision in morbidity and mortality counts. Studies have also recognized a heterogeneity of health outcomes among Hispanics based on nativity, acculturation, country of origin, and cultural differences (Arcia et al., 2001; Fiscella et al., 2002; Sudano & Baker, 2006). The debate over the Hispanic paradox remains unsettled as evidence for and against health and mortality advantages continue to be vigorously debated in the literature. Recent work by Boen & Hummer (2019) found limited evidence of healthy migrant patterns among foreign-born Hispanics, when they examined a range of health outcomes, including functional limitations, depressive symptoms, metabolic dysregulation, and C-reactive protein. Additionally, they reported that across all of these outcomes, socioeconomic differences between older age Hispanics, Blacks, and Whites were the key driver for health disparities, and that foreign-born Hispanics endured greater hardships, stress, and health risk despite potentially living longer lives.
The common threads linking the arguments on health and mortality outcomes in race/ethnic minorities (relative to non-Latino Whites) include (a) the fundamental influence of social status and economic disadvantages and (b) the consequences of ingrained and persistent social inequities to health damages over the life course. Still, recent research on middle-aged White males in the United States also suggests challenging mortality and health patterns in this traditionally advantaged group (Case & Deaton, 2015), resulting from decades of accumulation in social and economic stressors. The increase is larger among Whites with lower education and is attributed mainly to an increase in alcohol and drug poisonings, suicide, and chronic liver diseases among White men in this age range. The debate around Case and Deaton’s findings is ongoing (Gelman & Auerbach, 2016) to further clarify its extension to White women with similar socioeconomic profiles and to ascertain the shift in trajectory, establish its timing and duration, and establish whether it constitutes a permanent shift in trends for this group (Brown & Tucker-Seeley, 2018). A study that investigated Black–White disparities in life expectancy at age 1 found a substantial portion of the racial/ethnic differences in mortality is associated with socioeconomic and demographic characteristics, 80% for the case of males and 70% for the cases of females (Geruso, 2012). To the best of our knowledge, very few studies have investigated racial/ethnic mortality differences in midlife across two time periods. This study contributes to the emerging and critical debate on premature midlife death and analyzes the contribution of socioeconomic and demographic factors in midlife.
Living longer healthier lives and eliminating disparities across racial and ethnic groups are a stated goal of U.S. health policy (Hill et al., 2015). Traditional inequities in health and mortality are altered and inflated by decades-long widening of socioeconomic and wealth inequalities, dismantling of traditionally protective social institutions and norms and system safety nets, and relentless changes in national and international economic regimes. For example, Census statistics suggest that by the end of the first decade of the 21st century, slightly more than a third of Americans had at least one spell of poverty lasting at least 2 months (Current Population Reports, 2017). These changes are particularly important among middle-aged adults as they may bring about future health vulnerabilities at old age due to limited resources and have important systemic and familial economic and social consequences in an increasingly older and diversified society (Walker et al., 2010). Yet, the evidence regarding mortality outcomes among adults in late midlife remains underdeveloped, as the majority of research tends to examine life expectancy at birth or at age 65.
Late midlife is a critical stage in the life course. Previous work has addressed the physical, psychological, cognitive, and financial significance of this life stage (Cockerham et al., 2020; Martin & Willis, 2005; Mejía et al., 2015). In the following, we concisely describe some of these arguments. Briefly, on the one hand, late midlife represents a period of maximal mental maturity, individual agency, accomplishments, and resources. On the other hand, late midlife often ushers in fundamental changes, such as generational shifts (e.g., parental frailty or death, children setting up separate households), and for many, it is a final stage of occupation and economic attainment and the prelude to retirement. A death in this stage of life can crucially disrupt these processes. Late midlife is also critical for physical and mental health, it is the period where the cumulative effects of childhood and early adulthood circumstances and behaviors start showing, it sets off the development of chronic health problems (e.g., hypertension and heart disease) and the prevalence of physical inactivity and obesity, is a precursor to physical decline, and portends a fundamental recognition of aging and its attendant concerns about self and meaning. Outcomes at this stage of life reflect lifetime accumulation of disparities and inequities in the distributions of economic, social, and cultural determinants of health and health behaviors that are largely locked-in by then. Late midlife is akin to a “sifting mechanism” and overcoming this critical period slows down differentiation along with known social determinants of health and inaugurates the age-as-leveler of health phenomena (Ferraro & Farmer, 1996).
The primary aims of this study were (a) to examine whether and to what extent racial/ethnic differences in mortality rates among adults in late midlife have changed, and (b) to test the consistency in the contribution of various risk factors to group differences if they exist. We address our aims by analyzing nationally representative longitudinal data spanning 1998–2010. Our study updates findings from the work of Sudano and Baker (2006), who examined racial/ethnic differences in mortality among adults in late midlife for an earlier period, 1992–1998.
Method
Data and Study Population
We use data from the 1998, 2004, and 2010 waves of the RAND HRS version-P (Bugliari et al., 2016). In line with our focus on middle-age mortality and its risks, we restrict our analyses to two sets of HRS participants: those who were between age 50 and 64 in 1998 and those who were between age 50 and 64 in 2004. We focus on two time periods, 1998–2004 and 2004–2010, and examine whether mortality rates changed over time, both within and between racial/ethnic groups for adults in this age range.
In estimating models for our first period, we use the respondents’ baseline weights for 1998 and follow up respondents until 2004. For consistency of the estimates across models, only observations with complete information of all variables were used in analyses. We follow similar procedures for the second period, 2004–2010, using the baseline weight of 2004 and following up respondents until 2010. The first period includes 8,920 observations, age 50–64, of which 6,696 were Whites, 1,426 were Blacks, 390 were English-speaking Hispanics (hereafter, Hispanic-English), and 408 were Spanish-speaking Hispanics (hereafter, Hispanic-Spanish). The analytic sample for the second period includes 7,224 observations including 5,261 Whites, 1,148 Blacks, 452 Hispanic-English, and 363 Hispanic-Spanish (Table 1)
Table 1.
Descriptive Statistics of Baseline Study Population by Racial/Ethnic Group in the Health and Retirement Study From 1998 to 2004 and 2004–2010
| Period 1: 1998–2004 (unweighted N = 8,920) | Period 2: 2004–2010 (unweighted N = 7,224) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N = 6,696 | N = 1,426 | N = 390 | N = 408 | N = 8,920 | N = 5,261 | N = 1,148 | N = 452 | N = 363 | N = 7,224 | |
| NHW | NHB | HE | HS | Total | NHW | NHB | HE | HS | Total | |
| Gender (%)1***/2*** | ||||||||||
| Male | 49.8 (0.4) | 38.4 (0.8) | 47.9 (1.7) | 43.3 (1.6) | 47.5 (0.4) | 48.3 (0.6) | 38.1 (1.1) | 48.6 (2.3) | 46.5 (2.4) | 46.5 (0.5) |
| Female | 50.2 (0.4) | 61.6 (0.8) | 52.1 (1.7) | 56.7 (1.6) | 52.5 (0.4) | 51.7 (0.6) | 61.9 (1.1) | 51.4 (2.3) | 53.5 (2.4) | 53.5 (0.5) |
| Marital status (%)1***/2*** | ||||||||||
| Married/partnered | 80.6 (0.6) | 56.7 (1.9) | 73.5 (1.9) | 77.2 (2.0) | 76.2 (0.6) | 78.5 (0.6) | 54.9 (1.7) | 68.7 (2.0) | 75.2 (2.3) | 73.8 (0.6) |
| Separated/divorced | 10.7 (0.4) | 23.1 (1.2) | 16.5 (1.8) | 11.9 (1.5) | 13.1 (0.4) | 12.6 (0.5) | 25.4 (1.4) | 20.2 (2.0) | 12.9 (1.7) | 15.2 (0.5) |
| Widow/never married/spouse Abs. | 8.7 (0.4) | 20.2 (1.3) | 10.1 (1.4) | 10.9 (1.5) | 10.7 (0.4) | 8.8 (0.4) | 19.7 (1.2) | 11.1 (1.3) | 11.9 (1.8) | 11.0 (0.3) |
| Income in tertiles (%)1***/2*** | ||||||||||
| First—Bottom | 17.3 (0.8) | 42.5 (1.9) | 33.0 (2.5) | 60.0 (3.2) | 23.9 (0.9) | 16.8 (0.8) | 38.8 (1.7) | 34.9 (3.0) | 56.6 (4.1) | 23.5 (0.9) |
| Second—Middle | 30.6 (0.7) | 31.1 (1.5) | 39.2 (3.1) | 31.5 (3.7) | 31.0 (0.6) | 29.1 (1.1) | 29.5 (1.4) | 29.7 (3.2) | 35.7 (3.3) | 29.5 (0.8) |
| Third—Top | 52.2 (1.2) | 26.4 (1.8) | 27.8 (3.0) | 8.6 (1.8) | 45.0 (1.2) | 54.1 (1.2) | 31.7 (1.4) | 35.4 (3.9) | 7.6 (1.7) | 47.0 (1.1) |
| Wealth in tertiles (%)1***/2*** | ||||||||||
| First—Bottom | 23.7 (0.9) | 61.8 (2.3) | 47.4 (2.3) | 73.2 (2.7) | 33.2 (1.1) | 25.2 (1.0) | 60.0 (1.8) | 48.0 (3.8) | 66.3 (3.9) | 34.4 (1.2) |
| Second—Middle | 35.3 (1.0) | 29.1 (1.6) | 37.3 (2.7) | 22.7 (2.5) | 33.8 (0.9) | 35.0 (0.9) | 28.3 (1.5) | 33.2 (3.0) | 26.0 (3.1) | 33.3 (0.9) |
| Third—Top | 41.0 (1.2) | 9.1 (1.2) | 15.4 (3.0) | 4.2 (1.3) | 33.0 (1.0) | 39.9 (1.3) | 11.7 (1.1) | 18.7 (2.7) | 7.7 (1.6) | 32.3 (1.1) |
| Insurance plan (%)1***/2*** | ||||||||||
| No insurance plan | 24.6 (0.8) | 40.5 (2.2) | 38.8 (3.0) | 71.7 (2.8) | 29.8 (1.0) | 17.3 (0.6) | 37.2 (1.7) | 38.4 (3.3) | 60.6 (4.1) | 24.0 (0.9) |
| One or more insurance plan | 75.4 (0.8) | 59.5 (2.2) | 61.2 (3.0) | 28.3 (2.8) | 70.2 (1.0) | 82.7 (0.6) | 62.8 (1.7) | 61.6 (3.3) | 39.4 (4.1) | 76.0 (0.9) |
| Self-reported health status (%)1***/2*** | ||||||||||
| Excellent/very good/ good | 78.2 (0.7) | 60.0 (1.8) | 63.2 (2.4) | 47.4 (2.1) | 73.2 (0.8) | 79.6 (0.6) | 61.6 (1.8) | 61.2 (2.6) | 44.6 (2.8) | 73.8 (0.7) |
| Fair/poor | 21.8 (0.7) | 40.0 (1.8) | 36.8 (2.4) | 52.6 (2.1) | 26.8 (0.8) | 20.4 (0.6) | 38.4 (1.8) | 38.8 (2.6) | 55.4 (2.8) | 26.2 (0.7) |
| Smoking prevalence (%)1**/2** | ||||||||||
| No | 78.4 (0.8) | 77.1 (1.1) | 84.0 (1.4) | 82.6 (1.8) | 78.6 (0.6) | 80.8 (0.7) | 76.5 (1.4) | 82.2 (2.0) | 84.2 (2.3) | 80.3 (0.6) |
| Yes | 21.6 (0.8) | 22.9 (1.1) | 16.0 (1.4) | 17.4 (1.8) | 21.4 (0.6) | 19.2 (0.7) | 23.5 (1.4) | 17.8 (2.0) | 15.8 (2.3) | 19.7 (0.6) |
| Living parents (%)1***/2** | ||||||||||
| None alive | 55.2 (0.6) | 61.0 (1.6) | 54.6 (2.3) | 61.4 (1.8) | 56.4 (0.6) | 54.1 (0.6) | 58.7 (1.6) | 50.0 (2.9) | 51.0 (2.8) | 54.4 (0.7) |
| Atleast one alive | 44.8 (0.6) | 39.0 (1.6) | 45.4 (2.3) | 38.6 (1.8) | 43.6 (0.6) | 45.9 (0.6) | 41.3 (1.6) | 50.0 (2.9) | 49.0 (2.8) | 45.6 (0.7) |
| Drinking prevalence (%)1***/2*** | ||||||||||
| Never drinks | 42.8 (1.1) | 62.9 (1.5) | 47.7 (2.7) | 72.9 (1.8) | 47.6 (0.9) | 37.2 (0.9) | 54.9 (2.0) | 42.2 (3.3) | 67.8 (3.0) | 42.0 (0.9) |
| At most once a week | 31.5 (0.7) | 24.2 (1.4) | 31.9 (2.5) | 19.6 (1.8) | 29.8 (0.6) | 35.0 (0.9) | 28.4 (1.5) | 38.0 (3.1) | 22.4 (2.4) | 33.4 (0.8) |
| More than once | 25.7 (0.7) | 13.0 (0.9) | 20.4 (2.1) | 7.4 (1.0) | 22.6 (0.6) | 27.8 (0.8) | 16.7 (1.4) | 19.8 (1.9) | 9.8 (2.3) | 24.6 (0.6) |
| Death (%)1***/2*** | ||||||||||
| No | 93.7 (0.3) | 90.2 (0.7) | 93.2 (1.0) | 95.5 (0.9) | 93.2 (0.3) | 93.6 (0.3) | 88.3 (1.0) | 93.9 (1.2) | 92.8 (1.8) | 92.7 (0.3) |
| Yes | 6.3 (0.3) | 9.8 (0.7) | 6.8 (1.0) | 4.5 (0.9) | 6.8 (0.3) | 6.4 (0.3) | 11.7 (1.0) | 6.1 (1.2) | 7.2 (1.8) | 7.3 (0.3) |
| Age (in years)1***/2 | ||||||||||
| Mean age | 57.8 (3.9) | 58.0 (3.8) | 57.3 (3.9) | 58.4 (3.8) | 57.8 (3.9) | 57.6 (4.3) | 57.4 (4.3) | 56.7 (4.5) | 57.0 (4.7) | 57.4 (4.3) |
| Education (in years)1***/2*** | ||||||||||
| Mean education | 13.0 (2.5) | 11.7 (2.9) | 11.3 (3.5) | 6.4 (4.0) | 12.4 (3.0) | 13.5 (2.4) | 12.5 (2.6) | 11.7 (3.5) | 7.2 (4.5) | 12.9 (3.0) |
| BMI1***/2*** | ||||||||||
| Mean BMI | 28.4 (5.6) | 30.3 (6.1) | 28.7 (5.3) | 29.1 (5.2) | 28.8 (5.7) | 29.2 (6.1) | 31.8 (6.9) | 29.9 (6.6) | 29.6 (5.6) | 29.7 (6.3) |
| Number of children1***/2*** | ||||||||||
| Mean number of children | 3.1 (1.8) | 3.7 (2.4) | 3.5 (2.2) | 4.4 (2.7) | 3.3 (2.0) | 2.8 (1.8) | 3.4 (2.2) | 3.3 (2.2) | 3.9 (2.5) | 3.0 (1.9) |
| Number of siblings1***/2*** | ||||||||||
| Mean number of sibling | 2.6 (2.1) | 4.1 (2.8) | 4.2 (3.2) | 4.6 (3.0) | 3.0 (2.4) | 2.6 (2.0) | 4.4 (2.8) | 4.7 (3.0) | 5.0 (3.2) | 3.2 (2.5) |
Notes: BMI = body mass index (kg/m2); HE = English-speaking Hispanics; HS = Spanish-speaking Hispanics; N = number of observations; NHB = non-Hispanic Blacks (Blacks); NHW = non-Hispanic Whites (Whites). Standard errors are reported inside the parenthesis.
1*** p < .001 in Period 1; 2***p < .001 in Period 2.
1** p < .01 in Period 1; 2**p < .01 in Period 2.
1* p < .05 in Period 1, 2*p < .05 in Period 2. Lastly, 1 represents not significant in Period 1 and 2 represents not significant in Period 2.
All analyses were conducted using survey functionalities in Stata Version 15 SE, and throughout, a p value of .05 or lower was considered needed for statistical significance. All statistical analyses and modeling steps, unless otherwise specified, account for the complex survey design of the HRS, including stratification, clustering, and probability weighting (Heeringa & Connor, 1995).
Outcome
The outcome of interest is the binary variable “death” that measures whether the person was dead or alive by the end of period. The death indicator is based on the respondent’s “Interview Status” in the RAND HRS data set.
Primary Predictor
Given the sampling design of the HRS, we restrict our focus to three racial/ethnic groups: Whites, Blacks, and Hispanics. We exclude Asian Americans, Native Americans, and other minority groups because of their small HRS sample counts. Furthermore, we distinguish between Hispanic-English and Hispanic-Spanish. Dividing Hispanics into these two language groups allows us to examine whether mortality and its determinants differ based on acculturation/assimilation into U.S. society. Each of these groups is identified and coded using the Tracker file provided by the HRS.
Risk Factors and Covariates
Our choice of independent variables in the models to be estimated is guided by the conceptual models explaining the differences in mortality and health status between racial/ethnic groups (Mendes de Leon & Glass, 2004; Schulz et al., 2002). In accordance with these models, we propose that the propensity for premature death is a function of race/ethnicity, and that group differences are likely to be explained by a host of demographic characteristics, financial resources, and potential for health care access through insurance, and to vary by health status, health behaviors, and levels of social networks.
Nonfinancial demographics include age, gender, marital status (married/partnered, separated/divorced, or widowed/never married/spouse absent), and total years of education. Financial resources include baseline income and total household wealth, both measured at the start of the period. We use tertile indicators for both income and wealth and set the first tertile corresponding to “Bottom” as the reference category. We use binary indicators (0 = Uninsured; 1 = Insured) to account for health insurance status based on the “number of health insurance plans” of the respondent.
Health status is measured by baseline self-reported health (excellent/very good/good, or fair/poor). To account for health-related behaviors, we include the individual’s body mass index (BMI), risk of drink prevalence (never drinks/once a week/more than once a week), and whether they currently smoke. Social network variables include the number of living children the person has, their number of living siblings, and whether at least one parent is alive (none alive or at least one parent is alive).
Statistical Analysis
First, we generated descriptive statistics for the variables of interest to characterize our target population. Race/ethnic-specific statistics are presented in Table 1. We use survey adjusted t tests to test group differences for continuous variables and chi-squared tests for categorical indicators.
Second, to examine the association between race/ethnicity and death, we estimate a series of logistic regression models in each period, sequentially adjusting for other potential determinants (Supplementary Appendix Tables 2 and 3). In a baseline model (called Model 1), we model death as a function of race/ethnicity. Model 2 further adjusts for nonfinancial demographic factors, Model 3 includes adjustment for financial demographic factors, Model 4 further adjusts for self-rated health status, Model 5 includes additional adjustment for health insurance status, Model 6 adds adjustment for health behaviors, and lastly, Model 7 also adjusts for social networks. Of interest is how the association between death and race/ethnicity changes (attenuated/accentuated) through sequential adjustment to these variables.
Third, we conduct regression decomposition (RD) analyses to more formally quantify the relative importance of various contributing factors to the observed racial/ethnic differences in mortality (Table 3). Specifically, we conduct an Oaxaca–Blinder (OB) RD analysis, as modified for use in binary outcomes (Jann, 2008), in each period. OBRD reveals what portion of a difference in mortality, for example, between Blacks and Whites, is explained by differences in the measured characteristics of these two populations, such as by differences in health status, insurance coverage, and other correlates of mortality, and what portion is not explained by them. Detailed discussions of OBRD are available elsewhere (Blinder, 1973; Oaxaca, 1973). Supplementary Appendix Table 4 provides a brief description of our OBRD specification, and Supplementary Appendix Tables 2 and 3 report the logistic regression models estimated for this analysis. The difference in mortality rates was only significant between Whites and Blacks, and details of the differences are reported in Table 3.
Table 3.
Oaxaca–Blinder Regression Decomposition for Racial/Ethnic Group for 1998–2004 and 2004–2010
| Period 1: 1998–2004 | Period 2: 2004–2010 | |||||
|---|---|---|---|---|---|---|
| (1) NHB vs. NHW | Pr (death by 2004) | SE | p Value | Pr (death by 2010) | SE | p Value |
| NHB | 0.0983 | 0.007 | .0000*** | 0.1174 | 0.009 | .000*** |
| NHW | 0.0626 | 0.003 | .0000*** | 0.0636 | 0.003 | .000*** |
| Δ (NHB−NHW) | 0.0357 | 0.007 | .0000*** | 0.0538 | 0.010 | .000*** |
| Explained Δ | 0.0321 | 0.005 | .0000*** | 0.0374 | 0.006 | .000*** |
| Unexplained Δ | 0.0036 | 0.005 | .4318 | 0.0164 | 0.008 | .044 |
| Contributions to explained Δ | % Explained | p Value | % Explained | p Value | ||
| Nonfinancial factors | 7.4 | .505 | −19.4 | .080 | ||
| Financial factors | 53.1 | .001** | 40.0 | .003** | ||
| Insurance | 8.0 | .115 | 16.2 | .023* | ||
| Health status | 50.1 | .000*** | 55.8 | .000*** | ||
| Health behaviors | 6.9 | .378 | 11.3 | .125 | ||
| Social network | −25.4 | .005** | −3.8 | .725 | ||
| (2) HE vs. NHW | Pr (death by 2004) | SE | p Value | Pr (death by 2010) | SE | p Value |
| HE | 0.0685 | 0.010 | .000*** | 0.0615 | 0.012 | .000*** |
| NHW | 0.0626 | 0.003 | .000*** | 0.0636 | 0.003 | .000*** |
| Δ (HE − NHW) | 0.0059 | 0.011 | .580 | −0.0021 | 0.012 | .858 |
| Explained Δ | 0.0096 | 0.005 | .044* | 0.0157 | 0.005 | .004** |
| Unexplained Δ | −0.0037 | 0.010 | .706 | −0.0178 | 0.010 | .076 |
| Contributions to explained Δ | % Explained | p Value | % Explained | p Value | ||
| Nonfinancial factors | −15.1 | .660 | −43.1 | .250 | ||
| Financial factors | 100.2 | .006** | 35.5 | .102 | ||
| Insurance | 18.9 | .181 | 34.8 | .058 | ||
| Health status | 109.8 | .004** | 107.4 | .001** | ||
| Health behaviors | −15.6 | .109 | 1.3 | .886 | ||
| Social network | −98.2 | .059 | −35.9 | .292 | ||
| (3) HS vs. NHW | Pr (death by 2004) | SE | p Value | Pr (death by 2010) | SE | p Value |
| HS | 0.0447 | 0.010 | .000*** | 0.0723 | 0.016 | .000*** |
| NHW | 0.0626 | 0.003 | .000*** | 0.0636 | 0.003 | .000*** |
| Δ (HS − NHW) | −0.0179 | 0.010 | .084 | 0.0087 | 0.016 | .583 |
| Explained Δ | 0.0165 | 0.006 | .004** | 0.0254 | 0.010 | .014* |
| Unexplained Δ | −0.0343 | 0.007 | .000*** | −0.0167 | 0.011 | .145 |
| Contributions to explained Δ | % Explained | p Value | % Explained | p Value | ||
| Nonfinancial factors | −7.8 | .796 | −41.4 | .328 | ||
| Financial factors | 58.2 | .014* | 39.1 | .070 | ||
| Insurance | 14.4 | .187 | 25.5 | .120 | ||
| Health status | 62.8 | .000*** | 99.7 | .000*** | ||
| Health behaviors | 4.9 | .564 | 1.6 | .893 | ||
| Social network | −32.5 | .034* | −24.5 | .211 | ||
Notes: HE = English-speaking Hispanics; HS = Spanish-speaking Hispanics; NHB = non-Hispanic Black (Blacks); NHW = non-Hispanic Whites (Whites). All statistical tests are compared to the referent group (“‘NHW’”). Δ = changes; Pr = probability; SE = standard error.
*p < .05, **p < .01, ***p < .001.
Sensitivity Analysis
We repeated our analysis with a distinction between Hispanics based on nativity status (U.S.-born Hispanics vs. foreign-born Hispanics) rather than distinguishing between them based on their language of choice for HRS interviews. Our findings from this sensitivity analysis are reported in Supplementary Appendix Tables 6–12. Not surprisingly, U.S.-born Hispanics showed a strong preference for English as their language of choice for completing HRS surveys. The percentage of survey completion in English for U.S.-born Hispanics was 81.72% in Period 1 (1998–2004) and 89.64% in Period 2 (2004–2010). Similarly, foreign-born Hispanics showed a strong preference for Spanish as the language of choice for completing the HRS surveys. The percentage of survey completion in Spanish for foreign-born Hispanics was 79.49% in Period 1 (1998–2004) and 71.86% in Period 2 (2004–2010; Supplementary Appendix Table 5).
Results
Risk Profiles
Minority groups (Blacks, Hispanic-English, and Hispanic-Spanish) had consistently lower SES relative to Whites (Table 1). Whites had higher educational attainment (13.0 years in Period 1 and 13.5 years in Period 2), higher incomes, for example, 52.2% of Whites were in the top income tertile in Period 1 and 54.1% were in the top income tertile in Period 2, and higher accumulated household wealth: 41.0% of those in top wealth tertile in Period 1 and 39.9% in Period 2. Whites were also the most likely to report having health insurance (75.4% in Period 1 and 82.7% in Period 2) and Hispanic-Spanish were the least likely to do so with only 28.3% reporting being insured in Period 1 and 39.4% in Period 2.
Additionally, minority respondents more often reported poor/fair health compared to Whites, with Hispanic-Spanish being most likely to report poor/fair health, for example, 52.6% reported it in Period 1 and 55.4% in Period 2, respectively. Differences in the health behaviors profiles by race/ethnicity were more complex. Blacks reported the highest rate of smoking (22.9% in Period 1 and 23.5% in Period 2), as well as the highest mean BMI (30.3 in Period 1 and 31.8 in Period 2), whereas Whites reported the highest levels of alcohol consumption (on more than once category, 25.7% in Period 1 and 27.8% in Period 2). Finally, all minority groups had higher means than Whites for the number of living children and number of living siblings.
Differences in Death Rates
Of the 8,920 respondents in Period 1 (1998–2004), 597 died by 2004, including 408 Whites, 144 Blacks, 25 Hispanic-English, and 20 Hispanic-Spanish (Supplementary Appendix Table 1). Compared to Whites, Blacks had a baseline odds of death of 1.63, followed by 1.10 for Hispanic-English and 0.70 for Hispanic-Spanish, respectively (Table 2). Of the 7,224 respondents in Period 2 (2004–2010), 516 died by 2010, including 328 Whites, 135 Blacks, 27 Hispanic-English, and 26 Hispanic-Spanish (Supplementary Appendix Table 1). Blacks had a baseline odds of death of 1.96 relative to Whites, followed by 0.96 for Hispanic-English and 1.15 for Hispanic-Spanish, respectively (Table 2).
Table 2.
Logistic Regression Results Showing Changes in Relative Risk of Death by 2004 and 2010 for Each Racial/Ethnic Groups, Compared to Non-Hispanic Whites, in the Health and Retirement Study
| Period 1: 1998–2004 | Period 2: 2004–2010 | |||
|---|---|---|---|---|
| Dead by 2004 | Dead by 2010 | |||
| Unweighted N = 8,920 | Unweighted N = 7,224 | |||
| OR [95% CI] | OR [95% CI] | OR [95% CI] | OR [95% CI] | |
| M1 | M2 | M1 | M2 | |
| NHW* | 1.00 [1.00–1.00] | 1.00 [1.00–1.00] | 1.00 [1.00–1.00] | 1.00 [1.00–1.00] |
| NHB | 1.63*** [1.37–1.95] | 1.05 [0.88–1.25] | 1.96*** [1.55–2.47] | 1.33* [1.05–1.69] |
| HE | 1.10 [0.79–1.54] | 0.90 [0.59–1.39] | 0.96 [0.62–1.49] | 0.71 [0.45–1.13] |
| HS | 0.70 [0.46–1.08] | 0.36*** [0.22–0.59] | 1.15 [0.66–1.99] | 0.65 [0.37–1.16] |
Notes: CI = confidence interval; HE = English-speaking Hispanics; HS = Spanish-speaking Hispanics; N = number of observations; NHW = non-Hispanic Whites (Whites); NHB = non-Hispanic Blacks (Blacks). 95% CI is reported inside the parenthesis. All statistical tests are compared to the referent group (“NHW”). M1 is the base model with race adjusted. M2 is the fully adjusted model that also adjusts for age, gender, marital status, income (in tertiles), wealth (in tertiles), education, insurance plan, self-reported health status, smoking prevalence, drinking prevalence, body mass index, number of living parents, number of siblings, and number of children.
*p < .05, **p < .01, ***p < .001.
In Period 1, the baseline odds of death for Blacks relative to Whites was 1.63 (95% confidence interval [CI]: 1.37–1.95), which is statistically significant (Table 2). Yet, after controlling for all the contributing factors in the model (nonfinancial demographics, financial demographics, health insurance, health status, health behaviors, and social networks), the odds of death among Blacks drops to 1.05, which is statistically insignificant. Thus, upon adjusting for all the covariates, mortality rates for Blacks and Whites in Period 1 were indistinguishable.
The baseline odds of death among Hispanic-English relative to Whites in Period 1 is statistically insignificant (Table 2), and after controlling for all contributing factors it remains insignificant. Thus, there are no differences in the mortality between Hispanic-English and Whites in Period 1.
In contrast, among Hispanic-Spanish in Period 1, the baseline odds of death relative to Whites is 0.70, which is statistically insignificant (Table 2), but after controlling for all covariates in the model, their odds of death relative to Whites drops to 0.36 (95% CI: 0.22–0.59) with strong statistical significance. Thus, we see significant differences in mortality among Hispanic-Spanish in Period 1, and they outlive Whites by more than a factor of 2.5. The results for this minority group are very optimistic based on these Period 1 findings.
In Period 2 (2004–2010), the baseline odds of death for Blacks relative to Whites is 1.96 (95% CI: 1.55–2.47), which is statistically significant (Table 2). After controlling for all the covariates, the odds of death for Blacks relative to Whites drops to 1.33 (95% CI: 1.05–1.69) and remains statistically significant. Thus, upon adjusting for all covariates, we observe a significantly greater risk of death-by-end-of-period among Blacks in Period 2.
In Period 2, the baseline odds of death for Hispanic-English relative to Whites is statistically insignificant (Table 2), and after controlling for all covariates, it remains insignificant. A similar pattern of findings emerges for Hispanic-Spanish relative to Whites. Their mortality rate is indistinguishable from that of Whites in both the baseline and adjusted models (Table 2).
Differences Decomposition Between Blacks and Whites
Table 3 reports the underlying factors that explain the significant difference in mortality rates observed between Blacks and Whites. In Period 1 (1998–2004), the unadjusted mortality rate was 9.83% for Blacks and 6.26% for Whites, and the difference was 3.57% (p < .001). The OBRD analysis reveals that nearly all of this difference, specifically 89.9%, can be “explained.” Contributing factors to the “explained” part include health status, financial demographics, and social network. More specifically, the 89.9% “explained” difference can be further decomposed into three parts: 50.1% (p < .001) is due to worse health among Blacks, 53.1% (p = .001) is due to lower income and wealth among Blacks, and −25.4% (p = .005) is due to social network. The total sum of health status and financial demographics slightly exceeds 100.00% because a few other characteristics negatively contribute to the explained mortality difference, such as Blacks’ modest advantage in social networks −25.4% (p = .005).
For Period 2 (2004–2010), the OBRD indicates a similar explanation for Blacks’ higher mortality rate, as given in Table 3. In this period, Blacks and Whites had unadjusted mortality rates of 11.74% and 6.36%, with a difference of 5.38% (p < .001). The difference decomposes into 69.5% which is “explained.” Significant contributors to the explained part include 55.8% (p < .001) is due to worse health among Blacks, 40.0% (p = .003) due to lower income and wealth among Blacks, and 16.2% (p = .023) due to a more frequent lack of health insurance among Blacks.
Thus, in both periods, the most important contributors to the higher mortality of Blacks are, in order of importance: their worse health, lower income and wealth, and more frequent lack of health insurance and support from social networks. Our finding that Blacks have a small advantage in terms of nonfinancial factors is perhaps not surprising given that a larger percentage of Blacks in the HRS are women, for example, 61.6% versus 50.2% among Whites in Period 1 and 61.9% versus 51.7% among Whites in Period 2 (from Table 1), and women tend to outlive men.
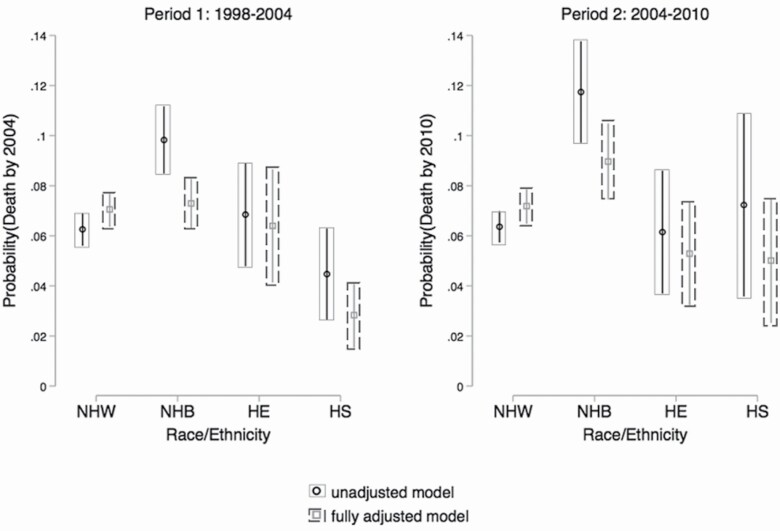
Additionally, we also test for the post hoc analysis of variance (ANOVA) contrast of average marginal effects for both crude (unadjusted) and fully adjusted logistic models (Table 4), in order to observe if these significant differences in mortality still persist between Blacks and Whites when all contributing factors are fully adjusted. Surprisingly, these differences tend to disappear in Period 1 (1998–2004). The average mortality difference between Blacks and Whites reduces from 3.6% to 0.3% in the fully adjusted model, and it also becomes statistically indistinguishable. The pattern is similar in Period 2 and the average mortality difference between Blacks and Whites reduces from 5.4% to 1.9%, but they do remain statistically significant (p = 0.03, Table 4). This is further illustrated in Figure 1 where the marginal estimates of the probability of death are plotted for both crude (unadjusted) and fully adjusted models for both time periods.
Table 4.
Post Hoc ANOVA Contrast of Average Marginal Effects
| Race | Contrasts | 95% CI | p Value | Contrasts | 95% CI | p Value |
|---|---|---|---|---|---|---|
| Period 1: 1998–2004 Unadjusted | Period 1: 1998–2004 Fully adjusted | |||||
| NHB vs. NHW | 3.6 | 2.2 to 5.0 | <.001*** | 0.3 | –0.8 to 1.4 | .58 |
| HE vs. NHW | 0.6 | −1.5 to 2.7 | .58 | –0.6 | –3 to 1.8 | .63 |
| HS vs. NHW | –1.8 | –3.7 to 0.1 | .06 | –4.3 | –5.7 to –2.8 | <.001*** |
| Period 2: 2004–2010 Unadjusted | Period 2: 2004–2010 Fully adjusted | |||||
| NHB vs. NHW | 5.4 | 3.2 to 7.6] | <.001*** | 1.9 | 0.2 to 3.6 | .03* |
| HE vs. NHW | –0.2 | –2.7 to 2.3 | .87 | –1.8 | –4.1 to 0.4 | .10 |
| HS vs. NHW | 0.9 | –2.8 to 4.5 | .64 | –2.2 | –4.8 to 0.3 | .09 |
Notes: CI = confidence interval; HE = English-speaking Hispanics; HS = Spanish-speaking Hispanics; NHB = non-Hispanic Blacks (Blacks); NHW = non-Hispanic Whites (Whites). 95% CI is reported inside the parenthesis. Estimates are based on crude and fully adjusted logistic regression models. All statistical tests are compared to the referent group (“NHW”). In the crude logistic model, covariates include only race. In the fully adjusted model, covariates include age, gender, marital status, income (in tertiles), wealth (in tertiles), education, insurance plan, self-reported health status, smoking prevalence, drinking prevalence, body mass index, number of living parents, number of siblings, and number of children.
*p < .05, **p < .01, ***p < .001.
Figure 1.
Marginal estimates results showing a probability of death by 2004 and 2010 for each racial/ethnic groups in unadjusted and fully adjusted models, in the Health and Retirement Study. HE = English-speaking Hispanics; HS = Spanish-speaking Hispanics; NHB = non-Hispanic Blacks (Blacks); NHW = non-Hispanic Whites (Whites). In the unadjusted model, covariates include only race. In the fully adjusted model, covariates include age, gender, marital status, income (in tertiles), wealth (in tertiles), education, insurance plan, self-reported health status, smoking prevalence, drinking prevalence, body mass index, number of living parents, number of siblings, and number of children.
Differences in Decomposition Between Hispanic-English and Whites
There appears to be no significant differences in mortality between Hispanic-English and Whites in both Period 1 (1998–2004) and Period 2 (2004–2010) when we looked at the OBRD analysis (Table 3). In Period 1, unadjusted mortality rate for Hispanic-English was 7.24% and for Whites it was 6.26% (Supplementary Appendix Table 1). Similarly, in Period 2, the unadjusted mortality rate for Hispanic-English was 6.15% and for Whites it was 6.36% (Supplementary Appendix Table 1).
When we tested for the post hoc ANOVA contrast of the average marginal effects, the difference remained statistically indistinguishable in both time periods (Table 4), and Figure 1 shows the CI bands of Hispanic-English overlapped with the CI bands of Whites, in both crude (unadjusted) and fully adjusted models in both Period 1 and Period 2, thus clearly demonstrating no significant difference between Hispanic-English and Whites.
Differences in Decomposition Between Hispanic-Spanish and Whites
According to the OBRD analysis (Table 3), there appears to be no significant difference between Hispanic-Spanish and Whites. The unadjusted mortality rate for Hispanic-Spanish was 6.03% and for Whites it was 6.26% (Supplementary Appendix Table 1). Similarly, in Period 2, the unadjusted mortality rate for Hispanic-Spanish was 7.67% and for Whites it was 6.36% (Supplementary Appendix Table 1). Interestingly, when we tested for the post hoc ANOVA contrast of the average marginal effects, the difference in deaths in Period 1 becomes −4.2% from −1.8% when controlling for all contributing factors, showing an even lower mortality rate among Hispanic-Spanish (Table 4) and it is statistically significant (p <.001, Table 4). This finding can be explained from the view of Hispanic paradox advantage. In our study, this mainly arises from a social network advantage of the Hispanic-Spanish, as they have a higher number of living parents, siblings, and children relative to Whites. This is also demonstrated in Figure 1 where the fully adjusted model clearly demonstrates a significant difference in death rates.
However, in Period 2, the average marginal estimates of the difference in death rates become statistically indistinguishable in the fully adjusted model suggesting a loss of the advantage for the Hispanic-Spanish (Table 4 and Figure 1). The CI bands are overlapping with each other in Figure 1 in Period 2, demonstrating no significant differences in death rate.
Sensitivity Results
The details of the sensitivity results are listed in Supplementary Appendix Tables 6–12. As expected, given the overlap between language preference and nativity in our data, the results were qualitatively consistent with the main findings.
Discussion
Five findings emerge from this analysis. First, among U.S. adults in late midlife, significant differences in mortality rates persist between Whites and Blacks. Compared to Whites aged 50–64, Blacks in this age range were 1.63 times more likely to die between 1998 and 2004, and 1.96 more likely to die between 2004 and 2010. When last measured for 1992 through 1998, Blacks were 1.82 times more likely to die than were Whites (Sudano & Baker, 2006). All three of these point estimates are statistically indistinguishable.
Second, after adjusting for all contributing factors, Blacks’ relative odds of death falls substantially in both periods, and it remained significant at 1.33 in the latter period (Table 2). This suggests that between 2004 and 2010 factors beyond those addressed through our models may have also contributed to higher mortality among Blacks. (We discuss this possibility in more detail below.)
Third, mortality rates for Hispanics differ depending on their spoken language. Rates for Hispanic-English were statistically indistinguishable from White mortality rates in both 1998–2004 and 2004–2010, regardless of whether or not the estimates were adjusted for individual characteristics. This finding too parallels the earlier finding of Sudano and Baker (2006) for 1992–1998.
Yet, the mortality rate of Hispanic-Spanish was lower than that of Whites in 1998–2004 after adjusting for individual characteristics. Rates for Hispanic-Spanish were statistically indistinguishable over Whites in 2004–2010. Evidence suggests that the observed longevity advantage for Hispanic-Spanish speakers is no longer stemming from a lower mortality risk in midlife, and this may have lessened their advantage during this time period. Although Hispanic-Spanish had the lowest socioeconomic profile of all the groups (Table 1), they experienced lower mortality in 1998–2004. Lower rates are also consistent with the findings of Sudano and Baker (2006) for 1992–1998. However, based on self-reported health, Hispanic-Spanish were highest in reporting poor/fair health (Table 1), but they had the lowest mortality of all groups in 1998–2004. More than half of Hispanic-Spanish reported they were in fair/poor health, regardless of their greater longevity. It may be the case that longevity alone may not fully explain the quality of life of individuals. The findings were also consistent with our sensitivity analysis of Hispanics with nativity status (U.S.-born Hispanics vs. foreign-born Hispanics) in Supplementary Appendix Tables 6–12. They yielded similar results as the majority of U.S.-born Hispanics were associated with Hispanic-English and foreign-born Hispanics were associated with Hispanic-Spanish as mentioned before.
Fourth, differences in the measured characteristics of Blacks and Whites explain nearly all of the difference in their mortality rates, both in 1998–2004 and 2004–2010. In both periods, worse health among Blacks was the single most important factor contributing to the difference. About half of the difference from Whites in both periods was due to their worse health. Lower income and wealth among Blacks was the second most important factor, accounting for another 40%–50% of the mortality gap, and their higher incidence of being uninsured was the third most important factor (in Period 2, 2004–2010) contributing to the difference in mortality. Lastly, Blacks exhibited protective effects from a social network (in Period 1, 1998–2004) and accounted approximately −25% of the difference in Period 1, 1998–2004 as they fared better relative to Whites.
Finally, comparing 1992–1998 (Sudano & Baker, 2006), 1998–2004, and 2004–2010, the broad picture that emerges is there has been no progress in reducing racial/ethnic differences in mortality among U.S. adults in late midlife. Differences in the risk of dying between Blacks and Whites in late midlife have not narrowed at all, and in 2004–2010, they are harder to explain via the measured characteristics of Blacks and Whites. Likewise, Hispanic-English made no gains over these 18 years in terms of their risk of dying compared to Whites. They were indistinguishable from Whites back in 1992–1998 and remained so up through 2004–2010. Hispanic-Spanish, however, held a modest “longevity advantage” during 1992–1998 and 1998–2004, but it vanished by 2004–2010.
The Blacks/Whites mortality gap may be harder to explain in 2004–2010 through measured characteristics because the Great Recession occurred during this time period, and it might have affected Blacks more than Whites. According to the Bureau of Labor Statistics (2010), Blacks experienced the highest rate of unemployment (14.8%) in 2009 compared to Whites (7.3%) and Hispanics (12.1%). This suggests Blacks likely experienced more job losses during this period, and job loss during recessions has been linked with higher mortality rate among adults aged 45–66 (Noelke & Beckfield, 2014). Also, during the 2007–2009 subprime mortgage crisis, Blacks lost a significant portion of their assets with a 53% drop in their median net worth, compared to a 16% drop among Whites and a 66% drop among Hispanics (Taylor et al., 2011). Blacks also comprised the largest group in terms of zero or negative assets (35%). Their worsening finances over this period may have also contributed to some deaths. Thus, the economic shocks of the Great Recession, for example, more joblessness, loss in income, and loss in assets may be partly why our model did not perform as well in the last period. Further analysis of this issue is clearly needed to determine whether Blacks were indeed disproportionately affected by that major economic recession.
This study extends the research on racial/ethnic differences in mortality and their determinants in several ways and includes several strengths. First, we analyze nationally representative HRS data covering a 12-year period, 1998–2010, a time frame more recent than the time periods considered in previous studies. Second, we examine racial/ethnic differences in mortality over two separate 6-year periods, 1998–2004 and 2004–2010, allowing us to see whether changes occurred between these two periods, or since the period, 1992–1998, which Sudano and Baker (2006) examined. Third, we pay special attention to the possibility that mortality rates differ between Hispanic-English and Hispanic-Spanish. The few studies that have divided Hispanics into these two subgroups (Sudano & Baker, 2006) found evidence of very different mortality rates, so they should be distinguished from each other. Fourth, in modeling the determinants of mortality, we control for the simultaneous contributions of race/ethnicity, nonfinancial demographic factors, financial demographic factors, health status, health insurance, health behaviors, and social networks. None of the studies discussed above controlled for all of these factors, but this study does. Finally, particularly unique is our use of RD techniques to decompose racial/ethnic differences in mortality into parts that are attributable to various factors, such as differences in health, differences in income, and so on.
Yet, there are several limitations of this analysis that should be noted. First, most of the differences in racial/ethnic groups are associated with financial demographic factors, health status, and health insurance. The controls for the other contributing factors (health behaviors and social networks) had quite small effect on the racial/ethnic differences (Supplementary Appendix Tables 2 and 3). Second, our measure of health, namely self-reported health status, is subjective and may have been reported differently by the minority groups due to cultural differences (Dowd & Todd, 2011). Studies have shown that this difference in reporting gets lower when they are used in shorter form (Peek et al., 2004). The RAND HRS already defines the self-reported health in shorter form of five categories, we further collapsed them into two categories thus reducing some of the bias. Third, we categorized the Hispanic groups into two subcategories based on language to capture the acculturation/assimilation as described in the work of Sudano and Baker (2006) and using their same argument we agree that we will not be able to capture all the effects and we may require additional data (such as country of origin) to be more specific. The additional sensitivity analysis of the Hispanics with nativity also reaffirms that our results were consistent (Supplementary Appendix Tables 6–12). Fourth, we were limited to use only a few variables for our social network variables. Our analysis would have been more comprehensive if we had more social variables such as number of friends, time spent on different social activities, etc. Similarly, for our health behavior variables, we could not find data on drug usage. Further research needs to be done in these areas and additional data sets could be used to supplement the research. Fifth, some of the deaths in the model might have occurred due to other reasons such as traffic accidents, suicides, etc. Lastly, we were not able to control some of our covariates that were time dependent and account for other external factors that could affect mortality.
In summary, our findings of a lack of any reduction in racial/ethnic disparities in mortality among adults in late midlife over two periods, 1998–2004 and 2004–2010, is discouraging. Since the early 1980s, with the surgeon general’s report that highlighted the widespread disparities in health in the United States, and over consecutive decades of evidence of health differences and inequities, disparities in mortality outcomes remain a problem in the United States. It is perhaps not surprising given that several key determinants of mortality rates in this age range have also not improved much over time for minority populations. In particular, gaps in income between Blacks and Whites and between Hispanics and Whites have widened over time rather than narrowed (Daly et al., 2017; Karageorge, 2017; U.S. Census Bureau, 2019), and Blacks and Hispanics continue to be more likely to lack health insurance (Centers for Disease Control and Prevention, 2011; Monheit et al., 2000). Rates of obesity and diabetes have also remained persistently higher among Blacks and Hispanics compared to Whites, and Blacks have consistently had much higher rates of hypertension than Whites (Centers for Disease Control and Prevention, 2011). Broadly speaking, unless the relative standing of minorities improves on these underlying determinants of mortality, disparities in mortality among adults in late midlife are likely to persist.
It is also quite possible that racial/ethnic disparities in mortality in late midlife have actually worsened since 2010. This is because the Great Recession led to larger declines in income and employment among Blacks and Hispanics than it did among Whites (Taylor et al., 2011), and because the Coronavirus pandemic, still unfolding across the United States, appears to be disproportionately hurting Blacks and Hispanics (Selden & Berdahl, 2020). If reducing and eliminating racial/ethnic disparities continues as a policy goal, then continuing research on this front is vital.
Funding
W. Tarraf is supported by the National Institute on Aging (NIA; R01AG48642). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the views of NIA.
Supplementary Material
Acknowledgments
We thank Allen Goodman and Shooshan Danagoulian for their valuable comments on the study.
Conflicts of Interest
None declared.
Author Contributions
A. Doza planned the study, conducted the data analysis, and wrote the article. W. Tarraf supervised all statistical analysis and helped to revise the article. G. Jensen helped to plan the study, including instrumentation, and to revise the article.
References
- Arcia, E., Skinner, M., Bailey, D., & Correa, V. (2001). Models of acculturation and health behaviors among Latino immigrants to the US. Social Science & Medicine (1982), 53(1), 41–53. doi: 10.1016/s0277-9536(00)00310-5 [DOI] [PubMed] [Google Scholar]
- Baker, D. W., Sudano, J. J., Albert, J. M., Borawski, E. A., & Dor, A. (2001). Lack of health insurance and decline in overall health in late middle age. The New England Journal of Medicine, 345(15), 1106–1112. doi: 10.1056/NEJMsa002887 [DOI] [PubMed] [Google Scholar]
- Blinder, A. S. (1973). Wage discrimination—Reduced form and structural estimates. Journal of Human Resources, 8(4), 436–455. doi:10.2307/144855 [Google Scholar]
- Boen, C. E., & Hummer, R. A. (2019). Longer-but harder-lives?: The Hispanic health paradox and the social determinants of racial, ethnic, and immigrant-native health disparities from midlife through late life. Journal of Health and Social Behavior, 60(4), 434–452. doi: 10.1177/0022146519884538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, L., & Tucker-Seeley, R. (2018). Commentary: Will ‘deaths of despair’ among whites change how we talk about racial/ethnic health disparities? Ethnicity & Disease, 28(2), 123–128. doi: 10.18865/ed.28.2.123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bugliari, D., Campbell, N., Chan, C., Hayden, O., Hurd, M., Main, R., Mallett, J., McCullough, C., Meijer, E., Moldoff, M., Pantoja, P., Rohwedder, S., & St.Clair, P. (2016). RAND HRS data documentation, version P. RAND Center for the Study of Aging. [Google Scholar]
- Bureau of Labor Statistics, U.S. Department of Labor . (2010). Unemployment rates by race and ethnicity, 2010. Retrieved from https://www.bls.gov/opub/ted/2011/ted_20111005.htm
- Case, A., & Deaton, A. (2015). Rising morbidity and mortality in midlife among white non-Hispanic Americans in the 21st century. Proceedings of the National Academy of Sciences of the United States of America, 112(49), 15078–15083. doi: 10.1073/pnas.1518393112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . (2011). CDC health disparities and inequalities report—United States, 2011. Morbidity and Mortality Weekly Report, 60(Health Insurance), 35–37. Retrieved from https://www.cdc.gov/mmwr/pdf/other/su6001.pdf [Google Scholar]
- Cockerham, W. C., D Wolfe, J., & Bauldry, S. (2020). Health lifestyles in late middle age. Research on Aging, 42(1), 34–46. doi: 10.1177/0164027519884760 [DOI] [PubMed] [Google Scholar]
- Current Population Reports . (2017). P60-259, income and poverty in the United States: 2016. U.S. Government Printing Office. [Google Scholar]
- Daly, M., Hobijn, B., & Pedtke, J. H. (2017). Disappointing facts about the black-white wage gap. FRBSF Economic Letter, 26, 1–5. http://www.frbsf.org/economic-research/files/el2017-26.pdf [Google Scholar]
- Dowd, J. B., & Todd, M. (2011). Does self-reported health bias the measurement of health inequalities in US adults? Evidence using anchoring vignettes from the Health and Retirement Study. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66(4), 478–489. doi: 10.1093/geronb/gbr050 [DOI] [PubMed] [Google Scholar]
- Ferraro, K. F., & Farmer, M. M. (1996). Double jeopardy, aging as leveler, or persistent health inequality? A longitudinal analysis of white and black Americans. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 51(6), 319–328. doi: 10.1093/geronb/51b.6.s319 [DOI] [PubMed] [Google Scholar]
- Fiscella, K., Franks, P., Doescher, M. P., & Saver, B. G. (2002). Disparities in health care by race, ethnicity, and language among the insured: Findings from a national sample. Medical Care, 40(1), 52–59. doi: 10.1097/00005650-200201000-00007 [DOI] [PubMed] [Google Scholar]
- Gelman, A., & Auerbach, J. (2016). Age-aggregation bias in mortality trends. Proceedings of the National Academy of Sciences of the United States of America, 113(7), E816–E817. doi: 10.1073/pnas.1523465113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geruso, M. (2012). Black-white disparities in life expectancy: How much can the standard SES variables explain? Demography, 49(2), 553–574. doi: 10.1007/s13524-011-0089-1 [DOI] [PubMed] [Google Scholar]
- Heeringa, S. G., & Connor, J. H. (1995). Technical description of the Health and Retirement Survey sample design. University of Michigan. [Google Scholar]
- Hill, C. V., Pérez-Stable, E. J., Anderson, N. A., & Bernard, M. A. (2015). The national institute on aging health disparities research framework. Ethnicity & Disease, 25(3), 245–254. doi: 10.18865/ed.25.3.245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho, J. Y., & Elo, I. T. (2013). The contribution of smoking to black-white differences in U.S. mortality. Demography, 50(2), 545–568. doi: 10.1007/s13524-012-0159-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jann, B. (2008). The Blinder-Oaxaca decomposition for linear regression models. Stata Journal, 8(4), 453–479. doi: 10.1177/1536867x0800800401 [DOI] [Google Scholar]
- Kahn, K. L., Pearson, M. L., Harrison, E. R., Desmond, K. A., Rogers, W. H., Rubenstein, L. V., Brook, R. H., & Keeler, E. B. (1994). Health care for black and poor hospitalized Medicare patients. Journal of the American Medical Association, 271(15), 1169–1174. [PubMed] [Google Scholar]
- Karageorge, E. (2017). The unexplainable, growing black-white wage gap. Monthly Labor Review, 140, 1. [Google Scholar]
- Martin, M., & Willis, S. L.(Eds.). (2005). Middle adulthood: A lifespan perspective. SAGE Publications, Inc. [Google Scholar]
- McBean, A. M., Li, S., Gilbertson, D. T., & Collins, A. J. (2004). Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: Whites, blacks, Hispanics, and Asians. Diabetes Care, 27(10), 2317–2324. doi: 10.2337/diacare.27.10.2317 [DOI] [PubMed] [Google Scholar]
- Mejía, S. T., Settersten, R. A.Jr, Odden, M. C., & Hooker, K. (2015). Responses to financial loss during the great recession: An examination of sense of control in late midlife. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(4), 734–744. doi: 10.1093/geronb/gbv054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon, C. F., & Glass, T. A. (2004). The role of social and personal resources in ethnic disparities in late-life health. In N. B. Anderson, R. A. Bulatao, & B. Cohen (Eds.), Critical perspectives on racial and ethnic differences in health in late life (pp. 353–405). The National Academies Press. doi: 10.17226/11086 [DOI] [PubMed] [Google Scholar]
- Miller, B. A. (1997). Racial/ethnic patterns of cancer in the United States: 1988–1992, Vol. 96. DIANE Publishing. [Google Scholar]
- Mokdad, A. H., Marks, J. S., Stroup, D. F., & Gerberding, J. L. (2004). Actual causes of death in the United States, 2000. Journal of the American Medical Association, 291(10), 1238–1245. doi: 10.1001/jama.291.10.1238 [DOI] [PubMed] [Google Scholar]
- Monheit, A. C., & Vistnes, J. P. (2000). Race/ethnicity and health insurance status: 1987 and 1996. Medical Care Research and Review, 57(Suppl. 1), 11–35. doi: 10.1177/1077558700057001S02 [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics . (2002). Chartbook on trends in the health of American. Department of Health and Human Services, Centers for Disease Control. Retrieved from https://www.cdc.gov/nchs/data/hus/hus02cht.pdf. doi: 10.1001/jama.289.7.838-b [DOI] [Google Scholar]
- National Center for Health Statistics . (2011). Health, United States, 2011 with special feature on socioeconomic status and health. Department of Health and Human Services, Centers for Disease Control. doi: 10.1037/e582072012-001 [DOI] [Google Scholar]
- National Center for Health Statistics . (2018). Health, United States, 2017: With special feature on mortality. Retrieved from https://www.cdc.gov/nchs/data/hus/2017/015.pdf
- Noelke, C., & Beckfield, J. (2014). Recessions, job loss, and mortality among older US adults. American Journal of Public Health, 104(11), e126–e134. doi: 10.2105/AJPH.2014.302210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oaxaca, R. (1973). Male-female wage differentials in urban labor markets. International Economic Review, 14, 693.– . doi: 10.2307/2525981 [DOI] [Google Scholar]
- Peek, M. K., Ray, L., Patel, K., Stoebner-May, D., & Ottenbacher, K. J. (2004). Reliability and validity of the SF-36 among older Mexican Americans. Gerontologist, 44(3), 418–425. doi: 10.1093/geront/44.3.418 [DOI] [PubMed] [Google Scholar]
- Quiñones, A. R., Liang, J., Bennett, J. M., Xu, X., & Ye, W. (2011). How does the trajectory of multimorbidity vary across black, white, and Mexican Americans in middle and old age? The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66(6), 739–749. doi: 10.1093/geronb/gbr106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruiz, J. M., Steffen, P., & Smith, T. B. (2013). Hispanic mortality paradox: A systematic review and meta-analysis of the longitudinal literature. American Journal of Public Health, 103(3), e52–e60. doi: 10.2105/AJPH.2012.301103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz, A. J., Williams, D. R., Israel, B. A., & Lempert, L. B. (2002). Racial and spatial relations as fundamental determinants of health in Detroit. The Milbank Quarterly, 80(4), 677–707, iv. doi: 10.1111/1468-0009.00028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Selden, T. M., & Berdahl, T. A. (2020). COVID-19 and racial/ethnic disparities in health risk, employment, and household composition: Study examines potential explanations for racial-ethnic disparities in COVID-19 hospitalizations and mortality. Health Affairs, 39. doi: 10.1377/hlthaff.2020.00897 [DOI] [PubMed] [Google Scholar]
- Sudano, J. J., & Baker, D. W. (2006). Explaining US racial/ethnic disparities in health declines and mortality in late middle age: The roles of socioeconomic status, health behaviors, and health insurance. Social Science & Medicine (1982), 62(4), 909–922. doi: 10.1016/j.socscimed.2005.06.041 [DOI] [PubMed] [Google Scholar]
- Taylor, P., Kochhar, R., Fry, R., Velasco, G., & Motel, S. (2011). Wealth gaps rise to record highs between Whites, Blacks and Hispanics. Pew Research Center, 37. [Google Scholar]
- U.S. Census Bureau . (2019). Income and poverty in the United States: 2018. Current Population Reports (P60-266).
- Walker, K. O., Steers, N., Liang, L. J., Morales, L. S., Forge, N., Jones, L., & Brown, A. F. (2010). The vulnerability of middle-aged and older adults in a multiethnic, low-income area: Contributions of age, ethnicity, and health insurance. Journal of the American Geriatrics Society, 58(12), 2416–2422. doi: 10.1111/j.1532-5415.2010.03189.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witbrodt, J., Mulia, N., Zemore, S. E., & Kerr, W. C. (2014). Racial/ethnic disparities in alcohol-related problems: Differences by gender and level of heavy drinking. Alcoholism, Clinical and Experimental Research, 38(6), 1662–1670. doi: 10.1111/acer.12398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong, M. D., Shapiro, M. F., Boscardin, W. J., & Ettner, S. L. (2002). Contribution of major diseases to disparities in mortality. The New England Journal of Medicine, 347(20), 1585–1592. doi: 10.1056/NEJMsa012979 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.