Abstract
Rationale: Patients with asthma were advised to avoid coronavirus disease (COVID-19) and comply with medication during the COVID-19 pandemic. Respiratory tract infection is a common cause of asthma exacerbations. There has not been evidence suggesting the link between COVID-19 and asthma exacerbation, especially in places with dramatic responses in infection control with universal masking and aggressive social distancing.
Objectives: To assess the number for admissions of asthma exacerbations in January to April 2020 in Hong Kong with reference to admission in the past 5 years.
Methods: Admission records of asthma exacerbations were retrieved from the Clinical Data Analysis and Reporting System. Patients aged 18 years or older with a known history of asthma admitted for asthma exacerbation were included. Log-linear was used to model count, with year and masking used as covariate and further analysis on ambient temperature and length of hospital stays. Fisher’s exact test was used to compare the mortality rate and mechanical ventilation between the periods. Admissions for myocardial infarction, ischemic stroke, and gastric ulcer were included as controls.
Results: The number of admissions for asthma exacerbations significantly decreased by 53.2% (95% confidence interval [CI], 50.4–55.8%) in 2020 compared with monthly average admission in 2015–2019, with a higher magnitude of decrease compared with control diagnoses. Admissions for asthma exacerbations decreased by 2.0% (95% CI, 1.8–2.2%) with every 1°C (1.8°F) increase in temperature and by 0.8% with every 1% increase in masking (95% CI, 0.8–0.9%).
Conclusions: Hospitalization number for asthma exacerbations significantly decreased in early 2020, with similar length of stay. This was observed with concomitant practice of universal masking and social distancing during the COVID-19 pandemic in Hong Kong. We proposed that universal masking and social distancing reduced respiratory viral infection, leading to fewer hospital admissions for asthma exacerbations.
Keywords: asthma, COVID-19, hospitalization, masks
Coronavirus disease (COVID-19) due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections was first reported in Wuhan, China, in late 2019. Since then, this disease has been spreading rapidly around the world (1). As of January 18, 2021, more than 95-million people were infected, causing more than 2-million deaths globally.
Asthma affects approximately 339.4-million people worldwide (2), causing 495,100 deaths globally in 2017, and is ranked as the second leading cause of death from chronic respiratory disease (3). In the United States, there were approximately 12-million cases of asthma exacerbations, of which one-fourth are estimated to require hospitalization (4). The most common trigger for asthma exacerbations was viral respiratory infections (5–8). Seasonal change was reported to be associated with increased asthma exacerbations, with some studies suggesting an association between cold weather and increase in exacerbations (9, 10).
The effect of COVID-19 on asthma is still under debate. Patients with asthma requiring higher baseline use of inhaled corticosteroids, long-acting β-agonists, and long-acting anticholinergic controllers were observed to have a higher hospitalization rate for COVID-19 (11). Whether stable asthma is associated with higher COVID-19 mortality is still controversial (12), but severe asthma was associated with increased risk of mortality due to COVID-19 (13). Experts suggested that patients with asthma avoid exposure to SARS-CoV-2 virus and continue all regular medications necessary to maintain asthma control during the COVID-19 pandemic (14, 15). However, nonadherence to COVID-19 preventive measures was observed in a local study (16).
Evidence regarding asthma exacerbation–related hospital admissions in regions with wide practice of universal masking and social distancing during the COVID-19 pandemic is lacking. Universal masking and social distancing have been widely adopted by Hong Kong citizens since the first reported case of COVID-19 on January 23, 2020. According to four cross-sectional telephone self-reported surveys among the general adult population in Hong Kong by the Hong Kong Public Opinion Research Institute, the percentage of individuals wearing masks was 74.5% on January 20–23, 2020 (n = 1,008), 97.5% on February 11–14, 2020 (n = 1,000), 98.8% on March 10–19, 2020 (n = 11,449), and 99% on April 9–24, 2020 (n = 10,421) (17). Universal masking in public areas was voluntarily performed by Hong Kong citizens as a preventive measure against infection by COVID-19. Social distancing measures were voluntarily practiced by public and implemented by the government beginning January 25, 2020 and include closing schools, encouraging work from home policies, closing recreational business and bars, and banning gatherings of more than four people in public places. These infection controls were shown to associated with a relatively low rate of COVID-19 in the first 4 months of 2020 and early termination of influenza season in Hong Kong, a city with close proximity with mainland China (18). Our previous study suggested that universal masking and social distancing were associated with significant reduction in acute exacerbations of chronic obstructive pulmonary disease (COPD) in a local hospital in Hong Kong (19). In the current study, we further assessed hospitalization due to asthma exacerbations and the length of hospital stay on a territory-wide basis in Hong Kong during the COVID-19 pandemic.
Methods
This was a retrospective study to assess the number of asthma exacerbations requiring hospitalization during the period of COVID-19 in all public hospitals under the Hospital Authority in Hong Kong, with reference to and comparison with the admission number in the past 5 years. The study period was from January 1, 2020 to April 30, 2020; the World Health Organization confirmed COVID-19 infection on January 9, 2020, with the first imported case from Wuhan to Hong Kong on January 23, 2020. Data from January 2015 to December 2019 were collected for comparison. The Hospital Authority is a public organization that provides 90% of in-patient services in Hong Kong (20). The service was organized into seven healthcare regions based on geographical locations, serving the city’s population of 7.5-million people. Public hospitals under the Hospital Authority provide care to patients with COVID-19 and other acute admissions through emergency departments. The service provided by the Hospital Authority for acute admission was on the same basis during and before the COVID-19 period.
Data Source
Episode-based data were obtained by retrieval of admission records from the Clinical Data Analysis and Reporting System (CDARS) of the Hospital Authority. Principal diagnosis with an International Classification of Diseases, Ninth Edition (ICD-9), code of 493 was searched on CDARS.
Inclusion/Exclusion Criteria
Inclusion criteria include 1) age of 18 years or more, 2) known diagnosis of asthma, 3) and exacerbation of asthma. Exclusion criteria include 1) age of less than 18 years, 2) asthma with admission for causes of dyspnea other than exacerbation, 3) coexisting pulmonary diseases, including COPD (ICD-9 code 496) and bronchiectasis (ICD-9 code 494), which were identified as secondary diagnoses in CDARS. Demographic data (including age, sex, and other comorbidities) and clinical data/investigations (including date of admission, length of stay [LOS], blood culture results, sputum culture results, mechanical ventilation [ICD-9 code 96.7], and death) were collected. Patients with asthma admitted for asthma exacerbations during pregnancy (ICD-9 codes 640–649, 659, 678–679, and V22.2) were also identified.
Admission numbers of common medical problems, including myocardial infarction (ICD-9 codes 410 and 411), ischemic stroke (ICD-9 codes 433 and 434), and gastric ulcer (ICD-9 code 531), were collected as control diagnoses. These were included to evaluate the possibility of decrease in hospital attendance because of various reasons such as fear of COVID-19 infection in the hospital. The total number of visits to the emergency department and inpatient discharge and death in Hospital Authority per annum for 2015–2019 was obtained from Hospital Authority Statistical Report, which was issued in May of the following year. Influenza incidence was collated from territory-wide laboratory surveillance data for both inpatients and outpatients in both public and private medical sectors from the Centre for Health Protection, Hong Kong Special Administrative Region (HKSAR), with a relatively stable number of specimens collected over the period (18, 21). Monthly mean ambient temperature was obtained from the Hong Kong Observatory. Air quality was measured by the air quality health index (AQHI), which was calculated by the Hong Kong Environmental Protection Department on the basis of the cumulative health risk attributable to 3-hour moving average concentrations of four air pollutants (namely, ozone [O3], nitrogen dioxide [NO2], sulfur dioxide [SO2], and particulate matter [PM2.5/PM10]). It was reported on scale of 1–10 and 10+and grouped into five health risk categories (namely, low [1–3], moderate [4–6], high [7], very high [8–10], and serious [10+]); different precautionary actions were advised to groups with different susceptibility to air pollution, including those with coexisting respiratory illness, the elderly, and the general public. People with respiratory illness were advised to reduce outdoor physical exertion and to minimize their outdoor stay when the AQHI was high, very high, or serious (high to serious). The AQHI was reported hourly in 13 stations located in different areas of Hong Kong. The total number of hours with the AQHI recorded as high to serious grades were summed up and expressed as a percentage of the total number of hours collected in a month.
Statistical Analyses
For comparison of the difference in admission counts between years, log-linear modeling was used to model count, and the year was treated as a covariate in the model. Further analyses were performed on the admission counts in different healthcare regions by γ regression. Factors with possible effects on the admission counts, including ambient temperature and masking percentage, in Hong Kong were analyzed by log-linear modeling. The average monthly admission counts and the standard deviations (SDs) for asthma and other diseases in January 2015 to December 2019 (baseline period) and January 2020 to April 2020 (COVID-19 period) were compared. The masking percentage in 2015–2019 was taken as 1%, accounting for the immunocompromised patients and pregnant women. We used γ regression to compare the LOS of individuals between the two time periods, with age at admission controlled as a covariate. Two-sided tests were conducted for general difference, and we set 5% as the significance level in the analysis. Fisher’s exact test was used to compare mortality rates and mechanical ventilation. The numbers of admissions in the two time periods were classified into two categories (for mortality: death/alive or whether there is need for mechanical ventilation) and hence formed a two-by-two contingency table. The percentages of AQHI grades (high to serious) in the different periods were compared by the Wilcoxon rank-sum test. Further details of these biostatistical methods are listed in Appendix 1. The study was approved by the institutional review board of the University of Hong Kong/Hospital Authority Hong Kong West Cluster (reference number UW-20–433).
Results
In 2015 to 2019, the total number of visits to emergency departments under Hospital Authority was 10,909,767, ranging from 2,157,617 to 2,231,951 (SD, 9,453) per annum. Total in-patient discharge and death was 8,029,560, ranging from 1,153,884 to 1,819,622 (SD, 27,055) per annum.
Asthma
In the period from January 2015 to April 2020, a total of 38,325 patients were admitted to public hospitals for asthma exacerbations. The patients had a mean age of 48 years (range, 18–97 yr). Overall, 37,067 patients were admitted between January 2015 and December 2019, and 1,258 were admitted between January 2020 and April 2020. The monthly average admission was 618 ± 103 episodes in January 2015 to December 2019 and 315 ± 140 episodes in January 2020 to April 2020. A lower admission count was observed in August each year (Figures 1 and 2). Based on log-linear modeling, admission for asthma exacerbation decreased by 53.2% (95% confidence interval [CI], 50.4–55.8%; P < 0.0001) from an average of 618 admissions per month in January 2015 to December 2019 to 315 admissions per month in January 2020 to April 2020. It dropped by 51.6% (95% CI, 48.7–54.4%; P < 0.0001) when comparing January 2020 to April 2020 against January to April of 2015–2019, from an average of 652 admissions per month to 315 admissions per month. Further analysis on asthma admission numbers in different healthcare regions revealed significant reductions in 2020 across all seven healthcare regions (Figures 1A and 1B, P < 0.05 for both first 4 months in 2015–2019 vs. first 4 months in 2020 and for 2015–2019 vs. 2020 comparisons in all healthcare regions).
Figure 1.
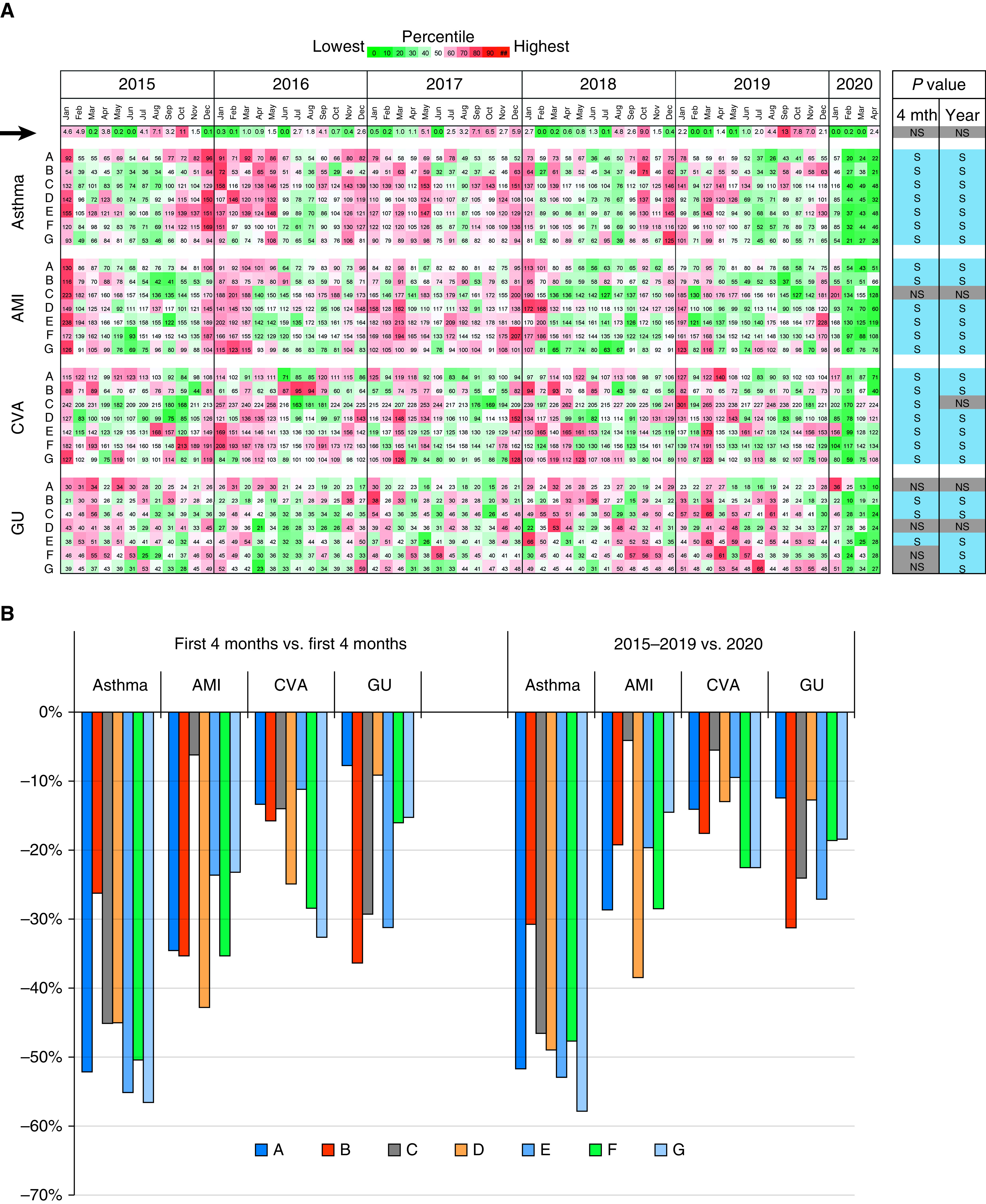
Changes in the hospital admission numbers for asthma exacerbations and control diagnoses by healthcare regions in Hong Kong, January 2015 to April 2020. (A) Heatmap of the monthly percentage of air quality health index (AQHI) with high to serious levels (black arrow) and hospital admissions for asthma, AMIs, CVAs, and GUs from January 2015 to April 2020. Letters A–G next to each diagnosis indicate the hospital admission numbers in different healthcare regions. The dates are indicated on the top panel by year and months. Heatmap illustrates the AQHI or admission data quantitatively for each row of time series. The heatmap scale above the panel shows the colors for every 10 increments in percentile from the lowest value (green) to the highest value (red). Time series that showed an S reduction (P < 0.05) in the first 4 months in 2015–2019 versus the first 4 months in 2020 (4 mth) and 2015–2019 versus 2020 (year) comparisons are illustrated by blue boxes on the right. Those with NS change were illustrated by gray boxes. (B) Percentage of reduction in admission by healthcare regions using first 4 months in 2015–2019 versus the first 4 months in 2020 and 2015–2019 versus 2020 comparisons. AMI = acute myocardial infarction; CVA = cerebrovascular accident; GU = gastric ulcer; NS = insignificant; S = significant.
Figure 2.
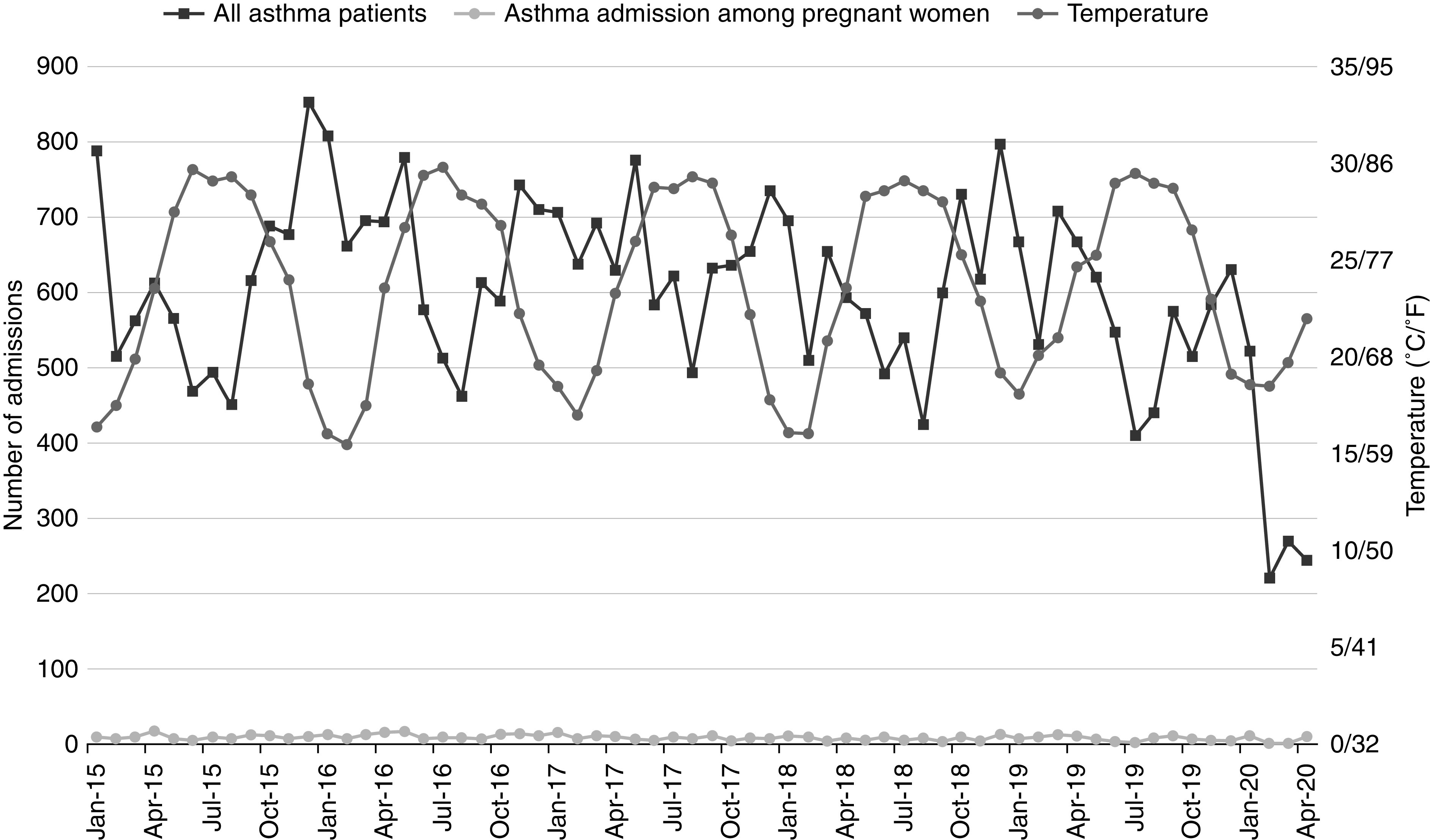
Relationship between hospital admission numbers for all patients with asthma, the subset of patients with asthma among pregnant women, and the temperature in the study period. Admission number of all patients with asthma decreased in January 2020 to April 2020 compared with the previous period (P < 0.001), whereas it was static over time among the pregnant women subset (P = 0.34)
The monthly average ambient temperature ranged from 15.5°C to 29.8°C (59.9–85.6°F), with highest temperature in June to August and the lowest temperature in January to February of each year (Figure 2). Admissions for asthma exacerbations decreased by 2.0% (95% CI, 1.8–2.2%) with each increase in 1°C (1.8°F) (P < 0.0001). The monthly percentage of the AQHI (high to serious) ranged from 0% to 13.1% (SD, 2.9%), with the worst air quality in September 2019 (Figures 1A and 3). Comparing the monthly percentage of the AQHI (high to serious) in January 2015to December 2019 or the first 4 months in 2015–2019 with January 2020 to April 2020 was statistically insignificant (P = 0.057 and P = 0.163, respectively). An increase in AQHI (high to serious) by 1% was associated with a 0.61% increase in admission (95% CI, 0.26–0.96%; P = 0.00062) (Table 1). A decrease in admissions for asthma exacerbations was observed with an increase in masking percentage. Hence, further analysis was performed on the possible relationship between the percentage of masking and asthma exacerbations. The results showed an increase of 1% in masking leads to a 0.8% fall in admissions (95% CI, 0.8–0.9%; P < 0.0001). The calculated admission dropped by 56.3% when the percentage of masking increased to 99% in April 2020 (17), whereas the calculated monthly admission dropped from 618 episodes to 271 episodes when other explanatory variables were excluded in the calculation.
Figure 3.
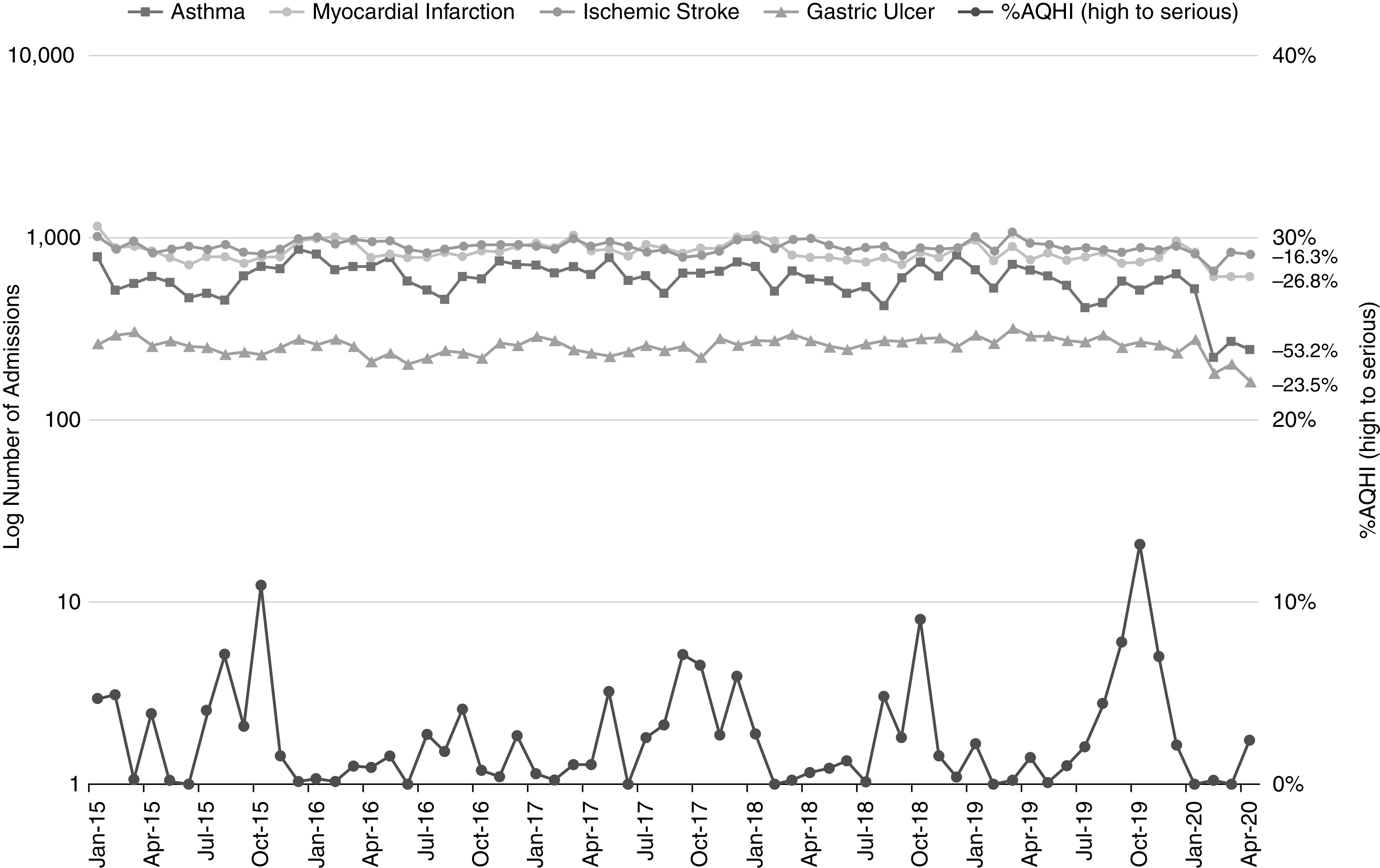
Relationship between hospital admission numbers for asthma, control diagnoses, and the monthly percentage of AQHI with high to serious levels over time. The percentage of reductions in January 2020 to April 2020 compared with 2015–2019 for the four diseases were labeled at the end of each line (P < 0.0001 for all four diseases). AQHI = air quality health index.
Table 1.
Admissions for asthma exacerbation and control diagnoses and influenza detection for different periods
| Time Period |
Estimated Decrease in Admission [%] |
Estimated Decrease in Admission with Increase of 1°C [%] | Estimated Effect on Admission with 1% Increase in High to Serious AQHI [%] |
|||||
|---|---|---|---|---|---|---|---|---|
| Only January 2020 to April 2020 (A) | Only January to April 2015–2019 (B) | All Months, 2015–2019 (C) | A vs. B | A vs. C | A vs. C | P Value | ||
| Admissions, monthly average | ||||||||
| Asthma exacerbation | 315 | 652 | 618 | 51.6* | 53.2* | 2.0* | +0.61 | 0.0062 |
| Myocardial infarction | 645 | 906 | 844 | 25.7* | 26.8* | 1.8* | +0.30 | 0.0520 |
| Cerebrovascular accident | 781 | 947 | 904 | 17.6* | 16.3* | 0.8* | −0.46 | 0.0021 |
| Gastric ulcer | 205 | 271 | 258 | 24.2* | 23.5* | 0.8* | −0.36 | 0.1970 |
| Influenza A or B detection, monthly average | ||||||||
| Number of viruses | 1,417 | 3,323 | 1,966 | 51.5* | 46.3* | — | — | — |
| Asthma exacerbation severity indicators | P value† (A vs. B) | P value† (A vs. C) | ||||||
| Length of stay, d | 3.38 | 3.63 | 3.58 | 0.0048 | 0.0072 | — | — | — |
| Mortality, % (n/total) | 0.32 (4/1,258) | 0.31 (41/13,034) | 0.35 (129/37,067) | 1 | 1 | — | — | — |
| Mechanical ventilation, % (n/total) | 1.27 (16/1,258) | 1.02 (133/13,034) | 1.10 (410/37,067) | 0.57 | 0.58 | — | — | — |
Definition of abbreviation: AQHI = air quality health index.
P value <0.0001.
Fisher exact tests.
Pregnant women were advised to wear masks in both 2015–2019 and 2020; hence, the number of asthma exacerbations in pregnancy subgroup was collected as an internal control to study the possible relationship between masking and asthma exacerbations. Asthma exacerbations in pregnant women ranged from 2 to 18 admissions per month in January 2015 to December 2019 and 1 to 11 admissions per month in January 2020 to April 2020. There was no statistically significant difference in monthly admissions between January 2015 to December 2019 and January 2020 to April 2020 or between first 4 months of 2015–2019 and the first 4 months of 2020 (P = 0.34 and P = 0.18, respectively) (Figure 2).
Further analyses were made on clinical data indicating severe asthma exacerbations, including the need for mechanical ventilation, death from asthma exacerbation and LOS. Longer LOS was observed in patients with severe asthma (22). The total number of patients requiring mechanical ventilation for asthma exacerbation was 426 during January 2015 to April 2020. The monthly average in January 2015 to December 2019 and January 2020 to April 2020 was 7 and 4, respectively (P = 1.0). The number of deaths due to asthma was 133 from January 2015 to April 2020, with 129 deaths in January 2015 to December 2019 and four in January to April 2020 and a mortality rate of 0.35% and 0.32%, respectively (P = 1.0). Monthly LOS from January 2015 to December 2019 ranged from 3.1 days to 3.4 days per patient, with an average of 3.6 days per patient, whereas that in January 2020 to April 2020 ranged from 2.9 days to 3.8 days per patient, with an average LOS of 3.4 days per patient. The LOS in January 2020 to April 2020 dropped by 11.2% (95% CI, 3.4–18.1%; P = 0.049) compared with the January 2015 to December 2019 period. Older age was associated with longer LOS, with a 1.0% increase in LOS for every 1-year increase in age (P < 0.0001) (Table 1). These findings suggested that the patients admitted in January 2020 to April 2020 had similar LOS with clinical conditions not more severe than those of the previous period.
Other Medical Diseases: Myocardial Infarction, Ischemic Stroke, and Gastric Ulcer
To evaluate the possibility of a decrease in hospital attendance because of various reasons, including fear of COVID-19 infection, admission counts for common medical diseases (namely, myocardial infarction, ischemic stroke, and gastric ulcer) in the study period were collected and analyzed. The total number of admissions for myocardial infarction was 53,302 from January 2015 to April 2020, with 50,643 admissions from January 2015 to December 2019 and 2,659 admissions from January 2020 to April 2020 (Figure 3). The monthly average admission was 844 ± 94 in January 2015 to December 2019 and 645 ± 114 in January 2020 to April 2020 (Figure 3). The average admission count in January 2020 to April 2020 decreased by 26.8% (95% CI, 23.9–29.7%; P < 0.0001) compared with that in 2015 to 2019, from 844 admissions per month for January 2015 to December 2019 to 645 admissions per month in January 2020 to April 2020. Comparing the first 4 months in 2020 with those in 2015–2019, the admission count decreased by 25.7% (95% CI, 22.7–28.7%; P < 0.0001), from 906 admissions per month to 645 admissions per month (Table 1). This was observed in all healthcare regions and was statistically significant in six of seven healthcare regions (Figures 1A and 1B). An increase in temperature by 1°C (1.8°F) was associated with a drop in admission by 1.8% (95% CI, 1.6–2.0%; P < 0.0001). The effect for AQHI was statistically insignificant (P = 0.052).
The total admission count for ischemic strokes was 57,342 in January 2015 to April 2020, with 54,218 admissions in January 2015 to December 2019 and 3,124 admissions in January 2020 to April 2020 (Figure 3). The monthly average admission in January 2015 to December 2019 and January 2020 to April 2020 was 904 ± 62 and 781 ± 84, respectively, with minimal variations between different months. The monthly average admission count in January 2020 to April 2020 decreased by 16.3% (95% CI, 13.2–19.4%; P < 0.0001) compared with January 2015 to December 2019, from 904 admissions per month to 781 admissions per month. Comparing only January to April, the average admission count decreased by 17.6% (95% CI, 14.5–20.7%; P < 0.0001), from 947 admissions per month in first 4 months in 2015–2019 to 781 admissions per month in January 2020 to April 2020 (Table 1). This phenomenon was observed in all healthcare regions and was statistically significant in six of seven healthcare regions (Figure 1).
The total admission count for gastric ulcers was 16,323 during January 2015 to April 2020. There were 15,504 and 3,124 admissions in January 2015 to December 2019 and January 2020 to April 2020, respectively. The monthly average admission count in January 2015 to December 2019 was 258 ± 24, and that in January-April 2020 was 205 ± 50 (Figure 3), with a 23.5% (95% CI, 17.9–28.8%; P < 0.0001) reduction in January 2020 to April 2020. Comparing January to April in 2015–2019 to January to April of 2020, the admission count decreased by 24.2% (95% CI, 18.5–29.6%; P < 0.0001), from 271 admissions per month to 205 admissions per month (Table 1), and was statistically significant in five of seven healthcare regions (Figure 1). Change in ambient temperature had minimal effects on ischemic stroke and gastric ulcer. An increase in temperature by 1°C (1.8°F) was associated with decrease in ischemic stroke admission by 0.8% (95% CI, 0.6–0.9%; P < 0.0001) and in gastric ulcer admission by 0.8% (95% CI, 0.5%–1.2%; P < 0.0001). An increase in the percentage of AQHI (high to serious) had a statistically insignificant effect on myocardial infarction (P = 0.052) but was associated with a decrease in ischemic stroke admission by 0.46% (95% CI, 0.17–0.75%; P = 0.0021) (Table 1 and Figures 1 and 3).
Influenza Activity and Asthma Exacerbation
The total number of patients with influenza A or B viruses detected from January 2015 to April 2020 in Hong Kong was 123,655. From January 2015 to December 2019, the monthly average of influenza A or B detection was 1,966 ± 2179. The number of patients with influenza virus peaked in the first 3 months of the year in 2015–2019, except in 2017, with a monthly average 3,958 ± 2,462. In January 2020 to April 2020, the monthly average dropped to 1,417 ± 2499 and was correlated with a decrease in asthma exacerbations (Figure 4). We observed a drastic drop in influenza incidence in April 2020, with an incidence of only 5. Influenza incidence in January 2020 to April 2020 decreased by 46.3% (95% CI, 44.9–47.7%; P < 0.0001) compared with that in January 2015 to December 2019 (Table 1 and Figure 4).
Figure 4.
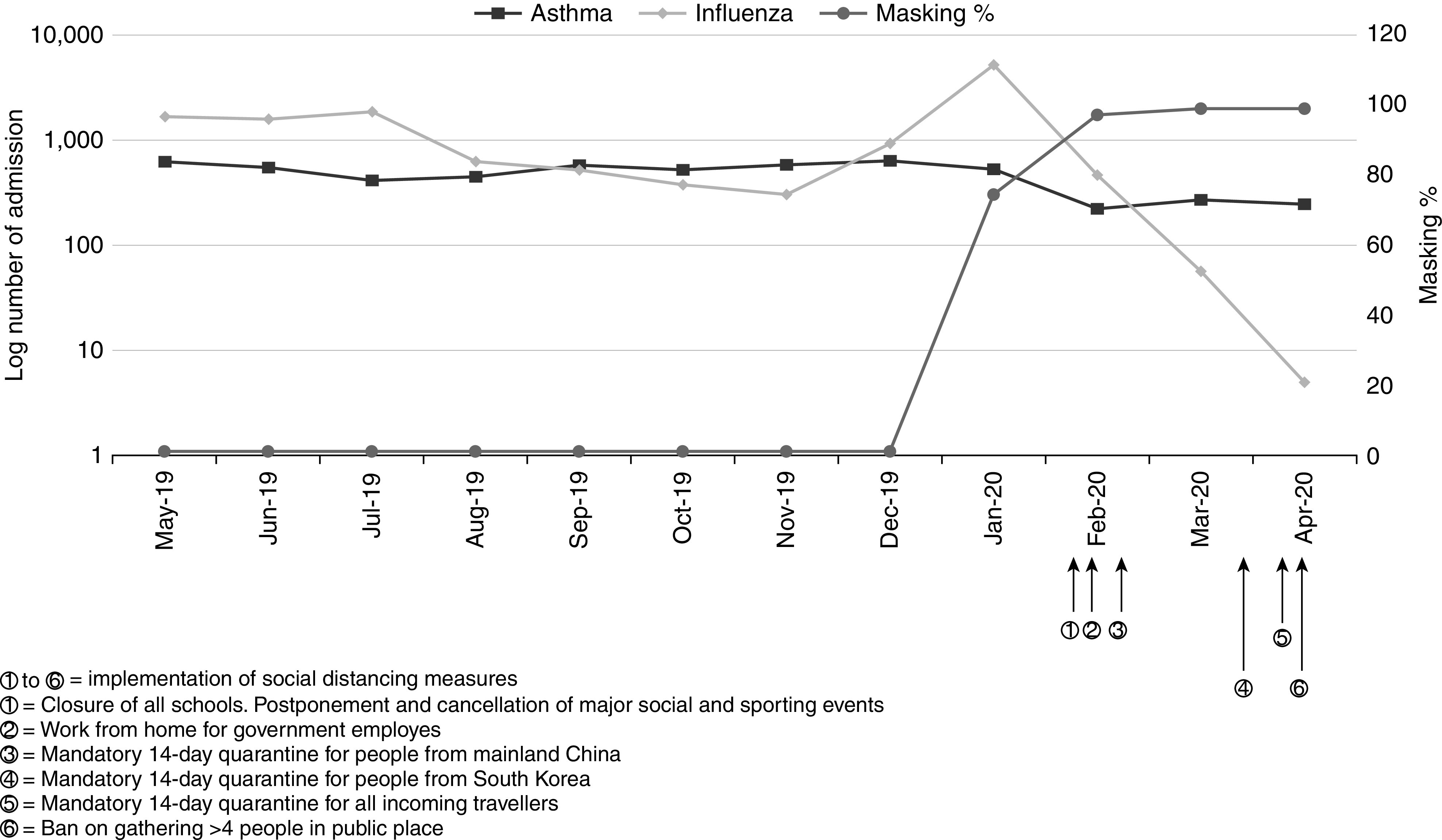
Relationship between incidence of influenza, hospital admissions for asthma, and public health actions taken to suppress coronavirus disease (COVID-19) transmission in Hong Kong. Decrease in incidence of influenza and asthma was observed with increase of masking percentage and implementation of public health measures.
Discussion
To the best of our knowledge, our study was the first to show a reduction in the number of hospital admissions for asthma exacerbations during the COVID-19 pandemic on a territory-wide basis. Hong Kong has a general population of 7.5 million, and universal masking and social distancing were widely practiced during the COVID-19 pandemic period. Compared with the admission numbers for other common medical conditions (namely, myocardial infarction, ischemic stroke, and gastric ulcer), the number of admissions for asthma decreased to a much greater extent. A decrease in acute coronary syndromes admissions was also observed in another study (23). However, our study showed a significant decrease in admissions for asthma exacerbation when compared with admissions for other common diagnoses, which could not be explained by health-seeking behavior alone. Compared with historical records, a drastic decrease in pediatric asthma–related emergency department visits was observed in two U.S. children’s hospitals (24, 25). Reasons for the observed decrease could include school closures preventing transmission of conventional respiratory viruses, reduced exposure to outdoor allergens, reductions in atmospheric pollution, and better parental supervision of asthma drugs (26).
Despite the introduction of newer therapies such as biologics and bronchial thermoplasty to prevent asthma exacerbation (27–30), the hospitalization numbers were not reduced from 2015 to 2019. Possible explanations include that biologics and bronchial thermoplasty both have stringent inclusion criteria, and the reduction in exacerbation is not absolute. Currently, omalizumab, mepolizumab, and benralizumab are available in the Hospital Authority’s drug formulary and can only be prescribed in patients with asthma with elevated IgE or eosinophilic asthma. Patients who have exacerbations can have mild asthma as well. The significant decrease in hospitalization for asthma exacerbations in early 2020 could be due to nonpharmacological interventions. The practice of wearing surgical masks was proved to have protective effects against respiratory infections and transmission (31, 32), and respiratory tract infection is a common trigger of asthma exacerbations (5–8). A high percentage of mask wearing was observed with a decrease in asthma exacerbation and influenza incidence in Hong Kong. We proposed that universal masking and social distancing have both contributed to a decrease in the transmission of respiratory tract infections and, hence, asthma exacerbations. This is supported by our results, which showed that an increase in masking of 1% leads to a 0.8% fall in admission, which is statistically significant. With the drastic increased in masking percentage in Hong Kong to 99% of the population, the admission numbers of asthma exacerbation in the territory fell drastically by 53.2% together with a fall in influenza incidence (Figure 4).
Moreover, we observed a reduction in the number of admissions for asthma exacerbations and myocardial infarctions with higher ambient temperature. This was consistent with findings of other previous studies (9, 10, 33), which may have an impact in the planning of healthcare resource utilization in Hong Kong, with an anticipated surge in admissions for asthma and myocardial infarctions in winter seasons.
Worsened air quality was associated with an increase in admission for asthma exacerbations and was statistically significant and consistent with previous findings (34, 35). The effects of air quality on myocardial infarctions and gastric ulcers were statistically insignificant. However, poor air quality had a decremental effect on cerebrovascular accident admissions, and the association was statistically significant. A possible explanation could be the relatively narrowed range in variation of percentage of AQHI (high to serious) grade (this was statistically insignificant between the two periods) together with steady admission of cerebrovascular disease.
The LOS for asthma exacerbations was shorter in 2020 compared with previous years. Increased age was also associated with a longer length of hospital stay. The need for ventilatory support and mortality both trended toward a decrease in early 2020. Longer LOS was observed in patients with severe asthma (22). However, our study showed that the LOS in 2020 was only shortened by 4.8 hours compared with all months in 2015–2019 and by 6 hours compared with January to April of 2015–2019 (Table 1). This phenomenon was observed in our study without taking account into the possible change in hospital efficiency during COVID-19 pandemics. Shortening LOS in terms of hours might not have any significance in clinical severity of the patient. However, this might reduce healthcare expenses, as the cost per patient day is $6,090 Hong Kong dollars ($785.4 U.S. dollars) in a general ward under the Hospital Authority. In our study, patients admitted for asthma exacerbations in 2020 had comparable severity with those admitted in 2015–2019. Respiratory viral and bacterial infections are important causes of asthma exacerbations and were observed in near-fatal asthma (8, 36, 37). Universal masking can prevent the transmission of respiratory viruses and hence may have a role in reducing the frequency of severe asthma exacerbations. This is further supported by the similar findings from our group that universal masking can reduce COPD exacerbations requiring hospitalization (19).
Although there were reports on collateral damage during the COVID-19 pandemic (38–40), evidence on the impact on COVID-19 on asthma was lacking, especially for places with relatively small numbers of COVID-19 cases. Hong Kong had effective infection control measures, leading to a relatively small number of COVID-19 cases in the first half of 2020. The health-seeking behavior of people in Hong Kong might be different from that in other countries, as suggested by the 25.7% reduction in myocardial infarctions in Hong Kong compared with 40% in England during the COVID-19 pandemic (23). Our study provided important information on the effects of the COVID-19 pandemic on common respiratory diseases in a city with a relatively low burden of COVID-19 and suggested that social distancing and universal masking are important low-cost measures to prevent hospitalization for asthma exacerbations that can be practiced in the future.
Limitations
This study focused on the number of admissions for asthma exacerbation. Patients with mild asthma exacerbations who were seen in primary care or did not require admission and those who attended emergency departments but were not admitted were not included in this study. However, patients with severe asthma attacks were referred to the hospital by the primary care unit and admitted on the basis of clinical need after assessment by clinicians in the emergency department. Hence, our study focused on the group of patients with asthma attacks that required hospital admission. Our study also showed that the LOS of patients was 3.63 days in 2015–2019 and 3.38 days in 2020. The number of patients requiring mechanical ventilation and mortality related to asthma exacerbations was also lower in 2020 compared with that of the past 5 years, which suggested comparable severity in patients admitted for asthma attacks in the two periods.
Moreover, this was an observational study that focused on the relationship between changes in environmental factors, including universal masking and social distancing, and hospitalizations for asthma exacerbations. Other factors, including ambient temperature and age of patients, were also taken into consideration. Our study was an ecological comparison that could not ascribe a causal relationship between wearing masks and social distancing with hospitalization for asthma. The phenomenon was observed with the possible relationship analyzed, which might or might not be accountable for the significant reduction in admission for asthma exacerbation.
Conclusions
The hospitalization number of asthma exacerbations significantly decreased in early 2020, with similar length of hospital stay. This was observed with universal masking and social distancing during the COVID-19 pandemic in Hong Kong. We proposed that universal masking and social distancing reduced respiratory viral infection and hence asthma exacerbations.
Footnotes
Supported by grants from the Consultancy Service for Enhancing Laboratory Surveillance of Emerging Infectious Disease for the HKSAR Department of Health and the Health and Medical Research Fund.
Author Contributions: K.-P.F.C. and T.-F.M. were involved in study concept and design; acquisition, analysis, and interpretation of data; drafting the work; and final approval of the manuscript. W.-C.K. was involved in acquisition, analysis, and interpretation of data; drafting the work; and final approval of the manuscript. C.-H.H., T.C.-C.T., J.K.-L.W., J.C.-M.H., D.C.-L.L., and M.S.-M.I. were involved in critical revision of manuscript for important intellectual content and final approval of the manuscript. P.-L.H. was involved in study concept and design; analysis and interpretation of data; drafting of the manuscript; critical revision of the manuscript for important intellectual content; study supervision; and approval of the final version of the manuscript.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 2.http://globalasthmareport.org/resources/Global_Asthma_Report_2018.pdf
- 3. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1736–1788. doi: 10.1016/S0140-6736(18)32203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fergeson JE, Patel SS, Lockey RF. Acute asthma, prognosis, and treatment. J Allergy Clin Immunol. 2017;139:438–447. doi: 10.1016/j.jaci.2016.06.054. [DOI] [PubMed] [Google Scholar]
- 5. Ahmed AH, Nicholson KG, Hammersley VS. The contribution of respiratory viruses to severe exacerbations of asthma in adults. Chest. 1996;109:588. doi: 10.1378/chest.109.2.588. [DOI] [PubMed] [Google Scholar]
- 6. Sokhandan M, McFadden ER, Jr, Huang YT, Mazanec MB. The contribution of respiratory viruses to severe exacerbations of asthma in adults. Chest. 1995;107:1570–1574. doi: 10.1378/chest.107.6.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Nicholson KG, Kent J, Ireland DC. Respiratory viruses and exacerbations of asthma in adults. BMJ. 1993;307:982–986. doi: 10.1136/bmj.307.6910.982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Libster R, Bugna J, Coviello S, Hijano DR, Dunaiewsky M, Reynoso N, et al. Pediatric hospitalizations associated with 2009 pandemic influenza A (H1N1) in Argentina. N Engl J Med. 2010;362:45–55. doi: 10.1056/NEJMoa0907673. [DOI] [PubMed] [Google Scholar]
- 9. Hyrkäs H, Ikäheimo TM, Jaakkola JJ, Jaakkola MS. Asthma control and cold weather-related respiratory symptoms. Respir Med. 2016;113:1–7. doi: 10.1016/j.rmed.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 10. Lam HCY, Hajat S, Chan EYY, Goggins WB., III Different sensitivities to ambient temperature between first- and re-admission childhood asthma cases in Hong Kong - a time series study. Environ Res. 2019;170:487–492. doi: 10.1016/j.envres.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 11. Wang L, Foer D, Bates DW, Boyce JA, Zhou L. Risk factors for hospitalization, intensive care, and mortality among patients with asthma and COVID-19. J Allergy Clin Immunol. 2020;146:808–812. doi: 10.1016/j.jaci.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lovinsky-Desir S, Deshpande DR, De A, Murray L, Stingone JA, Chan A, et al. Asthma among hospitalized patients with COVID-19 and related outcomes. J Allergy Clin Immunol. 2020;146:1027–1034, e4. doi: 10.1016/j.jaci.2020.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Williamson EJ, Walker AJ, Bhaskaran K, Bacon S, Bates C, Morton CE, et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020;584:430–436. doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.https://ginasthma.org/wp-content/uploads/2020/04/GINA-2020-full-report_-final-_wms.pdf
- 15. Ong KY, Tan TL, Chan AKW, Tan KLL, Koh MS. Managing asthma in the COVID19 pandemic and current recommendations from professional bodies: a review. J Asthma. doi: 10.1080/02770903.2020.1804578. [DOI] [PubMed] [Google Scholar]
- 16. Vázquez-Nava F, Vazquez-Rodriguez EM, Vazquez-Rodriguez CF, Betancourt NVO, Ruiz OC, Rodríguez-Castillejos GC. Risk factors of non-adherence to guidelines for the prevention of COVID-19 among young adults with asthma in a region with a high risk of a COVID-19 outbreak. J Asthma. doi: 10.1080/02770903.2020.1818774. [DOI] [PubMed] [Google Scholar]
- 17.Community Health Module Research Reports, Hong Kong Public Opinion Research Institute. https://www.pori.hk/research-reports
- 18. Chan KH, Lee PW, Chan CY, Lam KBH, Ho PL. Monitoring respiratory infections in covid-19 epidemics. BMJ. 2020;369:m1628. doi: 10.1136/bmj.m1628. [DOI] [PubMed] [Google Scholar]
- 19. Chan KPF, Ma TF, Kwok WC, Leung JKC, Chiang KY, Ho JCM, et al. Significant reduction in hospital admissions for acute exacerbation of chronic obstructive pulmonary disease in Hong Kong during coronavirus disease 2019 pandemic. Respir Med. 2020;171:106085. doi: 10.1016/j.rmed.2020.106085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hospital Authority (HA). Hospital authority statistical report. https://www3.ha.org.hk/data/HAStatistics/DownloadReport/2
- 21.Centre of Health Protection. https://www.chp.gov.hk/en/resources/29/304.html
- 22. Gonzalez-Barcala FJ, Calvo-Alvarez U, Salgado-Castro FJ, Facal D, Garcia-Sanz MT, Muñoz X, et al. Asthma exacerbations: factors related to longer hospital stay. Acta Clin Belg. 2017;72:379–384. doi: 10.1080/17843286.2017.1295524. [DOI] [PubMed] [Google Scholar]
- 23. Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396:381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kenyon CC, Hill DA, Henrickson SE, Bryant-Stephens TC, Zorc JJ. Initial effects of the COVID-19 pandemic on pediatric asthma emergency department utilization. J Allergy Clin Immunol Pract. 2020;8:2774–2776, e1. doi: 10.1016/j.jaip.2020.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Simoneau T, Greco KF, Hammond A, Nelson K, Gaffin JM. Impact of the COVID-19 pandemic on pediatric emergency department utilization for asthma. Ann Am Thorac Soc. doi: 10.1513/AnnalsATS.202007-765RL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gupta A, Bush A, Nagakumar P. Asthma in children during the COVID-19 pandemic: lessons from lockdown and future directions for management. Lancet Respir Med. 2020;8:1070–1071. doi: 10.1016/S2213-2600(20)30278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pavord ID, Korn S, Howarth P, Bleecker ER, Buhl R, Keene ON, et al. Mepolizumab for severe eosinophilic asthma (DREAM): a multicentre, double-blind, placebo-controlled trial. Lancet. 2012;380:651–659. doi: 10.1016/S0140-6736(12)60988-X. [DOI] [PubMed] [Google Scholar]
- 28. Ortega HG, Liu MC, Pavord ID, Brusselle GG, FitzGerald JM, Chetta A, et al. MENSA Investigators. Mepolizumab treatment in patients with severe eosinophilic asthma. N Engl J Med. 2014;371:1198–1207. doi: 10.1056/NEJMoa1403290. [DOI] [PubMed] [Google Scholar]
- 29. Castro M, Zangrilli J, Wechsler ME, Bateman ED, Brusselle GG, Bardin P, et al. Reslizumab for inadequately controlled asthma with elevated blood eosinophil counts: results from two multicentre, parallel, double-blind, randomised, placebo-controlled, phase 3 trials. Lancet Respir Med. 2015;3:355–366. doi: 10.1016/S2213-2600(15)00042-9. [DOI] [PubMed] [Google Scholar]
- 30. Bleecker ER, FitzGerald JM, Chanez P, Papi A, Weinstein SF, Barker P, et al. SIROCCO study investigators. Efficacy and safety of benralizumab for patients with severe asthma uncontrolled with high-dosage inhaled corticosteroids and long-acting β2-agonists (SIROCCO): a randomised, multicentre, placebo-controlled phase 3 trial. Lancet. 2016;388:2115–2127. doi: 10.1016/S0140-6736(16)31324-1. [DOI] [PubMed] [Google Scholar]
- 31. Offeddu V, Yung CF, Low MSF, Tam CC. Effectiveness of masks and respirators against respiratory infections in healthcare workers: a systematic review and meta-analysis. Clin Infect Dis. 2017;65:1934–1942. doi: 10.1093/cid/cix681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Cowling BJ, Zhou Y, Ip DK, Leung GM, Aiello AE. Face masks to prevent transmission of influenza virus: a systematic review. Epidemiol Infect. 2010;138:449–456. doi: 10.1017/S0950268809991658. [DOI] [PubMed] [Google Scholar]
- 33. Claeys MJ, Rajagopalan S, Nawrot TS, Brook RD. Climate and environmental triggers of acute myocardial infarction. Eur Heart J. 2017;38:955–960. doi: 10.1093/eurheartj/ehw151. [DOI] [PubMed] [Google Scholar]
- 34. Mazenq J, Dubus JC, Gaudart J, Charpin D, Viudes G, Noel G. City housing atmospheric pollutant impact on emergency visit for asthma: a classification and regression tree approach. Respir Med. 2017;132:1–8. doi: 10.1016/j.rmed.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 35. Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS One. 2015;10:e0138146. doi: 10.1371/journal.pone.0138146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tan WC, Xiang X, Qiu D, Ng TP, Lam SF, Hegele RG. Epidemiology of respiratory viruses in patients hospitalized with near-fatal asthma, acute exacerbations of asthma, or chronic obstructive pulmonary disease. Am J Med. 2003;115:272–277. doi: 10.1016/s0002-9343(03)00353-x. [DOI] [PubMed] [Google Scholar]
- 37. Puranik S, Forno E, Bush A, Celedón JC. Predicting severe asthma exacerbations in children. Am J Respir Crit Care Med. 2017;195:854–859. doi: 10.1164/rccm.201606-1213PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Tam CF, Cheung KS, Lam S, Wong A, Yung A, Sze M, et al. Impact of coronavirus disease 2019 (COVID-19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv. 2021;97:E194–E197. doi: 10.1002/ccd.28943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Masroor S. Collateral damage of COVID-19 pandemic: delayed medical care. J Card Surg. 2020;35:1345–1347. doi: 10.1111/jocs.14638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dore B. Covid-19: collateral damage of lockdown in India. BMJ. 2020;369:m1711. doi: 10.1136/bmj.m1711. [DOI] [PubMed] [Google Scholar]


