ABSTRACT
SCTA01 is a novel monoclonal antibody with promising prophylactic and therapeutic potential for COVID-19. This study aimed to evaluate the safety, tolerability, pharmacokinetics (PK) and immunogenicity of SCTA01 in healthy adults. This was a randomized, double-blind, placebo-controlled, dose escalation phase I clinical trial. Healthy adults were randomly assigned to cohort 1 (n = 5; 3:2), cohort 2 (n = 8; 6:2), cohort 3, or cohort 4 (both n = 10; 8:2) to receive SCTA01 (5, 15, 30, and 50 mg/kg, respectively) versus placebo. All participants were followed up for clinical, laboratory, PK, and immunogenicity assessments for 84 days. The primary outcomes were the dose-limiting toxicity (DLT) and maximal tolerable dose (MTD), and the secondary outcomes included PK parameters, immunogenicity, and adverse events (AE). Of the 33 participants, 18 experienced treatment-related AEs; the frequency was 52.0% (13/25) in participants receiving SCTA01 and 62.5% (5/8) in those receiving placebo. All AEs were mild. There was no serious AE or death. No DLT was reported, and the MTD of SCTA01 was not reached. SCTA01 with a dose range of 5 to 50 mg/kg had nearly linear dose-proportional increases in Cmax and AUC parameters. An antidrug antibody response was detected in four (16.0%) participants receiving SCTA01, with low titers, between the baseline and day 28, but all became negative later. In conclusion, SCTA01 up to 50 mg/kg was safe and well-tolerated in healthy participants. Its PK parameters were nearly linear dose-proportional. (This study has been registered at ClinicalTrials.gov under identifier NCT04483375.)
KEYWORDS: COVID-19, SARS-CoV-2, monoclonal antibody, safety, pharmacokinetics
INTRODUCTION
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and manifesting as respiratory tract infection with severe multiorgan dysfunction, has become a worldwide pandemic since the first reported case in December 2019 (1). The number of confirmed cases of COVID-19 has exceeded 103 million, with over 2 million deaths as of 1 February 2020 (2). Remdesivir, a nucleotide prodrug of an adenosine analog, is currently the only drug approved for the treatment of COVID-19 (3), and efficacious therapeutic strategies for COVID-19 are still largely lacking.
Antibody-based passive immunotherapies, including convalescent-phase plasma and monoclonal antibodies, are reported to be promising treatment options for COVID-19 as they neutralize SARS-CoV-2 by primarily targeting the receptor-binding domain (RBD) of the spike protein, which mediates its entry into the host cells (4–13). Previous studies have shown that convalescent-phase plasma is associated with improved viral load suppression, clinical symptoms, and survival in the treatment of COVID-19 (6–13). However, the collection of sufficient plasma from infected COVID-19 patients is not always feasible and practical. Thus, monoclonal antibodies are highly expected to play a critical role in fighting against COVID-19. Currently, more than 20 anti-SARS-CoV-2 monoclonal antibodies are being investigated in the preclinical and clinical trials (14). Based on the clinical benefits and verified viral load decline in outpatient trials, an antibody cocktail consisting of casirivimab plus imdevimab and bamlanivimab as a monotherapy were approved by the U.S. Food and Drug Administration in November 2020 for emergency use to treat patients with mild to moderate COVID-19 symptoms (5, 15, 16). Although bamlanivimab alone failed to demonstrate a clinical benefit for hospitalized COVID-19 patients without end-stage organ failure (17), a combination of bamlanivimab with etesevimab significantly reduced hospitalizations and deaths among high-risk patients recently diagnosed with COVID-19 (18). Increasing evidence suggests that anti-SARS-CoV-2 monoclonal antibodies are efficacious in the prevention and treatment of COVID-19 (19).
SCTA01, also named HB27, is a newly developed monoclonal antibody of the IgG1 subtype with functions similar to those of bamlanivimab but possesses unique features (20). The Fc-mutated (LALA) modification of SCTA01 not only reduces antibody-dependent enhancement (ADE) and antibody-dependent cell cytotoxicity (ADCC) but also guarantees its high-affinity neutralizing responses (see Fig. S1 in the supplemental material) (20). Our previous in vitro study validated the neutralizing activity of SCTA01 with a classical plaque reduction neutralization test value of 0.22 nM (20). In addition, both prophylactic and therapeutic efficacies of SCTA01 were demonstrated in animal experiments (20). Specifically, a single dose of 20 mg/kg administered either before or 2 h after SARS-CoV-2 exposure resulted in >99.9% reduction of the viral RNA load 5 days postinfection in the lungs and trachea in the mouse model, accompanied by alleviation of pulmonary pathological damage (20). In the rhesus monkey model, no obvious adverse events (AE) were observed when SCTA01 was administered at 10 times the effective dose (500 mg/kg) (20).
Based on these encouraging findings in vitro and in animal models, this randomized, double-blind, placebo-controlled phase I study was carried out to evaluate the safety, tolerability, pharmacokinetics (PK), and immunogenicity of SCTA01 targeting SARS-CoV-2 in healthy adults.
RESULTS
Demographics and baseline characteristics of the participants.
Overall, 33 participants (22 males and 11 females with an average age of 31.4 ± 6.8 years) were randomized to receive SCTA01 (n = 25) or placebo (n = 8) between 24 July 2020 and 21 August 2020. The baseline demographic characteristics were balanced across cohorts (Table 1).
TABLE 1.
Baseline demographic characteristics of the participants
| Characteristica | Value for: |
|||||
|---|---|---|---|---|---|---|
| SCTA01 dose group |
Total SCTA01 group (n = 25) | Placebo group (n = 8) | ||||
| 5 mg/kg (n = 3) | 15 mg/kg (n = 6) | 30 mg/kg (n = 8) | 50 mg/kg (n = 8) | |||
| Age (yrs) | ||||||
| Mean (SD) | 28.0 (4.4) | 31.8 (6.9) | 30.9 (8.8) | 33.4 (6.5) | 31.6 (7.0) | 30.8 (6.6) |
| Median (range) | 26.0 (25–33) | 34 (22–40) | 29.5 (20–42) | 34.5 (23–44) | 33.0 (20–44) | 28.5 (24–41) |
| Raceb | ||||||
| Han | 3 (100) | 6 (100) | 8 (100) | 8 (100) | 25 (100) | 8 (100) |
| Other | 0 | 0 | 0 | 0 | 0 | 0 |
| Sexb | ||||||
| Male | 1 (33.3) | 5 (83.3) | 5 (62.5) | 6 (75.0) | 17 (68.0) | 5 (62.5) |
| Female | 2 (66.7) | 1 (16.7) | 3 (37.5) | 2 (25.0) | 8 (32.0) | 3 (37.5) |
| Ht (cm) | ||||||
| Mean (SD) | 164.5 (4.1) | 169.3 (3.1) | 165.3 (9.4) | 163.7 (8.0) | 165.7 (7.3) | 166.8 (7.3) |
| Median (range) | 164.1 (160.6–168.8) | 170.1 (164.8–172.9) | 165.4 (153.8–179.2) | 163.8 (151.6–174.0) | 165.9 (151.6–179.2) | 168.6 (154.6–175.6) |
| Body wt (kg) | ||||||
| Mean (SD) | 60.5 (2.5) | 67.8 (2.4) | 60.9 (6.2) | 60.9 (7.8) | 62.5 (6.3) | 61.4 (5.8) |
| Median (range) | 60.3 (58.2–63.1) | 67.7 (65.1–70.9) | 63.3 (50.2–67.8) | 61.7 (49.6–70.5) | 64.3 (49.6–70.9) | 59.8 (54.1–71.9) |
| BMI (kg/m2) | ||||||
| Mean (SD) | 22.4 (0.3) | 23.7 (0.5) | 22.3 (1.9) | 22.7 (1.7) | 22.8 (1.5) | 22.1 (2.1) |
| Median (range) | 22.4 (22.1–22.6) | 23.8 (23.4–24.0) | 22.4 (20.8–23.3) | 22.4 (21.5–24.0) | 22.6 (20.2–24.0) | 22.8 (21.8–23.9) |
SD, standard deviation; BMI, body mass index.
Data are number of patients (percentage).
The average follow-up duration was 85.3 days for participants receiving SCTA01 and 84.5 days for those receiving the placebo. All participants completed the planned dose of SCTA01 or placebo (Table 2).
TABLE 2.
Administration of SCTA01 and placebo in the participantsa
| Parameter | Value for: |
|||||
|---|---|---|---|---|---|---|
| SCTA01 dose group |
Total SCTA01 group (n = 25) | Placebo group (n = 8) | ||||
| 5 mg/kg (n = 3) | 15 mg/kg (n = 6) | 30 mg/kg (n = 8) | 50 mg/kg (n = 8) | |||
| Duration of observation (days) | ||||||
| Mean (SD) | 85.0 (0.0) | 84.0 (0.0) | 86.1 (4.5) | 85.5 (1.4) | 85.3 (2.7) | 84.5 (0.5) |
| Median (range) | 85.0 (85–85) | 84.0 (84–84) | 84.0 (84–97) | 85.0 (85–89) | 85.0 (84–97) | 84.5 (84–85) |
| Actual total SCTA01 dose injected (mg) | ||||||
| Mean (SD) | 302.7 (12.3) | 1,016.3 (35.4) | 1,825.9 (185.3) | 3,043.8 (392.1) | 1,838.5 (1,001.6) | |
| Median (range) | 301.5 (291–316) | 1,015.5 (977–1,064) | 1,897.5 (1,506–2,034) | 3,082.5 (2,480–3,535) | 1,872.0 (291–3,525) | |
The 33 participants were randomized into four cohorts as follows (SCTA01:placebo): cohort 1, 3:2 (5 mg/kg SCTA01); cohort 2, 6:2 (15 mg/kg SCTA01); cohort 3, 8:2 (30 mg/kg SCTA01); and cohort 4, 8:2 (50 mg/kg SCTA01). Participants receiving placebo in the four cohorts were pooled. SD, standard deviation.
Safety and tolerability.
Overall, 21 participants experienced 49 AEs; 18 participants had 34 AEs that were classified as treatment-related AEs (TRAEs). The percentage of participants with TRAEs was lower in the SCTA01 group than the placebo group (13 [52.0%] versus 5 [62.5%]). All TRAEs were mild at grade 1 or 2, and no serious AE (SAE) or death was observed. Thus, there was no dose-limiting toxicity (DLT), and the maximal tolerable dose (MTD) of SCTA01 was not reached in the present study (Table 3; Table S1).
TABLE 3.
Number of participants with treatment-related adverse events within the 84 days
| Event | No. (%) of participants in group |
|||||
|---|---|---|---|---|---|---|
| SCTA01 dose |
Total SCTA01 (n = 25) | Placebo (n = 8) | ||||
| 5 mg/kg (n = 3) | 15 mg/kg (n = 6) | 30 mg/kg (n = 8) | 50 mg/kg (n = 8) | |||
| Any adverse event | 1 (33.3) | 2 (33.3) | 5 (62.5) | 5 (62.5) | 13 (52.0) | 5 (62.5) |
| Any adverse event of ≥grade 3 | 0 | 0 | 0 | 0 | 0 | 0 |
| Laboratory investigations | 1 (33.3) | 2 (33.3) | 4 (50.0) | 3 (37.5) | 10 (40.0) | 5 (62.5) |
| Increased conjugated bilirubin | 1 (33.3) | 0 | 2 (25.0) | 1 (12.5) | 4 (16.0) | 0 |
| Increased unconjugated bilirubin | 1 (33.3) | 0 | 1 (12.5) | 1 (12.5) | 3 (12.0) | 1 (12.5) |
| Increased blood bilirubin | 1 (33.3) | 0 | 1 (12.5) | 0 | 2 (8.0) | 0 |
| Increased alanine aminotransferase | 0 | 1 (16.7) | 0 | 0 | 1 (4.0) | 0 |
| Increased aspartate aminotransferase | 0 | 0 | 0 | 0 | 0 | 1 (12.5) |
| Decreased neutrophil count | 0 | 0 | 1 (12.5) | 0 | 1 (4.0) | 0 |
| Decreased lymphocyte count | 0 | 0 | 0 | 0 | 0 | 1 (12.5) |
| Increased fibrin D dimer | 0 | 0 | 1 (12.5) | 0 | 1 (4.0) | 0 |
| Increased platelet count | 0 | 0 | 1 (12.5) | 0 | 1 (4.0) | 0 |
| Decreased fibrinogen | 0 | 0 | 1 (12.5) | 0 | 1 (4.0) | 0 |
| Increased potassium | 0 | 0 | 0 | 1 (12.5) | 1 (4.0) | 0 |
| Increased white blood cell count in the urine | 0 | 0 | 0 | 1 (12.5) | 1 (4.0) | 1 (12.5) |
| Protein in urine | 1 (33.3) | 1 (16.7) | 0 | 0 | 2 (8.0) | 0 |
| Prolonged QT interval | 0 | 1 (16.7) | 0 | 0 | 1 (4.0) | 0 |
| Decreased diastolic blood pressure | 0 | 0 | 0 | 0 | 0 | 1 (12.5) |
| Respiratory, thoracic and mediastinal disorders | 0 | 0 | 0 | 1 (12.5) | 1 (4.0) | 0 |
| Epistaxis | 0 | 0 | 0 | 1 (12.5) | 1 (4.0) | 0 |
| Cardiac disorders | 0 | 1 (16.7) | 0 | 0 | 1 (4.0) | 0 |
| Sinus bradycardia | 0 | 1 (16.7) | 0 | 0 | 1 (4.0) | 0 |
| Skin and subcutaneous tissue disorders | 0 | 0 | 0 | 1 (12.5) | 1 (4.0) | 0 |
| Rash | 0 | 0 | 0 | 1 (12.5) | 1 (4.0) | 0 |
| Renal and urinary disorders | 0 | 0 | 1 (12.5) | 0 | 1 (4.0) | 0 |
| Hematuria | 0 | 0 | 1 (12.5) | 0 | 1 (4.0) | 0 |
Most TRAEs were experienced only by one participant receiving SCTA01. TRAEs occurring at a frequency greater than 10% included increased blood-conjugated bilirubin (n = 4; 16.0%) and unconjugated bilirubin (n = 3; 12.0%) in participants receiving SCTA01 and increased blood-unconjugated bilirubin (n = 1; 12.5%), increased aspartate aminotransferase (n = 1; 12.5%), decreased lymphocyte count (n = 1; 12.5%), increased white blood cells in the urine (n = 1; 12.5%), and decreased diastolic blood pressure (n = 1; 12.5%) in participants receiving the placebo. The increased levels of blood bilirubin and alanine aminotransferase did not exceed 2 times the upper limit of normal (ULN). TRAEs were mostly self-recovered. Rash that developed in a participant receiving 50 mg/kg of SCTA01 resolved after treatment with loratadine combined with mometasone furoate cream, and epistaxis that developed in another participant receiving 50 mg/kg of SCAT01 resolved after medications were used to treat the symptoms (Table 3).
PK profiles.
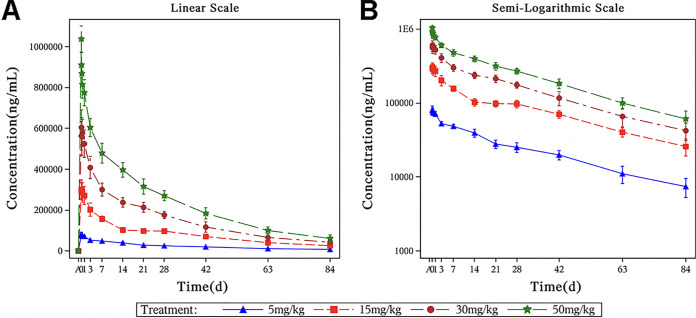
The mean SCTA01 serum concentrations versus time (linear and semilogarithmic) displayed dose dependency (Fig. 1).
FIG 1.
Mean SCTA01 serum concentrations in different dose groups. (A) Mean SCTA01 serum concentrations versus time (linear scaled) in different dose groups; (B) semilogarithmic plot of concentration-time data in different dose groups.
The median values for time to maximum concentration of drug in serum (Tmax) were 1.32, 1.92, 2.83, and 3.16 h for SCTA01 doses of 5 mg/kg, 15 mg/kg, 30 mg/kg, and 50 mg/kg, respectively. Maximum concentration of drug in serum (Cmax), area under the concentration-time curve from time zero to time t (AUC0–t), AUC from 0 to infinity (AUC0–∞), and AUC from 0 to 28 days (AUC0–28) increased in a dose-dependent manner after SCTA01 infusion. The mean half-lives (t1/2) for all dose groups were relatively close, between 25.8 and 30.2 days. In addition, similar clearance (CL) and volume of distribution (V) values at different doses of SCTA01 were observed (Table 4).
TABLE 4.
Pharmacokinetic parameters of SCTA01
| Parameter | Value for SCTA01 dose groupa |
|||
|---|---|---|---|---|
| 5 mg/kg (n = 3) | 15 mg/kg (n = 6) | 30 mg/kg (n = 8) | 50 mg/kg (n = 8) | |
| Tmax (h) | 1.32 (0.32–1.32) | 1.92 (0.92–8.92) | 2.83 (1.83–9.83) | 3.16 (3.15–3.17) |
| Cmax (μg/ml) | 84.8 | 307 | 607 | 1040 |
| AUC0–28 (day·μg/ml) | 1,120 | 3,750 | 7,700 | 11,900 |
| AUC0–t (day·μg/ml) | 1,940 | 6,690 | 12,700 | 19,600 |
| AUC0–∞ (day·μg/ml) | 2,270 | 7,760 | 14,400 | 21,900 |
| t1/2 (days) | 30.2 | 28.0 | 27.2 | 25.8 |
| CL (liters/h) | 0.00563 | 0.00552 | 0.00538 | 0.00587 |
| V (liters) | 5.82 | 5.31 | 5.00 | 5.16 |
| AUC0–∞/dose (day·μg/ml/mg) | 7.49 | 7.62 | 7.93 | 7.34 |
Data are presented as median (range) or arithmetic mean. Tmax, time taken to reach the maximum concentration; Cmax, maximum concentration; AUC, area under the concentration-time curve; AUC0–28, integral of the concentration-time curve from dosing to day 28; AUC0–t, integral of the concentration-time curve from dosing to time point t; AUC0–∞, integral of the concentration-time curve from dosing to infinity; CL, clearance; V, volume of distribution.
The dose-proportional PK properties after SCTA01 administration are shown in Table S2. Within the evaluated SCTA01 dose range (5 to 50 mg/kg), the slope of dose proportionality (β1) for the main PK parameters (Cmax, AUC0–t, AUC0–∞, and AUC0–28) were close to 1, indicating that PK of SCTA01 was linear and dose proportional in the dose range of 5 to 50 mg/kg (Fig. S2).
Immunogenicity.
The incidences of positive antidrug-antibody (ADA) were 1/3, 1/6, 1/8, and 1/8 and those of neutralizing-antibody (Nab) responses were 0/3, 1/6, 1/8, and 1/8 in the 5-, 15-, 30-, and 50-mg/kg cohorts, respectively. In total, 4 of 25 (4/25) and 3 of 25 (3/25) participants had positive ADA and Nab responses, respectively (Table 5). One participant receiving 50 mg/kg of SCTA01 had positive ADA and Nab responses at baseline and on day 7. One participant receiving 15 mg/kg of SCTA01 had a positive ADA response on days 7 and 28 and a positive Nab response at day 28. One receiving 30 mg/kg of SCTA01 had positive ADA and Nab responses on day 7. One receiving 5 mg/kg of SCTA01 had a positive ADA but negative Nab response on day 7. No correlation was found between the positive responses and SCTA01 doses, and all positive-response titers were low. All participants became negative for ADA and Nab responses at subsequent time points (Table 5).
TABLE 5.
Incidence of treatment-emergent antidrug antibody response after SCTA01 administration
| Response and follow-up timea | No. of participants with response in: |
||||
|---|---|---|---|---|---|
| SCTA01 dose group |
Total SCTA01 group (n = 25) | ||||
| 5 mg/kg (n = 3) | 15 mg/kg (n = 6) | 30 mg/kg (n = 8) | 50 mg/kg (n = 8) | ||
| ADA | |||||
| Baseline | 0 | 0 | 0 | 1 | 1 |
| Day 7 (±1 day) | 1 | 1 | 1 | 1 | 4 |
| Day 14 (±2 days) | 0 | 0 | 0 | 0 | 0 |
| Day 28 (+3 days) | 0 | 1 | 0 | 0 | 1 |
| Day 42 (±3 days) | 0 | 0 | 0 | 0 | 0 |
| Day 63 (±3 days) | 0 | 0 | 0 | 0 | 0 |
| Day 84 (±3 days) | 0 | 0 | 0 | 0 | 0 |
| Overall | 1 | 1 | 1 | 1 | 4 |
| Nab | |||||
| Baseline | 0 | 0 | 0 | 1 | 1 |
| Day 7 (±1 day) | 0 | 0 | 1 | 1 | 2 |
| Day 14 (±2 days) | 0 | 0 | 0 | 0 | 0 |
| Day 28 (+3 days) | 0 | 1 | 0 | 0 | 1 |
| Day 42 (±3 days) | 0 | 0 | 0 | 0 | 0 |
| Day 63 (±3 days) | 0 | 0 | 0 | 0 | 0 |
| Day 84 (±3 days) | 0 | 0 | 0 | 0 | 0 |
| Overall | 0 | 1 | 1 | 1 | 3 |
ADA, antidrug antibody response; Nab, neutralizing antibodies.
DISCUSSION
The ongoing COVID-19 pandemic underlines the urgent need to develop prophylactic and therapeutic agents. The novel monoclonal antibody SCTA01 for the treatment of COVID-19 was supported by our preclinical study, which proved its nonclinical safety and antiviral activity (20). This phase I clinical trial demonstrated that SCTA01 appeared to be safe and tolerable at a single dose up to 50 mg/kg in humans. All observed TRAEs were mild and most self-resolved, and no SAE or death was observed. The dose-proportional PK characteristics of SCTA01 supported a single intravenous administration which may well cover the clinical disease course of COVID-19. In addition, a transient ADA response with low titers was observed in a small proportion of participants receiving SCTA01.
The present phase I trial in healthy volunteers exhibited favorable safety in humans. During the 12-week observation period, no DLT was reported, and hence no MTD of SCTA01 was established. No TRAE with severity greater than grade 3 was observed. An increased blood bilirubin level was the most common TRAE experienced in participants receiving the SCTA01 (n = 7), but the level did not exceed 2 times the ULN. Protein in urine, sinus bradycardia, prolonged QT interval, and rash occurred in participants receiving SCTA01 but in none of those receiving the placebo. However, protein in urine observed in two participants receiving 5 mg/kg and 15 mg/kg was mild (grade 1), was transient, and self-resolved within 1 week after the completion of the SCTA01 administration. One participant receiving SCTA01 at 15 mg/kg had a baseline sinus rhythm of 62 beats per min, experienced sinus bradycardia (47 beats per minute) on day 3, and recovered without intervention after 7 h. Another one receiving the same dose of SCTA01 with a baseline QT interval close to the lower limit of normal (QTcB, 449 ms; QTcF, 442 ms) developed a prolonged QT interval at grade 1 or 2 on days 3 (QTcB, 460 ms; QTcF, 454 ms), 14 (QTcB, 451 ms; QTcF, 448 ms), 42 (QTcB, 458 ms; QTcF, 449 ms), and 84 (QTcB, 444 ms; QTcF, 449 ms). However, no cardiac symptoms were reported, and the electrocardiogram findings were not considered clinically significant. Rash in one participant receiving 50 mg/kg of SCTA01 was successfully treated with loratadine and mometasone furoate cream. It is noticeable that previous clinical trials of other neutralizing antibodies, LY-CoV555 and REGAN-COV2, in outpatients reported symptoms such as nausea, diarrhea, and dizziness, instead of laboratory abnormalities, as AEs (5, 15, 17). It is likely that it might be difficult to obtain regular laboratory results during the follow-up for trials conducted in outpatients with COVID-19 (5, 15). In the LY-CoV555 phase I trial, notable laboratory abnormalities, including a decreased absolute neutrophil count and an increased hepatic enzyme level, were reported, but they were declared to be non-drug related (5, 21). Considering the limited sample size in the present phase I study, the attribution of observed AEs to SCTA01 could not be fully determined, and further investigation is warranted.
In the present trial, the highest dose of SCTA01 (50 mg/kg) used in healthy adults achieved a Cmax of 1,040 μg/ml and an AUC0–28 of 11,900 day·μg/ml, which reached the target goal.
Based on our previous cell experiment and trials in animals of neutralization and efficacy evaluation, SCTA01 at 20 mg/kg remarkably reduced SARS-CoV-2 viral loads and alleviated lung inflammation in mice and rhesus monkeys, and SCTA01 at 500 mg/kg exhibited efficacy and tolerable safety, as reflected by normal laboratory results and organ functions in rhesus monkeys (20). The starting dose in the present study in healthy participants was 100 times lower than the maximum preclinical animal toxicity study dose of 500 mg/kg. Based on dose conversion from animals to humans, 50 mg/kg SCTA01 is speculated to be sufficient for viral neutralization. In addition, antibody LY-CoV555 at 2,800 mg in outpatients with COVID-19 was proved to be efficient in viral clearance (5). We therefore speculate that a single intravenous injection of SCTA01 at 50 mg/kg should be tried initially in subsequent human efficacy trials. In addition, unlike small molecules, monoclonal antibodies do not depend on the kidney or liver for clearance (22). Hence, corresponding organ failures in severe or critical COVID-19 patients may have a minimal effect on the clearance and metabolism of SCTA01 in the real clinical setting.
The PK profile of SCTA01 indicates that SCTA01 is active for a period that may exceed the clinical course of COVID-19. Among patients with SARS-CoV-2 infection, mild or moderate COVID-19 represents the majority, while approximately one-fifth are categorized as having severe (14%) or critical (5%) cases requiring hospitalization or emergency intervention (23). The median time from the onset of COVID-19 to dyspnea is 5 to 8 days, and the median time from onset to acute respiratory distress syndrome is 8 to 12 days (24–27). The median duration of viral shedding is 20.0 days in COVID-19 survivors (26). In the present study, the maximum concentration of SCTA01 occurred at 1 to 3 h after infusion and remained detectable for a long period, with a t1/2 around 25.8 to 30.2 days. All these data indicate the persistent antibody viral responses after a single dose application of SCTA01. Of course, the real distribution of SCTA01 might be different in patients with SARS-CoV-2 infection due to multiple affecting factors. Further studies are necessary to confirm the PK profiles and investigate the pharmacodynamics of SCTA01in infected patients.
As a heterologous protein, SCTA01 may cause a positive ADA response which may alter the PK properties of the drug, affect its efficacy, and eventually lead to clinical problems such as allergic reactions (28, 29). SCTA01 as a monoclonal antibody is considered to have low immunogenicity risk (30). Moreover, the target of SCTA01 is the spike protein of SARS-CoV-2, which is an exogenous target. In the present study, although four (16%) of 25 healthy participants receiving SCTA01 presented with a positive ADA response, all responses were transient with low titers and became negative during the follow-up. There was no correlation between positive ADA responses and SCTA01 doses. More importantly, there were no clinical allergic signs in these positive cases. Only one participant had a slight elevation of alanine aminotransferase (grade 1) concurrent with a positive ADA response, which resolved without medication. Furthermore, the baseline and PK characteristics in participants with a positive ADA response did not differ from that in those with negative responses. In our previous nonclinical study of SCTA01, no ADE response or ADCC phenomenon was detected (20). It is postulated that the Fc-mutated (LALA) modification of SCTA01 contributes to, at least partially, the reduction of ADE and ADCC. Therefore, a positive ADA response is thought to have limited clinically significant implications for SCTA01.
There are two limitations in the present study. First, the sample size was relatively small, and thus, the sample size was small in each cohort. Second, the study population were healthy participants, instead of patients with COVID-19. Thus, multicenter, phase II/III trials with a larger sample size are ongoing to fully assess the efficacy and safety of SCTA01 in adult patients with COVID-19.
In conclusion, a single infusion of SCTA01 up to 50 mg/kg is safe and well tolerated in healthy participants at potentially therapeutic exposures. PK parameters were nearly linear dose proportional, and ADA incidence was acceptable with low titers.
MATERIALS AND METHODS
Study design and participants.
This was a double-blind, placebo-controlled, single-dose escalation, phase I, randomized controlled trial. The inclusion criteria were as follows: (i) age of ≥18 years; (ii) body mass index (BMI) between 18.0 and 26.0 kg/m2, (iii) healthy status as evaluated by previous medical history, physical examination, 12-lead electrocardiogram, chest CT scan, and laboratory tests; and (iv) willingness to follow the study procedure and to use contraceptive measures during the study period and for 6 months after the end of the study. The exclusion criteria included (i) allergy to humanized monoclonal antibodies and any ingredient of SCTA01; (ii) suspected or verified SARS-CoV-2 infection; (iii) a history of severe allergies; (iv) infection or fever within 14 days before enrollment; (v) a history or presence of diseases, in the opinion of the investigator, which significantly affect the absorption, metabolism, or elimination of drugs; (vi) evidence of human immunodeficiency virus (HIV) infection and/or positive human HIV antibodies, (vii) confirmed presence of hepatitis virus and syphilitic antibody; and (viii) pregnancy or a plan to be pregnant within 6 months after the study.
Written informed consent was obtained from all participants. The study protocol was approved by the Institutional Review Board of Beijing Shijitan Hospital, Capital Medical University (approval number 2020-38). The study was performed in accordance with the local requirements and International Conference on Harmonization–Good Clinical Practice (ICH-GCP) guidelines. This trial was registered at ClinicalTrials.gov (number NCT04483375).
Randomization and dose escalation.
The random allocation sequence was generated using SAS v.9.4 (SAS Institute, Cary, NC) by a nonblind statistician. Randomization envelopes were used to randomly assign participants to receive a single dose of placebo or SCTA01 in one of four dose cohorts. Study participants and site investigators remained masked throughout the study. The dose escalation rule was adopted. In total, 33 participants were randomized into four cohorts as follows. In cohort 1, five participants were randomly assigned 3:2 to receive 5 mg/kg SCTA01 or placebo. A sentinel strategy was applied in the cohort. Initially, two participants (1:1) were recruited. Then, three more (2:1) were recruited, as no safety issues were observed. In cohort 2, eight participants were randomly assigned 6:2 to receive 15 mg/kg SCTA01 or placebo. In cohort 3, 10 participants were randomly assigned 8:2 to receive 30 mg/kg SCTA01 or placebo, and in cohort 4, 10 participants were randomly assigned 8:2 to receive 50 mg/kg SCTA01 or placebo.
Drug administration and blood sample preparation.
SCTA01 injection, which was manufactured by SCT, Inc. (China), and supplied in vials containing 25 mg/ml, was diluted with 0.9% normal saline to make a final concentration of 5 mg/ml for intravenous infusion. The participants in the four cohorts were given SCTA01 at doses of 5 mg/kg, 15 mg/kg, 30 mg/kg, and 50 mg/kg. The starting dose of 5 mg/kg was 100 times lower than the maximum preclinical animal toxicity study dose of 500 mg/kg (20). The same volume of placebo formulated with excipients without SCTA01 was administered to participants in each cohort. Participants were given drug or placebo under fasting conditions and remained fasting (with unlimited access to water) for 4 h after administration. The intravenous infusion rate was controlled to be lower than 3.33 ml/h/kg.
Blood samples were obtained within 0.5 h before infusion (baseline), immediately after infusion (+5 min), at 1, 4, and 8 h (postinfusion), and on days 1, 3, 7, 14, 21, 28, 42, 63, and 84 for PK analysis. In addition, blood samples were obtained within 0.5 h before infusion (baseline) and on days 7, 14, 28, 42, 63, and 84 for immunogenicity analysis.
Determination of serum SCTA01 concentrations and immunogenicity.
Serum SCTA01 concentrations were determined by enzyme-linked immunosorbent assay. Briefly, SARS-CoV-2 spike protein was used to coat a 96-well plate to capture SCTA01 in serum samples. Goat anti-human IgG-Fc secondary antibody was added, and streptavidin conjugated with horseradish peroxidase and 3,3′,5,5′-tetramethylbenzidine substrate were used for the reaction. The concentrations were detected at 450 nm and 620 nm with a Molecular Devices Microplate reader (Molecular Devices, San Jose, CA, USA). The minimum required dilution of serum samples was 1:200. The serum SCTA01 concentrations were quantified by using a linear regression of a SCTA01 standard curve covering a range of 200 to 10,000 ng/ml.
Blood samples collected for immunogenicity analysis were assessed for antidrug antibodies (ADA) and anti-SCTA01 neutralizing antibodies (Nab) on the basis of the Meso Scale Discovery (MSD) electrochemiluminescence homogenous bridging assay (Meso Scale Discovery, Rockville, MD, USA). After being separated from human serum by binding to SCTA01 in an enzyme-linked immunosorbent assay (ELISA) plate, anti-SCTA01 antibodies bind to both Ru-SCTA01 and Bio-SCTA01 molecules to form an antibody complex bridge, called biotinylated-SCTA01-ADA-SCTA01-ruthenylated, and then the complex binds to streptavidin (SA)-MSD plates. With the addition of 2× MSD read buffer, ruthenium label produces a chemiluminescent signal which is proportional to the concentration of ADA (Meso QuickPlex SQ120; MSD). Determination of ADA consisted of 3 sequential steps, i.e., screening, confirmation, and titer assays, as previously described (31). A titer cut point factor (TCPF) was set at 1.61, and positively confirmed samples with TCPF values of <1.61 were reported to have a titer of 1.
Determination of safety and tolerability of SCTA01.
Safety profiles, including clinical manifestations and abnormalities in electrocardiograms and laboratory tests, were closely monitored on days 0, 1, 3, 7, 14, 21, 28, 42, 63, and 84. Any adverse events (AEs) and serious AEs (SAEs) experienced by the participants were recorded. A treatment-related AE (TRAE) was defined as any AE that was possibly, probably, or definitely related to the study drug, as judged by the investigator, and the severity of a TRAE was determined based on the Division of AIDS (DAIDS) Table for Grading the Severity of Adult and Pediatric Adverse Events, version 2.1 (32).
The dose-limiting toxicity (DLT) was defined as a TRAE of grade 3 or higher (32). If necessary, the nonblind statistician was requested to summarize the occurrence of DLTs in the SCTA01 group, and the investigator and the sponsor decided together whether to discontinue the dose escalation, to lower the dose, or to continue with the next dose group. The maximum tolerated dose (MTD) was defined as the highest dose of SCTA01 at which one of three participants had DLT during the 84-day observation period (32).
Outcomes.
The primary endpoints were DLT and MTD of SCTA01. The secondary endpoints were the PK parameters, including the integral of the concentration-time curve from dosing to time point (AUC0–t), the integral of the concentration-time curve from dosing to infinity (AUC0–∞), half-life (t1/2), the time taken to reach the maximum concentration (Tmax), immunogenicity indicated by the generation of ADA, and safety reflected by the occurrence of AEs and SAEs.
Statistical analysis.
The sample size for this trial was based on the dose-escalation rule and not on any statistical criteria.
The safety analysis included all randomized participants who received any dose of the study drug. Participants receiving placebo in different cohorts were pooled. All participants who were randomized and received any dose of the SCTA01 or placebo were included in the intention-to-treat analysis, whereas those who completed the study were included in the per-protocol analysis. Categorical and continuous data, including clinical laboratory results, vital signs, and electrocardiographic features at each time point, were summarized descriptively, as they were not appropriate for statistical analysis due to the small sample size.
Participants who received SCTA01 and had at least one measurement of PK after the first dose were included in PK analysis. The PK parameters, including Tmax, Cmax, AUC0–∞, AUC0–t, the integral of the concentration-time curve from dosing to day 28 (AUC0–28), t1/2, V, and CL were calculated by a noncompartmental analysis with Certara Phoenix WinNonlin software (version 8.3.1). The Power Model was used to analyze the dose-proportionality for a 5- to 50-mg/kg dose range. The SAS software (version 9.4; SAS Institute, Cary, NC, USA) was used to perform statistical analysis.
Data availability.
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
ACKNOWLEDGMENTS
This work was supported by Beijing Municipal Science and Technology Project (Z201100005420017) and National Science and Technology Major Project (2018ZX09711003).
Liangzhi Xie is the CEO of Sinocelltech Ltd., Beijing, China. Chunyun Sun, Shuping Xu, Lixin Yan, Weiqiu Chen, Xisheng Liu, and Qing Liu are employees of Sinocelltech Ltd., Beijing, China. The other authors have no conflict of interest to declare.
X.W., L.X., S.X., C.S., W.C., and L.Y. conceived and designed research; Yinjuan Li, L.Q., H.B., Y.W., C.H., Yan Li, C.L., L.L., X.C., J.L., Y.T., M.S., X.L., and Q.L. collected data and conducted research; Yinjuan Li, L.Q., and H.B. analyzed and interpreted data; Yinjuan Li, L.Q., and H.B. wrote the initial paper; X.W. and L.X. revised the paper; and X.W. and L.X. had primary responsibility for final content. All authors read and approved the final manuscript.
Footnotes
Supplemental material is available online only.
Contributor Information
Liangzhi Xie, Email: liangzhi_xie@sinocelltech.com.
Xinghe Wang, Email: wangxh@bjsjth.cn.
REFERENCES
- 1.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, Ren R, Leung KSM, Lau EHY, Wong JY, Xing X, Xiang N, Wu Y, Li C, Chen Q, Li D, Liu T, Zhao J, Liu M, Tu W, Chen C, Jin L, Yang R, Wang Q, Zhou S, Wang R, Liu H, Luo Y, Liu Y, Shao G, Li H, Tao Z, Yang Y, Deng Z, Liu B, Ma Z, Zhang Y, Shi G, Lam TTY, Wu JT, Gao GF, Cowling BJ, Yang B, Leung GM, Feng Z. 2020. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med 382:1199–1207. 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurishima K, Watanabe H, Ishikawa H, Satoh H, Hizawa N. 2017. Survival of patients with lung cancer and diabetes mellitus. Mol Clin Oncol 6:907–910. 10.3892/mco.2017.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang Y, Zhang D, Du G, Du R, Zhao J, Jin Y, Fu S, Gao L, Cheng Z, Lu Q, Hu Y, Luo G, Wang K, Lu Y, Li H, Wang S, Ruan S, Yang C, Mei C, Wang Y, Ding D, Wu F, Tang X, Ye X, Ye Y, Liu B, Yang J, Yin W, Wang A, Fan G, Zhou F, Liu Z, Gu X, Xu J, Shang L, Zhang Y, Cao L, Guo T, Wan Y, Qin H, Jiang Y, Jaki T, Hayden FG, Horby PW, Cao B, Wang C. 2020. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 395:1569–1578. 10.1016/S0140-6736(20)31022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu NH, Nitsche A, Müller MA, Drosten C, Pöhlmann S. 2020. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181:271–280.E278. 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen P, Nirula A, Heller B, Gottlieb RL, Boscia J, Morris J, Huhn G, Cardona J, Mocherla B, Stosor V, Shawa I, Adams AC, Van Naarden J, Custer KL, Shen L, Durante M, Oakley G, Schade AE, Sabo J, Patel DR, Klekotka P, Skovronsky DM, BLAZE-1 Investigators. 2021. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med 384:229–237. 10.1056/NEJMoa2029849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, Zhou M, Chen L, Meng S, Hu Y, Peng C, Yuan M, Huang J, Wang Z, Yu J, Gao X, Wang D, Yu X, Li L, Zhang J, Wu X, Li B, Xu Y, Chen W, Peng Y, Hu Y, Lin L, Liu X, Huang S, Zhou Z, Zhang L, Wang Y, Zhang Z, Deng K, Xia Z, Gong Q, Zhang W, Zheng X, Liu Y, Yang H, Zhou D, Yu D, Hou J, Shi Z, Chen S, Chen Z, Zhang X, Yang X. 2020. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Natl Acad Sci USA 117:9490–9496. 10.1073/pnas.2004168117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, Wang F, Li D, Yang M, Xing L, Wei J, Xiao H, Yang Y, Qu J, Qing L, Chen L, Xu Z, Peng L, Li Y, Zheng H, Chen F, Huang K, Jiang Y, Liu D, Zhang Z, Liu Y, Liu L. 2020. Treatment of 5 critically ill patients with COVID-19 with convalescent plasma. JAMA 323:1582–1589. 10.1001/jama.2020.4783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abolghasemi H, Eshghi P, Cheraghali AM, Imani Fooladi AA, Bolouki Moghaddam F, Imanizadeh S, Moeini Maleki M, Ranjkesh M, Rezapour M, Bahramifar A, Einollahi B, Hosseini MJ, Jafari NJ, Nikpouraghdam M, Sadri N, Tazik M, Sali S, Okati S, Askari E, Tabarsi P, Aslani J, Sharifipour E, Jarahzadeh MH, Khodakarim N, Salesi M, Jafari R, Shahverdi S. 2020. Clinical efficacy of convalescent plasma for treatment of COVID-19 infections: results of a multicenter clinical study. Transfus Apher Sci 59:102875. 10.1016/j.transci.2020.102875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rasheed AM, Fatak DF, Hashim HA, Maulood MF, Kabah KK, Almusawi YA, Abdulamir AS. 2020. The therapeutic potential of convalescent plasma therapy on treating critically-ill COVID-19 patients residing in respiratory care units in hospitals in Baghdad, Iraq. Infez Med 28:357–366. [PubMed] [Google Scholar]
- 10.Salazar E, Christensen PA, Graviss EA, Nguyen DT, Castillo B, Chen J, Lopez BV, Eagar TN, Yi X, Zhao P, Rogers J, Shehabeldin A, Joseph D, Leveque C, Olsen RJ, Bernard DW, Gollihar J, Musser JM. 2020. Treatment of coronavirus disease 2019 patients with convalescent plasma reveals a signal of significantly decreased mortality. Am J Pathol 190:2290–2303. 10.1016/j.ajpath.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perotti C, Baldanti F, Bruno R, Del Fante C, Seminari E, Casari S, Percivalle E, Glingani C, Musella V, Belliato M, Garuti M, Meloni F, Frigato M, Di Sabatino A, Klersy C, De Donno G, Franchini M. 2020. Mortality reduction in 46 severe Covid-19 patients treated with hyperimmune plasma. A proof of concept single arm multicenter trial. Haematologica 10.3324/haematol.2020.261784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu STH, Lin HM, Baine I, Wajnberg A, Gumprecht JP, Rahman F, Rodriguez D, Tandon P, Bassily-Marcus A, Bander J, Sanky C, Dupper A, Zheng A, Nguyen FT, Amanat F, Stadlbauer D, Altman DR, Chen BK, Krammer F, Mendu DR, Firpo-Betancourt A, Levin MA, Bagiella E, Casadevall A, Cordon-Cardo C, Jhang JS, Arinsburg SA, Reich DL, Aberg JA, Bouvier NM. 2020. Convalescent plasma treatment of severe COVID-19: a propensity score-matched control study. Nat Med 26:1708–1713. 10.1038/s41591-020-1088-9. [DOI] [PubMed] [Google Scholar]
- 13.Hegerova L, Gooley TA, Sweerus KA, Maree C, Bailey N, Bailey M, Dunleavy V, Patel K, Alcorn K, Haley R, Johnsen JM, Konkle BA, Lahti AC, Alexander ML, Goldman JD, Lipke A, Lim SJ, Sullivan MD, Pauk JS, Pagel JM. 2020. Use of convalescent plasma in hospitalized patients with COVID-19: case series. Blood 136:759–762. 10.1182/blood.2020006964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li L, Zhang W, Hu Y, Tong X, Zheng S, Yang J, Kong Y, Ren L, Wei Q, Mei H, Hu C, Tao C, Yang R, Wang J, Yu Y, Guo Y, Wu X, Xu Z, Zeng L, Xiong N, Chen L, Wang J, Man N, Liu Y, Xu H, Deng E, Zhang X, Li C, Wang C, Su S, Zhang L, Wang J, Wu Y, Liu Z. 2020. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial. JAMA 324:460–470. 10.1001/jama.2020.10044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weinreich DM, Sivapalasingam S, Norton T, Ali S, Gao H, Bhore R, Musser BJ, Soo Y, Rofail D, Im J, Perry C, Pan C, Hosain R, Mahmood A, Davis JD, Turner KC, Hooper AT, Hamilton JD, Baum A, Kyratsous CA, Kim Y, Cook A, Kampman W, Kohli A, Sachdeva Y, Graber X, Kowal B, DiCioccio T, Stahl N, Lipsich L, Braunstein N, Herman G, Yancopoulos GD, Trial Investigators. 2021. REGN-COV2, a neutralizing antibody cocktail, in outpatients with Covid-19. N Engl J Med 384:238–251. 10.1056/NEJMoa2035002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gottlieb RL, Nirula A, Chen P, Boscia J, Heller B, Morris J, Huhn G, Cardona J, Mocherla B, Stosor V, Shawa I, Kumar P, Adams AC, Van Naarden J, Custer KL, Durante M, Oakley G, Schade AE, Holzer TR, Ebert PJ, Higgs RE, Kallewaard NL, Sabo J, Patel DR, Klekotka P, Shen L, Skovronsky DM. 2021. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA 325:632–644. 10.1001/jama.2021.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lundgren JD, Grund B, Barkauskas CE, Holland TL, Gottlieb RL, Sandkovsky U, Brown SM, Knowlton KU, Self WH, Files DC, Jain MK, Benfield T, Bowdish ME, Leshnower BG, Baker JV, Jensen JU, Gardner EM, Ginde AA, Harris ES, Johansen IS, Markowitz N, Matthay MA, Østergaard L, Chang CC, Davey VJ, Goodman A, Higgs ES, Murray DD, Murray TA, Paredes R, Parmar MKB, Phillips AN, Reilly C, Sharma S, Dewar RL, Teitelbaum M, Wentworth D, Cao H, Klekotka P, Babiker AG, Gelijns AC, Kan VL, Polizzotto MN, Thompson BT, Lane HC, Neaton JD, ACTIV-3/TICO LY-CoV555 Study Group. 2021. A neutralizing monoclonal antibody for hospitalized patients with Covid-19. N Engl J Med 384:905–914. 10.1056/NEJMoa2033130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karlin NJ, Amin SB, Buras MR, Kosiorek HE, Verona PM, Cook CB. 2018. Patient outcomes from lung cancer and diabetes mellitus: a matched case-control study. Future Sci OA 4:FSO248. 10.4155/fsoa-2017-0081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tuccori M, Ferraro S, Convertino I, Cappello E, Valdiserra G, Blandizzi C, Maggi F, Focosi D. 2020. Anti-SARS-CoV-2 neutralizing monoclonal antibodies: clinical pipeline. MAbs 12:1854149. 10.1080/19420862.2020.1854149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhu L, Deng Y-Q, Zhang R-R, Cui Z, Sun C-Y, Fan C-F, Xing X, Huang W, Chen Q, Zhang N-N, Ye Q, Cao T-S, Wang N, Wang L, Cao L, Wang H, Kong D, Ma J, Luo C, Zhang Y, Nie J, Sun Y, Lv Z, Shaw N, Li Q, Li X-F, Hu J, Xie L, Rao Z, Wang Y, Wang X, Qin C-F. 2021. Double lock of a potent human therapeutic monoclonal antibody against SARS-CoV-2. Natl Sci Rev 8:nwaa297. 10.1093/nsr/nwaa297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jeong SS, Choi PJ, Yi JH, Yoon SS. 2017. Impact of lifestyle diseases on postoperative complications and survival in elderly patients with stage I non-small cell lung cancer. Korean J Thorac Cardiovasc Surg 50:86–93. 10.5090/kjtcs.2017.50.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sivapalasingam S, Kamal M, Slim R, Hosain R, Shao W, Stoltz R, Yen J, Pologe LG, Cao Y, Partridge M, Sumner G, Lipsich L. 2018. Safety, pharmacokinetics, and immunogenicity of a co-formulated cocktail of three human monoclonal antibodies targeting Ebola virus glycoprotein in healthy adults: a randomised, first-in-human phase 1 study. Lancet Infect Dis 18:884–893. 10.1016/S1473-3099(18)30397-9. [DOI] [PubMed] [Google Scholar]
- 23.Wu Z, McGoogan JM. 2020. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 323:1239–1242. 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 24.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, Cao B. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395:497–506. 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z. 2020. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323:1061–1069. 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, Xiang J, Wang Y, Song B, Gu X, Guan L, Wei Y, Li H, Wu X, Xu J, Tu S, Zhang Y, Chen H, Cao B. 2020. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 395:1054–1062. 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang X, Yu Y, Xu J, Shu H, Xia J, Liu H, Wu Y, Zhang L, Yu Z, Fang M, Yu T, Wang Y, Pan S, Zou X, Yuan S, Shang Y. 2020. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 8:475–481. 10.1016/S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.De Groot AS, Scott DW. 2007. Immunogenicity of protein therapeutics. Trends Immunol 28:482–490. 10.1016/j.it.2007.07.011. [DOI] [PubMed] [Google Scholar]
- 29.Hansel TT, Kropshofer H, Singer T, Mitchell JA, George AJ. 2010. The safety and side effects of monoclonal antibodies. Nat Rev Drug Discov 9:325–338. 10.1038/nrd3003. [DOI] [PubMed] [Google Scholar]
- 30.Kernstock R, Sperinde G, Finco D, Davis R, Montgomery D. 2020. Clinical immunogenicity risk assessment strategy for a low risk monoclonal antibody. AAPS J 22:60. 10.1208/s12248-020-00440-5. [DOI] [PubMed] [Google Scholar]
- 31.Xue L, Clements-Egan A, Amaravadi L, Birchler M, Gorovits B, Liang M, Myler H, Purushothama S, Manning MS, Sung C. 2017. Recommendations for the assessment and management of pre-existing drug-reactive antibodies during biotherapeutic development. AAPS J 19:1576–1586. 10.1208/s12248-017-0153-x. [DOI] [PubMed] [Google Scholar]
- 32.van de Poll-Franse LV, Houterman S, Janssen-Heijnen ML, Dercksen MW, Coebergh JW, Haak HR. 2007. Less aggressive treatment and worse overall survival in cancer patients with diabetes: a large population based analysis. Int J Cancer 120:1986–1992. 10.1002/ijc.22532. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental tables and figures. Download AAC.01063-21-s0001.pdf, PDF file, 0.3 MB (265.2KB, pdf)
Data Availability Statement
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.