Abstract
The potential negative effects of the COVID-19 pandemic on health-compromising behaviors including overeating, processed food intake, and alcohol use have been well documented. However, it is possible the COVID-19 pandemic has had positive effects on some health-promoting behaviors like cooking and fruit and vegetable intake. The current study was a preregistered secondary data analysis using data from a U.S. national, crowdsourced study (n = 868) on eating behaviors during the early stages of the COVID-19 pandemic. The objectives of the current study were to compare levels of cooking, fruit and vegetable intake, and physical activity among U.S. adults during the early stages of the COVID-19 pandemic to pre-pandemic levels in reference groups of U.S. adults, and test whether subjective stress from the pandemic was associated with health-promoting behaviors by obesity status. During the early stages of the COVID-19 pandemic, participants cooked more often and ate 0.23 more cups of fruits and vegetables per day, but 28.8% fewer participants met federal physical activity guidelines. Greater COVID-19 stress was minimally to moderately associated with greater cooking, fruit and vegetable intake, and physical activity. The positive association between COVID-19 stress and fruit and vegetable intake was stronger for individuals with obesity. The COVID-19 pandemic might have encouraged U.S. adults, especially those at risk for complications, to engage in some health-promoting behaviors while creating barriers for other behaviors.
Keywords: COVID-19, Health-promoting behaviors, Stress
1. Introduction
The COVID-19 pandemic may be impacting how often people engage in behaviors that affect their health (Parekh & Deierlein, 2020). Several studies show that adults engaged in health-compromising behaviors like overeating, eating processed food, and drinking alcohol during the early stages of the pandemic (Ammar et al., 2020; Branley-Bell & Talbot, 2020; Buckland et al., 2021; Cherikh et al., 2020; Huber et al., 2020; Kaya et al., 2020; Robinson et al., 2021; Rolland et al., 2020). However, fewer studies have indicated whether adults shifted their engagement in health-promoting behaviors like cooking, eating fruits and vegetables, and being physically active in response to the early stages of the pandemic (Buckland et al., 2021; Flanagan et al., 2020; Gerritsen et al., 2020; Huber et al., 2020; Lamarche et al., 2021; Robinson et al., 2021). Greater engagement in health-promoting behaviors may promote resilience in face of infectious diseases like COVID-19 and prevent chronic diseases including cardiovascular disease and diabetes (Mokdad et al., 2018).
The early stages of the COVID-19 pandemic may have impacted health-promoting behaviors through multiple pathways. First, measures to reduce viral spread created new contexts for behavior. For example, social distancing could have led adults to cook and eat at home more often; yet, it may have encouraged adults to stock up on non-perishable foods at the expense of fresh produce, and may have created barriers for physical activity (e.g., gym closures) (Parekh & Deierlein, 2020). Second, there have been unprecedented subjective stress levels among adults in response to the early stages of the pandemic (American Psychologcal Association, 2020), and subjective stress is robustly associated with greater engagement in health-compromising behaviors (Siegrist & Rodel, 2006). Subjective stress may, in parallel, be associated with less engagement in health-promoting behaviors (Ng & Jeffery, 2003). Third, during the early stages of the pandemic, adults may have been more motivated to engage in health-promoting behaviors to prevent infection. This may especially be true among at-risk populations such as those with obesity (Caci et al., 2020). However, individuals with obesity may be more likely to eat in response to subjective stress (Gibson, 2012).
The current study adds to the growing empirical literature on the COVID-19 pandemic and health-promoting behaviors including cooking, fruit and vegetable intake, and exercise (Buckland et al., 2021; Flanagan et al., 2020; Gerritsen et al., 2020; Huber et al., 2020; Lamarche et al., 2021; Robinson et al., 2021). Moreover, in a majority of prior studies on the influence of the pandemic on health-compromising and health-promoting behaviors, participants retrospectively determined what their behaviors were like pre- and post-pandemic, which could introduce recall bias (Ammar et al., 2020; Branley-Bell & Talbot, 2020; Buckland et al., 2021; Cherikh et al., 2020; Flanagan et al., 2020; Huber et al., 2020; Robinson et al., 2021; Rolland et al., 2020). The potential effect of recall bias on scientific understanding of effects of the COVID-19 pandemic was recently demonstrated by a longitudinal study from January to April 2020 that found, while there were no significant changes in weight among participants, more than a quarter of participants reported they had gained weight in April 2020 (Keel et al., 2020). In the current study, we therefore used the alternative approach of comparing data from a U.S. national, crowdsourced survey on March 31st, 2020 with publicly available data collected before 2020 from reference groups of U.S. adults. On March 31st, 2020, there were 186,101 total reported cases of COVID-19 infection in the U.S., 32 states had executed statewide stay-at-home orders, and 12 states had executed partial stay-at-home orders (Centers for Disease Control and Prevention, 2020; Mervosh et al., 2020).
The current study was a secondary data analysis; the aims of the primary data analysis regarded examining the influence of the COVID-19 pandemic on health-compromising behaviors (e.g., added sugars intake) and are fully described in Cummings et al., 2021. In contrast, the aims of this secondary data analysis regarded examining the influence of the COVID-19 pandemic on health-promoting behaviors. Aim 1 was to compare levels of cooking, fruit and vegetable intake, and physical activity among U.S. adults during the COVID-19 pandemic to pre-pandemic levels. We hypothesized that U.S. adults would cook more frequently during the early stages of the pandemic; however, we hypothesized that U.S. adults would eat fewer fruits and vegetables and be less physically active. Aim 2 was to investigate associations of subjective stress from the COVID-19 pandemic with cooking, fruit and vegetable intake, and physical activity. We hypothesized that greater COVID-19 stress would be associated with less cooking, fruit and vegetable intake, and physical activity. Aim 3 was to investigate whether associations between COVID-19 stress and variables of interest would differ by obesity status; here, there was no hypothesis. Hypotheses for this secondary data analysis were preregistered separately from the primary data analysis on the Open Science Framework: https://osf.io/m3hfk.
2. Methods
The current study used data from a national, crowdsourced study on eating behaviors during the early stages of the COVID-19 pandemic (Cummings et al., 2021). Relevant details of the method are summarized below; see Cummings et al., 2021 for full details.
2.1. Participants
On March 31st, 2020, a sample of 1038 participants >18 years old, living in the U.S., and who were highly rated by other investigators (≥95% approval ratings) agreed to participate in “A Study on Beliefs about Eating and Drinking #2” in which they would “complete questionnaires that ask about your beliefs, behaviors, thoughts, and feelings related to eating and drinking” via Amazon's Mechanical Turk platform. Approval ratings represent the proportion of completed studies by an Amazon Mechanical Turk worker that have been approved by other investigators in the past. According to preregistration plans, participants were removed from final analysis if they did not follow instructions, completed the study in <3 min, reported improbable values for height/weight, or incorrectly answered quality control questions (n = 170).
The final sample comprised 868 participants (51.9% women; 71.2% White). Participants were on average 39.32 years old (SD = 12.86), and had an average body mass index (BMI) of 25.99 (SD = 5.98; 4.3% “underweight,” 45.3% “normal,” 32.9% “overweight,” and 17.4% “obese”). Education levels among participants were 0.3% < high school, 7.2% high school graduate, 17.2% some college, 11.7% associate degree, 46.2% bachelor's degree, and 17.4% advanced degree.
2.2. Procedure
The University Institutional Review Board approved the procedure in accordance with the provisions of the World Medical Association Declaration of Helsinki. Participants provided informed consent, answered questionnaires, and were compensated $1.00 for, on average, 14.63 min of their time.
2.3. Measures
Cooking. Participants reported how many times they cooked breakfast, lunch, and dinner; made a meal from fresh ingredients, packaged products, and frozen products; and used a recipe to make a meal during the past 7 days. Cooking frequency questions were modeled after questions from prior national surveys and the National Health and Nutrition Examination Survey (Wolfson et al., 2020a).
Fruit and vegetable intake. Participants reported fruit and vegetable intake (i.e., fresh, frozen, or canned fruit; salad; potatoes; beans; other vegetables; salsa; tomato sauce) in the past month via the National Cancer Institute's Dietary Screener Questionnaire (Thompson et al., 2017). Cups of fruits and vegetables/day were estimated based on publicly available scoring algorithms (Thompson et al., 2017).
Physical activity. Participants responded to: “During the past 7 days, how many days have you engaged in at least 30 min of exercise, to the point of being at least moderately out of breath?” The physical activity question was modeled after questions from the National Health Interview Survey used to calculate individuals who met federal physical activity guidelines based on moderate-intensity physical activity (Centers for Disease Control and Prevention, 2019).
Subjective stress. We modified the Impact of Event Scale – Revised, which measures subjective stress in response to a specific traumatic event (Weiss et al., 1997), to assess subjective stress in response to the ongoing COVID-19 pandemic (Cummings et al., 2021). This modification included revising the prompt to emphasize the ongoing nature of the COVID-19 pandemic and to ask participants to indicate how distressing each difficulty had been for them in the past 7 days (March 25th-March 31st); revising items to reflect the ongoing nature of the COVID-19 pandemic (e.g., “I had trouble staying asleep” was modified to “I am having trouble staying asleep”); and removing three not-applicable items (“Any reminder brought back feelings about it,” “I found myself acting or feeling like I was back at that time,” and “I tried to remove it from my memory”). Participants reported their subjective stress during the past 7 days by ranking items on a scale from 1 (“Not at all”) to 5 (“Extremely”). Sample items include, “I have been jumpy and easily startled,” “I have been thinking about it when I don't mean to,” and “I am aware that I am having a lot of feelings about it, but I have not been dealing with the feelings.” Items were averaged such that higher COVID-19 stress scores indicated greater subjective stress from the pandemic (M(SD) = 2.31(1.03), min-max = 1–5, α = 0.96).
Demographics. Participants reported their age, gender, race/ethnicity, highest education level, height, and weight.
2.4. Analytic plan & reference groups
Data are publicly available on the Open Science Framework: https://osf.io/myfts. The analytic plan for this secondary data analysis was preregistered on the Open Science Framework: https://osf.io/m3hfk. For Aim 1, we compared cooking, fruit and vegetable intake, and physical activity data to publicly available data collected before 2020 from reference groups of U.S. adults. Specifically, we used a one-sample t-test to compare the means of cooking items to those from a nationally representative sample collected in April 2015 (Wolfson et al., 2016); a one-sample t-test to compare the mean of fruit and vegetable intake to that from a recruitment-matched sample3 collected in February 2019 (Cummings et al., 2020); and a one-sample binomial test to compare the percentage of adults who met federal physical activity guidelines (≥150 min a week of moderate-intensity physical activity) to early release physical activity estimates based on data from the nationally representative National Health Interview Survey collected in 2018 (Centers for Disease Control and Prevention, 2019). We chose these reference groups because they, respectively, had completed the cooking, fruit and vegetable intake, and physical activity measures that were completed by participants in the current study and were nationally representative or recruitment-matched. The current study authors were involved with prior data collection from the cooking and fruit and vegetable intake reference groups.
The demographics of the cooking and fruit and vegetable intake reference groups are provided in Table S1 in Supplemental Materials. Details on the physical activity reference group are provided at: https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201905_tech.pdf. There were differences in age, race/ethnicity, education, and BMI between the cooking reference group and the current study sample, and there were differences in age, gender, and annual household income between the fruit and vegetable intake reference group and the current study sample (see Table S1). Therefore, in addition to conducting the Aim 1 preregistered analyses for cooking and fruit and vegetable intake, we conducted post hoc sensitivity analyses using a stepwise regression approach controlling for these differences and including a dummy code to compare between samples (0 = Reference Group, 1 = March 2020 Group).
For Aim 2, we conducted bivariate correlations among COVID-19 stress, cooking, fruit and vegetable intake, and physical activity. For Aim 3, we conducted multiple regressions predicting variables of interest from COVID-19 stress and obesity status (main effect and interaction). Obesity status was dummy coded (0 = Without obesity, 1 = With obesity).
Cooking and physical activity variables were normally distributed. The fruit and vegetable intake variable showed skew and kurtosis. We thus conducted analysis using the original and log-transformed fruit and vegetable intake variables; results were consistent across models. For ease of unit interpretation, we report estimates from analysis using the original fruit and vegetable intake variable. All analyses were conducted in SPSS Version 25 (IBM Corporation, Armonk, NY). For t-tests and multiple regressions, statistical significance was set at p < .0028 in accordance with a Bonferonni adjustment.
3. Results
3.1. Aim 1
Table 1 presents descriptives and test statistics. There were significant differences in cooking, fruit and vegetable intake, and physical activity compared to reference groups. During the pandemic, participants cooked breakfast, lunch, and dinner 0.79, 1.27, and 0.60 more times per week, respectively. Participants cooked with fresh, packaged, and frozen ingredients 1.04, 1.08, and 0.56 more times per week, respectively, and used a recipe to make a meal 1.00 more times per week. Participants ate 0.23 more cups of fruits and vegetables per day, but 28.8% fewer participants met federal physical activity guidelines. Post hoc sensitivity analyses results for cooking and fruit and vegetable intake are provided in Table S2 in Supplemental Materials; controlling for sample differences in demographics did not change the direction, magnitude, or significance patterns of the results.
Table 1.
Comparison of health-promoting behaviors among U.S. Adults in March 2020 to reference groups.
| 95% CI |
||||||
|---|---|---|---|---|---|---|
| M or % | SD | t or Z | p | Lower | Upper | |
| Cooked breakfast | 9.00 | <.001 | 0.61 | 0.96 | ||
| March 2020 | 3.59 | 2.56 | ||||
| April 2015 | 2.80 | |||||
| Cooked lunch | 15.32 | <.001 | 1.10 | 1.43 | ||
| March 2020 | 3.95 | 2.43 | ||||
| April 2015 | 2.68 | |||||
| Cooked dinner | 8.53 | <.001 | 0.46 | 0.74 | ||
| March 2020 | 5.05 | 2.05 | ||||
| April 2015 | 4.45 | |||||
| Cooked with fresh ingredients | 13.45 | <.001 | 0.89 | 1.19 | ||
| March 2020 | 3.92 | 2.27 | ||||
| April 2015 | 2.88 | |||||
| Cooked with packaged products | 15.04 | <.001 | 0.94 | 1.23 | ||
| March 2020 | 2.44 | 2.11 | ||||
| April 2015 | 1.36 | |||||
| Cooked with frozen products | 8.03 | <.001 | 0.42 | 0.70 | ||
| March 2020 | 2.79 | 2.05 | ||||
| April 2015 | 2.23 | |||||
| Used a recipe to make a meal | 12.55 | <.001 | 0.84 | 1.16 | ||
| March 2020 | 2.64 | 2.33 | ||||
| April 2015 | 1.64 | |||||
| Fruit and vegetable intake (cups/day) | 4.24 | <.001 | 0.12 | 0.34 | ||
| March 2020 | 1.88 | 1.59 | ||||
| February 2019 | 1.65 | |||||
| Physical activity (% meeting federal guidelines) | −16.93 | <.001 | 0.22 | 0.28 | ||
| March 2020 | 24.50 | |||||
| 2018 | 53.30 | |||||
Table 2 presents correlation coefficients. COVID-19 stress was significantly correlated with all variables of interest except for cooking dinner. There were small positive associations between COVID-19 stress and cooking breakfast, cooking lunch, cooking with fresh ingredients, fruit and vegetable intake, and physical activity. There were moderate positive associations between COVID-19 stress and cooking with packaged ingredients, cooking with frozen ingredients, and using a recipe to make a meal.
Table 2.
Correlations between COVID-19 stress and health-promoting behaviors among U.S. Adults in March 2020.
| 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|
| 1. COVID-19 stress | .21*** | .15*** | -.01 | .09** | .40*** | .32*** | .33*** | .12** | .09** |
| 2. Cooked breakfast | .55*** | .37*** | .35*** | .27*** | .27*** | .35*** | .22*** | .18*** | |
| 3. Cooked lunch | .45*** | .40*** | .23*** | .24*** | .33*** | .14*** | .13*** | ||
| 4. Cooked dinner | .53*** | .12** | .19*** | .28*** | .14*** | .10*** | |||
| 5. Cooked with fresh ingredients | -.01 | .13*** | .46*** | .25*** | .23*** | ||||
| 6. Cooked with packaged products | .47*** | .25*** | .17*** | .07 | |||||
| 7. Cooked with frozen products | .30*** | .14*** | .09** | ||||||
| 8. Used a recipe to make a meal | .25*** | .17*** | |||||||
| 9. Fruit and vegetable intake | .26*** | ||||||||
| 10. Physical activity |
Notes: *p < .05, **p < .01, ***p < .001.
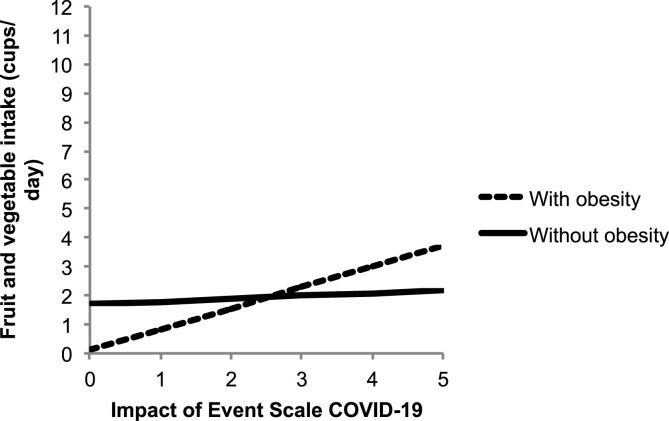
Associations of COVID-19 stress with cooking behaviors and physical activity did not significantly differ by obesity status (ps > .05). Associations between COVID-19 stress and fruit and vegetable intake did differ by obesity status [B(SE) = 0.04(0.01), p < .001, 95% CI (0.02, 0.06)]. Fig. 1 presents predicted values for fruit and vegetable intake as a function of COVID-19 stress in participants with and without obesity. For participants without obesity, the simple slope between COVID-19 stress and fruit and vegetable intake was not significant [B(SE) = 0.09(0.06), p = .088, 95% CI (−0.02, 0.21)]. For participants with obesity, there was a significant simple slope between COVID-19 stress and fruit and vegetable intake [B(SE) = 0.72(0.14), p < .001, 95% CI (0.44, 1.00)]. For each 1-unit increase in COVID-19 stress, participants with obesity ate 0.72 more cups of fruits and vegetables per day.
Fig. 1.
The predicted values for fruit and vegetable intake in March 2020 as a function of COVID-19 stress in participants with and without obesity.
4. Discussion
The current study results suggest that the early stages of the COVID-19 pandemic may have impacted engagement in health-promoting behaviors among U.S. adults. In accordance with our hypothesis, results suggest U.S. adults cooked more frequently during the early stages of the pandemic but were less physically active. More frequent engagement in cooking and less frequent engagement in physical activity may have been a byproduct of social distancing that encouraged adults to eat more often at home but created barriers for physical activity (Parekh and Deierlein, 2020). U.K. adults similarly reported they were less physically active during the government-mandated social lockdown (Robinson et al., 2021).
In contrast to our hypothesis, results suggest U.S. adults ate more fruits and vegetables during the early stages of the pandemic. Although adults may have purchased less fresh produce during the early stages of the pandemic, they may have compensated by buying more frozen/canned produce. Moreover, frequent cooking is associated with better diet quality so more frequent engagement in cooking may have prompted shifts in fruit and vegetable intake (Wolfson & Bleich, 2015). The current study finding that U.S. adults may have eaten more fruits and vegetables during the early stages of the pandemic is consistent with results from the only existing longitudinal study (to our knowledge) assessing healthy eating during the early stages of the pandemic (Lamarche et al., 2021). From June 2019–February 2020 to April–May 2020, adults in Quebec, Canada reported small but significant improvements on the Healthy Eating Index, including increased intake of vegetables (Lamarche et al., 2021). In international cross-sectional studies where participants reported on their perceptions of how their fruit and vegetable intake changed during the pandemic, 28–49% reported their intake increased but 38–56% of respondents reported it was unchanged and 11–16% reported it decreased (Buckland et al., 2021; Huber et al., 2020).
Also in contrast to our hypothesis, COVID-19 stress was minimally to moderately associated with greater cooking, fruit and vegetable intake, and physical activity. Subjective stress has been associated with less engagement in health-promoting behavior in some prior research (Ng & Jeffery, 2003). One possible explanation for the current results is that a subgroup of individuals used health-promoting behaviors to cope with their stress. Habitually active individuals do exercise more frequently in response to subjective stress (Stults-Kolehmainen & Sinha, 2013). Another possible explanation is that the effects of subjective stress on behavior may be modified by contexts like food or time availability, which were impacted by the pandemic. While practicing social distancing and staying at home, individuals may have responded to their stress by eating more of whatever food was available to them, leading them to cook more and eat more canned/frozen produce. Individuals also may have had more time to cook or exercise in response to their stress because they lost their jobs or were not commuting to work or social events. Rodent models demonstrate that the effects of stress on food intake are modified by food availability; rodents typically eat more lard or sucrose (not chow) when exposed to stressors, yet in the absence of lard or sucrose, will eat more chow when exposed to stressors (Adam & Epel, 2007). Future research in humans should translate these findings and explicitly test how contexts like food and time availability modify the relations of stress with health-compromising and health-promoting behaviors. It is also possible people ate more fruits and vegetables in addition to eating more processed food and drinking alcohol in response to subjective stress from the pandemic. One study in Bavaria found that those with increased mental stress during the pandemic reported greater increases in overall food intake (Huber et al., 2020).
People might also have been more motivated to engage in health-promoting behaviors in response to COVID-19 stress to build resilience against infection. Indeed, the current study found the link between COVID-19 stress and fruit and vegetable intake was much stronger for those with obesity; these findings are comparable to results from two other recent studies (Flanagan et al., 2020; Lamarche et al., 2021) and may reflect increased motivation among a vulnerable group (Caci et al., 2020). However, this might also reflect that those with obesity are more likely to eat in response to stress, and may have simultaneously eaten more of other foods in addition to fruit and vegetables (Gibson, 2012). International studies have shown that those with higher BMI reported greater increases in overall food intake and appetitive drive in response to the pandemic (Buckland et al., 2021; Huber et al., 2020; Robinson et al., 2021). It will be important for future research to explore whether health motivations mediate associations between stress and engagement in health-promoting behaviors, especially among those with obesity.
Although levels of health-promoting behaviors during the early stages of the pandemic were compared to pre-pandemic levels in reference groups to limit recall bias, sample differences might explain the current study results. The current study sample was not nationally representative whereas the reference groups for cooking and physical activity were. However, we recruited participants through Amazon's Mechanical Turk, which is a national, crowdsourced platform, and several studies document that recruiting participants through this platform versus traditional methods (e.g., department subject pools, other Internet panel samples) results in more demographically varied participants (Berinsky et al., 2012). The gender and race breakdown of the current study sample is fairly consistent with U.S. census estimates (United States Census Bureau, 2020). Due to data availability, we were able to conduct post hoc sensitivity analysis comparing cooking and fruit and vegetable intake between the current study sample and the reference groups using a regression controlling for sample differences in demographics. Results were consistent with the alternative approach. Overall, the current study methods improve the existing literature on the COVID-19 pandemic and health-promoting behaviors by limiting recall bias, but future research should nonetheless recruit more representative samples or use repeated measures designs.
Associations between COVID-19 stress and variables of interest were cross-sectional so causal conclusions about the effect of COVID-19 stress on health-promoting behaviors cannot be inferred from this study. In assessing cooking in the current study, the healthiness of the foods that participants cooked was not assessed. Although greater cooking frequency has been associated with better diet quality in multiple studies (Mills et al., 2017; Taillie & Poti, 2017; Wolfson et al., 2020b), participants in the current study may have cooked nutrient-poor foods. In addition, the current study methods preclude investigating whether health benefits of pandemic-driven increases in cooking and fruit and vegetable intake are negated by potentially simultaneous increases in health-compromising behavior. Future research should consider approaches like administering comprehensive dietary intake measures and calculating summative diet scores (e.g., Healthy Eating Index) as well as measuring health outcomes (e.g., disease diagnosis) to examine the net effect of pandemic-driven behavior on health. It is also important to note that the data for this study were collected at one time point early on in the COVID-19 pandemic. As the pandemic and the associated stressors have evolved and circumstances have changed over time, it is unknown whether the associations we observed in this study have remained. It will be important for additional research to examine subjective stress levels and their role in shaping Americans’ behavior as the pandemic continues.
Focusing on the impact of the COVID-19 pandemic on health-promoting behaviors may shed light on beneficial effects of the pandemic in addition to health-compromising effects. The current study results suggest that the unique circumstances of the pandemic might have encouraged U.S. adults to cook more frequently and eat more fruits and vegetables while creating barriers for physical activity. Work of this kind is important given the broad impacts of health-promoting behavior (Mokdad et al., 2018).
Ethical statement
The University Institutional Review Board approved the procedure in accordance with the provisions of the World Medical Association Declaration of Helsinki.
Declaration of competing interest
None.
Acknowledgements
Financial support: The Eunice Kennedy Shriver National Institute of Child Health and Human Development provided funds for the present research and supported Jenna R. Cummings (T32HD079350, Intramural Research Program). The National Institutes of Diabetes and Digestive And Kidney Diseases supported Julia A. Wolfson (K01DK119166). These funding agencies had no role in the design, analysis, or writing of this article.
Footnotes
In February 2019, we conducted a national, crowdsourced survey in which we measured fruit and vegetable intake with the National Cancer Institute's Dietary Screener Questionnaire. We used a near-identical recruitment procedure, recruiting participants >18 years old, living in the U.S., and with ≥95% approval ratings to participate in “A Study on Beliefs about Eating and Drinking” in which they would “complete questionnaires that ask about your beliefs, behaviors, thoughts, and feelings related to eating and drinking” via Amazon's Mechanical Turk platform.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.appet.2021.105659.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Adam T.C., Epel E.S. Stress, eating and the reward system. Physiology & Behavior. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- American Psychologcal Association . 2020. Stress in the time of COVID-19: Volume one.https://www.apa.org/news/press/releases/stress/2020/report (Accessed 10 August 2020) [Google Scholar]
- Ammar A., Brach M., Trabelsi K., et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients. 2020;12:1583. doi: 10.3390/nu12061583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berinsky A.J., Huber G.A., Lenz G.S. Evaluating online labor markets for experimental research: Amazon. com's Mechanical Turk. Political Analysis. 2012;20(3):351–368. [Google Scholar]
- Branley-Bell D., Talbot C.V. Exploring the impact of the COVID-19 pandemic and UK lockdown on individuals with experience of eating disorders. Journal of Eating Disorders. 2020 doi: 10.1186/s40337-020-00319-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckland N.J., Swinnerton L.F., Ng K., Price M., Wilkinson L.L., Myers A., Dalton M. Susceptibility to increased high energy dense sweet and savoury food intake in response to the COVID-19 lockdown: The role of craving control and acceptance coping strategies. Appetite. 2021 Mar 1;158:105017. doi: 10.1016/j.appet.2020.105017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caci G., Albini A., Malerba M., Noonan D.M., Pochetti P., Polosa R. COVID-19 and obesity: Dangerous liasons. Journal of Clinical Medicine. 2020;9(8):2511. doi: 10.3390/jcm9082511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Previous U.S. COVID-19 case data. https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/previouscases.html Retrieved June 19th, 2020 from.
- Centers for Disease Control and Prevention . 2019. Early release of selected estimates based on data from the 2018 National Health Interview Survey.https://www.cdc.gov/nchs/nhis/releases/released201905.htm#7A accessed. [Google Scholar]
- Cherikh F., Frey S., Bel C., Attanasi G., Alifano M., Ianneli A. Behavioral food addiction during lockdown: Time for awareness, time to prepare the aftermath. Obesity Surgery. 2020 doi: 10.1007/s11695-020-04649-3. Published online: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J.R., Ackerman J.M., Wolfson J.A., Gearhardt A.N. COVID-19 stress and eating and drinking behaviors in the United States during the early stages of the pandemic. Appetite. 2021;162:105163. doi: 10.1016/j.appet.2021.105163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings J.R., Joyner M.A., Gearhardt A.N. Development and preliminary validation of the anticipated effects of food scale. Psychology of Addictive Behaviors. 2020;34(2):403–413. doi: 10.1037/adb0000544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan E.W., Beyl R.A., Fearnbach S.N., Altazan A.D., Martin C.K., Redman L.M. The impact of COVID‐19 stay‐at‐home orders on health behaviors in adults. Obesity. October 2020 doi: 10.1002/oby.23066. Published online: 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerritsen S., Egli V., Roy R., Haszard J., Backer C.D., Teunissen L., Cuykx I., Decorte P., Pabian S., Van Royen K., Te Morenga L. Seven weeks of home-cooked meals: Changes to New Zealanders' grocery shopping, cooking and eating during the COVID-19 lockdown. J R Soc N Z. Published online. 16 November 2020 doi: 10.1080/03036758.2020.1841010. [DOI] [Google Scholar]
- Gibson E.L. The psychobiology of comfort eating: Implications for neuropharmacological interventions. Behavioural Pharmacology. 2012;23(5–6):442–460. doi: 10.1097/FBP.0b013e328357bd4e. [DOI] [PubMed] [Google Scholar]
- Huber B.C., Steffen J., Schlichtiger J., Brunner S. Altered nutrition behavior during COVID-19 pandemic lockdown in young adults. European Journal of Nutrition. 2020 doi: 10.1007/s00394-020-02435-6. Dec 1:1-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaya S, Uzdil Z, Çakroğlu FP. Evaluation of the effects of fear and anxiety on nutrition during the COVID-19 Pandemic in Turkey. Public Health Nutr. Published online: 25 September 2020. doi: 10.1017/S1368980020003845. [DOI] [PMC free article] [PubMed]
- Keel P.K., Gomez M.M., Harris L., Kennedy G.A., Ribeiro J., Joiner T.E. Gaining “The Quarantine 15:” perceived versus observed weight changes in college students in the wake of COVID-19. Int J Eat. 2020;53(11):1801–1808. doi: 10.1002/eat.23375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamarche B., Brassard D., Lapointe A., Laramée C., Kearney M., Côté M., Bélanger-Gravel A., Desroches S., Lemieux S., Plante C. Changes in diet quality and food security among adults during the COVID-19–related early lockdown: Results from NutriQuébec. American Journal of Clinical Nutrition. 2021 doi: 10.1093/ajcn/nqaa363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mervosh S., Lu D., Swales V. https://www.nytimes.com/interactive/2020/us/coronavirus-stay-at-home-order.html?action=click&module=Top Stories&pgtype=Homepage See which states and cities have told residents to stay home. Retrieved March 31st, 2020 from.
- Mills S., Brown H., Wrieden W., White M., Adams J. Frequency of eating home cooked meals and potential benefits for diet and health: Cross-sectional analysis of a population-based cohort study. International Journal of Behavioral Nutrition and Physical Activity. 2017 Dec;14(1) doi: 10.1186/s12966-017-0567-y. 1-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A.H., Ballestros K., Echko M., Glenn S., Olsen H.E., Mullany E., et al. The state of US health, 1990-2016: Burden of diseases, injuries, and risk factors among US states. Journal of the American Medical Association. 2018;319(14):1444–1472. doi: 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng D.M., Jeffery R.W. Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology. 2003;22(6):638. doi: 10.1037/0278-6133.22.6.638. [DOI] [PubMed] [Google Scholar]
- Parekh N, Deierlein A. Health behaviors during the COVID-19 pandemic: Implications for obesity. Public Health Nutr. Published online: 4 August 2020. doi: 10.1017/S1368980020003031. [DOI] [PMC free article] [PubMed]
- Robinson E., Boyland E., Chisholm A., Harrold J., Maloney N.G., Marty L., Mead B.R., Noonan R., Hardman C.A. Obesity, eating behavior and physical activity during COVID-19 lockdown: A study of UK adults. Appetite. 2021 Jan 1;156:104853. doi: 10.1016/j.appet.2020.104853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rolland B., Haesebaert F., Zante E., Benyamina A., Haesebaert J., Franck N. Global changes and factors of increase in caloric/salty food, screen, and substance use, during the early COVID-19 containment phase in France: A general population online survey. JMIR Public Health and Surveill. 2020;6(3) doi: 10.2196/19630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegrist J., Rodel A. Work stress and health risk behavior. Scandinavian Journal of Work, Environment & Health. 2006;32(6):473–481. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- Stults-Kolehmainen M., Sinha R. The effects of stress on physical activity and exercise. Sports Medicine. 2013;44(1) doi: 10.1007/s40279-013-0090-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taillie L.S., Poti J.M. Associations of cooking with dietary intake and obesity among supplemental nutrition assistance program participants. American Journal of Preventive Medicine. 2017 Feb 1;52(2):S151–S160. doi: 10.1016/j.amepre.2016.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson F.E., Midthune D., Kahle L., Dodd K.W. Development and evaluation of the national cancer institute's dietary screener questionnaire scoring algorithms. Journal of Nutrition. 2017;147(6):1226–1233. doi: 10.3945/jn.116.246058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau QuickFacts. https://www.census.gov/quickfacts/fact/table/US/PST045219
- Weiss D.S., Marmar C.R. In: Assessing psychological trauma and PTSD: A practitioner's handbook. Wilson J.P., Keane T.M., editors. Gulford Press; New York: 1997. The impact of event scale - revised; pp. 399–411. [Google Scholar]
- Wolfson J.A., Bleich S.N. Is cooking at home associated with better diet quality and weight loss intention? Public Health Nutrition. 2015;18(8):1397–1406. doi: 10.1017/S1368980014001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Clegg Smith K., Frattaroli S., Bleich S.N. Public perceptions of cooking and the implications for cooking behaviour in the USA. Public Health Nutrition. 2016;19(9):1606–1615. doi: 10.1017/S1368980015003778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Lahne J., Raj M., Insolera N., Lavelle F., Dean M. Food agency in the United States: Associations with cooking behavior and dietary intake. Nutrients. 2020;12(3):877. doi: 10.3390/nu12030877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolfson J.A., Leung C.W., Richardson C.R. More frequent cooking at home is associated with higher Healthy Eating Index-2015 score. Public Health Nutrition. 2020 Sep;23(13):2384–2394. doi: 10.1017/S1368980019003549. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.