Abstract
Background
Due to the current Coronavirus Disease 2019 (COVID-19) pandemic, there is a realization for innovation in procedures and protocols to minimize hospital stay and at the same time ensure continued evidence-based treatment delivered to the patients. We present a same-day discharge protocol for transcatheter mitral valve repair (TMVR) using MitraClip under general anaesthesia in a six-patient case series. This protocol aims to reduce the length of hospital stay, thereby minimizing potential for nosocomial COVID-19 infections and to promote safe discharge with cautious follow-up.
Case summary
Six patients with severe symptomatic mitral valve (MV) regurgitation underwent successful transfemoral MV repair using standard procedures. Following repair, patients were monitored on telemetry in the recovery area for 3 h, ambulated to assess vascular access stability and underwent post-procedural transthoracic echocardiogram to assess for any pericardial effusion or post-procedural prosthetic mitral stenosis.
Conclusion
Same-day discharge after TMVR is possible when done cautiously with close follow-up, can minimize hospital stay, improve resource utilization, and reduce risk of nosocomial COVID-19 infection.
Keywords: Transcatheter mitral valve repair, MitraClip, Same-day discharge, Day case procedure, Case series, Case report, COVID-19
Learning points
Patients with stable heart failure symptoms, low bleeding risk, and without intraprocedural complications can be considered for same-day discharges (SDDs) following transcatheter mitral valve repair.
SDD to selected patients might be of benefit in preventing potential exposure during the Coronavirus Disease 2019 pandemic.
Introduction
Mitral valve disease is the most common valvular disease in the USA with moderate or higher mitral regurgitation (MR) present in ∼2% of the US adult population.1 Transcatheter mitral valve repair (TMVR) using MitraClip is an effective treatment option with low complication rates for severe symptomatic primary MR patients at high risk for open-heart surgery or severe secondary MR patients who remain symptomatic despite optimization of medical therapy.2,3 Over the past year, elective procedures and surgeries were initially cancelled to mitigate exposure to the Coronavirus Disease 2019 (COVID-19).4 Later on, they were rescheduled after implementing rules and restrictions using local, state, and federal guidelines to prevent exposure to patients and healthcare personnel.5 There is a dire need for innovation in procedural protocols to adapt to this change, which experts believe will remain relevant even after the pandemic.6 Given the potential risk of delaying treatment for patients with severe symptomatic MR, we developed a protocol for same-day discharge (SDD) for TMVR using MitraClip in the form of a case series with the goal of reducing the length of stay, resource utilization, and risk for nosocomial COVID-19 infection.
Timeline
| Characteristics | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | |
|---|---|---|---|---|---|---|---|
| Age | 80 | 89 | 92 | 83 | 62 | 74 | |
| Sex | Male | Male | Male | Male | Male | Male | |
| Hypertension | Present | Present | Present | Present | Absent | Present | |
| Coronary artery disease | Non-obstructive disease | None | Mild | none | Mild | Present | |
| Chronic kidney disease | None | None | III | none | III | III | |
| Atrial fibrillation present? | Yes | No | No | No | No | Yes | |
| Symptoms | Exertional dyspnoea | Exertional dyspnoea | Progressive dyspnoea | Exertional dyspnoea | Dyspnoea lower extremity swelling orthopnoea | Exertional dyspnoea | |
| Katz score | 6 | 6 | 6 | 6 | 6 | 6 | |
| Exam | 3/6 holosystolic murmur best heard at the apex without radiation to the axilla | 3/6 holosystolic murmur best heard at the apex with radiation to the axilla | 3/6 holosystolic murmur best heard at the apex with radiation to the axilla 2+ pitting oedema | 3/6 holosystolic murmur best heard at the apex with radiation to the axilla | 4/6 holosystolic murmur best heard at the apex without radiation to the axilla | 3/6 holosystolic murmur best heard at the apex without radiation to the axilla | |
| New York Heart Association/American Heart Association | IIIC | IIIC | IIID | IIIC | IV | III | |
| Brain natriuretic peptide | 186 | 119 | 2752 | 191 | 189 | 79 | |
| Ejection fraction (%) | 65 | 70 | 45 | 55 | 30 | 50 | |
| Society of Thoracic Surgeons score (%) | Repair | 1.4 | 2 | 7.7 | 2.5 | 3.4 | 3.5 |
| Replacement | 2.4 | 2.3 | 12.9 | 3.4 | 6.4 | 4.6 | |
| Regurgitation type | Primary | Primary | Functional | Primary | Functional | Functional | |
| Regurgitation jet | Eccentric | Eccentric | Eccentric | Central | Eccentric | Eccentric | |
| Mitral valve mean gradient (mmHg) | Pre-clip | 1 | 2 | 2 | 2 | 2 | 2 |
| Post-clip | 1 | 1 | 1 | 3 | 2 | 3 | |
| Mitral regurgitation grade | Pre-clip | 4+ | 4+ | 4+ | 4+ | 4+ | 4+ |
| Post-clip | Trace | Trace | Trace | 2+ | 1+ | 1+ | |
| Left ventricular end-systolic diameter (cm) | 3.5 | 6.4 | 3.48 | 3.4 | 6.73 | 5.46 | |
| Left ventricular end-diastolic diameter (cm) | 5.2 | 3.4 | 4.67 | 4.8 | 7.07 | 6.38 | |
| Effective regurgitant orifice area (cm2) | Pre-clip | 0.62 | 1.31 | 0.50 | 0.40 | 0.37 | 0.27 |
| Post-clip | 0.09 | 0.15 | Indeterminate | 0.19 | 0.05 | Not available | |
| Procedure performed | XTR to A2–P2 | XTR to A2–P3 | XTR to A2–P2 | XTR to A2–P2 | XTW to A2–P2 | XTW to A2–P2 DES to mid-left anterior descending artery | |
| Anaesthesia | General | General | General | General | General | General | |
| Access site | Right femoral vein | Right femoral vein | Right femoral vein | Right femoral vein | Right femoral vein | Right femoral vein Right femoral artery |
|
| Procedural time (min) | 120 | 124 | 95 | 91 | 91 | 174 | |
| Number of clips | 1 | 1 | 1 | 1 | 1 | 2 | |
| Anticoagulation on discharge | Aspirin Apixaban | Aspirin | Aspirin | Aspirin | Aspirin | Aspirin Plavix Coumadin |
|
| HAS-BLED score | 2 | NA | NA | NA | NA | 3 | |
| Electrocardiogram on discharge | Normal sinus rhythm | Sinus rhythm with first degree AV block | Sinus rhythm with old left bundle branch block | Normal sinus rhythm | Paced rhythm (A-sensed. V-paced) | Atrial fibrillation | |
| Readmission or emergency department visits post-discharge | None | None | None | None | None | Readmitted 6 days later for acute gastrointestinal bleeding secondary to gastric arteriovenous malformation | |
Case series and timelines
Thirty-seven patients were evaluated for TMVR in the outpatient office between 19 February 2020 and 2 December 2020. All patients evaluated were considered for SDD. Based on volume status, bleeding risk and frailty, risks and benefits of SDD were discussed and six patients consented to SDD. Patients generally underwent the procedure ∼1–2 months following initial evaluation. A detailed description of the individual characteristics of each patient is presented in Timeline. All patients considered tested negative for COVID-19 prior to the procedure, they were ambulatory and independent with adequate social support at home or from supervised facilities.
80-year-old male with severe symptomatic MR due to degenerative mitral valvular disease who underwent uncomplicated placement of one MitraClip XTR attached to the middle segment (A2) and the middle scallop (P2) of the mitral leaflet.
89-year-old male with severe symptomatic primary MR secondary to degenerative mitral valvular disease who underwent uncomplicated MitraClip XTR placement to the middle segment (A2) and posterior scallop (P3) of the mitral leaflet.
91-year-old male with history ischaemic cardiomyopathy and severe functional MR who underwent uncomplicated MitraClip XTR placement to the A2–P2 scallops.
83-year-old male with severe symptomatic MR with prolapsed posterior mitral leaflet consistent with primary MR, underwent uncomplicated MitraClip XTR placement to the A2–P2 scallops.
62-year-old male with a history of non-ischaemic cardiomyopathy and severe functional MR with symptoms despite maximal guideline-directed medical therapy, underwent MitraClip XTW placement to the A2–P2 scallops.
74-year-old male with symptomatic primary MR, underwent both coronary angioplasty with percutaneous intervention to mid-left anterior descending artery with 4 mm × 20 mm synergy drug-eluting stent and two MitraClip XTW placement to the A2–P2 scallops. The patient was readmitted a week later for anaemia secondary to gastrointestinal bleeding through a gastric arteriovenous malformation (AVM) that was photocoagulated.
In all patients, the procedure was performed under general anaesthesia and vascular access was obtained using a micropuncture technique through the right femoral vein that was closed with perclose sutures after completion of the procedure. Procedure time was estimated from administration of sedation to extubation and on average was 115 min. The patients were observed on telemetry in the post-anaesthesia care unit. Two hours following the procedure, the patients were ambulated multiple times and a post-procedural transthoracic echocardiogram (TTE) was then completed. All patients were noted to have MitraClip in the appropriate position, without any significant regurgitation and absence of pericardial effusion. All patients were discharged home within 3–4 h after the MitraClip procedure. No changes were made in medical therapy prior to discharge. A tele-visit was conducted the following day focused on three key questions, (i) access site pain or bleeding, (ii) follow-up of prior symptoms or any new symptoms, and (iii) general well-being. A virtual visit was performed at 2 weeks and 30 days with the structural heart disease team.
Discussion
Transcatheter mitral valve repair using MitraClip is an effective minimally invasive procedure for patients with symptomatic severe MR.7 With the cost of 30-day hospital readmissions reaching up to 41.3 billion US dollars, the focus is not only on early discharge but also for preventing readmissions in such patients.8 The 30-day readmission rates in patients undergoing TMVR vary from 11.7% to 15%.8–10 The leading cause of early readmissions (<30 days) includes heart failure, infections, cardiac arrhythmias, bleeding, and other post-procedural complications.11 Recently Case et al.10 reported that early discharge (<48 h) was actually associated with lower readmission rates (10.1% vs 13.5%). Operator experience and procedural success may also be contributing factors. Same-day discharge is increasingly being adopted in larger centres, as demonstrated by an observational study by Marmagkiolis et al.12 in which 89 patients who underwent uncomplicated MitraClip placement under moderate conscious sedation were discharged the same day without any major complications. The feasibility of SDD in tertiary centres and with general anaesthesia remains uncertain, especially given operator experience and procedural success are contributing factors to minimal complications.8 Tamburino et al. retrospectively determined factors associated with late discharge (defined as >72 h), including the presence of atrial fibrillation, elevated N-terminal pro-brain natriuretic peptide (BNP) levels, reduction in glomerular filtration rate, and a higher STS score. The late discharge cohort also had increased bleeding events compared to the early discharge cohort.13
Our series included patients with both primary and functional regurgitation, all of whom were underwent an elective TMVR with the MitraClip. All patients were discharged the same day after a post-procedural TTE noted no pericardial effusion, absence of prosthetic stenosis, and significant residual regurgitation. Of the patients discharged, one of the patients was readmitted within a week for symptomatic anaemia from a gastric AVM requiring transfusion support. The reason for major bleeding was likely due to triple anticoagulation therapy in the setting of stent placement and concomitant atrial fibrillation. This is consistent with the findings noted by Tamburino et al.,13 who attributed the prolonged length of stay in patients with atrial fibrillation to be due to anticoagulation management. Hence, patients with atrial fibrillation requiring anticoagulation and with a HAS-BLED score ≥3, may require extended stay for serial haemoglobin and haematocrit monitoring and should be excluded from this protocol. In patients with functional MR, one of the three patients had markedly elevated BNP and clinical findings indicative of decompensated congestive heart failure. Despite the favourable outcome in the patient included in our series, outcomes of MitraClip in patients with decompensated heart failure is not well established14 and further studies are necessary to investigate short outcomes prior to considering SDD in these patients. Hence, our protocol is primarily directed towards patients with functional MR and stable heart failure symptoms with a BNP <500 ng/L. While repair using MitraClip is directed towards frail high-risk surgical patients, frailty in itself has been linked to prolonged recovery and increased susceptibility to complications.15 All patients in our case series were independent with their activities of daily living as demonstrated by a score of 6/6 on the Katz index, a pragmatic measure that has shown to be a good predictor of early adverse outcomes in patients undergoing transaortic valve implantation16 and cardiac surgery.17
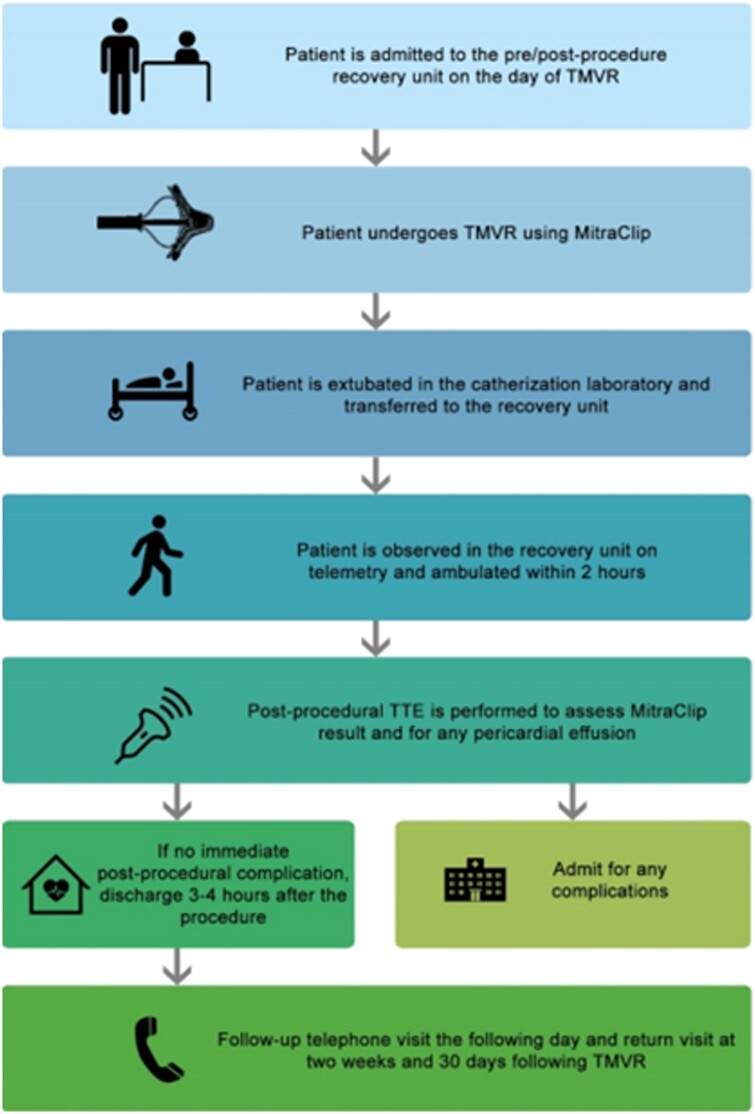
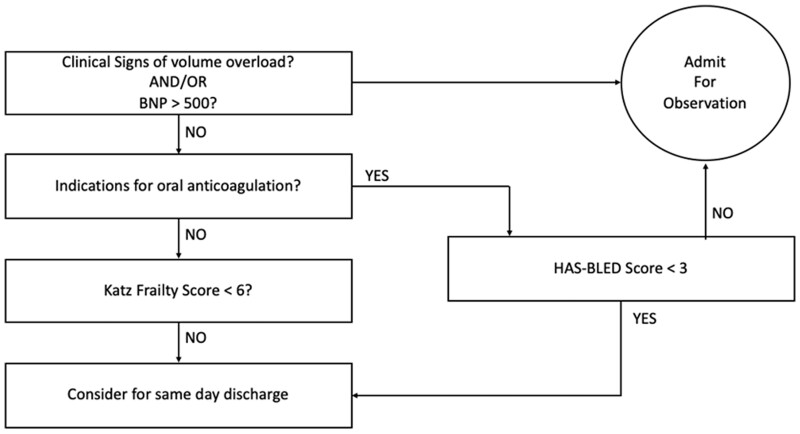
Figure 1 shows a proposed protocol for selection of patients with favourable characteristics for SDD. Based on the patients described in the case series, the protocol is applicable to electively admitted patients with primary or functional MR, without any clinical findings for decompensated congestive heart failure, with a KATZ score <6 and in patients on aspirin alone or on oral anticoagulants with a HAS-BLED score of <3 and with good social support. Figure 2 provides an overview of the temporal events on the day of the procedure to guide safe discharge. To qualify for safe discharge, patients are to undergo uncomplicated MitraClip placement without any local access site vascular complications and should not have any arrhythmias or pauses on telemetry or electrocardiogram post-procedure while at rest and ambulation. Post-procedural TTE is necessary to confirm MitraClip position, residual regurgitation or prosthetic stenosis, and absence of pericardial effusion.
Figure 1.
Proposed protocol for selection of patients with favourable characteristics for same-day discharge. TMVR, transcatheter mitral valve repair; TTE, transthoracic echocardiography
Figure 2.
Pre- and post-procedural protocol for same-day discharge following transcatheter mitral valve repair. BNP, brain natriuretic peptide.
Our case series highlights that SDD can be safely performed following MitraClip and has the potential to reduce exposure to COVID-19. This can potentially translate to better resource utilization and likely improved patient satisfaction as demonstrated in other percutaneous procedures with SDD protocol such as percutaneous coronary intervention18 and more recently valvular procedures such as transcatheter aortic valve replacement.19 Same-day discharge following MitraClip appears to be safe and maybe included among these procedures. However, further studies are needed prior to considering this as a standard of care.
Conclusion
Same-day discharge after TMVR is possible when done cautiously with close follow-up, it has the potential to improve resource utilization and improve patient satisfaction.
Lead author biography

Jeremiah P. Depta is the Director of the Advanced Valvular and Structural Heart Disease Program at Sands-Constellation Heart Institute at Rochester General Hospital in Rochester, New York. He serves as a proctor for TAVR instructing physicians across the USA and abroad. He completed his residency at Cleveland Clinic, General Cardiology Fellowship at Washington University in St Louis, and Interventional Cardiology/Structural Fellowship at Brigham and Women’s Hospital/Harvard Medical School. He serves as the principal site investigator for several multicentre randomized controlled trials with multiple publication in peer-reviewed journals.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including images and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: J.P.D. discloses the following relationships—Consultant/Advisory Board: Edwards Lifesciences, Boston Scientific, WL Gore & Associates. D.L.B. discloses the following relationships—Advisory Board: Cardax, Cereno Scientific, Elsevier Practice Update Cardiology, Level Ex, Medscape Cardiology, PhaseBio, PLx Pharma, Regado Biosciences; Board of Directors: Boston VA Research Institute, Society of Cardiovascular Patient Care, TobeSoft; Chair: American Heart Association Quality Oversight Committee; Data Monitoring Committees: Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Cleveland Clinic (including for the ExCEED trial, funded by Edwards), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo), Population Health Research Institute; Honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Vice-Chair, ACC Accreditation Committee), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor in Chief, Harvard Heart Letter), Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor in Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), Medtelligence/ReachMD (CME steering committees), Level Ex, MJH Life Sciences, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), Slack Publications (Chief Medical Editor, Cardiology Today’s Intervention), Society of Cardiovascular Patient Care (Secretary/Treasurer), WebMD (CME steering committees); Other: Clinical Cardiology (Deputy Editor), NCDR-ACTION Registry Steering Committee (Chair), VA CART Research and Publications Committee (Chair); Research Funding: Abbott, Afimmune, Amarin, Amgen, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers Squibb, Cardax, Chiesi, CSL Behring, Eisai, Ethicon, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Idorsia, Ironwood, Ischemix, Lexicon, Lilly, Medtronic, Pfizer, PhaseBio, PLx Pharma, Regeneron, Roche, Sanofi Aventis, Synaptic, The Medicines Company; Royalties: Elsevier (Editor, Cardiovascular Intervention: A Companion to Braunwald’s Heart Disease); Site Co-Investigator: Biotronik, Boston Scientific, CSI, St. Jude Medical (now Abbott), Svelte; Trustee: American College of Cardiology; Unfunded Research: FlowCo, Merck, Novo Nordisk, Takeda.
Funding: None declared.
Supplementary Material
References
- 1. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP. et al. ; On behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 2019;139:e56–e528. [DOI] [PubMed] [Google Scholar]
- 2. Elbadawi A, Elgendy IY, Elzeneini M, Mentias A, Elsherbeny AM, Abbott JD. et al. Temporal trends and outcomes of transcatheter mitral valve repair and surgical mitral valve intervention in patients with prior CABG. JACC Cardiovasc Interv 2019;12:2445–2447. [DOI] [PubMed] [Google Scholar]
- 3. Kheiri B, Zayed Y, Barbarawi M, Osman M, Chahine A, Ahmed S. et al. Interventions for secondary mitral regurgitation in patients with heart failure: a network meta-analysis of randomized controlled comparisons of surgery, medical therapy and transcatheter intervention. Cardiovasc Revasc Med 2020;21:155–163. [DOI] [PubMed] [Google Scholar]
- 4. Medical Association A. Factsheet: State Action Related to Delay and Resumption of “Elective” Procedures during COVID-19 Pandemic State Directives Ordering a Delay in Elective Procedures and Related Guidance from the Federal Government and the American College of Surgeons (ACS) Guidelines from the Centers for Medicare and Medicaid Services (CMS), the Centers for Disease Control and Prevention (CDC) and ACS. 2020. https://www.cdc.gov/coronavirus/2019-ncov/ (14 March 2021).
- 5. Shah PB, Welt FGP, Mahmud E, Phillips A, Kleiman NS, Young MN. et al. Triage considerations for patients referred for structural heart disease intervention during the COVID-19 pandemic: an ACC/SCAI position statement. JACC Cardiovasc Interv 2020;13:1484–1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang X, Bhatt DL.. COVID-19: an unintended force for medical revolution? J Invasive Cardiol 2020;32:E81–E82. [DOI] [PubMed] [Google Scholar]
- 7. Eggebrecht H, Schelle S, Puls M, Plicht B, Von Bardeleben RS, Butter C. et al. Risk and outcomes of complications during and after MitraClip implantation: experience in 828 patients from the German TRAnscatheter mitral valve interventions (TRAMI) registry. Catheter Cardiovasc Interv 2015;86:728–735. [DOI] [PubMed] [Google Scholar]
- 8. Tripathi B, Sawant AC, Sharma P, Tandon V, Patel T, Klein J. et al. Short term outcomes after transcatheter mitral valve repair. Int J Cardiol 2021;327:163–169. [DOI] [PubMed] [Google Scholar]
- 9. Lima FV, Kolte D, Rofeberg V, Molino J, Zhang Z, Elmariah S. et al. Thirty-day readmissions after transcatheter versus surgical mitral valve repair in high-risk patients with mitral regurgitation: analysis of the 2014–2015 Nationwide readmissions databases. Catheter Cardiovasc Interv 2020;96:664–674. [DOI] [PubMed] [Google Scholar]
- 10. Case BC, Yerasi C, Forrestal BJ, Wang Y, Musallam A, Hahm J. et al. MitraClip 30-day readmissions and impact of early discharge: an analysis from the nationwide readmissions database 2016. Cardiovasc Revasc Med 2020;21:954–958. [DOI] [PubMed] [Google Scholar]
- 11. Sorajja P, Vemulapalli S, Feldman T, Mack M, Holmes DR, Stebbins A. et al. Outcomes with transcatheter mitral valve repair in the United States: an STS/ACC TVT registry report. J Am Coll Cardiol 2017;70:2315–2327. [DOI] [PubMed] [Google Scholar]
- 12. Marmagkiolis K, Kilic ID, Ates I, Kose G, Iliescu CC.. Feasibility of same-day discharge approach after transcatheter mitral valve repair procedures. J Invasive Cardiol 2021;33:E123–E126. [DOI] [PubMed] [Google Scholar]
- 13. Tamburino C, Buccheri S, Popolo Rubbio A, Scandura S, Di Salvo ME, Mangiafico S. et al. Feasibility and predictors of early discharge after percutaneous edge-to-edge mitral valve repair. Heart 2017;103:931–936. [DOI] [PubMed] [Google Scholar]
- 14. Schau T, Isotani A, Neuss M, Schöpp M, Seifert M, Höpfner C. et al. Long-term survival after MitraClip® therapy in patients with severe mitral regurgitation and severe congestive heart failure: a comparison among survivals predicted by heart failure models. J Cardiol 2016;67:287–294. [DOI] [PubMed] [Google Scholar]
- 15. Iliadis C, Schwabe L, Müller D, Stock S, Baldus S, Pfister R.. Impact of frailty on periprocedural health care utilization in patients undergoing transcatheter edge-to-edge mitral valve repair. Clin Res Cardiol 2021;110:658–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Puls M, Sobisiak B, Bleckmann A, Jacobshagen C, Danner BC, Hünlich M. et al. Impact of frailty on short- and long-term morbidity and mortality after transcatheter aortic valve implantation: risk assessment by Katz Index of activities of daily living. EuroIntervention 2014;10:609–613. [DOI] [PubMed] [Google Scholar]
- 17. Lee DH, Buth KJ, Martin BJ, Yip AM, Hirsch GM.. Frail patients are at increased risk for mortality and prolonged institutional care after cardiac surgery. Circulation 2010;121:973–978. [DOI] [PubMed] [Google Scholar]
- 18. Shroff A, Kupfer J, Gilchrist IC, Caputo R, Speiser B, Bertrand OF. et al. Same-day discharge after percutaneous coronary intervention: Current perspectives and strategies for implementation. JAMA Cardiol 2016;1:216–223. [DOI] [PubMed] [Google Scholar]
- 19. Rai D, Tahir MW, Chowdhury M, Ali H, Buttar R, Abtahian F. et al. Transcatheter aortic valve replacement same-day discharge for selected patients: a case series. Eur Hear J Case Rep 2021;5. https://academic.oup.com/ehjcr/article/doi/10.1093/ehjcr/ytaa556/6089178 (22 February 2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.