Abstract
Purpose
The current number of breast cancer survivors (BCS) in the United States is approximately 3.8 million, and this number is further expected to increase with improvement in treatments. Survivorship care plans (SCPs) are patient-centered tools that are designed to meet cancer survivors' informational needs about their treatment history, recommended health care, and health maintenance. However, the data on SCP benefits remain uncertain, especially in low-income and racial and ethnic minority cancer survivors. Patient navigation is an effective intervention to improve patient adherence and experience of interdisciplinary breast cancer treatment.
Objectives
This study sought to understand the role of lay patient navigators (LPN) in survivorship care planning for BCS in safety-net settings.
Methods
This study is a mixed methods pilot randomized clinical trial to understand the role of patient navigation in cancer survivorship care planning in a public hospital. We invited BCS who had completed active breast cancer treatment within 5 years. LPNs discussed survivorship care planning and survivorship care-related issues with BCS in the intervention arm over a 6-month intervention period and accompanied patients to their primary care appointment. LPNs also encouraged survivors to discuss health care issues with oncology and primary care providers. The primary objective was to assess BCS’ health-related quality of life (HRQOL). The secondary objectives were self-efficacy and implementation. We assessed implementation with 45–60-min semi-structured interviews with 15 BCS recruited from the intervention arm and 60-min focus groups with the oncologists and separately with LPNs.
Results
We enrolled 40 patients, 20 randomized to usual care and 20 randomized to LPN navigation. We did not find a statistically significant difference between the two arms in HRQOL. There was also no difference in self-efficacy between the two arms. Qualitative analysis identified implementation barriers to intervention that may have contributed to less effective intervention.
Implications for Cancer Survivors
Future survivorship care planning interventions need to consider: Cancer survivors’ needs and preferences, the need for dedicated resources, and the role of electronic health records in survivorship care plan delivery.
Keywords: Cancer survivors, safety net, patient navigation, survivorship care plans, implementation, care delivery
The current number of breast cancer survivors (BCS)1-5 in the United States is approximately 3.8 million, 6 and this number is further expected to increase with improvement in treatments. The major challenge of survivorship care is providing access to cost-effective, comprehensive care focused on identifying cancer recurrence, managing symptoms, identifying, and managing late effects of treatment, and health promotion.7,8 Medically underserved patients who are racial/ethnic minorities, are uninsured, and have limited English proficiency (LEP) are more likely to suffer worse health-related quality of life (HRQOL) and have unmet informational and psychosocial needs during survivorship.9-11 Moreover, safety-net hospitals and health networks in the United States that provide care for low-income and uninsured or underinsured patients often experience persistent shortages of personnel and resources.
In 2016, the American College of Surgeons, Committee on Cancer (COC) implemented an accreditation standard requiring cancer care programs to provide survivorship care plans (SCP) standard 3.3 to all patients treated for cancer with curative intent with the annual evaluation of these plans. 8 To date, the research suggests that existing SCP templates fail to address the information needs of cancer survivors and have limited value in addressing patients' needs and or as a coordination tool for transition from oncology to primary care.2,12 Burg et al described the delivery of SCPs in low literacy, minority BCS. They found that 45% of patients did not remember being given a treatment summary 13 and only 8.5% had shown it to another provider. 14 There is a lack of effective survivorship care interventions in medically underserved low-income, racial, and ethnic minority BCS who often continue to experience worse HRQOL.15,16
Burke et al conducted formative research with English-, Spanish-, Russian-, Tagalog-, and Cantonese-speaking breast cancer survivors to inform the development of materials for low literacy, multi-lingual patients to support the care transition from oncology to primary care and needs of low-income BCS. 17 Napoles et al have described the needs of Latina BCS and developed a framework for providing survivorship care. 18 These studies offer many insights into the disjointed and often chaotic experience of breast cancer treatment, the varied nature of these experiences and the prevalence of ineffective communication between cancer survivors and their cancer care teams highlights a need for a process and a written document to help women transition from oncology to primary care, particularly in safety-net settings. 17 Patient navigation is an effective intervention to improve patient adherence and treatment experience. The 2002 Institute of Medicine Report 19 outlined the disparities experienced by racial and ethnic minorities, and in response to this, the US Congress passed the Patient Navigator Outreach and Chronic Disease Prevention Act in 2005. 20 This act envisioned patient navigation as an effective intervention to improve health outcomes by reducing delays to quality care throughout the healthcare continuum. 21 Patient navigation is a patient-centered tool designed to mitigate multilevel barriers for the most at-risk populations by increasing access to diagnosis, treatment, supportive care services, psychosocial support, and education into the cancer care continuum.22,23 Since the mid-1990s, many US hospitals have implemented patient navigation programs to improve follow-up and treatment rates for cancer among medically underserved populations.24,25 Studies have shown that navigation improves patients’ experiences and satisfaction with care.26-29 While navigation may be provided by nurses, social workers, or lay patient navigators (LPNs), current data do not support one model over another. However, cost consideration may make LPNs more feasible in resource constrained settings. Lay patient navigation in safety-net settings provides patients with psychosocial, emotional, and information support to improve their care experience.30,31 BCS often describe being abandoned by health care systems once active treatment ends. 17 Written materials, including well-designed SCPs, can be supplemented with patient navigation to enhance communication about treatment, symptom management which will provide a transition that is currently missing in public hospital patients’ experiences of survivorship care.
We hypothesized that integrating the SCP within linguistically and culturally concordant lay patient navigation would improve HRQOL for breast cancer survivors compared to receiving an SCP as part of usual care. The goal of this mixed methods study was to develop and evaluate the efficacy of an intervention utilizing a culturally and linguistically suitable SCP with or without patient navigation in safety-net BCS. We chose patient navigation as an intervention due to the robust literature supporting its use in the cancer care continuum for medically underserved patients.26,32,33 Prior studies have documented many gaps in the use of SCPs in real-world clinical settings, 34 and thus we included implementation outcomes as part of our study. Implementation beyond efficacy is critical to understand if and how to move interventions from the research setting into practice. 35
Methods
Study design and procedures
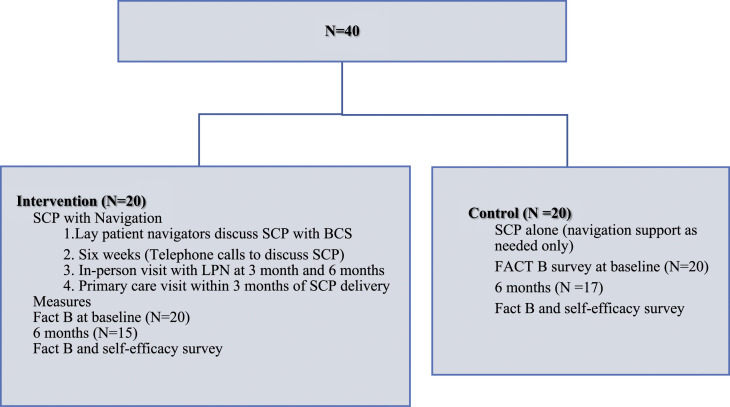
This mixed methods randomized study was conducted between January and December 2018 with BCS recruited from a multidisciplinary clinic for breast cancer patients and BCS in a public hospital in California providing care for low-income residents. The institutional review board (IRB) approved the study (IRB # 16-20607). We randomized 40 participants to receive survivorship care planning with or without navigation (Figure 1). All participants signed written informed consent. All participating BCS completed a demographic survey and baseline measures on enrollment (see details in measures section). In the intervention arm (see details in intervention), LPNs discussed the SCP and survivorship issues and encouraged BCS to discuss healthcare issues with oncology providers and primary care providers (PCP) at the time of SCP delivery, at six weeks by phone, and in-person at three months and six months. LPNs also accompanied women in the intervention arm to their first primary care appointment with the PCP for a coordinating visit within three months of SCP delivery. BCS in the control arm received standard care, which includes navigation support only on as needed basis.
Figure 1.
Schema.
Study Setting
This was a single-site study conducted at the multidisciplinary breast cancer clinic in a publicly funded, safety-net integrated health network. The majority of the patients in the network have public health insurance or are uninsured. The barriers to care include low health literacy, LEP, housing and food insecurity, immigration status, socio-economic barriers, substance use disorders, and mental health concerns. Approximately 40% of patients speak English, 30% speak Cantonese, and 20-25% speak Spanish. A team of five LPNs are employed by the network and support the clinic; two LPNs are bilingual Spanish/English, and two LPNs are bilingual Cantonese/English. LPNs are college graduates but do not have a healthcare background and receive training once they join the program as LPNs. All new patients are matched by language concordance to LPNs who speak one of these languages. LPNs provide active case management during the active cancer treatment phase, including interpretation services during clinic visits as needed, and they perform a comprehensive needs assessment individually for each new patient. 30 LPNs help breast cancer patients with appointment adherence by providing appointment reminders and assistance with transport. They also assist with filling out important forms, applying for health insurance and disability, and providing information about resources in the community. During the survivorship phase following the completion of active treatment, LPNs are available only on an as-needed basis and do not provide specific services related to SCPs or in delivery of BCS care.
Intervention
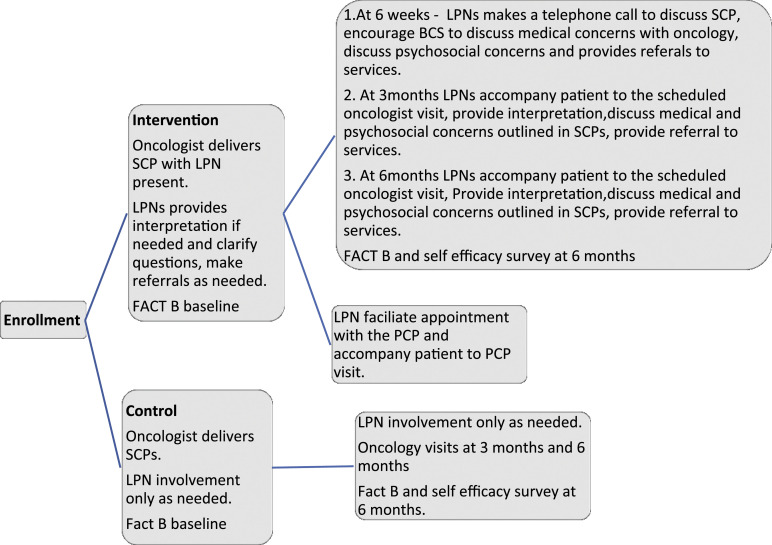
Building upon the current literature, we created a process for survivorship care delivery appropriate for the safety-net setting. We adapted the American Clinical Society of Oncology (ASCO) SCP template 13 for low literacy, simplifying the layout and translating it into Spanish and Chinese (see Appendix). We have previously described the development of the Spanish language SCP. 36 The simplified Chinese language SCP was adapted with the help of a multidisciplinary team including an oncologist, physician assistant, a bilingual (Cantonese/English) oncology nurse, a trilingual (Cantonese/Mandarin/English) social worker, and two bilingual (Cantonese/English) patient navigators and was back translated. 37 We randomized 40 BCS to receive SCPs with or without patient navigation to enhance the understanding and use of the SCP. The intervention consisted of active follow-up in the intervention arm by patient navigators after SCP delivery at six weeks by phone and in person at three months and six months. LPNs also made an appointment for a PCP visit with the BCS and accompanied the patient for a warm hand-off.
LPNs received two hours of training specific to survivorship care, their role in survivorship care, and participated in monthly research meetings. Their role with SCP delivery is outlined in Figure 2.
Figure 2.
Domains that affect the adoption of survivorship care planning.
Eligibility and recruitment
Eligibility criteria consisted of BCS with a histroy of breast cancer stage 1–3 treated with curative intent; English, Spanish, or Cantonese-speaking; and within 1–5 years of having completed active treatment for breast cancer, including surgery, radiation, and chemotherapy. We permitted the inclusion of BCS receiving ongoing endocrine therapy. Exclusion criteria included recurrent or metastatic breast cancer or history of second cancer other than non-melanoma skin cancer. BCS were invited to participate and signed informed consent and were randomized with a study ID envelope containing information about the assigned study arm. Participants were paid $25 gift cards upon enrollment and at the end of the study.
Measures
The study’s primary endpoint was the difference in the HRQOL at six months between intervention and usual care as has been used in prior studies of cancer survivorship.38-41 We measured HRQOL with a widely used, validated instrument, the Functional Assessment of Cancer Therapy—a general scale (FACT-G) together with the breast cancer subscale (FACT-B), to assess survivorship care planning.42,43 The study team administered the FACT-B questionnaire at the time of enrollment and six months. A higher score indicates a better quality of life. As in prior studies of breast cancer survivorship,44-46 we pre-specified self-efficacy as a secondary endpoint. We used an 8-item self-efficacy scale derived from prior studies for managing cancer care.29,36 A higher score indicates higher confidence. An example question is “How confident are you that you will be able to take care of your health over the next year?” with response options of “not at all confident, somewhat confident, very confident, completely confident, or don’t know.” In addition, we assessed knowledge of breast cancer, for example, we asked, “What stage was your breast cancer when it was first diagnosed?”
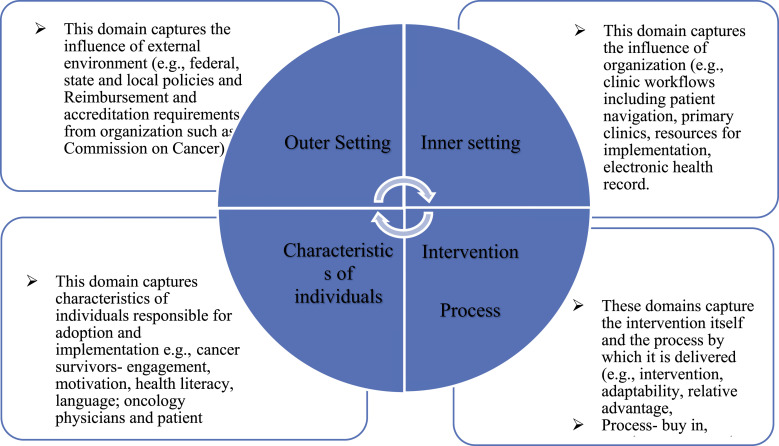
Implementation
We recognized the literature on SCPs to date has not shown benefit in patient-related outcomes and therefore chose implementation as one of our secondary endpoints. 2 We wanted to understand how implementation of SCP delivery is affected by various factors, including stakeholders, in the implementation setting. To assess the implementation of the intervention, we used a theoretical framework, the Consolidated Framework for Implementation Research (CFIR), which comprises a set of domains to understand the implementation of programs/intervention across different contexts and settings. 47 The five overarching domains of CFIR examine the implementation process, individuals involved, the inner setting, defined as the specific environment in when the intervention occurs, and the outer setting, or external structural factors, including policy and payment models, that affect the implementation of an intervention. We hypothesized that understanding the implementation context will allow us a deeper understanding of SCP delivery in a safety-net setting, including its implementation, and contextualize the outcomes of the quantitative measures of the intervention. We sampled three stakeholder groups involved in the cancer survivorship to reflect the needs and perspectives of stakeholders on adoption and implementation. We performed semi-structured debriefing interviews with 15 BCS and asked about their perception of SCPs, their perceived usefulness and about their survivorship care needs. Five BCS from each language group in the intervention arm—English, Spanish, and Cantonese—were invited. Interviews were audiotaped, translated to English from Spanish and Cantonese verbally, and then transcribed. Participants received a $25 gift card for each interview to compensate for their time. In addition, we conducted focus groups for LPNs and oncologists. Five LPNs were invited to participate in a focus group (all agreed). Four oncology providers were invited and three participated in a focus group. LPNs and oncologists were given $50 each in appreciation of their time. We used a template analysis approach to code and organize data for analysis. We used deductive qualitative analysis, in which we defined themes a priori based on CFIR. 48 We identified 15 study specific contextual factors that best described the data. We grouped these into categories based on five major domains of CFIR framework that may influence successful implementation, including uptake, effectiveness, and sustained use of SCPs. The focus group and interviews were independently coded by two coders and mapped to the most relevant CFIR domains. We discussed and resolved any disagreement between the coders. Finally, we analyzed the themes across the five major CFIR domains to consolidate into three overarching themes that best represented the data.
Data Management and Analysis
Data were stored in a HIPAA compliant REDCap database. 49 We used SAS 9.4 software for quantitative analysis and generated descriptive statistics for demographics. For HRQOL assessment, the mean total HRQOL score was compared in each arm using a non-parametric Wilcoxon–Mann–Whitney test. We compared the mean self-efficacy score between the two study arms with the independent Student T-test. We transcribed the qualitative data verbatim and analyzed it for themes, and two coders separately coded the data. We transcribed the audio recordings of interviews done in English, and bilingual research personnel translated and transcribed audio recordings in Spanish and Cantonese. The focus groups for LPNs and oncologists were audiotaped and transcribed. We used Dedoose web-based software to facilitate qualitative data analysis.
Results
Demographic characteristics
We enrolled a total of 40 participants, 20 in each arm. There were ten English speaking, five monolingual Spanish and five monolingual Cantonese speaking BCS in each arm. Our sample was racially diverse with 22.5% white, 41% Asian, and 10% African American. Twenty-five percent of women reported Hispanic ethnicity. Most participants reported public health insurance (Medicare or Medicaid) (82%), with 50% of women only on Medicaid (Table 1). One hundered percent of BCS underwent surgery, with 35% receiving chemotherapy and 87% receiving endocrine therapy. Women who received chemotherapy, radiation, and hormone therapy were equally distributed in each arm. At the time of final data collection, five patients were unavailable in the intervention arm, one due to disease progression, two due to insurance changes, and two were not reachable by phone within the specified time frame. In the control arm, three were unavailable due to the inability to reach them within the specified time frame.
Table 1.
Demographics.
| Demographics | N (%) 40 (100) |
| Race | |
| White | 9 (22.5) |
| Asian | 16 (41) |
| Black/AA | 4 (10) |
| Native Hawaiian | 1 (2.5) |
| Not reported/missing | 2 (5) |
| Other | 7 (17.5) |
| Ethnicity | |
| Hispanic | 10 (25) |
| Non-Hispanic | 26 (66.7) |
| Education | |
| 6 years or less | 4 (10) |
| 6–11 years | 9 (22.5) |
| 12 years or more | 26 (64) |
| Occupation | |
| Full-time | 12 (30) |
| Homemaker/caregiver | 12 (30) |
| Retired | 7 (17) |
| English proficiency | |
| Poor/not at all | 16 (40) |
| Fairly well/well | 12 (30) |
| Very well | 10 (25) |
| Marital status | |
| Married/partner | 12 (30) |
| Country of birth | |
| USA | 10 (25) |
| Other | 29 (72.5) |
| Medical insurance | |
| Medicaid | 21 (52) |
| Medicare | 4 (10) |
| Medicaid/medicare | 8 (20) |
| Treatment received | |
| Surgery | 40 (100) |
| Chemotherapy | 11 (35) |
| Endocrine therapy | 35 (87) |
Quality of life and self-efficacy measures
The FACT-B scores improved over six months in both groups. The change from baseline in HRQOL score at six months was numerically higher in the intervention group than the control group, although the difference was not statistically significant. Numerically higher scores were noted in the intervention group for social/family well-being, emotional well-being, functional well-being, and breast cancer subscale, but they were not statistically significant (see Table 2). The self-efficacy score, which was measured at six months, showed no difference between the two arms (P value .3). Twenty four (75%) of BCS remembered receiving SCPs, equal in both arms, and 14 (44%) BCS said they read and reviewed the SCP. Eleven (31%) reported sharing the SCP with their primary care doctors, Ten (30%) shared it with friends and family members. While most BCS did not recall the name of endocrine therapy, 96% could correctly identify the duration of the endocrine treatment of five years.
Table 2.
Functional Assessment of Chemotherapy- Breast (FACT-B) scores.
| FACT-B domains change in score from baseline | Control | Intervention | P value/Z Score |
|---|---|---|---|
| Physical well-being | 18(10-25) | 16(9-24) | .84/−.19 |
| Social/family well-being | 13 (8-22) | 20 (9-25) | .55/.6 |
| Emotional well-being | 12(8-22) | 19 (10-26) | .27/1.1 |
| Functional well-being | 16 (8-22) | 20 (12-29) | .22/1.23 |
| Breast cancer subscale | 16 (9-20) | 25(6-27) | .44/.78 |
Implementation evaluation
Contextual factors identified for SCP delivery are grouped below within the five major CFIR domains (Table 3).
Table 3.
Contextual factors for survivorship care planning.
| CFIR domains | Contextual factors | Exemplar quotes |
| Outer settings | Accreditation requirements | "We are a COC-accredited organization, COC recognizes how many patients were treated and completed their active treatment with a curative intent in the hospital. So they actually have a list of patients that you have to cover 50 percent of those patients." (ONC#1) |
| Reimbursement | "Because right now there is no way— no ICD-10 code or there's no billing mechanism to bill for a survivorship care visit as such." (ONC#2) | |
| Inner setting | Clinic workflow | "for providers, it wasn't a priority for them, because their priority was to check up on people who were more on active treatment. Like they were more prioritizing their time for people doing chemo." (LPN#2) |
| "a dedicated time that's just dedicated, an appointment or clinic, to survivorship so that they would come back to a special clinic that addresses that rather than trying to do it in an interdisciplinary clinic that's addressing surgical and oncology things." (LPN#1) | ||
| Electronic medical records | "sometimes it got uploaded in EMR under documents, or sometimes it got uploaded under labs." (ONC#2) | |
| “I only went on one visit and I know I emailed the provider but she didn't know where it was. Like, she knew it existed, but she didn't know where it was." (LPN#4) | ||
| Lack of time | "For me, actually, I don't think I did a great job explaining it. I think I filled it out and I told them what it was. I never went through it in great detail. I don't think I went over the last page with all the different lifestyle things.” (ONC#1) | |
| "They were frustrated because it is time-consuming and it wasn't quite their—on their agenda, right." (LPN#3) | ||
| "Or making a brand-new PCP appointment just to go over the survivorship care plan wasn't good use of the PCP's time or the patient's time or the navigator's time." (LPN#4) | ||
| Primary care clinic appointments | "Getting to a PCP visit if it's not in the hospital is a challenge. Getting an appointment is a challenge" (LPN#2). | |
| Embedded LPN | "We have patient navigators also who refer patients to different programs that they need to be referred to. And so, there is a system to provide survivorship care that was happening even before the survivorship care planning was introduced.” (ONC#1) | |
| Integrated survivorship resources | "I think in general; our patients don't ask for too many things. But we do have certain things built up in our own clinic. So we—for example, we have a lymphedema program so patients are evaluated by a person who educates patients about lymphedema and also refers patients who need to see physical therapy, for example." (ONC#2) | |
| Participants’ characteristics | Symptom related needs of BCS | “I have a lot going on, and I don't like to keep taking pain killers constantly because, you know, _____ can affect your stomach and stuff and, you know, I don't like – so I have the creams and patches I do put on to ease the pain, the cream _____ help.” (EBCS#3) |
| "It's like we automatically had that because we have that connection, we felt obligated, and sort of we wanted to give a full picture for the patient to see, 'This is important.'" (LPN #2) | ||
| Need for dedicated resources for diverse BCS | "—To me, the most helpful part was to go to _____ support group. I mean my friends are all cancer survivors. Due to the fact that a lot of people out there discriminate us who have cancer.” (CBCS#1) | |
| "Yeah, and I think the only other thing I would add to that is the educational resources. I think they are available sometimes in English and Spanish. Like for example, we—if patients want to know more about, for example, insomnia or something, and then most of the resources are only available in English. They're at a higher literacy level. And some of them might be available. Some places may have it in Spanish but finding it in Chinese is even harder." (ONC#2) | ||
| BCS engagement | "So, some patients are very involved in their care and some patients are not, and it's not dependent on what language they speak or other things. It really depends on individual patients. For example, one of my patients I think after maybe one or two years after I gave her the survivorship care plan actually brought a copy this week and wanted me to go over it again." (ONC#1) | |
| "It was a mix—for the clients who I helped with I had a mix of Chinese—Cantonese-speaking clients and some English-speaking clients. Some of them were sort of grateful to have something documented from the hospital to give to them, but there were some people who, when I went to the primary care, they didn't really prioritize that as a discussion with their primary care. It was just another paper—I have it, but I don't really think I'm gonna bring it, but you could bring it for me if you want as a navigator." (LPN#2) | ||
| Implementation Process | Buy-in | "But I think buy-in from the providers was very hit or miss. It was very hit or miss." (LPN#4) |
| Lack of planning and ongoing support | "To get an extra visit, it would make other patients not be able to get in because they were—and they need—that would just be a nightmare, I think, on the scheduling." (ONC#3) | |
| Intervention characteristics | SCP as an imperfect tool | "The most helpful, I guess the initial information. When was your surgery, what was going on so you have like this whole this was going on if I would tell somebody else or a different doctor? You also have it on paper so it's not like oh, I had this and this or you can make anything up in the end. But you have like a piece of paper where it's all like here, yes, I have that treatment?" (EBCS#1) |
| "I think if you look at it like a patient gets admitted, they get a discharge summary, and you really want two different things for the patient and provider. You know, your patient wants to know what—they should take these antibiotics for six days and then if there's any problem, they should go to the doctor, while doctor should hear about, you know, this _____ gave this patient antibiotics for six days and if he's still symptomatic when they come and see you, then maybe you wanna consider something else.” (ONC#1) | ||
| Evidence of usefulness for SCP | "So, when we started implementing the survivorship care plan, we were aware of some of the data that had been published before that because we did some reading before implementation. And one of the things was that maybe it was not as helpful to the patient, and probably also as a communication tool with the providers." (ONC #2) |
Abbreviations: ONC, oncologist; CBCS, cantonese speaking BCS; EBCS, english speaking BCS; LPN, lay patient navigator.
Outer setting
Outer setting domains of the CFIR refer to the external environment, which includes federal, state, and local health policy and regulatory requirements for an accrediting organization.
Regulatory requirements: As the safety-net institution is credentialled by the Commission on Cancer (COC) and needed to implement SCPs as an accreditation standard, oncologists identified this regulatory requirement as an impetus for implementation of SCPs underscoring the role of accreditation standards in implementation of interventions.
“We are a COC-accredited organization, COC recognizes how many patients were treated and completed their active treatment with a curative intent in the hospital. So they actually have a list of patients that you have to cover 50% of those patients.” (ONC#1)
Oncologists identified a lack of reimbursement policy and lack of coding and measures to capture the effort required to implement SCPs. Substantial effort and time needed for survivorship care planning and delivery is not captured in the current billing, and this may lead to their efforts not being recognized at the administrative level, for example,
“Because right now there is no way—no ICD 10 code or there’s no billing mechanism to bill for a survivorship care visit as such.” (ONC#2)
Inner Setting
The inner setting domain of CFIR refers to the local environment. The contextual factors identified in this domain included clinic workflow, electronic medical records (EMR), lack of time, primary care clinic appointments, embedded navigation program with LPN invested in survivorship, and knowledge about survivorship resources and integrated survivorship care resources.
Clinical workflow
LPN focus group participants identified clinic workflow as a significant barrier. In the multidisciplinary clinic, patients who are receiving active cancer treatments including chemotherapy are seen simultaneously as cancer survivors. Oncologists deprioritized survivorship care and were more focused on patients receiving active treatment. The LPNs in focus groups captured this tension
“For providers it wasn’t a priority for them, because their priority was to check up on people who were more on active treatment. Like they were more prioritizing their time for people doing chemo.” (LPN#2)
LPNs themselves also noted the difficulty of focusing on SCP in a busy clinic and expressed that providing effective survivorship care will require dedicated clinical time, dedicated personnel, and dedicated resources.
“A dedicated time that’s just dedicated, an appointment or clinic, to survivorship so that they would come back to a special clinic that addresses that rather than trying to do it in an interdisciplinary clinic that’s addressing surgical and oncology things.” (LPN#1)
Electronic Medical Records (EMR)
Both LPNs and oncology providers in focus groups identified the EMR as a significant barrier to SCP delivery and communication between Oncology and PCPs. The SCPs were not integrated into the EMR and needed to be scanned and uploaded, requiring additional time and designation of a consistent place in the EMR. It was often inconsistently labeled, making it difficult to access when needed.
“Sometimes it got uploaded in EMR under documents, or sometimes it got uploaded under labs.” (ONC#2)
The paper SCPs also required an additional step of scanning into the EMR, which was an additional step for clinic staff. The inconsistent scanning resulted in SCPs not always being accessible when needed in the EMR, which may have limited its use after delivery. LPNs expressed this challenge in primary care visits where patients did not bring their SCPs, and PCPs could not always locate it for discussion.
“I only went on one visit and I know I emailed the provider but she didn’t know where it was. Like, she knew it existed, but she didn’t know where it was.” (LPN#4)
Lack of time
Oncologists delivered SCPs inconsistently and were not always able to spend the time needed to discuss it fully and were dissatisfied with the process:
“For me, actually, I don’t think I did a great job explaining it. I think I filled it out and I told them what it was. I never went through it in great detail. I don’t think I went over the last page with all the different lifestyle things.” (ONC#1)
LPNs also noted that it might not have been a priority for the oncologist to create and deliver a SCP due to time constraints.
“They were frustrated because it is time-consuming and it wasn’t quite their—on their agenda, right.” (LPN#3)
Some LPNs also did not see the delivery of SCPs as a good use of their own time, and some did not spend enough time delivering the intervention. LPNs also felt that it was not a good use of PCP time to specifically make an appointment in a busy system for a coordinating visit. One LPN stated:
“Or making a brand-new PCP appointment just to go over the survivorship care plan wasn’t good use of the PCP’s time or the patient’s time or the navigator’s time.” (LPN#4)
Primary care visit
The biggest challenge for the LPNs for the transition of care was the primary care appointment. In a busy safety-net healthcare system, primary care clinics may not have available appointments for a coordinating visit for BCS. In addition, it was even harder for PCP clinics located off-campus visits.
“Getting to a PCP visit if it’s not in the hospital is a challenge. Getting an appointment is a challenge.” (LPN#2)
Integrated LPN
LPNs who were already integrated in the clinic were invested in the SCPs as they felt connected to cancer survivors and wanted them to be more knowledgeable about survivorship care and help the BCS manage their health. Oncologists also identified LPNs as vital for the delivery of survivorship care in the setting where they perform case management and provide essential services, including applying for insurance and referral to community-based resources which are not necessarily labeled survivorship care.
“We have patient navigators also who refer patients to different programs that they need to be referred to. And so, there is a system to provide survivorship care that was happening even before the survivorship care planning was introduced.” (ONC#1)
Integrated survivorship resources
Oncologists identified that there were additional resources that are available for cancer survivors and well-integrated within the clinic. While these are crucial to cancer survivors, they would not be captured as survivorship care if the only measure of survivorship care is SCP delivery. For example, the multidisciplinary clinic also included prospective lymphedema prevention and treatment, including a health educator and physical therapist who provide education for lymphedema prevention and referral and treatment for lymphedema but also a referral for patients who needed additional physical therapy:
“I think in general; our patients don’t ask for too many things. But we do have certain things built up in our own clinic. So we—for example, we have a lymphedema program so patients are evaluated by a person who educates patients about lymphedema and also refers patients who need to see physical therapy, for example.” (ONC#2)
Participants’ characteristics
Several excerpts from all stakeholders recognized the needs of cancer survivors including symptomatic needs and information needs. The engagement of the BCS with SCPs was variable. With a diverse BCS population, the availability of resources in languages other than English was noted to be beneficial.
Symptoms related needs for BCS
BCS had ongoing symptomatic needs despite having completed their active treatment. The survivorship care needs are driven by the ongoing symptom burden. For example, an English speaking BCS (EBCS) reported her ongoing symptom burden.
“I have a lot going on, and I don’t like to keep taking pain killers constantly because, you know, _____ can affect your stomach and stuff and, you know, I don’t like—so I have the creams and patches I do put on to ease the pain, the cream _____ help.” (EBCS#3)
LPNs and oncologists also recognized the needs of BCS and acknowledged the reluctance of their BCS to seek additional support and the importance of being proactive as health care providers in offering the support. Recognition of this unmet need by stakeholders was an essential facilitator to survivorship care planning. The LPNs provide a significant amount of support to BCS and considered survivorship care to be of enormous significance to BCS and prioritized survivorship care and SCPs.
“It’s like we automatically had that because we have that connection, we felt obligated, and sort of we wanted to give a full picture for the patient to see, ‘This is important.’” (LPN #2)
Need for dedicated resources for diverse BCS
BCS expressed the desire for additional support and highlighted the importance of the help they received in cancer support groups, especially those available in different languages. A Cantonese-speaking BCS (CBCS) stated about a support group dedicated to Chinese monolingual BCS:
“—To me, the most helpful part was to go to _____ support group. I mean my friends are all cancer survivors. Due to the fact that a lot of people out there discriminate us who have cancer.” (CBCS#1)
Oncologists also identified a greater need for resources for BCS with limited health literacy and LEP.
“Yeah, and I think the only other thing I would add to that is the educational resources. I think they are available sometimes in English and Spanish. Like for example, we—if patients want to know more about, for example, insomnia or something, and then most of the resources are only available in English. They’re at a higher literacy level. And some of them might be available. Some places may have it in Spanish but finding it in Chinese is even harder.” (ONC#2)
Engagement of BCS
The engagement with SCPs was variable among BCS, and some were more engaged with the SCP delivery, and some were less so. While some BCS brought up questions about their SCPs, but it was not common for them to discuss their SCPs. An oncologist stated:
“So some patients are very involved in their care and some patients are not, and it’s not dependent on what language they speak or other things. It really depends on individual patients. For example, one of my patients I think after maybe one or two years after I gave her the survivorship care plan actually brought a copy this week and wanted me to go over it again.” (ONC#1)
Navigators also noticed this:
“It was a mix—for the clients who I helped with I had a mix of Chinese—Cantonese-speaking clients and some English-speaking clients. Some of them were sort of grateful to have something documented from the hospital to give to them, but there were some people who, when I went to the primary care, they didn’t really prioritize that as a discussion with their primary care. It was just another paper—I have it, but I don’t really think I’m gonna bring it, but you could bring it for me if you want as a navigator.” (LPN#2)
Implementation process
The CFIR domain of implementation process addresses factors such as buy-in, planning, and ongoing support. Several excerpts identified a lack of buy-in from oncologists and LPNs as a barrier.
Most importantly, LPNs noted that buy-in from the oncologist was not consistent, leading to inconsistent delivery of SCP. While some oncology providers were more invested in survivorship care and SCP, others did not share the same priorities. LPN specifically identified this in the focus group:
“But I think buy-in from the providers was very hit or miss. It was very hit or miss.” (LPN#4)
A busy interdisciplinary clinic with limited planning and lack of ongoing support made it hard to identify BCS that needed the SCPs in advance and create a 60-min time slot, allowing enough time to discuss the SCP and led to inconsistent SCP delivery.
“To get an extra visit, it would make other patients not be able to get in because they were—and they need—that would just be a nightmare, I think, on the scheduling.” (ONC#3)
Intervention characteristics
We identified intervention characteristics as essential factors. For example, although the lack of individualization and perceived lack of benefits of intervention were barriers, BCS identified information about their cancer care as the most crucial aspect of SCPs, allowing them to hold on to information and share it with their families and other providers and highlighted this need for critical information from the BCS perspective.
“The most helpful, I guess the initial information. When was your surgery, what was going on so you have like this whole this was going on if I would tell somebody else or a different doctor? You also have it on paper so it’s not like oh, I had this and this or you can make anything up in the end. But you have like a piece of paper where it’s all like here, yes, I have that treatment?” (EBCS#1)
Oncologists identified SCPs as an imperfect tool and not tailored for either PCPs or the BCS. Oncologists in the focus group disagreed with a single SCP for both PCPs and BCS and believed that the current form was not very helpful to either patients or the PCPs and suggested a separate communication tailored to different audiences. As an oncologist noted,
“I think if you look at it like a patient gets admitted, they get a discharge summary, and you really want two different things for the patient and provider. You know, your patient wants to know what—they should take these antibiotics for six days and then if there’s any problem, they should go to the doctor, while doctor should hear about, you know, this _____ gave this patient antibiotics for six days and if he’s still symptomatic when they come and see you, then maybe you wanna consider something else.” (ONC#1)
Oncologists remained skeptical about the value of SCPs based on the current data and questioned the usefulness of implementing SCPs in limited-resource settings. Oncologists mentioned the literature that has shown that SCPs may not be helpful, especially in safety-net settings:
“So, when we started implementing the survivorship care plan, we were aware of some of the data that had been published before that because we did some reading before implementation. And one of the things was that maybe it was not as helpful to the patient, and probably also as a communication tool with the providers.” (ONC #2)
Synthesizing across CFIR domains, we identified three overarching themes.
1. Survivorship care interventions need to consider survivors' needs and preferences.
The data highlighted the importance of tailoring survivorship care and SCPs to match the needs of cancer survivors. Overall, there is a significant paucity of survivorship care resources and SCPs tailored to a diverse BCS. This data underscores a lack of investment in culturally and linguistically tailored resources to support and educate BCS about managing their symptoms and to fulfill their information needs. Stakeholders also identified several limitations to SCPs. BCS wanted to have information about their treatment, but not all of them would have attached importance to the SCPs themselves, thus limiting their use in overall survivorship care. Finally, all stakeholders described several aspects of survivorship care, for example, support groups tailored by language and embedded lymphedema care that were helpful to BCS, highlighting important implications for designing survivorship care programs beyond the delivery of SCPs, and emphasized existing resources within and outside the organization in the broader community as essential components of survivorship care.
2. Need for dedicated survivorship resources.
We also identified that focusing on survivorship care in a setting where clinical workflows are designed for patients receiving active cancer treatment may lead to ineffective survivorship care. All stakeholders identified this conflict and highlighted that SCP delivery in this setting was suboptimal. While survivorship interventions such as active symptomatic needs, proactive management of lymphedema, assistance for insurance, and referral to community resources need to be addressed simultaneously with active cancer treatment. There is a need for dedicated personnel and resources to provide SCPs, and survivorship care education in clinical settings focused on survivorship care. While this will require investments in additional resources and personnel, it is more likely to meet the needs of cancer survivors.
3. The EMR is an essential component of survivorship care.
Our existing EMR was a significant barrier overall to survivorship care planning. Lack of SCPs and treatment summaries tailored to diverse populations available in languages other than English necessitated the use of paper SCPs in our study. This limitation led to paper SCPs that needed to be scanned into the EMR and were challenging to find. EMR functionality with the ability to populate details regarding diagnosis and treatments into an SCP or treatment summary may increase uptake by the providers. We found that the lack of a templated SCP that can be frequently updated as necessary is also likely to result in ineffective SCP delivery. In addition, we also found that coordinating visits with PCPs was not a good use of time by our stakeholders. EMR can play an essential role in improving this coordination by providing an avenue for two-way communication between PCPs and oncologists.
Discussion
This mixed methods study sought to understand the role of patient navigation in SCP delivery in a safety-net population. The intervention of SCPs with patient navigation was intended to provide support to BCS and coordinate care between primary care and oncology by linking the BCS back into primary care with the help of LPNs.
Our primary goal was to assess the impact on HRQOL of BCS when supported by patient navigation on the FACT-B scale. While we found numerically higher HRQOL in the intervention arm, it was not statistically significant. Although patient navigation based intervention have shown improvement in some domains of HRQOL, 50 several prior studies results with SCP intervention have shown no improvement 2 or have shown even worsening of HRQOL. 51 We also assessed self-efficacy and found that self-efficacy was also not different in either of the arms, this is consistent with prior literature which has shown mixed results in self-efficacy with SCP.2,44,52 Finally, we sought to understand the implementation of SCP related intervention in safety-net setting. Prior research has also emphasized that SCP may not be of benefit to cancer survivors2,53 and suggests that implementation challenges may be inherent in these outcomes. 54
The intervention was implemented in a climate where BCS have a significant need for knowledge and support and amidst the calls for SCP implementation from accrediting organizations.8,17,18 However, implementation of SCPs remains an unfunded mandate with significant time and resource commitment 55 without any financial or billing support for implementing SCPs. 55 Thus, the implementation of SCPs can be a significant burden in a resource-limited healthcare system. Given limited resources, we chose to implement SCP delivery in a regular clinic workflow. We found that although it may be more convenient to include SCP delivery in the same clinic where routine cancer care is delivered, it is challenging to deliver SCPs due to competing priorities of stakeholders. Our findings suggest that successful delivery of SCPs in this setting requires institutional support and focus on survivorship care. A dedicated survivorship care clinic with designated space, personnel, and resources prioritizing survivorship care may be more impactful for the care of BCS. Our experience suggests that SCP delivery may meet the requirements set by the accrediting organizations, it is unlikely to meet the needs of BCS.
Oncologists in our clinical settings remained skeptical of the value of SCPs in survivorship care, and this may have resulted in inconsistent SCP delivery. Currently, SCPs are considered a tool for education for cancer survivors but also a tool for communication with PCPs.56,57 However, their efficacy in care coordination remains unclear, and to address this, oncologists in our focus group emphasized that content should be different for patients and PCPs. One of the major limitation of SCPs we identified, is lack of individualization and ability to modify as needed, during the cancer trajectory. Prior research has also identified that SCPs may not contain all the Institute of Medicine recommended components, are at high reading level and not tailored to diverse cancer survivors.12,58 Although the EMR may assist with SCP delivery, 59 we found that if not well designed, it may also be a significant barrier for SCP implementation and create an undue burden on health care personnel. Due to limited functionality for SCPs in our EMR, we had to implement paper-based SCPs, which was necessary for our linguistically diverse patients, but these were hard to integrate with the EMR and could not be easily personalized or updated. These barriers may be addressed by patient-centered SCPs embedded in EMR, with availability in multiple languages, and at appropriate reading levels to address the needs of diverse cancer survivors.
There was variable buy-in from oncology providers, and a lack of consistent process between oncologists posed a significant barrier to implementation of the intervention. Thus, planning and optimizing implementation are essential. 55 In addition, while the navigators recognized the importance of survivorship care, they may not have had a similar focus on delivery and follow-up of SCPs. We also found that there may be a significant waiting period for PCP appointments in the safety-net and adding new coordinating appointments may not be the best use of this limited resource. Other innovative care coordination measures leveraging the EMR to coordinate care between PCP and oncologists may be more beneficial.
In addition, survivorship care resources such as cancer support groups and embedded lymphedema education and surveillance and referral to community-based resources were important component of survivorship care in our health care setting. To provide survivorship care and education to cancer survivors, particularly in safety-net settings, new innovative approaches tailored to this population are needed, and patient navigators and health educators can be valuable partners in providing this care. For example, a group medical visit approach often used to promote self-management in chronic disease management may be one such intervention to address the needs of cancer survivors. 60
A significant strength of our study is informed framework driven assessment of the implementation of SCPs in a safety-net setting (Figure 3), identifying factors that influence implementation of SCP delivery beyond the evaluation of SCPs as has been done extensively in prior literature.2,53 We were successful in recruiting and following BCS for 6 months which can often be challenging in safety-net settings. In addition, the mixed methods nature of the study provided important insights into SCP delivery in safety-net settings and contextualized the findings from the quantitative component. The strength of the qualitative data comes from LPNs who delivered the intervention and provided an honest and comprehensive assessment of overall SCP delivery and process and provided a unique opportunity to learn from their perspectives. Our study also has several limitations. As a pilot study, we recruited a small sample of BCS from a single safety-net institution. Thus, generalizability may be limited. However, challenges in the implementation of SCPs are not unique to our institution. 55 In addition, perspectives of PCPs would have provided additional information; however, the limited nature of this study did not allow that.
Figure 3.
Study intervention: abbreviations—Lay Patient navigator (LPN), breast cancer survivors (BCS), Functional Assessment of Cancer therapy with breast cancer subscale (FACT-B).
Finally, our study underscores that care of cancer survivors and effective SCP delivery requires dedicated resources, personnel, space, and time. In addition, innovative care delivery for cancer survivors needs to move beyond SCPs and must leverage innovative coordination strategies to engage all stakeholders including PCPs in survivorship care.
ORCID iD
Niharika Dixit https://orcid.org/0000-0001-6954-2383.
Footnotes
Declaration of conflicting interests: Dr. Dixit is on an advisory board for Bristol Myers Squibb. Other authors do not report any conflicts of interest. All authors had the access to data and vouch for its authenticity.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Centers of Excellence grant from Avon Breast Cancer Crusade. Dr. Sarkar and Dr. Dixit are supported by the National Cancer Institute (R01CA241128). Dr. Sarkar is supported by the National Cancer Institute (K24CA212294).
Ethics Approval: The institutional review board (IRB) at the University of California, San Francisco approved the study
Consent: All participants signed written informed consent.
References
- 1.Society AC. breast-cancer-facts-and-figures-2019-2020 (1). 2020.
- 2.Hill RE, Wakefield CE, Cohn RJ, Fardell JE, Brierley ME, Kothe E, et al. Survivorship Care Plans in Cancer: A Meta-Analysis and Systematic Review of Care Plan Outcomes . Oncol. 2020:25(2):e351-e372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meade CD, Wells KJ, Arevalo M, Calcano ER, Rivera M, Sarmiento Y, et al. Lay navigator model for impacting cancer health disparities . J Canc Educ, 2014. 29(3):449-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gunn C, Battaglia TA, Parker VA, Clark JA, Paskett ED, Calhoun E, et al. What Makes Patient Navigation Most Effective: Defining Useful Tasks and Networks . J Health Care Poor Underserved, 2017. 28(2):663-676. [DOI] [PubMed] [Google Scholar]
- 5.Freeman HP. Patient navigation as a targeted intervention: For patients at high risk for delays in cancer care . Cancer, 2015. 121(22):3930-3932. [DOI] [PubMed] [Google Scholar]
- 6.S.c.g.s.h.c.h.s.c.g.s.h.c.h.U . 2014,
- 7.Luctkar-Flude M, Aiken A, McColl MA, Tranmer J. A comprehensive framework and key guideline recommendations for the provision of evidence-based breast cancer survivorship care within the primary care setting . Fam Pract, 2015. 32(2):129-140. [DOI] [PubMed] [Google Scholar]
- 8.Cancer, Co . 2016. https://www.facs.org/quality-programs/cancer/coc/standards
- 9.Ashing-Giwa KT, Lim J-W. Examining the impact of socioeconomic status and socioecologic stress on physical and mental health quality of life among breast cancer survivors . Oncol Nurs Forum, 2009. 36(1):79-88. [DOI] [PubMed] [Google Scholar]
- 10.Ashing-Giwa KT, Lim J-W. Examining emotional outcomes among a multiethnic cohort of breast cancer survivors . Oncol Nurs Forum, 2011. 38(3):279-288. [DOI] [PubMed] [Google Scholar]
- 11.O'Malley DM, Hudson SV, Ohman-Strickland PA, Bator A, Lee HS, Gundersen DA, et al. Follow-up Care Education and Information: Identifying Cancer Survivors in Need of More Guidance . J Canc Educ. Off J Amer Assoc Cancer Edu, 2016. 31(1):63-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wen K-Y, Hu A, Ma G, Fang C, Daly M. Information and communication needs of Chinese American breast cancer patients: perspectives on survivorship care planning . The Journal of Community and Supportive Oncology, 2014. 12(12):439-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ASCO. American Society of Clinical Oncology . ASCO Cancer Treatment Summaries. 2005. Available from: http://www.cancer.net/survivorship/asco-cancer-treatment-summaries [Google Scholar]
- 14.Burg MA, Lopez ED, Dailey A, Keller ME, Prendergast B. The potential of survivorship care plans in primary care follow-up of minority breast cancer patients . J Gen Intern Med, 2009. 24 Suppl 2 suppl 2:S467-S471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mollica M, Nemeth L. Transition from patient to survivor in African American breast cancer survivors . Canc Nurs, 2015. 38(1):16-22. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez P, Nuñez A, Wang-Letzkus M, Lim J-W, Flores KF, Nápoles AM. Coping with breast cancer: Reflections from Chinese American, Korean American, and Mexican American women . Health Psychol, 2016. 35(1):19-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke NJ, Napoles TM, Banks PJ, Orenstein FS, Luce JA, Joseph G. Survivorship Care Plan Information Needs: Perspectives of Safety-Net Breast Cancer Patients . PloS One, 2016. 11(12):e0168383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Napoles AM, Ortiz C, Santoyo-Olsson J, Stewart A, Lee H, Duron Y, et al. Posttreatment survivorship care needs of Spanish-speaking Latinas with breast cancer . The Journal of Community and Supportive Oncology, 2017. 15(1):20-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freund KM, Battaglia TA, Calhoun E, Dudley DJ, Fiscella K, Paskett E, et al. National Cancer Institute Patient Navigation Research Program . Cancer, 2008. 113(12):3391-3399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patient Navigator Outreach and Chronic Disease Prevention Act of 2005 . SEC. 2. Patient navigator grants. 2005. [Google Scholar]
- 21.Dudley DJ, Drake J, Quinlan J, Holden A, Saegert P, Karnad A, et al. Beneficial effects of a combined navigator/promotora approach for Hispanic women diagnosed with breast abnormalities . Cancer Epidemiol Biomark Prev, 2012. 21(10):1639-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freeman HP. The history, principles, and future of patient navigation: commentary . Semin Oncol Nurs, 2013. 29(2):72-75. [DOI] [PubMed] [Google Scholar]
- 23.Freund KM, Battaglia TA, Calhoun E, Darnell JS, Dudley DJ, Fiscella K, et al. Impact of patient navigation on timely cancer care: the Patient Navigation Research Program . Journal of the National Cancer Institute, 2014. 106(6):dju115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gabriel Chamie CM, Crawford E, Peng J, Petersen M, Schwab D, Schwab J, et al. Community Transmission During Shelter-in-Place in San Francisco . 2020. 10.1101/2020.06.15.20132233 [DOI]
- 25.Freeman HP, The origin, evolution, and principles of patient navigation . Cancer Epidemiol Biomark Prev, 2012. 21(10):1614-1617. [DOI] [PubMed] [Google Scholar]
- 26.Ferrante JM, Chen P-H, Kim S, The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial . J Urban Health, 2008. 85(1):114-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jean-Pierre P, Cheng Y, Wells KJ, Freund KM, Snyder FR, Fiscella K, et al. Satisfaction with cancer care among underserved racial-ethnic minorities and lower-income patients receiving patient navigation . Cancer, 2016. 122(7):1060-1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koh C, Nelson JM, Cook PF, Evaluation of a patient navigation program . Clin J Oncol Nurs, 2011. 15(1):41-48. [DOI] [PubMed] [Google Scholar]
- 29.Campbell C, Craig J, Eggert J, Bailey-Dorton C, Implementing and measuring the impact of patient navigation at a comprehensive community cancer center . Oncol Nurs Forum, 2010. 37(1):61-68. [DOI] [PubMed] [Google Scholar]
- 30.Gabitova G, Burke NJ. Improving healthcare empowerment through breast cancer patient navigation: a mixed methods evaluation in a safety-net setting . BMC Health Serv Res, 2014. 14:407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Biro D, Freeman R, Meade J, Roberts S, Guilford T. Pigeons combine compass and landmark guidance in familiar route navigation . Proc Natl Acad Sci Unit States Am, 2007. 104(18):7471-7476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, et al. Patient navigation: state of the art or is it science? Cancer, 2008. 113(8):1999-2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ko NY, Darnell JS, Calhoun E, Freund KM, Wells KJ, Shapiro CL, et al. Can patient navigation improve receipt of recommended breast cancer care? Evidence from the National Patient Navigation Research Program . J Clin Oncol, 2014. 32(25):2758-2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LaGrandeur W, Armin J, Howe CL, Ali-Akbarian L. Survivorship care plan outcomes for primary care physicians, cancer survivors, and systems: a scoping review . Journal of Cancer Survivorship, 2018. 12(3):334-347. [DOI] [PubMed] [Google Scholar]
- 35.Oh A, Vinson CA, Chambers DA. Future directions for implementation science at the National Cancer Institute: Implementation Science Centers in Cancer Control . Transl Behav Med, 2020. 11:121-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nápoles AM, Santoyo-Olsson J, Chacón L, Stewart AL, Dixit N, Ortiz C. Feasibility of a Mobile Phone App and Telephone Coaching Survivorship Care Planning Program Among Spanish-Speaking Breast Cancer Survivors . JMIR Cancer, 2019. 5(2):e13543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Niharika Dixit PW, McBride R, Hernandez D, Cicerelli B, Survivorship Care Plans in Safety Net: Bridging the Barriers. 2018. [Google Scholar]
- 38.Ahn SH, Park BW, Noh DY, Nam SJ, Lee ES, Lee MK, et al. Health-related quality of life in disease-free survivors of breast cancer with the general population . Ann Oncol, 2007. 18(1):173-182. [DOI] [PubMed] [Google Scholar]
- 39.Ashing-Giwa K, Lam CM, B Xie, Assessing health-related quality of life of Chinese-American breast cancer survivors: a measurement validation study . Psycho Oncol, 2013. 22(3):704-707. [DOI] [PubMed] [Google Scholar]
- 40.Paskett ED, Alfano CM, Davidson MA, Andersen BL, Naughton MJ, Sherman A, et al. Breast cancer survivors' health-related quality of life . Cancer, 2008. 113(11):3222-3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.de Ligt KM, Heins M, Verloop J, Ezendam NPM, Smorenburg CH, Korevaar JC, et al. The impact of health symptoms on health-related quality of life in early stage breast cancer survivors . Breast Canc Res Treat, 2019. 178(3):703-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brennan ME, Butow P, Spillane AJ, Boyle F, Patient-reported quality of life, unmet needs and care coordination outcomes: Moving toward targeted breast cancer survivorship care planning . Asia Pac J Clin Oncol, 2016. 12(2):e323-e331. [DOI] [PubMed] [Google Scholar]
- 43.Hastert TA, McDougall JA, Strayhorn SM, Nair M, Beebe‐Dimmer JL, Schwartz AG, Social needs and health‐related quality of life among African American cancer survivors: Results from the Detroit Research on Cancer Survivors study . Cancer, 2021. 127(3):467-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nápoles AM, Ortíz C, O'Brien H, Sereno AB, Kaplan CP, Coping resources and self-rated health among Latina breast cancer survivors . Oncol Nurs Forum, 2011. 38(5):523-531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Shelby RA, Edmond SN, Wren AA, Keefe FJ, Peppercorn JM, Marcom PK, et al. Self-efficacy for coping with symptoms moderates the relationship between physical symptoms and well-being in breast cancer survivors taking adjuvant endocrine therapy . Support Care Canc, 2014. 22(10):2851-2859. [DOI] [PubMed] [Google Scholar]
- 46.Chen JY, Diamant AL, Thind A, Maly RC, Determinants of breast cancer knowledge among newly diagnosed, low-income, medically underserved women with breast cancer . Cancer, 2008. 112(5):1153-1161. [DOI] [PubMed] [Google Scholar]
- 47.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC, Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science . Implement Sci, 2009. 4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Keith RE, Crosson JC, O’Malley AS, Cromp D, Taylor EF, Using the Consolidated Framework for Implementation Research (CFIR) to produce actionable findings: a rapid-cycle evaluation approach to improving implementation . Implement Sci, 2017. 12(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support . J Biomed Inf, 2009. 42(2):377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ramirez AG, Muñoz E, Long Parma D, Perez A, Santillan A, Quality of life outcomes from a randomized controlled trial of patient navigation in Latina breast cancer survivors . Cancer Medicine, 2020. 9(21):7837-7848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.de Rooij BH, Ezendam NPM, Nicolaije KAH, Lodder P, Vos MC, Pijnenborg JMA, et al. Survivorship care plans have a negative impact on long-term quality of life and anxiety through more threatening illness perceptions in gynecological cancer patients: the ROGY care trial . Qual Life Res, 2018. 27(6):1533-1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kenzik KM, Kvale EA, Rocque GB, Demark‐Wahnefried W, Martin MY, Jackson BE, et al. Treatment Summaries and Follow‐Up Care Instructions for Cancer Survivors: Improving Survivor Self‐Efficacy and Health Care Utilization . Oncol, 2016. 21(7):817-824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brennan ME, Gormally JF, Butow P, Boyle FM, Spillane AJ, Survivorship care plans in cancer: a systematic review of care plan outcomes . Br J Canc, 2014. 111(10):1899-1908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Birken SA, Clary AS, Bernstein S, Bolton J, Tardif-Douglin M, Mayer DK, et al. Strategies for Successful Survivorship Care Plan Implementation: Results From a Qualitative Study . Journal of Oncology Practice, 2018. 14(8):e462-e483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Birken SA, Raskin S, Zhang Y, Lane G, Zizzi A, Pratt-Chapman M, Survivorship Care Plan Implementation in US Cancer Programs: a National Survey of Cancer Care Providers . J Canc Educ, 2019. 34(3):614-622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Earle CC, Failing to plan is planning to fail: improving the quality of care with survivorship care plans . J Clin Oncol, 2006. 24(32):5112-5116. [DOI] [PubMed] [Google Scholar]
- 57.Chaput G, The survivorship care plan: a valuable tool for primary care providers? Curr Oncol, 2018. 25(3):194-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lyson HC, et al. Communicating Critical Information to Cancer Survivors: an Assessment of Survivorship Care Plans in Use in Diverse Healthcare Settings. J Cancer Educ, 2020. 21:121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tevaarwerk AJ, Wisinski KB, Buhr KA, Njiaju UO, Tun M, Donohue S, et al. Leveraging electronic health record systems to create and provide electronic cancer survivorship care plans: a pilot study . Journal of Oncology Practice, 2014. 10(3):e150-e159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Barnett KG. Group Medical Visits: The Future of Healthcare? Global Advances in Health and Medicine, 2015. 4(6):6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]