Abstract
Bedsharing (sharing a bed with others during sleep) in early childhood (3–5 years) is common across western and non-western societies alike. Though prior work indicates that bedsharing may relate to impairments in child sleep quantity and/or quality, the majority of studies conducted in young children are limited to parent-child bedsharing and rely almost exclusively on caregiver reports to measure child sleep. Here, we endeavored to gain further insights into the diversity of bedsharing practices among children in the United States, including how different bedsharing partners (caregivers, siblings) might impact actigraphy-derived measures of children’s sleep. Using a sample of 631 children ages 2:9–5:11 years, we found that over 36% of children bedshared in some form overnight, with approximately 22% bedsharing habitually. In a subset of children for whom actigraphy measures were collected (n=337), children who bedshared habitually (n=80) had significantly shorter overnight sleep, later sleep and wake times, and longer naps than solitary sleepers (n=257), even when controlling for socioeconomic status. Despite supplementing their shorter overnight sleep with longer naps, habitually bedsharing children had significantly shorter 24-hour sleep time than solitary sleepers, though differences in sleep efficiency were non-significant for all sleep periods. Additionally, sleep efficiency, onset latency and duration did not differ between children who habitually bedshared with siblings versus those who habitually bedshared with parents. Our results add to prior work examining family contextual correlates of sleep differences in early childhood, and provide a more objective account of relations between bedsharing and child sleep.
Keywords: Sleep, bedsharing, co-sleeping, early childhood, siblings
Introduction
In early childhood, sharing a bed with others during sleep, referred to as bedsharing, is a globally widespread, yet controversial practice (McKenna, Ball, & Gettler, 2007; Mileva-Seitz, Bakermans-Kranenburg, Battaini, & Luijk, 2017). Despite the ubiquity of bedsharing (Mileva-Seitz et al., 2017), debate regarding the impact of bedsharing on children’s sleep and development continues to exist, particularly in the United States (Ball, 2006; Owens, 2004). With organizations such as the American Academy of Pediatrics developing guidelines regarding safe sleeping practices in infants and children (Moon, Darnall, Feldman-Winter, Goodstein, & Hauck, 2016), a better scientific understanding of the ages and contexts under which bedsharing occurs and whether it benefits or adversely affects sleep is crucially needed.
Across later toddlerhood and childhood specifically, research findings on bedsharing and its effects have been inconsistent (Cortesi, Giannotti, Sebastiani, Vagnoni, & Marioni, 2008; Hayes, Parker, Sallinen, & Davare, 2001; Jenni, Fuhrer, Iglowstein, Molinari, & Largo, 2005; Kim, Lee, & Cain, 2017; Latz, Wolf, & Lozoff, 1999; Liu, Liu, & Wang, 2003; Lozoff, Wolf, & Davis, 1984; Mindell, Sadeh, Kwon, & Goh, 2013; Okami, Weisner, & Olmstead, 2002). While some work indicates greater sleep disturbances in bedsharing children (e.g. Cortesi et al., 2008; Hayes et al., 2001; Kim et al., 2017), other studies indicate no detrimental effects (e.g. Okami et al., 2002). In part, this discrepancy in findings may reflect a lack of objective sleep assessments, as most published work has used parent-reported questionnaires or interviews (Cortesi et al., 2008; Jenni et al., 2005; Kim et al., 2017; Liu et al., 2003; Mindell et al., 2013; also see Mileva-Seitz et al., 2017 for review). Such subjective methods may present a confound when evaluating child sleep outcomes, because parents who bedshare may notice subtler disturbances in their child’s sleep (or alternatively, may have positive attitudes toward bedsharing that bias their responses in favor of higher child sleep quality) compared to parents who do not bedshare. Aside from this limitation, current work has also largely confined analyses to bedsharing between children and parents, either failing to measure or purposely excluding arrangements in which children bedshare with a sibling or pet (e.g., Kim et al., 2017; Lozoff et al., 1984).
In the present study, we used actigraphy to explore, in a large cohort of young children, the frequency and sleep correlates of bedsharing, both with caregivers and other sleep partners. By doing so, we aimed to extend the current state of knowledge regarding child bedsharing practices, and to determine whether sleep partner type might play a role in the degree to which bedsharing influences child sleep.
Bedsharing in young children, and relations to sleep health
Bedsharing among children is ostensibly common. In a recent cross-cultural analysis of sleep habits in children ages 3–6 years, approximately 13.1% of U.S. caregivers reported sharing a bed with their child (Mindell et al., 2013). Though bedsharing prevalence at this age was higher among samples from predominantly Asian countries, bedsharing was nonetheless practiced among over 9% of families from primarily western countries. Furthermore, in a longitudinal study of bedsharing among Swiss children, 44% of parents reported that their child shared a bed with them for at least one year at some point between ages 2 and 7 years (Jenni et al., 2005). Within this sample, the age at which bedsharing reached peak prevalence was 4 years, at which age 38% of all children were bedsharing at least once per week. Together, these findings suggest that bedsharing in early childhood is not rare even among western nations, though its frequency may also be moderated by cultural factors.
Regarding bedsharing’s relations to child sleep, observational studies have begun to provide insights. In a sample of 67 preschool-enrolled children ages 2.4–5.6 years in the U.S., children who bedshared with parents had longer sleep onsets, less consistent bedtimes, and more frequent parent seeking and night waking according to parent reports (Hayes et al., 2001). Bedsharing children were also parent-rated as less adaptable and more sensitive; however, teachers’ child temperament ratings did not align with parents’, and only parents’ ratings varied by child bedsharing status. Given these caregivers’ potential biases, and the fact that sleep measures were limited to parent report, it is unknown whether child sleep differences would be detected via less subjective measures. Additionally, the observational nature of this study and others (e.g. Cortesi et al., 2008; Kim et al., 2017; Tan, Marfo, & Dedrick, 2009) makes it difficult to parse whether bedsharing is a cause or consequence of child sleep or temperament difficulties. Nonetheless, some studies have linked parent-child bedsharing with child sleep problems, including parent-reported shorter child sleep duration, greater bedtime resistance and behavior challenges, or greater overall sleep disturbance (Cortesi et al., 2008; Kim et al., 2017).
In contrast, additional longitudinal and cross-sectional analyses have indicated either that parent-child bedsharing does not predict child sleep (Okami et al., 2002), or that bedsharing is associated with child sleep disturbances only in certain demographic groups (Latz et al., 1999; Lozoff et al., 1984). For instance, one U.S. study indicated that for children ages 6 months to 4 years, bedsharing was associated with greater disruptive sleep problems (consistent night wakings, struggles surrounding bedtime) in White children, but not in Black children (Lozoff et al., 1984). Approximately twice the percentage of Black families in this study bedshared compared to White families, perhaps indicating cultural or socioeconomic differences in the variables prompting bedsharing between these groups. Similarly, a study analyzing parent-child bedsharing between families in the U.S. and Japan reported that bedsharing was more prevalent among young children in Japan (59% vs. 15% of U.S. families), and that bedsharing was associated with greater child sleep difficulties and bedtime protests only in the U.S. (Latz et al., 1999). These patterns suggest that bedsharing among certain demographic groups (i.e., White families in the U.S.) may be initiated more as a response to existing child sleep problems, rather than as an intentional or purposeful cultural practice (Mileva-Seitz et al., 2017).
Importantly, all studies to our knowledge examining bedsharing and sleep health in childhood beyond infancy have relied only on caregiver reports of child sleep, rather than objective measures. In addition, bedsharing studies in young children have primarily focused on evaluating overnight sleep only, despite napping being common for many under age 5 years (Galland, Taylor, Elder, & Herbison, 2012; Weissbluth, 1995). Although focusing on children’s overnight sleep may make sense if that is the bout in which bedsharing most consistently occurs, not measuring children’s daytime sleep may result in an incomplete picture of how nighttime bedsharing affects 24-hour sleep duration. Finally, prior studies have not always accounted for factors that may covary with bedsharing and relate independently to sleep, such as socioeconomic status (SES). As SES is associated both with increased caregiver bedsharing and decreased sleep quality in some studies (Betsy Lozoff, Askew, & Wolf, 1996; Marco, Wolfson, Sparling, & Azuaje, 2011; Salm Ward & Ngui, 2015), it is important to consider this factor when assessing bedsharing and sleep health in early childhood.
Bedsharing beyond parents
Research on child bedsharing aside from parent-child dyads is limited. One study exploring the sleeping arrangements of preschool-aged children adopted from China reported that bedsharing with siblings was rarer than bedsharing with adoptive parents at this age (9% vs. 24%; Tan et al., 2009). Although parent-child bedsharing in this study was associated with higher child sleep problems, sibling bedsharing and room sharing were unrelated to parent-reported child sleep difficulties. Notably, these bedsharing practices may have been influenced by the child’s adoptive status (prior sleep arrangements or need to bond with parent), and sleep was assessed by parent report. Aside from this study, sibling bedsharing research has been limited to twin crib sharing studies in early infancy (Ball, 2006; Damato, Brubaker, & Burant, 2012). Such studies have found bedsharing-dependent differences in infant sleep durations at some ages but not others (i.e., 3 months vs. 1 month; Ball, 2006), as well as a negative effect of early twin crib sharing and parent room sharing on parents’ sleep durations (Damato et al., 2012). Given the paucity of work on sibling bedsharing beyond infancy, it is relevant to explore the prevalence of this practice in a contemporary sample of young children, and its implications for sleep health as compared to other forms of bedsharing or solitary sleeping.
The present study
Given the gaps in research surrounding the prevalence of different bedsharing configurations and sleep partners of young children in the U.S., as well as the effects of bedsharing on objective measures of sleep duration and quality, the current study had three objectives. First, we aimed to characterize in more depth the diversity of bedsharing arrangements observed in early childhood, an age at which bedsharing practices and child sleep patterns overall are clearly changing (Galland et al., 2012; Jenni et al., 2005; Weissbluth, 1995). Within this characterization, we sought to expand the investigation of bedsharing beyond the parent-child dyad, to include bedsharing with siblings, family pets, or any other individual or combination of individuals. In documenting these arrangements, we sought to gain a more accurate view of the prevalence of bedsharing in early childhood among U.S. families, and to determine factors, such as SES and culture, that might predict bedsharing in this age group.
Second, we aimed to quantify relations between bedsharing and sleep health in preschool-aged children using more objective measures than previous questionnaire-based work. To accomplish this, we employed actigraphy, an accelerometer-based method of estimating sleep (Meltzer, Montgomery-Downs, Insana, & Walsh, 2012), in addition to sleep diaries completed by caregivers. Based on prior work indicating an effect of bedsharing on caregiver-reported child sleep, we hypothesized that bedsharing may correspond to more nighttime sleep disruption. Specifically, we hypothesized that overnight sleep among bedsharing children would be shorter (measured by nighttime sleep duration) and less efficient (measured by the percent of time asleep to time in bed), and that sleep onset would be delayed relative to non-bedsharing children (Cortesi et al., 2008; Hayes et al., 2001). However, prior work also suggests that when night sleep is decreased in young children, children may at least partly compensate with longer daytime naps (Helm & Spencer, 2019; Ward, Gay, Anders, Alkon, & Lee, 2008). Thus, we hypothesized that if nighttime sleep was disturbed by bedsharing, children’s naps would be longer in duration and more efficient, possibly resulting in comparable 24-hour sleep durations among bedsharing and non-bedsharing children.
Additionally, we aimed to understand whether the identity of children’s bedsharing partners (e.g., parent, sibling) differently influenced child sleep. Although the only study published to our knowledge on this topic found that parent bedsharing predicted child sleep difficulties while sibling bedsharing did not (Tan et al., 2009), the study population—children adopted from China by families across 3 westernized countries—may be unique, making it difficult to generalize the findings to non-adopted children or children of different cultural backgrounds. Additionally, the parent-report nature of their sleep measure may have led to unintentional over-endorsement of sleep problems in children who bedshared with parents, as these parents would be in closer proximity to their children during sleep and perhaps more likely to notice subtler sleep disturbances. Thus, we hypothesized that sibling bedsharing would be associated with shorter/less efficient overnight sleep and later sleep onsets (e.g., if children were encouraged by siblings to stay awake and socialize at bedtime). Finally, we hypothesized that if children who bedshared with siblings had shorter and/or less efficient overnight sleep than children who bedshared with caregivers, then sibling bedsharers’ naps would, in turn, be longer and more efficient as a means of compensating for disrupted night sleep. Overall, we anticipated that our study would allow for more clarity regarding child bedsharing habits in the U.S. and their associations with objective measures of child sleep.
Method
Participants
To assess the general bedsharing habits of young napping children, we aggregated sleep diary and questionnaire data from 631 children (287 female, mean age 51.46 months, range 33 – 71 months) from western Massachusetts. Demographics for the full sample are in Supplemental Table S1. This sample was taken from a larger study of memory and napping, conducted between 2012–2020. As part of the study, caregivers were asked to complete a sleep diary and questionnaires for their child, and to encourage their child to wear the actigraph watch to assess sleep for up to 16-days. For the present analysis, we included all participants for whom caregivers responded to questions pertaining to bedsharing, and for whom sufficient actigraphy data were available. Exclusion criteria for initial study enrollment included diagnosis of a sleep disorder other than mild parasomnia, diagnosis of a developmental disability, use of sleep-affecting or psychotropic medications, severe uncorrected hearing or vision impairment, or acute fever/respiratory illness at the time of testing. Children were also excluded if they had traveled across time zones in the week before data collection.
Of the 631 children with data on bedsharing habits, 408 had sufficient actigraphy to assess overnight sleep quantity (durations) and quality (efficiency and onset latencies). Additionally, 379 had sufficient actigraphy data to assess nap quantity and quality. After excluding children with less than 2 days of actigraphy data1, as well as half-night bed sharers and infrequent bed sharers, the final subsample included 337 children whose overnight sleep was assessed, of which 281 had sufficient nap data (using the criterion of at least 2 naps across the study). Among the full subsample, children had an average of 9.8 days of actigraphy data. Specifically, 0.3% had eighteen scorable days; 5.3% had fifteen; 6.5% had fourteen; 13.1% had thirteen; 14.8% had twelve; 11.6% had eleven; 7.4% had ten; 8.0% had nine; 5.3% had eight; 8.0% had seven; 4.5% had six; 3.6% had five; 6.5% had four; 4.2% had three; and, 0.9% had two. Additional information on this subsample is in Table 1. Both the full sample and subsample reflected the diversity of western Massachusetts, with over 20% identifying as of Hispanic, Latinx, or Spanish origin and less than 66% identifying as White. Approximately half of both samples also identified as low or middle class.
TABLE 1.
Demographic Characteristics of Children Included in Final Sleep Comparison Analyses
| Demographic Variables |
Habitual Bed Sharers (n=80) | Solitary Sleepers (n=257) |
Total Sample (n=337) |
|---|---|---|---|
|
| |||
| Child Age, | |||
| Months | |||
| M(SD) | 53.00 (9.95) | 50.88 (9.34) | 51.38 (9.52) |
| Child Sex | |||
| (% Female) | 45.0% | 42.8% | 43.3% |
| Socio-Economic Status | |||
| Composite Score | |||
| M (SD) | 3.96 (1.89) | 4.92 (1.96) | 4.69 (1.98) |
| % Low SES (score 0–2) | 28.6% | 15.6% | 18.7% |
| % Middle SES (score 3–4) | 33.8% | 23.6% | 26.0% |
| % High SES (score 5–7) | 37.7% | 60.8% | 55.4% |
| Child Ethnicity | |||
| % Non-Hispanic | 61.3% | 76.3% | 72.7% |
| % Hispanic, Latinx, or Spanish origin | 36.3% | 20.6% | 24.3% |
| % Refused to answer | 2.5% | 3.1% | 3.0% |
| Child Race | |||
| % White | 48.8% | 70.4% | 65.3% |
| % Black, African-American | 10.0% | 7.4% | 8.0% |
| % Asian (East/Southeast and Asian Indian) | 3.8% | 3.2% | 3.3% |
| % Pacific Islander | 0.0% | 0.0% | 0.0% |
| % Other race not listed | 16.3% | 5.4% | 8.0% |
| % Biracial/Multiracial | 15.0% | 8.2% | 9.8% |
| % Refused to answer | 6.3% | 5.4% | 5.6% |
| Enrollment in Preschool | |||
| % Enrolled at least 1 day/wk | 96.3% | 96.9% | 96.7% |
| % Did not answer | 3.8% | 3.1% | 3.3% |
|
Actigraphy Variablesa M (SD) |
|||
| # of scorable actigraphy days | 9.71 (3.48) | 9.85 (3.47) | 9.82 (3.47) |
| Avg. Deviation in bedtime across days (min) | 41.04 (19.15) | 42.10 (20.51) | 41.85 (20.17) |
| Avg. Deviation in morning waketime across days (min) | 34.00 (14.12) | 35.65 (17.64) | 35.26 (16.86) |
| Avg. Deviation in overnight duration across days (min) | 46.18 (14.60) | 49.65 (23.40) | 48.82 (21.67) |
| Avg. Deviation in nap duration across days (min; n=281) | 23.01 (12.32) | 22.75 (12.22) | 22.81 (12.22) |
| Average bedtime (hr:min)b | 21:55 (±57min) | 21:10 (±49min) | 21:21 (±55min) |
| Average waketime (hr:min)b | 07:21 (±50min) | 06:52 (±39min) | 06:59 (±44min) |
For the number of actigraphy days and sleep regularity variables (average deviations across days), exploratory t-tests were conducted to determine whether bedsharing groups differed on these parameters. No comparisons reached significance (all ps>.11), suggesting that habitual bedsharers and solitary sleepers showed similar levels of day-to-day consistency in their sleep patterns.
Exploratory t-tests showed that average bedtimes and waketimes significantly differed between habitual bedsharers and solitary sleepers (see pp. 21–22 in the main text for more information).
M=Mean; SD= Standard Deviation; SES= socioeconomic status; wk= week; hr= hours; min= minutes.
Materials
Health and Demographic questionnaire.
An in-house Health and Demographic questionnaire (previously described in Helm & Spencer, 2019) was used to collect basic demographic characteristics of the child and child’s family (i.e., race, ethnicity), as well as health and socioeconomic variables. Items of interest for our study included the child’s age, race, ethnicity, and sex, as well as socioeconomic measures including caregiver education level, household income, and caregivers’ employment status.
Actigraphy.
Actigraphy is a sensor-based, noninvasive means of estimating sleep by monitoring individuals’ levels of activity (accelerations; Meltzer et al., 2012). This study used the Philips Actiwatch Spectrum and Spectrum Plus devices (Philips Respironics, Bend OR). Both devices are waterproof and wrist-worn and collect movement data using an accelerometer with a sensitivity of <.01g and a sampling rate of 32 Hz. Data are stored in 15-second epochs. Both devices include an event marker button. Compared with polysomnography, research-grade actigraphy devices including Philips Spectrum models have shown a high degree of accuracy (>.96) and sensitivity (>.86) across adult populations (Marino et al., 2013), and have been validated for use in preschool-aged children and other pediatric populations (Meltzer et al., 2012; Meltzer, Walsh, & Peightal, 2015).
Sleep diary.
To measure children’s bedsharing habits and sleeping location, and to help verify actigraphy-derived daily sleep timings, caregivers completed a daily sleep diary (modified for children from diaries available through the National Institutes of Health: https://www.nhlbi.nih.gov/health-topics/all-publications-and-resources/sleep-diary). The diary included questions regarding children’s typical sleep location, bedsharing status, and with whom the bed is shared (if shared). Additionally, the diary included daily entries regarding nap and overnight sleep timing, sleep location(s) throughout the night, and any medications taken that could affect sleep. To quantify children’s bedsharing frequency specifically, caregivers were asked, “Is the bed normally shared?”, with the multiple-choice options of “yes”, “no” or “sometimes”. If bedsharing was indicated, a follow-up question asked, “If so, with whom? (Check all that apply)”, providing caregivers with the multiple response options of Parent, Sibling, Pet, and/or Other.
Procedure
Data in the current analyses were collected in the context of a larger ongoing study investigating the benefits of naps in on cognitive performance and memory consolidation in early childhood. Children were asked to wear the Actiwatch on their non-dominant wrist for 16 days, and caregivers were encouraged to “log” sleep events on the Actiwatch using the event marker button along with filling out the sleep diary for each day that their child wore the device. This 16-day window was scheduled to avoid daylight saving time. Additionally, caregivers were asked to complete the Health and Demographics questionnaire at any point during the 16-day window. Caregivers received up to $30 compensation for completing the questionnaires, and children received a children’s book.
Data Processing
Quantification of bedsharing groups and SES.
Based on caregivers’ responses to the question “Is the bed normally shared?” in children’s sleep diaries, children were classified as habitual bed sharers (caregiver selected “yes”), infrequent bed sharers (caregiver selected “sometimes”), and solitary sleepers (caregiver selected “no”). Additionally, children whose parents indicated that the child switched beds (either to or from a shared bed) in the night were classified as half-night bed sharers.
Following guidelines released from the Bureau of Justice Statistics (Berzofsky, Smiley-McDonald, Moore, & Krebs, 2014), we created a holistic composite of each family’s SES based on 3 items from the Health and Demographic questionnaire: 1) Caregivers’ highest level of education (rated 0 to 3, with “0” signifying less than high school and “3” indicating a Master’s or Doctorate-level degree); 2) Family income as a percentage of the federal poverty level, adjusting for family size (rated 0 to 3, with “0” signifying ≤ 100% of the federal poverty level, and “3” indicating ≥ 401% above the federal poverty level); and, 3) Caregivers’ employment status (rated 0 to 1, with “0” indicating unemployed). Given the multifaceted nature of SES and the disparate approaches used to quantify it (see Hoff, Laursen, & Bridges, 2012 for review), we viewed using a composite score as a way to account for some of the multiple dimensions contributing to socioeconomic level while also avoiding unnecessary multiple comparisons of highly related predictors. In line with measurement instructions specified in Berzofsky et al. (2014, pp. 16–23), scores from all three items were added, and the SES composite was treated as a continuous variable ranging from 0–7 for subsequent analyses.
Actigraphy scoring.
Following data collection, Actiwatch Spectrum data were scored using Philips Respironics Actiware software. Coders blind to the study hypotheses verified rest onsets and offsets manually using information obtained both from the actigraphs (i.e., event markers, light, activity level changes) and from caregivers’ sleep diary entries. If diary entries or event markers were missing, coders identified sleep onset by counting backward from the first 3 consecutive minutes of sleep identified by Actiware automatic activity thresholds. Similarly, sleep offset for missing entries was defined as the end of the final 5 consecutive minutes of sleep prior to an active/wake epoch in Actiware. Discrepancies between diary entries and actigraphs were resolved via consensus between two naïve coders, and rest intervals for which onsets/offsets could not be verified through consensus or any other method were excluded.
Once rest onsets and offsets were identified, the remainder of each rest interval was autoscored by Actiware using the Oakley method (Oakley, 1997). Sleep measures of interest for the present analysis included: 1) Average total sleep durations (i.e., actual time asleep after subtracting wake intervals) for overnight sleep, naps/daytime sleep, and 24-hour sleep across the data collection period; 2) average sleep efficiency (SE; total time asleep/total time in bed) for overnight sleep and naps; and, 3) average sleep onset latency (SOL) for overnight sleep bouts.
Statistical Analyses
All statistical analyses were conducted using SPSS Statistics version 25 (IBM Corp).
Bedsharing groups and demographic characteristics.
To explore bedsharing rates among children in our sample, we first quantified the relative percentages of children who fell into each bedsharing status (habitual, infrequent, half-night, and solitary sleeper) using descriptive statistics. We then used Fisher’s exact test to compare the identities of children’s sleep partners between habitual and infrequent bed sharers. Next, to determine whether relevant demographic variables (age, SES) were predicted by bedsharing status, we conducted separate univariate ANOVAs using bedsharing group as the independent variable. Levene’s test was applied to each ANOVA as well to test the assumption of equal variances (this test was not significant at the p<.05 level for either ANOVA, suggesting that this assumption was met). Significant ANOVAs were followed up with Bonferroni post-hoc tests, and demographic variables significantly related to bedsharing were added as covariates in the sleep comparisons outlined below.
Sleep quantity and quality comparisons.
Due to the confounding effect of waking up to move beds on actigraphy measures, half-night bed sharers were excluded from all sleep analyses. Specifically, it was difficult to reliably differentiate in this group which wake onset intervals (used in the sleep duration/efficiency calculations) were due to the child waking up to move beds, versus the child being disrupted by their bed partner after moving to share the bed. Additionally, given that half-night bed sharers theoretically have two SOLs (their initial SOL, plus a second SOL after waking up and moving beds), we were uncertain which SOL in this group would be conceptually comparable to the SOLs of the other groups. Infrequent bed sharers were also excluded from these analyses, given the non-uniformity in the percentage of days that children in this group shared a bed (mean=31% of days, range= 0%−100%) as well as the fact that some caregivers in this sample (26%) failed to report at all the days in which the child actually shared a bed. Thus, following exclusions, sleep comparisons were conducted only between habitual bed sharers (n=80) and solitary sleepers (n=257) who had 2 or more days of available actigraphy data (demographic information available in Table 1).
To assess differences in sleep quantity and quality between bedsharing children and solitary sleepers in accordance with our main hypotheses, we first ran independent samples t-tests evaluating whether habitual bed sharers differed from solitary sleepers in overnight, daytime, and 24-hour sleep durations, as well as in overnight SOL. For SE, we ran a 2 (Sleep Period) x 2 (Bedsharing Group) mixed ANOVA to determine both how SE might systematically differ between naps and overnight sleep, and whether habitual bedsharing resulted in a discrepancy between nap and overnight SE (i.e., worse overnight but better nap SE) compared to solitary sleeping. Significant differences for all t-tests and ANOVAs were followed up with ANCOVAs controlling for bedsharing-related demographic factors. Finally, to test the hypothesis that bed sharers’ sleep may be more disrupted by sibling bed partners than caregivers, we ran between-subjects t-tests assessing sleep differences (overnight/nap duration, SE, and SOL) between children who habitually bedshared with parents only compared to siblings only. Though we were also interested in preliminarily exploring how other sleep partners (e.g., pets) differently impacted sleep, the limited sample size of children who shared with sleep partners other than siblings or caregivers precluded such analyses; thus, our assessment was restricted to parents vs. siblings. Again, prior to running all t-tests and ANOVAs, we used Levene’s test to assess the assumption of equal variances, and applied Welch’s correction (denoted by “Welch’s t” in the results text) for any analyses that violated this assumption. For ANCOVAs, Levene’s test violations were handled by running the ANCOVA as a linear mixed model with a diagonal covariance structure, which allows for heterogeneity of variances.
Results
Frequency of Bedsharing and Sleep Partner Types, and Bedsharing Group Demographics
Frequency of bedsharing types.
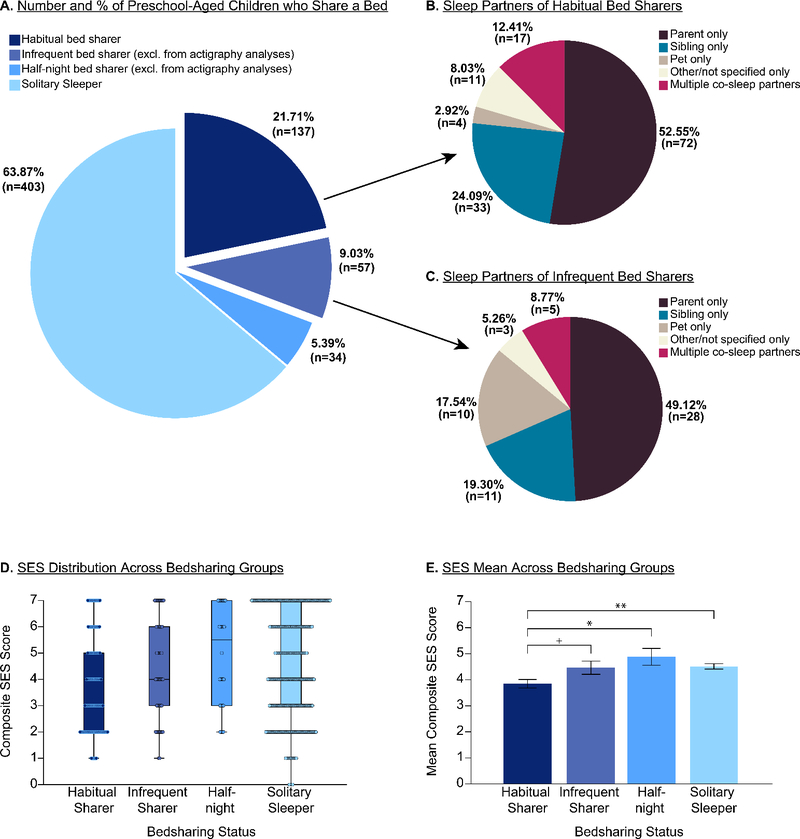
Although most children were solitary sleepers, a substantial percentage of children (36.1%) bedshared in at least some form, with 21.7% sharing a bed habitually according to caregivers’ sleep diary reports (Figure 1A). The primary sleep partner of all bedsharing children were parents; approximately 55.0% of bedsharing children (20.0% of the entire participant sample) shared with parents only, with an additional 12.2% of bed sharers (4.5% of all children) sharing with parents and at least one other sleep partner. Sibling bedsharing was also common; 19.2% of all bed sharers (7.0% of all children) shared with siblings only, and an additional 8.8% of sharers (3.1% of the overall sample) shared with a sibling and at least one other sleep partner (typically parents and/or pets). Despite the frequencies of parent and sibling bedsharing being similar between habitual and infrequent bed sharers (Fig. 1 B–C), a two-sided Fisher’s exact test indicated that the percentage composition of sleep partner identities significantly differed between habitual and infrequent bed sharers (FET= 11.63, p=.018, Cramer’s V= .26). Follow-up Bonferroni-adjusted z-tests (Sharpe, 2015), in which each sleep partner type was compared between habitual and infrequent bed sharers, showed that these bedsharing groups significantly differed in the percentage of children who bedshared with pets. Specifically, more infrequent bed sharers shared their bed with only pets (17.5% of children) compared with habitual bed sharers (2.9% of children; p<.001 after Bonferroni adjustment2), perhaps reflecting the dependence of pet bedsharing consistency on the sleep habits of the pet.
Figure 1. Bedsharing frequencies and characteristics.
A) Overall prevalence of bedsharing among preschool-aged children. B) Sleep partners of habitual bed sharers. C) Sleep partners of infrequent bed sharers. D) Distribution boxplots of household socioeconomic status (SES) of different bedsharing groups, and E) Mean SES of bedsharing groups. Error bars in E) represent ±1SE. **p<.01 after SPSS Bonferroni adjustment (calculated by multiplying the original p-value by the number of comparisons made). *p<.05 after Bonferroni adjustment. +p<.05 prior to Bonferroni adjustment, but significance was reduced to >.20 after correction.
Bedsharing group demographics.
Descriptive statistics regarding demographic variables for each bedsharing type are listed in Supplemental Table S1. A one-way ANOVA indicated no significant differences in children’s ages when compared across bedsharing groups (F(3,628)=.799, p=.495, ηp2=.004). However, there was a significant relation between bedsharing group and mean SES level (F(3,605)=4.62, p=.003, ηp2=.023), with habitual bed sharers being from lower SES households (Figure 1 D–E). Post-hoc tests employing the Bonferroni correction showed that the differences in SES were significant between habitual bed sharers and solitary sleepers (mean SES score difference=.67, adjusted p=.005) and between habitual bed sharers and half-night bed sharers (mean difference=1.04, adjusted p=.037), but not between any other groups (e.g., infrequent bed sharers) after adjusting for multiple comparisons (Fig. 1E).
Additional demographic analyses.
As an exploratory analysis, we considered whether bedsharing varied by ethnicity and race of the child. The frequency distributions of families identifying as Hispanic significantly differed across bedsharing groups (FET= 13.24, p=.029, Cramer’s V=.11). Follow-up Bonferroni-adjusted z-tests showed that a significantly higher percentage of habitual bed sharers identified as Hispanic compared to the percentages of solitary sleepers (adjusted p=.048) or half-night bed sharers (adj. p=.021), and that a higher percentage of half-night bed sharers identified as Non-Hispanic compared to habitual bed sharers (adj. p=.009). Furthermore, only 46.7% of habitually bedsharing families identified their children as White compared to an average of 61.8% of families across the whole sample (and 68% of solitary sleepers). The differences in racial diversity across bedsharing groups was significant (FET= 23.90, p<.001, Cramer’s V=.14), with Bonferroni-adjusted z-tests indicating a difference only between habitual bed sharers and solitary sleepers (p<.001). Importantly however, families of different ethnic and racial groups also differed significantly in SES; specifically, mean SES composite scores among participants who completed the demographic questionnaire were lower among Hispanic families compared to non-Hispanic White families (Mean(SD) Hispanic= 2.68(1.36), non-Hispanic White=5.02(1.77); Welch’s t(404.89)= 17.31, p<.001, d=1.49). Additionally, White families had significantly higher SES than families endorsing membership in other racial groups (Mean(SD) White=4.80(1.88), all other racial categories combined=3.64(1.91); t(573)=7.03, p<.001, d= .62).
Considering the relations between SES and race/ethnicity, and between these variables and bedsharing status, we ran one final follow-up analysis exploring whether race and ethnicity predicted bedsharing status when controlling for SES. To control for SES, we conducted a binary logistic regression using ethnicity (Non-Hispanic White vs. Hispanic, with Hispanic as the reference group), race (White vs. all other races combined, with all other races as the reference group), and SES (z-standardized) as predictors of group membership into either the habitual bed sharer or solitary sleeper bedsharing categories (as these were the only groups in which race and ethnicity percentages significantly differed). All predictors were added in the first block of the model, and goodness-of-fit was confirmed by a nonsignificant Hosmer-Lemeshow test (χ2=6.19, p=.52). The overall model including predictors was significant compared to the null model (χ2=22.58, p<.001), with the model explaining an additional 6.7% of the variance in outcome (R2=.067). The effect of Ethnicity was not significant: B(SE)= −.075(.27), Wald=.077, p=.78. However, the effect of Race was significant (B(SE)=.77(.23), Wald=11.455, p=.001), with estimated odds ratios suggesting that children of families identifying as White are approximately twice as likely to be solitary sleepers compared to non-White families (Exp(B)=2.16 (95% CI: 1.38, 3.37)). The effect of SES was also significant (B(SE)=.27(.13), Wald=4.32, p=.038), with the estimated odds ratio suggesting that children are 1.3x more likely to be a solitary sleeper with each standard deviation increase in SES (Exp(B)=1.31 (95% CI: 1.02, 1.69)).
Sleep Quantity and Quality Comparisons
Sleep durations of habitual bed sharers compared with solitary sleepers.
We first analyzed whether sleep quantity (durations) differed between our two most dichotomous bedsharing groups (habitual bed sharers versus solitary sleepers). Figure 2 depicts the distributions and averages of nap, overnight, and 24-hour sleep durations for habitual bed sharers and solitary sleepers. Between-subjects t-tests indicated significant differences in sleep duration between habitual bed sharers and solitary sleepers for all sleep bouts. Specifically, habitual bed sharers slept 15.6 minutes less overnight on average than solitary sleepers (t(335)=−3.08, p=.002, d=.395), and napped for 10.7 minutes more (t(279)=3.39, p=.001, d=.477). Despite their longer naptimes, habitual bed sharers’ 24-hour sleep durations were still approximately 13 minutes shorter than those of solitary sleepers on average (t(335)=−2.86, p=.004, d=.367); using only the nap sample, t(275)=−2.10, p=.036, d=.300), suggesting less total sleep among habitual bed sharers.
Figure 2. Sleep duration comparisons between bedsharers and solitary sleepers.
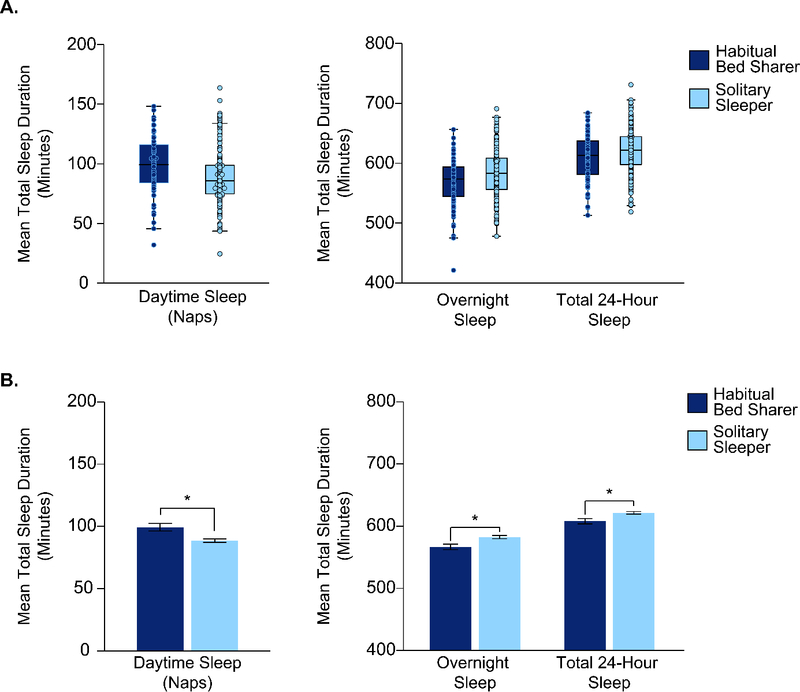
A) Distribution boxplots of sleep durations for daytime naps, overnight sleep, and sleep across 24 hours between habitual bed sharers and solitary sleepers. B) Mean sleep durations for daytime naps, overnight sleep, and sleep across 24 hours between habitual bed sharers and solitary sleepers. Error bars in B) represent ±1SE. *p<.05 after controlling for SES.
Given the differences in SES observed between habitual bed sharers and solitary sleepers, we also conducted 3 separate ANCOVA analyses including a) bedsharing status and b) SES (z-standardized for ease of interpretation) as predictors of children’s sleep durations for overnight sleep, naps, and total 24-hour sleep respectively. For overnight sleep, the main effect of bedsharing status on sleep duration remained significant even after controlling for SES, (F(1,323)=3.91, p=.049, ηp2=.012). The effect of SES was also significant (F(1,323)=24.76, p<.001, ηp2=.071), with parameter estimates suggesting that habitual bed sharers’ sleep durations were expected to increase by 12.2 minutes with every standard deviation increase in SES. There was no significant interaction between bedsharing status and SES on overnight sleep duration (F(1,323)=.063, p=.80, ηp2< .001), indicating that the beneficial effect of SES on overnight sleep duration was not significantly impacted by bedsharing group.
The main effect of bedsharing status on nap duration also remained significant after controlling for SES (F(1,268)=5.84, p=.016, ηp2=.021). The effect of SES on nap duration was significant as well (F(1,268)=22.48, p<.001, ηp2=.077), with parameter estimates predicting a 9.4-minute decrease in nap duration for habitual bed sharers with each standard deviation increase in SES. There was no significant interaction between bedsharing status and SES on children’s nap durations (F(1,268)=1.22, p=.27, ηp2=.005), again suggesting that the effects of SES on children’s nap durations were not significantly moderated by bedsharing group.
Finally, when assessing children’s total 24-hour sleep time, the main effect of bedsharing remained significant (F(1,323)=4.37, p=.037, ηp2=.013). There was also a main effect of SES (F(1,323)=14.55, p<.001, ηp2=.043), with parameter estimates predicting an increase in sleep duration of 10.4 minutes for every standard deviation increase in SES. The interaction between bedsharing status and SES was not significant (F(1,323)=.17, p=.68, ηp2=.001).
Sleep quality of habitual bed sharers versus solitary sleepers.
To assess the effects of bedsharing on SE (Figure 3A–B) and compare differences in SE across naps and overnight sleep, we ran a 2 (Sleep Period: Nap vs. Overnight, within-subjects) x 2 (Bedsharing Group: Habitual vs. Solitary, between-subjects) ANOVA. There was no main effect of Sleep Period (F(1,262)= .75, p=.39, ηp2=.003), indicating that SE did not differ systematically between naps and overnight sleep. There was also no main effect of Bedsharing Group (F(1,262)= .36, p=.36, ηp2=.003), and no Sleep Period x Bedsharing Group interaction (F(1,262)= .97, p=.33, ηp2=.004).
Figure 3. Sleep quality comparisons between bedsharers and solitary sleepers.
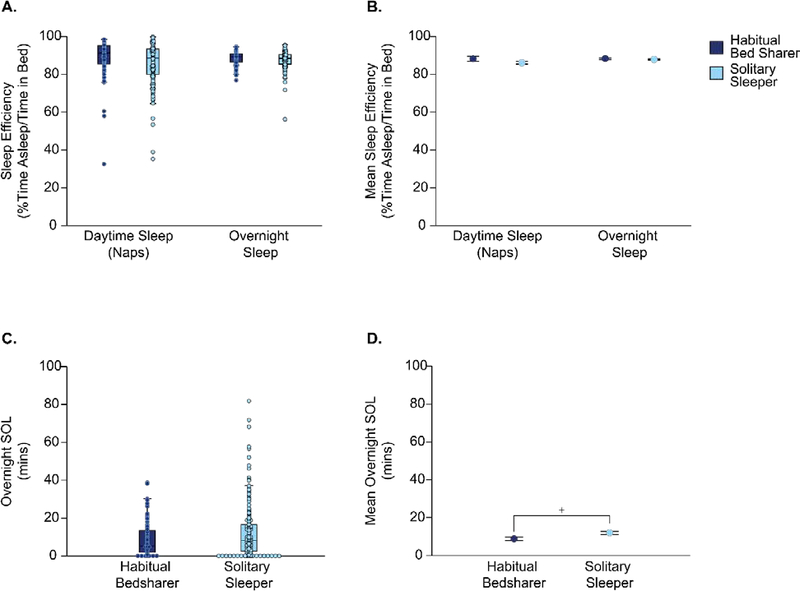
A) Distribution boxplots and B) simple means plots of nap and overnight % sleep efficiency (SE) between habitual bedsharers and solitary sleepers. C) Distribution boxplots and D) simple means plots of overnight sleep onset latency (SOL) between habitual bedsharers and solitary sleepers. Error bars on simple means plots represent ±1SE. +p<.10 after controlling for SES.
Regarding SOL (Figure 3C–D), we found a significant difference in overnight SOL between the groups (Welch’s t=−2.41, p=.017, d=.280). Contrary to our predictions, habitual bed sharers had a shorter SOL on average (M(SD)= 8.8 (9.2) min) than solitary sleepers (M(SD)= 12.0 (13.2) min). To control for SES, we performed an ANCOVA including bedsharing status and SES as predictors of overnight SOL, using the SPSS MIXED command with a diagonal covariance structure to adjust for unequal variances. The effect of bedsharing became nonsignificant (F(1,200.11)=2.83, p=.094). There was a significant main effect of SES (F(1,185.20)=13.61, p<.001), with parameter estimates suggesting a 2.53-minute increase in SOL for habitual bed sharers for every standard deviation increase in SES. The interaction between bedsharing status and SES was not significant (F(1,185.20)=.013, p=.91).
Sleep quantity and quality of children who habitually bedshare with either parents or siblings.
We explored whether the sleep of children who habitually shared a bed was influenced by who they shared a bed with. Specifically, we focused on differences between parent-child bedsharing and sibling bedsharing (Supplemental Figure S1), as these were the most common bedsharing arrangements and arrangements for which we had specific hypotheses. Prior to analyzing sleep partner effects on overnight sleep, we first conducted two independent-samples t-tests exploring whether parent-child bed sharers differed in age or SES from sibling bed sharers. There were no significant differences in either age or SES between the two groups (both ps>.42). Next, we conducted independent samples t-tests evaluating the effects of sleep partner identity on overnight and nap sleep duration, SE, and SOL. No comparisons reached significance (all ps>.18), suggesting no substantive effect of partner type on children’s sleep.
Additional control and exploratory analyses.
Given that bedsharing predicted total sleep durations but not wake during sleep (captured by SE), we explored post-hoc whether habitual bedsharers and solitary sleepers differed significantly in their typical bedtimes and waketimes (Table 1 and Figure 4) to help explain sleep duration differences. Using between subjects t-tests (Fig. 4C), we found that habitual bedsharers both went to bed significantly later (mean difference 45 minutes; t(334)=6.81, p<.001, d=.872) and woke up significantly later (mean difference ~29 minutes; Welch’s t(111.84)=4.79, p<.001, d=.648) compared to solitary sleepers. The effect of bedsharing status on both bedtimes and waketimes also remained significant when controlling for SES (see Appendix Supplemental Analyses section for full ANCOVA results and parameter estimates), with the effect of SES also being significant for both measures.
Figure 4. Bedtimes and waketimes of habitual bedsharers vs. solitary sleepers.
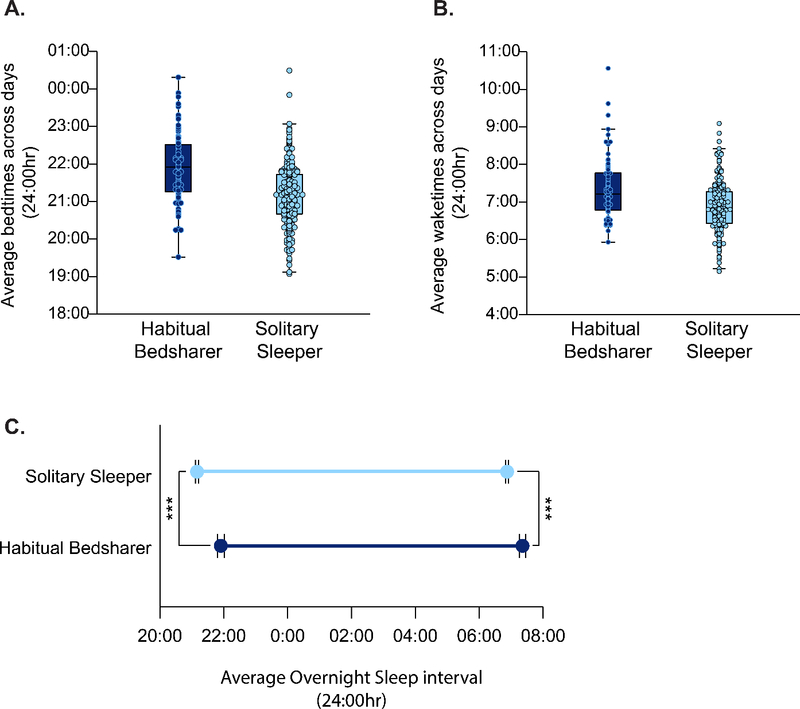
A) Distribution boxplots of average bedtimes across actigraphy days for habitual bedsharers and solitary sleepers. B) Distribution boxplots of average waketimes across actigraphy days for habitual bedsharers and solitary sleepers. C) Dropline plot depicting the average timing of habitual bedsharers’ and solitary sleepers’ overnight sleep. Error bars in C) represent ±1SE. ***p<.001, even after controlling for SES (see supplemental material for control analyses).
Additionally, although children’s age did not differ significantly between bedsharing groups, given the known effects of age on sleep length and nap transitions (Kurth et al., 2016), we also ran supplemental ANCOVA analyses including age as a covariate for our significant sleep duration findings (comparing nap, overnight, and 24-hr sleep between habitual bedsharers and solitary sleepers) and the significant bedtime/waketime findings reported above. When controlling for age, the effect of bedsharing status remained significant for all duration and bedtime/waketime measures, with the independent effect of age also being significant for 24-hour sleep duration (but not nap or overnight duration separately) and bedtime (but not waketime). These analyses are reported in full in the Appendix Supplemental Analyses section.
Discussion
The purpose of our study was threefold. First, we endeavored to gain a more holistic understanding of the range of bedsharing practices and associated background factors that occur during the preschool years in a sample of U.S. children, by expanding the study of bedsharing to include sleep partners beyond parents and caregivers. Our results suggest that child bedsharing is a frequent occurrence in families with 3–5-year-old children, with over 30% of children sharing a bed in some form. Additionally, although bedsharing with parents alone is the most common arrangement observed, the range of sleep partners that children may share a bed with, from siblings to pets to other caregivers, is diverse and non-trivial. Specifically, only approximately half of all bedsharing occurred in the context of parent sharing alone, and while bedsharing with a sibling alone was the second most common arrangement, sharing with multiple partners or pets occurred in more than 10% of all bedsharing settings. The fact that these additional arrangements and their effects have not been examined previously in early childhood (and could not be probed more thoroughly in our study due to sample size limitations) indicates an opportunity for future work to consider the dynamics of bedsharing beyond the dyadic caregiver-child framework.
We also found that children who bedshared habitually came from significantly lower SES homes on average than children who either did not bedshare or only bedshared for part of the night. This relation could suggest that bedsharing in our sample might be determined in part by socioeconomic pressures rather than preferences. For instance, the fact that habitual bed sharers come from lower-SES households on average may mean that bedsharing is a matter of necessity due to housing or space constraints (smaller houses with fewer rooms) and/or financial constraints (cannot afford the additional bed). Alternatively, lower SES could be associated with other unobserved variables such as heightened child stress or behavioral difficulties (Bradley & Corwyn, 2002; Huaqing qi & Kaiser, 2003; Letourneau, Duffett-Leger, Levac, Watson, & Young-Morris, 2013; Lupien, King, Meaney, & McEwen, 2000), which may induce children or parents to prefer bed sharing as a matter of regulation or emotional support.
Furthermore, we found greater ethnic and racial diversity among bedsharing families. More habitual bed sharers identified as Hispanic compared to solitary sleepers or part-night bed sharers, and fewer habitual bed sharers identified as White compared to solitary sleepers. Our observations are similar to prior work suggesting differences in bedsharing prevalence across racial and ethnic groups (Latz et al., 1999; Lozoff et al., 1984; Mindell et al., 2013), though no prior work to our knowledge has found a higher prevalence of child bedsharing among U.S. Hispanic families specifically. However, when we controlled for SES, identifying as Hispanic did not independently impact the likelihood of bedsharing, which is in line with other studies indicating either no differences in bedsharing between Hispanic and non-Hispanic families (Milan, Snow, & Belay, 2007) or reduced parent bedsharing among Hispanic families compared to other non-Hispanic minority groups (Mathews, Joyner, Oden, Alamo, & Moon, 2015). Nonetheless, race remained a significant predictor of bedsharing even when controlling for SES in our sample, suggesting that bedsharing may be influenced by non-SES social factors (e.g. culture, beliefs) as well. Though sample limitations prevented a more fine-grained analysis of bedsharing differences between racial subgroups, future work should endeavor to explore these differences across a broader range of cultures (e.g., Mindell et al., 2013).
Our second aim was to critically examine relations between bedsharing and child sleep by testing these relations using more objective sleep measures than those found in previous work. To our knowledge, ours is the first study of this scale to measure associations between bedsharing and young children’s sleep using actigraphy, and the first to analyze napping in addition to overnight and 24-hour sleep. We found that children who habitually bedshare sleep for significantly less time across 24 hours than children who sleep alone, even when accounting for the differences in SES. Furthermore, we found (contrary to our expectations) that habitual bed sharers had marginally shorter overnight sleep onset latencies than solitary sleepers, though these bed sharers also went to bed significantly later (and woke up later) than solitary sleepers. Also in contrast to our predictions, we did not find relations between bedsharing and SE, a sleep quality measure that identifies the relative amount of time that children are registered as awake vs. asleep during a sleep bout. While previous studies have found relations between caregiver-reported child sleep disturbances and bedsharing (e.g. Cortesi et al., 2008; Hayes et al., 2001), our null result could indicate that these prior findings were based on bedsharing parents’ increased awareness of child wakings rather than actual differences in sleep disruption. Alternatively, as caregiver reports also capture more emotional elements of disruption such as sleep anxiety (Cortesi et al., 2008), it could be that more emotion-focused sleep quality measures may have revealed differences between bedsharing groups. Additionally, future work employing finer-grained methods such as sleep staging or fragmentation analyses (# of wakings rather than % of time awake) may reveal more subtle differences in child sleep disturbance not captured by SE, particularly if bedsharing children quickly fall back to sleep after being disturbed or awoken.
With respect to children’s sleep durations, although habitually bedsharing children slept for significantly less time overnight (presumably due to their later bedtimes, even when accounting for their later wake onset), there was evidence to suggest that they may attempt compensate for lost overnight sleep by taking longer naps. However, even with longer naps, habitual bed sharers’ sleep time across 24 hours was still shorter than that of solitary sleepers. It is intriguing that SES itself also predicted sleep duration differences for all sleep bouts (naps, overnight sleep, and 24-hour sleep), and that higher SES was related to shorter naps but longer overnight and 24-hour total sleep time. Why SES relates in opposing fashion to nap and overnight sleep durations is an open question, though it could indicate that longer naps are less essential for children from high-SES families on account of longer and higher quality overnight sleep (Ward et al., 2008) or greater brain development (Riggins & Spencer, 2020). Regardless, our results may indicate the importance of maintaining nap opportunities in schools, to allow children who might not get the same overnight sleep opportunities at home to compensate at least partially for their lost sleep.
Our final study objective was to explore how the relations between bedsharing and child sleep health may be moderated by the type of sleep partner with whom children share a bed. Although a lack of literature in this area prevented us from making strong a priori predictions, we speculated that perhaps sibling-child bedsharing would result in more child sleep disruptions than parent-child bedsharing, due to the potentially less authoritative and more social nature of sibling relationships. Contrary to our predictions, we found no differences in children’s sleep quantity or quality when comparing habitual parent-child bed sharers to sibling-child bed sharers. Our result also contrasts conceptually from one of the only studies to assess differences in child sleep between parent-child and sibling-child bed sharers, which found that sibling-child bed sharing was unassociated with child sleep difficulties while parent-child bed sharing was (Tan et al., 2009). However, given that the prior study focused specifically on adopted children and relied solely on caregivers’ reports of child sleep, this difference in findings is not surprising. In turn, the fact that children’s sleep partner did not predict sleep differences suggests that when measured objectively, children’s sleep may be impacted equally by different human sleep partners at this age. As a relatively low number of children in our sample bedshared with household pets, we were unable to compare the sleep quality of pet bedsharing children to that of human bedsharing children; nonetheless, it would be of interest in future work to explore whether pet bedsharing confers benefits or disadvantages for child sleep, particularly given recent reports of paradoxical relations between pet bedsharing and sleep in adults (e.g. Hoffman, Stutz, & Vasilopoulos, 2018; Patel et al., 2017; Rodriguez, Bryce, Granger, & O’Haire, 2018).
Although our robust sample size, sample diversity, and the use of actigraphy to measure sleep are strengths of the current work, some limitations must be noted. First, we recognize that while actigraphy provides a more objective measure of sleep compared to the questionnaire-based sleep measures of prior work, actigraphy is nonetheless limited in its accuracy. In this case, it is possible that the actigraph picked up movement from the bed partners that was scored as wake for the child when the child may have been, in reality, undisturbed. To address this issue, future studies should consider use of actigraphy on both participants in the bedsharing dyad (parent and child or siblings) to assess coincident wakings. Second, akin to prior work in this area, our study is purely observational, with measures of sleep quantity and quality taken concurrently with questions probing bedsharing habits. Thus, we are unable to draw any conclusions regarding direction of causality from this study. Short-term experimental work in which young children are assigned to bedshare or not bedshare is critically needed to complement the observational studies conducted on this topic, and to probe whether bedsharing in fact “causes” sleep disturbances or differences at this age. Third, future work should make sure to inquire more thoroughly about families’ bedsharing history and reasons for bedsharing, as prior work has suggested differential associations between sleep and reactive vs. purposeful or “intentional” bedsharing (Mileva-Seitz et al., 2017). Similarly, knowledge of participants’ sleep patterns at earlier ages prior to data collection would provide additional insights, along with more extensive knowledge of bedtime routines leading up to sleep (including naps, which often occurred outside of the home in this sample and thus could have been affected by subtle differences in preschool/daycare teachers’ nap-promoting routines). Such factors could be used for more complex analytic strategies such as structural equation modeling, which could provide more in-depth results by modeling bidirectional relationships between relevant variables. Finally, our findings likely only explain bedsharing in the U.S. and, even so, bedsharing practices may vary regionally. It will be important to extend these findings to more geographical locations.
Overall, our study provides further insight into the diversity and prevalence of bedsharing practices among preschool-aged children in the U.S., as well as how bedsharing and related factors may be associated with objective measure of child sleep. As early childhood presents a critical period for sleep as well as broader brain and cognitive development (Kurth, Achermann, Rusterholz, & Lebourgeois, 2013; Riggins & Spencer, 2020), it is vital to understand the many factors that may influence sleep at this age, including children’s external sleeping arrangements. Thus, while additional longitudinal and experimental work is needed, we hope that our work may be combined with future research to inform pediatric and policy recommendations regarding best sleep practices during early childhood.
Supplementary Material
Acknowledgements
We would like to thank all of the families who participated in our work.
Footnotes
Declaration of Interest: No conflicts of interest to disclose.
As studies differ in their recommendations of a minimum number of days needed for reliable actigraphy measures, we first ran our statistical analyses using both a 2-day minimum (Helm & Spencer, 2019; Thomas & Burr, 2008) and a 3-day minimum (as in Cremone et al., 2018; De Jong et al., 2016). All significant findings remained either way; thus, in the interest of data retention, findings reported in the main text use the 2-day minimum.
For Bonferroni adjustment, the original p-values were multiplied by the number of comparisons and compared to the conventional α<.05 threshold.
Data availability statement:
Access to blinded data for this paper is available on OSF via https://osf.io/5r8te/?view_only=fd9066b50e6046a393ac5fe0e8c56ee2
References
- Ball Helen L. (2006). Caring for twin infants: sleeping arrangements and their implications. Evidence Based Midwifery, 4(1), 10–16. [Google Scholar]
- Ball Helen Louise. (2006). Night-time infant care: cultural practice, evolution, and infant development. In Childrearing and infant care issues : a cross-cultural perspective (pp. 47–61). Melbourne: Nova Science. [Google Scholar]
- Berzofsky M, Smiley-McDonald H, Moore A, & Krebs C (2014). Measuring Socioeconomic Status (SES) in the NCVS: Background, Options, and Recommendations. Bureau of Justice Statistics, U.S. Department of Justice, (0213170), 65. 10.1007/BF03061070 [DOI] [Google Scholar]
- Bradley RH, & Corwyn RF (2002). Socioeconomic status and child development. Annual Review of Psychology, 53, 371–399. 10.1146/annurev.psych.53.100901.135233 [DOI] [PubMed] [Google Scholar]
- Cortesi F, Giannotti F, Sebastiani T, Vagnoni C, & Marioni P (2008). Cosleeping versus solitary sleeping in children with bedtime problems: child emotional problems and parental distress. Behavioral Sleep Medicine, 6(2), 89–105. 10.1080/15402000801952922 [DOI] [PubMed] [Google Scholar]
- Cremone A, de Jong DM, Kurdziel LBF, Desrochers P, Sayer A, LeBourgeois MK, … McDermott JM (2018). Sleep Tight, Act Right: Negative Affect, Sleep and Behavior Problems During Early Childhood. Child Development, 89(2), e42–e59. 10.1111/cdev.12717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crittenden AN, Samson DR, Herlosky KN, Mabulla IA, Mabulla AZP, & McKenna JJ (2018). Infant co-sleeping patterns and maternal sleep quality among Hadza hunter-gatherers. Sleep Health, 4(6), 527–534. 10.1016/j.sleh.2018.10.005 [DOI] [PubMed] [Google Scholar]
- Damato EG, Brubaker JA, & Burant C (2012). Sleeping Arrangements in Families With Twins. Newborn and Infant Nursing Reviews, 12(3), 171–178. 10.1053/j.nainr.2012.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Jong DM, Cremone A, Kurdziel LBF, Desrochers P, LeBourgeois MK, Sayer A, … Spencer RMC (2016). Maternal Depressive Symptoms and Household Income in Relation to Sleep in Early Childhood. Journal of Pediatric Psychology, 41(9), 961–970. 10.1093/jpepsy/jsw006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galland BC, Taylor BJ, Elder DE, & Herbison P (2012). Normal sleep patterns in infants and children: A systematic review of observational studies. Sleep Medicine Reviews, 16(3), 213–222. 10.1016/j.smrv.2011.06.001 [DOI] [PubMed] [Google Scholar]
- Goldberg W, & Keller M (2007). Parent-Infant Co-Sleeping: Why the Interest and Concern? Infant and Child Development, 16, 331–339. [Google Scholar]
- Hayes MJ, Parker KG, Sallinen B, & Davare AA (2001). Bedsharing, temperament, and sleep disturbance in early childhood. Sleep, 24(6), 657–662. 10.1093/sleep/24.6.657 [DOI] [PubMed] [Google Scholar]
- Helm AF, & Spencer RMC (2019). Television use and its effects on sleep in early childhood. Sleep Health, 5(3), 241–247. 10.1016/j.sleh.2019.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoff E, Laursen B, & Bridges K (2012). Measurement and Model Building in Studying the Influence of Socioeconomic Status on Child Development. In The Cambridge Handbook of Environment in Human Development (pp. 590–606). 10.1017/cbo9781139016827.033 [DOI] [Google Scholar]
- Hoffman CL, Stutz K, & Vasilopoulos T (2018). An Examination of Adult Women’s Sleep Quality and Sleep Routines in Relation to Pet Ownership and Bedsharing. Anthrozoos, 31(6), 711–725. 10.1080/08927936.2018.1529354 [DOI] [Google Scholar]
- Horsley T, Clifford T, Barrowman N, Bennett S, Yazdi F, Sampson M, … Côté A (2007). Benefits and harms associated with the practice of bed sharing a systematic review. Archives of Pediatrics and Adolescent Medicine, 161(3), 237–245. 10.1001/archpedi.161.3.237 [DOI] [PubMed] [Google Scholar]
- Huaqing qi C, & Kaiser AP (2003). Behavior Problems of Preschool Children From Low-Income Families: Review of the Literature. Topics in Early Childhood Special Education, 23(4), 188–216. 10.1177/02711214030230040201 [DOI] [Google Scholar]
- Jenni OG, Fuhrer HZ, Iglowstein I, Molinari L, & Largo RH (2005). A Longitudinal Study of Bed Sharing and Sleep Problems Among Swiss Children in the First 10 Years of Life. Pediatrics, 115(1), 233–240. 10.1542/peds.2004-0815e [DOI] [PubMed] [Google Scholar]
- Kim E, Lee R, & Cain KC (2017). Cosleeping, sleep disturbances, children’s behavioral problems, and parenting self-efficacy among Korean American families. Journal of Child and Adolescent Psychiatric Nursing, 30(2), 112–120. 10.1111/jcap.12182 [DOI] [PubMed] [Google Scholar]
- Kurth S, Achermann P, Rusterholz T, & Lebourgeois MK (2013). Development of brain EEG connectivity across early childhood: Does sleep play a role? Brain Sciences, 3(4), 1445–1460. 10.3390/brainsci3041445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurth S, Lassonde JM, Pierpoint LA, Rusterholz T, Jenni OG, McClain IJ, … LeBourgeois MK (2016). Development of nap neurophysiology: preliminary insights into sleep regulation in early childhood. Journal of Sleep Research, 25(6), 646–654. 10.1111/jsr.12427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latz S, Wolf AW, & Lozoff B (1999). Cosleeping in context: Sleep practices and problems in young children in Japan and the United States. Archives of Pediatrics and Adolescent Medicine, 153(4), 339–346. 10.1001/archpedi.153.4.339 [DOI] [PubMed] [Google Scholar]
- Letourneau NL, Duffett-Leger L, Levac L, Watson B, & Young-Morris C (2013). Socioeconomic Status and Child Development: A Meta-Analysis. Journal of Emotional and Behavioral Disorders, 21(3), 211–224. 10.1177/1063426611421007 [DOI] [Google Scholar]
- Liu X, Liu L, & Wang R (2003). Bed sharing, sleep habits, and sleep problems among Chinese school-aged children. Sleep, 26(7), 839–844. 10.1093/sleep/26.7.839 [DOI] [PubMed] [Google Scholar]
- Lozoff B, Wolf AW, & Davis NS (1984). Cosleeping in urban families with young children in the United States. Pediatrics, 74(2), 171–182. 10.1016/s0002-7138(09)60436-2 [DOI] [PubMed] [Google Scholar]
- Lozoff Betsy, Askew GL, & Wolf AW (1996). Cosleeping and early childhood sleep problems: Effects of ethnicity and socioeconomic status. Journal of Developmental and Behavioral Pediatrics, 17(1), 9–15. 10.1097/00004703-199602000-00002 [DOI] [PubMed] [Google Scholar]
- Lupien SJ, King S, Meaney MJ, & McEwen BS (2000). Child’s stress hormone levels correlate with mother’s socioeconomic status and depressive state. Biological Psychiatry, 48(10), 976–980. 10.1016/S0006-3223(00)00965-3 [DOI] [PubMed] [Google Scholar]
- Marco CA, Wolfson AR, Sparling M, & Azuaje A (2011). Family Socioeconomic Status and Sleep Patterns of Young Adolescents. Behavioral Sleep Medicine, 10(1), 70–80. 10.1080/15402002.2012.636298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, … Buxton OM (2013). Measuring sleep: Accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep, 36(11), 1747–1755. 10.5665/sleep.3142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews AA, Joyner BL, Oden RP, Alamo I, & Moon RY (2015). Comparison of Infant Sleep Practices in African–American and US Hispanic Families: Implications for Sleep-Related Infant Death. Journal of Immigrant and Minority Health, 17(3), 834–842. 10.1007/s10903-014-0016-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenna JJ, Ball HL, & Gettler LT (2007). Mother-infant cosleeping, breastfeeding and sudden infant death syndrome: What biological anthropology has discovered about normal infant sleep and pediatric sleep medicine. American Journal of Physical Anthropology, 134(S45-Supplement: Yearbok of Physical Anthropology), 133–161. 10.1002/ajpa.20736 [DOI] [PubMed] [Google Scholar]
- Meltzer LJ, Montgomery-Downs HE, Insana SP, & Walsh CM (2012). Use of actigraphy for assessment in pediatric sleep research. Sleep Medicine Reviews, 16(5), 463–475. 10.1016/j.smrv.2011.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer LJ, Walsh CM, & Peightal AA (2015). Comparison of actigraphy immobility rules with polysomnographic sleep onset latency in children and adolescents. Sleep and Breathing, 19(4), 1415–1423. 10.1007/s11325-015-1138-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milan S, Snow S, & Belay S (2007). The context of preschool children’s sleep: Racial/ethnic differences in sleep locations, routines, and concerns. Journal of Family Psychology, 21(1), 20–28. 10.1037/0893-3200.21.1.20 [DOI] [PubMed] [Google Scholar]
- Mileva-Seitz VR, Bakermans-Kranenburg MJ, Battaini C, & Luijk MPCM (2017). Parent-child bed-sharing: The good, the bad, and the burden of evidence. Sleep Medicine Reviews, 32, 4–27. 10.1016/J.SMRV.2016.03.003 [DOI] [PubMed] [Google Scholar]
- Mindell JA, Sadeh A, Kwon R, & Goh DYT (2013). Cross-cultural differences in the sleep of preschool children. Sleep Medicine, 14(12), 1283–1289. 10.1016/j.sleep.2013.09.002 [DOI] [PubMed] [Google Scholar]
- Moon RY, Darnall RA, Feldman-Winter L, Goodstein MH, & Hauck FR (2016). SIDS and other sleep-related infant deaths: Updated 2016 recommendations for a safe infant sleeping environment. Pediatrics, 138(5). 10.1542/peds.2016-2938 [DOI] [PubMed] [Google Scholar]
- Oakley NR (1997). Validation with polysomnography of the Sleepwatch sleep/wake scoring algorithm used by the Actiwatch activity monitoring system. Bend: Mini Mitter, Cambridge Neurotechnology. [Google Scholar]
- Okami P, Weisner T, & Olmstead R (2002). Outcome correlates of parent-child bedsharing: an eighteen-year longitudinal study. Journal of Developmental and Behavioral Pediatrics : JDBP, 23(4), 244–253. [DOI] [PubMed] [Google Scholar]
- Owens JA (2004, October 28). Sleep in children: Cross-cultural perspectives. Sleep and Biological Rhythms, Vol. 2, pp. 165–173. 10.1111/j.1479-8425.2004.00147.x [DOI] [Google Scholar]
- Patel SI, Miller BW, Kosiorek HE, Parish JM, Lyng PJ, & Krahn LE (2017). The Effect of Dogs on Human Sleep in the Home Sleep Environment. Mayo Clinic Proceedings, 92(9), 1368–1372. 10.1016/j.mayocp.2017.06.014 [DOI] [PubMed] [Google Scholar]
- Riggins T, & Spencer RMC (2020). Habitual sleep is associated with both source memory and hippocampal subfield volume during early childhood. Scientific Reports, 10(1). 10.1038/s41598-020-72231-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodriguez KE, Bryce CI, Granger DA, & O’Haire ME (2018). The effect of a service dog on salivary cortisol awakening response in a military population with posttraumatic stress disorder (PTSD). Psychoneuroendocrinology, 98(April), 202–210. 10.1016/j.psyneuen.2018.04.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salm Ward TC, & Ngui EM (2015). Factors Associated with Bed-Sharing for African American and White Mothers in Wisconsin. Maternal and Child Health Journal, 19(4), 720–732. 10.1007/s10995-014-1545-5 [DOI] [PubMed] [Google Scholar]
- Sharpe D (2015). Your chi-square test is statistically significant: Now what? Practical Assessment, Research and Evaluation, 20(8), 1–10. 10.7275/tbfa-x148 [DOI] [Google Scholar]
- Tan TX, Marfo K, & Dedrick RF (2009). Preschool-age adopted chinese children’s sleep problems and family sleep arrangements. Infant and Child Development, 18(5), 422–440. 10.1002/icd.630 [DOI] [Google Scholar]
- Thomas KA, & Burr RL (2008). Circadian Research in Mothers and Infants: How Many Days of Actigraphy Data Are Needed to Fit Cosinor Parameters? Journal of Nursing Measurement, 16(3). 10.1891/1061-3749.16.3.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkovich E, Ben-Zion H, Karny D, Meiri G, & Tikotzky L (2015). Sleep patterns of co-sleeping and solitary sleeping infants and mothers: A longitudinal study. Sleep Medicine, 16(11), 1305–1312. 10.1016/j.sleep.2015.08.016 [DOI] [PubMed] [Google Scholar]
- Ward TM, Gay C, Anders TF, Alkon A, & Lee KA (2008). Sleep and napping patterns in 3-to-5-year old children attending full-day childcare centers. Journal of Pediatric Psychology, 33(6), 666–672. 10.1093/jpepsy/jsm102 [DOI] [PubMed] [Google Scholar]
- Weissbluth M (1995). Naps in Children: 6 Months-7 Years. Sleep, 18(2). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Access to blinded data for this paper is available on OSF via https://osf.io/5r8te/?view_only=fd9066b50e6046a393ac5fe0e8c56ee2