Abstract
Objective:
The object of this study is to examine factors and symptoms associated with low-lying IUDs as defined by ultrasound.
Study Design:
This is a cross-sectional sub-study of participants in the Study of Environment, Life-style, and Fibroids (SELF). SELF participants had screening ultrasounds for fibroids at study enrollment; those with an IUD in place are included in this sub-study. Low-lying IUDs were identified and localized. Logistic regression was used to identify factors and symptoms associated with low-lying IUDs.
Results:
Among 168 women with IUDs at ultrasound, 28 (17%) had a low-lying IUD. Having a low-lying IUD was associated with low education level (≤high school: aOR 3.1 95% CI 1.14-8.55) and with increased BMI (p=0.002). Women with a low-lying IUD were more likely to report a “big problem” with dysmenorrhea (the highest option of the Likert scale) as compared to women with a normally-positioned IUD (OR 3.2 95% CI 1.07-9.54).
Conclusion:
Our study found that women with a low-lying IUD are more likely to be of lower education and higher BMI, and to report more dysmenorrhea.
Implications:
Women who are obese may benefit from additional counseling and closer follow-up after IUD placement. Future research is warranted to investigate IUD placement and possible IUD migration among women who are obese.
Keywords: Intrauterine contraception device, Low-lying, malposition, dysmenorrhea, obesity, expulsion
1. Introduction
The use of long acting reversible contraception (LARC) has steadily risen from 8.5% in 2009 to 11.6% in 2012 in the U.S.; this has been largely due to the increasing popularity of the intrauterine device (IUD) [1, 2]. IUDs provide highly effective contraception, and levonorgestrel IUDs also treat heavy menstrual bleeding [3-5]. However, some women will experience IUD expulsion or IUD displacement [6-9] even if the IUD was positioned appropriately in the fundus at the time of insertion [10]. There have been prior studies on risk factors for IUD malposition [7, 9, 11-17]. However, the types of malpostition varied; they included expulsions, low-lying or partially expelled IUDs, IUD perforations, and/or embedded/rotated IUDs and often unspecified combinations of these. While some research suggests that many low-lying and/or abnormally-located IUDs may resolve spontaneously [10, 18, 19], other studies have observed an increased risk of expulsions [8, 20]. Data also suggest that low-lying IUDs may contribute to pelvic pain [6, 8, 21] and reduced contraceptive efficacy has been reported for copper IUDs [22, 23]. In the current study, we examined factors associated with well-defined, low-lying IUDs as diagnosed by ultrasound.
We identified low-lying IUDs, defined as IUDs located in the lower uterine segment and/or cervix, during a screening ultrasound examination systematically conducted at study enrollment for a large prospective study of uterine fibroid development [24]. Study participants using IUDs constitute the sample for this current, cross-sectional study. Because participants in the parent study underwent ultrasound examination regardless of symptoms, this study has the unique advantage of allowing us to assess pelvic pain symptoms associated with low-lying IUDs without bias from selective referral for follow-up of IUD position.
2. Materials and Methods
2.1. Participants
The parent study, the Study of Environment, Lifestyle & Fibroids (SELF), is designed to investigate risk factors for fibroid development including fibroid incidence and fibroid growth. Women were eligible for enrollment in SELF if they were between the ages of 23-34 self-identified as African-American or black, had an intact uterus, resided in the U.S., and were willing to complete study activities over a five-year period [24]. Women who had a prior diagnosis of uterine fibroids, radiation or chemotherapy for cancer, or a diagnosis of lupus, Grave’s disease, Sjogren’s syndrome, scleroderma, or multiple sclerosis that required medication were not eligible for SELF. Institutional Review Boards at the National Institute of Environmental Health Sciences and Henry Ford Health System, the collaborating group in Detroit, approved the parent study. The current analysis includes all SELF participants with IUDs in place at the time of enrollment.
2.2. Data Collection
We published details of the SELF protocol elsewhere [24]. Participants usually completed a telephone interview and self-administered questionnaires prior to attending a clinic visit. Participants who had not completed the questionnaires prior to the clinic visit did so at their clinic visit. Trained interviewers conducted the computer-assisted telephone interviews to provide uniformly-collected data on reproductive and contraceptive history. Data included number of prior IUDs, type, age at insertion(s), and reasons for use. A web-based questionnaire elicited demographic and medical history data including dysmenorrhea over the past 12 months. Women reported how much of a problem they had with menstrual cramps or discomfort using the following Likert scale: not a problem, small problem, medium problem, big problem. Women also reported if their menstrual cramps or discomfort interfered with daily activities: not at all, a little, some, a lot.
At the clinic visit study staff measured weight and height. Experienced gynecologic sonographers who were trained on the study protocol conducted a 2-D transvaginal ultrasound examination. They recorded uterine position as anteverted or retroverted, and uterine size as measured in duplicate (sagittal, longitudinal, and transverse measures). Uterine volume was calculated for each duplicate set of measures with the ellipsoid formula, and averaged. The sonographer noted the presence of any low-lying IUDs, those located in the lower segment and/or cervix (Figure 1, for example), and study staff informed the participant. Two study authors (MM, ED) used the stored images to confirm the position of the low-lying IUDs and to document lower uterine segment versus cervical location. They also independently measured the distances from the fundus to the IUD for all low-lying IUDs.
Figure 1:
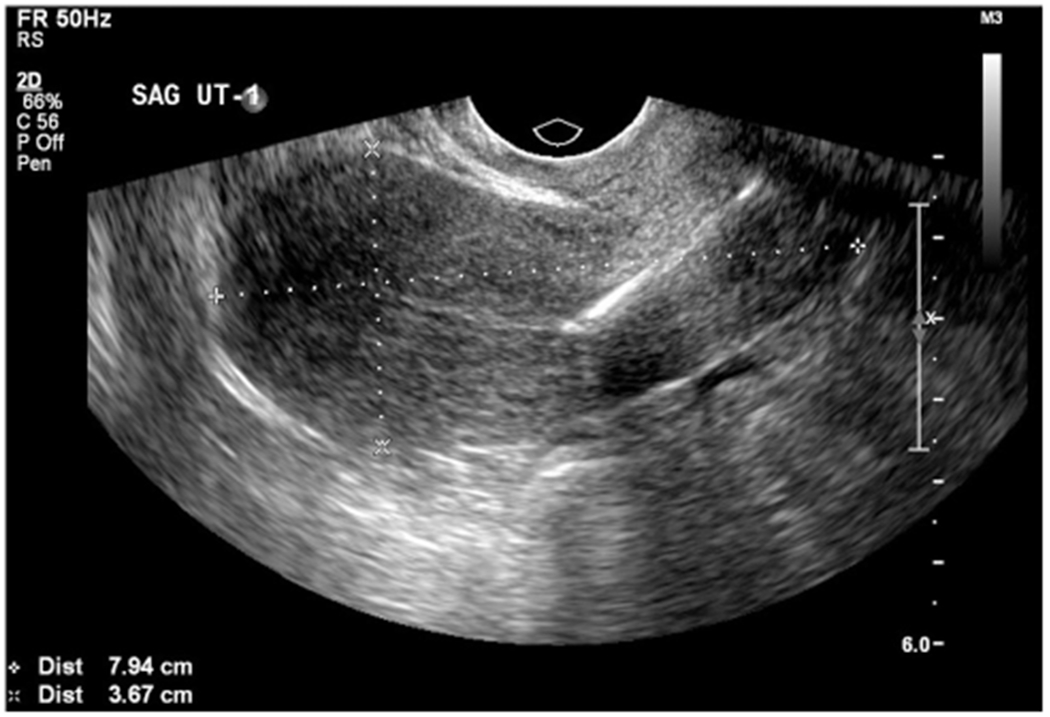
Example of a low-lying IUD from a SELF participant.
2.3. Data Analysis
We calculated the prevalence odds ratio (OR) for low-lying IUDs associated with each participant characteristic using univariate logistic regression. The factors of interest for which we had data were age, education, body mass index (BMI), parity, retroverted uterus, uterine volume, fibroid status, and type of IUD. Data on insurance status was also available for a subset of the participants, but since it was highly correlated with education, only education level was examined. Age, BMI, and uterine volume were analyzed as continuous variables as well as categorically. When possible, we categorized variables for analysis so that each category had at least 5 low-lying IUDs. Exceptions due to small numbers (categories of parity, fibroid status in Table 2, and BMI in Figure 2) are noted with the results. We dichotomized the education variable to ≤ high school vs > high school because we were particularly interested in the effect of low education. To examine BMI categorically, we initially dichotomized it (<35/≥35). Then, to further assess any dose-response relationship between BMI and low-lying IUDs, we examined BMI using Centers for Disease Control obesity guidelines [25]. However, due to low frequencies of women with a low-lying IUD among non-obese women, we evaluated BMI using the categories of <30, 30-<35, 35-<40, and ≥40. We used multivariable logistic regression models to simultaneously examine all variables that were significantly associated with low-lying IUDs, and kept variables that changed the association for another significant factor by at least 10%. We repeated the analysis looking at the association between significant factors after excluding the 3 participants whose IUD was low-lying but not in the cervix.
Table 2:
Associations between baseline characteristics and low-lying IUD position (N=168)
| OR (95% CI) N=28 |
aOR (95% CI) N=140 |
P-valuea | |
|---|---|---|---|
| Age at IUD insertion | |||
| Continuous (years) | 0.9 (0.83, 1.07) | 1.0 (0.86, 1.12) | 0.75 |
| Categorical | |||
| 20-26 | 1.0 (ref) | 1.0 (ref) 0.7 (0.30, 1.70) |
0.45 |
| 27-34 | 0.7 (0.29, 1.47) | ||
| Education | |||
| ≤High school or GED | 2.9 (1.10, 7.59) | 3.1 (1.14, 8.55) | 0.03 |
| >High school or GED | 1.0 (ref) | 1.0 (ref) | |
| Body mass index (kg/m2) | |||
| Continuous (1 unit) | 1.1 (1.03, 1.13) | 1.1 (1.03, 1.14) | 0.002 |
| Categorical | |||
| <35 | 1.0 (ref) | 1.0 (ref) 3.0 (1.26, 7.20) |
0.01 |
| ≥35 | 3.1 (1.30, 7.28) | ||
| Parity b | |||
| 0 | 1.0 (ref) | 1.0 (ref) | 0.34 |
| ≥ 1 | 0.6 (0.15, 2.26) | 0.5 (0.12, 2.29) | |
| Retroverted uterus | |||
| No | 1.0 (ref) | 1.0 (ref) | 0.76 |
| Yes | 1.1 (0.36, 3.04) | 1.2 (0.39, 3.69) | |
| Uterine volume (cc) | |||
| Continuous (1cc) | 1.0 (1.00, 1.01) | 1.0 (1.00, 1.01) | 0.15 |
| Categorical (quartiles) | |||
| 41-82 | 1.0 (ref) | 1.0 (ref) | 0.31 |
| 83-107 | 1.7 (0.52, 5.84) | 2.6 (0.72, 9.56) | |
| 108-136 | 1.0 (0.27, 3.75) | 1.0 (0.26, 4.20) | |
| 2.3 (0.72, 7.47) | 2.3 (0.67, 7.93) | ||
| 137-401 | |||
| Fibroids at enrollmen b | |||
| No | 1.0 (ref) | 1.0 (ref) 0.6 (0.15, 2.10) |
0.39 |
| Yes | 0.6 (0.16, 2.00) | ||
| Type of current IUD | |||
| Mirena® | 1.0 (ref) | 1.0 (ref) 1.1 (0.41, 2.79) |
0.88 |
| Paragard® | 1.1 (0.45, 2.74) |
OR: Odds Ratio, 95% CI: 95% Confidence Interval, aOR: Odds Ratio adjusted for continuous BMI and education, except BMI variables were only adjusted for education and education was only adjusted for continuous BMI.
p-value for overall effect of variable;
Results based on limited sample size (one of the categories had only 3 low-lying IUDs).
Figure 2:
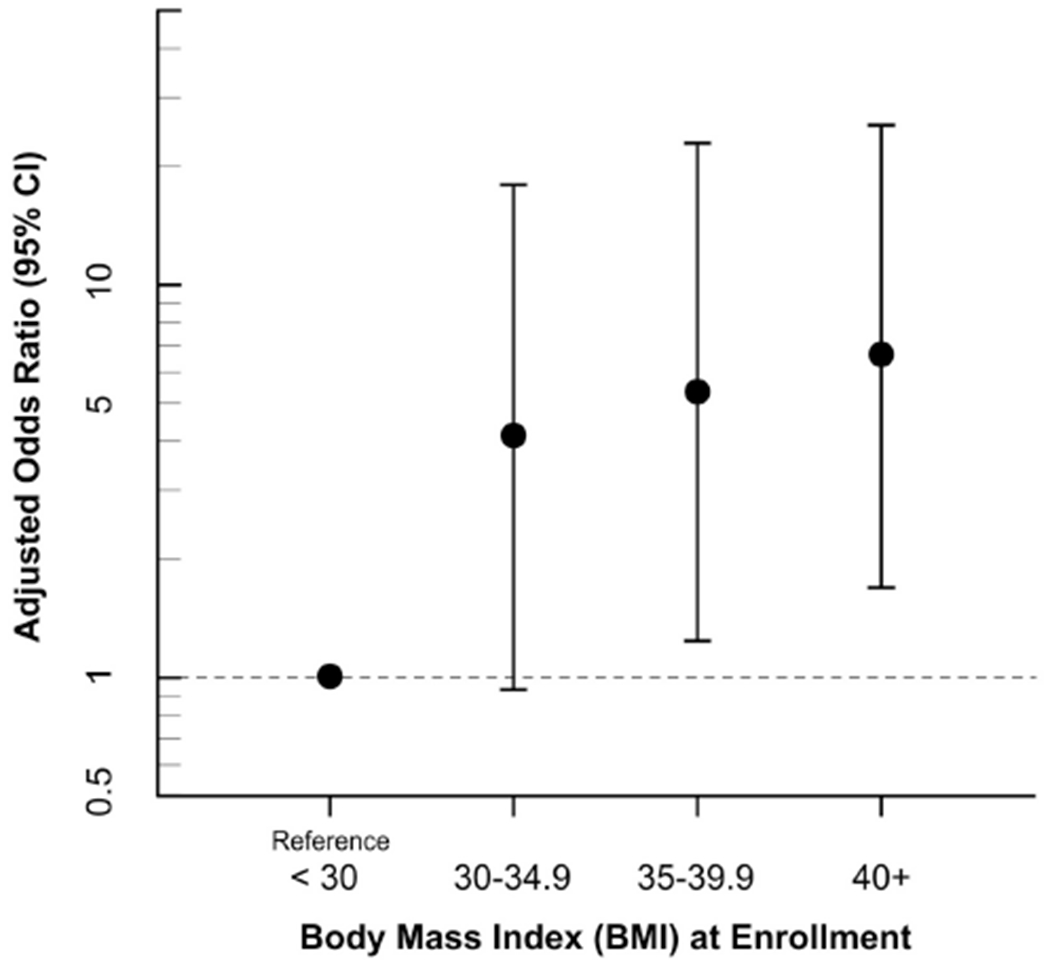
Dose-response relationship between body mass index and having a low-lying IUD (n = 168, adjusted for education, reference category sample is limited (only 3 low-lying IUDs).
We examined the association between having a low-lying IUD and dysmenorrhea based on two dichotomized menstrual-pain variables: 1) menstrual pain reported to be a big problem vs. not a big problem and 2) menstrual pain that interfered with daily activities some or a lot vs. none or a little. We used logistic regression to calculate the odds ratio for the association between a low-lying IUD and dysmenorrhea. To evaluate possible bias that could arise if women with a low-lying IUD were more likely to use an IUD as a possible way of reducing dysmenorrhea, we examined reported reasons for using the IUD.
Analyses were performed using SAS software version 9.3 [26].
3. Results
3.1. Low-lying IUDs: prevalence and risk factors.
Of the 1693 women enrolled in SELF, 168 (10%) had an IUD currently in place. These current IUD users were mostly first-time users (89%). The average length of use at the time of enrollment was 2.2 years (range <1 to 8), as estimated by subtracting age at insertion from age at enrollment. Twenty-eight of the 168 women (17%) had a low-lying IUD; those with and without a low-lying IUD had their IUD inserted at similar ages (26.1 years vs 26.8 years). Twenty-five of the low-lying IUDs were located at least partially in the cervix, and all of the low-lying IUDs were greater than 2 cm from the fundus, a distance which would have been considered low enough for removal for many studies assessing IUD malposition [15, 20, 21].
Table 1 shows descriptive characteristics of participants as a group and by IUD position. The majority of participants were educated beyond high school, had BMIs in the overweight or obese categories, and were parous. Nearly three quarters were using the Mirena IUD. The sample of women with a low-lying IUD had a higher proportion of women who were young, less educated, in higher BMI categories, and with larger uteri compared with normally-positioned IUD users. The two groups were similar in proportions of parity, retroverted uterine position, fibroids status, and IUD type. The two statistically important factors associated with low-lying IUD position were lower education and higher BMI (Table 2). Women with no more than a high school education had an adjusted odds ratio of having a low-lying IUD of 3.1 (95% CI 1.14-8.55). As BMI increased (using the continuous measure of BMI), so did the odds of having a low-lying IUD (p=0.002). We observed a dose-response pattern using the following BMI categories (<30reference, 30-<35, 35-<40, ≥40). The aOR increased from 4.1 (95% CI 0.94-17.78) to 6.6 (1.71-25.24) (Figure 2). The analysis excluding participants whose IUDs were low-lying but not in the cervix (n=3) showed essentially the same results (data not shown).
Table 1:
Characteristics of participants by position of IUD (N=168)
| Analysis Population N=168 | Low-lying IUD N=28 | Normally positioned IUD N=140 | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| N | % | N | (%) | N | (%) | |
| Age at IUD insertion (years) | ||||||
| 20-26 | 81 | 48 | 16 | 57 | 65 | 46 |
| 27-34 | 87 | 52 | 12 | 43 | 75 | 54 |
| Education | ||||||
| ≤High school or GED | 143 | 85 | 8 | 29 | 17 | 12 |
| >High school or GED | 25 | 15 | 20 | 71 | 123 | 88 |
| Body mass index (kg/m2) | ||||||
| <25 | 22 | 13 | 2 | 7 | 20 | 14 |
| 25-<30 | 37 | 22 | 1 | 4 | 36 | 26 |
| 30-<35 | 33 | 20 | 6 | 21 | 27 | 19 |
| 35-<40 | 30 | 18 | 7 | 25 | 23 | 16 |
| 40+ | 46 | 27 | 12 | 43 | 34 | 24 |
| Parity | ||||||
| 0 | 12 | 7 | 3 | 11 | 9 | 6 |
| ≥ 1 | 156 | 93 | 25 | 89 | 131 | 94 |
| Retroverted uterus | ||||||
| No | 139 | 83 | 23 | 82 | 116 | 83 |
| Yes | 29 | 17 | 5 | 18 | 24 | 17 |
| Uterine volume (cc, quartiles) | ||||||
| 41-82 | 42 | 25 | 5 | 18 | 37 | 26 |
| 83-107 | 42 | 25 | 8 | 29 | 34 | 24 |
| 108-136 | 42 | 25 | 5 | 18 | 37 | 26 |
| 137-401 | 42 | 25 | 10 | 36 | 32 | 23 |
| Fibroids at enrollment | ||||||
| No | 140 | 83 | 25 | 89 | 115 | 82 |
| Yes | 28 | 17 | 3 | 11 | 25 | 18 |
| Type IUD | ||||||
| Mirena® | 123 | 73 | 20 | 71 | 103 | 74 |
| Paragard® | 45 | 27 | 8 | 29 | 37 | 26 |
3.2. Low-lying IUDs and dysmenorrhea
Women with a low-lying IUD were more likely to report a “big problem” with dysmenorrhea in the past 12 months than women with a normally-positioned IUD (OR 3.2 95% CI 1.07-9.54) (Table 3). Although proportionately more women with a low-lying IUD reported dysmenorrhea that interfered with activities of daily living, the association was not statistically significant (Table 3). We found that women with a low-lying IUD were not more likely than those with normally-positioned IUDs to report choosing the IUD to alleviate menstrual pain symptoms (7.1% versus 8.6%, P=0.79, based on chi-square test), suggesting that the increased dysmenorrhea in the group with low-lying IUDs was not due to problems with dysmenorrhea prior to IUD insertion.
Table 3:
Dysmenorrhea among participants with a low-lying IUD compared to normally positioned IUD at time of enrollment (N=168)
| IUD position | Dysmenorrhea in past 12 months | ||||
|---|---|---|---|---|---|
|
| |||||
| None or Medium Problem N=151 | Big Problem N=17 | OR (95% CI) | |||
| N | % | N | % | ||
| Normally positioned | 129 | 85 | 11 | 65 | 1.0 (ref) |
| Low-lying | 22 | 15 | 6 | 35 | 3.2 (1.07, 9.54) |
|
| |||||
| IUD position | Dysmenorrhea interferes with daily activities in past 12 months | ||||
|
| |||||
| None or A Little | Some or A Lot | OR (95% CI) | |||
| N=142 | N=26 | ||||
| N | % | N | % | ||
| Normally positioned | 120 | 85 | 20 | 77 | 1.0 (ref) |
| Low-lying | 22 | 16 | 6 | 23 | 1.6 (0.59, 4.54) |
3. Discussion
In our study of young African-American women, increased BMI was strongly associated with having a low-lying IUD and showed a dose-response pattern. One fourth of IUD users with a BMI ≥35 had a low-lying IUD. This BMI category is no longer rare. Based on National Health and Nutrition Examination Survey data, 15% of all reproductive-age women 20-39 and 31% of African-American women of these ages have BMIs ≥35 [27]. When we examined the association with finer categories of BMI, an increased risk appeared to begin with level 1 obesity (BMI=30-<35). However, our small sample size precluded looking at overweight women as a separate category.
To our knowledge, BMI has been examined in three other IUD malposition/expulsion studies. In a U.S. study Madden et al. [9] studied risk factors associated with complete and partial expulsions among 5,403 reproductive-age women. The IUD position data were based on women’s self-report gathered during phone interviews or clinic contact during a 2-year follow-up. Complete and partial expulsions were combined in their analysis. The authors reported increased expulsion rates associated with BMI ≥30. A study conducted in Finland, which identified only complete expulsions, reported a significantly-elevated relative odds of expulsion for BMI >30 [14]. Additionally, Saito-Tom et al. [28] found that Hawaiian women with a BMI over 40 were 3 times more likely to expel their LNG-IUD compared to women with a BMI of <35. The mechanism(s) by which obesity might increase risk of a low-lying IUD is unknown and is worthy of further research. Obesity could make initial placement more difficult. It is also possible that factors associated with obesity, such as differing hormone levels, might influence migration. We are not aware of any studies that have examined BMI-related factors as potential risk factors for IUD migration.
The other factor significantly associated with a low-lying IUD was having no more than a high school education. This association is consistent with prior studies evaluating factors that reflect socioeconomic status and IUD expulsion/malposition [7, 9]. Education level may be a surrogate for less access to care, or care by less experienced providers, an observed risk factor for adverse events during and after IUD insertion in some studies [11, 29], but not all [21].
We also examined age, parity, retroverted uterine position, uterine volume, fibroid status, and IUD type. None were significantly associated with low-lying IUD position. However, given the narrow age-range of participants and our sample size of only 12 nulliparous women, our ability to investigate these factors was limited.
The primary strength of our study is the systematic ultrasound screening for detection of the low-lying IUDs. This allowed us to fill an important research gap in the data on possible dysmenorrhea associated with abnormally-positioned IUDs. Our data from women who were screened regardless of symptoms, demonstrates that the link between abnormal IUD position and pelvic pain that has previously been reported [6, 8, 21], is unlikely to be an artifact of selective self-referral among symptomatic women. Also, future studies of risk factors may benefit from more precise definitions of IUD position that can be done with ultrasound data, because partial IUD expulsions and complete expulsions may differ in their risk factors.
The primary limitation of our study was the small number of cases. We could not investigate IUD type when looking at BMI given that our sample included only 8 copper IUD users with low-lying IUDs. Nor could we adjust for potential confounding in the dysmenorrhea analysis. In addition, some IUDs that are low-lying in the uterus may spontaneously migrate to a normal fundal position [10, 18, 19], but we only had a single measure of IUD position.
3.1. Conclusion
Our study adds to the evidence that high BMI is a risk factor for low-lying IUDs [9, 14, 28]. The American College of Obstetricians and Gynecologists (ACOG) states that LARC is the most effective reversible contraception, and can be offered to the majority of women regardless of BMI [30, 31]. Our findings should not be considered as a contraindication for IUD use among women with high BMI. However, women with high BMIs may benefit from additional counseling and follow-up regarding risk of dysmenorrhea and expulsion.
Acknowledgements
We thank Dr. Christie Barker-Cummings, SELF study manager, and the SELF Teams at both Henry Ford Health System and at Social & Scientific Systems, Inc. Drs. Janet Hall and Allen Wilcox provided helpful comments on an earlier version of the manuscript.
Funding
This research was supported by the Intramural Research Program of the National Institute of Health, National Institute of Environmental Health Sciences [grant number Z01ES0490003] and in part by funds allocated for health research by the American Recovery and Reinvestment Act.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
All authors declare no conflict of interest.
References:
- [1].Branum AM, Jones J. Trends in long-acting reversible contraception use among U.S. women aged 15-44. NCHS Data Brief 2015:1–8. [PubMed] [Google Scholar]
- [2].Kavanaugh ML, Jerman J, Finer LB. Changes in use of long-acting reversible contraceptive methods among U.S. women, 2009-2012. Obstet Gynecol 2015;126:917–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Imai A, Matsunami K, Takagi H, Ichigo S. Levonorgestrel-releasing intrauterine device used for dysmenorrhea: five-year literature review. Clin Exp Obstet Gynecol 2014;41:495–8. [PubMed] [Google Scholar]
- [4].Zapata LB, Whiteman MK, Tepper NK, Jamieson DJ, Marchbanks PA, Curtis KM. Intrauterine device use among women with uterine fibroids: a systematic review. Contraception 2010;82:41–55. [DOI] [PubMed] [Google Scholar]
- [5].Adeyemi-Fowode OA, Santos XM, Dietrich JE, Srivaths L. Levonorgestrel-releasing intrauterine device use in female adolescents with heavy menstrual bleeding and bleeding disorders: single institution review. J Pediatr Adolesc Gynecol 2017;30:479–83. [DOI] [PubMed] [Google Scholar]
- [6].Benacerraf BR, Shipp TD, Bromley B. Three-dimensional ultrasound detection of abnormally located intrauterine contraceptive devices which are a source of pelvic pain and abnormal bleeding. Ultrasound Obstet Gynecol 2009;34:110–5. [DOI] [PubMed] [Google Scholar]
- [7].Braaten KP, Benson CB, Maurer R, Goldberg AB. Malpositioned intrauterine contraceptive devices: risk factors, outcomes, and future pregnancies. Obstet Gynecol 2011;118:1014–20. [DOI] [PubMed] [Google Scholar]
- [8].Gupta S, Malik S, Sinha R, Shyamsunder S, Mittal MK. Association of the position of the Copper T 380a as determined by the ultrasonography following its insertion in the immediate postpartum period with the subsequent complications: an observational study. J Obstet Gynaecol India 2014;64:349–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Madden T, McNicholas C, Zhao Q, Secura GM, Eisenberg DL, Peipert JF. Association of age and parity with intrauterine device expulsion. Obstet Gynecol 2014;124:718–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Shimoni N, Davis A, Westhoff C. Can ultrasound predict IUD expulsion after medical abortion? Contraception 2014;89:434–9. [DOI] [PubMed] [Google Scholar]
- [11].Aoun J, Dines VA, Stovall DW, Mete M, Nelson CB, Gomez-Lobo V. Effects of age, parity, and device type on complications and discontinuation of intrauterine devices. Obstet Gynecol 2014;123:585–92. [DOI] [PubMed] [Google Scholar]
- [12].Grimes DA, Lopez LM, Schulz KF, Stanwood NL. Immediate postabortal insertion of intrauterine devices. Cochrane Database Syst Rev 2010:CD001777. [DOI] [PubMed] [Google Scholar]
- [13].Grimes DA, Lopez LM, Schulz KF, Van Vliet HA, Stanwood NL. Immediate post-partum insertion of intrauterine devices. Cochrane Database Syst Rev 2010:CD003036. [DOI] [PubMed] [Google Scholar]
- [14].Kaislasuo J, Heikinheimo O, Lahteenmaki P, Suhonen S. Menstrual characteristics and ultrasonographic uterine cavity measurements predict bleeding and pain in nulligravid women using intrauterine contraception. Hum Reprod 2015;30:1580–8. [DOI] [PubMed] [Google Scholar]
- [15].Liang H, Li L, Yuan W, Zou Y, Gao ES, Duffy JM, et al. Dimensions of the endometrial cavity and intrauterine device expulsion or removal for displacement: a nested case-control study. BJOG 2014;121:997–1004. [DOI] [PubMed] [Google Scholar]
- [16].Shipp TD, Bromley B, Benacerraf BR. The width of the uterine cavity is narrower in patients with an embedded intrauterine device (IUD) compared to a normally positioned IUD. J Ultrasound Med 2010;29:1453–6. [DOI] [PubMed] [Google Scholar]
- [17].Zhang J, Feldblum PJ, Chi IC, Farr MG. Risk factors for copper T IUD expulsion: an epidemiologic analysis. Contraception 1992;46:427–33. [DOI] [PubMed] [Google Scholar]
- [18].Faundes D, Perdigao A, Faundes A, Bahamondes L, Petta CA. T-shaped IUDs accommodate in their position during the first 3 months after insertion. Contraception 2000;62:165–8. [DOI] [PubMed] [Google Scholar]
- [19].Morales-Rosello J Spontaneous upward movement of lowly placed T-shaped IUDs. Contraception 2005;72:430–1. [DOI] [PubMed] [Google Scholar]
- [20].Petta CA, Faundes D, Pimentel E, Diaz J, Bahamondes L. The use of vaginal ultrasound to identify copper T IUDs at high risk of expulsion. Contraception 1996;54:287–9. [DOI] [PubMed] [Google Scholar]
- [21].de Kroon CD, van Houwelingen JC, Trimbos JB, Jansen FW. The value of transvaginal ultrasound to monitor the position of an intrauterine device after insertion. A technology assessment study. Hum Reprod 2003;18:2323–7. [DOI] [PubMed] [Google Scholar]
- [22].Anteby E, Revel A, Ben-Chetrit A, Rosen B, Tadmor O, Yagel S. Intrauterine device failure: relation to its location within the uterine cavity. Obstet Gynecol 1993;81:112–4. [PubMed] [Google Scholar]
- [23].Inal MM, Ertopcu K, Ozelmas I. The evaluation of 318 intrauterine pregnancy cases with an intrauterine device. Eur J Contracept Reprod Health Care 2005;10:266–71. [DOI] [PubMed] [Google Scholar]
- [24].Baird DD, Harmon QE, Upson K, Moore KR, Barker-Cummings C, Baker S, et al. A prospective, ultrasound-based study to evaluate risk factors for uterine fibroid incidence and growth: methods and results of recruitment. J Womens Health (Larchmt) 2015;24:907–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Centers for Disease Control and Prevention. Defining overweight & obesity 2016, https://www.cdc.gov/obesity/adult/defining.html [accessed 10.09.17].
- [26].SAS Institute Inc., Base SAS 9.3, Cary, NC: SAS Institute Inc., 2002–2010. [Google Scholar]
- [27].Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014;311:806–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Schneider ME. Beware hormonal IUD expulsion in obese women. Ob Gyn News 2017. [Google Scholar]
- [29].Farmer M, Webb A. Intrauterine device insertion-related complications: can they be predicted? J Fam Plann Reprod Health Care 2003;29:227–31. [DOI] [PubMed] [Google Scholar]
- [30].American College of Obstetricians and Gynecologists. ACOG practice bulletin No. 121: long-acting reversible contraception: Implants and intrauterine devices. Obstet Gynecol 2011;118:184–96. [DOI] [PubMed] [Google Scholar]
- [31].Curtis KM, Tepper NK, Jatlaoui TC, Berry-Bibee E, Horton LG, Zapata LB, et al. U.S. medical eligibility criteria for contraceptive use, 2016. MMWR Recomm Rep 2016;65:1–103. [DOI] [PubMed] [Google Scholar]


