Abstract
Background: The COVID-19 pandemic provided a unique opportunity to explore the impact of the mandated lockdown and social distancing policies on engagement in daily occupations for individuals with multiple sclerosis (MS) and able bodied (i.e. healthy) adults. The study also examined whether the changes in daily occupations were associated with health-related quality of life (HrQOL).
Methods: Between the spring and early fall of 2020, 69 persons with MS and 95 healthy adults completed an online survey that included measurements of 26 activities of daily life. For each activity, participants reported whether they continued to perform the activity (with or without adjustments), whether they stopped, or started to perform the activity during the pandemic. Social support, HrQOL, and demographics, including financial distress were also obtained.
Results: Participants with MS and healthy adults both reduced the number of activities performed during the pandemic. Healthy adults continued to do more activities with and without adjustments compared with participants with MS. In both groups, better HrQOL was associated with the number of activities participants continued to do with and without adjustments, and worse HrQOL with the number of activities they stopped doing.
Conclusions: Fewer persons with MS engaged in everyday occupations than healthy adults following the COVID-19 pandemic. The ability to maintain occupational engagement and to participate in social and daily activities is important for maintaining high HrQOL in both groups. Thus, these results call for attention in treatment and self-management of MS symptomatology.
Keywords: Activities of daily living, Quality of life, Multiple sclerosis, Covid-19
Introduction
Since the outbreak of Coronavirus Disease 2019 (COVID-19) individuals throughout the world have had to make significant life adjustments, including leaving one's home only when absolutely necessary, social distancing, wearing of masks, and performing extensive hygiene protocol. These adjustments have affected occupations of daily living, which include activities associated with paid and unpaid work, self-care, leisure, and rest. However, engaging in occupations of daily life is crucial for one's sense of well-being and satisfaction with life (Steger et al., 2008). Therefore, restriction and adjustments associated with the COVID-19 pandemic may have impacted quality of life (QOL) and well-being.
Indeed, following pandemic restrictions, negative life changes were observed in various aspects of life – in healthcare, economics, social interactions, and everyday tasks for both persons with and without disabilities. For example, European healthy adults reported that they slept more, exercised and walked less, spent more time on electronic screens and devices, and gained more body mass during the pandemic (Pišot et al., 2020). Interestingly, the same study also reported some positive life changes, such as more regular and healthier meals, less alcohol consumption, and less smoking (Pisot 2020). Another study of 571 Israeli healthy adults reported high levels of psychological distress, significant reduction in participation in daily life activities, and decreased QOL (Lipskaya-Velikovsky, 2020). In addition, Szczepańska and Pietrzyka (2021) reported that young college age healthy people were negatively affected by the restrictions in the access to public spaces, which resulted in deteriorated physical and psychological well-being and overall QOL.
Negative life changes following the COVID-19 outbreak were also observed in people with disabilities. For example, people with intellectual and developmental disability experienced behavioral difficulties due to disruptions to routines and support systems (Courtenay, 2020). Umucu and Lee (2020) found that people with chronic illnesses reported a moderate level of stress, depression, and anxiety during the COVID-19 pandemic. In fact, Lund et al. (2020) reported that people with disabilities in the United States have been more exposed to various sources of stress and trauma during the COVID-19 pandemic compared to people without disabilities. These stressors included but were not limited to concerns about health care rationing and ableism in health care, isolation, and deaths and illnesses of loved ones and community members. In addition, many people with disabilities were already living with occupational restrictions that had a devastating impact on their health-related quality of life (HrQOL) even before the pandemic started. The pandemic further limited engagement in daily occupations due to confinement and various restrictions that were needed and required to keep them safe (Kendall et al., 2020). Interestingly, there is a lack of published research on the impact of the pandemic on daily occupations and participation in everyday activities for individuals with disabilities, including multiple sclerosis (MS).
MS affects up to a million people in the United States (Wallin et al., 2019) and often results in limitations and restrictions in occupations of daily living (Goverover et al., 2015, 2020) and a reduced HrQOL (Goverover et al., 2020). The challenges imposed by the pandemic may have had an additive negative effect on various aspects of life for individuals with MS. In contrast to healthy adults, individuals with MS have diagnosis-specific medical concerns and existing activity restrictions (Goverover et al., 2015, 2021). Nonetheless, some recent studies reported that the pandemic restrictions have worsened the sleep quality of persons with MS (Luis et al., 2021) and their quality of life (Manacorda et al., 2021). Additionally a study showed that approximately half of the study sample of persons with MS ceased or decreased their physical activity leisure time during the COVID-19 epidemic (Kalron et al., 2021).
In this current study, we explored how pandemic restrictions have affected daily occupations and whether these changes are related to current HrQOL of persons with multiple sclerosis (MS) compared to healthy adults. We hypothesized that individuals with MS and healthy adults would both experience changes in occupations of daily life due to general restrictions applied to everyone. However, healthy adults may make more efficient adjustments to be able to carry out these activities during the COVID-19 pandemic compared with persons with MS. Furthermore, we aimed to investigate whether engagement in occupations of daily life during the COVID-19 pandemic can predict participants’ current HrQOL above and beyond financial stress, social support, and resilience (known predictors of HrQOL). We hypothesized that individuals who continued to perform more occupations of daily life with and without adjustments would report better HrQOL than people who discontinued activities.
Material and methods
2.1. Participants
A total of 69 respondents with MS and 95 healthy adults (HAs) participated in this study. Table 1 summarizes participants’ demographic characteristics. The MS group was significantly older than the HA group F(1, 161) = 5.4, p = .02). The HA group reported more years of formal education than participants with MS (F(1, 161) = 3.2, p = .07). More HAs were employed compared to persons with MS (49.3% in MS vs. 63.1% in HA; χ2(1) = 5.1, p = .03) and reported higher household income than the MS group (median income: $50,000-$74,000 in MS vs. > $75,000 in HA; W = 3274.5, p = .003). Additionally, the HA households had more children under age 18 (F (1, 161) = 14.2; p <0.001) and included more people than those of the MS group (F(1, 161) = 4.9; p = .01). The MS sample consisted of predominantly relapsing-remitting phenotype (68%). Although a formal measure of disability was not utilized, the authors computed the patient determined disease steps (PDDS) score based on MS participants responses to questions related to their MS related symptoms and these symptoms impact on their life. Participants’ mean score on the PDDS was 3, indicating ”gait disability” (Hohol et al., 1995; Kahraman et al., 2021). 42% of participants in the HA group were tested for COVID-19, and from them only 2 participants (1.6%) were positive. In the MS group, 29% were tested for COVID-19, and 3 of them were found positive (4.3%). In terms of electronic use, both MS and HA groups reported frequent and regular smartphone or cellphone use and owned a desktop or laptop computer (including tablets). In both groups they reported access to high speed internet and frequent internet use.
Table 1.
Description of participants.
| MS (n = 69) | HA (n = 95) | p | |
| Age | 48.1 (13.17) | 42.9 (14.5) | .02 |
| Years of education | 18.6 (2.1) | 19.16 (1.8) | .07 |
| Sex | |||
| Males | 12 | 16 | >0.05 |
| Females | 56 | 79 | |
| Marital Status | |||
| Never Married | 18 | 28 | .05 |
| Married | 37 | 46 | |
| Divorced/separated | 8 | 4 | |
| Domestic partners | 3 | 11 | |
| Widowed | 1 | 4 | |
| Other | 2 | 2 | |
| Employment status | |||
| Employed | 34 | 60 | .03 |
| Household income | |||
| Less than $25,000 | 10 | 9 | .005 |
| $25-$49,000 | 7 | 12 | |
| $50-$74,000 | 11 | 3 | |
| More than $75,000 | 30 | 63 | |
| Don't know or don't want to answer | 11 | 8 | |
| How many children below 18 live in your household? | .34 | .91 | <0.001 |
| Number of people live in household | 2.5 (1.3) | 3.1 (1.5) | .01 |
| Type of MS | |||
| Relapsing-Remitting | 47 (68%) | ||
| Secondary Progressive | 9 (13%) | ||
| Primary Progressive | 9 (13%) | ||
| Other | 4 (6%) | ||
| PDDS | 3 (2.3) |
Note. Group differences were analyzed by Pearson's chi-squared tests (MS vs. HA). MS: multiple sclerosis. HA: healthy adults. PDDS: patient determined disease steps (PDDS).
2.2. Measures
The current study focused on questions related to occupations of daily life, HrQOL, resilience, social support, and financial distress. Note that all assessment except for question related to engagement in daily occupations were adopted from the NIH Office of Behavioral and Social Sciences Research that compiled surveys, for assessing COVID-19-relevant Behavioral and Social Science (https://www.nlm.nih.gov/dr2/COVID-19_BSSR_Research_Tools.pdf, retrieved April 2, 2021).
Engagement in occupations of daily life was assessed by the 26-item Participation Objective Participation Subjective scale (POPS; Brown et al., 2004), and modified specifically for use during the COVID-19 pandemic. The POPS is a questionnaire designed to assess level of engagement in home and community activities and the respondent satisfaction with their level of engagement. In the current study, all activities presented in the original POPS were included; however, the questions were modified to reflect changes in engagement in daily occupations during the pandemic. For each activity, participants were asked to indicate whether they (1) did this task prior to the pandemic (at least once a week); (2) continued to do the activity after the pandemic started; (3) continued to do the activity after the pandemic started (but with changes or modifications); (4) had given up the activity; or (5) started doing the activity for the first time. The POPS activities described by the participants was used to create four composite scores: (1) number of activities participants continued to do; (2) number of activities they continued to do with modifications; (3) number of activities they stopped doing during the pandemic, and (4) number of activities they started doing for the first time during the pandemic.
HrQOL was assessed by the Functional Assessment of Cancer Therapy-7 (FACTG7), a brief well-validated and widely available measure of HrQOL (Mah et al., 2020; Penedo et al., 2020). This questionnaire was modified to include language relevant to MS only, and not cancer. It assesses the patient's physical and emotional well-being. A sum score was composed (after reversing three items) to indicate levels of HrQOL, where lower scores indicate better HrQOL
Resilience was assessed using the four-item Brief Resilient Coping Scale (Sinclair and Wallston, 2004), designed to assess tendencies to cope with stress adaptively. The scale focuses on the tendency to effectively use coping strategies in flexible, committed ways to actively solve problems, despite stressful circumstances. Scores range from 4 to 20, with higher scores indicating better resilience.
Social support was assessed by the abbreviated Medical Outcomes Study (MOS) Social Support Survey (Gjesfjeld et al., 2008; Sherbourne and Stewart, 1991). It is a brief, self- administered, social support survey that was developed for patients in the MOS. Using a five-point Likert scale, participants rated the extent to which they agreed with each of the 10 items regarding support they receive from others. Higher scores indicate more support.
Financial distress was assessed by questions from the COVID-19: Impact of the Pandemic and HRQOL in Cancer Patients and Survivors scale (Penedo et al., 2020). Respondents used a five-point Likert scale to rate the extent to which they agreed with statements related to financial stress when specifically thinking about the peak pandemic time period: a total score was created by totaling the answers to these statements. Higher scores indicate more financial stress.
2.3. Procedures
Data collection occurred between July and October 2020. During this time, most states just started to reduce some of the restrictions that were in place from March to May of 2020. Data was collected by a survey administered via Research Electronic Data Capture (REDCap) tools, hosted by Rutgers New Jersey Medical School. Participants were recruited via various social networks (e.g. Facebook, Instagram), and personal communications (support groups and word of mouth). During the recruitment process (either via social network or personal communication), all participants clicked on a secure link for information about the study, followed by informed consent. The data was collected and stored on a HIPAA compliant encrypted application (REDCap) which was designed to securely handle research data. Prior to downloading the data, any identifiable protected health information (PHI) was removed so that all data was de-identified. Further, PHI was restricted to email address. All participants provided consent to participate via the REDCap survey, which was approved by the Kessler Foundation Institutional Review Board. The survey took approximately 30 to 40 min to complete.
Data analysis
In inferential statistical analyses, responses of “don't know” or “prefer not to answer” were converted to missing values. Values were reversed in scales when needed to have all responses scored in the same direction (e.g., HrQOL). Pearson's chi-squared tests were performed to analyze group differences (MS vs. HA) in occupational engagement-related questions (i.e., POPS). One way analysis of covariance was done to compare MS and HA groups on the four occupational engagement composite scores with age as a covariate. Spearman ranked correlation was used to calculate coefficients for four variables related to engagement in occupation of daily activities (i.e., continued to do activities; continued to do activities with modification; stopped doing activities due to COVID-19; and started doing this activity since COVID-19) with HrQOL, resilience, social support, and financial distress. These analyses were done for the whole sample, and in each group separately (MS and HA sample). Lastly, linear hierarchical multiple regression was performed to examine predictors of HrQOL in HA and persons with MS. During Step 1, demographics (age and education) were entered; during Step 2, resilience, social support, and financial distress were added; and during Step 3, the four POPs activity scales were entered.
3. Results
3.1. Changes in levels of occupations of daily living since the pandemic
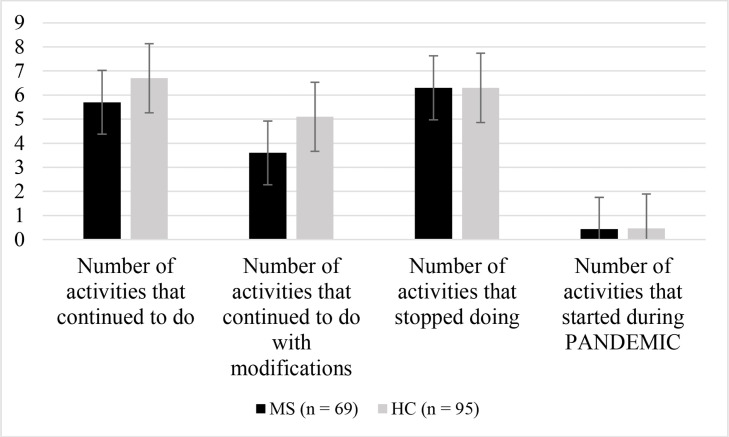
Fig. 1 presents comparisons between HA and MS while controlling for age for the four composite scores of number of activities participants continued to do during the pandemic; continued to do with modifications; stopped doing during the pandemic, and activities they started doing during the pandemic. The number of activities that participants with MS continued to do with modifications [F(2, 164) = 10.1, p = 0.002], and without modifications [F(2, 164) = 6.6, p = 0.01], were significantly fewer than the number of activities HA group continued to do. Numbers of activities they stopped and started doing during the pandemic were similar between the two groups. For itemized description of activities, see supplementary Table 1.
Fig. 1.
Mean number of daily activities participants in the MS and HA groups started, stopped, continued or continued to do with modifications during the pandemic. Note. Error bars indicate standard error. MS = Multiple sclerosis; HA = Heathy Adults.
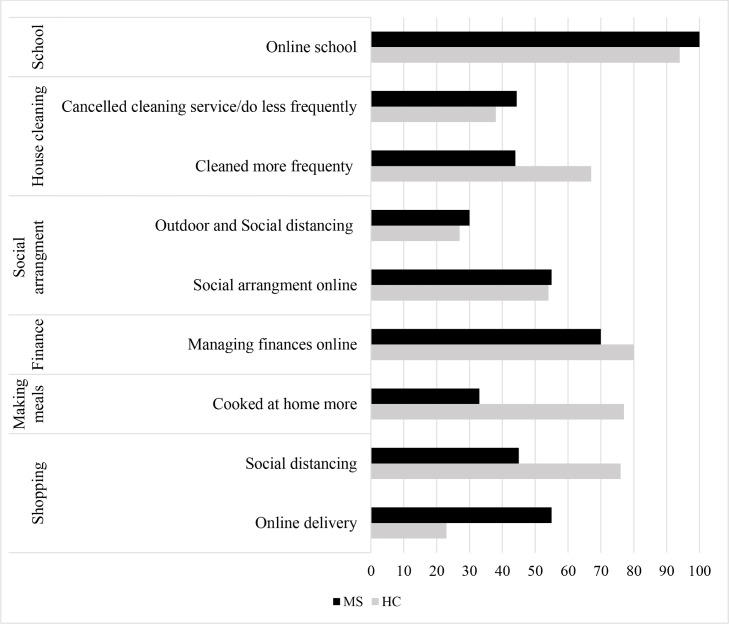
Importantly, most of the modifications noted by participants in both groups involved engaging in the activities online, the telephone or performing virtual activities (e.g. Zoom, Skype, FaceTime, etc.); only essential activities (e.g., shopping for groceries and necessities) were performed in person utilizing social distancing and personal protective equipment in both groups. Fig. 2 provides description of some of the most frequent adjustments reported by both groups for selected activities.
Fig. 2.
Parentage of sample of adjustments participants with MS and HA used during the pandemic when engaging in occupations of everyday life.
3.2. Relationship between HrQOL, engagement in occupations, social support, resilience, and financial distress
At the time of this study, during the pandemic, participants with MS reported lower HrQOL (MS: M = 16.1; SD = 4.6;. HA: M = 11.1, SD =4.7); F(1177) = 48.2, p < .001) and less social support (MS: M = 37.9; SD = 9.9 vs. HA: M = 40.6, SD = 6.8; F(1201) = 5.2, p = .03) compared to HA. Both groups reported similar levels of resilience (F(1, 201) = 0.69, p = 0.32).
Table 2 presents results of the Spearman ranked correlation coefficients for the entire sample (MS and HA). Higher levels of HrQOL, resilience, and social support were associated with more activities that participants were doing during the pandemic with and without modifications. Years of education were associated with more activities that participants were doing during the pandemic with modifications, and with activities they stopped doing. Similar correlations were observed when the HA and MS groups were analyzed separately.
Table 2.
Correlations between activity and participation, and HRQOL (n = 164).
| Number of activities Continue to do | Number of activities Continue to do with modification | Number of Activities stopped doing | Number of Activities started doing during the pandemic | |
| Age | .08 | −0.03 | −0.05 | −0.05 |
| Education | .11 | .18* | .23** | .12 |
| Gender | .15 | −0.06 | −0.03 | −0.02 |
| PDDSϯ | −0.06 | −0.04 | −0.006 | −0.07 |
| Resilience and coping | .23** | .21** | .15* | .12 |
| Social support | .32** | .22** | .20** | −0.006 |
| HrQOL | −0.26** | −0.22** | .05 | −0.01 |
| Financial distress | −0.31** | −0.08 | −0.05 | .13 |
** p <0.01.
*** p <0.001.
Note. HRQOL = health-related quality of life; PDDS: patient determined disease steps (PDDS).
Ϯ correlation was done only with MS participants.
Multiple hierarchical linear regression was performed to examine whether patterns of engagement in occupations could predict HrQOL, while controlling for demographics (age and education), financial distress, resilience, and social support, as those variables were significantly associated with HrQOL. These analyses were done with the entire sample, as patterns of correlations were similar in both groups. Results of the hierarchical analyses are presented in Table 3 . As summarized in Table 3 (Model 1), age and years of education were not significant contributors to Model 1 [F(2, 122) = 1.6, p > .05] and accounted for 2% of the variation in HrQOL. Introducing resilience, social support and financial distress (Model 2) explained an additional 5% of variation in HrQOL, and this model was not significant [F(5, 122) = 1.9, p > .05]. Finally, the addition of engagement in occupations to the regression model (Model 3) explained an additional 12% of the variation in HrQOL, and the model was significant [F(9, 122) = 2.9, p < .01]. That is, only number of activities that participants continued to do (p = .01), activities continue to do with modifications (p = .006), and numbers of activity stopped (p = .01) were significant independent predictors of HrQOL.
Table 3.
Predicting HRQOL from Activity Patterns resilience and social support (n = 164).
| Model 1 | Model 2 | Model 3 | ||||||
| B | SE | B | SE | B | SE | |||
| Age | .02 | .04 | .04 | .04 | .04 | .04 | ||
| Education | −0.42 | .24 | −0.29 | .25 | −0.37 | .24 | ||
| Resilience | −0.20 | .21 | −0.08 | .20 | ||||
| Social Support | −0.09 | .06 | −0.06 | .06 | ||||
| Financial distress | .12 | .09 | .25 | .09 | ||||
| # of activities continue to do | −0.34* | .14 | ||||||
| #of activities continue to do with modifications | −0.43** | .15 | ||||||
| # activities stopped | .35* | .13 | ||||||
| # Activities Started | −0.06 | .54 | ||||||
| R2 | .02 | .07 | .19** |
*p < .05, **p < .01.
Note. B = unstandardized coefficient; SE = standard error; HRQOL = health-related quality of life; Bolded numbers indicate statistical significance.
4. Discussion
The current study examined engagement in occupations of daily living among individuals with MS and HAs during the COVID-19 pandemic relative to before the pandemic. As expected, both groups changed their patterns of activity engagement due to restrictions posed by the pandemic and/or imposed by the government or recommended by public health organizations such as the Centers for Disease Control and Prevention (Szczepańska and Pietrzyka, 2021). Importantly, both groups were able to continue to perform many activities with modifications (e.g., using an online platform). This ability to adapt is important, as we demonstrated that the number of activities participants continued to perform (with or without adjustments) were significantly associated with their HrQOL.
We hypothesized that persons with MS and HAs would both experience changes in occupations of daily life but that HA would make more adjustments to the ways they performed activities in response to restrictions posed by COVID-19 pandemic compared with persons with MS. This hypothesis was supported by the results of this current study. A significant finding of the current study is that more HA were engaged in everyday occupations with and without modifications compared with persons with MS. We were not surprised to find that persons with MS were less engaged than HA in daily occupations during the pandemic. It is known that persons with MS usually experience some levels of restriction in occupations of daily living imposed by symptoms of their disease regardless of the pandemic (Conradsson et al., 2018; Goverover et al., 2020). In addition, we found that changes in daily occupations were made by both groups in most activities, however, HA used more modifications than MS to maintain engagement. One of the most reported occupational modifications in this study was the use of internet-based technology for various activities, for example, shopping and socialization. Note that previous research have shown that better cognitive skills are associated with performance of internet-based technologies in persons with MS (Goverover et al., 2021). In this current study, cognitive functions were not assessed. However, based on the study by Goverover et al. (2021) and others that were done in older adults (Freese et al., 2006), it is possible that individuals with MS with poor cognitive skills were having difficulties applying such modifications due their deficits. It is also possible that by the time the COVID-19 pandemic hit, for some activities, persons with MS may have exhausted or did not have the emotional, personal, and environmental resources for successful modification to continue engaging in these daily occupations. Thus, the pandemic presented an additional challenge to their already limited capacity.
The results also showed (when looking at the answers participants gave to the individual items of the questionnaire) that some activities were done at a similar rate during the pandemic to before the pandemic in both groups. Such activities as shopping for groceries and necessities, may have been considered “necessary” which may have increased the desire to continue to do the activity, making modifications when necessary (Pettigrew et al., 2017). Other activities such as arranging social gatherings may have been modified as they were important for emotional well-being and HrQOL (Koutsogeorgou et al., 2020).
Our study indicates that persons with MS reported worse HrQOL in comparison to HA. This finding is not surprising because HrQOL is in general reduced in MS as compared to healthy adults (Nicholl et al., 2005). Nonetheless recent studies demonstrated that both persons with MS and HA reported that restrictions enforced during the COVID-19 pandemic contributed to a significant decline in the mood, psychological well-being and HrQOL (Lipskaya-Velikovsky, 2020; Naseri et al., 2021; Szczepańska and Pietrzyka, 2021). The current study is the first that examined the effect of the pandemic on engagement in occupations of daily living in individuals with neurologic disability and how such changes in everyday engagement were associated with HrQOL above and beyond attributes such as loneliness, social support and financial distress in persons with MS. The results of the current study support the postulate posed by various health professionals about the positive relationship between engagement in occupations, health, and wellbeing (Bar and Jarus, 2015; Townsend and Polatajko, 2007). In this study we found that participants in both groups who continued to engage in more daily occupations also reported better resilience and coping, stronger social support, less financial distress and better HrQOL than people who did less or stopped doing daily occupation. Previous studies described similar relationships between engagement in everyday activities and QOL in people with neurological illnesses (Forsberg et al., 2015; Sun et al., 2018). Engagement in daily occupations provides a sense of agency and self-determination, leading to greater life satisfaction and QOL (Burkhart, 2019; Steger et al., 2008). Nonetheless, this current study extends these results to the area of maintenance of daily occupational during a time of crisis such as the COVID-19 pandemic, and further emphasize the importance of engagement in everyday activities to maintain HrQOL in persons with MS.
This study has several limitations, including the use of a modified version of the POPs, which was designed to measure activity changes and satisfaction with these activities pre to post an illness. While the use of the POPs in the current study allowed us to examine activity change during the pandemic, we understand that the questionnaire was not designed to examine this particular issue. However, we thought the study question was important to examine, even in the absence of validated tools. Additionally, we assessed activity change, but did not examine what caused the change in activity. For example, some activities may have been stopped because individuals felt they did not have the choice to continue due to government-imposed restrictions. Future studies will examine why activities were stopped or modified. It is important to note that while our study may have implications for many disability groups, we only examined individuals with MS which may have had unique stressors during the pandemic. In order to fully understand how the pandemic affected others with disability, we would need to examine other disability groups. Finally, the sample power was not considered for this study as it was a convenience sample, and thus, the study results should be interpreted cautiously. Also, participants with MS and HA presented with different demographic characteristics (e.g. age, employment and income) which could have an effect on the study results; nonetheless, such characteristic differences are common in these samples, and were controlled statistically in the comparison and regression analysis.
4.1. Conclusions
Life during the COVID-19 pandemic resulted in consequences for many around the world. These consequences include (and are not limited to) deteriorated quality of life (Manacorda et al., 2021; Naseri et al., 2021; Pfefferbaum and North, 2020), reduced and modified work capacity (Brynjolfsson et al., 2020), and risks of physical health problems and increased mortality (Mehra et al., 2020). This current study demonstrates that the pandemic affected engagement in activities of daily life for both HA and MS. Yet, it is important to remember that even before the pandemic, people with MS were less engaged in everyday occupations compared with HA (Goverover et al., 2015, 2020), and thus changes caused by the pandemic put them in a higher risk of reduced engagement in everyday life activities and HrQOL. In addition, HAs made more adjustments to many of these activities compared with persons with MS. Given the importance of engagement in everyday occupations for HrQOL, the results of this study call for health professionals to address engagement in daily occupations for persons with MS through compensational interventions that can be applied during different stages of disability. For example, practicing and leaning to use internet-based technology for better every day occupational engagement.
CRediT authorship contribution statement
Yael Goverover: Conceptualization, Formal analysis, Methodology, Writing – original draft. Michelle H. Chen: Data curation, Writing – review & editing. Amanda Botticello: Writing – review & editing. Gerald T. Voelbel: Writing – review & editing. Grace Kim: Writing – review & editing. John DeLuca: Writing – review & editing. Helen M. Genova: Conceptualization, Resources, Software, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.msard.2021.103339.
Appendix. Supplementary materials
References
- Bar M.A., Jarus T. The effect of engagement in everyday occupations, role overload and social support on health and life satisfaction among mothers. Int. J. Environ. Res. Public Health. 2015;12(6):6045–6065. doi: 10.3390/ijerph120606045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown M., Dijkers M.P.J.M., Gordon W.A., Ashman T., Charatz H., Cheng Z. Participation objective, participation subjective: a measure of participation combining outsider and insider perspectives. J. Head Trauma Rehabil. 2004;19(6):459–481. doi: 10.1097/00001199-200411000-00004. [DOI] [PubMed] [Google Scholar]
- Brynjolfsson E., Horton J.J., Ozimek A., Rock D., Sharma G., TuYe H.-.Y. National Bureau of Economic Research; 2020. COVID-19 and Remote Work: an Early Look at US Data (No. w27344) [DOI] [Google Scholar]
- Tichá R., Bitova V., Legostaeva E., Muratova A. In: Handbook on Community Living and Employment. Tichá R., editor. Russian Federation: Life Route Foundation; Minneapolis, MN, USA: University of Minnesota; Moscow: 2019. Importance of Engagement in Activities of Daily Living (Chapter 7) [Google Scholar]
- Conradsson D., Ytterberg C., von Koch L., Johansson S. Changes in disability in people with multiple sclerosis: a 10-year prospective study. J. Neurol. 2018;265(1):119–126. doi: 10.1007/s00415-017-8676-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtenay K. Covid-19: challenges for people with intellectual disability. BMJ. 2020 doi: 10.1136/bmj.m1609. m1609. [DOI] [PubMed] [Google Scholar]
- Forsberg A., Widén-Holmqvist L., Ahlström G. Balancing everyday life two years after falling ill with Guillain-Barré syndrome: a qualitative study. Clin. Rehabil. 2015;29(6):601–610. doi: 10.1177/0269215514549564. [DOI] [PubMed] [Google Scholar]
- Freese J., Rivas S., Hargittai E. Cognitive ability and Internet use among older adults. Poetics. 2006;34(4):236–249. doi: 10.1016/j.poetic.2006.05.008. [DOI] [Google Scholar]
- Gjesfjeld C.D., Greeno C.G., Kim K.H. A confirmatory factor analysis of an abbreviated social support instrument: the MOS-SSS. Res. Soc. Work Pract. 2008;18(3):231–237. doi: 10.1177/1049731507309830. [DOI] [Google Scholar]
- Goverover Y., Genova H.M., Smith A., Lengenfelder J., Chiaravalloti N.D. Changes in activity participation after multiple sclerosis diagnosis. Int. J. MS Care. 2020;22(1):23–30. doi: 10.7224/1537-2073.2018-036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goverover Y., Stern B.Z., Hurst A., DeLuca J. Internet-based technology in multiple sclerosis: exploring perceived use and skills and actual performance. Neuropsychology. 2021;35(1):69–77. doi: 10.1037/neu0000695. [DOI] [PubMed] [Google Scholar]
- Goverover Y., Strober L., Chiaravalloti N., DeLuca J. Factors that moderate activity limitation and participation restriction in people with multiple sclerosis. Am. J. Occup. Ther. 2015;69(2) doi: 10.5014/ajot.2015.014332. [DOI] [PubMed] [Google Scholar]
- Hohol M.J., Orav E.J., Weiner H.L. Disease steps in multiple sclerosis: a simple approach to evaluate disease progression. Neurology. 1995;45(2):251–255. doi: 10.1212/wnl.45.2.251. [DOI] [PubMed] [Google Scholar]
- Kahraman T., Özdoğar A.T., Özakbaş S. Cross-cultural adaptation, validity and reliability of the Turkish version of the patient determined disease steps scale in persons with multiple sclerosis. Physiother. Theory Pract. 2021;37(4):527–534. doi: 10.1080/09593985.2019.1633715. [DOI] [PubMed] [Google Scholar]
- Kalron A., Dolev M., Greenberg-Abrahami M., Menascu S., Frid L., Avrech-Shezifi S., Harari G., Magalashvili D., Achiron A. Physical activity behavior in people with multiple sclerosis during the COVID-19 pandemic in Israel: results of an online survey. Mult. Scler. Relat. Disord. 2021;47 doi: 10.1016/j.msard.2020.102603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall E., Ehrlich C., Chapman K., Shirota C., Allen G., Gall A., Kek-Pamenter J.-.A., Cocks K., Palipana D. Immediate and long-term implications of the COVID-19 pandemic for people with disabilities. Am. J. Public Health. 2020;110(12):1774–1779. doi: 10.2105/AJPH.2020.305890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koutsogeorgou E., Chiesi A.M., Leonardi M. Social capital components and social support of persons with multiple sclerosis: a systematic review of the literature from 2000 to 2018. Disabil. Rehabil. 2020;42(24):3437–3449. doi: 10.1080/09638288.2019.1597182. [DOI] [PubMed] [Google Scholar]
- Lipskaya-Velikovsky L. COVID-19 isolation in healthy population in Israel: challenges in daily life, mental health, resilience, and quality of life. Int. J. Environ. Res. Public Health. 2020;1(1):1–2. doi: 10.3390/ijerph2004010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luis A.-.C., Domingo R.-.C., Pedro M., Oriol A.-A., H, C.L., Jacobo Á R.-.A. Effect of COVID-19 home confinement in people with multiple sclerosis: sleep and cardiac autonomic function monitorization. Physiol. Behav. 2021 doi: 10.1016/j.physbeh.2021.113392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mah K., Swami N., Le L.W., Chow R., Hannon B.L., Rodin G., Zimmermann C. Validation of the 7-item Functional Assessment of Cancer Therapy-General (FACT-G7) as a short measure of quality of life in patients with advanced cancer. Cancer. 2020;126(16):3750–3757. doi: 10.1002/cncr.32981. [DOI] [PubMed] [Google Scholar]
- Manacorda T., Bandiera P., Terzuoli F., Ponzio M., Brichetto G., Zaratin P., Bezzini D., Battaglia M.A. Impact of the COVID-19 pandemic on persons with multiple sclerosis: early findings from a survey on disruptions in care and self-reported outcomes. J. Health Serv. Res. Policy. 2021;26(3):189–197. doi: 10.1177/1355819620975069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Cardiovascular disease, drug therapy, and mortality in Covid-19. N. Engl. J. Med. 2020;382(25):e102. doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Naseri A., Nasiri E., Talebi M., Talebi M. The effects of the COVID-19 pandemic on quality of life; a survey of mildly disabled multiple sclerosis patients. East. Mediterr. Health J. 2021 doi: 10.26719/emhj.21.034. [DOI] [PubMed] [Google Scholar]
- Nicholl L., Hobart J.C., Cramp A.F., Lowe-Strong A.S. Measuring quality of life in multiple sclerosis: not as simple as it sounds. Mult. Scler. J. 2005;11(6):708–712. doi: 10.1191/1352458505ms1235oa. [DOI] [PubMed] [Google Scholar]
- Penedo, F.J., Cohen, L., Bower, J., & Antoni, M.H. (2020). COVID-19: impact of the pandemic and HRQOL in cancer patients and survivors. Unpublished Questionnaire, 3, https://www.nlm.nih.gov/dr2/COVID-19_IMPACT_HRQOL_QUESTIONNAIRE_FINAL.pdf.
- Pettigrew S., Worrall C., Biagioni N., Talati Z., Jongenelis M. The role of food shopping in later life. Appetite. 2017;111:71–78. doi: 10.1016/j.appet.2016.12.035. [DOI] [PubMed] [Google Scholar]
- Pfefferbaum B., North C.S. Mental health and the Covid-19 pandemic. N. Engl. J. Med. 2020;3:510–512. doi: 10.1056/NEJMp2008017. [DOI] [PubMed] [Google Scholar]
- Pišot S., Milovanović I., Šimunič B., Gentile A., Bosnar K., Prot F., Bianco A., Lo Coco G., Bartoluci S., Katović D., Bakalár P., Kovalik Slančová T., Tlučáková L., Casals C., Feka K., Christogianni A., Drid P. Maintaining everyday life praxis in the time of COVID-19 pandemic measures (ELP-COVID-19 survey) Eur. J. Public Health. 2020;30(6):1181–1186. doi: 10.1093/eurpub/ckaa157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne C.D., Stewart A.L. The MOS social support survey. Soc. Sci. Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-B. [DOI] [PubMed] [Google Scholar]
- Sinclair V.G., Wallston K.A. The development and psychometric evaluation of the brief resilient coping scale. Assessment. 2004;11(1):94–101. doi: 10.1177/1073191103258144. [DOI] [PubMed] [Google Scholar]
- Steger M.F., Kashdan T.B., Oishi S. Being good by doing good: daily eudaimonic activity and well-being. J. Res. Pers. 2008;42(1):22–42. doi: 10.1016/j.jrp.2007.03.004. [DOI] [Google Scholar]
- Sun M., Mainland B.J., Ornstein T.J., Mallya S., Fiocco A.J., Sin G.L., Shulman K.I., Herrmann N. The association between cognitive fluctuations and activities of daily living and quality of life among institutionalized patients with dementia. Int. J. Geriatr Psychiatry. 2018;33(2):e280–e285. doi: 10.1002/gps.4788. [DOI] [PubMed] [Google Scholar]
- Szczepańska A., Pietrzyka K. The COVID-19 epidemic in Poland and its influence on the quality of life of university students (young adults) in the context of restricted access to public spaces. J. Public Health (Bangkok) 2021 doi: 10.1007/s10389-020-01456-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Townsend E.A., Polatajko H.J. 2007. Enabling Occupation II: Advancing an Occupational Therapy, Vision of Health, Well-Being & Justice Through Occupation. [Google Scholar]
- Umucu E., Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil. Psychol. 2020;65(3):193–198. doi: 10.1037/rep0000328. [DOI] [PubMed] [Google Scholar]
- Wallin M.T., Culpepper W.J., Campbell J.D., Nelson L.M., Langer-Gould A., Marrie R.A., Cutter G.R., Kaye W.E., Wagner L., Tremlett H., Buka S.L., Dilokthornsakul P., Topol B., Chen L.H., LaRocca N.G. The prevalence of MS in the United States: a population-based estimate using health claims data. Neurology. 2019;92(10):e1029–e1040. doi: 10.1212/WNL.0000000000007035. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.