Abstract
Background
The initial COVID-19 pandemic shutdown led to the canceling of elective surgeries throughout most of the USA and Canada.
Objective
This survey was carried out on behalf of the Parkinson Study Group (PSG) to understand the impact of the shutdown on deep brain stimulation (DBS) practices in North America.
Methods
A survey was distributed through RedCap® to the members of the PSG Functional Neurosurgical Working Group. Only one member from each site was asked to respond to the survey. Responses were collected from May 15 to June 6, 2020.
Results
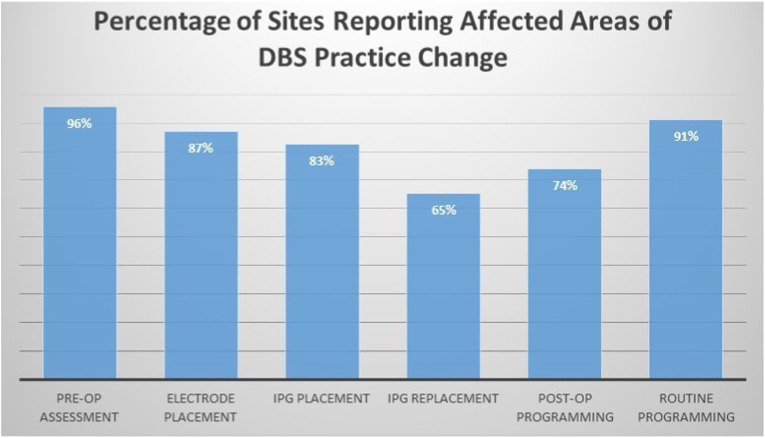
Twenty-three sites participated; 19 (83%) sites were from the USA and 4 (17%) from Canada. Twenty-one sites were academic medical centers. COVID-19 associated DBS restrictions were in place from 4 to 16 weeks. One-third of sites halted preoperative evaluations, while two-thirds of the sites offered limited preoperative evaluations. Institutional policy was the main contributor for the reported practice changes, with 87% of the sites additionally reporting patient-driven surgical delays secondary to pandemic concerns. Pre-post DBS associated management changes affected preoperative assessments 96%; electrode placement 87%; new implantable pulse generator (IPG) placement 83%; IPG replacement 65%; immediate postoperative DBS programming 74%; and routine DBS programming 91%.
Conclusion
The COVID-19 pandemic related shutdown resulted in DBS practice changes in almost all North American sites who responded to this large survey. Information learned could inform development of future contingency plans to reduce patient delays in care under similar circumstances.
Keywords: Deep brain stimulation, DBS, COVID-19, North America, Survey
1. Introduction
At the time of writing of this report, the United States has had over 37 million new cases and over 628,000 deaths due to COVID-19. In the USA, daily cases of COVID-19 initially peaked in April 2020, which was followed by six subsequent peaks. Canada was less affected than the USA, with more than 1.4 cases and more than 26,000 deaths [1]. Just when we thought the vaccines maybe winning the war against COVID, we are seeing the emergence of more virulent strains with rising cases especially in the unvaccinated population. Hospitals in some US cities are again putting elective surgeries on hold due to hospital resources getting overwhelmed.
During the first shutdown in May 2020, elective surgeries were canceled in most medical centers in the USA and Canada. DBS related delays were experienced in DBS patient candidacy screening, preoperative surgical preparations and DBS electrode implantation. Understanding how patient care was managed at centers treating patients with DBS during the pandemic shutdown will provide essential insights into contingency planning or long-term practice modifications that might be integral to sustain access to care for patients with advanced movement disorders. A previous multicenter report from Italy found that COVID-19 shutdown measures were associated with patient-perceived worsening of motor and psychiatric symptoms in PD patients with DBS [2], underscoring the importance of ensuring continued access to care in this population. Therefore, we surveyed DBS practices in North America on behalf of the PSG to understand how the pandemic-associated shutdown impacted DBS associated management. To our knowledge, this is the only large survey of clinicians on this subject in North America.
2. Methods
This study was approved by the ethics committee of Wake Forest School of Medicine IRB: IRB00065689. A REDCap® survey was distributed to all members of the Functional Neurosurgical Working Group of the PSG. Study data were collected and managed using REDCap [3] electronic data capture tools hosted at Wake Forest School of Medicine (UL1TR00142). One member from each site was instructed to complete the survey based on data from their site activity. Survey responses were collected from May 15 to June 6, 2020 after the first shutdown. Survey questions identified practice type and location, and addressed whether changes occurred in the following areas of DBS practice: pre-operative assessments, stage 1 electrode placements, stage 2 IPG placement, IPG replacements, post-operative and routine programming. Where relevant, respondents were asked to provide the best estimate of their affected volume in respective areas. For example, for reduction in presurgical evaluation volumes choices included usual numbers, 1–25% reduction from usual numbers, 26–50%, 51–75%, 76–99% and unable to evaluate. For questions assessing patient counts, choices included <5, 5–10, 11–15, >15. Otherwise categorical responses were required.
3. Results
Twenty-three PSG sites (21 academic, 2 private practice) participated. Nineteen (83%) sites were from the USA and 4 (17%) from Canada (Appendix A). All sites reported changes in their DBS practice (Fig. 1 ). COVID-19-associated restrictions impacted DBS care practices (preoperative, surgical, and postoperative management) for a median of 8 (range 4–16) weeks.
Fig. 1.
Percentage of sites reporting affected areas of DBS practice change.
3.1. Impact on preoperative assessment
All institutions reported cancellation or postponement of preoperative assessments driven by institutional policy mandates. 87% of sites reported that patients also elected to cancel or postpone DBS electrode implants due to concern for COVID-19 exposure. A third of sites discontinued preoperative evaluations, while the remaining experienced reduction in the number of preoperative evaluations. Both neurologists and neurosurgeons were able to continue patient preoperative evaluations at 2/3rd of sites, albeit with markedly reduced numbers. Neuropsychology evaluations continued at only 1/3rd of sites. 92% of sites reported that preoperative levodopa motor ON/OFF evaluations were postponed, although some concurrently conducted it in-person (22%) or via video-based (13%) assessments. No site made a surgical decision to proceed with DBS for PD patients without an in-person levodopa motor ON/OFF evaluation.
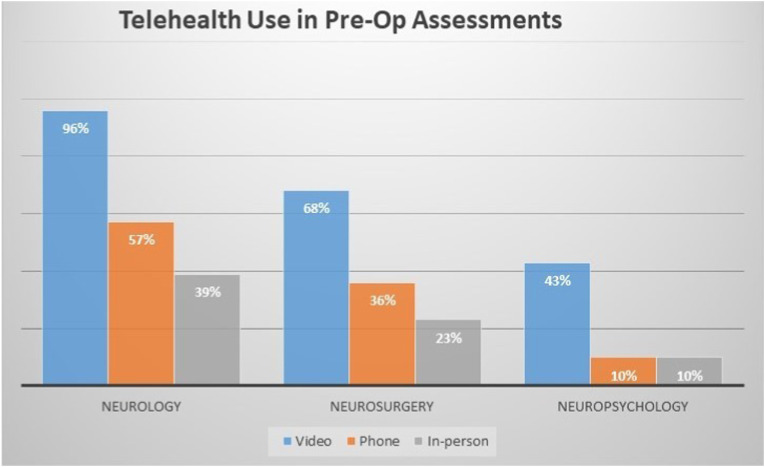
3.2. Telehealth in preoperative assessment
Preoperative neurological, neurosurgical, and neuropsychological evaluations were conducted using a combination of in-person, phone, and video visits. All except one site reported the use of telehealth in such pre-surgical evaluations. The proportion using video visits was highest, followed by phone visits and in-person visits. Telehealth use was highest in neurology, followed by neurosurgery. However, the use of telehealth by neuropsychology was markedly lower (Fig. 2 ).
Fig. 2.
Telehealth use in pre-op assessments.
3.3. Impact on surgical practice
All sites reported postponement of electrode placement (Stage 1) surgery. The majority of sites (55%) estimated the number of Stage 1 surgeries postponed to be between 5 and 10 (range less than 5 to more than 15), with four sites (18%) having postponed 11 or more stage 1 procedures. Stage 2 implantable pulse generator (IPG) implantation in any patient was postponed at 83% of the sites and otherwise continued as scheduled at the remaining sites. Amongst sites reporting IPG related postponements, 36% estimated postponing less than five cases, 47% postponed an estimated 5–10 cases, and the remainder postponed greater than ten. Two sites reported the use of local instead of general anesthesia for initial IPG implantation to minimize aerosol emission. IPG replacement surgeries were reported to be postponed by 70% of the sites, with 44% of sites estimating less than five postponements and 50% estimating 5–10. Device removal due to infection and hardware malfunction was postponed at one site and two sites respectively. The decision to replace an IPG was made on a case-by-case basis by 62% and as per uniform hospital policy by 38% of the sites. The majority of sites (86%) did not consider disease type in the decision making process to replace IPGs, while the remaining did.
3.4. Impact on postoperative care
Postop DBS programming for newly implanted patients was managed in a variety of ways. 38% of sites reported a complete halt in programming sessions for this group of patients, while 24% reported that they could continue as usual (i.e., in-person). 14% of sites offered programming for the first visit for newly implanted patients. 38% of the sites offered programming on a case by case basis. 42% of sites deferred postoperative imaging for documentation of lead location. Routine in-person programming sessions (defined as more than 6 months post-implantation) were performed at half of the sites, but most often when patients were determined to need urgent evaluation or programming (73%) and less commonly upon patient request for an in-person session (27%).
3.5. Telehealth Use in DBS programming
Telehealth was used for remote assessment of routine programming by 68% of the sites. 70% of sites used telehealth only, or estimated using a predominance of telehealth visits, while 25% reported that more in-person visits than telehealth were utilized for these visits. To accomplish DBS adjustment remotely, 78% of sites reported using previously programmed patient control parameters to guide patient self-adjustment of DBS settings. 65% of sites reported that they enabled patient control parameters to adjust DBS settings during the shutdown remotely, and the majority utilized this strategy once enabled. 70% of survey respondents rated remote programming capabilities as an essential device capability to utilize in the future, while 26% said it was ‘somewhat important.’
4. Discussion
This large North American survey of 23 sites regarding DBS practices during the initial shutdown from the COVID-19 pandemic confirms significant effects on all aspects of DBS care, including preoperative, surgical, and postoperative management. Care delivery by all associated specialties (neurologists, neurosurgeons, and neuropsychologists) were impacted during the shutdown with reliance on telemedicine. Although DBS is considered an elective procedure, unanticipated changes in the practice or care delivery landscape, or interruption in access to DBS-related care can prolong or impose substantial disability. During the initial COVID-19 pandemic shutdown, the challenge was balancing this risk of disability with the risk of exposure to the virus during the act of seeking care (for patients as well as healthcare workers). Access to clinicians was quite often subject to the public health and geographically heterogeneous institutional policies implemented across the country. As a consequence of these dynamics, several key findings from this survey warrant further discussion and exploration.
While preoperative assessments were nearly uniformly canceled or postponed at sites participating in this survey, an unexpected finding was that neuropsychological assessment was disproportionately disrupted compared to neurology and neurosurgery assessments. While models of remote DBS assessments exist [4], DBS teams considering a telehealth contingency plan for remote preoperative assessments should be aware of unique telehealth challenges to neuropsychology practices [5].
Recommendations regarding DBS candidacy are dependent on the assessment of preoperative medication response, which in PD patients requires the measurement of symptoms both ON and OFF dopaminergic medications. The importance of this assessment is evidenced by the fact that none of the sites participating in this survey reported making a surgical decision in a PD patient without it. Although many sites implemented remote preoperative neurology evaluations conducted via video visits [6], its validity in the preoperative assessment of DBS candidates warrants further investigation.
All sites postponed stage 1 electrode placement surgery in keeping with the prevailing view that DBS placement is an elective procedure. While some may challenge this view, especially when considering the substantial impairment in quality of life experienced by patients proceeding with DBS treatment, the decision to complete stage 2 in cases where pre-pandemic electrode placement had been performed posed a different kind of dilemma in terms of how long to delay the procedure.
The proportion of sites postponing IPG replacement was unexpectedly high at 70%. The potential risks of abrupt cessation of DBS therapy have been described [7], ranging from symptom recurrence that can be successfully managed with medication titration to life-threatening disease exacerbations. The postponement of revision related to hardware malfunction and removal related to infection is also noteworthy in this context. Although the exact nature and severity of these latter cases were not explicitly explored in the survey, we believe that such IPG surgeries should be considered an urgent, non-elective procedure due to the potential risks involved [8].
Telehealth methods were used by the majority of sites to conduct routine post-DBS assessment and management. Since the majority of DBS devices cannot be comprehensively interrogated or adjusted remotely, sites developed workarounds to maintain care delivery, including enabling patient control parameters that clinicians can instruct patients or caregivers to adjust by telehealth. Limitations include lack of information about hardware status, difficulties assessing stimulation-induced side effects, and challenges that patients may have interacting with their therapy controller [9]. While preliminary evidence regarding a remote programming platform exists [10,11], and a recent clinical trial has investigated the feasibility and safety of remote programming (ACTRN12619001660178) [12], this technology is device specific. An overwhelming number of respondents indicated that remote programming capabilities are considered essential.
Our study had its limitations. The PSG network includes mostly academic centers, leading to a selection bias in responses received. This survey assessed the impact of the pandemic-related shutdown on DBS management without investigating the implementation of various strategies or the impact(s) of these strategies on patient outcomes. Though this survey was taken immediately after the first shutdown there maybe less accuracy in reporting numbers.
In conclusion, the COVID-19 pandemic related shutdown resulted in significant changes in all aspects of DBS care at all sites in North America who responded to this survey. Sites should have a viable contingency plan for DBS care if a similar shutdown were to happen again. Many outpatient DBS-related assessments could be conducted via telemedicine. Further work is needed to determine persistence of remote DBS assessments beyond the pandemic. Telehealth examinations will need to be validated against standardized in-person exams, especially for neuropsychological testing. Regulatory and reimbursement policy changes are needed to permit continued remote assessments. Technology companies should work with regulatory agencies to hasten the development of remote programming of DBS devices in a way that is safe, HIPAA-compliant, and reimbursable.
Ethical compliance statement
This study was approved by ethics committee of Wake Forest University School of Medicine IRB00065689. No informed consent was needed. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Author roles
Mustafa S. Siddiqui:
1) Research project: Conception, Organization, Execution;
2) Statistical Analysis: Design, Execution.
3) Manuscript: Writing of the first draft.
Joohi Jimenez-Shahed:
1) Research project: Conception, Organization, Execution;
2) Statistical Analysis: Design, Review and Critique;
3) Manuscript: Review and Critique.
Sol De Jesus, Harini Sarva, Michele York, Jim McInerney, Fedor Panov, Jason Schwalb, Zoltan Mari, Benjamin Walter, Joshua Rosenow, Neepa Patel, Lin Zhang, John Bertoni: Manuscript: Review and Critique.
Funding sources and conflict of interest
No specific funding was received for this work and the authors declare that there are no conflicts of interest relevant to this work.
Financial disclosures for the previous 12 months
In the past year from the date of submission, the following contributors have received support unrelated to this research (e.g., grants, advisory boards, employment, consultancies, contracts, honoraria, royalties, expert testimony, partnerships, or stock ownership in medically-related fields):
Mustafa S. Siddiqui: Advisory Board: Neuropoint Alliance (RAD-PD Steering Committee), Boston Scientific Neuromodulation, Abbvie Inc. Research Grants received by my institution: Sunovion Pharma, grants from Biogen MA Inc., Theravance Biopharma, Neuropoint Alliance/Michael J Fox Foundation, Impax Lab, Sun Pharma, Boston Scientific Neuromodulation, Neuraly
Joohi Jimenez-Shahed: Advisory Board Abbott.
Zoltan Mari: Grants: NIH. Consulting/Honoraria/Advisory board: Global Kinetics Corporation, GB Sciences, Inc, CNS Ratings, LLC, AbbVie, Inc, Amneal, Kyowa Kirin, Sanofi Genzyme.
Joshua Rosenow: Honoraria, research grants, advisory board: Boston Scientific Neuromodulation.
Benjamin Walter: Consulting/Honoraria: Medtronic, Abbott, Teva.
Sol De Jesus: Consulting: Medtronic.
Fedor Panov: Consulting: Zimmer Biomet.
Jason Schwalb: Name: NeuroPoint Alliance, (Steering Committee for RAD-PD), Blue Cross Blue Shield of Michigan (Salary support paid to my employer). Medtronic, Neuros, SetPoint Medical, (Research funding paid to my employer).
Michele York: Michael J Fox Foundation- RAD-PD, Type of support: RAD-PD DBS Registry Steering Committee, PPMI Neuropsychological Training.
Harini Sarva: CALAHealth, Acorda: Type of support: advisory board, Novo Nordisk, Type of Support: (Protocol review), Insightec (Research Support).
Following authors do not have any disclosures to report: Jim McInerney, Neepa Patel, Lin Zhang, John Bertoni.
Appendix A. List of Cities of Participating Sites
| City | State/Province | Country | Type of DBS Practice |
|---|---|---|---|
| Winston-Salem | NC | USA | Academic |
| Houston | TX | USA | Academic |
| West Bloomfield | MI | USA | Private practice |
| Boston | MA | USA | Academic |
| Aurora | CO | USA | Academic |
| Ottawa | ON | Canada | Academic |
| Omaha | NE | USA | Academic |
| Montreal | QC | Canada | Academic |
| Rochester | NY | USA | Academic |
| NYC | NY | USA | Academic |
| Buffalo | NY | USA | Academic |
| Nashville | TN | USA | Academic |
| Toronto | ON | Canada | Academic |
| Boston | MA | USA | Private practice |
| Detroit | MI | USA | Academic |
| Toronto | ON | Canada | Academic |
| Chicago | IL | USA | Academic |
| Las Vegas | NV | USA | Academic |
| Hershey | PA | USA | Academic |
| Baltimore | MD | USA | Academic |
| Indianapolis | IN | USA | Academic |
| New York | NY | USA | Academic |
| Milwaukee | WI | USA | Academic |
References
- 1.Center JHCVR 2021;.Pageshttps://coronavirus.jhu.edu/map.html.
- 2.Piano C., Bove F., Tufo T., Imbimbo I., Genovese D., Stefani A., et al. Effects of COVID-19 lockdown on movement disorders patients with deep brain stimulation: a multicenter survey. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.616550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Harris P.A., Taylor R., Minor B.L., Elliott V., Fernandez M., O'Neal L., et al. The REDCap consortium: building an international community of software platform partners. J. Biomed. Inf. 2019;95 doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jitkritsadakul O., Rajalingam R., Toenjes C., Munhoz R.P., Fasano A. Tele-health for patients with deep brain stimulation: the experience of the Ontario Telemedicine Network. Mov. Disord. 2018;33(3):491–492. doi: 10.1002/mds.27230. [DOI] [PubMed] [Google Scholar]
- 5.York M.K., Farace E., Pollak L., Floden D., Lin G., Wyman-Chick K., et al. Parkinsonism & Related Disorders; 2021. The Global Pandemic Has Permanently Changed the State of Practice for Pre-DBS Neuropsychological Evaluations. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hassan A., Mari Z., Gatto E.M., Cardozo A., Youn J., Okubadejo N., et al. Global survey on telemedicine utilization for movement disorders during the COVID-19 pandemic. Mov. Disord. 2020;35(10):1701–1711. doi: 10.1002/mds.28284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Miocinovic S., Ostrem J.L., Okun M.S., Bullinger K.L., Riva-Posse P., Gross R.E., et al. Recommendations for deep brain stimulation device management during a pandemic. J. Parkinsons Dis. 2020;10:903–910. doi: 10.3233/JPD-202072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gross R.E., Buetefisch C.M., Miocinovic S., Bullinger K.L., Okun M.S., Ostrem J.L., et al. Letter: evaluation and surgical treatment of functional neurosurgery patients with implanted deep brain stimulation and vagus nerve stimulation pulse generators during the COVID-19 pandemic. Neurosurgery. 2020;87(2):E222–E226. doi: 10.1093/neuros/nyaa185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kostick K., Storch E.A., Zuk P., Blumenthal-Barby J.S., Torgerson L., Yoshor D., et al. Strategies to mitigate impacts of the COVID-19 pandemic on patients treated with deep brain stimulation. Brain Stimul. 2020;13(6):1642–1643. doi: 10.1016/j.brs.2020.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu J., Wang J., Keith S., Zhang M., Yang C., Yuan Q., et al. Management of Parkinson’s disease patients after DBS by remote programming: preliminary application of single center during quarantine of 2019-nCoV. J. Neurol. 2020;268(4):1295–1303. doi: 10.1007/s00415-020-10273-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang C., Zhang Y., Zhan S., Li D., Jin H., Denys D., et al. Telemedical deep brain stimulation: merits and limitations. Stereotact. Funct. Neurosurg. 2018;96(4):272–273. doi: 10.1159/000491603. [DOI] [PubMed] [Google Scholar]
- 12.Registry ANZCT;Pageshttps://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=378612.