Abstract
A woman in her 30s with underlying Graves’ disease, who recently completed radioactive iodine treatment, presented with 2 weeks of acutely altered behaviour associated with auditory hallucinations and religious preoccupations. Laboratory investigation demonstrated elevated free thyroxine levels and suppressed thyroid-stimulating hormone levels. Additionally, there was a presence of antithyroid peroxidase antibodies consistent with autoimmune thyroid disease. She responded to antipsychotics and achieved biochemical euthyroidism. Subsequently, antipsychotic was tapered off during outpatient follow-up at the patient’s own request, with supplement thyroxine continuing. After 1 week, acute hallucinations and religious preoccupations re-emerged, driving her to inflict self-injuries by swallowing coins and nails and banging her head against the wall, sustaining laceration wounds. Furthermore, she hammered a roofing nail into the external genitalia, embedded in the symphysis pubis. After supplemental thyroxine was stopped and olanzapine was started, she achieved biochemical euthyroid followed by remission of psychosis within 1 week. This case illustrates the importance of elucidating organic causes of psychosis as they are easily and swiftly reversible.
Keywords: thyroid disease, psychotic disorders (incl schizophrenia), suicide (psychiatry), vulvovaginal disorders, general surgery
Background
Individuals who have acute psychosis may pose a risk of violence towards themselves and others. A substantial proportion of patients with first-episode psychosis report suicide attempts or deliberate self-harm (DSH) before presenting for treatment. In a meta-analysis,1 the data suggest that positive symptoms are unrelated to DSH before or after treatment for first-episode psychosis. The presence of depression and substance use in early psychosis are more associated with DSH. The other associated factors included the young age of psychosis onset, duration of untreated psychosis and suicidal ideas that could precipitate the DSH.
Generally, the DSH can present various forms of tissue injuries and rarely as genital self-mutilation (GSM). GSM has been well described in males but is rarely reported in females.2 It is also a severe type of self-injurious behaviour usually observed among patients with command hallucination, delusions and distorted body image.3 At the same time, the presentation with unusual and florid psychiatric symptoms in an acute fashion without a particular prodromal period should prompt clinicians to perform a thorough search for alternative organic presentations.
Hyperthyroidism may associate with emotional lability, easily anxiety and irritability. In extreme cases, they may have psychiatric symptoms of hallucinations and delusions. A clear association between hyperthyroidism and attempted or completed suicide has not been previously shown.4 5 The literature review is sparse and there is a case reported by Petrich et al6 regarding attempts to suicide due to hyperthyroidism. The case illustrated a 24-year-old woman who presented with a week history of a mood swing, palpitation and insomnia, had ingested 100 tablets of paracetamol and was admitted to Intensive Care Unit (ICU) for anticipation of severe liver damage. The thyroid function test revealed high T4 and low thyroid stimulating hormones (TSH), followed by anti-thyroid peroxidase (anti-TPO) antibodies consistent with the diagnosis of Graves’ disease. The anxiety and suicidal thoughts resolved, followed by initiation of acute treatment in the first few weeks. Usually, there is the biopsychosocial interplay between thyroid disorder and psychiatric manifestation, leading to self-harm behaviour or suicide. Despite hyperthyroid symptoms usually resolved with antithyroid therapy, there are long-standing neuropsychiatric symptoms following hyperthyroidism shown in those under regular treatment.7 8 We present an interesting case of hyperthyroidism and acute psychosis, complicated with uncommon GSM and multiple foreign body ingestion.
Case presentation
A woman in her 30s was brought to the emergency department with 2 weeks of altered behaviour and had physical violence towards the family members. She seemed more preoccupied religiously than usual manner, talked about God and day of judgement repetitively and prayed throughout the day. She also stated that the faint voices were talking to her, which she perceived as God’s voices. But she was not sure about the content of hallucinatory voices. There was disorganised behaviour witnessed by the caregiver, as the patient would crawl on the floor while reciting holy texts inappropriately. A day before visiting the emergency department, the patient had an episode of violent behaviour at home, she kicked and hit her father and husband several times and shouted in irrelevant speech. For safety reason, the attending doctor had to admit her for stabilisation and acute treatment. Throughout hospitalisation, she was initiated on olanzapine 20 mg daily and attained symptomatic remission within a week. After being discharged from the ward, she came for regular outpatient follow-up and appeared calmer than before, with no obvious psychotic symptoms.
The olanzapine was gradually tapered off over 2 weeks by the treating doctors on patient’s request due to her wish to avoid side effects; at that time, she was not compliant to her concurrently prescribed thyroxine. This led to similar psychotic symptoms recurring over a week, as the patient started hearing multiple God-like voices throughout the day and disturbed her sleep. The voices occurred involuntarily and distracted her from doing the household chores at home. The husband reported that his wife appeared to be more anxious than before, reluctant to talk and seemed suspicious. Before the current hospitalisation, she had excessive fears and worries about being sinful to God and asked for a divorce from her husband impulsively. Husband tried to console her and she seemed indifferent to the family members. At midnight, the patient developed sudden, intense, unpleasant feelings of distress and was overwhelmed by sinful thoughts of God. Hence, she started to bang her head against a brick wall repetitively and sustained head wounds with bleeding. Subsequently, she swallowed a bent nail and a few coins in the bedroom without hesitancy. The self-injury behaviour was further perpetuated when she held a wood-made shoe and hammered a silver roof nail passed through her right external genitalia. These actions were under her voluntary will, without interference from external forces or commanding hallucination. There was no history suggestive of delusions or dissociative states. After that, her husband found out about the incident and brought her to the hospital for immediate treatment.
There was no significant psychiatric history.
She has underlying hyperthyroidism for 8 years and was subsequently diagnosed with Graves’ disease in the medical history. The endocrine team initiated treatment, primarily tablet carbimazole and tablet propranolol. Despite adequate oral treatment, her hyperthyroid symptoms persisted, such as easily anxiety, irregular menstrual cycles and tremors. The thyroid function tests demonstrated a significant hyperthyroid state with low TSH and high free T4. Eventually, the patient agreed to the radioactive iodine therapy and completed the therapy 6 months later. She went into a hypothyroid state as evidenced by high TSH followed by low free T4. Hence, she was prescribed with tablet thyroxine 75 mcg daily. However, inadequate family supervision caused the patient to consume more thyroid tablets (up to five tablets a day) on most days.
There was no significant surgical history.
There was no family history of mental illness. For the part of personal history, she was married for 5 years and had no children. There was no previous history of pregnancy or postpartum related psychiatric symptoms ever. There was no significant history of illicit substance use.
The physical examination revealed that she was conscious and alert, with blood pressure, pulse rate and temperature within normal ranges. Mental state examination revealed a young woman of average build and proper hygiene, guarded, had poor eye contact and not forthcoming to the interviewer. She spoke in the Malay language coherently and relevantly, mostly spoke in short sentences and minimal amount, low tone and volume. She described her mood as sad, whereas her affect appeared restricted and incongruent to thoughts. She denied having perceptual disturbances or delusions. It was clinically visible that she was mumbling to herself. She was oriented to time, place and person but cognitively had insufficient attention and concentration. The overall judgement and insight were poor towards her current state of condition.
The following genital examination by gynaecologists revealed that a roofing nail had punctured her right labia superior medially and was embedded into her symphysis pubis.
Investigations
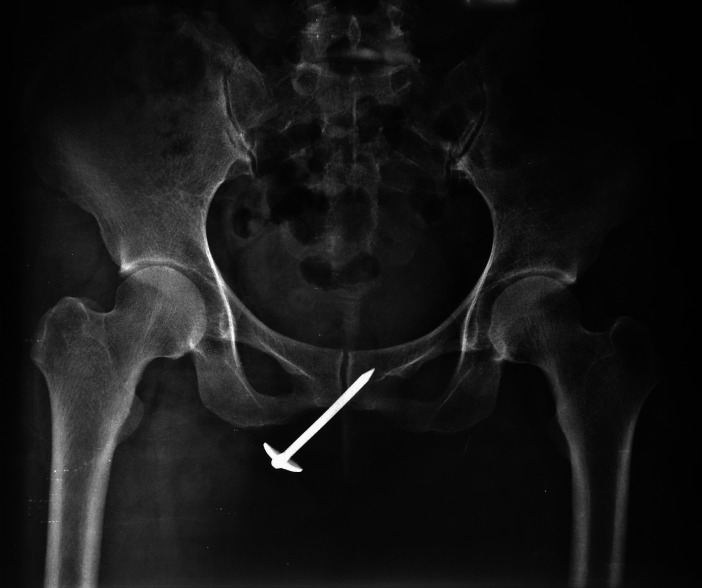
Complete blood count reported as normal. In addition, kidney function and liver function tests were within normal limits. Two X-rays were performed, with figure 1 demonstrating an X-ray of the abdomen showing a bent nail measured 50 mm located over the transverse colon, with multiple coins seen over the ascending colon. The second X-ray, as per figure 2, was an X-ray of the pelvis which showed a roofing nail measuring 50 mm embedded over the symphysis pubis.
Figure 1.
X-ray of the abdomen shows a bent nail measured 50 mm located over the transverse colon, with multiple coins seen over the ascending colon.
Figure 2.
X-ray of the pelvis shows a roofing nail measuring 50 mm embedded over the symphysis pubis.
The thyroid function tests revealed hyperthyroidism as evidence by low TSH (<0.01 μlU/mL) followed by high free T4 (26.51 pmol/L). Serology tests showed elevated anti-TPO: >1000 IU/mL (reference range <34 IU/mL) and normal level of antithyroglobulin: <0.1 μg/L (reference range <78 μg/L).
A complete autoimmune workup was carried out to exclude the possibility of autoimmune encephalitis conclusively. The indirect immunofluorescent antibody test of autoimmune encephalitis revealed negative results for the following encephalitis receptors in the patient’s cerebral spinal fluid: N-methyl-D-aspartate receptor antibody, gamma-aminobutyric acid receptor antibody, leucine-rich glioma-inactivated protein 1 antibody, contactin-associated protein 2 antibody and dipeptidyl aminopeptidase-like protein antibody.
Cerebrospinal fluid (CSF) analysis revealed clear and colourless CSF on appearance, with the normal CSF glucose and CSF protein levels. In addition, white cell count, neutrophils and lymphocytes were not present in the CSF.
Electroencephalography (EEG) demonstrated that the background consisted of theta rhythms at 5–6 cps, with intermittent generalised, frontal maximal delta slowing with superimposed fast activities. No epileptiform discharge was seen. Overall, the EEG showed mild encephalopathic changes. CT scan of the brain revealed no significant abnormalities.
Differential diagnosis
According to Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM-5), the possible working diagnosis would be psychotic disorder due to another medical condition: hyperthyroidism with a specifier of predominant hallucinations. The point to support hyperthyroidism included noticeable mood changes with easily anxious and uneasy, due to excessive ingestion of thyroid supplement. However, there were no physical symptoms of hyperthyroidism such as weight loss, heat intolerance, amenorrhea or diarrhoea. There are several aspects of clinical symptoms that suggest that the psychosis leans towards organic, in origin, instead of functional causes, such as acute and rapid symptom progression and a background history of thyroid dysfunctions. Throughout the years, there were significant chronic thyroid dysfunctions with recent radioactive iodine treatment followed by excessive supplementary thyroxine consumption. Moreover, the longitudinal history demonstrated a clear temporal relationship between thyroid dysfunction and acute onset of psychiatric symptoms. Despite being given a high dose of antipsychotics during the first hospitalisation, her psychotic symptoms did not remit satisfactorily and recurred.
One of the differential diagnosis is an autoimmune-related disease, specifically Hashimoto thyroiditis. It is frequently associated with autoimmune encephalitis that may give rise to similar episodes of acute psychosis. The point to support Hashimoto’s encephalopathy is that the EEG finding demonstrated slow delta wave background activity. The presence of slow waves on the EEG may indicate some level of encephalopathy changes. However, there was no clinical evidence of hypothyroidism that could be part of Hashimoto’s thyroiditis. The CSF analysis showed an average protein level, suggesting a low probability of active inflammation processes. Another diagnostic possibility related to hyperthyroidism could be that symptoms were due to active consumption of thyroxine supplement. This patient had a history of excessive thyroxine ingestion, which might have precipitated and perpetuated the hyperthyroid condition. Once potential organic causes were ruled out, only the acute psychotic episode could be evaluated as functional psychosis in origin or brief psychotic disorder. The point to support this differential diagnosis is that predominant auditory hallucination lasted for at least 1 day and less than 1-month duration. Plus, the psychotic symptoms relapsed once tablet olanzapine taper off within 2 weeks of the first presentation.
Treatment
Emergency OGDS was performed for therapeutic purposes to visualise and remove the ingested foreign body. The procedure was done under light sedation with midazolam. The finding of oesophagogastroduodenoscopy (OGDS) revealing some gastric erosions and no foreign body was seen in the stomach region. So, no apparent foreign body was removed throughout the procedure.
Next, the patient was sent to the operation theatre for examination under anaesthesia, mainly to remove foreign bodies in the vulva, wound debridement and washout procedures. Intraoperatively, 50 mm length of silver roof nail was entirely removed from the soft tissue of the right vulva with minimal blood loss. After the procedure, she received a short duration of prophylactic antibiotics: intravenous metronidazole 500 mg three times a day and intravenous cefuroxime 1.5 g three times a day. The psychotic symptoms were treated with tablet olanzapine 10 mg two times per day. In addition, tablet diazepam 5 mg was prescribed as necessary for chemical tranquillisation. The thyroxine was withheld because of significant hyperthyroidism symptoms, namely anxiety, palpitation and irregular menses. Repeated thyroid function tests were within normal ranges. Subsequently, she appeared less anxious in the following week and psychotic symptoms were reduced significantly.
Outcome and follow-up
The patient improved tremendously after tablet thyroxine was withheld in the ward for 5 days, followed by complete resolution of psychosis in the following week. She was prescribed with a regular dose of tablet olanzapine 10 mg two times per day on discharge from the hospital. A week later, she had no more psychotic symptoms at her follow-up visit and was maintaining relatively well at home. She was also referred for further longitudinal endocrine assessment and evaluation due to fluctuating thyroid function tests. The subsequent psychiatric outpatient visit in 2 weeks shows the patient improved satisfactorily. There were no more psychotic symptoms and her mood was relatively calm. Therefore, the tablet olanzapine was reduced to 5 mg daily.
Discussion
This case ties in multiple thyroid-related aetiologies of acute psychosis, be it the thyroid dysfunction per se, the medications or the radioiodine treatments. Leading causes of hyperthyroidism include Graves’ disease, toxic multinodular goitre and toxic adenomas. Sometimes, however, hyperthyroidism can be due to ingestion of an excessive amount of thyroid hormone or secretion of thyroid hormone from an ectopic site. The hyperthyroid state can present various psychological symptoms, including anxiety, emotional lability, dysphoria and mania.9 Other neuropsychiatric symptoms of Graves’ disease include irritability, depression and insomnia.10 In addition, the depressed patients seem to have altered TSH response to thyrotropin-releasing hormone (TRH), which may associate with a greater risk of suicide.11 The thyroid hormones play essential roles among mood modulating neurotransmitter alike serotonin system, which may explain the association with mood symptoms and possible DSH.12 Acute psychosis is a rare clinical presentation of hyperthyroidism, present in as low as 1% of patients in a hyperthyroid state.13
Examining thyroid aetiologies that are not purely endocrine in origin, another differential diagnosis under suspicion in this case is an uncommon autoimmune thyroiditis related condition known as Hashimoto’s encephalopathy. The classical presentation encompasses altered consciousness, acute psychosis, seizure and focal neurological deficits. Most cases are, however, euthyroid but can be mildly hypothyroid or even hyperthyroid.14 The suspicion index is correspondingly higher in a young person presenting in a delirious state with florid psychotic symptoms associated with deranged thyroid function tests. In that case, the clinician can consider further autoimmune workups, especially serum antithyroid antibodies, which are classically elevated. The exact cause is unknown but is believed to be immune-mediated and closely related to Hashimoto’s thyroiditis. The course of the disease can be remitting and relapsing over time and is generally responsive to steroid treatment. This patient’s biochemical test shows a high level of antithyroid antibodies, followed by clear evidence of slow-wave activity in EEG. Despite such features suggestive of Hashimoto’s encephalopathy, this patient remitted within a short period without steroid administration, which could be related to tablet thyroxine cessation.
This case presents a few exciting and crucial take-home messages. First, it is rare that an isolated psychotic episode can be part of hyperthyroidism, as it is usually correlated with mood symptoms. The case was further complicated by the multiple self-injuries culminating in GSM. There are limited case reports in the literature with similar findings. Although most reported cases of female genital mutilation involve self-induced abortions or insertion of a foreign body, one report describes a female who masturbated with a pair of scissors.15 The presence of high thyroid autoantibodies level is associated with autoimmune-mediated thyroid disease. That may give rise to the suspicion of autoimmune encephalitis, which can be manifested as acute psychosis clinically. Third, this woman had florid psychotic symptoms and unusually DSH, hammering a roofing nail into her genitalia. In similar case reports, most psychotic patients with GSM are commonly male, in the form of self-castration. However, she did not suffer from psychotic symptoms despite being in hyperthyroid state for nearly 8 years. She only experienced psychosis only after she had hyperthyroidism due to thyroxine overdose. There are hence most probably other unknown issues that could have contributed to the pathogenesis of psychosis.
Intentional self-mutilation is defined as deliberate and direct physical self-injury, mostly occurring in a state of cultural or psychopathological background. The DSH primarily involves substantial tissue injury in other body parts and rarely involves GSM. Patients with genital mutilation usually can be categorised into four types: psychotic patients with delusions of genitalia, patients with severe personality disorder, transsexuals with self-sexual reassignment and people whose mutilation reflects religious or cultural beliefs.16 Although GSM among females is typically reported in the form of foreign body insertion or cutting method, the use of nail hammered into the genitalia parts in this report may suggest more atypical and unique psychopathology, which may warrant more attention and clinical evaluation. Further, intentional GSM can be traumatising to the victim and caregiver, usually encountered among patients with severe mental illness. Unfortunately, cases of GSM are under-reported, so the prevalence of GSM is challenging to estimate.
One of the few early cases documented in the literature involved a man performing GSM by autocastration, who believed that his sexual organ’s presence caused the failure in his life.17 Another case study of female GSM with underlying schizophrenia was reported,18 where the patient used a razor blade to cut through her labia majora complicated with excessive bleed. She believed that her genitalia had enlarged because of masturbation and she was determined to cut-off her clitoris as the primary source of distress. Such self-mutilation behaviour may be partially interpreted as a result of delusional ideas of genitalia premorbid with body-image preoccupation, forced early sexual activity and hence profound ambivalence towards adult sexuality.
A recent systematic review of identifying potential psychiatric issues and psychosocial factors among males with intentional GSM results demonstrated that about half of patients with GSM had schizophrenia, followed by substance use (18.5%) and personality disorders (15.9%).19 When assessing a patient with GSM, the clinician must consider the root cause of GSM, whether it involves sociocultural beliefs, delusional thoughts or primarily due to underlying mental illness. Looking into our case, the patient had intentional GSM, multiple laceration wounds over her scalp and attempted to swallow nails and coins simultaneously. Although suicidal ideation and intention are infrequently associated with GSM, we still need to perform a thorough suicidal risk assessment, especially of psychopathology, including auditory hallucination, religious theme of delusions and pathological guilt preoccupations.
Patient’s perspective.
I do not know what I was doing and why I harmed myself in such a way, only God knows. But I really feel like I had taken too much of my thyroid tablets earlier and I am afraid of taking the olanzapine tablets now because of the side effects.
Learning points.
Thyroid-related disorders have broad neuropsychiatric manifestations ranging from mild anxiety and depression to rarely as psychosis.
Early recognition of organic psychosis and effective treatment can minimise unnecessary harm and adverse complications of psychotic symptoms.
Genital self-mutilation is less common in females than males, requiring a multidisciplinary approach and comprehensive risk assessment, especially in acutely psychotic individuals.
Footnotes
Contributors: HHW contributed to conceptualising and authorship. NTPP contributed to editing and proofreading.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Challis S, Nielssen O, Harris A, et al. Systematic meta-analysis of the risk factors for deliberate self-harm before and after treatment for first-episode psychosis. Acta Psychiatr Scand 2013;127:442–54. 10.1111/acps.12074 [DOI] [PubMed] [Google Scholar]
- 2.Greilsheimer H, Groves JE. Male genital self-mutilation. Arch Gen Psychiatry 1979;36:441–6. 10.1001/archpsyc.1979.01780040083009 [DOI] [PubMed] [Google Scholar]
- 3.Favazza AR, Rosenthal RJ. Diagnostic issues in self-mutilation. Hosp Community Psychiatry 1993;44:134–40. 10.1176/ps.44.2.134 [DOI] [PubMed] [Google Scholar]
- 4.Drummond L, Lodrick M, Hallstrom C. Thyroid abnormalities and violent suicide. Br J Psychiatry 1984;144:213. 10.1192/S0007125000202080 [DOI] [PubMed] [Google Scholar]
- 5.Abraham-Nordling M, Lönn S, Wallin G, et al. Hyperthyroidism and suicide: a retrospective cohort study in Sweden. Eur J Endocrinol 2009;160:437–41. 10.1530/EJE-08-0749 [DOI] [PubMed] [Google Scholar]
- 6.Petrich CE, Bui MP, Farrell HM. A case of a suicide attempt associated with hyperthyroidism. Gen Hosp Psychiatry 2013;35:576.e9. 10.1016/j.genhosppsych.2012.12.006 [DOI] [PubMed] [Google Scholar]
- 7.Bunevicius R, Velickiene D, Prange AJ. Mood and anxiety disorders in women with treated hyperthyroidism and ophthalmopathy caused by Graves' disease. Gen Hosp Psychiatry 2005;27:133–9. 10.1016/j.genhosppsych.2004.10.002 [DOI] [PubMed] [Google Scholar]
- 8.Trzepacz PT, McCue M, Klein I, et al. A psychiatric and neuropsychological study of patients with untreated Graves' disease. Gen Hosp Psychiatry 1988;10:49–55. 10.1016/0163-8343(88)90084-9 [DOI] [PubMed] [Google Scholar]
- 9.Feldman AZ, Shrestha RT, Hennessey JV. Neuropsychiatric manifestations of thyroid disease. Endocrinol Metab Clin North Am 2013;42:453–76. 10.1016/j.ecl.2013.05.005 [DOI] [PubMed] [Google Scholar]
- 10.Bunevicius R, Prange AJ. Psychiatric manifestations of Graves??? hyperthyroidism. CNS Drugs 2006;20:897–909. 10.2165/00023210-200620110-00003 [DOI] [PubMed] [Google Scholar]
- 11.Musselman DL, Nemeroff CB. Depression and endocrine disorders: focus on the thyroid and adrenal system. Br J Psychiatry Suppl 1996;168:123–8. 10.1192/S0007125000298504 [DOI] [PubMed] [Google Scholar]
- 12.Bauer M, Heinz A, Whybrow PC. Thyroid hormones, serotonin and mood: of synergy and significance in the adult brain. Mol Psychiatry 2002;7:140–56. 10.1038/sj.mp.4000963 [DOI] [PubMed] [Google Scholar]
- 13.Gagliardi JP, Clary GL. Treatment of thyrotoxicosis-induced psychosis. Psychopharmacol Bull 2002;36:7–13. [PubMed] [Google Scholar]
- 14.Montagna G, Imperiali M, Agazzi P, et al. Hashimoto's encephalopathy: a rare proteiform disorder. Autoimmun Rev 2016;15:466–76. 10.1016/j.autrev.2016.01.014 [DOI] [PubMed] [Google Scholar]
- 15.Favazza A. Masturbation or mutilation. Med Aspects Hum Sex 1991;25: :45–6. [Google Scholar]
- 16.Favazza AR. Bodies under siege: self-mutilation and body modification in culture and psychiatry. JHU Press, 1996. [Google Scholar]
- 17.Stroch D. Self-Castration. J Am Med Assoc 1901;XXXVI:270. 10.1001/jama.1901.02470040048018 [DOI] [Google Scholar]
- 18.Krasucki C, Kemp R, David A. A case study of female genital self-mutilation in schizophrenia. Br J Med Psychol 1995;68:179–86. 10.1111/j.2044-8341.1995.tb01824.x [DOI] [PubMed] [Google Scholar]
- 19.Veeder TA, Leo RJ. Male genital self-mutilation: a systematic review of psychiatric disorders and psychosocial factors. Gen Hosp Psychiatry 2017;44: :43–50. 10.1016/j.genhosppsych.2016.09.003 [DOI] [PubMed] [Google Scholar]