Abstract
The aim is to assess the commonalities and interdependence referred to body-image avoidance among 118 couples newly introduced to first-level assisted reproductive techniques. Results showed non-clinical functioning levels, and partners showed a correlated, yet low, dyadic adjustment. The couple-effect was modeled through an Actor Partner Interdependence Model. For both partners, dyadic adjustment’s actor-effect associates with body-image avoidance. Moreover, psychological symptoms’ actor-effect associate to body-image avoidance, resulting significantly more influential than the partner-effect. Only for males, alexithymia’s actor-effect was significant. To conclude, partners’ functioning is quite specular yet not interdependent, as they do not show a couple-as-a-unit modality of functioning. Clinical implications are discussed.
Keywords: assisted reproduction techniques, body-image avoidance, dyadic adjustment, attachment, psychological distress, alexithymia, actor partner interdependent model
Introduction
According to the National Institute for Health and Clinical Excellence guideline (NICE; Gurunath et al., 2011), infertility is a condition whereby couples are not able to conceive naturally after 24 months of regular unprotected sexual intercourse, or difficulty to conceive after having already conceived. Infertility prevalence ranges from 9 to 20% worldwide (European Society of Human Reproduction and Embryology, 2014) and is considered inexplicable (idiopathic infertility) in 15–30% of cases. It is often perceived as the most stressful event of a couple’s life, felt like a mourning process (El Kissi et al., 2013) and representing a shared experience where the reaction of one partner could significantly influence the adjustment of the other (Donarelli et al., 2012). Research highlights some differences in men’s and women’s reaction to infertility (De Berardis et al., 2014; Huppelschoten et al., 2013; Glover et al., 1996; Peloquin, 2013), although studies have mainly focused on female’s experiences (Donarelli et al., 2012), most probably because they are those facing the pervasiveness of infertility treatments (Peloquin, 2013).
In this regard, assisted reproductive techniques (ART) are helpful for couples that are trying to solve their infertility problems, thus supporting the fulfillment of their desire for parenthood. ART includes different treatment methods (Istituto Superiore Di Sanità, 2016 [Higher Institute of Health, 2016]): from insemination procedures with ovulation induction (first level) to in-vitro-fertilization procedures (IVF; second level) as well as treatments made with laparoscopy (third level). Stanhiser and Steiner (2019) underlined the necessity to measure psycho-social dimensions relevant to infertility research and practices as ART might significantly influence couples’ well-being, embedding aspects referred to mental equilibrium, self-identity, and personal agency, as well as sexual and marital relationships. The effectiveness of ART is strictly linked to age and so is the time couples actively spend trying for a natural pregnancy, forcing couples, and particularly women, to face the natural limits of their own reproductive system (Wyndham et al., 2012). It is estimated that, on average, just one over four women will get pregnant and successfully give birth following a single ART cycle (Kushnir et al., 2017), meaning that a big majority of couples undergo through multiple ART cycles and abortions, thus leading to a lengthening of timing as well as increased negative experiences. Both infertile men and women experience great psychological distress (Simionescu et al., 2021). Noteworthy, a recent meta-analysis (Purewala et al., 2018) showed that state anxiety and depression scores at baseline and during the ART treatments were associated with treatment outcome in women (Purewala et al., 2018; Simionescu et al., 2021) which associated with reduced chances of ART treatments’ success (Simionescu et al., 2021; Stanhiser and Steiner, 2019). Moreover, it was also reported that, infertile women, tend to experience greater depression and anxiety symptoms and greater psychological consequences overall compared to infertile men, which instead show greater stress symptoms and psychosomatic distress (Simionescu et al., 2021). The greater impact of infertility upon women’s well-being, compared to men, is in line with evidence highlighting how infertility undermines women’s self-esteem and body image referred to feelings of emptiness and loss of maternal identity, further damaging their self-identity as women (De Berardis et al., 2014; El Kissi et al., 2013; Huppelschoten et al., 2013; Ramirez-Ucles et al., 2015). Moreover, among infertile women, body image also associates with marital adjustment as referred to the agreement within the couple, satisfaction with life and the capacity to express emotions (Karamidehkordi and Roudsari, 2014). Instead, infertile man, compared to the fertile ones, show greater body dissatisfaction referred to the perception of reduced physical fitness and health, leading also to a diminished health-oriented attitude, as well as a reduced body satisfaction more generally (Akhondi et al., 2011). Male infertility is perceived as mining body virility and masculinity (Samadaee-Gelehkolaee et al., 2016), as these aspects are perceived in conjunction with males’ reproductive capacities (Peloquin, 2013). As such, men tend to experience unexpressed feelings of shame, anger, guilt, isolation, loss, and personal failure (Reis et al., 2013), which should be taken into account when undergoing ART treatments, as also male depression is reported to associate with reduced probabilities of conceiving and overall pregnancy success (Martínez-Pampliega et al., 2019; Stanhiser and Steiner, 2019). To current knowledge, no study has focused on how body image and dissatisfaction and related psychosocial symptoms among infertile men influences and/or is influenced by couples’ life satisfaction. Yet, a current study reported that, when undergoing ART procedures, the psychological symptoms of both couple’s partners longitudinally associates with the couple’s relationship quality (Martínez-Pampliega et al., 2019).
Couples should be considered as a unit when referring to marital satisfaction, and particularly in the context of infertility (Maroufizadeh, et al., 2019) as marital satisfaction in general is influenced both by ones’ own and the partners’ perceived stress (Randall and Bodenmann, 2009; Maroufizadeh et al., 2019). This seems to be true particularly among women, as studies report that among couples in a situation of infertility, women’s depression symptoms are greatly influenced by men’s marital satisfaction than men are by their wives’ marital satisfaction (Maroufizadeh, et al., 2019). As such, women report both lower quality of life as well as reduced dyadic adjustment as compared to their husbands (Zeren et al., 2019). In this regard, studies have evidenced how higher levels of dyadic adjustment functions as a protective factor for couples involved in natural pregnancies (Martínez-Pampliega et al., 2019) as well as artificial reproductive paths (Newton et al., 1990) as favoring communication, mutual support and cohesion within the couple. On the other hand, critical are the findings whereby marital adjustment is mined by poor body image satisfaction in infertile women, particularly associated with reduced agreement and consent within the couple as well as diminished expression of emotions within the family context (Karamidehkordi and Roudsari, 2014). Still, consideration of both partners concerning their overall well-being and dyadic adjustment would allow a more accurate analysis of couples undergoing ART treatments (Hammarberg et al., 2008; Maroufizadeh et al., 2019), particularly considering the relevance that the body and body-esteem plays in couples lives (Meltzer and McNulty, 2010). The quality of marital life plays an important role when trying to adjust to a situation of infertility (Mahajan et al., 2008). Low dyadic adjustment predicts the development of post-natal depressive and anxious symptoms in both mothers and fathers (Rollè et al., 2017) thereby affecting children’s behavior and engagement during parent–child interactions (Shigeto et al., 2014). Referring specifically to couples undergoing ART, it was reported that couples’ relationship quality is associated with the level of communication between the partners, which was in turn associated with both partners’ levels of psychological symptoms (Martínez-Pampliega et al., 2019). The authors further highlighted that the association between these variables was of greater magnitude among women, thereby suggesting that women perceive greater negative experiences associated to problematic couple communication, compared to men, in the context of the ART journey. As such, the stress resulting from a situation of infertility might lead to a heightened activation of attachment models, with consequences on the couples’ well-being (Moura-Ramos et al., 2017).
Coherent with the just mentioned evidence, women indeed most often show an anxious romantic attachment defined by a strong over-commitment toward the relationship and by anxious-like strategies characterized by worry and negative affectivity influencing their own well-being and that of their partner’s (Donarelli et al., 2012; Moura-Ramos et al., 2017). Men, on the other hand, more frequently show an avoidant romantic attachment (Donarelli et al., 2012; Moura-Ramos et al., 2017) which describes a state of aloofness and disinterest toward the partner and the relation in general (Hepper and Carnelley, 2012), also observed to mediate the association between their own desire for parenthood and their well-being (Moura-Ramos et al., 2017). Still, both anxious and avoidant attachment are associated with heightened stress within the couple (Donarelli et al., 2012), while a secure attachment style would instead play a protective role toward the psychological well-being of both men and women (Amir et al. (1999), as secure romantic attachment associates to a more satisfying and balanced couple-life (Hepper and Carnelley, 2012).
Referring to the ART context specifically, a recent study (Renzi et al., 2020a, 2020b) showed that, among women undergoing ART, higher attachment avoidance predicted poorer ART outcome, explaining that such relation might be given by the negative consideration that avoidant individuals have of others and the related reduced tendency to seek external support. As such, the authors continued hypothesizing that this could then lead to heighten stress hindering ART outcome. In line with this, although both anxious and avoidant attachment are associated with both men and women’s infertility stress, within a dyadic perspective, attachment avoidance in women specifically associated with men’s infertility stress and relationship concerns (Donarelli et al., 2012). This association might be explained by the link between infertile women reduced emotional expression and both body dissatisfaction and reduced sexual desire and interest (Karamidehkordi and Roudsari, 2014). The negative body-experience and sorrow associated to an impossibility to naturally conceive, might lead women to be more emotionally detached that they would otherwise be, as attempt to contain such negative experiences with consequences on the couple’s relationship. In this regard, the alexithymia construct, a personality trait that describes a difficulty in understanding and communicating feelings and emotional states (Sifneos 1973; Taylor and Bagby 2012), might be of relevance, particularly since greater negative affects mediate the association between alexithymia and reduced relationship quality (Lyvers et al., 2021). Yet, alexithymia seems more relevant for males (Conrad et al., 2001; Simionescu et al., 2021), which is in line with the above-mentioned greater avoidant attachment observed among males and defined by aloofness and an emotional detachment from the relationship (Donarelli et al., 2012; Moura-Ramos et al., 2017). Men are more likely to suppress painful and negative emotions, defending themselves from depression and depression-like symptoms (Conrad et al., 2001). On the other hand, alexithymia measured on infertile women undergoing in-vitro treatments was associated with maladaptive coping strategies and psychological stress (Gourounti et al., 2016) further considered as a risk factor for symptoms of anxiety, depression, psychological distress (Juriü Vukeliü et al., 2019), and reduced quality of life (Renzi et al., 2020a, 2020b). Moreover, alexithymia also results as predictive of greater body checking and body dissatisfaction as compared to non-alexithymic women (De Berardis et al., 2007). Still, findings are inconsistent and, to our knowledge, only one study (Ramirez-Ucles et al., 2015) considered both male and female regarding the association between infertility and alexithymia.
In light of the reviewed literature, the aim of the present study is to bridge the gap of previous research by considering the multiple psychological characteristics of couples in a situation of infertility and undergoing first level ART for the first time. The sole consideration of couples newly introduced to the first level of ART has the intent to evaluate couples’ characteristics before they experience other infertility-related medical treatments, thereby before treatments’ pervasiveness increases. This would provide further insight useful to support couples’ well-being throughout the ART cycles and levels by providing information relevant to design psychosocial interventions and prevention practices aimed at supporting and preventing the development of psychosocial difficulties among infertile couples undergoing ART, while increasing the chances for successful ART outcomes (Purweal et al., 2017; Simionescu et al., 2021). Attention will be particularly paid to body image avoidance referred to body image dissatisfaction, gender differences as well as couples’ commonalities and interdependence. More specifically, three macro-areas have been considered: psychological distress, couple adjustment, and romantic attachment. Psychological distress was operationalized in terms of psychiatric symptoms’ level and alexithymic features and body image avoidance. Romantic attachment, instead, refers to two attachment dimensions, namely avoidant and anxious. Moreover, the time spent trying to get pregnant was considered as a possible factor in predicting increased body image avoidance. We have hypothesized that: (1) considering that couples are the very beginning of the ART journey, men and women will not show clinical levels of psychological symptoms and will not be significantly dissimilar in their psychological symptoms and relational features; (2) romantic avoidant and anxious attachment will positively associate with psychological distress and body image dissatisfaction; (3) men will present greater avoidant attachment, while women greater anxious attachment; (4) in the APIM, actor and partner coefficients of the couples’ members will not significantly differ among each other, highlighting partners specular functioning; (5) for both couples’ partners, the actor effect will be more influential than the partner effect since they are at the first level of the ART; (6) body image avoidance will be positively predicted by psychological distress variables (i.e., psychological symptoms and alexithymia) and negatively predicted by a good dyadic adjustment.
Method
Procedure
This study is a part of an ongoing transversal and longitudinal project, started in 2012, investigating the well-being of couples undergoing ART. The project complies with the Declaration of Helsinki (Italian law 196/2003), with the ethical standards for research of the University of Padua (num. 1214/2012) and with those outlined in the APA Ethical Principles of Psychologists and Code of Conduct. Couples were recruited in different Italian hospitals and private clinics for couples in a situation of infertility. Both partners signed written informed consent for participation before data collection and, separately, they completed the anamnestic schedule and the questionnaires in a quiet room. Confidentiality was assured by replacing the participant’s personal information with a numeric code. No incentives were awarded, and voluntary participation was emphasized. In general, approximately 85% of the couples invited to participate in the study agreed to participate. For the presentarticle, just a small part of the existing database was considered, including only heterosexual couples that were currently undergoing, for the first time, the first stage of the ART procedures. Couples at more advanced stages of ART, or that did not fully answer the self-report measures, were excluded.
Participants
A power analysis was initially performed through the APIMPowerR Program (Ackerman and Kenny, 2016) to determine the minimum sample size to retain a power of .8, yielding a minimum required of N = 79 couples. The final sample comprises 118 couples, age ranging between 24 and 46 years. The mean age was 34.92 for women (SD = 3.98) and 37.45 for men (SD = 5.26), reflecting a significant age difference between the partners (t = 4.42, p < .0001). Couples belong to a medium socio-economic status ([Hollingshead, 1975] SES M = 37.40, SD = 12.48) and declared that the number of years for which they are trying to become pregnant and have a child ranges from 1 to 8 years (M = 3.18, SD = 1.99). Neither men nor women participants ever had children, either from the current relationships or previous ones. About 22.9% of the women participants had at least one abortion. The 27.2% of the sample reported being affected by physical illness not associated to infertility (44 women and 24 men; χ2 = 6,93, p = .011) and none had a psychiatric disorder. The total sample had undergone only the ART first level techniques (81.4% intra-uterine insemination; 18.6% intra-cervical insemination).
Measures
The variables considered in the present study are the following: from the anamnestic data (a) gender, (b) time spent trying to get pregnant (i.e., the time declared trying to get pregnant and have a child); from the specific measures: (c) the global severity index of psychological symptoms, (d) body image avoidance, (e) alexithymia features level, (f) dyadic adjustment, and (g) romantic attachment.
Symptom check list-90-revised
The Symptom Check List-90-Revised (SCL-90-R; Derogatis, 1983) is a self-report assessing distress and psychopathology, able to screen for many psychiatric symptoms and providing a global severity index (GSI) of functioning, which will be considered in the presentarticle. This tool, consisting of 90 items measured on a 5-point Likert scale, from “not at all” (0) to “extremely” (4), displays nine scores along primary symptom dimensions and three scores among global distress indices. Items refer to symptoms experienced during the week preceding the test and higher scores index greater symptoms severity. Cronbach’s alpha for the GSI score is α = 0.95 for males and α = 0.96 for females.
Body image avoidance questionnaire
The Body Image Avoidance Questionnaire (BIAQ; Rosen et al., 1991) is a self-report measure assessing body image-related distress or dissatisfaction referred to aspects of behavioral avoidance of specific experiences. The questionnaire comprises 19 items across four behavioral factors: clothing, social activities, eating restraint and grooming/weighing. All items are scored on a 6-point scale, from “never” (0) to “always” (5). It provides a BIAQ total score, which will be considered in the present paper, with higher scores indexing greater body avoidance. The BIAQ demonstrates a good validity (Maiano et al., 2009) and temporal stability across ages and gender (Timko et al., 2014). In the present sample, Cronbach’s alpha for the BIAQ total score is α=0.80 for males and α=0.83 for females.
Toronto alexithymia scale-20
The Toronto Alexithymia Scale-20 (TAS-20; Bagby et al., 1994) is a 20-item self-report aimed at assessing alexithymia and comprising three subscales: difficulty describing feelings, difficulty identifying feeling, and externally oriented thinking. Items are rated using a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree) providing a final total score of alexithymia. The TAS-20 cutoff scores are the following: 52 to 60 = possible alexithymia, equal to or greater than 61 = alexithymia. TAS-20 shows a good internal consistency (Cronbach’s alpha=.81) and test–retest reliability (.77, p<.01); research using this tool showed adequate levels of convergent and concurrent validity (Ciarrochi and Bilich, 2006). The Italian version was validated by Bressi and colleagues (1996), confirming its original factorial structure. In the present study, the TAS-20 total score will be considered and the Cronbach’s alpha is α=0.79 for women and α=0.73 for men.
Dyadic adjustment scale
The Dyadic Adjustment Scale (DAS; Spanier, 1976) is a self-report measure aimed at assessing couples’ relationship quality and adjustment. It comprises 32 items referred to four subscales: relationship satisfaction, positive relationship behaviors, similarity in goals and beliefs, and affectional expression. The DAS total adjustment score, considered in the presentarticle, ranges from 0 to 151; higher values indicate a general better marital adjustment. The DAS Italian version was validated by Gentili and collaborators (2002), confirming its original factorial structure and good internal reliability. A good dyadic adjustment is considered around 100 points (Spanier, 1976). In the present study, Cronbach’s alpha for the DAS total adjustment score is α = 0.86 for men and α = 0.89 for women.
Experiences in close relationships scale-revised
The Experiences in Close Relationships Scale-Revised (ECR-R; Fraley et al., 2000) is a 36-item self-report assessing adult attachment and providing a dimensional measure of both attachment-related avoidance and anxiety in close relationships. Participants had to indicate the extent to which they agreed with each statement on a 7-point Likert scale ranging from 1 (disagree strongly) to 7 (agree strongly). The Italian version was validated by Calvo 2008. The ECR-R demonstrated excellent psychometric properties (Brennan et al., 1998; Mikulincer and Shaver, 2007). The tool presents a two-factorial structure referred to the avoidant and anxious attachment dimensions; both factors will be considered, and higher scores indicate greater avoidant or anxious romantic attachment. In the present study, avoidant and anxious attachment dimensions demonstrated high (α = 0.82 for women and α = 0.83 for men) and moderate (α = 0.65 for women and α = 0.64 for men) internal consistency, respectively.
Data analysis
All the analyses were performed using the R software (R Core Team, 2016) and PASW Statistics, Release Version 21.00 (SPSS Inc.). Results were considered significant at p < .05. Exploratory statistics and graphs (i.e., boxplots) were initially considered to check for the presence of outliers in the study variables; no extreme outliers were identified. Cases were eliminated when 20% or more of the items of each measure were left unanswered, resulting in a final sample of 118 couples.
Preliminary analysis consists of Pearson r correlations (p < .05; CI = 95%), performed separately for men and women as well as between partners, and considered to evaluate if the couples could be treated as distinguishable as regards the considered variables. Moreover, multivariate permutation tests to assess gender differences. Specifically, multivariate rank tests and multiplicity control were applied through the R package flip (Finos, 2018).
An Actor Partner Interdependence Model (APIM; [(Cook and Kenny, 2005)]) was then performed using the structural equation model (SEM) for distinguishable dyads through the R package lavaan (Rosseel, 2012). The APIM considers the dyad as the unit of analysis and was performed to assess differences and commonalities in the psychological variables (i.e., predictors: TAS-20; DAS; GSI; ECR avoidance; ECR anxiety; and time spent trying to get pregnant) that associate with body-image dissatisfaction (BIAQ; i.e., dependent variable) in men and women also allowing to account for the interdependence of couple’s partners. The model estimates “actor” and a “partner” effects. The actor effect describes the effect of a person’s variable on a given outcome while the partner effect describes the effect, on that same outcome, of the same variable yet measured on the other member of the dyad. Both effects are estimated while controlling for that of the other. Actor and partner effects were further compared to assess which is more influential for males or females. Moreover, in the final model, all the independent variables that did not show an interaction with gender were constrained to be equal (i.e., equal slope). The model was fit on standardized variables and goodness of fit was assessed by considering the chi-square significance level; since the chi-square statistics are sensitive to sample size, two relative measures of fit (i.e., comparative fit index [CPI; Schermelleh-Engel et al., 2003] and incremental fit index [IFI; Bollen’s 1989]) and two absolute measures of fit (i.e., RMSEA and SMRS) were considered. A non-significant chi-square, a CFI and IFI greater than .95 (Hu and Bentler, 1995; Schermelleh-Engel et al., 2003), and an RMSEA and SMRS lower than .10 (Hooper et al., 2007) indicate good model fit. The model goodness was ultimately supported by comparing the final and the saturated model, considered as nested models, through the chi-square difference test using the Satorra (2000) method.
Results
Preliminary analysis
Pearson r correlations performed separately for men and women as well as between partners are shown in Table 1 and report different underlying processes for variables association for men and women. Moreover, the overall psychological symptoms (GSI; clinical cutoff = 1), the alexithymic features level (TAS-20; clinical cut-off = 60), and the body image avoidance referred to body image dissatisfaction (BIAQ; clinical cut-off = 1.2) show non-clinical levels neither for men nor for women (Table 2). Multivariate rank tests (Table 2) show significant gender differences for BIAQ, GSI, and ECR anxiety in which women report higher mean levels. All other variables show non-significant gender differences. These results were confirmed also when multiplicity control was applied.
Table 1.
Pearson r correlations for males, females, and between partners.
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. ECR avoidance | .053 | .449*** | −.086 | .371*** | .242** | .342*** |
| 2. ECR anxiety | .272** | .068 | −.109 | .446*** | .357*** | .171 |
| 3. DAS | −0.090 | .203** | .293*** | .141 | .187* | .153* |
| 4. GSI | .120 | .504*** | .106 | .258*** | .437*** | .360*** |
| 5. TAS-20 | −.044 | .153 | .099 | .331*** | .160* | .178** |
| 6. BIAQ | .006 | .275** | .107 | .433*** | .021 | .088 |
Note: Values above the diagonal, and colored in green, show correlational data assessed on males only (N = 118); Values below the diagonal, and colored in yellow, show correlational data assessed on females only (N = 118). Correlations assessed between males and females’ reports are shown in the blank diagonal (N = 118 couples). * p< .05; ** p<.01; *** p< .001.
Table 2.
Multivariate rank test to assess gender differences among couple’s partners.
| Males | Females | |||||
|---|---|---|---|---|---|---|
| M | SD | M | SD | Stat | adjusted p-value | |
| ECR avoidance | 69.66 | 7.83 | 70.82 | 7.32 | 1.91 | .15 |
| ECR anxiety | 49.31 | 17.33 | 55.78 | 16.83 | −3.33 | 0.005** |
| DAS | 59.62 | 7.02 | 58.97 | 7.99 | 0.48 | 0.88 |
| GSI | .31 | .26 | .44 | .32 | −4.58 | 0.001*** |
| TAS-20 | 41.96 | 7.06 | 41.24 | 5.87 | 0.04 | 0.96 |
| BIAQ | .89 | .39 | 1.18 | .43 | −5.73 | .001*** |
Note: N = 118 couples; adjusted p-value based on multiplicity correction; * p< .05; ** p<.01; *** p< .001.
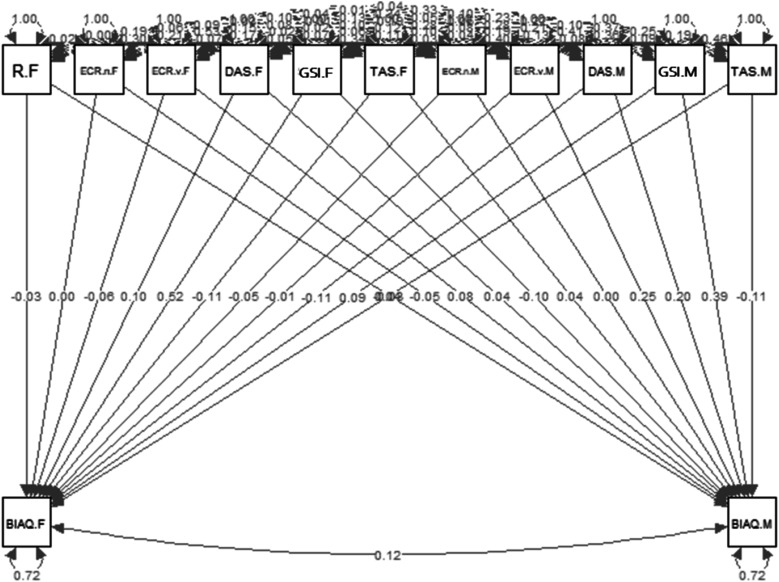
Actor–partner interdependence model
The APIM (Figure 1) results show that two actor effects, females’ DAS (β = 0.133; p = .026) and GSI (β = 0.467; p < .00), positively and significantly predict female BIAQ. Specularly, the equivalent males’ actor effects (DAS [β = 0.133; p = .026] and GSI [β = 0.499; p = .001]) positively and significantly predict males’ BIAQ. Moreover, males’ TAS-20 (β = − 0.499; p = .001) negatively and significantly predicts males’ BIAQ. No significant partner effects have emerged. Comparing the level of influence of actor and partner effects within partners, for both males and females, the GSI actor effect results as significantly more influential than the corresponding partner effect (respectively, Δ = 0.587, p = .001; Δ = 0.378, p = .015). Moreover, the model shows good fit as indexed by the CFI and IFI greater than .95, chi-square significance level (p > .05) and RMSEA and SMRS lower than .10. Finally, comparing the un-contrained and constrained model, the chi-square difference test supports the goodness of the considered constrained model (p = .105) as shown by the smaller AIC and BIC coefficients.
Figure 1.
Actor-partner interdependence model.
Discussion
Stressful bodily emotions and body perception related to infertility and ART procedures are a critical aspect of people desiring to get pregnant and have children when they are unable to do so. The present study aimed to bridge the gap of previous research by analyzing couples’ psychological and relational characteristics during the initial phases of the ART. The sole consideration of couples newly introduced to first-level ART procedure had the intent to shed light on couples’ characteristics before treatments’ pervasiveness increase. This would provide insight useful to design psychosocial interventions and prevention practices aimed at supporting the well-being of couples in a situation of infertility, thereby further increasing the likelihood of successful ART outcomes (Purweal et al., 2017; Simionescu et al., 2021). Attention was particularly paid to body image avoidance referred to body image dissatisfaction, and gender differences in all considered variables as well as the couple’s commonalities and interdependence.
In the present study, the sample reported normative levels of psychological symptoms, alexithymia features, and body image avoidance, although showing significant gender differences in psychological symptoms (Agostini et al., 2017; Karlidere et al., 2007), body image avoidance (Brennan et al., 2010), and romantic anxious attachment (Donarelli et al., 2012; Moura-Ramos et al., 2017), all greater in women. These results, whereby couples do not show psychological difficulties of clinical relevance, suggest that the psychological distress of the couples that are undergoing ART might be linked to the medical pervasiveness of more advanced treatments and the presence of previous treatment failures (Agostini, et al., 2017), while the current sample was just introduced to first-level ART procedures implying reduced treatment pervasiveness and no prior treatment failures. As expected (Jackson et al., 2014), couples showed very similar ratings of marital adjustment and satisfaction. However, couples involved in these early stages demonstrated higher romantic avoidant attachment levels and lower dyadic adjustment than what was expected from people desiring to enlarge their families. Their scores were not high enough for them to be considered “happy couples” (M = 114.8; Spainer, 1976), nor low enough to suggest them to undertake couple therapy (M = 90,94; Prouty et al., 2000), or to be identified with Spanier’s sample of divorcees (M =70.7). These findings might be interpreted as a result of a “setting bias” as recruitment within a hospital setting, where psychological, relational, and subjective features are less expected to be investigated, compared with medical conditions, could predispose patients to be less prone to showing their intimate relational characteristics.
Interestingly, differences in the correlational patterns of males and females have emerged and showed differing underlying processes accounting for variables associations. Coherent with past literature (Donarelli et al., 2012; Moura-Ramos et al., 2017), romantic avoidant attachment resulted more relevant for males, while romantic anxious attachment for females, and particularly as regards the association with body image avoidance. Moreover, although dyadic adjustment, psychological symptoms and alexithymia significantly associated between partners, it then emerged a different associative pattern referred to alexithymia traits among males as compared to females. Specifically, only for males, alexithymia positively associates with all the considered variables, supporting past research that observed greater alexithymia traits among males (Levant et al., 2009). In this regard, considering dyadic data analyzed through the APIM, which allows to isolate the effect of a variable on the considered outcome (Kenny et al., 2006), only among males alexithymia resulted as significantly associated with body-image avoidance, yet showing a negative association, which would suggest that the more concrete and superficial is the emotional consciousness of males, the less it seems to be their need for behavioral avoidance referred to body image dissatisfaction and distress. To control for variables' effects means that the association between two variables is isolated and estimated by excluding the potential influence of confounding variables. As such, this evidence suggests that, when controlling for the influence of all the other variables, greater alexithymia might acquire a “protective/defensive” role for males, thereby supporting the maintenance of a more positive body perception. This would be in line with the ‘secondary alexithymia’ hypothesis, whereby an incapacity to understand and communicate emotions would mitigate painful affects and even function as defense against the depression symptoms associated infertility (Conrad et al., 2001). This finding should be further investigated, particularly in light of past evidence reporting that although both couple’s partners are negatively affected by infertility and ART, males’ psychological symptomatology seem particularly associated with pregnancy achievement (Martínez-Pampliega et al., 2019).
Overall, the present APIM showed optimal goodness of fit indices, strongly indicating the presence of an underlying process connecting the variables considered in respect to body image avoidance, in both males and females. Comparing partners, for both males and females body image avoidance was significantly and positively influenced by their own (actor effect) level of dyadic adjustment and psychological symptoms. These findings depict a picture quite odd to explain since, although it could be expected that greater overall psychological symptoms associate with greater body image avoidance, as it is referred to body image dissatisfaction and distress, (Barnes et al., 2020; Duchesne et al., 2016; Rosen et al., 1991), it is not obvious how this avoidance positively associates with a more favorable perception of dyadic adjustment in both partners. Considering the low rating of marital adjustment in the present sample, which is correlated between partners, and the non-clinical level of body image avoidance reported, it seems that these couples maintained a just sufficient level of good dyadic adjustment and a low level of body image dissatisfaction; it might be useful to see, along the ART procedure stages, if these two variables will maintain such kind of relationship. Noteworthy, specifically referring to the significant influence of each partner’s psychological symptoms on their experience of body avoidance and dissatisfaction, the current findings point to the relevance of providing specific and individual support to the couple’s partners already from the very early stages of the ART procedure. This is also supported by past literature highlighting the need to provide psychosocial care to people initiating ART procedures, with the potential to prevent the development or the worsening of psychosocial difficulties and symptoms (Purewala et al., 2018) that could hinder the likelihood of ART cycles success (Purweal et al., 2017; Renzi et al., 2020a, 2020b; Simionescu et al., 2021).
Conclusion
In the very early stages of the ART, couples resulted similar and non-clinical with respect to the considered variables (Jackson et al., 2014). Moreover, support is also provided as regards a shred of well-known evidence found on the literature and not just ART-related: females are on average significantly more anxious in their romantic relationships then males are (Donarelli et al., 2012; Moura-Ramos et al., 2017; Salcuni et al., 2015).
In the current study, couples can be considered “untouched” by the possible effects and consequences of the ART journey, since they were undergoing first-level ART for the first time. Coherently, couples’ partners psychological well-being does not seem to have been compromised by the ART procedures they were currently undergoing. Males and females are consistent within couples, showing both similar levels in the measured variables, and comparable modalities of influence: both are more self-influenced (actor effect) then partner-influenced in respect to their psychological state and body image avoidance and dissatisfaction. The presence of psychological symptoms accounts for the body image avoidance that results from body image dissatisfaction and distress, both for men and women. Furthermore, for both, the actor effect seems significantly more influential; on the contrary, alexithymic features only seem to have a protective function toward males’ body image dissatisfaction, functioning as a “defensive” factor. Yet, the present findings also suggest that by posing less control on the intervening effect of external variables, thus resembling to a greater extent the reality and complexity of human psychology, greater alexithymia might instead favor reduced overall well-being in an overwhelming and stressful situation like that of infertility and of ART, which is particularly relevant for clinical practice.
This research has some positive remarks, such as the evaluation of the very early stages of the ART procedures and the exploration of both partners’ effect on the individual’s variables and the effect of the interaction of both partners’ variables on the individual’s outcome. However, the sole consideration of couples undergoing first-level ART for the first time can also be considered a limit of the current work, as preventing the possibility to assess differences in the psychological state of couples as treatment pervasiveness increases. Further limitations that should be acknowledged are the sample small size, the homogeneity among couples as well as their voluntary participation and the use of only self-report measures (Schermelleh-Engel et al., 2003). Furthermore, this study lacks a control sample that would have provided data to evaluate whether the recognized processes are relevant only to the couples undergoing ART or if they are so for all the couples trying to conceive. Thus, future research is suggested regarding a longitudinal research design and particularly considering the association between dyadic adjustment and body image avoidance. Future longitudinal studies are also suggested as regards the second level of the ART as well as the percentage of positive ART outcomes at different stages. Furthermore, it would be interesting to assess what is the effect of the type of infertility and which partner, together with its origins, on the analyzed constructs. Although the limited differences that have emerged among partners and the low overall level of dyadic adjustment, which is considered as a protective factor for positive ART outcomes (Martínez-Pampliega et al., 2019), our results support the importance of differentiating gender-specific psychological interventions along the ART path, to prevent and mitigate the negative impact of infertility and the ART on the individuals, and in particular on their body image avoidance and dissatisfaction, as well as the couples and future children’s well-being (Monti et al., 2009).
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Elisa Mancinelli https://orcid.org/0000-0003-2089-3507
References
- Agostini F, Monti F, Andrei F, et al. (2017) Assisted reproductive technology treatments and quality of life: a longitudinal study among subfertile women and men. Journal of assisted Reproduction and Genetics. 34, 1307–1315. DOI: 10.1007/s10815-017-1000-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerman RA, Kenny DA. (2016) APIMPowerR: an interactive tool for actor-partner interdependence model power analysis. Available at: https://robert-a-ackerman.shinyapps.io/APIMPowerRdis/ (Accessed: April 2020).
- Akhondi MM, Dadkhah A, Bagherpour A, et al. (2011) Study of body image in fertile and infertile men. Journal of Reproduction and Infertility. 12(4): 295–298. [PMC free article] [PubMed] [Google Scholar]
- Amir M, Horesh N, Lin-Stein T. (1999) Infertility and adjustment in women: the effects of attachment style and social support. Journal of Clinical Psychology in Medical Settings. 6(4): 463–479. [Google Scholar]
- Bagby RM, Parker JDA, Taylor GJ. (1994) The twenty-item Toronto Alexithymia scale I. Item selection and cross-validation of the factor structure. Journal of Psychosomatic Research. 38(1): 23–32. [DOI] [PubMed] [Google Scholar]
- Barnes M, Abhyankar P, Dimova E, et al. (2020) Associations between body dissatisfaction and self-reported anxiety and depression in otherwise healthy men: A systematic review and meta-analysis. Plos One. 15(2): e0229268. DOI: 10.1371/journal.pone.0229268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bollen KA. (1989) A new incremental fit index for general structural equation models. Sociological Methods and Research. 17(3): 303–316. [Google Scholar]
- Brennan KA, Clark CL, Shaver PR. (1998) Self-report measurement of adult attachment: an integrative overview. In Simpson JA, Rholes WS. (eds) Attachment Theory and Close Relationships. New York, NY: Guilford Press, 46–76. [Google Scholar]
- Brennan MA, Lalonde CE, Bain JL. (2010) Body image perceptions: do gender difference exist? Psy Chi Journal of Undergraduate Research. 15(3): 130–138. DOI: 10.24839/1089-4136.JN15.3.130. [DOI] [Google Scholar]
- Bressi C, Taylor G, Parker J, et al. (1996) Cross validation of the factor structure of the 20-item Toronto Alexithymia Scale: an Italian multi center study. Journal of Psychosomatic Research. 41(6): 551–559. DOI: 10.1016/s0022-3999(96)00228-0. [DOI] [PubMed] [Google Scholar]
- Calvo V. (2008) Il questionario ECR-R: aspetti di validazione della versione italiana dello strumento [TheECR-R questionnaire: aspects of validation of the Italianversion of the instrument]. Poster Presented at the X National Congress of the Section of Clinical and Dynamic Psychology of the Italian Association of Psychology (AIP): Padova, IT. [Google Scholar]
- Ciarrochi J, Bilich L. (2006) Acceptance and Commitment therapy. Measures Package. Unpublished manuscript, University of Wollongong, Wollongong, Australia. [Google Scholar]
- Conrad R, Schilling G, Langenbuch M, et al. (2001) Alexithymia in male infertility. Human Reproduction. 16(3): 587–592. DOI: 10.1093/humrep/16.3.587. [DOI] [PubMed] [Google Scholar]
- Cook WL, Kenny DA. (2005) The actor–partner interdependence model: a model of bidirectional effects in developmental studies. International Journal of Behavioral Development. 29(2): 101–109. DOI: 10.1080/01650250444000405. [DOI] [Google Scholar]
- De Berardis D, Carano G, Campanella G, et al. (2007) Alexithymia and its relationships with body cheching and body image in a non-clinical female sample. Eating behaviour. 8: 296–304. DOI: 10.1016/j.eatbeh.2006.11.005. [DOI] [PubMed] [Google Scholar]
- De Berardis D, Mazza M, Marin S, et al. (2014) Psychopathology, emotional aspects and psychological counselling in infertility: a review. Clinica Terapeutica. 165(3): 163–169. DOI: 10.7417/CT.2014.1716. [DOI] [PubMed] [Google Scholar]
- Derogatis L. (1983) The SCL-90 R Manual-II: Administration, Scoring and Procedures. Baltimore, MD: Clinical Psychometric Research. [Google Scholar]
- Donarelli Z, Lo Coco G, Gullo S, et al. (2012) Are attachment dimensions associated with infertility-related stress in couples undergoing their first IVF treatment? A study on the individual and cross-partner effect. Human Reproduction. 27(11): 3215–3225. DOI: 10.1093/humrep/des307. [DOI] [PubMed] [Google Scholar]
- Duchesne AP, Dion J, Lalande D, et al. (2016) Body dissatisfaction and psychological distress in adoldescents: is self-estem a mediator? Journal of Health Psychology . 22(12): 1–7. DOI: 10.1177/1359105316631196. [DOI] [PubMed] [Google Scholar]
- El Kissi Y, Ben Romdhane A, Hidar S, et al. (2013) General psychopathology, anxiety, depression and self-esteem in couples undergoing infertility treatment: a comparative study between men and women. European Journal of Obstetrics and Gynecology Reproductive Biology. 167(2): 185–189. DOI: 10.1016/j.ejogrb.2012.12.014. [DOI] [PubMed] [Google Scholar]
- European Society of Human Reproduction and Embryology (2014) ART fact sheet. Available at: http://www.eshre.eu/Guidelines-and-Legal/ART-fact-sheet.aspx (Accessed: June 2020).
- Finos L. (2018) flip: multivariate permutation tests. R package version 2.4.3. Available at: https://CRAN.R-project.org/package=flip (Accessed: September 2020).
- Fraley RC, Waller NG, Brennan KA. (2000) An item response theory analysis of self-report measures of adult attachment. Journal of Personality and Social Psychology. 78(2): 350–365. DOI: 10.1037/0022-3514.78.2.350. [DOI] [PubMed] [Google Scholar]
- Gentili P, Contreras L, Cassaniti M, et al. (2002) La Dyadic adjustment scale: una misura dell' adattamento di coppia [A measurement of dyadic adjustment: the dyadic adjustment scale]. Minerva Psichiatrica. 43(2): 107–116. [Google Scholar]
- Glover L, Gannon K, Sherr L, et al. (1996) Distress in sub-fertile men: a longitudinal study. Journal of Reproductive and Infant Psychology. 14(1): 23–36. [Google Scholar]
- Gourounti K, Anagnostopoulos F, Griva F, et al. (2016) Alexithymia and fertility-related stress. Women health. 56(3): 312–325. DOI: 10.1080/03630242.2015.1088119. [DOI] [PubMed] [Google Scholar]
- Gurunath S, Pandian Z, Anderson RA, et al. (2011) Defining infertility—a systematic review of prevalence studies. Human Reproduction Update. 17(5): 575–588. DOI: 10.1093/humupd/dmr015. [DOI] [PubMed] [Google Scholar]
- Hammarberg K, Fisher JRW, Wynter KH. (2008) Psychological and social aspects of pregnancy, child birth and early parenting after assisted conception: a systematic review. Human Reproduction Update.14(5): 395–414. DOI: 10.1093/humupd/dmn030. [DOI] [PubMed] [Google Scholar]
- Hepper EG, Carnelley KB. (2012) Attachment and romantic relationships: The role of models of self and other. In: Paludi M. (ed) The Psychology of Love. Santa Barbara, CA: Praeger, (Vol. 1), 133–154. [Google Scholar]
- Hollingshead AB. (1975) Four factor index of social status . Unpublished working paper, Department of Sociology, Yale University, New Haven, CT. [Google Scholar]
- Hooper D, Coughlan J, Mullen MR. (2007) Structural equation modeling: guidelines for determining model fit. Electronic Journal on Business Research Methods. 6(1): 53–60. [Google Scholar]
- Hu LT, Bentler PM. (1995) Evaluating model fit. In: Hoyle RH. (ed) Structural Equation Modeling: Concepts, Issues, and Applications . Thousand Oaks, CA, US: Sage Publications, Inc, 76–99. [Google Scholar]
- Huppelschoten AG, Van Dongen AJCM, Verhaak CM, et al. (2013) Differences in quality of life and emotional status between infertile women and their partners. Human Reproduction. 28(8): 2168–2176. DOI: 10.1093/humrep/det239. [DOI] [PubMed] [Google Scholar]
- Jackson JB, Miller RB, Oka M, et al. (2014) Gender differences in marital satisfaction: a meta‐analysis. Journal of marriage and family. 76(1): 105–129. DOI: 10.1111/jomf.12077. [DOI] [Google Scholar]
- Juriü Vukeliü D, Kuševiü Z, Horvatiü J. (2019) Alexithymia and psychological distress among women undergoing in vitro fertilization. Psychiatria Danubina. 31(4): 437–477. DOI: 10.24869/psyd.2019.473. [DOI] [PubMed] [Google Scholar]
- Karamidehkordi A, Roudsari RL. (2014) Body image and its relationship with sexual function and marital adjustment in infertile women. Iranian Journal of Nursing and Midwifery Research. 19(1): 51–58. [PMC free article] [PubMed] [Google Scholar]
- Karlidere T, Bozkurt A, Yetkìn S, et al. (2007) Is there a gender difference in infertile couples without Axis I psychiatric disorders in the context of emotinal symptoms, social support, and sexual function? Turkish Journal of Psychiatry. 18(4): 1–11. [PubMed] [Google Scholar]
- Kenny AD, Kashy DA, Cook WL. (2006) Dyadic Data Analysis. Simpson J.A. (Ed.) The Guildford Press. [Google Scholar]
- Kushnir VA, Barad DH, Albertini DF, et al. (2017) Systematic review of worldwide trends in assisted reproductive technology 2004–2013. Reproductive Biology and Endocrinology. 15(1): 6. DOI: 10.1186/s12958-016-0225-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Istituto Superiore di Sanità [Higher Institute of Health] (2016) Relazione del Ministro della Salute al parlamento sullo stato di attuazione della legge contenente norme in materia di procreazione medicalmente assistita (legge 19 febbraio 2004, n. 40, articolo 15) [Report by the Minister of Health to Parliament on the state of implementation of the law containing rules on assisted reprodactive techniques (Law n. 40 of 19 February 2004, Art. 15)]. Report, Rome, Italy: Istituto Superiore di Sanità [Higher Institute of Health]. https://www.salute.gov.it/imgs/C_17_pubblicazioni_2511_allegato.pdf [Google Scholar]
- Levant RF, Hall RJ, Williams CM, et al. (2009) Gender differences in alexithymia. Psychology of Men and Masculinity. 10(3): 190–203. DOI: 10.1037/a0015652. [DOI] [Google Scholar]
- Lyvers M, Pickett L, Needham K, et al. (2021) Alexithymia, fear of intimacy, and relationship satisfaction. Journal of Family Issue . 3(2): 1–22. DOI: 10.1177/0192513X211010206 [DOI] [Google Scholar]
- Mahajan NN, Turnbull DA, Davies MJ, et al. (2008) Adjustment to infertility: the role of intrapersonal and interpersonal resources/vulnerabilities. Human reproduction. 24(4): 906–912. DOI: 10.1093/humrep/den462. [DOI] [PubMed] [Google Scholar]
- Maiano C, Morin AJS, Monthuy-Blanc J, et al. (2009) The body image avoidance questionnaire: assessment of its construct validity in a community sample of French adolescents. International Journal of Behavioral Medicine. 16(2): 125–135. DOI: 10.1007/s12529-009-9035-7. [DOI] [PubMed] [Google Scholar]
- Maroufizadeh S, Hosseini M, Foroushani AR, et al. (2019) The relationship between perceived stress and marital satisfaction in couples with infertility: actor-partner interdependence model. International Journal of Fertility and Sterility. 13(1): 66–71. DOI: 10.22074/ijfs.2019.5437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer AL, McNulty JK. (2010) Body image and marital satisfaction: evidence for the mediating role of sexual frequency and sexual satisfaction. Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43). 24(2): 156–164. DOI: 10.1037/a0019063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. (2007) Attachment in Adulthood: Structure, Dynamics, and Change. New York, NY: Guilford Press. [Google Scholar]
- Monti F, Agostini F, Fagandini P, et al. (2009) Depressive symptoms during late pregnancy and early parenthood following assisted reproductive technology. Fertility and Sterility. 91(3): 851–857. DOI: 10.1016/j.fertnstert.2008.01.021. [DOI] [PubMed] [Google Scholar]
- Moura-Ramos M, Santos TA, Canavarro MC. (2017) The role of attachment anxiety and attachment avoidance on the psychosocial well-being of infertile couples. Journal of Clinical Psychology in Medical Settings. 24(2): 132–143. DOI: 10.1007/s10880-017-9496-9. [DOI] [PubMed] [Google Scholar]
- Newton CR, Hearn MT, Yuzpe AA. (1990) Psychological assessment and follow-up after in vitro fertilization: assessing the impact of failure. Fertility and Sterility. 54(5): 879–886. [DOI] [PubMed] [Google Scholar]
- Martínez-Pampliega A, Cormenzana S, Martín S, et al. (2019) Marital functioning and treatment outcome in couples undergoing assisted reproduction. Journal of advanced nursing. 75(2): 338–347. DOI: 10.1111/jan.13844. [DOI] [PubMed] [Google Scholar]
- Peloquin K. (2013) Infertility: a social and spousal reality that needs to be studied. Integrating Science and Practice. 3(2): 22–26. [Google Scholar]
- Prouty A, Markowski EM, Barnes HL. (2000) Using the dyadic adjustment scale in marital therapy: an exploratory study. The Family Journal. 8(3): 250–257. DOI: 10.1177/1066480700083006. [DOI] [Google Scholar]
- Purweal S, Chapman SCE, van den Akker OBA. (2017) A systematic review and meta-analysis of psychological predictors of successful assisted reproductive technologies. BMC Research Notes, 10(1): 711. DOI: 10.1186/s13104-017-3049-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purewala S, Chapmanb SCE, van den Akkerc OBA. (2018) Depression and state anxiety scores during assisted reproductive treatment are associated with outcome: a meta-analysis. Reproductive Bio Medicine Online. 36(6): 646–657. DOI: 10.1016/j.rbmo.2018.03.010. [DOI] [PubMed] [Google Scholar]
- R Core Team (2016) R: a language and environment for statistical computing. Vienna, AT: R Foundation for Statistical Computing. https://www.rproject.org/. [Google Scholar]
- Ramirez-Ucles IM, Del Castillo-Aparicio M, Moreno-Rosset C. (2015) Variables psicologicas predictoras del desajuste emocional en personas infertiles: analisis del papel modulador del sexo [Psychological predictor variables of emotional maladjustment in infertility: analysis of the moderating role of gender]. Clinica y Salud. 26(1): 57–63. DOI: 10.1016/j.clysa.2015.01.002. [DOI] [Google Scholar]
- Randall AK, Bodenmann G. (2009) The role of stress on close relationships and marital satisfaction. Clinical Psychology Review. 29(2):105–115. DOI: 10.1016/j.cpr.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Reis S, Xavier MR, Coelho R, et al. (2013) Psychological impact of single and multiple courses of assisted reproductive treatments in couples: a comparative study. European Journal of Obstetrics and Gynecology and Reproductive Biology. 171(1): 61–66. DOI: 10.1016/j.ejogrb.2013.07.034. [DOI] [PubMed] [Google Scholar]
- Renzi A, Di Trani M, Solano L, et al. (2020. a) Alexithymia, infertility-related stress and quality of life in women undergoing an assisted reproductive treatment. Stress & Health . 36(5): 654–662. DOI: 10.1002/smi.2967. [DOI] [PubMed] [Google Scholar]
- Renzi A, Di Trani M, Solano L, et al. (2020. b) Success of assisted reproductive technology treatment and couple relationship: A pilot study on the role of romantic attachment. Health Psychology Open. 7(1): 2055102920933073. DOI: 10.1177/2055102920933073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollè L, Prino LE, Sechi C, et al. (2017) Parenting stress, mental health, dyadic adjustment: a structural equation model. Frontiers in Psychology. 23(8): 839. DOI: 10.3389/fpsyg.2017.00839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen JC, Srebnik D, Saltzberg E, et al. (1991) Development of a body image avoidance questionnaire. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 3(1): 32–37. [Google Scholar]
- Rosseel Y. (2012) Lavaan: an R package for structural equation modeling. Journal of Statistical Software. 48(2): 1–36. [Google Scholar]
- Salcuni S, Miconi D, Altoè G, et al. (2015) Dyadic adjustment and parenting stress in internationally adoptive mothers and fathers: the mediating role of adult attachment dimensions. Frontiers In Psychology. 6: 1279. DOI: 10.3389/fpsyg.2015.01279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samadaee-Gelehkolaee K, McCarthy BW, Khalilian A, et al. (2016) Factors associated with marital satisfaction in infertile couples: a comprehensive literature review. Global Journal of Health Science. 8: 96–109. DOI: 10.5539/gjhs.v8n5p96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A. (2000) Scaled and adjusted restricted tests in multi-sample analysis of moment structures. In: Heijmans DDH, Pollock DSG, Satorra A. (eds) Innovations in Multivariate Statistical Analysis: A Festschrift for Heinz Neudecker . Dordrecht: Kluwer Academic, 233–247. [Google Scholar]
- Schermelleh-Engel K, Moosbrugger H, Muller H. (2003) Evaluating the fit of structural equation models: tests of significance and descriptive goodness-of-fit measures. Methods of Psychological Research Online. 8(2): 23–74. [Google Scholar]
- Shigeto A, Mangelsdorf SC, Brown GL. (2014) Roles of family cohesiveness, marital adjustment, and child temperament in predicting child behavior with mothers and fathers. Journal of Social and Personal Relationships. 31(2): 200–220. DOI: 10.1177/0265407513490586. [DOI] [Google Scholar]
- Sifneos PE. (1973) The prevalence of alexithymic characteristics in psychosomatic patients. Psychotherapy and Psychosomatics. 22: 255–262. [DOI] [PubMed] [Google Scholar]
- Simionescu G, Doroftei B, Maftei R, et al. (2021) The complex relationship between infertility and psychological distress (Review). Experimental and Therapeutic Medicine. 21(4): 306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spanier GB. (1976) Measuring dyadic adjustment: new scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family. 38(1): 15–28. [Google Scholar]
- Stanhiser J, Steiner AZ. (2019) Psychosocial aspects of fertility and assisted reproductive technology. Obstetrics and Gynecology Clinics of North America. 45: 563–574. DOI: 10.1016/j.ogc.2018.04.006. [DOI] [PubMed] [Google Scholar]
- Taylor GJ, Bagby RM. (2012) The Alexithymia Personality Dimension. New York, US: Oxford Handbooks online. DOI: 10.1093/oxfordhb/9780199735013.013.0030. [DOI] [Google Scholar]
- Timko CA, Juarascio AS, Martin LM, et al. (2014) Body image avoidance: an underexplored yet important factor in the relationship between body image dissatisfaction and disordered eating. Journal of Contextual Behavioral Science. 3(3): 203–211. DOI: 10.1016/j.jcbs.2014.01.002i. [DOI] [Google Scholar]
- Wyndham N, Marin Figueira PN, Patrizio P. (2012) A persistent misperception: assisted reproductive technology can reverse the “aged biological clock”'. Fertility and Sterility. 97(5): 1044–1047. DOI: 10.1016/j.fertnstert.2012.02.015. [DOI] [PubMed] [Google Scholar]
- Zeren F, Gursoy E, Colak E. (2019) The quality of life and dyadic adjustment of couples receiving infertility treatment. African Journal of Reproductive health. 23(1): 117–127. DOI: 10.29063/ajrh2019/v23i1.12. [DOI] [PubMed] [Google Scholar]