Abstract
Objective
To evaluate differences in access to behavioral health services for Medicaid enrollees covered by a Medicaid entity that integrated the financing of behavioral and physical health care (“carve‐in group”) versus a Medicaid entity that separated this financing (“carve‐out group”).
Data Sources/Study Setting
Medicaid claims data from two Medicaid entities in the Portland, Oregon tri‐county area in 2016.
Study Design
In this cross‐sectional study, we compared differences across enrollees in the carve‐in versus carve‐out group, using a machine learning approach to incorporate a large set of covariates and minimize potential selection bias. Our primary outcomes included behavioral health visits for a variety of different provider types. Secondary outcomes included inpatient, emergency department, and primary care visits.
Data Collection
We used Medicaid claims, including adults with at least 9 months of enrollment.
Principal Findings
The study population included 45,786 adults with mental health conditions. Relative to the carve‐out group, individuals in the carve‐in group were more likely to access outpatient behavioral health (2.39 percentage points, p < 0.0001, with a baseline rate of approximately 73%). The carve‐in group was also more likely to access primary care physicians, psychologists, and social workers and less likely to access psychiatrists and behavioral health specialists. Access to outpatient behavioral health visits was more likely in the carve‐in arrangement among individuals with mild or moderate mental health conditions (compared to individuals with severe mental illness) and among black enrollees (compared to white enrollees).
Conclusions
Financial integration of physical and behavioral health in Medicaid managed care was associated with greater access to behavioral health services, particularly for individuals with mild or moderate mental health conditions and for black enrollees. Recent changes to incentivize financial integration should be monitored to assess differential impacts by illness severity, race and ethnicity, provider types, and other factors.
Keywords: managed care, Medicaid, mental health
What is known on this Topic
Many state Medicaid programs and managed care entities are moving away from systems that “carve‐out” behavioral health (with a separate entity holding financial risk and managing behavioral health services) to an integrated “carve‐in” model (with a single entity responsible for managing physical and behavioral health).
Relatively little is known about the potential implications of these models on access to behavioral health services and whether they vary by the severity of mental illness or by race and ethnicity.
What this study Adds
This study finds that “carving in” behavioral health services is associated with increased access to behavioral health services, particularly among individuals with mild to moderate mental health conditions.
Carve‐ins are also associated with increased access to outpatient behavioral health visits for black enrollees relative to white enrollees.
Carve‐ins and carve‐outs may also affect the types of providers that Medicaid enrollees use for care, with carve‐ins associated with a higher likelihood of accessing primary care physicians for behavioral health needs and a lower likelihood of accessing psychiatrists.
1. INTRODUCTION
Medicaid is a significant source of financing for mental health services in the United States, accounting for 25% of all mental health spending in 2014. 1 In states with Medicaid managed care organizations (MCOs), mental health care has frequently been “carved out” to a separate managed behavioral health organization (BHO). In these scenarios, physical health is managed and reimbursed by the primary MCO, and mental health services are managed and reimbursed by a BHO. Carve‐out arrangements reflected financial and political concerns about the extent to which MCOs might inhibit access to behavioral health care. Advocates for carve‐outs expressed concerns that plans focused on physical health management would not understand the nuances of mental health conditions and would have difficulties establishing specialty provider networks. Advocates also voiced concerns that a blending of funds might favor physical health services at the expense of needed mental health services.
Despite these rationales, legacy carve‐out arrangements are now perceived as a critical barrier to better outcomes for Medicaid enrollees, 2 , 3 , 4 , 5 , 6 , 7 particularly given evidence supporting the integration of primary care and behavioral health care in clinical settings. 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 The goals of integrated care may be incompatible with separate financing of medical and physical health services. Carve‐outs create separate payers and separate networks, restricting reimbursement for services that include both physical and mental health, creating impediments to communications across systems, and introducing other barriers to care, including requirements for additional or separate credentialing and empaneling of providers. Clinical integration may be inhibited if, for example, mental health providers co‐located with primary care providers are not included in the physical health MCO's network. In these instances, even if the clinic can deliver integrated care, patients with mental health conditions may still be referred to outside mental health providers, reducing the likelihood of timely and coordinated treatment.
Two federal rules, issued in 2016, incentivized states to move away from carve‐out arrangements. The first was the Center for Medicare and Medicaid Services 2016 Medicaid managed care regulations, which included language‐supporting integrated care and encouraging comprehensive patient assessments. The second was a rule change for Medicaid managed care, which defined compliance responsibilities for the Mental Health Parity and Addiction Equity Act of 2008. This rule change created an extra administrative and financial burden for states that retained behavioral health carve‐outs, providing an incentive to move toward financially integrated models. 17 Over time, carve‐out models have become less common. In 2019, 39 states and the District of Columbia contracted with MCOs; 18 among those states, only six carved out all of their behavioral health services (CA, CO, MD, MI, PA, and UT). Twenty‐two states carved in all of their behavioral health services, and 10 used some mixture of approaches (e.g., carving out specialty services only). However, these numbers may overstate the extent to which full integration has occurred. In many states that carve‐in behavioral health, Medicaid managed care plans accept full physical and behavioral health financing while subcontracting with BHOs. In this “health plan carve‐out,” 19 the MCO subdelegates the management and risk of behavioral health care to the BHO.
This study assesses differences in outcomes for two MCO‐like organizations serving the Portland, Oregon market in 2016. Since 2012, Medicaid beneficiaries in Oregon have been enrolled in Coordinated Care Organizations (CCOs). 20 , 21 , 22 CCOs are similar to MCOs in how they accept financial risk and pay for care. However, unlike traditional MCOs, CCOs are accountable to performance metrics and have governing boards that include stakeholders in the local health systems.
CCOs operate within global budgets and receive funding for all acute care services, including physical and behavioral health care. CCOs can manage and pay for all of these services in an integrated fashion. Conversely, they may choose to focus on general medical care and subdelegate the risk and management of behavioral health care to a separate entity. This study compares outcomes between two CCOs with similar provider networks and patient populations but differing approaches to behavioral health care, with one CCO integrating financing and another using separate physical and behavioral health risk‐accepting entities.
The objective of this study is to assess the association between carve‐in versus carve‐out arrangements and access to physical and behavioral health services among adult Medicaid beneficiaries with mental health conditions. Our study updates a large literature on carve‐outs, including an extensive 2007 review by Frank and Garfield. 19 Generally, carve‐outs have been associated with reductions in overall costs and inpatient utilization and increases in access, with mixed effects on quality. However, there have been relatively few studies of carve‐outs in Medicaid since the advent of the Affordable Care Act and an increased focus on integration at the clinical level.
Because carve‐out arrangements may affect patients differently, we also assess differences among individuals with serious mental illness (SMI) versus those with mild to moderate mental health conditions. Our assessment of differential impacts for those with and without SMI is based on the hypothesis that financial integration will improve opportunities to incorporate mental health services in the primary care setting, with the main beneficiaries being individuals with mild and moderate mental health conditions. In contrast, individuals with SMI are more likely to receive their health services through community mental health centers, which may have longstanding relationships with behavioral health carve‐outs. Although some states have opted to develop carve‐in models that focus on the SMI population only, relatively little is known about the differential impacts of carve‐ins versus carve‐outs by severity of mental illness.
We also test for differential impacts among black, Hispanic, and white enrollees because of the documented impact of racism on health 23 , 24 and because a large number of studies have revealed significant disparities in access, quality, and outcomes for black and Hispanic individuals with mental illnesses relative to their white counterparts. 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 Some studies suggest that behavioral health integration may improve care for black and Hispanic patients. 33 , 34 , 35 , 36 , 37 , 38 By assessing the potential for reduced disparities through financial integration, we aim to add to the existing literature. Furthermore, the state of Oregon identified “Health Equity and Eliminating Health Disparities” as a key goal for its Medicaid program. 39 Although the state enacted a variety of initiatives to reduce disparities, the extent to which carve‐in versus carve‐out approaches may affect disparities is unknown.
2. METHODS
2.1. Study design
In this observational, cross‐sectional study, we compared two Portland‐area CCOs with overlapping service areas, covering similar populations with geographic access to the same set of providers. Although Medicaid beneficiaries were not randomized to CCOs, the Oregon Health Authority attempted to balance population demographics when assigning members to CCOs. The state reported that it was unusual for members to exercise their right to switch between CCOs. 40 Therefore, we expect minimal selection effects, although we cannot rule them out entirely. To minimize concerns of confounding and selection, we deployed the machine‐learning approach described below.
Although they covered similar populations, the study CCOs differed in their financing of behavioral health services. The first CCO (the “carve‐in group”) paid for and managed physical and behavioral health services as a single entity. The second CCO (denoted the “carve‐out group”) separated these finances, subcontracting with a separate entity to take on the financing and management of behavioral health services.
2.2. Study population
Our study population included adults who were enrolled in Oregon Medicaid between January 1 and December 31, 2016, and received at least 9 months of coverage during that time. We restricted our focus to individuals with a mental health condition (defined below) in 2016. We focused on 2016 because this represented the most recent year of available data and allowed for sufficient program maturity following the 2012 transition to CCOs. We excluded observations where the member was dually eligible for Medicare and Medicaid, had less than 3 months of enrollment in the prior year, did not reside in the tri‐county service area shared by the study CCOs, or did not have a mental health condition. We also excluded members who switched plans (see Appendix, Figure A1 for additional details). Claims and enrollment data were obtained from the Oregon Health Authority.
We identified patients with SMI by searching the claims data for any inpatient or psychiatric residential claim, or at least two outpatient claims on separate dates, with a primary diagnosis of schizophrenia (F20 and F25), bipolar I (F30 and F31.0–F31.78), severe episodes of major depressive disorder (F32.2, F32.3, F33.2, and F33.3), or other schizophrenia spectrum or psychotic disorder (F28). We classified patients as having mild or moderate mental health conditions if they had a mental illness diagnosis that did not meet the criteria for SMI. Other mental illness diagnoses were identified through the Clinical Classifications Software Refined (CCSR) 41 categories, which aggregates over 70,000 ICD‐10‐CM diagnosis codes into approximately 500 clinically meaningful categories. We categorized MBD001–MBD011 and MBD013 as mental health diagnoses (see Appendix, Table A1 for details).
2.3. Variables
Our covariates included enrollee age, gender, self‐reported race‐ethnicity, county of residence, months enrolled during the study year, and primary spoken language. To control for differences in clinical risk, we included 536 CCSR indicators, based on diagnoses observed during the study year. We used this expansive list of diagnoses to more accurately capture differences in risk that might be lost in an aggregate risk score. 42
Our outcome variables included visits for selected service types, including inpatient, emergency department (ED), and outpatient care. We classified visits as behavioral health related if they had a primary diagnosis related to mental health, substance use, suicide, or intentional self‐injury, as defined by the CCSR (see Appendix, Table A2a). Primary care visits, based on a definition proposed by Chang and colleagues, 43 were modified to include telehealth consultations (CPT codes 99441‐3). Our outpatient behavioral health visit definition required patient‐facing care and included psychotherapy, counseling, evaluation and management, skills training, peer services, and assertive community treatment. It excluded laboratory tests, imaging, and medication administration (see Appendix, Table A2b).
Within the overall category of “outpatient behavioral health visits,” we created seven mutually exclusive subcategories defined by the type of provider who delivered the service: primary care; psychiatrist; psychologist; advanced practice nursing provider specializing in mental health; behavioral health specialist (including other counselors and therapists); social workers; and all other providers. Provider specialties were defined using National Plan and Provider Enumeration System taxonomies (see Appendix, Table A2c). To improve specificity, our definition of psychiatrist visits was restricted to evaluation and management codes only because other providers often bill for services under a supervising psychiatrist (see Appendix, Table A2b).
For each of these visit types, we provided descriptive summaries and statistical analyses of access (any visit) as well as the number of visits, conditional on accessing care.
2.4. Statistical analysis
To estimate the impact of carve‐in versus carve‐out financing on our outcomes of interest, we used causal forests, 44 a form of nonparametric statistical estimation based on random forests, 45 a popular machine‐learning approach. Causal forests estimate the effect or association of a variable D on an outcome Y, controlling for a vector of confounders, X, producing outputs (an estimate and SE) similar to a standard parametric linear or logistic regression. The advantages of the causal forest approach are twofold. First, the causal forest includes routines for sample‐splitting, allowing for the inclusion of a large set of covariates while minimizing concerns of overfitting. Second, causal forests are nonparametric and do not make restrictive assumptions about the functional form. In Monte Carlo studies, causal forests have been shown to reduce bias by substantial amounts (50% or more) relative to traditional parametric models. 46 Machine‐learning‐based estimators are particularly useful in automating the choice of the most important covariates and in reducing bias that might arise from an incorrectly specified parametric model. They are useful under the assumption of exogeneity 47 but do not create new ways to identify causal effects if endogeneity is present. In sensitivity analyses, we compared a subset of estimates from the causal forest approach to a linear probability model. These analyses were conducted to assess the extent to which causal forest estimates differ from more traditional modeling approaches. To investigate the possibility of heterogeneous treatment effects, we conducted analyses of subgroups based on race and ethnicity (white, black, and Hispanic) and severity of mental illness (SMI vs. mild and moderate mental illness). We fit our causal forest models with default settings and tested model fit with an omnibus test for the quality of the random forest estimates. We report the estimated treatment effects and 95% confidence intervals (CIs), with p‐values based on two‐sided tests of statistical significance, defined as p < 0.05. Analyses were conducted using R version 3.6.2 (R Project for Statistical Computing). Additional details and R code are provided in the Appendix.
3. RESULTS
Table 1 displays characteristics of the 15,601 adults with mental health conditions in the carve‐in group and the 30,185 adults with mental health conditions in the carve‐out group, along with standardized differences between the groups (a standardized difference of greater than 0.1 is conventionally considered to indicate meaningful differences between covariates in two groups 48 ). The two populations were reasonably well balanced, although the carve‐in group had more individuals in the 27‐49 age range, a lower percentage of black and Hispanic enrollees, and fewer individuals with schizophrenia and other psychotic disorders.
TABLE 1.
Comparison of study population characteristics in Medicaid carve‐in versus carve‐out group, 2016
| Carve‐in group (N = 15,601) | Carve‐out group (N = 30,185) | Standardized difference | |
|---|---|---|---|
| Age (years) | 0.13 | ||
| 18–26 | 18.2% | 17.4% | |
| 27–49 | 59.9% | 55.1% | |
| 50–64 | 21.9% | 27.4% | |
| Female gender | 64.4% | 64.3% | 0.002 |
| Race‐ethnicity | 0.14 | ||
| White | 62.4% | 61.5% | |
| Hispanic | 5.5% | 6.1% | |
| Black | 4.5% | 6.7% | |
| Asian/Hawaiian/Pacific Islander | 2.5% | 3.3% | |
| American Indian/Alaska Native | 2.9% | 3.3% | |
| Other | 2.8% | 2.0% | |
| Unknown | 19.4% | 17.1% | |
| Primary spoken language | 0.03 | ||
| English | 89.6% | 90.2% | |
| Spanish | 1.8% | 1.9% | |
| Other/undetermined | 8.6% | 7.9% | |
| County of residence | 0.07 | ||
| Multnomah | 57.0% | 57.9% | |
| Washington | 21.7% | 23.3% | |
| Clackamas | 21.4% | 18.8% | |
| Mental illness severity | 0.10 | ||
| Serious mental illness | 9.2% | 12.3% | |
| Mild to moderate mental illness | 90.8% | 87.7% | |
| Mental health conditions | |||
| Anxiety and fear‐related disorders | 56.5% | 52.8% | 0.07 |
| Depressive disorders | 53.5% | 52.7% | 0.02 |
| Trauma‐ and stress‐related disorders | 31.9% | 30.4% | 0.03 |
| Bipolar and related disorders | 9.6% | 10.6% | 0.03 |
| Schizophrenia spectrum and other psychotic disorders | 6.6% | 9.8% | 0.12 |
| Miscellaneous mental and behavioral disorders/conditions | 6.9% | 6.6% | 0.01 |
| Personality disorders | 2.5% | 2.7% | 0.01 |
| Other specified and unspecified mood disorders | 2.4% | 2.6% | 0.01 |
| Obsessive–compulsive and related disorders | 1.7% | 1.8% | 0.01 |
| Feeding and eating disorders | 1.5% | 1.1% | 0.03 |
| Somatic disorders | 1.3% | 1.6% | 0.03 |
| Disruptive, impulse‐control, and conduct disorders | 0.8% | 1.0% | 0.02 |
Note: Population restricted to individuals with mental health condition. Standardized difference greater than 0.1 generally indicates meaningful differences between groups. Mental health conditions are defined by the Clinical Classification System, Refined (CCSR).
Table 2 displays (1) unadjusted probabilities of accessing any care and (2) the average number of visits, conditional on accessing care, for physical health and behavioral health services. Slightly more than 70% of individuals with mental health conditions had at least one outpatient visit for behavioral health care. The most frequently accessed providers were primary care providers (36.6% and 34.8% in the carve‐in and carve‐out groups, respectively) and behavioral health specialists (counselors and therapists). The probability of any visit to a psychiatrist or psychologist was relatively low, ranging from 3.5%.to 10.1%. Conditional on accessing behavioral health care, enrollees averaged 15 visits. Approximately, 80% of enrollees accessed primary care for physical health conditions at least once during the year.
TABLE 2.
Unadjusted measures of service use for Medicaid carve‐in and carve‐out groups, 2016
| Access rate | Total visits (conditional on at least one visit) | |||
|---|---|---|---|---|
| Carve‐in group (%) | Carve‐out group (%) | Carve‐in group mean (SD) | Carve‐out group mean (SD) | |
| Outpatient behavioral health visits | ||||
| All | 74.4% | 71.6% | 15.15 (23.71) | 15.11 (26.43) |
| With a primary care provider a | 36.6% | 34.8% | 4.25 (12.54) | 2.82 (6.10) |
| With a psychiatrist b | 6.7% | 10.1% | 3.33 (3.02) | 3.78 (3.05) |
| With a psychologist | 6.5% | 3.5% | 6.89 (9.76) | 6.59 (8.92) |
| With an advanced practice nursing provider c | 12.6% | 12.7% | 3.36 (2.92) | 3.66 (3.11) |
| With a behavioral health specialist d | 37.6% | 39.4% | 12.93 (17.08) | 13.08 (18.71) |
| With a social worker | 16.7% | 16.0% | 7.72 (10.94) | 6.56 (10.27) |
| With another provider type e | 25.0% | 27.5% | 9.91 (19.00) | 9.29 (18.21) |
| Other behavioral health visits | ||||
| Inpatient | 4.6% | 4.7% | 1.39 (0.88) | 1.43 (0.94) |
| Emergency department | 9.9% | 10.1% | 2.15 (2.94) | 2.31 (3.26) |
| Physical health visits | ||||
| Inpatient | 10.7% | 12.1% | 1.39 (0.97) | 1.52 (1.37) |
| Emergency department | 39.0% | 42.8% | 2.51 (2.82) | 2.74 (3.59) |
| Primary care | 80.5% | 80.5% | 4.24 (3.74) | 4.38 (4.02) |
Note: Carve‐in group includes 15,601 individuals; carve‐out group includes 30,185 individuals.
Includes physicians, physician assistants, and advanced practice nursing providers specializing in primary care.
Restricted to the subset of outpatient services that are for evaluation and management.
Includes nurse practitioners and clinical nurse specialists specializing in mental health.
Includes counselors, therapists, and psychoanalysts.
All providers not included in other outpatient visit subtypes.
Table 3 displays differences between the carve‐in and carve‐out groups after adjusting for covariates and using the causal forest to control for potential interactions and nonlinearities among those variables. Individuals in the carve‐in group were more likely to have outpatient behavioral health visits compared to those in the carve‐out group (2.39 percentage points, p < 0.0001, with a baseline rate of approximately 73%). Conditional on accessing care, relative to the carve‐out group, individuals in the carve‐in group were likely to have 1.04 additional behavioral health visits (p < 0.0001).
TABLE 3.
Adjusted differences in service use for Medicaid carve‐in and carve‐out groups
| Difference in the probability of any visit (SE) | Difference in the number of visits (conditional on having at least one visit) (SE) | |
|---|---|---|
| Outpatient behavioral health visits | ||
| All | 2.39 *** (0.40) | 1.04 *** (0.24) |
| With a primary care provider a | 1.07 * (0.46) | 1.35 *** (0.16) |
| With a psychiatrist b | −1.99 *** (0.24) | −0.36 ** (0.11) |
| With a psychologist | 2.82 *** (0.22) | 0.23 (0.41) |
| With an advanced practice nursing provider c | 0.82 ** (0.31) | −0.22 ** (0.08) |
| With a behavioral health specialist d | −1.60 *** (0.43) | 0.38 (0.27) |
| With a social worker | 1.15 *** (0.35) | 1.51 *** (0.26) |
| With another provider type e | −1.72 *** (0.40) | 1.05 ** (0.33) |
| Other behavioral health visits | ||
| Inpatient | 0.27 (0.18) | −0.04 (0.04) |
| Emergency department | 0.01 (0.25) | −0.07 (0.08) |
| Physical health visits | ||
| Inpatient | 0.16 (0.25) | −0.06 (0.03) |
| Emergency department | −1.27 *** (0.38) | −0.12 ** (0.04) |
| Primary care | 1.58 *** (0.34) | 0.23 (0.03) |
Note: Carve‐in group includes 15,601 individuals; carve‐out group includes 30,185 individuals.
Bold values indicate significant results.
Includes physicians, physician assistants, and advanced practice nursing providers specializing in primary care.
Restricted to the subset of outpatient services that are for evaluation and management.
Includes nurse practitioners and clinical nurse specialists specializing in mental health.
Includes counselors, therapists, and psychoanalysts.
All providers not included in other outpatient visit subtypes.
p < 0.05.
p < 0.01.
p < 0.001.
Carve‐in status was also associated with the types of providers delivering behavioral health services to enrollees. The carve‐in was associated with a greater likelihood that primary care physicians, psychologists, and social workers delivered services. In contrast, the carve‐out group was associated with a greater likelihood that psychiatrists and behavioral health specialists delivered services. These results were generally consistent for estimates of the number of visits, conditional on accessing care, with four exceptions. We found no association with the number of visits for psychologists or behavioral health specialists. Beneficiaries in the carve‐in were more likely to access an advanced practice nursing provider, but had slightly fewer visits (−0.22) conditional on accessing care. Conversely, beneficiaries in the carve‐in were less likely to access “other” providers (not categorized as one of our provider subtypes) but had slightly more visits (1.05) conditional on accessing care. We observed no difference in behavioral health inpatient and ED use.
With respect to general medical services, after adjusting for covariates, individuals in the carve‐in group were more likely to have at least one primary care visit (1.58 percentage points, p < 0.0001) and less likely to have any ED visits (−1.27 percentage points, p < 0.0001). There was no difference in inpatient hospital use between the groups.
Figure 1 displays differential impacts of carve‐in status for individuals with SMI versus those with more moderate mental health conditions. The top panel displays access to any outpatient behavioral health care. The carve‐in was associated with greater access to outpatient behavioral health services for individuals with mild and moderate mental health conditions (2.78 percentage points; 95% CI 1.92, 3.64). However, among individuals with SMI, there was no significant association with carve‐in status (−0.27 percentage points; 95% CI −1.10, −0.56).
FIGURE 1.
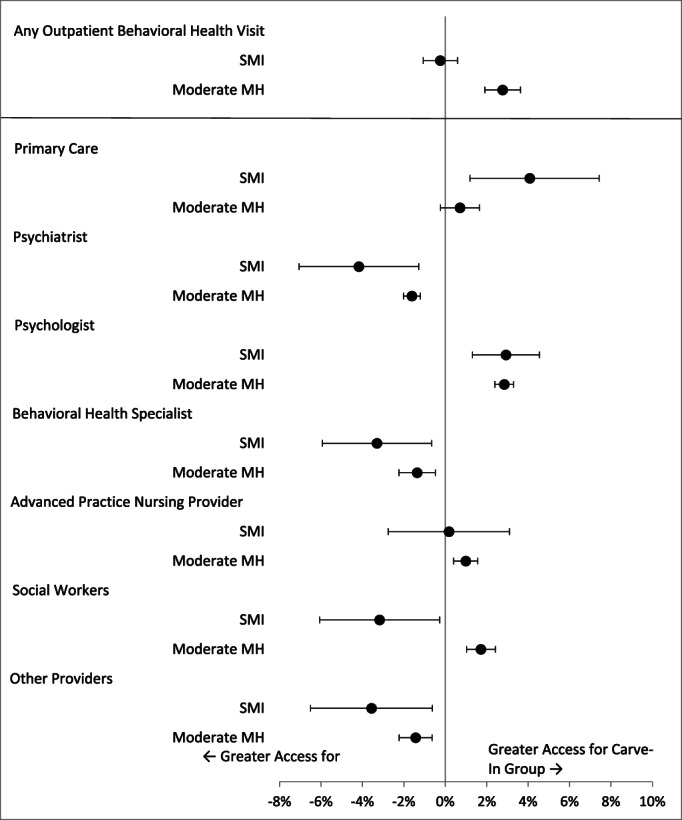
Difference in access rates for behavioral health visits for Medicaid carve‐in versus carve‐out, by mental health severity. The graph shows the adjusted estimates and 95% confidence intervals of difference in accessing care (probability of at least one visit) by carve‐in versus carve‐out for Medicaid enrollees with moderate mental health conditions (moderate MH) and serious mental illness (SMI)
The lower panel of Figure 1 displays the differences in access to behavioral health services by seven different provider types. Carve‐in status was associated with greater use of primary care physicians for behavioral health services among individuals with SMI. However, there was no association between carve‐in status and the use of primary care physicians for behavioral health services among individuals with mild or moderate mental health conditions. There was relatively little difference among most other provider types, except for social workers. The carve‐in was associated with greater access to social workers for individuals with mild and moderate mental health conditions but reductions in access for those with SMI.
Figure 2 displays differences in behavioral health access for black, Hispanic, and white individuals. Relative to white individuals, black individuals in the carve‐in model were more likely to have a behavioral health visit. There was no difference in the association of carve‐in status among white and Hispanic beneficiaries in overall behavioral health visits. As displayed in the lower panel, there was relatively little difference in the association of carve‐in status among black, Hispanic, and white individuals across the subtypes of outpatient behavioral health visits. However, Hispanic individuals were more likely than white individuals to access “other” providers.
FIGURE 2.
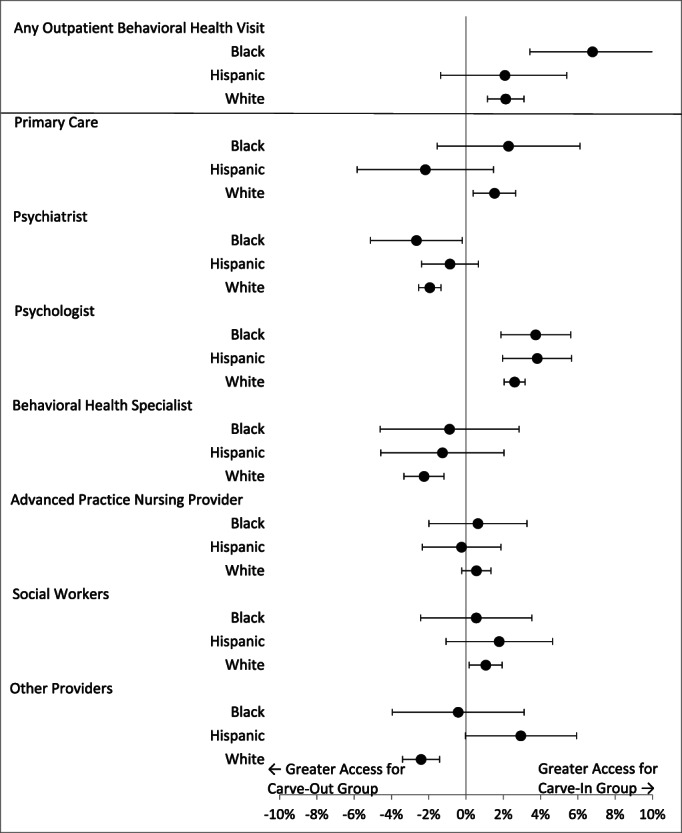
Difference in access rates for behavioral health visits for carve‐in versus carve‐out, comparing black, Hispanic, and white enrollees. The graph shows the adjusted estimates and 95% confidence intervals of difference in accessing care (probability of at least one visit) by carve‐on versus carve‐out for black, Hispanic, and white Medicaid enrollees
In sensitivity analyses, we compared estimates from the causal forest model to those with a linear probability model (see Appendix, Table A3). We conducted two comparisons: a set of estimates replicating the first column of Table 3 on the general population and a separate comparison focused on individuals with SMI. The majority of estimates were qualitatively similar in terms of estimates and SEs. However, the causal forest and linear probability models differed in their point estimates for some measures. For example, estimates of access for any outpatient behavioral health visit were higher in the causal forest model (2.39, p < 0.001) than the linear probability model (1.68, p < 0.001). In the SMI population, estimates of the probability of a behavioral health visit with a primary care provider were larger (3.94, p < 0.01) than the linear probability model (2.20, p = 0.15). The causal forest model's estimates for social workers were also larger in magnitude than the linear probability model. These differences may be a result of complex interactions or nonlinearities captured in the nonparametric causal forest model but not present in the linear probability model specification.
4. DISCUSSION
In this cross‐sectional study of two Oregon CCOs, we found that financial integration of behavioral health (“carving‐in”) was associated with greater access to outpatient behavioral health services for the average enrollee with mental illness. However, the magnitude of these associations differed by illness severity: individuals with mild to moderate mental illness were more likely to access behavioral health services if they were in a carve‐in arrangement, but we found no difference between carve‐in and carve‐out status for individuals with SMI. Furthermore, our findings varied across subtypes of outpatient behavioral health visits, with the carve‐in group associated with greater access to primary care providers, psychologists, and social workers but lower access to psychiatrists or behavioral health specialists. The carve‐in group was also associated with greater access to outpatient behavioral health visits for black patients relative to white patients. Among Hispanic patients, there was no association with carve‐in status and access to outpatient behavioral health care.
Our study on the carve‐out question in a Medicaid population is among the first conducted after the Affordable Care Act (ACA) brought on changes to Medicaid financing and benefit design and promoted the adoption of value‐based payment models. Although there is a large literature on behavioral health carve‐outs, many prior studies compared fee‐for‐service arrangements to managed care carve‐outs, a comparison that is less salient in an environment now dominated by managed care. Moreover, studies of carve‐out or carve‐in arrangements published since 2010 have primarily focused on the commercially insured population. 49 , 50 , 51 , 52
Perhaps as a result of a changing policy environment, contrary to older studies showing carve‐outs to be associated with reductions in inpatient care, 19 we did not observe similar effects. One potential reason is that successful efforts to reduce inpatient utilization through policy and delivery reforms implemented over the past decade have made it harder to reduce residual inpatient utilization.
Our study adds to literature suggesting that behavioral health integration may reduce racial and ethnic disparities in access to behavioral health services. 33 , 34 , 35 , 36 , 37 , 38 Carving‐in was associated with greater access for black patients relative to white patients, but there was no differential association for Hispanic patients. In Oregon, the behavioral health workforce is less diverse than the primary care workforce. 53 Thus, black patients seeking culturally appropriate care may have been more likely to obtain behavioral health services through integrated primary care sites. There is a need for additional research to elucidate the mechanisms that may reduce disparities in behavioral health services and to understand how these impacts may differ by race and ethnicity,
Our results suggest that carve‐in versus carve‐out arrangements introduce different tradeoffs on service use for patients with SMI compared to those with mild or moderate mental health conditions. Individuals with SMI may receive more specialist care through behavioral health settings, including community mental health centers, which have a tradition of contracting and networking with carve‐out models. 54 , 55 , 56 Moreover, those with SMI typically need greater access to psychiatrists, as primary care providers may lack the specialized training and resources to provide adequate treatment for this population. In comparison, individuals with mild and moderate mental health conditions may be adequately managed by generalists and more likely to benefit from behavioral health integration in primary care settings.
The extent to which carve‐in versus carve‐out arrangements align care delivery with specific behavioral health needs has implications for how states design their managed care contracts. While many states are moving away from Medicaid carve‐outs, there is significant heterogeneity in how they implement these changes. For example, Arizona and Florida's efforts to financially integrate plans have focused primarily on individuals with SMI. In contrast, New York has carved behavioral health services into its mainstream MCOs while designating a subset of plans that are designed specifically for individuals with SMI. 57 These models take into account the needs of a smaller group of enrollees with specific and more complex behavioral health conditions and acknowledge that some behavioral health specialization may have distinct advantages, including a single point of accountability and management expertise, access to specialized behavioral health provider networks, and greater levels of clinical specialization.
Our study suggests several directions for future research. Given the trend toward greater financial integration, there is a need for studies that can produce rigorous causal estimates of the impacts of these changes in Medicaid, potentially leveraging natural experiments. There is also a need for greater understanding of the ways these changes may impact different patient populations. Carve‐ins, or financial integration, may have differential impacts according to illness severity. Future studies should consider the optimal arrangements for these groups as well as for adults versus adolescents and children. Finally, there is a need for greater understanding of the role of subcontracting—an arrangement where the Medicaid managed care plan appears to have financially integrated care, but behavioral health and physical health are managed separately, with BHOs holding financial risk. These arrangements could potentially mediate the benefits anticipated with truly integrated services. In addition, subcontracting may offer states less control over access, quality, and network adequacy than in the arrangements where states pay BHOs directly or do not allow for subcontracting by MCOs.
4.1. Limitations
Our study had several limitations. First, as this study was cross‐sectional, groups were not randomized to carve‐in versus carve‐out models, and patients may differ in unobserved ways that could bias our estimates. However, the state attempted to balance population demographics when assigning members to CCOs, and our use of a wide range of covariates and machine‐learning‐based methods was designed to minimize selection effects.
Second, our analysis focused on CCOs, which are related to, but distinct from traditional MCOs. Furthermore, CCOs were subject to value‐based contracts with the state of Oregon. These contracts included incentive payments for performance on 18 measures, with three (alcohol or other substance misuse screening; screening for depression and use of a follow‐up plan; and follow‐up after hospitalization for mental illness) connected to behavioral health. Both CCOs were eligible for and received bonus payments in 2016; a portion of the bonus payment was transferred to the behavioral health carve‐out. Thus, incentive payments for behavioral health providers in each CCO were similar in theory, although we do not know about the relative magnitude of payments that providers received. These incentives may have reduced differences in utilization between the two CCOs in our study.
Third, although our study assessed differences in utilization, we did not examine other important outcomes, including the quality of behavioral and physical health care or the cost of care. In addition, our study used administrative claims data, which may not capture all clinically relevant information.
Fourth, this study uses data from a tri‐county area in a single state with a unique Medicaid model, comparing two CCOs. Our results may not be generalizable to other state or local contexts.
Finally, we focused on differences in how behavioral health financial risk was managed between two CCOs. However, the CCOs differed on a variety of other dimensions. The carve‐out group was almost twice the size of the carve‐in group and had received a $17M grant spanning 2012–2015 that may have allowed them to implement and scale interventions in a way that was not possible for the smaller carve‐in group. The CCOs differed in governance. The carve‐out CCO took a more decentralized approach, serving as a convener, whereas the carve‐in CCO's governance may be considered more centralized and cohesive. The carve‐in group reportedly paid higher rates for primary care (although we do not have access to the capitation rates or proprietary contracts). Differences in payment rates may partially explain higher rates of behavioral health service use in primary care in the carve‐in model. Additional research is needed to identify the causal impacts of integration and to provide more generalizable results. However, this paper does point to areas that may be worth investigating, including heterogeneous effects across services and patients.
5. CONCLUSIONS
In this study, Medicaid enrollees in a carve‐in arrangement were more likely to have outpatient behavioral health visits, although these findings varied by provider type and mental health severity. Current efforts to improve the integration of physical and behavioral health by financially integrating these services in Medicaid managed care may improve access to care. However, states and policy makers should anticipate that integration may lead to different outcomes according to illness severity, race and ethnicity, and provider type.
Supporting information
FIGURE A1 Cohort selection
TABLE A1. Mental health diagnosis categories, from the Refined Clinical Classification System (CCS‐R)
TABLES A2a, A2b, and A2c outline our approach for defining outpatient behavioral visits by provider type
TABLE A3. Comparison of causal forest with linear probability model
TABLE A4. RECORD statement—checklist of items, extended from the STROBE statement that should be reported in observational studies using routinely collected health data
ACKNOWLEDGMENTS
Joint Acknowledgement/Disclosure Statement by the National Institute of Mental Health K08MH123624; R01MH122199; R01MH123416; and the National Institute on Minority Health and Health Disparities R01MD011212. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Charlesworth CJ, Zhu JM, Horvitz‐Lennon M, McConnell KJ. Use of behavioral health care in Medicaid managed care carve‐out versus carve‐in arrangements. Health Serv Res. 2021;56(5):805-816. 10.1111/1475-6773.13703
See related Debate‐Commentary by Frank.
Funding information National Institute of Mental Health, Grant/Award Numbers: K08MH123624, R01MH122199, R01MH123416; National Institute on Minority Health and Health Disparities, Grant/Award Number: R01MD011212
REFERENCES
- 1. Mark TL, Yee T, Levit KR, Camacho‐Cook J, Cutler E, Carroll CD. Insurance financing increased for mental health conditions but not for substance use disorders, 1986–2014. Health Aff. 2016;35(6):958‐965. 10.1377/hlthaff.2016.0002 [DOI] [PubMed] [Google Scholar]
- 2. Katon W. Collaborative depression care models: from development to dissemination. Am J Prev Med. 2012;42(5):550‐552. 10.1016/j.amepre.2012.01.017 [DOI] [PubMed] [Google Scholar]
- 3. Unützer J, Schoenbaum M, Druss BG, Katon WJ. Transforming mental health care at the interface with general medicine: report for the Presidents Commission. Psychiatr Serv. 2006;57(1):37‐47. 10.1176/appi.ps.57.1.37 [DOI] [PubMed] [Google Scholar]
- 4. Bachman J, Pincus HA, Houtsinger JK, Unützer J. Funding mechanisms for depression care management: opportunities and challenges. Gen Hosp Psychiatry. 2006;28(4):278‐288. 10.1016/j.genhosppsych.2006.03.006 [DOI] [PubMed] [Google Scholar]
- 5. Frank RG, Huskamp HA, Pincus HA. Aligning incentives in the treatment of depression in primary care with evidence‐based practice. Psychiatr Serv. 2003;54(5):682‐687. 10.1176/appi.ps.54.5.682 [DOI] [PubMed] [Google Scholar]
- 6. Goldberg RJ. Financial incentives influencing the integration of mental health care and primary care. Psychiatr Serv. 1999;50(8):1071‐1075. 10.1176/ps.50.8.1071 [DOI] [PubMed] [Google Scholar]
- 7. Shmerling AC, Gold SB, Gilchrist EC, Miller BF. Integrating behavioral health and primary care: a qualitative analysis of financial barriers and solutions. Transl Behav Med. 2020;10(3):648‐656. 10.1093/tbm/ibz026 [DOI] [PubMed] [Google Scholar]
- 8. Thota AB, Sipe TA, Byard GJ, et al. Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta‐analysis. Am J Prev Med. 2012;42(5):525‐538. 10.1016/j.amepre.2012.01.019 [DOI] [PubMed] [Google Scholar]
- 9. Unutzer J, Katon WJ, Callahan CM, et al. Collaborative care management of late‐life depression in the primary care setting: a randomized controlled trial. J Am Med Assoc. 2002;288(22):2836‐2845. 10.1001/jama.288.22.2836 [DOI] [PubMed] [Google Scholar]
- 10. Archer J, Bower P, Gilbody S, et al. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev. 2012;10:CD006525. 10.1002/14651858.CD006525.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. O'Connor EA, Whitlock EP, Beil TL, Gaynes BN. Screening for depression in adult patients in primary care settings: a systematic evidence review. Ann Intern Med. 2009;151(11):793‐803. 10.7326/0003-4819-151-11-200912010-00007 [DOI] [PubMed] [Google Scholar]
- 12. Siu AL, Bibbins‐Domingo K, Grossman DC, et al. Screening for depression in adults: US preventive services task force recommendation statement. JAMA. 2016;315(4):380‐387. 10.1001/jama.2015.18392 [DOI] [PubMed] [Google Scholar]
- 13. Gilbody S, Bower P, Fletcher J, Richards D, Sutton AJ. Collaborative care for depression: a cumulative meta‐analysis and review of longer‐term outcomes. Arch Intern Med. 2006;166(21):2314‐2321. 10.1001/archinte.166.21.2314 [DOI] [PubMed] [Google Scholar]
- 14. Hunkeler EM, Katon W, Tang L, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ. 2006;332(7536):259‐263. 10.1136/bmj.38683.710255.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Woltmann E, Grogan‐Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta‐analysis. Am J Psychiatry. 2012;169(8):790‐804. 10.1176/appi.ajp.2012.11111616 [DOI] [PubMed] [Google Scholar]
- 16. Miller CJ, Grogan‐Kaylor A, Perron BE, Kilbourne AM, Woltmann E, Bauer MS. Collaborative chronic care models for mental health conditions: cumulative meta‐analysis and meta‐regression to guide future research and implementation. Med Care. 2013;51(10):922‐930. 10.1097/MLR.0b013e3182a3e4c4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Edwards E. Assessing Changes to Medicaid Managed Care Regulations: Facilitating Integrationof Physical and Behavioral Health Care. New York: Commonwealth Fund; 2017. https://www.commonwealthfund.org/publications/issue-briefs/2017/oct/assessing-changes-medicaid-managed-care-regulations-facilitating. Accessed November 13, 2018. [PubMed] [Google Scholar]
- 18. Gifford K, Ellis E, Lashbrook A, Nardone MA, Hinton E, Rudowitz R, et al. A View from the States: Key Medicaid Policy Changes: Results from a 50‐State Medicaid Budget Survey for State Fiscal Years 2019 and 2020. San Francisco, CA: Kaiser Family Foundation; 2019. https://www.kff.org/medicaid/report/a-view-from-the-states-key-medicaid-policy-changes-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2019-and-2020/. Accessed January 4, 2021. [Google Scholar]
- 19. Frank RG, Garfield RL. Managed behavioral health care carve‐outs: past performance and future prospects. Annu Rev Public Health. 2007;28(1):303‐320. 10.1146/annurev.publhealth.28.021406.144029 [DOI] [PubMed] [Google Scholar]
- 20. McConnell KJ. Oregon's Medicaid coordinated care organizations. JAMA. 2016;315(9):869‐870. 10.1001/jama.2016.0206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. McConnell KJ, Chang AM, Cohen D, et al. Oregon's Medicaid transformation: an innovative approach to holding a health system accountable for spending growth. Health Care J Deliv Sci Innov. 2014;2(3):163‐167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. McConnell KJ, Renfro S, Lindrooth RC, Cohen DJ, Wallace NT, Chernew ME. Oregon's Medicaid reform and transition to global budgets were associated with reductions in expenditures. Health Aff. 2017;36(3):451‐459. 10.1377/hlthaff.2016.1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Phelan JC, Bruce G. Is racism a fundamental cause of inequalities in health? Annu Rev Sociol. 2015;41(1):311‐330. [Google Scholar]
- 24. Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annu Rev Public Health. 2019;40:105‐125. 10.1146/annurev-publhealth-040218-043750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Horvitz‐Lennon M, McGuire TG, Alegria M, Frank RG. Racial and ethnic disparities in the treatment of a Medicaid population with schizophrenia. Health Serv Res. 2009;44(6):2106‐2122. 10.1111/j.1475-6773.2009.01041.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Horvitz‐Lennon M, Volya R, Donohue JM, Lave JR, Stein BD, Normand S‐LT. Disparities in quality of care among publicly insured adults with schizophrenia in four large U.S. states, 2002–2008. Health Serv Res. 2014;49(4):1121‐1144. 10.1111/1475-6773.12162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Horvitz‐Lennon M, Volya R, Garfield R, Donohue JM, Lave JR, Normand S‐LT. Where you live matters: quality and racial/ethnic disparities in schizophrenia care in four state Medicaid programs. Health Serv Res. 2015;50(5):1710‐1729. 10.1111/1475-6773.12296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cook BL, Liu Z, Lessios AS, Loder S, McGuire T. The costs and benefits of reducing racial‐ethnic disparities in mental health care. Psychiatr Serv. 2015;66(4):389‐396. 10.1176/appi.ps.201400070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cook BL, McGuire TG, Zuvekas SH. Measuring trends in racial/ethnic health care disparities. Med Care Res Rev. 2009;66(1):23‐48. 10.1177/1077558708323607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cook BL, Zuvekas SH, Carson N, Wayne GF, Vesper A, McGuire TG. Assessing racial/ethnic disparities in treatment across episodes of mental health care. Health Serv Res. 2014;49(1):206‐229. 10.1111/1475-6773.12095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Copeland LA, Zeber JE, Valenstein M, Blow FC. Racial disparity in the use of atypical antipsychotic medications among veterans. Am J Psychiatry. 2003;160(10):1817‐1822. 10.1176/appi.ajp.160.10.1817 [DOI] [PubMed] [Google Scholar]
- 32. Kreyenbuhl J, Zito JM, Buchanan RW, Soeken KL, Lehman AF. Racial disparity in the pharmacological management of schizophrenia. Schizophr Bull. 2003;29(2):183‐194. 10.1093/oxfordjournals.schbul.a006996 [DOI] [PubMed] [Google Scholar]
- 33. McGuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: policy implications. Health Aff. 2008;27(2):393‐403. 10.1377/hlthaff.27.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Miranda J, Schoenbaum M, Sherbourne C, Duan N, Wells K. Effects of primary care depression treatment on minority patients' clinical status and employment. Arch Gen Psychiatry. 2004;61(8):827‐834. 10.1001/archpsyc.61.8.827 [DOI] [PubMed] [Google Scholar]
- 35. Ell K, Katon W, Xie B, et al. Collaborative care management of major depression among low‐income, predominantly Hispanic subjects with diabetes a randomized controlled trial. Diabetes Care. 2010;33(4):706‐713. 10.2337/dc09-1711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ell K, Katon W, Cabassa LJ, et al. Depression and diabetes among low‐income Hispanics: design elements of a socio‐culturally adapted collaborative care model randomized controlled trial. Int J Psychiatry Med. 2009;39(2):113‐132. 10.2190/PM.39.2.a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Areán PA, Ayalon L, Hunkeler E, et al. Improving depression care for older, minority patients in primary care. Med Care. 2005;43(4):381‐390. [DOI] [PubMed] [Google Scholar]
- 38. Wolff LS, Flynn A, Xuan Z, Errichetti KS, Tapia Walker S, Brodesky MK. The effect of integrating primary care and mental health services on diabetes and depression: a multi‐site impact evaluation on the US‐Mexico border. Med Care. 2021;59(1):67‐76. 10.1097/MLR.0000000000001429 [DOI] [PubMed] [Google Scholar]
- 39. McConnell KJ, Charlesworth CJ, Meath THA, George RM, Kim H. Oregon's emphasis on equity shows signs of early success for black and American Indian Medicaid enrollees. Health Aff. 2018;37(3):386‐393. 10.1377/hlthaff.2017.1282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vorenberg S. Health Share and FamilyCare: A Tale of Two CCOs. Portland, OR: Lund Report; 2017. https://www.thelundreport.org/content/health-share-and-familycare-tale-two-ccos. [Google Scholar]
- 41. Agency for Healthcare Research and Quality . Clinical Classifications Software. Published 2016. Rockville, MD; 2020. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccsfactsheet.jsp. [Google Scholar]
- 42. Einav L, Finkelstein A, Mullainathan S, Obermeyer Z. Predictive modeling of U.S. health care spending in late life. Science. 2018;360(6396):1462‐1465. 10.1126/science.aar5045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Chang C‐H, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries' health outcomes. J Am Med Assoc. 2011;305(20):2096‐2104. 10.1001/jama.2011.665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Athey S, Tibshirani J, Wager S. Generalized random forests. Ann Stat. 2019;47(2):1148‐1178. 10.1214/18-AOS1709 [DOI] [Google Scholar]
- 45. Breiman L. Random forests. Mach Learn. 2001;45(1):5‐32. 10.1023/A:1010933404324 [DOI] [Google Scholar]
- 46. McConnell KJ, Lindner S. Estimating treatment effects with machine learning. Health Serv Res. 2019;54(6):1273‐1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Imbens GW. Nonparametric estimation of average treatment effects under exogeneity: a review. Rev Econ Stat. 2004;86(1):4‐29. 10.1162/003465304323023651 [DOI] [Google Scholar]
- 48. Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity‐score matched samples. Stat Med. 2009;28(25):3083‐3107. 10.1002/sim.3697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ettner SL, Xu H, Azocar F. What happens when employers switch from a “carve‐out” to a “carve‐in” model of managed behavioral health? J Ment Health Policy Econ. 2019;22(3):85‐94. [PubMed] [Google Scholar]
- 50. Harwood JM, Azocar F, Thalmayer A, et al. The mental health parity and addiction equity act evaluation study: impact on specialty behavioral healthcare utilization and spending among carve‐in enrollees. Med Care. 2017;55(2):164‐172. 10.1097/MLR.0000000000000635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Friedman SA, Thalmayer AG, Azocar F, et al. The mental health parity and addiction equity act evaluation study: impact on mental health financial requirements among commercial “carve‐in” plans. Health Serv Res. 2018;53(1):366‐388. 10.1111/1475-6773.12614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Friedman S, Xu H, Azocar F, Ettner SL. Carve‐out plan financial requirements associated with national behavioral health parity. Health Serv Res. 2020;55(6):924‐931. 10.1111/1475-6773.13542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Oregon Health Authority . The Diversity of Oregon's Licensed Health Care Workforce; Salem, OR: Oregon Health Authority; 2021. https://www.oregon.gov/oha/HPA/ANALYTICS/HealthCareWorkforceReporting/2021-Workforce-Diversity-for-web.pdf. Accessed March 1, 2021. [Google Scholar]
- 54. Cunningham P, McKenzie K, Taylor EF. The struggle to provide community‐based care to low‐income people with serious mental illnesses. Health Aff. 2006;25(3):694‐705. 10.1377/hlthaff.25.3.694 [DOI] [PubMed] [Google Scholar]
- 55. Drake RE, Green AI, Mueser KT, Goldman HH. The history of community mental health treatment and rehabilitation for persons with severe mental illness. Community Ment Health J. 2003;39(5):427‐440. 10.1023/A:1025860919277 [DOI] [PubMed] [Google Scholar]
- 56. Whitaker RG, Kilany M, Wells R, Domino ME. Are certain health centers better patient‐centered medical homes for people with severe mental illness? Psychiatry Q. 2021;92:107‐122. 10.1007/s11126-020-09754-1 [DOI] [PubMed] [Google Scholar]
- 57. Soper MH. Integrating Behavioral Health into Medicaid Managed Care: Lessons from State Innovators. Hamilton, NJ: Center for Health Care Strategies; 2016. https://www.chcs.org/resource/integrating‐behavioral‐health‐into‐medicaid‐managed‐care‐design‐and‐implementation‐lessons‐from‐state‐innovators/. Accessed July 12, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
FIGURE A1 Cohort selection
TABLE A1. Mental health diagnosis categories, from the Refined Clinical Classification System (CCS‐R)
TABLES A2a, A2b, and A2c outline our approach for defining outpatient behavioral visits by provider type
TABLE A3. Comparison of causal forest with linear probability model
TABLE A4. RECORD statement—checklist of items, extended from the STROBE statement that should be reported in observational studies using routinely collected health data


