Abstract
Background:
Cardiac rehabilitation (CR) programs have evolved from exercise-only programs designed to improve cardiovascular fitness to secondary prevention programs with a broader mandate to alter lifestyle-related behaviors that control cardiac risk factors and, thereby, reduce overall cardiovascular risk. As the obesity epidemic has evolved in the late 20th and early 21st centuries, the prevalence of type 2 diabetes mellitus and the metabolic syndrome have soared and blunted the otherwise expected downturn in deaths from coronary heart disease related to better control of risk factors. In that the causes of obesity are behavioral in origin, the most effective treatment strategy requires a comprehensive, behavioral based approach.
Purpose:
In this review we outline optimal lifestyle approaches that can be delivered in the CR setting to assist cardiac patients with their long-term goals of reducing weight and improving cardiac risk factors while concurrently improving cardiovascular fitness. We also performed a survey of CR programs throughout the U.S. and found that only 8% currently deliver a behavioral weight programs.
Conclusions:
Cardiac rehabilitation programs need to take on an important challenge of secondary prevention which is to develop behavioral weight loss programs to assist cardiac patients to lose weight and, thereby, improve multiple risk factors and long-term prognosis.
Keywords: cardiac rehabilitation, obesity, treatment
Condensed Abstract
Cardiac rehabilitation (CR) programs have evolved from exercise-only programs designed to improve cardiovascular fitness to secondary prevention programs with a broader mandate to alter lifestyle-related behaviors that control cardiac risk factors and, thereby, reduce overall cardiovascular risk. In this context, to optimize clinical outcomes, CR programs need to establish and operationalize behavioral weight loss programs.
BACKGROUND
Obesity: Definitions, Prevalence and Negative Consequences
Obesity is most commonly defined by the body mass index (BMI) which is the ratio of body weight (kg) to height in meters2. A healthy or normal BMI is 18.5–24.9 kg/m2 overweight is 25.0–29.9 kg/m2, and obesity ≥30 kg/m2. In an individual patient, BMI does not have the ability to distinguish body weight that is muscle or fat; thus, it should be supplemented with a waist circumference (WC) measurement to assess abdominal obesity. A WC measurement of > 88 cm (36 inches) in women and 102 cm (40 inches) in men reflects a body weight with excessive abdominal adiposity1.
Over 200 million adults (72 %) in the U.S. are overweight or obese, whereas 42% are classified as obese2. Obesity contributes to a shortened life span due to associations with atherosclerotic cardiovascular disease (ASCVD), type 2 Diabetes Mellitus (T2DM), insulin resistance (IR), hypertension, kidney disease, obstructive sleep apnea, and other conditions3. Obesity is an independent risk factor for the development and progression of ASCVD. Due to this association, nearly half of individuals attending CR are obese4,5 and 80% of individuals are overweight or obese4.
Obesity has been recognized by the Centers for Disease Control as an epidemic in the U.S. since the late 1970’s6. Rates of obesity have risen steadily from a prevalence of 30% in 1999 to 42% in 20182. The combination of overweight/obesity has similarly increased over this time period from 56% in 1999 to 72% in 2018 2.
The primary mechanistic role of obesity in the development of ASCVD is its predisposition to the development of T2DM and IR3. It also predisposes to hypertension and a generalized inflammatory state7,8.
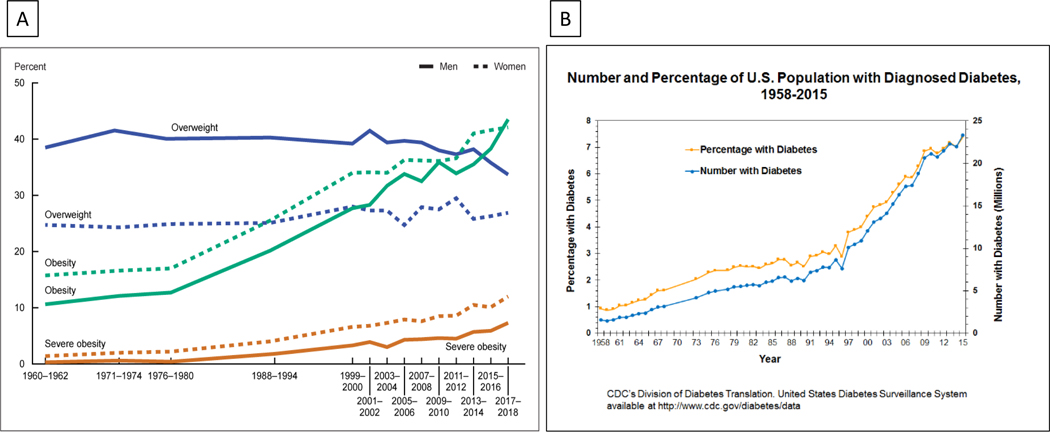
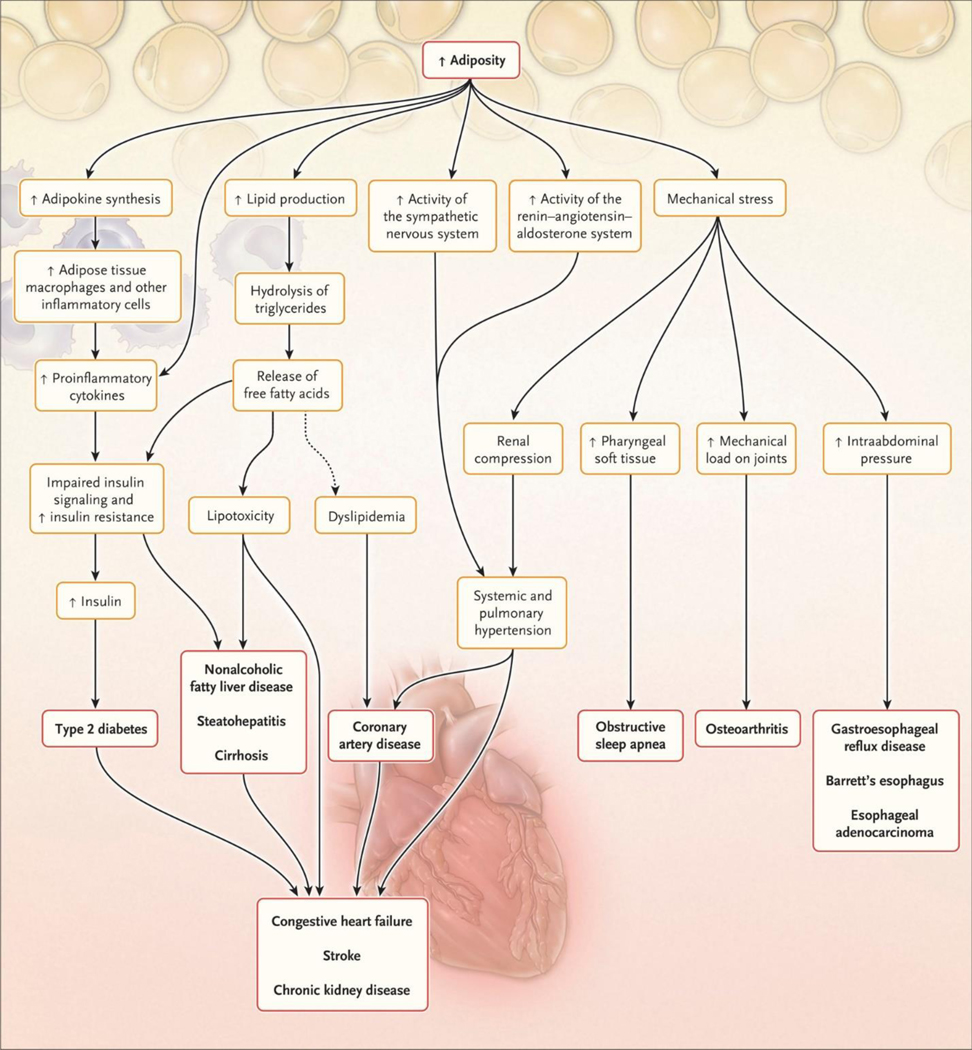
Increases in rates of T2DM in the U.S. have mirrored the rates of obesity with an approximate delay of 10 – 15 yr (Figure 1)9,10. There is overwhelming evidence that BMI, abdominal obesity and the increase in adiposity are associated with the development of T2DM11–13 and hypertension. Mechanistically, excess adipocytes release free fatty acids and inflammatory cytokines that contribute to impaired insulin signaling and the insulin-resistant state (Figure 2)8. Obesity leads to hypertension through a combination of chronic over-activity of the sympathetic nervous system and increased activity of the renin-angiotensin system. The presence of excess intra-abdominal adipose tissue is particularly linked to IR and its sequelae8.
Figure 1.
Rates of Overweight / Obesity (Left Panel) 1960 2018, Rates of Diabetes (Right Panel) in the U.S. 1958 – 2015.
Figure 2.
Some Pathways through Which Excess Adiposity Leads to Major Risk Factors and Common Chronic Diseases (11). Reproduced with Permission New Engl J Med.
In a CR population, the combined prevalence of IR (44%) and T2DM (23%) is 67%, which paralleled the prevalence of metabolic syndrome, present in 65% of patients14. Metabolic syndrome is defined by the presence of at least three of the following five characteristics: Waist circumference >102cm in men, >88cm in women, blood pressure (BP) > 130 systolic or 85 mm diastolic, fasting triglycerides > 150mg/dL, fasting HDL cholesterol < 40 mg/dL or fasting glucose > 100mg/dL (or on T2DM medication)15. Women in CR have a higher prevalence of IR than men (73 vs 64%) and a greater percentage with an elevated WC (71 vs 60%)14. In patients with ASCVD, rates of obesity have been increasing steadily4 (Table 1).
Table 1.
Trends in Obesity and Obesity-Related Risk Factors in Cardiac Rehabilitation 1996– 2015
| 1996–2000 | 2011–2015 | P Value | |
|---|---|---|---|
| Body Weight, kg | 84.8 ± 18.1 | 87.6 ± 19.1 | <.0001 |
| Body Mass Index, kg/m 2 | 28.8 ± 5.4 | 29.9 ± 5.9 | <.001 |
| Prevalence of Obesity | 33 | 41 | <.001 |
| Prevalence of Diabetes | 17 | 23 | <.05 |
| Prevalence of Hypertension | 51 | 63 | <.001 |
Data are presented as mean ± SD or %.
Adapted from Gaalema, et al. 4
Effects of Weight Loss on Cardiac Risk Factors in the General Population
In non-cardiac populations, the beneficial effects of weight loss on obesity-related risk factors have been very well studied3,16–18. Most importantly, weight loss is clearly beneficial in reducing the risk of developing T2DM. In the Diabetes Prevention Program, which included a combination of weight loss and exercise, a median weight loss of 5.5% over 2.8 yr reduced the risk of progressing from prediabetes to T2DM by 58%17. Additionally, a small study (n=12) of individuals with recently diagnosed T2DM (<1 year), not yet on diabetic medications, and a mean BMI of 35.8 kg, a 6-mo program of behavioral weight loss (BWL) and almost daily walking of 45 min resulted in a mean weight loss of 9.7 kg. With this intervention 8/12 patients (67%) went into partial remission of their T2DM with the mean Hemoglobin A1c dropping from 6.8 to 6.2%19.
In patients with hypertension, weight loss is the most powerful, non-pharmacologic intervention to reduce BP. A low salt diet, reduced alcohol consumption and exercise also have favorable effects20, 21. In a meta-analysis, weight loss averaging 5.1 kg after diet and/or exercise reduced BP by 4.4/3.5 mm Hg (systolic BP/diastolic BP)22. Weight loss resulting from either reductions in caloric intake or increases in physical activity is associated with improvements in lipid profile, BP and insulin sensitivity16. A sustained weight loss of >5% is an agreed upon target to reduce cardiac risk factors. In addition, weight loss is also recommended for the management of persistent and paroxysmal atrial fibrillation23. Finally, exercise has the additional favorable effect of improving cardiorespiratory fitness, a well-established and independent coronary risk factor24.
Cardiac Rehabilitation as Secondary Prevention Program
Cardiac rehabilitation has evolved from an exercise-only program designed to improve fitness after a prolonged hospitalization for a cardiac event to a multi-risk intervention individualized to modify coronary risk factors (and fitness) and the atherosclerotic process25,26,27 The benefits of a multirisk intervention with individualized goals was demonstrated in the Stanford Coronary Risk Intervention Project25. Using a case-management model, coronary patients were treated with lifestyle interventions to goals that included exercise, weight reduction and smoking cessation and this resulted in a reduced rate of progression of angiographic disease and fewer hospitalizations at 4 yr.
In a meta-analysis by Pack et al of 35,335 cardiac patients, the effect of weight loss in cardiac patients on combined clinical outcomes of all-cause mortality, cardiovascular mortality and major cardiac adverse events was assessed28. Intentional weight loss was associated with improved combined clinical outcomes, whereas, observational or non-intentional weight loss was associated with worsening outcomes28.
Effects of “Standard Cardiac Rehabilitation” on Body Weight and Body Composition.
In the absence of a focused BWL program or a specific exercise intervention, 3 mo of CR results in minimal weight loss and modest changes in body composition. In a study of over 1300 CR participants, overall, mean weight loss after 12 wk of CR was 1.2 kg (<2%)5. However, for patients who were obese (BMI≥ 30 kg/m2), the mean weight loss was 2 kg (<3%)5. This is consistent with other studies in the CR setting in the absence of a focused approach to weight loss29–31. Of note, in the time frame after the cardiac hospitalization until starting CR, patients who underwent a surgical procedure lose more weight than medically treated patients whereas the inverse is true within CR.32
The baseline assessment of patients entering CR should include a standardized measure of height (stadiometer) and body weight on a calibrated scale (shoes off and pockets emptied) such that BMI can be calculated. Abdominal obesity should also be assessed with a standardized measure of WC as follows: The WC should be measured with a flexible tape measure directly over the skin in a horizontal plane halfway between the lowest rib and the iliac crest. The waist measurement should be recorded at the end of a normal expiration.
The quality, but not caloric quantity, of the patient’s diet can be assessed using a standardized questionnaire such as Picture Your Plate which has been validated and is considered to be a reliable dietary assessment tool for CR populations33. Additionally, documenting 3 d of food consumption can be a useful tool to assess dietary pattern.
As a prelude to this review, the authors undertook a survey to gather insight into the specific interventions employed by CR programs to facilitate weight loss. Using the American Association for Cardiovascular and Pulmonary Rehabilitation (AACVPR) program directory we emailed a 4 question survey to 99 CR programs throughout the U.S. representing 34 states. Programs were selected on a state by state basis with questionnaires sent to the first three programs for which an email address was available. A broad geographic representation was attained. The vast majority were non-academic, clinical programs with only 2 responses being returned from university hospitals. We received complete questionnaires from 36/99 (36%) These results are described in Table 2 and indicate that weight loss is not systematically addressed in most CR programs. Only 8% of programs had a formal weight loss program within CR or a hospital weight loss program to which patients could be referred. A total of 64% of programs did provide individualized nutrition counseling to patients that may have included weight control advice. Only 11% of programs knew the mean weight change of overweight/obese patients in CR, ranging from .5 to 4 kg, and only 19% oriented the exercise prescription to promote weight loss in overweight patients by maximizing caloric expenditure.
Table 2.
Survey of Current Weight Loss Practices in Cardiac Rehabilitation
| Comments | ||
|---|---|---|
| Do you have a weight loss program within CR? | 3 (8) | Two of the three were hospital-based programs |
| Does a dietician meet with patients? | 23 (64) | Not clear if dietician addressed weight loss or other issues |
| Do you know average weight change of your patients? | 4 (11) | |
| Do you advise overweight/obese patients to exercise in a certain way to assist with weight loss? | 7 (19) |
Data are presented as n (%).
Staff from 99 CR programs in 30 states were contacted, 36 surveys were returned
To measure program effectiveness, it is critically important that programs track outcomes such as body weight, BMI and waist circumference. It is important to have baseline data to assess the efficacy of any programmatic changes you may make to, thereby, assess quality improvement. In general terms, modifiable behaviors that influence weight loss for overweight/obese patients fall into two broad categories: caloric expenditure (i.e. physical activity) and caloric intake (i.e. dietary intake).
Approach to Exercise and Physical Activity
When it comes to BWL programming, CR has a unique advantage that should be leveraged. Unlike community-based BWL programs, all patients enrolling in CR understand that they are participating in an exercise program thus, they have agreed to exercise. Moreover, participants rely on the recommendation of CR professionals to establish exercising parameters. Therefore, recommendations regarding exercise and physical activity, when appropriate, should be oriented toward maximizing caloric expenditure
The standard CR exercise prescription generally includes moderate intensity exercise employing multiple modalities such as treadmill walking, cycling or rowing and strength training. This volume and intensity of exercise will increase exercise capacity in obese patients34. The caloric energy expenditure of this type of exercise (3 d/wk), however, is < 800 kcal/wk total35,36. Assuming that caloric intake remains unchanged, caloric expenditure of approximately 3500 kcal is required to lose .5 kg of body weight. Thus, expending roughly 800 kcal/week beyond baseline metabolic rate with CR exercise over 12 wk would be expected to yield a weight loss of approximately 1.5 kg over 12 wk (12 × 800 /3500). This is remarkably consistent with what was seen in CR in the study of Gomodam et al5.
Exercise, as a sole intervention, can be an effective means for slow and gradual weight loss37. To facilitate weight loss, the exercise prescription should be oriented towards maximize caloric expenditure by including nearly daily, longer distance walking. Non-weight supported exercise such as walking or elliptical expends more calories than weight supported exercise such as cycling, rowing, seated-ergometry or swimming. The duration of exercise should be gradually increased over time.
The American College of Sports Medicine (ACSM) advises that individuals should strive to get between 150 – 250 min of moderate to vigorous exercise, or 22–35 min/d each week to promote weight loss38. Also, it is acknowledged that more is better; greater than 250 min/wk of moderate to vigorous activity is associated with more substantial weight loss. Consequently, to achieve the recommended 250 min/wk requires an average of > 35 min/d. By necessity, high caloric exercise training requires that individuals perform some, if not most, of their exercise away from CR. Therefore, when it is determined to be safe and appropriate, CR professionals need to assist patients to establish a program that can be done at home. In addition to expand the volume of purposeful exercise sessions, caloric expenditure can be maximized by also taking every opportunity to increase physical activity. This can include parking further from the entrance, taking the stairs rather than elevators and walking for chores rather than driving, whenever possible.
In the CR setting, a study by Savage, et al had as its goal to increase caloric expenditure of exercise for overweight individuals without any change in diet39. Patients were counseled to gradually increase their walking up to > 60 min session as tolerated, 5–7 d/wk. After 4 mo patients lost a mean of 4.6 kg of which 3.6 kg was fat mass. This was associated with favorable effects on the lipid profile, lower insulin levels and peak aerobic capacity increased by 21%. In a study by Mertens, et al in cardiac patients, an exercise prescription of daily walking was utilized which was gradually increased from 20 to on average 43 min/d over a 3 mo period of time. The patients were followed for 9 more months with no associated dietary restriction. The mean weight loss was 4.5 kg over 1 yr and was associated with favorable risk factor benefits40.
The weight loss brought on by exercise alone is slow and gradual. For example if you increase caloric expenditure by 100 kcal/d or the equivalent of walking an extra mile per day, it will take 35 d to accomplish a caloric deficit of 3500 kcal and accomplish 1 lb of weight loss assuming that diet is kept steady. If this is maintained for a year, a 10 lbs weight loss would be accomplished. The patient should be counseled as to this pace of weight loss. For many, this pace of weight loss is too slow. Therefore, to accelerate the rate of weight loss, exercise should be combined with a hypocaloric diet (see below).
A comprehensive study of high-caloric expenditure exercise combined with a hypocaloric diet in the CR setting was published by Ades et al41. Individuals were randomized to either high caloric exercise training or standard CR exercise. Both groups received BWL dietary counseling. Patients who performed the high-caloric exercise program eventually expended 3,000–3500 kcal/wk mostly by ramping up to 45 min/d of walking, 6–7 d/wk. Over 4 mo, individuals in the high caloric exercise group lost double the weight (8.2 vs 3.7 kg) and double the fat mass (5.9 vs 2.8 kg) as participants who performed standard CR exercise. The high caloric exercise + diet group also reduced IR and the Cholesterol/HDL Cholesterol atherogenic ratio and components of the metabolic syndrome (BP, triglycerides, HDL-Chol, waist circumference, glucose) to a greater degree than the group that performed standard CR exercise + diet. The diet program used for this study was adapted from the LEARN (Lifestye, Exercise, Attitudes, Relationships, Nutrition) program42. Table 3 includes a list of the positive effects of exercise and weight loss for participants in CR43,44.
Table 3.
Beneficial Effects of Weight Loss and Exercise in Cardiac Rehabilitation
| Obesity Related Factor | Strength of Evidence * |
|---|---|
| Reduction in Obesity25,39,41,47 | + + + |
| Decrease Risk of Developing Type 2 Diabetes Mellitus17 | + + + |
| Remission of Type 2 Diabetes Mellitus19 | + |
| Decrease Fasting Glucose39,41 | + + + |
| Improve Insulin Sensitivity39,41 | + + + |
| Lower Blood Pressure41 | + + + |
| Reduction in Atrial Fibrillation Burden23 | + + |
| Improve Vascular Function43 | + + + |
| Reduction in Components of Metabolic Syndrome41 | + + + |
| Decrease Platelet Reactivity44 | + |
| Decrease Markers of Systemic Inflammation41 | + + + |
| Improve Atherogenic Ratio (Total Cholesterol/HDL-Cholesterol)41 | + + + |
Strength of scientific evidence:
+ Some evidence
+ + Moderate evidence
+ + + Strong evidence
Behavioral Weight Loss
The dietary approach to weight loss in the CR setting should be oriented toward food consumption that is hypocaloric for the duration of weight reduction. It should be a heart-healthy dietary pattern that can be sustained for a lifetime. It should emphasize fresh fruits and vegetables and the avoidance of processed foods. During the weight loss period of the program the diet needs to be hypocaloric but after a weight loss goal is achieved, caloric intake should become eucaloric to avoid weight recidivism. Continued exercise is a key to sustaining weight loss over a longer period45,46. Since the goal of the lifestyle program is to accomplish and maintain weight loss, physical activity needs to be considered as an inextricable component of a comprehensive BWL program. One can say to patients that “exercise is a part of your diet”.
Whereas the LEARN program is designed to be delivered over a 16 wk period with weekly weigh-ins and topic discussions, we have reported modifying the program in the CR setting to a 4 week program that we have found accomplishes a mean of 4.5 kg of weight loss over 3 mo32. We found that a longer program of 9 weekly sessions had a much lower attendance rates.
Weekly discussion topics are consolidated and discussed in the 4 weekly 1 hr sessions and include the topics of self-monitoring, keeping a daily calorie count, stimulus control, goal-setting and problem solving42. The sessions can be led by a registered nurse, a dietician or clinical exercise physiologist with, in each case, the individual becoming expert in delivering the LEARN program topics. The group leader facilities discussion and strategies that are used by participants to navigate eating behaviors.
Each patient is given a caloric goal of a daily caloric deficit of 500 kcal from maintenance requirements. An equation to determine an approximate maintenance daily caloric intake: multiplies body weight in lbs. by twelve42. Thus, for a 200 lb individual, daily maintenance calories would be 2400 kcal/d and a daily caloric deficit of 500 kcal would yield a targeted daily caloric goal of 1900 Kcal.
To calculate the caloric content of foods, these can be measured using phone apps such as MyFitness pal or by doing this manually in a notebook using a manual calorie and fat counter such as Calorie King47. It is key that all foods are recorded as the act of counting calories is a significant educational aspect of the intervention.
At the completion of the CR program, plans are made to outline the long term caloric goal and physical activity prescription that would be required to maintain the weight loss. Others have adapted the LEARN program to the CR setting. Aggarwal et al tested the LEARN program just after completion of 3 months of CR and found that its use was associated with 6.0 kg of weight loss over 12 wk48.
Other options besides the LEARN program are available to assist with weight loss in the CR setting and include referring patients to commercial weight loss programs such as Weight Watchers or Noom which have online programs that include monthly fees. In one study from the Netherlands, 44 patients with coronary heart disease were referred to a commercial weight loss program (Weight Watchers) concurrent with their CR program49. Thirty five patients completed the program and mean weight loss was 5.8 kg with 20 patients (57%) attaining 5% weight loss.
Smart phone applications (apps) that assist with weight loss and food logging include MyFitnessPal, Lose it!, Fitbit and others. Also available are prepared meals programs such as Nutrisystem or Jenny Craig although these need to be adapted for long term weight loss by altering inherent dietary patterns.
In terms of diet quality, the dietary patterns that are most associated with long-term health benefits for cardiac patients are the Mediterranean, DASH and Ornish diets50–52. These are not weight loss diets per se but focus on the quality of the diet. It is notable that some BWL programs focus only on calories, whereas patients with ASCVD need also to watch the quality of their dietary intake. Studies by Gardner et al of weight loss approaches followed over a year have shown that while low carbohydrate diets are effective for weight loss, so are lower fat diets53. The key is that they be hypocaloric, contain a variety of foods, avoid processed foods and simple carbohydrates and are tolerable for the long-term.
It has been shown that patients in CR who set a weight loss goal are more likely to accomplish weight loss than patients who do not 54,55. Thus, a part of the initial case manager’s evaluation should include setting a realistic weight loss goal in CR54,55.
Practical Considerations
Every CR program needs to lay out a practical, workable approach to weight reduction given their resources, staffing and patient population. Ignoring obesity in cardiac patients is not an option. Optimally, most programs can identify one staff member to become knowledgeable about the LEARN program. If that is not possible, patients should be referred either to a hospital weight loss program, a community program, such as Weight Watchers or an on-line program. Cardiac rehabilitation case managers should assess patents progress as they move through CR and their chosen approach to weight reduction. As a means of prioritizing, individuals with a BMI of ≥ 30 kg/m2 and patients with a BMI of ≥ 27 kg/m2 and associated abdominal obesity (from waist circumference) should be targeted for the BWL intervention.
While the CR setting is, in many ways, an optimal place to deliver a weight loss intervention, challenges do exist. First is the issue of patient motivation.. It is incumbent on the case manager to educate the patient about the deleterious effects of obesity and the importance of prioritizing the need for weight loss. Second, high caloric exercise training is relatively time consuming and can, thus, cause a bottleneck in the CR program when it comes to, for example, treadmill availability. Individuals need to perform much of their exercise away from CR. Tracking progress and providing guidance regarding home exercise will require logging activity (either electronically or on paper). These logs need to be reviewed systematically, requiring staff time. Traditionally, BWL sessions are delivered in a group setting. This requires additional time for both staff and patients. It can be challenging to find the resources to implement and sustain a BWL intervention, particularly when reimbursement for such services are not available.
Weight Loss Medications and Bariatric Surgery
It is beyond the purview of this review to describe the effects of weight loss medications or surgical approaches to weight loss for individuals with extreme obesity and an inability to lose weight with lifestyle programs. These approaches generally occur after a serious attempt at BWL. Pharmacologic agents indicated for weight loss include orlistat, lorcaserine, phentermine/topiramate extended release, liraglutide, diethylpropion, phentermine, benzphetamine and phendimetrazine56. Semaglutide is a very promising agent that was recently approved by the FDA for the treatment of obesity. In one recent study, after a treatment period of 68 wk, a mean weight loss of 14.9% (15.3 kg) was accomplished with 86% of individuals accomplishing ≥ 5% weight loss57.
The eligibility criteria for bariatric surgery include, BMI ≥ 40 kg/m2 or ≥ 35 kg/m2 with at least one weight-related health condition (standard conditions include coronary heart disease, diabetes, hypertension, and obstructive sleep apnea and failure at non-surgical weight loss attempts). Several types of weight loss surgeries are available and each has advantages and specific side effects. In a meta-analysis of bariatric surgery, at 1 yr weight loss ranges from 17 – 32% with high rates of resolution of diabetes and improvements in BP and lipid profiles but also high rates of early and late complications56.
The Obesity Paradox
Patients with many types of CVD may have a better prognosis if classified by BMI as overweight or obese; a phenomenon known as the obesity paradox58. This seeming paradox is due in part to the fact that underweight patients, or patients who are losing weight unintentionally, often have a worse prognosis than normal weight or overweight patients59. Furthermore, it is known that BMI is a poor assessment of body fat distribution and adiposity. When data sets of CVD patients are adjusted for waist-hip ratio (body fat distribution) or adiposity, the paradoxical relationship between BMI and CVD outcomes is eliminated60,61. Additionally, in a meta-analysis and systematic review of weight loss in 35,335 patients with coronary artery disease, intentional weight loss was associated with improved outcomes whereas observational weight loss was associated with worse outcomes28. Thus, it is evident that intentional weight loss for obese patients in CR will be associated with both improved long term clinical outcomes and ASCVD risk factors62.
SUMMARY AND FUTURE DIRECTIONS
Obesity is the “elephant in the room” in CR programs. Obesity is associated with the onset and the progression of ASCVD. However, overweight/obesity is difficult to treat and is easily ignored. While there have been relatively few studies, weight loss in the CR setting is linked to improvements in multiple ASCVD risk factors and better outcomes28, 41.
It is incumbent on all CR programs to develop an approach to weight loss that is appropriate to their size, resources and patient populations. Optimal would be the delivery of a comprehensive BWL on site. Once an in-CR weight loss program is developed it could be broadened to accept patients from the local medical community with medically-indicated weight loss, such as patients with T2DM, IR, hypertension, sleep apnea or atrial fibrillation.
If a CR program does not have the capacity or resources to develop its own BWL program, it is then important to refer patients to a dietician or a community based group weight loss program. Case managers need to make clear to individuals entering CR that managing their weight is critical due to the broad risk factor benefits.
As CR programs take on the challenge of weight reduction for overweight/obese patients, AACVPR should consider developing practice guidelines and treatment modules to assist members in their efforts at BWL. Additionally, the AACVPR database could be used to track obesity outcomes. Moreover, the presence of a BWL program should be considered an essential component of CR programming and count towards achieving program certification.
Acknowledgments
Sources of Funding:
This work was supported by National Institutes of Health Center of Biomedical Research Excellence award from the National Institute of General Medical Sciences: P20GM103644
Footnotes
Conflict of Interest:
REFERENCES
- 1.Alberti CKGM, Eckel RE, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WPT, Loria CM, Smith SC Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation: 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
- 2.Adult Obesity Facts. https://www.cdc.gov/obesity/data/adult.html.
- 3.Bray GA, Heisel WE, Afshin A, Jensen MD, Dietz WH, Long M, Kushner RK,Daniels SR,Wadden TA,Tsai AG,Hu FB,Jakicic, JM, Ryan DH,Wolfe BM,Inge TH. The Science of Obesity Management: An Endocrine Society Scientific Statement. Endocr Rev. 2018; 39: 79–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaalema DE, Savage PD, Leadholm K, Rengo J, Naud S, Priest JS, Ades PA. Clinical and Demographic Trends in Cardiac Rehabilitation: 1996–2015. J Cardiopulm Rehabil Prev. 2019;39:266–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomadam PS, Douglas CJ, Sacrinty MT, Brady MM, Paladenech CC, Robinson KC. Degree and Direction of Change of Body Weight in Cardiac Rehabilitation and Impact on Exercise Capacity and Cardiac Risk Factors. Am J Cardiol. 2016;117:580–584. [DOI] [PubMed] [Google Scholar]
- 6.Dietz WH. The response of the US Centers for Disease Control and Prevention to the obesity epidemic. Annu Rev Public Health. 2015;36:575–96. [DOI] [PubMed] [Google Scholar]
- 7.Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, Munusamy S, Smith G, Stec DE. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. Biol Chem. 2010;285:17271–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tchkonia T, Thomou T, Zhu Y, Karagiannides I, Pothoulakis C, Jensen MD, Kirkland JL Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab. 2013;17:644–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. http://www.cdc.gov/diabetes/data.
- 10. https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm.
- 11.Heymsfield SB, Wadden TA. Mechanisms, Pathophysiology, and Management of Obesity. N Engl J Med. 2017;376:254–266. [DOI] [PubMed] [Google Scholar]
- 12.Bray DeFronzo RA, Ferrannini E, Groop L, Henry RR, Herman WH, Holst JJ, Hu FB, Kahn CR, Raz I, Shulman GI, Simonson DC, Testa MA, Weiss R. Type 2 Diabetes Mellitus. Nat Rev Dis Primers. 2015;1:15–19. [DOI] [PubMed] [Google Scholar]
- 13.Galassi A, Reynolds K, He J. Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med. 2006;119:812–819. [DOI] [PubMed] [Google Scholar]
- 14.Khadanga S, Savage PD, Ades PA. Insulin Resistance and Diabetes Mellitus in Contemporary Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2016;36:331–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC Jr, Spertus JA, Fernando Costa. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: Executive Summary. Crit Pathw Cardiol. 2005;4:198–203. [DOI] [PubMed] [Google Scholar]
- 16.Weiss EP, Albert SG, Reeds DN, Kress KS, McDaniel JL, Klein S, Villareal DT. Effects of matched weight loss from calorie restriction, exercise, or both on cardiovascular disease risk factors: a randomized intervention trial. Am J Clin Nutr. 2016;104:576–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin NIH external link. New Engl J Med. 2002;346:393–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Look AHEAD Research Group* Cardiovascular Effects of Intensive Lifestyle Intervention in Type 2 Diabetes. N Engl J Med 2013; 369:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ades PA, Savage PD, Marney AM, Harvey J, Evans KA. Remission of Recently Diagnosed Type 2 Diabetes Mellitus with Weight Loss and Exercise. J Cardiopulm Rehabil Prev. 2015; 35: 193–197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 21.Appel LJ,Brands MW, Daniels SR, Karanja N, Elmer PJ, Sacks FM. Dietary Approaches to Prevent and Treat Hypertension. A Scientific Statement From the American Heart Association Hypertension 2006. 47;1:296–308. [DOI] [PubMed] [Google Scholar]
- 22.Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials Hypertension. 2003;42:878–84. [DOI] [PubMed] [Google Scholar]
- 23.Chung MK, Eckhardt LL, Chen LY, Ahmed HM, Gopinathannair R, Joglar JA, Noseworthy PA, Pack QR, Sanders P, Trulock KM; American Heart Association Electrocardiography and Arrhythmias Committee and Exercise, Cardiac Rehabilitation, and Secondary Prevention Committee of the Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; Council on Cardiovascular and Stroke Nursing; and Council on Lifestyle and Cardiometabolic Health. Lifestyle and Risk Factor Modification for Reduction of Atrial Fibrillation: A Scientific Statement From the American Heart Association. Circulation. 2020. 21;141:e750–e772. [DOI] [PubMed] [Google Scholar]
- 24.Villareal DT, Chode S, Parimi N, Sinacore DR, Hilton T, Armamento-Villareal R, Napoli N, Quall C, Shah K. Weight Loss, Exercise, or Both and Physical Function in Obese Older Adults N Engl J Med. 2011; 364: 1218–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Haskell WL, Alderman EL, Fair JM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP) Circulation. 1994. 89:975–990. [DOI] [PubMed] [Google Scholar]
- 26.DeBusk RF, Miller NH, Superko HR, Dennis CA, Thomas RJ, Lew HT, Berger WE 3rd, Heller RS, Rompf J, Gee D, Kraemer HC, Bandura A, Ghandour G, Clark M, Shah RV, Fisher L, Taylor CB. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–9. [DOI] [PubMed] [Google Scholar]
- 27.Franklin BA, Myers J, Kokkinos P. Importance of Lifestyle Modification on Cardiovascular Risk Reduction: Counseling Strategies To Maximize Patient Outcomes. J Cardiopulm Rehabil Prev. 2020;40:138–143. [DOI] [PubMed] [Google Scholar]
- 28.Pack QP, Rodriguez-Escudero JP, Thomas RJ, Ades PA, West CP, Somers VK, Lopez-Jimenez F. The prognostic importance of weight loss in coronary artery disease: a systematic review and meta-analysis. Mayo Clin Proc. 2014; 89: 1368–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bader DS, Maguire TE, Spahn CM, O’Malley CJ, Balady GJ. Clinical profile and outcomes of obese patients in cardiac rehabilitation stratified according to National Heart, Lung, and Blood Institute criteria. J Cardiopulm Rehabil. 2001;21:210–7. [DOI] [PubMed] [Google Scholar]
- 30.Brochu M, Poehlman ET, Savage P, Fragnoli-Munn K, Ross S, Ades PA. Modest effects of exercise training alone on coronary risk factors and body composition in coronary patients. J Cardiopulm Rehabil. 2000;20:180–8. [DOI] [PubMed] [Google Scholar]
- 31.Lavie CJ, Milani RV. Effects of cardiac rehabilitation and exercise training in obese patients with coronary artery disease. Chest. 1996;109:52–6. [DOI] [PubMed] [Google Scholar]
- 32.Savage PD, Lakoski SG, Ades PA. Course of body weight from hospitalization to exit from cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2013;33:274–80. [DOI] [PubMed] [Google Scholar]
- 33.Aberegg ES, Collins KK, Hinderliter JM, Smalling SL, Fung TT, Gizlice Z, Johnston LF, Ammerman AS, Keyserling TC. Validity and Reliability of a Brief Dietary Assessment Questionnaire in a Cardiac Rehabilitation Program, J Cardiopulmon Prev Rehabil. 2020;40:280–283. [DOI] [PubMed] [Google Scholar]
- 34.Braga M, Nascimento H, Pinto R, Araújo P, Nunes A, Rodrigues J, Araújo V, Parada-Pereira F, Maciel MJ, Rocha A. Benefits of Cardiac Rehabilitation in Coronary Artery Disease: Does Weight Matter ? J Cardiopulm Rehabil Prev. 2019;39:386–390. [DOI] [PubMed] [Google Scholar]
- 35.Schairer JR, Kostelnik T, Proffitt SM, Faitel KI, Windeler S, Rickman LB, Brawner CA, Keteyian SJ. Caloric expenditure during cardiac rehabilitation. J Cardiopulm Rehabil.1998;18:290–4. [DOI] [PubMed] [Google Scholar]
- 36.Savage PD, Brochu M, Scott P, Ades PA. Low caloric expenditure in cardiac rehabilitation. Am Heart J. 2000;140:527–33. [DOI] [PubMed] [Google Scholar]
- 37.Jakicic JM, Rogers RJ, Davis KK, Collins KA. Role of Physical Activity and Exercise in Treating Patients with Overweight and Obesity. Clin Chem. 2018;64:99–107. [DOI] [PubMed] [Google Scholar]
- 38.Donnelly JE, Blair SN, Jakicic JM, et al. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459–71. [DOI] [PubMed] [Google Scholar]
- 39.Savage PD, Brochu M, Poehlman ET, Ades PA. Reduction in obesity and coronary risk factors after high caloric exercise training in overweight coronary patients. Am Heart J. 2003;146:317–23. [DOI] [PubMed] [Google Scholar]
- 40.Mertens DJ, Kavanagh T, Campbell RB, Shephard RJ Exercise without dietary restriction as a means to long-term fat loss in the obese cardiac patient. J Sports Med Phys Fitness. 1998; 38:310–6. [PubMed] [Google Scholar]
- 41.Ades PA, Savage PD, Toth MJ, Harvey-Berino J, Schneider DL, Bunn JY, Audelin MC, Ludlow M. High-Caloric Expenditure Exercise: A New Approach to Cardiac Rehabilitation for Overweight Coronary Patients. Circulation. 2009;119:2671–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brownell K. The LEARN program for weight management. 10th Edition American Health Publishing Company; Dallas TX.: 2004. [Google Scholar]
- 43.Ades PA, Savage PD, Lischke S, et al. The effect of weight loss and exercise training on flow-mediated dilatation in coronary heart disease: a randomized trial. Chest. 2011;140(6):1420–1427. doi: 10.1378/chest.10-3289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Keating FK, Schneider DJ, Savage PD, Bunn JY, Harvey-Berino J, Ludlow M, Toth MJ, Ades PA. Effect of exercise training and weight loss on platelet reactivity in overweight patients with coronary artery disease. J Cardiopulm Rehabil Prev. 2013;33:371–7. [DOI] [PubMed] [Google Scholar]
- 45.Thomas JG, Bond DS, Phelan S, Hill JO, Wing RR. Weight-loss maintenance for 10 years in the National Weight Control Registry. Am J Prev Med. 2014;46:17–23 [DOI] [PubMed] [Google Scholar]
- 46.Jensen MD, Ryan DH, Donato KA, Apovian CM, Ard JD, Comuzzie AG, Hu FB, Hubbard VS,Jakicic JM, Kushner RF, Loria CM, Millen BE, Nonas CA, Pi-Sunyer FX, Stevens J, Stevens VJ, Wadden TA, Wolfe BM,Yanovski SZ. Guidelines (2013) for managing overweight and obesity in adults. Obesity 2014;22(S2):S1–S410 [Google Scholar]
- 47.CalorieKing 2019. Calorie, Fat & Carbohydrate Counter 2019 edition. Allan Borushek. CalorieKing.com [Google Scholar]
- 48.Aggarwal S, Arena R, Cuda L, Hauer T, Martin BJ, Austford L, Stone JA. The independent effect of traditional cardiac rehabilitation and the LEARN program on weight loss: a comparative analysis. J Cardiopulm Rehabil Prev. 2012;32:48–52. [DOI] [PubMed] [Google Scholar]
- 49.Minneboo M, Peters RJ, Miller-Kovach K, Lemmens J, Bucx JJ. Referral to a Commercial Weight Management Program in Patients With Coronary Heart Disease: A Pilot Study in the Netherlands. J Cardiopulm Rehabil Prev. 2015;35:268–71. [DOI] [PubMed] [Google Scholar]
- 50.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, Fiol M, Lapetra J, Lamuela-Raventos RM, Serra-Majem L, Pintó X, Basora J, Muñoz MA, Sorlí JV, Martínez JA, Fitó M, Gea A, Hernán MA, Martínez-González MA; Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. PREDIMED Study Investigators. N Engl J Med. 2018. 21;378(25):e34. [DOI] [PubMed] [Google Scholar]
- 51.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997. 17;336(16):1117–24. [DOI] [PubMed] [Google Scholar]
- 52.Ornish D, Scherwitz LW, Billings JH, Brown SE, Gould KL, Merritt TA, Sparler S, Armstrong WT, Ports TA, Kirkeeide RL, Hogeboom C, Brand RJ. Intensive lifestyle changes for reversal of coronary heart disease. JAMA. 1998;280:2001–7. [DOI] [PubMed] [Google Scholar]
- 53.Gardner CG, Trepanowski JF, Del Gobbo L, Hauser ME, Rigdon J, Ioannidis JPA, Desai M, King AC. Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association With Genotype Pattern or Insulin Secretion: The DIETFITS Randomized Clinical Trial. JAMA. 2018;319:667–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Barrett KV, Savage PD, Ades PA. Effects of Behavioral Weight Loss and Weight Loss Goal Setting in Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2020;40:383–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aspry K, Dunsiger S, Breault C, Stabile L, DeAngelis J, Wu WC. Effect of Case Management With Goal-Setting on Diet Scores and Weight Loss in Cardiac Rehabilitation Patients. J Cardiopulm Rehabil Prev. 2018;38:380–387. [DOI] [PubMed] [Google Scholar]
- 56.Turer CB Tools for Successful Weight Management in Primary Care. Am J Med Sci. 2015; 350: 485–497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, McGowan BM, Rosenstock J, Tran MTD, Wadden TA, Wharton S, Yokote K, Zeuthen N, Kushner RF; STEP 1 Study Group. Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med. 2021;384:989. [DOI] [PubMed] [Google Scholar]
- 58.Elagizi A, Kachur S, Lavie CJ, Carbone S, Pandey A, Ortega FB, Milani RV. An Overview and Update on Obesity and the Obesity Paradox in Cardiovascular Diseases. Prog Cardiovasc Dis. 2018;61:142–150 [DOI] [PubMed] [Google Scholar]
- 59.Ades PA, Savage PD. The obesity paradox: perception vs knowledge. Mayo Clin Proc. 2010. 20: 85:112–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Medina-Inojosa JR, Somers VK, Thomas RJ, Jean N, Jenkins SM, Gomez-Ibarra MA, Supervia M, Lopez-Jimenez F. Association Between Adiposity and Lean Mass With Long-Term Cardiovascular Events in Patients With Coronary Artery Disease: No Paradox. J Am Heart Assoc. 2018: 8;7:e007505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Medina-Inojosa JR, Batsis JA, Supervia M, Somers VK, Thomas RJ, Jenkins S, Grimes C, Lopez-Jimenez F. Relation of Waist-Hip Ratio to Long-Term Cardiovascular Events in Patients With Coronary Artery Disease. Am J Cardiol. 2018;12:903–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sierra-Johnson J, Romero-Corral A, Somers VK, Lopez-Jimenez F, Thomas RJ, Squires RW, Allison TG. Prognostic importance of weight loss in patients with coronary heart disease regardless of initial body mass index. Eur J Cardiovasc Prev Rehabil. 2008;15:336–40. [DOI] [PubMed] [Google Scholar]