In April 2020, the American Heart Association (AHA) Emergency Cardiovascular Care (ECC) Committee and Get With The Guidelines-Resuscitation Adult and Pediatric Task Forces published their Interim Guidance for Basic and Advanced Cardiac Life Support in Adults, Children, and Neonates With Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) at the start of the SARS-CoV-2 pandemic. In October 2020, the AHA published new cardiopulmonary resuscitation (CPR) guidelines with the latest evidence-based algorithms and recommendations for Basic Life Support, Advanced Cardiac Life Support, Pediatric Advanced Life Support, Neonatal Advanced Life Support, and Maternal Cardiac Arrest Resuscitation.1
As the COVID-19 pandemic continues into 2021 and beyond, there is now a more accurate understanding of the transmissibility of SARS-CoV-2, a stabilizing of personal protective equipment (PPE) availability, and widespread vaccination of health care providers and some communities prompting the committee and task forces to update the initial interim guidance.2 Both nationally and internationally, the prevalence of COVID-19 and variants, vaccination, and risk of transmission are variable, and individual systems and settings can utilize this guidance to match local risk. While the initial interim guidance was focused on the use of PPE, as well as early intubation and control of the airway to decrease potential transmission risk to medical personnel, the updated 2021 interim guidance now aligns with the 2020 AHA guidelines for CPR and ECC with the provision of appropriate PPE usage and aerosol control for suspected and confirmed COVID-19 patients in settings where vaccinations have been readily adopted.
International data early during the COVID-19 pandemic described worse survival outcomes for both out-of-hospital and in-hospital cardiac arrests compared with prior years.3–6 This worsening of outcomes may have been multifactorial; the severity of SARS-CoV-2–related cardiac arrest, the implementation of termination of resuscitation guidance, local crisis standards of care, or patient hesitancy to seek medical care contributing to delays in care.7 The provision of prompt chest compressions and defibrillation may also have been delayed due to the additional time required in donning PPE or securing the airway, and the PPE may have accelerated rescuer fatigue resulting in decreased CPR quality.8,9 Concerns that resuscitation from cardiac arrest due to COVID-19 may be futile may have led to earlier termination of resuscitative efforts, and overwhelmed Emergency Medical Services systems may have had insufficient resources to respond to increased number of calls for arrests in regions with high rates of COVID-19.3,10,11 Lastly, significant delays in presentation for medical care, such as a tripling of the time from onset of chest pain to presentation to emergency care, may have contributed to an increase in out-of-hospital cardiac arrests rates during the pandemic as compared with before the pandemic.12
With increased scientific knowledge, a more stable PPE supply chain, and vaccination of frontline health care providers and the general public, application of the best resuscitation science available must be once again assessed and prioritized. The following guidance should be applied to patients with suspected or confirmed COVID-19 infection (Figures 1 through 8). The standard 2020 CPR algorithms and recommendations for resuscitation should apply to those patients who are known to be COVID-19 negative.
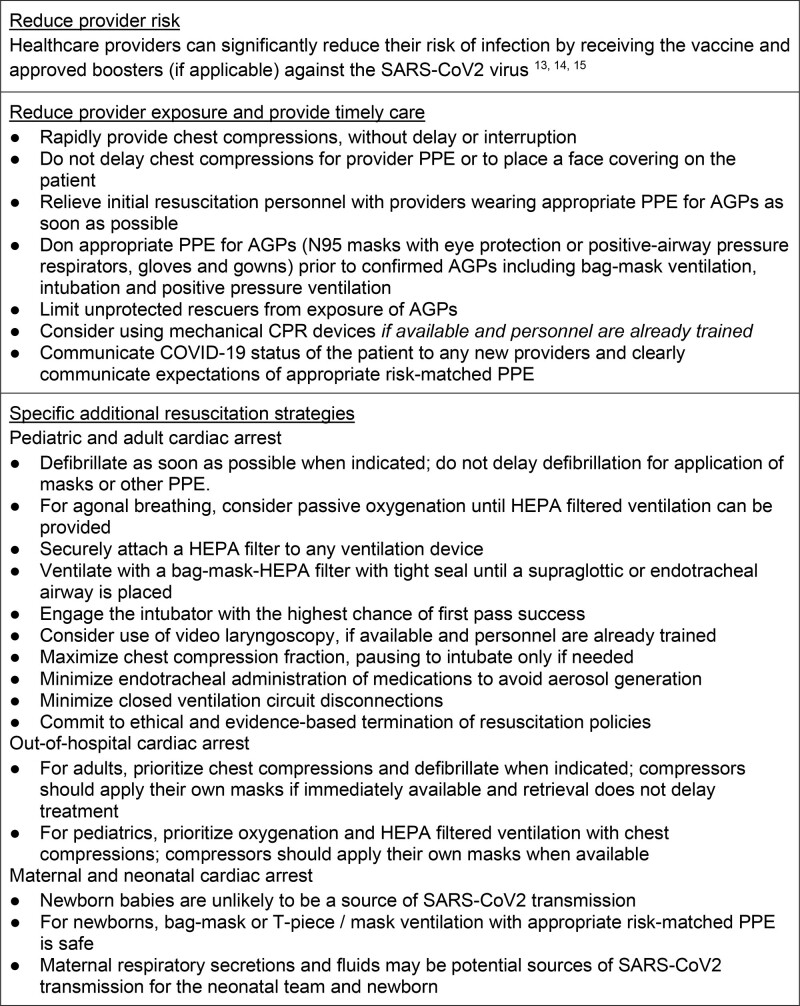
Figure 1.
Summary of adjustments to cardiopulmonary resuscitation (CPR) algorithms in patients with suspected or confirmed coronavirus disease 2019 (COVID-19).13–15 AGP indicates aerosol generating procedure; HEPA, high efficiency particulate air; PPE, personal protective equipment; and SARS-CoV-2, severe acute respiratory syndrome coronovirus 2.
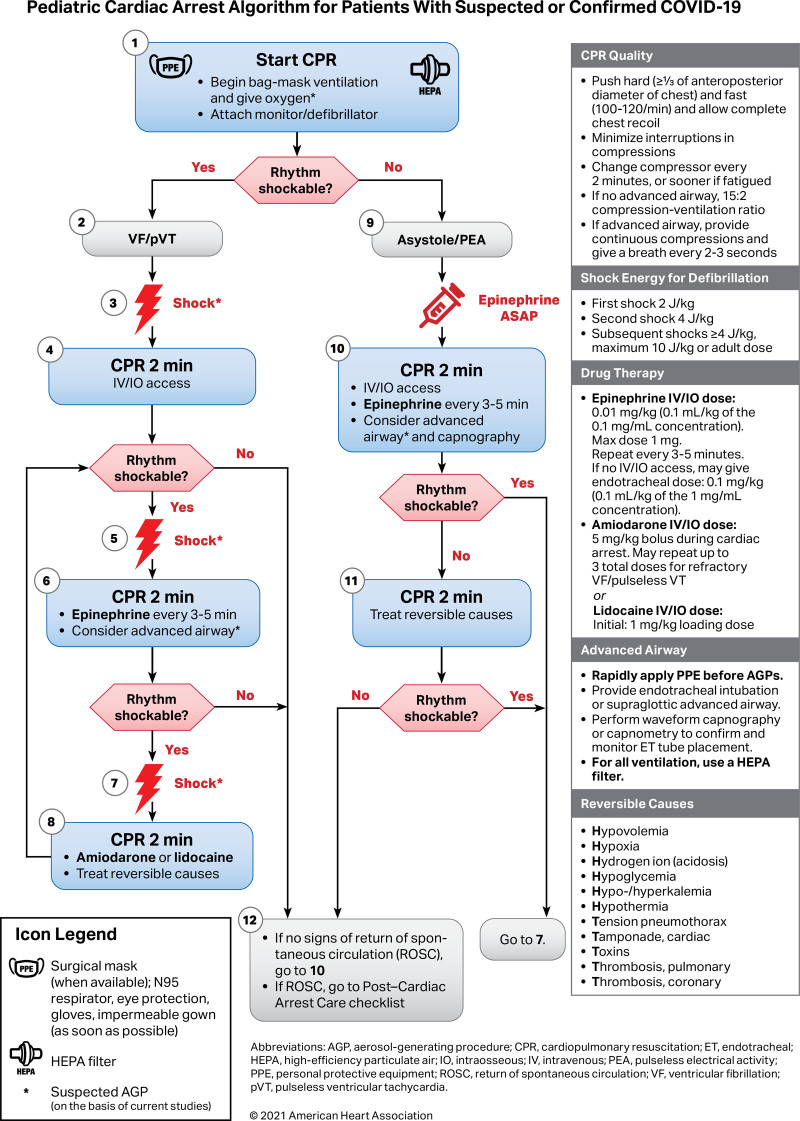
Figure 8.
Pediatric cardiac arrest algorithm for patients with suspected or confirmed coronavirus disease 2019 (COVID-19).
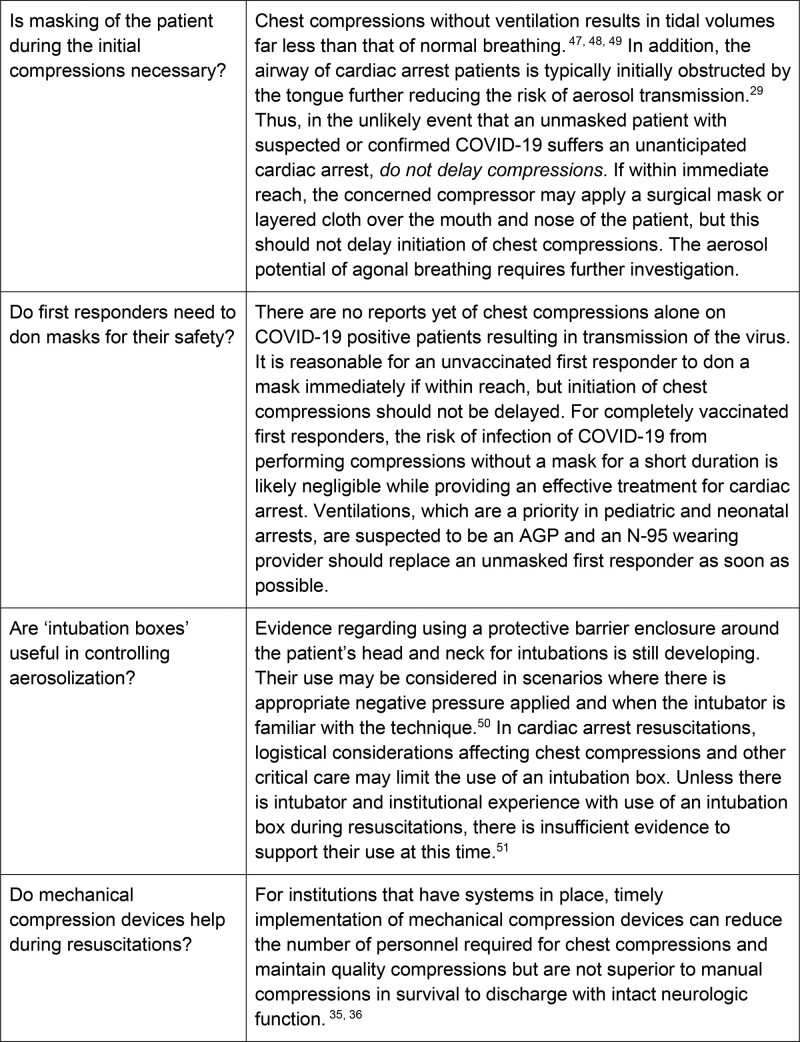
Figure 2.
Frequently asked questions. AGP indicates aerosol generating procedure; and COVID-19, coronavirus disease 2019.
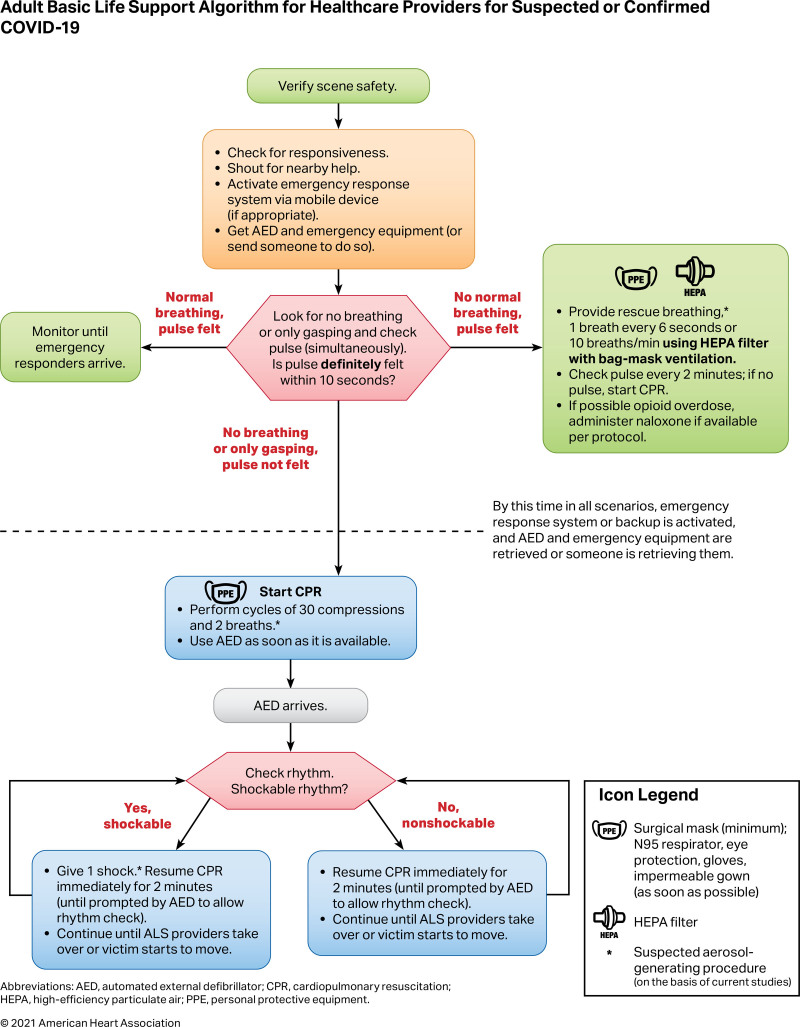
Figure 3.
Adult basic life support algorithm for health care providers for suspected or confirmed coronavirus disease 2019 (COVID-19).
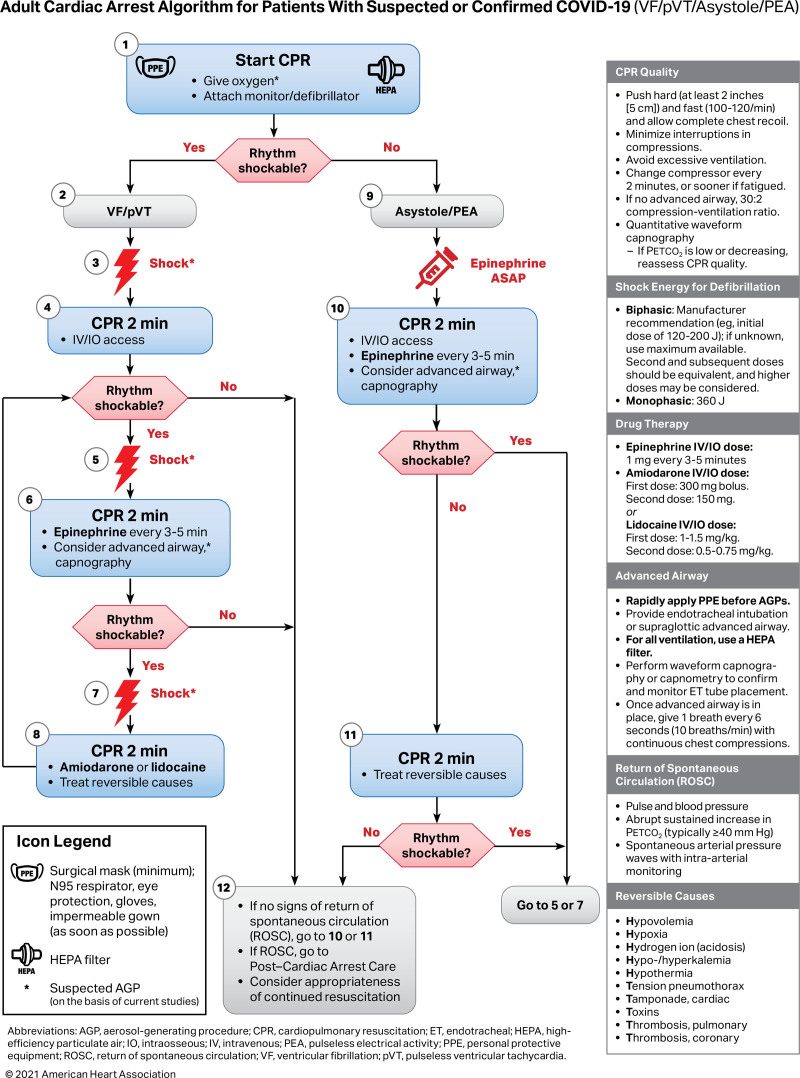
Figure 4.
Adult cardiac arrest algorithm for patients with suspected or confirmed coronavirus disease 2019 (COVID-19; VF/pVT/asystole/PEA).
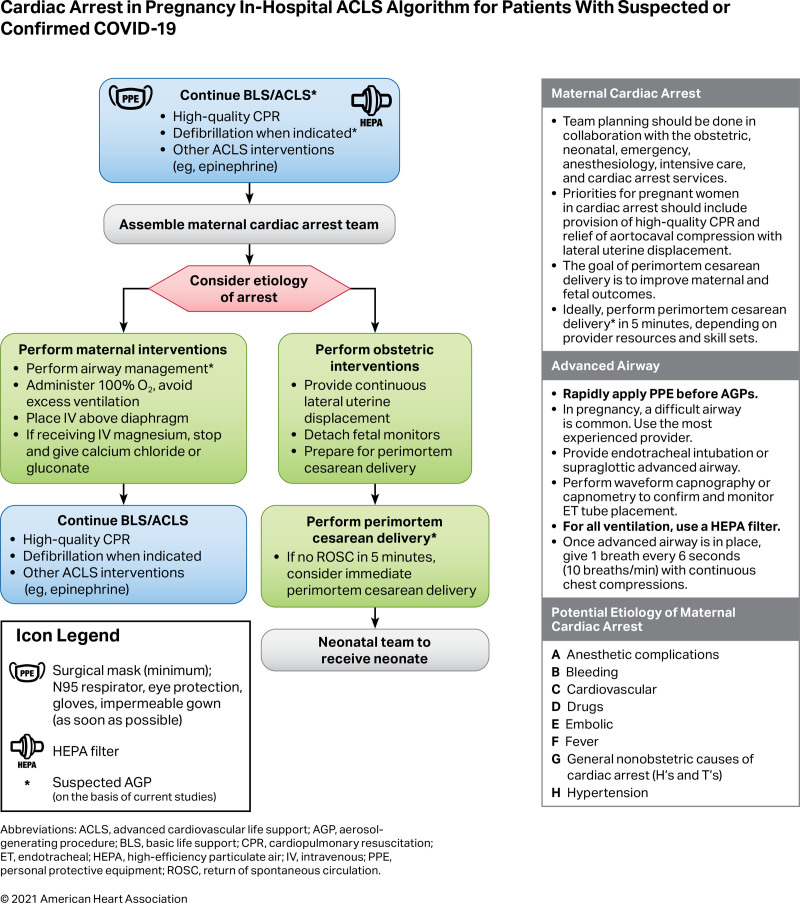
Figure 5.
Cardiac arrest in pregnancy in-hospital Advanced Cardiac Life Support (ACLS) algorithm for patients with suspected or confirmed coronavirus disease 2019 (COVID-19).
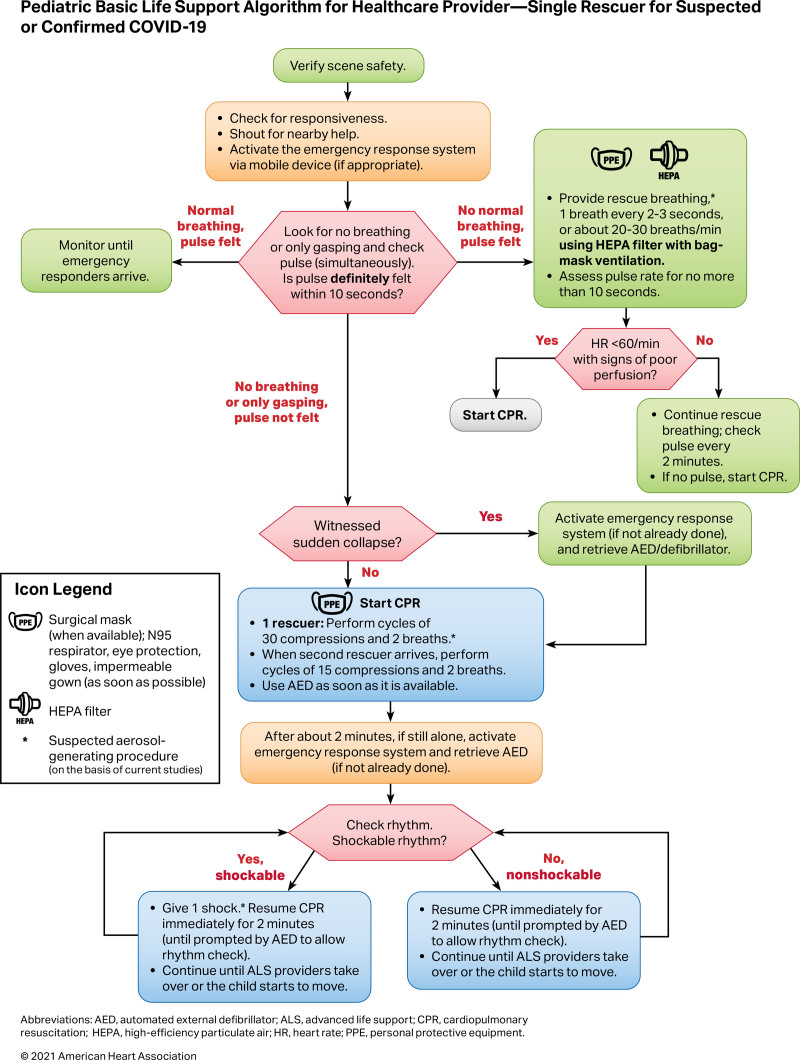
Figure 6.
Pediatric basic life support algorithm for health care provider—single rescuer for suspected or confirmed coronavirus disease 2019 (COVID-19).
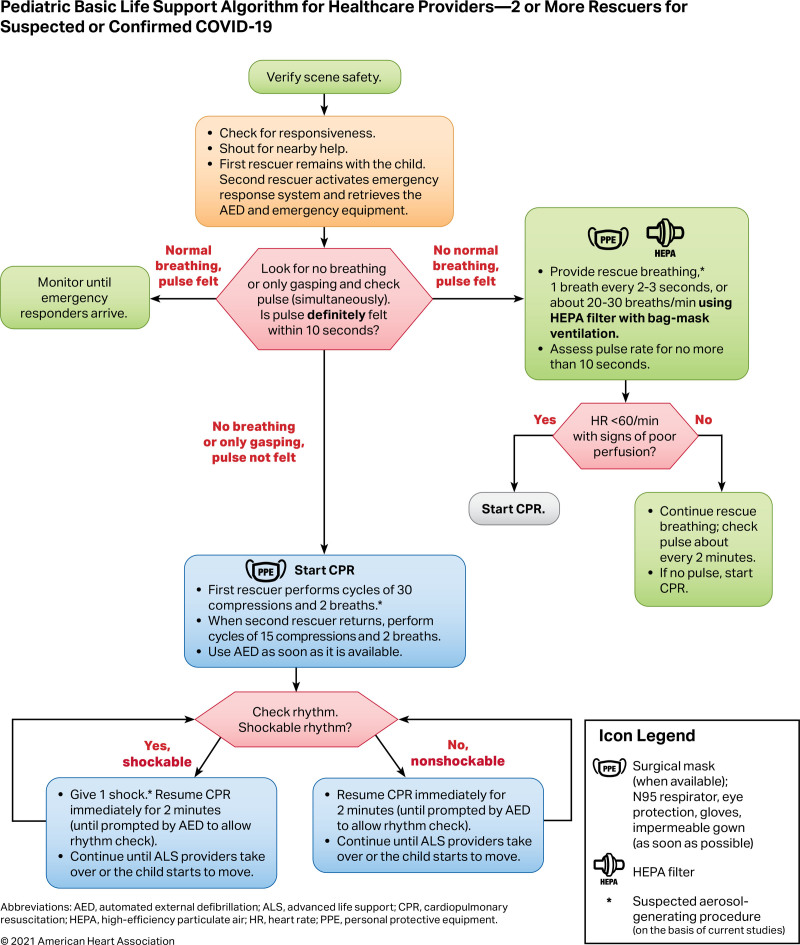
Figure 7.
Pediatric basic life support algorithm for health care providers—2 or more rescuers for suspected or confirmed coronavirus disease 2019 (COVID-19).
Reduce Provider Risk
Rationale
Frontline health care providers are at significant risk for contracting respiratory illnesses due to frequent contact with symptomatic patients. Adequate PPE including N-95 masks or positive air pressure respirators, especially during aerosol generating procedures (AGPs), can reduce the risk of coronavirus transmission.16 Provider risk may vary based on individual (age/ethnicity/comorbidities/vaccination status) and system factors. Health care organizations may need to consider redoubling efforts to maintain a sufficient supply of PPE for AGPs if vaccination of their staff is incomplete as only full vaccination of health care providers ensures an extremely low rate of infection.15 Even as immunity to SARS-CoV-2 is achieved with health care provider vaccination, it is reasonable for health care providers to continue taking appropriate precautions against COVID-19 and its variants since CPR includes AGPs and vaccination rates of health care providers remain below 100%.17,18 On the other hand, the risk to the patient by withholding or delaying the response for cardiac arrest is extremely high compared with the much lower risk that the resuscitation provider will contract COVID-19 and develop serious illness. This risk is particularly low in the vaccinated or unvaccinated provider who provides care while wearing appropriate PPE for AGPs.19 Although the effectiveness of available vaccines has been demonstrated against the wild-type SARS-CoV-2 and variants of concern, breakthrough infections, which are usually not life threatening, may still occur. Boosters addressing emerging variants of concern may be required.15,20
Reduce Provider Exposure and Provide Timely Care
Rationale
The data regarding which procedures are aerosol generating are conflicting and continue to develop. Some components of CPR are suspected to be aerosol generating.21 SARS-CoV-2 is transmitted primarily by respiratory droplets and aerosols, with little transmission by fomites.22–24 Rapid initiation of chest compressions is critical for successful resuscitation and, in light of the low incidence of documented transmission to health care providers to date, is likely low risk to the compressor.25–27 In witnessed sudden arrests of patients with suspected or confirmed COVID-19, chest compressions should not be delayed. Chest compressions can be performed initially by a chest compressor with or without a surgical mask until relieved by responders with appropriate PPE for AGPs. Although data continue to develop, in light of the low incidence of documented transmission to health care providers to date, chest compressions should not be delayed for retrieval and application of a mask or face covering for either the patient or provider. Masks may be considered for providers once compressions have started and before the arrival of responders with appropriate PPE for AGPs.28 Unless there are active efforts to maintain an open airway, it is typically occluded in the unconscious patient with minimal air movement during chest compressions.29
The case definitions of suspected and confirmed COVID-19 have changed over time.30 For communities and facilities with a higher prevalence of COVID-19 and lower immunization rates, the continuous use of an N-95 respirator and eye protection should be considered when the patient′s COVID-19 status is unknown and resuscitation involves AGP interventions to which compressors and other personnel will be exposed. Provided there is sufficient PPE, additional compressors may be required due to increased fatigue or potential for N-95 respirator slippage resulting from compressions.31–33 The application of mechanical compression devices can reduce the number of health care providers required for compressions; however, these devices may not be appropriate or available for morbidly obese adults, infants, children, and small adolescents or for all clinical scenarios.34 Training and regular practice in the use and rapid application of mechanical compressions devices is required to minimize the early no-flow time and to ensure proper application and utilization of the device. Although the clinical use of mechanical devices has not demonstrated improvement in outcome compared with manual CPR, it may reduce the number of additional staff who are needed to participate in the resuscitation event.35,36
As not every resuscitation space has negative pressure ventilation, closing the door may help limit contamination of adjacent indoor spaces. In out-of-hospital cardiac arrest, taking measures to better ventilate a confined space such as opening windows or doors may reduce the local concentration of aerosols for health care providers if this does not risk contamination of other spaces in the adjacent vicinity. In addition, some health care organizations may have continued shortages in PPE supply, low vaccination rates among staff, and personnel limitations; this guidance needs to be adapted to local protocols with consideration of current COVID-19 disease burden and resource availability.
Specific Additional Resuscitation Strategies
Rationale
It remains unclear whether defibrillation itself is an AGP; however, preliminary animal data suggest chest compressions following defibrillation may be aerosol generating.37 On the other hand, case-control and retrospective cohort studies of other infectious agents spread by aerosolization indicate that the relative risk of transmission during defibrillation is minimal.38 A surgical mask on a patient with COVID-19 may help deflect exhaled respiratory particles that can pass through some oxygen-delivering masks. However, mask availability should not delay or prevent time-sensitive lifesaving therapies like chest compressions or defibrillation. When actively ventilating using bag-mask ventilation, a supraglottic airway, or an endotracheal tube, a high-efficiency particulate air (HEPA) filter on the ventilation exhaust port can capture aerosolized particles. Endotracheal intubation should be timed with having sufficient PPE-protected personnel to perform the procedure.
Situation- and Setting-Specific Considerations
Pediatric and Adult Cardiac Arrests
In the witnessed sudden arrest, initiate chest compressions immediately and, if not already masked, the provider should don their mask without delaying or interrupting compressions. If immediately available, a face covering for the patient may be considered but should not delay or interrupt compressions.
Ventilations that are prioritized in pediatric arrests are suspected to be aerosol generating. Upon arrival, providers wearing appropriate PPE for AGPs should excuse providers without risk-matched PPE.
Defibrillate as soon as indicated. Masking of the unvaccinated provider and patient may reduce the uncertain transmission risk following defibrillation but should not prevent or delay defibrillation. Patient masks are not needed if providers are wearing appropriate PPE for AGPs.
A HEPA filter should be securely attached to any manual or mechanical ventilation device along the exhalation port before all ventilation devices such as, but not limited to, bag-mask-valve, supraglottic airway devices, endotracheal tubes, and ventilator mechanical circuits. Alternatively, a low-dead space viral filter or a heat and moisture exchanging filter with >99.99% viral filtration efficiency may be placed between the ventilation device and the airway. The viral filter or the heat and moisture exchanging filter should remain attached to the airway when changing ventilation devices.
Secure placement of a supraglottic airway with HEPA filters can help maximize chest compression fraction and control aerosol generation before endotracheal intubation.
Agonal breathing has been observed during early phases of cardiac arrest and may be seen during resuscitation particularly during transient periods of restored spontaneous circulation. In such cases, consider passive oxygenation overlaid with a surgical facemask (if readily available) when a bag-mask device or an advanced airway with a HEPA filter is not being utilized.
Before intubation, ventilate with a bag-mask-HEPA filter and a tight seal using practiced 2-person technique, ideally. The second team member can help provide extra support for additional procedures such as compressions once the airway is established.
Assign the intubator with the highest chance of first pass success using the method the intubator is most comfortable with while protected with appropriate PPE for AGPs. Intubate with a cuffed endotracheal tube to minimize aerosolization of respiratory particles.
Consider use of video laryngoscopy if available and if the operator is experienced with this technique as this may reduce direct exposure of the intubator to respiratory aerosols. Currently, there is no evidence of a difference in transmission risk using video versus direct laryngoscopy in the setting of providers wearing appropriate PPE for AGPs.
As in any resuscitation, maximize the chest compression fraction, pausing only to facilitate intubation if needed. Minimizing noncompression time can require team-based instruction including pulse checks, advanced airway placement, and focused ultrasound evaluation coordinated with pulse checks and other necessary interruptions.
Avoid endotracheal administration of medications; disconnections may be a source of aerosolization due to unfiltered exhalation.
Prearrest
Closely monitor for signs and symptoms of clinical deterioration to minimize the need for emergency intubations that put patients and providers at higher risk.
Address advanced care directives and goals of care with all patients with suspected or confirmed COVID-19 (or proxy) on hospital arrival and with any subsequent significant change in clinical status.
If the patient is at risk for cardiac arrest, consider proactively moving the patient to a negative-pressure room/unit, if available, to minimize risk of exposure to rescuers during a resuscitation.
Close the door when possible to prevent airborne contamination of adjacent indoor space. Conversely, for out-of-hospital cardiac arrests, ventilating confined spaces by opening windows or doors may help disperse aerosolized particles if this does not risk exposure of others in the vicinity and not already in an outdoor setting.
Out-of-Hospital Cardiac Arrest
Guidance regarding Emergency Medical Services and lay rescuer is described in detail in other literature.39,40
For the out-of-hospital, public, cardiac arrest chest compressions should be immediately initiated. It is reasonable for the compressor to don a mask immediately, but initiation of chest compressions should not be delayed. Delays due to mask retrieval may increase the risk of death for the patient from delayed CPR while providing little benefit to the provider.
If immediately available, placing a face covering on a known COVID-19 patient may reduce the uncertain risk of aerosol exposure from compressions following defibrillation but should not prevent or delay defibrillation or chest compressions and is unnecessary for providers in appropriate PPE for AGPs.
Before or upon arrival, Emergency Medical Service providers should rapidly don appropriate PPE for AGPs without delay or interruption of chest compressions and excuse unprotected persons from the immediate scene of care as soon as possible.
Pediatric arrests occur primarily from respiratory causes, and ventilation is a lifesaving priority. Since ventilation of suspected and confirmed COVID-19 pediatric arrests poses a transmission risk, HEPA-filtered ventilation and health care provider masking, when available, can reduce the risk of transmission during CPR until providers arrive wearing appropriate PPE for AGPs.
In-Hospital Cardiac Arrest
Crowd control for effective direction of resuscitation by the minimum number of people required is advised. Closing the door to the resuscitation area, when possible, may minimize airborne contamination of adjacent indoor space. Health care personnel should continue to wear appropriate PPE for clinical care including masks, eye protection, and gloves as recommended by the Centers for Disease Control and Prevention.41 The standard 2020 AHA guidelines for CPR and ECC should apply to those patients who are known to be COVID-19 negative.1
Patients Who Are Intubated Before Arrest
Consider leaving the patient on a mechanical ventilator with a HEPA filter to maintain a closed circuit and to reduce aerosolization and adjust the ventilator settings to allow asynchronous ventilation with the following suggestions:
Increase the FiO2 to 1.0.
Use either pressure or volume control ventilation and limit pressure or tidal volume to generate adequate chest rise (4–6 mL/kg ideal body weight is often targeted for adults and neonates, 5–8 mL/kg for children).
Adjust the trigger settings to prevent the ventilator from auto-triggering with chest compressions and possibly prevent hyperventilation and air trapping.
Adjust respiratory rate to 10 breaths/min for adults, 20 to 30 breaths/min for infants and children, and 30 breaths/min for neonates.
Assess the need to adjust the positive end-expiratory pressure level to balance lung volumes and venous return.
Adjust ventilator settings to deliver full breaths with asynchronous chest compressions.
Ensure endotracheal tube/tracheostomy and ventilator circuit continuity to prevent unplanned airway dislodgement or tubing disconnections.
If return of spontaneous circulation is achieved, set ventilator settings as appropriate to the patients′ clinical condition and treat the underlying cause of cardiac arrest.
Patients Who Are in Prone Position at the Time of Arrest
Anticipation and preparation are important in rotating patients to a supine position. The limited evidence for providing CPR in the prone position suggests it may be better than not providing CPR. For patients in the prone position with an advanced airway, it may be reasonable to provide manual compressions in the prone position until a patient can be safely transitioned to a supine position with a trained team. If deemed necessary for optimal clinical care, such as assessing endotracheal tube patency and positioning, the following steps for transitioning a patient to a supine position are suggested:
Provide compressions with hands centered over the T7/T10 vertebral bodies.
Arrange for sufficient, trained, PPE-protected personnel to achieve safe supination on the first attempt.
If already intubated, ensure ventilation and vascular tubing continuity and apply the posterior defibrillator pad to the patient′s back before rotating.
Immediately resume CPR supine once the patient has been rotated. Confirm tubing and access lines have not been dislodged and are in working order.
Postarrest Patients
Health care providers wearing appropriate PPE should continue to provide postcardiac arrest care per the 2020 AHA guidelines for CPR and ECC.42,43
Appropriateness of Starting and Continuing Resuscitation
Address and follow the patient′s goals of care and commit to ethical and evidence-based organizational policies to guide the determination of initiation and continuing resuscitative efforts. Follow the 2020 AHA guidelines for CPR and ECC for termination of resuscitation.42
Unsuccessful Resuscitations With Suspected and Confirmed COVID-19
Inquire with the infection control officer or medical examiner if further postmortem testing is required for epidemiological or contact tracing purposes.44
Maternal and Neonatal Considerations
Neonatal Resuscitation
Every newborn baby should have a skilled attendant prepared to resuscitate regardless of the COVID-19 status. The newborn baby is unlikely to be a source of COVID-19 transmission even when mothers have confirmed COVID-19, but maternal respiratory secretions and fluids may be a potential source of SARS-COV-2 transmission for the neonatal team and newborn.45 When appropriate, mothers can be encouraged to wear a surgical mask during the delivery. For suspected or confirmed COVID-19–infected mothers, health care providers should don appropriate PPE for AGPs to decrease the risk of transmission to themselves and the baby.
Initial steps: routine neonatal care and the initial steps of neonatal resuscitation are unlikely to be aerosol generating; they include drying, tactile stimulation, placement into a plastic bag or wrap, assessment of heart rate, and placement of pulse oximetry and electrocardiographic leads.
Suction: suction of the airway after delivery should not be performed routinely for clear or meconium-stained amniotic fluid. Suctioning is a suspected AGP and is not indicated for uncomplicated deliveries, regardless of the COVID-19 status.
Endotracheal medications: endotracheal instillation of medications such as surfactant or epinephrine is suspected to be an aerosol generating procedure, especially via an uncuffed tube. Intravenous delivery of epinephrine via a low-lying umbilical venous catheter is the preferred route of administration during neonatal resuscitation, regardless of the COVID-19 status.
Positive pressure ventilation remains the main resuscitation strategy for newborns for apnea, ineffective breathing (gasping), and bradycardia. Chest compressions occur later in the resuscitation algorithm.
Delayed cord clamping and skin-to-skin contact may be practiced in the setting of a suspected or confirmed COVID-19–positive mother in stable neonates provided the mother is appropriately masked.
Until confirmed to be COVID-19 negative, suspected or confirmed COVID-19–positive mothers should practice hand and breast hygiene and wear a mask during care and feeding.
Closed incubators: closed incubator transfer and care (with appropriate distancing) should be used for neonatal intensive care patients when possible, but incubators do not protect against aerosolized particles.
Maternal Cardiac Arrest
Symptomatic pregnant patients with COVID-19 are at increased risk of more severe illness compared with nonpregnant peers. Although the absolute risk for severe COVID-19 is low, data indicate an increased risk of ICU admission, need for mechanical ventilation and ventilatory support, and death in pregnant women with symptomatic COVID-19 infection.46
Preparation for perimortem cesarean delivery, to occur by 5 minutes of advanced cardiac life support without return of spontaneous circulation, should be initiated early to allow the obstetric and neonatal teams to apply appropriate PPE for AGPs before they enter the resuscitation area.
Oxygenation with intubation should be prioritized earlier in pregnant women with symptomatic COVID-19 who experience cardiac arrest. Provide chest compressions with concurrent left lateral uterine displacement when the uterine fundus is at the level of the umbilicus or greater.
Disclosures
Dr Kudenchuk reports compensation from the National Institutes of Health for other services, compensation from King County Emergency Medical Services for other services, and employment by the University of Washington. Dr Atkins reports compensation from the National Institutes of Health for data and safety monitoring services. Dr Brooks reports a patent pending for AED on the Way remotely activated device for automated external defibrillator recruiting, grants from the Canadian Institutes of Health Research, gifts from Action First Aid, and grants from Ontario Ministry of Health and Long-Term Care. Dr Cheng reports grants from the Canadian Institutes of Health Research and employment by Alberta Health Services. B.M. Clemency reports compensation from Stryker Corporation for consultant services. Dr Edelson reports a patent (ARCD. P0535US.P2) pending for risk stratification algorithms for hospitalized patients and employment by AgileMD. Dr Fuchs reports royalty from UpToDate. Dr Girotra reports compensation from the American Heart Association for other services. C. Hinkson reports employment by Providence Health Care and service as Director-at-Large for American Association for Respiratory Care. Dr Kamath-Rayne reports employment by the American Academy of Pediatrics. Dr Kleinman reports compensation from the Beth Israel Deaconess Medical Center for data and safety monitoring services, employment by the Boston Children′s Hospital, and compensation from the American Heart Association for consultant services. Dr Lavonas reports compensation from the American Heart Association for consultant services. Dr Lehotzky reports employment by the American Heart Association. Dr Mancini reports compensation from Stryker Corporation for other services. Dr McBride reports compensation from the American Heart Association for consultant services. Dr Moitra reports compensation from Malpractice Expert for expert witness services. Dr Morgan reports grants from the National Institutes of Health. K. Roberts reports compensation from the American Association of Critical Care Nurses for consultant services. Dr Sayre reports gifts from Stryker Corporation. Dr Zelop reports compensation from Uptodate for consultant services. The other authors report no conflicts.
Footnotes
For Disclosures, see page 1116.
Contributor Information
Antony Hsu, Email: antony.hsu@gmail.com.
Peter J. Kudenchuk, Email: pKudenchuk@cardiology.washington.edu.
Dianne L. Atkins, Email: dianne-atkins@uiowa.edu.
Khalid Aziz, Email: khalid.aziz@ualberta.ca.
Lance B. Becker, Email: Lance.Becker@northwell.edu.
Robert A. Berg, Email: bergra@email.chop.edu.
Farhan Bhanji, Email: farhan.bhanji@mcgill.ca.
Steven M. Bradley, Email: steven.bradley@allina.com.
Steven C. Brooks, Email: steven.brooks@kingstonhsc.ca.
Melissa Chan, Email: paulchan.mahi@gmail.com.
Paul S. Chan, Email: paulchan.mahi@gmail.com.
Adam Cheng, Email: chenger@me.com.
Brian M. Clemency, Email: bc34@buffalo.edu.
Allan de Caen, Email: allan.decaen@albertahealthservices.ca.
Jonathan P. Duff, Email: jduff@ualberta.ca.
Dana P. Edelson, Email: dperes@medicine.bsd.uchicago.edu.
Gustavo E. Flores, Email: gflores@ecctrainings.com.
Susan Fuchs, Email: sfuchs@luriechildrens.org.
Saket Girotra, Email: saket-girotra@uiowa.edu.
Carl Hinkson, Email: Carl.Hinkson@providence.org.
Benny L. Joyner, Jr, Email: benny_joyner@med.unc.edu.
Beena D. Kamath-Rayne, Email: bkamathrayne@aap.org.
Monica Kleinman, Email: monica.kleinman@childrens.harvard.edu.
Javier J. Lasa, Email: jjlasa@texaschildrens.org.
Eric J. Lavonas, Email: eric.lavonas@dhha.org.
Henry C. Lee, Email: hclee@stanford.edu.
Rebecca E. Lehotzky, Email: Becky.Lehotzky@heart.org.
Arielle Levy, Email: arielle.levy007@gmail.com.
Mary E. Mancini, Email: mmcbride@luriechildrens.org.
Mary E. McBride, Email: mmcbride@luriechildrens.org.
Garth Meckler, Email: Garth.Meckler@cw.bc.ca.
Raina M. Merchant, Email: Raina.Merchant@pennmedicine.upenn.edu.
Vivek K. Moitra, Email: vm2161@cumc.columbia.edu.
Ryan W. Morgan, Email: morganr1@email.chop.edu.
Vinay Nadkarni, Email: Nadkarni@chop.edu.
Ashish R. Panchal, Email: Ashish.Panchal@osumc.edu.
Mary Ann Peberdy, Email: mpeberdy@aol.com.
Tia Raymond, Email: tiaraymond@me.com.
Kathryn Roberts, Email: robertske1103@gmail.com.
Michael R. Sayre, Email: sayrem@uw.edu.
Stephen M. Schexnayder, Email: schexnaydersm@uams.edu.
Robert M. Sutton, Email: suttonr@chop.edu.
Mark Terry, Email: mark.terry.ems@gmail.com.
Brian Walsh, Email: brian.walsh@childrenscolorado.org.
David S. Wang, Email: dsw2144@cumc.columbia.edu.
Carolyn M. Zelop, Email: cmzelop@comcast.net.
Alexis Topjian, Email: topjian@chop.edu.
References
- 1.Merchant RM, Topjian AA, Panchal AR, Cheng A, Aziz K, Berg KM, Lavonas EJ, Magid DJ; Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups. Part 1: executive summary: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020; 142(16 suppl 2):S337–S357. doi: 10.1161/CIR.0000000000000918 [DOI] [PubMed] [Google Scholar]
- 2.Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, Berg RA, Bradley SM, Brooks SC, Cheng A, et al. ; American Heart Association ECC Interim COVID Guidance Authors. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the Emergency Cardiovascular Care Committee and Get With The Guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020; 141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardio. 2021; 6:296–303. doi: 10.1001/jamacardio.2020.6210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baert V, Jaeger D, Hubert H, Lascarrou JB, Debaty G, Chouihed T, Javaudin F; GR-RéAC. Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: registry-based study. Scand J Trauma Resusc Emerg Med. 2020; 28:119. doi: 10.1186/s13049-020-00813-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Palo A, Contri E, Ronchi V, Beretta G, et al. ; all the Lombardia CARe Researchers. Treatment of out-of-hospital cardiac arrest in the COVID-19 era: a 100 days experience from the Lombardy region. PLoS One. 2020; 15:e0241028. doi: 10.1371/journal.pone.0241028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ball J, Nehme Z, Bernard S, Stub D, Stephenson M, Smith K. Collateral damage: hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020; 156:157–163. doi: 10.1016/j.resuscitation.2020.09.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sun C, Dyer S, Salvia J, Segal L, Levi R. Worse Cardiac Arrest Outcomes During The COVID-19 Pandemic In Boston Can Be Attributed To Patient Reluctance To Seek Care. Health Aff (Millwood). 2021; 40:886–895. doi: 10.1377/hlthaff.2021.00250 [DOI] [PubMed] [Google Scholar]
- 8.Miles JA, Mejia M, Rios S, Sokol SI, Langston M, Hahn S, Leiderman E, Salgunan R, Soghier I, Gulani P, et al. Characteristics and outcomes of In-Hospital Cardiac Arrest Events During the COVID-19 Pandemic. Circ Cardiovasc Qual Outcomes. 2020; 13:e007303. doi: 10.1161/circoutcomes.120.007303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen J, Lu KZ, Yi B, Chen Y. Chest compression with personal protective equipment during cardiopulmonary resuscitation: a randomized crossover simulation study. Medicine (Baltimore). 2016; 95:e3262. doi: 10.1097/MD.0000000000003262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hayek SS, Brenner SK, Azam TU, Shadid HR, Anderson E, Berlin H, Pan M, Meloche C, Feroz R, O′Hayer P, et al. ; STOP-COVID Investigators. In-hospital cardiac arrest in critically ill patients with covid-19: multicenter cohort study. BMJ. 2020; 371:m3513. doi: 10.1136/bmj.m3513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lai PH, Lancet EA, Weiden MD, Webber MP, Zeig-Owens R, Hall CB, Prezant DJ. Characteristics associated with out-of-Hospital cardiac arrests and resuscitations during the novel coronavirus disease 2019 pandemic in New York City. JAMA Cardiol. 2020; 5:1154–1163. doi: 10.1001/jamacardio.2020.2488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aldujeli A, Hamadeh A, Briedis K, Tecson KM, Rutland J, Krivickas Z, Stiklioraitis S, Briede K, Aldujeili M, Unikas R, et al. Delays in presentation in patients with acute myocardial infarction during the COVID-19 pandemic. Cardiol Res. 2020; 11:386–391. doi: 10.14740/cr1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Heart Association. Heart disease and stroke medical experts urge public to get COVID-19 vaccinations. 2021. Accessed May 20, 2021. https://newsroom.heart.org/news/heart-disease-and-stroke-medical-experts-urge-public-to-get-covid-19-vaccinations
- 14.Keehner J, Horton LE, Pfeffer MA, Longhurst CA, Schooley RT, Currier JS, Abeles SR, Torriani FJ. SARS-CoV-2 infection after vaccination in Health Care Workers in California. N Engl J Med. 2021; 384:1774–1775. doi: 10.1056/NEJMc2101927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thompson MG. Interim estimates of vaccine effectiveness of BNT162b2 and mRNA-1273 COVID-19 vaccines in preventing SARS-CoV-2 infection among health care personnel, first responders, and other essential and frontline workers — eight U.S. locations, December 2020–March 2021. MMWR Morb Mortal Wkly Rep. 2021; 70:495–500. doi: 10.15585/mmwr.mm7013e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Raboud J, Shigayeva A, McGeer A, Bontovics E, Chapman M, Gravel D, Henry B, Lapinsky S, Loeb M, McDonald LC, et al. Risk factors for SARS transmission from patients requiring intubation: a multicentre investigation in Toronto, Canada. PLoS One. 2010; 5:e10717. doi: 10.1371/journal.pone.0010717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Galloway SE, Prabasaj P, MacCannell DR, Slayton RB, Tong S, Silk BJ, Armstrong GL, Biggerstaff M, Dugan VG. Emergence of SARS-CoV-2 B.1.1.7 Lineage — United States, December 29, 2020–January 12, 2021. MMWR Morb Mortal Wkly Rep. 2021; 70:95–99. doi: 10.15585/mmwr.mm7003e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Z, Schmidt F, Weisblum Y, Muecksch F, Barnes CO, Finkin S, Schaefer-Babajew D, Cipolla M, Gaebler C, Lieberman JA, et al. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. Nature. 2021; 592:616–622. doi: 10.1038/s41586-021-03324-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown A, Schwarcz L, Counts CR, Barnard LM, Yang BY, Emert JM, Latimer A, Drucker C, Lynch J, Kudenchuk PJ, et al. Risk for acquiring coronavirus disease illness among emergency medical service personnel exposed to aerosol-generating procedures. Emerg Infect Dis. 2021; 27:2340–2348. doi: 10.3201/eid2709.210363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hacisuleyman E, Hale C, Saito Y, Blachere NE, Bergh M, Conlon EG, Schaefer-Babajew DJ, DaSilva J, Muecksch F, Gaebler C, et al. Vaccine breakthrough infections with SARS-CoV-2 variants. N Engl J Med. 2021; 384:2212–2218. doi: 10.1056/NEJMoa2105000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Infection Control - Which procedures are considered aerosol generating procedures in healthcare settings? 2020. Accessed May 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/faq.html
- 22.Horoho S, Musik S, Bryant D, Brooks W, Porter IM. Questioning COVID-19 surface stability and fomite spreading in three aeromedical cases: a case series. Mil Med. 2020; 186:e832–e835. doi: 10.1093/milmed/usaa548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Centers for Disease Control and Prevention. Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic. 2020. Accessed May 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html
- 24.Centers for Disease Control and Prevention. SARS-CoV-2 and Surface (Fomite) Transmission for Indoor Community Environments. 2021. Accessed May 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/more/science-and-research/surface-transmission.html [PubMed]
- 25.Couper K, Taylor-Phillips S, Grove A, Freeman K, Osokogu O, Court R, Mehrabian A, Morley PT, Nolan JP, Soar J, et al. COVID-19 in cardiac arrest and infection risk to rescuers: a systematic review. Resuscitation. 2020; 151:59–66. doi: 10.1016/j.resuscitation.2020.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abrahamson SD, Canzian S, Brunet F. Using simulation for training and to change protocol during the outbreak of severe acute respiratory syndrome. Crit Care. 2006; 10:R3. doi: 10.1186/cc3916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Killingley B, Horby P. New and Emerging Respiratory Virus Threats Advisory Group. 2020. Accessed May 20, 2021. https://www.swast.nhs.uk/assets/1/cpr_as_an_agp_-_evidence_review_and_nervtag_consensus.pdf
- 28.Ott M, Milazzo A, Liebau S, Jaki C, Schilling T, Krohn A, Heymer J. Exploration of strategies to reduce aerosol-spread during chest compressions: a simulation and cadaver model. Resuscitation. 2020; 152:192–198. doi: 10.1016/j.resuscitation.2020.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Safar P. Ventilation and cardiopulmonary resuscitation. Curr Opin Anaesthesiol. 1999; 12:165–171. doi: 10.1097/00001503-199904000-00010 [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Coronavirus Disease 2019 (COVID-19) | 2020 Interim Case Definition. 2020. Accessed May 20, 2021. https://wwwn.cdc.gov/nndss/conditions/coronavirus-disease-2019-covid-19/case-definition/2020/08/05/
- 31.Tian Y, Tu X, Zhou X, Yu J, Luo S, Ma L, Liu C, Zhao Y, Jin X. Wearing a N95 mask increases rescuer′s fatigue and decreases chest compression quality in simulated cardiopulmonary resuscitation. Am J Emerg Med. 2020; S0735-6757:30424–30421. doi: 10.1016/j.ajem.2020.05.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kienbacher CL, Grafeneder J, Tscherny K, Krammel M, Fuhrmann V, Niederer M, Neudorfsky S, Herbich K, Schreiber W, Herkner H, et al. The use of personal protection equipment does not impair the quality of cardiopulmonary resuscitation: a prospective triple-cross over randomised controlled non-inferiority trial. Resuscitation. 2021; 160:79–83. doi: 10.1016/j.resuscitation.2021.01.021 [DOI] [PubMed] [Google Scholar]
- 33.Malysz M, Dabrowski M, Böttiger BW, Smereka J, Kulak K, Szarpak A, Jaguszewski M, Filipiak KJ, Ladny JR, Ruetzler K, et al. Resuscitation of the patient with suspected/confirmed COVID-19 when wearing personal protective equipment: a randomized multicenter crossover simulation trial. Cardiol J. 2020; 27:497–506. doi: 10.5603/CJ.a2020.0068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim HT, Kim JG, Jang YS, Kang GH, Kim W, Choi HY, Jun GS. Comparison of in-hospital use of mechanical chest compression devices for out-of-hospital cardiac arrest patients: AUTOPULSE vs LUCAS. Medicine (Baltimore). 2019; 98:e17881. doi: 10.1097/MD.0000000000017881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wang PL, Brooks SC. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2018; 8:CD007260. doi: 10.1002/14651858.CD007260.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bhatnagar A, Khraishah H, Lee J, Hsu D, Hayes M, Joseph B, Moskowitz A. Rapid implementation of a mechanical chest compression device for in-hospital cardiac arrest during the COVID-19 pandemic. Resuscitation. 2020; 156:4–5. doi: 10.1016/j.resuscitation.2020.08.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hsu CH, Tiba MH, Boehman AL, McCracken BM, Leander DC, Francalancia SC, Pickell Z, Sanderson TH, Ward KR, Neumar RW. Aerosol generation during chest compression and defibrillation in a swine cardiac arrest model. Resuscitation. 2021; 159:28–34. doi: 10.1016/j.resuscitation.2020.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tran K, Cimon K, Severn M, Pessoa-Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012; 7:e35797. doi: 10.1371/journal.pone.0035797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sayre MR, Barnard LM, Counts CR, Drucker CJ, Kudenchuk PJ, Rea TD, Eisenberg MS. Prevalence of COVID-19 in out-of-Hospital cardiac arrest: implications for bystander cardiopulmonary resuscitation. Circulation. 2020; 142:507–509. doi: 10.1161/CIRCULATIONAHA.120.048951 [DOI] [PubMed] [Google Scholar]
- 40.Goodloe JM, Topjian A, Hsu A, Dunne R, Panchal AR, Levy M, McEvoy M, Vaillancourt C, Cabanas JG, Eisenberg MS, et al. Interim guidance for emergency medical services management of out-of-Hospital Cardiac Arrest During the COVID-19 Pandemic. Circ Cardiovasc Qual Outcomes. 2021; 14:e007666. doi: 10.1161/CIRCOUTCOMES.120.007666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.COVID-19. Strategies for Optimizing the Supply of N95 Respirators. 2021. Accessed May 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/respirators-strategy/
- 42.Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, Kudenchuk PJ, Kurz MC, Lavonas EJ, Morley PT, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020; 142(16 suppl 2):S366–S468. doi: 10.1161/cir.0000000000000916 [DOI] [PubMed] [Google Scholar]
- 43.Topjian AA, Raymond TT, Atkins D, Chan M, Duff JP, Joyner BL, Jr, Lasa JJ, Lavonas EJ, Levy A, Mahgoub M, et al. ; Pediatric Basic and Advanced Life Support Collaborators. Part 4: pediatric basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020; 142(16 suppl 2):S469–S523. doi: 10.1161/CIR.0000000000000901 [DOI] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Collection and Submission of Postmortem Specimens from Deceased Persons with Confirmed or Suspected COVID-19. 2020. Updated December 2, 2020. Accessed May 20, 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-postmortem-specimens.html
- 45.Vivanti AJ, Vauloup-Fellous C, Prevot S, Zupan V, Suffee C, Do Cao J, Benachi A, De Luca D. Transplacental transmission of SARS-CoV-2 infection. Nat Commun. 2020; 11:3572. doi: 10.1038/s41467-020-17436-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zambrano LD, Ellington S, Strid P, Galang RR, Oduyebo T, Hong VT, Woodworth KR, Nahabedian JF, Azziz-Baumgartner E, Gilboa SM, et al. Update: characteristics of symptomatic women of reproductive age with laboratory-confirmed SARS-CoV-2 infection by pregnancy status — United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1641–1647. doi: 10.15585/mmwr.mm6944e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Safar P, Brown TC, Holtey WJ, Wilder RJ. Ventilation and circulation with closed-chest cardiac massage in man. JAMA. 1961; 176:574–576. doi: 10.1001/jama.1961.03040200010003 [DOI] [PubMed] [Google Scholar]
- 48.McDannold R, Bobrow BJ, Chikani V, Silver A, Spaite DW, Vadeboncoeur T. Quantification of ventilation volumes produced by compressions during emergency department cardiopulmonary resuscitation. Am J Emerg Med. 2018; 36:1640–1644. doi: 10.1016/j.ajem.2018.06.057 [DOI] [PubMed] [Google Scholar]
- 49.Deakin CD, O′Neill JF, Tabor T. Does compression-only cardiopulmonary resuscitation generate adequate passive ventilation during cardiac arrest? Resuscitation. 2007; 75:53–59. doi: 10.1016/j.resuscitation.2007.04.002 [DOI] [PubMed] [Google Scholar]
- 50.FDA. Protective Barrier Enclosures Without Negative Pressure Used During the COVID-19 Pandemic May Increase Risk to Patients and Health Care Providers - Letter to Health Care Providers. 2020. Accessed May 20, 2021. https://www.fda.gov/medical-devices/letters-health-care-providers/protective-barrier-enclosures-without-negative-pressure-used-during-covid-19-pandemic-may-increase
- 51.Begley JL, Lavery KE, Nickson CP, Brewster DJ. The aerosol box for intubation in coronavirus disease 2019 patients: an in-situ simulation crossover study. Anaesthesia. 2020; 75:1014–1021. doi: 10.1111/anae.15115 [DOI] [PMC free article] [PubMed] [Google Scholar]