Abstract
Objective
To improve food insecurity interventions, we sought to better understand the hypothesized bidirectional relationship between food insecurity and health care expenditures.
Data Source
Nationally representative sample of the civilian noninstitutionalized population of the United States (2016‐2017 Medical Expenditure Panel Survey [MEPS]).
Study Design
In a retrospective longitudinal cohort, we conducted two sets of analyses: (a) two‐part models to examine the association between food insecurity in 2016 and health care expenditures in 2017; and (b) logistic regression models to examine the association between health care expenditures in 2016 and food insecurity in 2017. We adjusted for demographic and socioeconomic variables as well as 2016 health care expenditures and food insecurity.
Data Collection
Health care expenditures, food insecurity, and medical condition data from 10 886 adults who were included in 2016‐2017 MEPS.
Principal Findings
Food insecurity in 2016, compared with being food secure, was associated with both a higher odds of having any health care expenditures in 2017 (OR 1.29, 95% CI: 1.04 to 1.60) and greater total expenditures ($1738.88 greater, 95% CI: $354.10 to $3123.57), which represents approximately 25% greater expenditures. Greater 2016 health care expenditures were associated with slightly higher odds of being food insecure in 2017 (OR 1.007 per $1000 in expenditures, 95% CI: 1.002 to 1.012, P =0.01). Exploratory analyses suggested that poor health status may underlie the relationship between food insecurity and health care expenditures.
Conclusions
A bidirectional relationship exists between food insecurity and health care expenditures, but the strength of either direction appears unequal. Higher health care expenditures are associated with a slightly greater risk of being food insecure (adjusted for baseline food insecurity status) but being food insecure is associated with substantially greater subsequent health care expenditures (adjusted for baseline health care expenditures). Interventions to address food insecurity and poor health may be helpful to break this cycle.
Keywords: chronic disease, external debt, food insecurity, health expenditures, prescription drugs
What is already known on this topic
Food insecurity is associated with higher health care expenditures
It is unclear whether this association reflects food insecurity causing poorer health and thus higher expenditures, or higher expenditures draining household food budgets and leading to food insecurity
A bidirectional relationship between food insecurity and healthcare expenditures is hypothesized.
What This Study Adds
Utilizing a nationally representative panel survey that, for the first time, includes information on individual food insecurity and health care expenditures across at least two years, we demonstrate that a bidirectional relationship exists between food insecurity and health care expenditures.
However, the association between food insecurity and health care expenditures in the following year appears larger than the association between health care expenditures and food insecurity in the following year.
To break the cycle between food insecurity and health care expenditures, interventions that address food insecurity may have greater impact than those that offset health care expenditures.
1. INTRODUCTION
Food insecurity, inconsistent access to enough food for an active, healthy life, affected over 37 million Americans in 2018 (11.1% of households). 1 Early reports suggest that food insecurity has nearly tripled as a consequence of the COVID‐19 pandemic. 2 Food insecurity is associated with a range of cardiometabolic (eg, diabetes mellitus, coronary heart disease) and other chronic conditions. 3 , 4 , 5 , 6 , 7 , 8 Reasons for these associations include lower diet quality, tradeoffs between food and other necessities such as medications, and the stress of food insecurity which shifts attentions toward meeting immediate needs and away from long‐term health. 3 , 9 , 10 , 11 Food insecurity is also associated with more emergency department visits, inpatient hospitalizations, and greater health care expenditures. 12 , 13 , 14 , 15 , 16 For these reasons, food insecurity has emerged as a key target for programs that seek to address health‐related social needs in order to improve health, reduce hospitalizations, and lower health care costs. 17 , 18
However, much remains to be understood about the relationship between food insecurity and health care expenditures. A leading conceptual model 3 posits a “bidirectional” relationship such that food insecurity is associated with worse health (leading to greater health care expenditures), but also that poor health (and associated greater health care expenditures) can lead households to become food insecure (eg, by impeding the ability to work or diverting resources needed for food toward medical expenses) (Figure 1). While both directions are plausible, it has been difficult to examine this hypothesis in detail owing to lack of data. Specifically, nationally representative data that simultaneously assess food insecurity and health care expenditures at two time points have not previously been available. This represents an important knowledge gap, particularly with regard to food insecurity interventions. Better understanding the strength of the relationship between food insecurity and health care costs, in both directions, would inform interventions that seek to break this vicious cycle.
FIGURE 1.
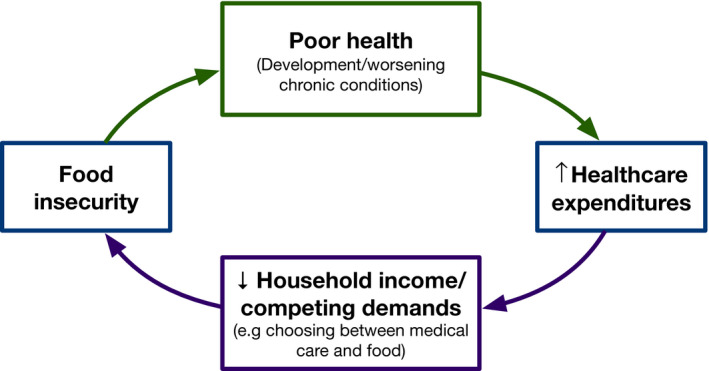
Conceptual model of the relationship between food insecurity and health care expenditures
In this study, we take advantage of recently available data from the Medical Expenditure Panel Survey (MEPS), 19 which assesses food insecurity and health care expenditures longitudinally. We use these data to examine the bidirectional hypothesis, examining whether food insecurity, accounting for baseline health care expenditures, is associated with greater subsequent health care expenditures, and whether health care expenditures, accounting for baseline food insecurity, are associated with subsequent food insecurity risk. In keeping with our conceptual model, we hypothesize support for both associations.
2. METHODS
2.1. Data source and study population
Data for this study came from the 2016 and 2017 Household Component Data Files of the Medical Expenditure Panel Survey (MEPS), a nationally representative, longitudinal survey conducted by the Agency for Healthcare Research and Quality (AHRQ). 19 MEPS follows the same cohort of individuals for two years of observation. Food insecurity, assessed using the 10 adult‐referenced items of the USDA Household Food Security Survey Module with a 30‐day look‐back period (full questionnaire available at ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Survey_Questionnaires/NHIS/2011/English/qfamily.pdf), was available in MEPS in 2016 and 2017. Questions include, for instance, whether “anyone in the household [did] not eat for a whole day because there wasn't enough money for food.” We merged responses from the 2016 and 2017 Food Insecurity File to the 2016 and 2017 Full Year Consolidated Data File. We included all adults (age ≥ 18 years at study entry) who participated in MEPS in 2016 and 2017. Because this study used only publicly available deidentified data, it was not considered human subject research.
2.2. Exposures and outcomes
Given the bidirectional hypothesis examined in this study, two measures constituted either the main outcome or the exposure variable in our analysis: food insecurity status and annual health care expenditures. In accordance with the typical USDA scoring system, food security status was categorized as food insecure if a positive response was recorded for any two or more questions within the 10‐item food insecurity questionnaire, and as food secure otherwise. 20 Annual health care expenditures (total and broken down by type: inpatient, outpatient, emergency department, prescription drug, and out‐of‐pocket) were gathered from MEPS and expressed as continuous variables. According to AHRQ, “expenditures in MEPS are comprised of direct payments for care provided during the year, including out‐of‐pocket payments and payments by private insurance, Medicaid, Medicare, and other sources.” 19
2.3. Covariates and data extraction
The potential association between food insecurity and health care expenditures could be confounded by several socioeconomic and demographic variables. These variables were extracted from the merged data file and included responses to questions concerning race/ethnicity (Hispanic, non‐Hispanic white, non‐Hispanic black, non‐Hispanic Asian /multirace/other), gender (male, female), age, income level (expressed as percent of the Federal Poverty Level [FPL], which accounts for household size), education level (less than high school diploma, high school diploma, greater than high school diploma), region of residence (Northeast, Midwest, South, West), and health insurance status (private only, any Medicare, other public [which includes Medicaid and SCHIP], and uninsured). To examine associations between food insecurity and expenditures among those with chronic medical conditions 5 , 21 and disability, 22 we also extracted information concerning self‐reported chronic medical conditions (arthritis, high blood pressure, diabetes, chronic obstructive pulmonary disorder [emphysema or chronic bronchitis], stroke) and disabilities (determined by reported limitations in any of the following domains: ambulatory, cognitive, hearing, vision, independent living or self‐care). We also extracted information on self‐reported medical debt, 23 to examine how this may relate to food insecurity and health care expenditures. Medical debt was expressed as a binary variable and positive if an affirmative response was recorded for any of three questions concerning problems with paying medical bills, medical bills being paid off over time, or having medical bills that are unable to be paid off.
2.4. Statistical analysis
This study consisted of two main analyses. The first considered the association between food insecurity status in 2016 and total health care expenditures in 2017. Given known difficulties in modeling health care expenditures (eg, point mass at zero, extreme observations), we used a two‐part model. 24 , 25 The first part consisted of multivariable logistic regression to model the association between food insecurity in 2016 and having any health care expenditures in 2017. The second part used a generalized linear model (GLM) with a log link and a gamma distribution to model, among those with nonzero expenditures, the association between food insecurity in 2016 and the overall amount of total health care expenditures in 2017. We used a modified Park test to determine that a gamma distribution was the appropriate distributional form for the GLM. 24 Both model parts were adjusted for race/ethnicity, gender, age, income level, education level, region of residence, and health insurance (our primary adjustment set) along with total health care expenditures in 2016. Hypothesis testing was conducted on the odds ratio (OR) from the logistic model (first part) and the exponentiated coefficient from the gamma GLM (second part) associated with food insecurity status in 2016. The exponentiated coefficient from a gamma GLM represents a ratio of expenditures between the two groups (eg, a value of 1.5 would indicate that mean expenditures were 1.5 times greater in the group of interest relative to the comparison group).
Our second set of analyses used health care expenditures as the exposure and food insecurity as the outcome. To examine the association between total health care expenditures in 2016 and food insecurity in 2017, we utilized a multivariable logistic regression model in which the primary dependent variable was food insecurity status in 2017 and the primary independent variable was total health care expenditures in 2016, expressed in $1000s to facilitate coefficient interpretation. Additional covariates in this model included our primary adjustment set along with food insecurity status in 2016. Hypothesis testing was conducted on the odds ratio associated with total health care expenditures in 2016.
To express results more clearly, we used outcome predictions estimated by the “margins” command in STATA. Given the distortion outliers have when estimating predicted margins, we used a winsorizing cutoff at the 97.5th percentile of total expenditures, which was $39 151 in this sample, and conducted sensitivity analyses at different thresholds, including not winsorizing. Given the complex survey design of MEPS, we used STATA svy commands for all analyses in order to calculate appropriate standard errors and include survey weights. Following guidance given by AHRQ, individual panel weights used in our models were the average of individual panel weights from the 2016 and 2017 data files. 19 Because missingness for any variable was <5%, missing data were not imputed. Given the two main analyses, a two‐sided P‐value < 0.025 was taken to indicate statistical significance.
2.5. Secondary analyses
In a set of secondary analyses, we considered the bidirectional relationship between food insecurity and health care expenditures across different sources of health care expenditures and within subgroups of individuals with several self‐reported chronic medical conditions.
Expenditure types (emergency department, outpatient, inpatient, prescription drugs, and out‐of‐pocket) were substituted for the dependent variable when using our two‐part model to estimate the association between food insecurity status in 2016 and health care expenditures in 2017 and as the independent variable when using our logistic model to estimate the association between health care expenditures in 2016 on food insecurity status in 2017. To examine the relationship between food insecurity and health care expenditures in subpopulations defined by different comorbidities, we fit the same regression models as in our main analyses but in samples stratified by comorbidity status (hypertension, COPD, arthritis, stroke, and diabetes mellitus).
2.6. Exploratory analyses
To better understand potential mechanisms underlying the relationship between total health care expenditures in 2016 and food insecurity in 2017, we conducted several exploratory analyses. Given that individuals may be food insecure due to financial trade‐offs between food and competing expenses, we sought to understand how medical debt may affect the association between food insecurity and health care expenditures. We interrogated this mechanism by incorporating an indicator of medical debt into our main analysis. Next, if the association between health care expenditures and food insecurity is in large part based on health care expenditures serving as an indicator for poor health status, then adjusting for other indicators of poor health should weaken this association. To assess this idea, we conducted an exploratory analysis in which we added a self‐reported disability variable to our main analysis.
2.7. Sensitivity analyses
To test whether the results of our main analyses were sensitive to alternative modeling specifications, we conducted several sensitivity analyses. First, we conducted sensitivity analyses modeling expenditures as the outcome using Poisson and negative binomial distributions, rather than a gamma distribution. Next, we conducted analyses at different winsorizing cutoffs (90th, 95th, and 99th percentiles, and no winsorization). Next, we conducted analyses in which health care expenditures were treated as a categorical rather than continuous variable (expressed as deciles). Finally, we conducted analyses adjusting for both 2016 and 2017 health insurance status.
3. RESULTS
Our final study sample consisted of 10 866 respondents. In 2016, 1365 (weighted percent 8.97%) of our sample were food insecure (Table 1). Among other differences, compared with those who were food secure in 2016, those who were food insecure in 2016 were more likely to self‐identify as a racial/ethnic minority, be uninsured, have medical debt, and less likely to have a high school diploma or have private insurance.
TABLE 1.
Characteristics of study sample a
| Total (N = 10 886) Weighted percent (n) or mean (standard error) b | Food secure (N = 9521) Weighted percent (n) or mean (standard error) b | Food insecure (N = 1365) Weighted percent (n) or mean (standard error) b | P value | |
|---|---|---|---|---|
| Age (years) | 47.73 (0.3) | 48.17 (0.31) | 43.33 (0.6) | <0.0001 |
| Female | 52% (5922) | 51% (5096) | 57% (826) | 0.0035 |
| Race/ethnicity | ||||
| Hispanic | 16% (3169) | 15% (2637) | 24% (532) | 0.0012 |
| Non‐Hispanic white only | 64% (4660) | 66% (4271) | 48% (389) | <0.001 |
| Non‐Hispanic black only | 12% (2019) | 11% (1660) | 21% (359) | <0.001 |
| Non‐Hispanic Asian/multirace/other | 8% (1038) | 8% (953) | 7% (85) | <0.001 |
| Education attainment | ||||
| <High school diploma | 14% (2390) | 13% (1873) | 30% (517) | <0.001 |
| High school diploma | 44% (4756) | 43% (4103) | 50% (653) | 0.0074 |
| >High school diploma | 42% (3740) | 44% (3545) | 20% (195) | <0.001 |
| Income (% FPL) | 441.2 (8.05) | 466.57 (8.54) | 183.71 (8.54) | <0.001 |
| Income categories | ||||
| <100% FPL | 11% (1792) | 9% (1331) | 30% (461) | <0.001 |
| 100%‐199% FPL | 16% (2339) | 14% (1839) | 35% (500) | <0.001 |
| >200% FPL | 73% (6755) | 77% (6351) | 35% (404) | <0.001 |
| Census region | ||||
| Northeast | 18% (1763) | 18% (1548) | 14% (215) | 0.1043 |
| Midwest | 21% (2123) | 21% (1876) | 22% (247) | 0.5645 |
| South | 38% (4178) | 37% (3582) | 41% (596) | 0.1877 |
| West | 23% (2822) | 24% (2515) | 22% (307) | 0.5981 |
| Insurance type | ||||
| Private only | 59% (5557) | 61% (5133) | 36% (424) | <0.001 |
| Other public | 20% (1987) | 21% (1846) | 10% (141) | <0.001 |
| Any medicare | 13% (1966) | 10% (1426) | 37% (540) | <0.001 |
| Uninsured | 8% (1376) | 7% (1116) | 17% (260) | <0.001 |
| Medical debt status | 22% (2434) | 19% (1826) | 51% (608) | <0.001 |
| Any disability | 19% (2088) | 18% (1657) | 34% (431) | <0.001 |
| Health conditions | ||||
| Hypertension | 33% (3670) | 33% (3172) | 34% (498) | 0.5700 |
| COPD c | 4% (365) | 3% (268) | 9% (97) | <0.001 |
| Arthritis | 27% (2686) | 26% (2314) | 30% (372) | 0.1526 |
| Stroke | 4% (439) | 4% (353) | 6% (86) | 0.1114 |
| Diabetes mellitus | 11% (1293) | 10% (1079) | 14% (214) | 0.0140 |
All characteristics based on 2016 data, restricted to individuals aged ≥18 years
Proportions and standard errors adjusted for survey weights
Individuals categorized as COPD had been given a diagnosis of either chronic bronchitis or emphysema
3.1. Main analyses
3.1.1. Food insecurity as predictor of health care expenditures
In analyses adjusted for race/ethnicity, gender, age, income level, education level, region of residence, health insurance status, and total health care expenditures in 2016, our two‐part model estimated that being food insecure in 2016 was associated with a greater odds of having any health care expenditures in 2017 (OR: 1.29, 95% CI: 1.04 to 1.60) and, among those with nonzero expenditures, a greater amount of total expenditures (ratio of expenditures: 1.26, 95% CI: 1.08 to 1.48). When combining both parts of the model, we estimate that food insecurity in 2016 was associated with $1739 (95% CI: $354 to $3124) more total health care expenditures in 2017 (Table 2 ). This represents 25% greater expenditures ($8566 95%CI $7164 to $9969 in 2017 annual health care expenditures associated with food insecurity; $6827 95%CI $6372 to $7282 associated with food security). The full model output is presented in Appendix S1: Table S1.
TABLE 2.
Bidirectional association between food insecurity and health expenditures
| Association between food insecurity in 2016 on total health care expenditures in 2017 | ||||
|---|---|---|---|---|
| Food Insecurity Status | Adjusted b odds ratio of nonzero expenditures (95% CI) | Adjusted b ratio of expenditures c from gamma glm (95% CI) | Annual estimated total 2017 health care expenditures (95% CI) | Annualized difference in estimated total health care expenditures between those who experience food insecurity and those who are food secure (95% CI) |
| Food Insecure | 1.29 (1.04, 1.60) | 1.26 (1.08, 1.48) | $8566 ($7164, $9969) | $1739 ($354, $3124) |
| Food Secure | Referent | Referent | $6827 ($6372, $7282) | ‐ |
| Association between healthcare expenditures in 2016 ($1000s) and food insecurity in 2017 | |
|---|---|
| Unadjusted odds ratio (95% CI) | Adjusted a odds ratio (95% CI) |
| 1.006 (1.001, 1.01) | 1.007 (1.002, 1.01) |
Abbreviation: GLM, generalized linear model
Adjusted for age, sex, income level, health insurance status, education level, race, and food insecurity status in 2016
Adjusted for age, sex, income level, health insurance status, education level, race, and total health care expenditures in 2016.
Interpretation of “Ratio of Expenditures” from GLM: The geometric mean expenditures from individuals experiencing food insecurity will be 1.26 times the amount of expenditures of individuals who are food secure, adjusted for other variables in the model.
Health care expenditures reported in 2017 USD.
3.1.2. Health care expenditures as predictor of food insecurity
In analyses adjusted for race/ethnicity, gender, age, income level, education level, region of residence, health insurance status, and food insecurity levels in 2016, our multivariable logistic model estimated that every increase in $1000 of total expenditures was associated with slightly greater odds of being food insecure in 2017 (OR: 1.007, 95% CI: 1.002 to 1.01). The full model output is presented in Appendix S1: Table S2.
3.2. Secondary analyses
To examine how food insecurity may be associated with specific categories of health care expenditures, we refit our main analyses while replacing total health care expenditures with specific expenditure categories as the outcome. Associations between food insecurity and these categories were most pronounced for prescription spending (Table 3). The association between 2016 out‐of‐pocket expenditures and 2017 food insecurity status was not significant. Estimated expenditures across all expenditure types are presented in Appendix S1: Table S3.
TABLE 3.
Bidirectional association between food insecurity and health expenditures by expenditure type
| Association between 2016 food insecurity and 2017 health care expenditures a | |||
|---|---|---|---|
| Expenditure type | Food security status | Adjusted b odds ratio of nonzero expenditures (95% CI) | Adjusted b ratio of expenditures from GLM (95% CI) |
| Emergency Department | Food insecure | 1.676 (1.397, 2.01) | 0.966 (0.777, 1.201) |
| Food secure | Referent | Referent | |
| Outpatient | Food insecure | 1.288 (1.032, 1.608) | 1.099 (0.795, 1.52) |
| Food secure | Referent | Referent | |
| Inpatient | Food insecure | 1.445 (1.12, 1.865) | 0.973 (0.757, 1.251) |
| Food secure | Referent | Referent | |
| Prescription | Food insecure | 1.528 (1.27, 1.839) | 1.479 (1.199, 1.824) |
| Food secure | Referent | Referent | |
| Out‐of‐pocket | Food insecure | 1.323 (1.101, 1.59) | 0.947 (0.796, 1.128) |
| Food secure | Referent | Referent | |
| Association between Type of 2016 Healthcare Expenditures ($1000s) and 2017 Food Insecurity Status | ||||
|---|---|---|---|---|
| Emergency Department | Outpatient | Inpatient | Prescription | Out‐of‐Pocket |
| Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) |
| 1.01 (0.96, 1.07) | 1.01 (0.99, 1.03) | 1.001 (0.995, 1.008) | 1.02 (1.01, 1.03) | 1.03 (0.99, 1.06) |
Health care expenditures reported in 2017 USD
Adjusted for age, sex, income level, health insurance status, education level, race, and total health care expenditures in 2016.
Adjusted for age, sex, income level, health insurance status, education level, race, and food insecurity status in 2016
When examining associations in subpopulations stratified by comorbidities, wide confidence intervals owing to smaller sample sizes prevented definitive conclusions from being drawn (Table 4). The magnitude of the association between food insecurity and having any health care expenditures (1st part of the model) was greater among those with comorbidities compared to the overall population. The magnitude of the association between food insecurity and expenditures among those who had any expenditures (2nd part of the model) was similar to or slightly smaller among those with comorbidities compared to the overall population. Estimated expenditures within all subpopulations are presented in Appendix S1: Table S4.
TABLE 4.
Bidirectional association between food insecurity and health care expenditures by medical condition
| Association between food insecurity in 2016 and total health care expenditures in 2017 | |||
|---|---|---|---|
| Medical condition a | Food security status | Adjusted b odds ratio of nonzero expenditures (95% CI) | Adjusted b ratio of expenditures from GLM (95% CI) |
| Hypertension | Food insecure | 1.336 (0.831, 2.147) | 1.191 (0.942, 1.505) |
| Food secure | Referent | Referent | |
| COPD | Food insecure | 2.196 (0.568, 8.484) | 1.063 (0.839, 1.347) |
| Food secure | Referent | Referent | |
| Arthritis | Food insecure | 1.579 (0.84, 2.967) | 1.169 (0.916, 1.492) |
| Food secure | Referent | Referent | |
| Stroke | Food insecure | 3.369 (0.768, 14.791) | 0.919 (0.622, 1.358) |
| Food secure | Referent | Referent | |
| Diabetes | Food insecure | 1.115 (0.389, 3.191) | 1.145 (0.917, 1.431) |
| Food secure | Referent | Referent | |
| Association between total health care expenditures in 2016 and food insecurity status in 2017 | ||||
|---|---|---|---|---|
| Hypertension | COPD | Arthritis | Stroke | Diabetes |
| Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) | Adjusted c Odds Ratio (95% CI) |
| 1.009 (1.002, 1.02) | 1.001 (0.99, 1.02) | 1.01 (0.999, 1.02) | 0.998 (0.98, 1.01) | 1.01 (1.001, 1.02) |
Individuals were included in the restricted population if they had at least the appropriate condition. Those with multiple chronic conditions were present in multiple subgroups.
Adjusted for age, sex, income level, health insurance status, education level, race, and total health care expenditures in 2016.
Adjusted for age, sex, income level, health insurance status, education level, race, and food insecurity status in 2016.
3.3. Exploratory analyses
To assess for the mechanisms by which the relationship between total health care expenditures in 2016 and food insecurity status in 2017 may exist, we analyzed three additional models, which further adjusted for the total number of inpatient days, medical status, and disability status. When adjusting our main analysis for medical debt, the association between 2016 health care expenditures and 2017 food insecurity status is qualitatively smaller than in the primary adjusted model (OR for health care expenditures: 1.006, 95% CI: 1.001 to 1.011) while medical debt is strongly associated with food insecurity (OR 1.66, 95% CI 1.24 to 2.22). Similarly, the association between health care expenditures and food insecurity is smaller when adjusting self‐reported disability (OR 1.003, 95% CI 0.998 to 1.009), and disability status is strongly associated with food insecurity (OR 1.92, 95% CI 1.51 to 2.44).
3.4. Sensitivity analyses
Analyses examining the relationship between food insecurity as exposure and health care expenditures as outcome were not substantively changed by using alternative distributions (Appendix S1: Table S1). Different winsorizing thresholds did not meaningfully change results (Appendix S1: Table S5). When expressing 2016 health care expenditures as a categorical variable, the association between 2016 food insecurity and the presence of any 2017 health care expenditures was weaker than in the main analyses, but the association between 2016 food insecurity and 2017 total health care expenditures among those who had any expenditures was similar (Appendix S1: Table S6). Adjusting for both 2016 and 2017 health insurance did not affect the results.
4. DISCUSSION
In this study of nationally representative data, we found support for both directions of the relationship between food insecurity and healthcare expenditures—food insecurity is associated with greater health care expenditures, and greater health care expenditures are associated with food insecurity. However, the strength of these associations appears to be unequal. Though we found a statistically significant association between health care expenditures and subsequent food insecurity, the difference in odds () was small—about 1% greater risk of food insecurity per $1000 difference in health care expenditures. When examining the association between food insecurity and subsequent health care expenditures, the difference in expenditures between food insecure and food secure participants was relatively larger—approximately 25% greater expenditures for those who were food insecure. This suggests that upstream efforts that seek to address food insecurity may have greater impact than downstream efforts that seek to address health care expenditures directly.
Expenditures for prescriptions made up the largest share of the difference in health care spending between those who were food insecure and those who were food secure. Furthermore, with regard to the relationship between health care expenditures (as predictor) and food insecurity status (as outcome), we found evidence that greater health care expenditures may be an indicator of underlying poor health status. In models that adjusted for both indicator health care expenditures and indicators of poor health (eg, disability) the association between health care expenditures (as predictor) and food insecurity status (as outcome) was weakened, while the association between disability and subsequent food insecurity was strong. This suggests that high health care expenditures may be associated with food insecurity risk because they indicate poor health (which can impair the ability to work), rather than because they drain household resources directly. The finding that out‐of‐pocket expenditures is not associated with food insecurity risk also supports this idea.
The results of this study align with estimates calculated from prior studies on the association between food insecurity and health care expenditures. A cross‐sectional study using Canadian data from 2005 to 2010 estimated that having severe food insecurity was associated with 121% more health care expenditures, with roughly half of this association driven by prescription drugs. 14 Using food insecurity assessed prior to MEPS participation, a study analyzing 2012‐2013 data estimated that food insecurity was associated with an additional $1863 in total health care expenditures, but this study was limited by only assessing food insecurity at one time point and not having food insecurity assessment be contemporaneous with health care expenditure assessment. 12 Prior cross‐sectional studies have also shown a relationship between the presence of disability or chronic disease and food insecurity. 5 , 21 , 22 A prior study conducted using data from the Panel Study of Income Dynamics found that reported medical debt was associated more than twice the odds (OR: 2.04) of household food insecurity (even after accounting for key socioeconomic variables). 23
The results of this study have several implications. First, the confluence of comorbidities, health care expenditures, and food insecurity suggests that attempting to address food insecurity without paying attention to comorbidity could limit the effectiveness of the intervention. Rather than viewing food insecurity as one standalone issue to address, it may be more effective to think of addressing food insecurity as one aspect of a more comprehensive disease management plan. Relatedly, given that the strength of the association appears larger when food insecurity is the predictor and greater health care expenditures is the outcome (compared with when these roles are reversed), disease management plans, which target the upstream determinants of food insecurity and general poor health, may be more efficacious at breaking this cycle than interventions that merely offset the cost of disease management. Thirdly, the category of prescription expenditures stands out in our analyses. One reason for this may be that if food insecurity increases the risk for the development or worsening of chronic conditions, it could lead to increasingly complicated medication regimens, with attendant costs. 3 Finally, the lack of association between out‐of‐pocket expenditures and food insecurity, coupled with a strong association between medical debt and food insecurity, warrants closer attention. Current insurance benefit design often considers out‐of‐pocket expenditures (eg, yearly out‐of‐pocket maximums set at an absolute number) without considering medical debt. More nuanced design that takes into account an individual's ability to match resources to expenditures (eg, yearly out‐of‐pocket maximums set as a percentage of income or assets) may better protect individuals from the consequences of out‐of‐pocket costs.
The results of this study should be interpreted in light of several limitations. This study is observational, and unmeasured factors could confound the associations seen. Though the longitudinal design provides protection against unmeasured time‐invariant factors, we cannot exclude the possible role of unmeasured time‐varying factors. Next, the disability indicator used is a very blunt indicator of health status. Sample size did not permit more granular investigations (eg, of specific disabilities), but this is an important direction for future work. Similarly, small sample sizes increased the uncertainty of estimates conducted in chronic disease subgroups. Third, the two‐year time frame of this study is too short to permit investigation of some relevant pathways. For example, a key mechanism through which food insecurity may increase health care expenditures is through greater incidence of expensive chronic conditions, such as diabetes. However, as the annual incidence of diabetes is very low compared with its prevalence, we were unable to investigate that potential pathway in this study. These limitations, however, are balanced by several strengths. Data came from a large, nationally representative survey that used validated methods to assess food insecurity and health care expenditures. The longitudinal design allowed us to establish the time ordering of exposures and outcomes, and in sensitivity analyses, results were robust to alternative specifications and modeling strategies.
In this longitudinal study of nationally representative MEPS data, we found that food insecurity was associated with higher subsequent health care expenditures and that health care expenditures were associated with greater risk for subsequent food insecurity. However, these two associations appeared to be of different strengths. The association from health care expenditures to subsequent food insecurity showed a 1% difference in odds per $1000 difference in health care expenditures, but the association between food insecurity and subsequent health care expenditures showed 25% greater health care expenditures for those who were food insecure, compared with food secure. The presence of these relationships sets up the potential for a self‐reinforcing “vicious cycle” whereby food insecurity worsens health and worse health increases the risk for food insecurity. Given the different directional associations, however, interventions targeted at addressing food insecurity as a part of chronic disease management may be a more promising way to break this cycle and improve health for disadvantaged individuals.
AUTHOR CONTRIBUTION
KTJ and SAB conceived of the study and drafted the manuscript. DP, SB, and HKS contributed to interpretation and revised the manuscript critically for important intellectual content. All authors give approval of the manuscript version to be submitted.
Supporting information
Supplementary Material
Appendix S1
ACKNOWLEDGMENTS
Joint Acknowledgement/Disclosure Statement: Disclosures: SAB reports receiving personal fees from the Aspen Institute, outside the submitted work. All other authors report nothing to disclose.
Johnson KT, Palakshappa D, Basu S, Seligman H, Berkowitz SA. Examining the bidirectional relationship between food insecurity and healthcare spending. Health Serv Res. 2021;56:864–873. 10.1111/1475-6773.13641
Funding information
Funding for SAB's and HKS's role on the study was provided by the National Institute of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health under Award Numbers K23DK109200 and P30DK092924 respectively. DP is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number K23HL146902. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- 1. Coleman‐Jensen A, Rabbitt MP, Gregory CA, Singh A. Household Food Security in the United States in 2018. Published September 4, 2019. http://www.ers.usda.gov/publications/pub‐details/?pubid=94848. Accessed April 16, 2020.
- 2. Fitzpatrick KM, Harris C, Drawve G. Assessing Food Insecurity in the United States During COVID‐19 Pandemic. Published online April 1, 2020. https://fulbright.uark.edu/departments/sociology/research‐centers/community‐family‐institute/_resources/community‐and‐family‐institute/revised‐assessing‐food‐insecurity‐brief.pdf. Accessed May 29, 2020
- 3. Seligman HK, Schillinger D. Hunger and socioeconomic disparities in chronic disease. N Engl J Med. 2010;363(1):6‐9. 10.1056/NEJMp1000072 [DOI] [PubMed] [Google Scholar]
- 4. Seligman HK, Bindman AB, Vittinghoff E, Kanaya AM, Kushel MB. Food insecurity is associated with diabetes mellitus: results from the National Health Examination and Nutrition Examination Survey (NHANES) 1999–2002. J Gen Intern Med. 2007;22(7):1018‐1023. 10.1007/s11606-007-0192-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Seligman HK, Laraia BA, Kushel MB. Food insecurity is associated with chronic disease among low‐income NHANES participants. J Nutr. 2010;140(2):304‐310. 10.3945/jn.109.112573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Berkowitz SA, Berkowitz TSZ, Meigs JB, Wexler DJ. Trends in food insecurity for adults with cardiometabolic disease in the United States: 2005–2012. PLoS One. 2017;12(6):e0179172. 10.1371/journal.pone.0179172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gundersen C, Ziliak JP. Food Insecurity And Health Outcomes. Health Aff Proj Hope. 2015;34(11):1830‐1839. 10.1377/hlthaff.2015.0645 [DOI] [PubMed] [Google Scholar]
- 8. Crews DC, Kuczmarski MF, Grubbs V, et al. Effect of food insecurity on chronic kidney disease in lower‐income Americans. Am J Nephrol. 2014;39(1):27‐35. 10.1159/000357595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Seligman HK, Berkowitz SA. Aligning programs and policies to support food security and public health goals in the United States. Annu Rev Public Health. 2019;40:319‐337. 10.1146/annurev-publhealth-040218-044132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berkowitz SA, Seligman HK, Choudhry NK. Treat or eat: food insecurity, cost‐related medication underuse, and unmet needs. Am J Med. 2014;127(4):303‐310.e3. 10.1016/j.amjmed.2014.01.002 [DOI] [PubMed] [Google Scholar]
- 11. Orr CJ, Keyserling TC, Ammerman AS, Berkowitz SA. Diet quality trends among adults with diabetes by socioeconomic status in the U.S.: 1999–2014. BMC Endocr Disord. 2019;19(1):54. 10.1186/s12902-019-0382-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Berkowitz SA, Basu S, Meigs JB, Seligman HK. Food Insecurity and Health Care Expenditures in the United States, 2011‐2013. Health Serv Res. 2018;53(3):1600‐1620. 10.1111/1475-6773.12730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Berkowitz SA, Seligman HK, Meigs JB, Basu S. Food insecurity, healthcare utilization, and high cost: a longitudinal cohort study. Am J Manag Care. 2018;24(9):399‐404. [PMC free article] [PubMed] [Google Scholar]
- 14. Tarasuk V, Cheng J, de Oliveira C, Dachner N, Gundersen C, Kurdyak P. Association between household food insecurity and annual health care costs. CMAJ. 2015;187(14):E429‐E436. 10.1503/cmaj.150234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Garcia SP, Haddix A, Barnett K. Incremental health care costs associated with food insecurity and chronic conditions among older adults. Prev Chronic Dis. 2018;15:E108. 10.5888/pcd15.180058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berkowitz SA, Basu S, Gundersen C, Seligman HK. State‐level and county‐level estimates of health care costs associated with food insecurity. Prev Chronic Dis. 2019;16:E90. 10.5888/pcd16.180549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities‐addressing social needs through medicare and medicaid. N Engl J Med. 2016;374(1):8‐11. 10.1056/NEJMp1512532 [DOI] [PubMed] [Google Scholar]
- 18. Verma S. CMS Approves North Carolina’s Innovative Medicaid Demonstration To Help Improve Health Outcomes. Published October 1, 2018. https://www.healthaffairs.org/do/10.1377/hblog20181024.406020/full/. Accessed October 30, 2018
- 19. AHRQ . Medical Expenditure Panel Survey Home. Published June 26, 2020. https://meps.ahrq.gov/mepsweb/. Accessed June 26, 2020
- 20. United States Department of Agriculture Economic Research Service . Food Security Survey Module. https://www.ers.usda.gov/topics/food‐nutrition‐assistance/food‐security‐in‐the‐us/survey‐tools/. Accessed January 17, 2018
- 21. Laraia BA. Food insecurity and chronic disease. Adv Nutr. 2013;4(2):203‐212. 10.3945/an.112.003277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Coleman‐Jensen A, Nord M. Food Insecurity Among Households With Working‐Age Adults With Disabilities. Published January 2013. http://www.ers.usda.gov/publications/pub‐details/?pubid=45040. Accessed June 26, 2020
- 23. Brewer M. Household debt and children’s risk of food insecurity. Soc Probl. 2020;67(3):565‐584. 10.1093/socpro/spz027 [DOI] [Google Scholar]
- 24. Manning WG, Mullahy J. Estimating log models: to transform or not to transform? J Health Econ. 2001;20(4):461‐494. [DOI] [PubMed] [Google Scholar]
- 25. Belotti F, Deb P, Manning WG, Norton EC. Twopm: two‐part models. Stata J Promot Commun Stat Stata. 2015;15(1):3‐20. 10.1177/1536867X1501500102 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material
Appendix S1


