Abstract
Purpose
During the first few months of the COVID-19 outbreak, healthcare workers (HCW) faced levels of personal risk, emotional distress, and professional strain not seen in their lifetimes. This study described how these stressors influenced various aspects of their sleep patterns.
Methods
From May 19 to June 20, 2020, an electronic, cross-sectional survey was administered to a convenience sample of in- and outpatient HCW in a large, nonprofit healthcare system. Respondents described the pandemic’s initial impact on personal and professional life and various sleep dimensions: regularity, efficiency, duration, timing, quality, and daytime sleepiness.
Results
Two hundred seven providers responded, representing 17 different healthcare roles. Most (82%) were women with a median age of 39 years (IQR1–3, 31–53). A majority of respondents (81%) worked in an inpatient setting, with half (46%) primarily on the “frontline.” Approximately one-third of respondents (37%) were physicians and one-quarter (28%) were nurses. Overall, 68% of HCW reported at least one aspect of sleep worsened during the beginning of the pandemic; the most impacted were daytime sleepiness (increased in 43%) and sleep efficiency (worse in 37%). After adjusting for COVID exposure and burnout, frontline providers had twofold higher odds of poor pandemic sleep, aOR 2.53, 95%CI 1.07–5.99. Among frontline providers, physicians were fivefold more likely to develop poor pandemic sleep compared to nurses (OR 5.73, 95%CI 1.15–28.57).
Conclusions
During the initial wave of COVID-19, a majority of HCW reported a decline in sleep with an increase in daytime sleepiness and insomnia. Frontline workers, specifically physicians, were at higher risk.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11325-021-02515-9.
Keywords: Pandemic, Sleep, Healthcare worker, Insomnia, COVID-19
Introduction
Well before the SARS-CoV-2 (COVID-19) pandemic, healthcare workers (HCW) in the USA were already suffering from poor sleep and high rates of professional burnout. A recently pooled data found that most (61%) nurses sleep poorly [1], and physicians, on average, get an inadequate amount of sleep due to professional demands [2]. Similarly, burnout affects at least 1 in 2 physicians [3] and is increasing in prevalence [4]. Inadequate sleep and professional burnout have been independently linked to poor patient and provider outcomes such as medical errors [5], and provider depression, substance abuse, and suicide [3, 6].
Unfortunately, these problems are likely magnified by the uncertainties of a once-in-a-century pandemic, including personal risk of infection and transmission to close contacts, shifting professional obligations, and financial instability [7]. Early international data found that burnout rates and poor sleep patterns among frontline HCW increased after only a few weeks of COVID-19 response in those countries with the largest initial outbreaks (China and Italy) [8, 9]. As the pandemic spread, studies in India [10], Bahrain [11], and the USA [12] have reported similar pandemic-related declines in mental health and sleep quality.
Few US studies have focused specifically on describing changes to HCW sleep patterns as the pandemic began to spread in this country. Furthermore, most HCW studies examine the pandemic impact specifically on frontline providers [12], despite the fact that outpatient practitioners are subject to similar (if not exaggerated) professional strain. Identifying HCW subpopulations who are especially vulnerable to sleep detriment, and its characterization, is necessary for the development of targeted interventions and preparation for future crises. Indeed, initiatives driving sleep and mental hygiene have been shown to have both immediate [13] and long-term consequences [14]. Even in the absence of a healthcare crisis, inadequate sleep impairs the immune system and attenuates vaccine response. As expected, data from the current outbreak found that HCW who slept an hour more than their peers had 12% lower odds of contracting COVID-19. Similarly, those with 3 or more sleep problems prior to the pandemic had 88% greater odds of catching COVID-19 [15]. Previous outbreaks have left lingering effects on the healthcare workforce in terms of post-traumatic stress and anxiety, sometimes for years [14]. The long-term effects on sleep in this and previous pandemics are not well described.
This observational, cross-sectional study was performed to describe changes in multiple aspects of sleep in HCWs in all roles during the first COVID-19 wave in one of the initial US epicenters, New York.
Material and methods
Study design and dissemination
This was an anonymous, cross-sectional survey accessed via an electronic link to the institution’s RedCap (Research Electronic Data Capture, LLC) website. The local Institutional Review Board approved the project with a modified consent process to protect subject anonymity.
Eligible participants included HCW of any provider role in a large, nonprofit healthcare system affiliated with the University at Buffalo. This system encompasses six distinct hospitals and numerous outpatient facilities. When the pandemic began in the area in March 2020, daily COVID updates were uploaded on institutional website homepages and concurrently emailed to staff. These updates served to highlight epidemiologic trends, identify an expanding resource pool, and (re-)organize staff around changing policies and chains of command. Email recipients included hospital employees, affiliated community providers, faculty physicians, and trainees. For three consecutive days in May (19–21) 2020, a brief description and electronic link to the survey were included in the body of these emails. As this was a survey intended to capture a convenience sample, no personalized invitations were extended. This methodology prohibited the calculation of a true response rate.
In the 3 weeks that the survey link was left open, local COVID prevalence was increasing by approximately one hundred cases, with roughly 10–15 deaths, each day. Buffalo-area schools and non-essential business were closed and elective surgeries had all been canceled, in accordance with the New York State mandates (in effect for approximately 10 weeks).
Survey content
Demographics collected included provider role, age, ethnicity, race, sex, relationship status, and number of children in the home. Respondents reported how the pandemic changed professional, childcare, and household responsibilities (survey included as Supplement 1). Participants were asked to report how often they exhibited healthy sleep habits across six domains: Regularity (“How often do you have a set sleep schedule?”), Duration (“How often do you get 6 to 8 h of sleep per day?”), Efficiency (“How often do you spend less than 30 min awake total while trying to sleep?”), Timing (“How often are you asleep between 2 and 4 am?”), Quality (“How often do you wake up refreshed?”) and Daytime Sleepiness (“How often do you stay awake all day without napping or dozing off?”) [16]. A six-point Likert scale was used to quantify frequency for both pre- and intra-pandemic sleep patterns, with a higher number indicative of more frequent healthy sleep patterns. This sleep health score was chosen for its brevity and efficiency in gauging multiple aspects of sleep when compared to using individual sleep questionnaires for insomnia, sleep quality, and sleepiness. This sleep health score has been validated in large population studies and has been shown to correlate well with other measures of sleep as well as daytime health [17–21].
A composite sleep health score was calculated for both pre- and intra-pandemic patterns by dividing the point total (maximum of 30) by the number of dimensions answered (maximum of 6). To our knowledge, even though validated thresholds exist for each individual sleep dimension [17], there are no validated thresholds of an aggregate sleep health score across all 6 dimensions that allow for good or poor sleep patterns. Utilizing an indexed composite allowed for statistical comparisons of pre- and intra-pandemic behaviors. An index of 3 (analogous to self-reporting healthy sleep at least “Often” for all dimensions) served as a cut-point in the stratification of respondents as “good” vs. “poor” sleepers. To exclude HCW who were “poor sleepers” pre-pandemic [1, 2], secondary analyses were performed without those with a pre-COVID index score less than 3. This was intended to identify HCW whose sleep was most impacted by the pandemic.
The survey contained screens for burnout, depression, and stress using an abridged Maslach Burnout Scale [22], 2-items from the Patient Health Questionnaire (PHQ), and a ten-item Perceived Stress Scale (PSS) [23], respectively. PSS scores above 12 indicated moderate to severe stress, as previously reported [23]. Frequency of habits known to impact sleep—screen time, alcohol, caffeine, and tobacco use before bed—were also elicited. Lastly, respondents were asked about occupational COVID exposure and infection status. No question was mandatory.
Statistical analysis
As an anonymous survey, answers were reviewed for plausibility but ensuring data reliability was not possible. Of note, all respondents answered more than one question so every response was included. Missing answers were omitted case-wise. Data were summarized as proportions of participants responding to each question. All aspects of professional and personal life changes that were investigated in the survey were compared between the groups described above (e.g., good versus poor sleepers, frontline providers versus others). Kruskal–Wallis or Mann–Whitney U tests compared non-parametric continuous data between categorical variables. Paired t-tests compared parametric data within participants from different time points. Chi-square and odds ratios with 95% confidence intervals compared categorical variables between groups. Any comparisons between groups that reached a p-value of 0.10 were included in logistic regression analyses to control for potential confounders affecting the measures of association. For clarity and brevity, not all analyses performed were presented here. Analyses were performed using IBM SPSS software, version 25 (Chicago, IL) with significance set at a p-value < 0.05 using two-sided comparisons.
Results
Study population
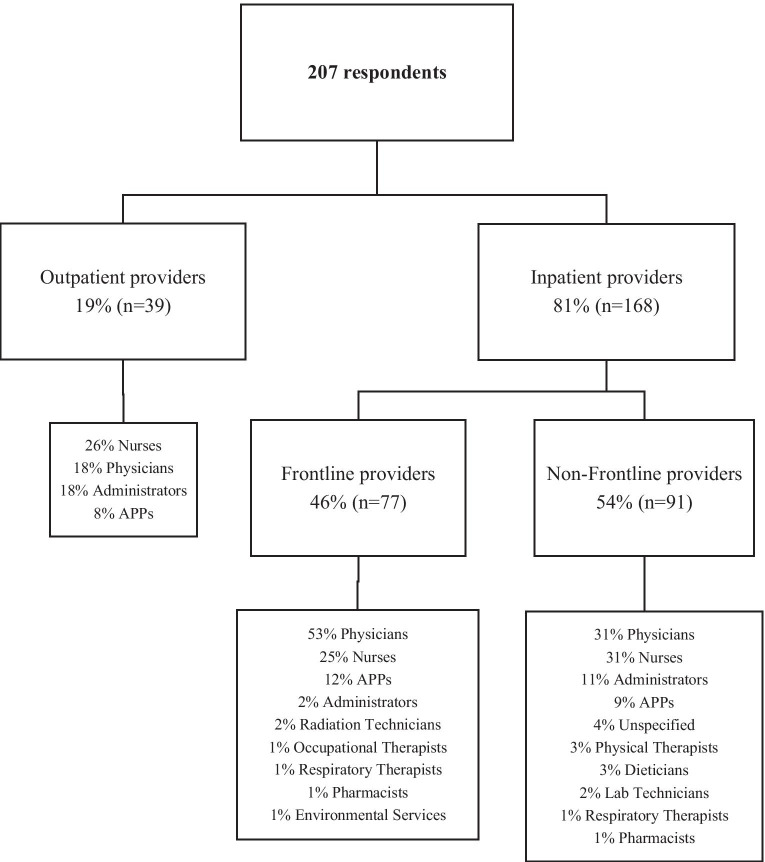
Among the 207 participants, the median age was 39 years (IQR1–3, 31–53) and mostly identified as White (89.7%) and female (82.3%). Figure 1 shows the respondent breakdown by work location (including inpatient, outpatient), and “frontline” status (defined as reporting a primary work location of an Emergency Room or Intensive Care Unit). Respondents did represent seventeen distinct roles (Table 1); however, physicians (36.7%) and nurses (27.5%) constituted the largest proportion of participants. Over half (58.2%) of respondents were married and many (42.6%) were primary caregivers to at least one child.
Fig. 1.
Breakdown of the participants’ healthcare work type and location during the first wave of the COVID-19 pandemic. Frontline providers are defined as those who reported working primarily in an emergency room or intensive care unit. APP = advanced practice provider
Table 1.
Demographics of healthcare workers responding to a survey on sleep health during the first wave of the COVID-19 pandemic in Buffalo, New York
| All respondents (n = 207) | ||
|---|---|---|
| Median age, in years | 39 (31–53) | |
| Female sex | 163/198 (82.3%) | |
| Race | White | 175/195 (89.7%) |
| African American | 8/195 (4.1%) | |
| Asian | 11/195 (5.6%) | |
| Relationship status | Single | 37/201 (18.4%) |
| Married | 117/201 (58.2%) | |
| Unmarried, dating | 35/201 (17.4%) | |
| Divorced or separated | 6/201 (3%) | |
| Healthcare role | Physician | 76 (36.7%) |
| Registered nurse | 57 (27.5%) | |
| Physician’s assistant or advanced nurse practitioner | 20 (9.7%) | |
| Radiology technician | 2 (1%) | |
| Laboratory technician | 5 (2.4%) | |
| Respiratory therapist | 3 (1.4%) | |
| Physical or occupational therapist | 5 (2.4%) | |
| Administration or registration staff | 19 (9.2%) | |
| Pharmacist | 2 (1%) | |
| Medical assistant | 1 (0.5%) | |
| Environmental service worker | 1 (0.5%) | |
| Registered dietician | 3 (1.4%) | |
| Other: Educator (n = 1), psychologist (n = 1), research staff (n = 2), social worker (n = 1), information technologist (n = 1), unspecified (n = 7) | 13 (6.3%) | |
| Physician role | Resident | 39/76 (51.3%) |
| Fellow | 4/76 (5.3%) | |
| Attending | 33/76 (43.4%) | |
| Work primarily in outpatient setting | 39/204 (18.8%) | |
| Work primarily in intensive care unit or emergency room | 77/203 (37.9%) | |
| Have at least 1 child for whom he/she is primary caregiver | 86/202 (42.6%) | |
Data are reported as median (IQR1–3) or frequency (column proportion) unless otherwise specified
The survey link was sent to an email distribution list of approximately 2000 emails including expired and redundant emails for the same person. Therefore, this study population is a convenience sample of an estimated 10–20% of the target population.
Sleep patterns before and during the pandemic
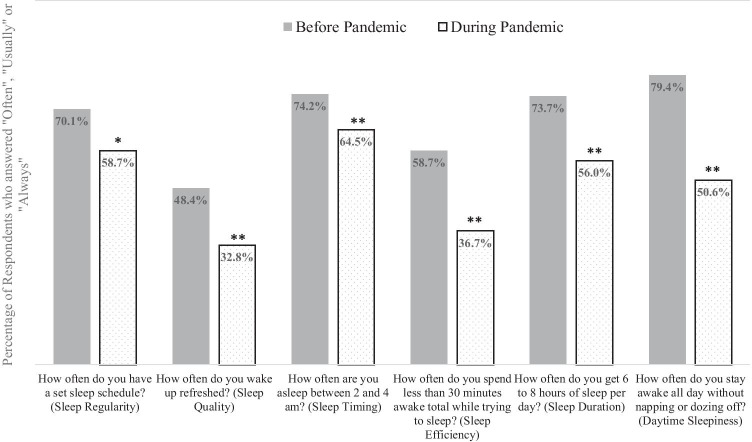
Before the pandemic, most HCWs reported good (i.e., “Often” through “Always”) sleep regularity (70.1%), efficiency (58.7%), duration (73.7%), and timing (74.2%), as well as a lack of daytime sleepiness (79.4%). Just under half of HCWs reported experiencing refreshing sleep “often” (48.4%). There was a significant decrease in the proportion of participants reporting frequent healthy sleep patterns during the beginning of the pandemic (Fig. 2). Over two-thirds (67.8%) had at least one sleep dimension worsen from pre-pandemic levels, with most (55%) having at least two. Nearly one in ten participants saw a decline in all six dimensions of sleep.
Fig. 2.
The comparison of the percentage of respondents who reported good sleep habits “Often” or more in each individual aspect of sleep before the pandemic and during the beginning of the COVID-19 pandemic. Differences from before the pandemic to during the first wave were all statistically significant when compared using chi-square testing, *p < 0.05, **p < 0.001
Two aspects of sleep saw the greatest intra-pandemic deterioration when compared to pre-COVID levels: excessive daytime sleepiness and sleep efficiency. While one-fifth of participants (20.6%) reported excessive daytime sleepiness before the pandemic, this doubled to nearly 1 in 2 (49.4%) during the pandemic (p < 0.001). Additionally, nearly half (42.6%) of all participants reported an increase in their frequency of daytime sleepiness during the pandemic. As a metric of insomnia, “sleep efficiency” declined in over one-third (37.4%) of respondents as the pandemic began. The number of HCW reporting good sleep efficiency “often” dropped from 58.7 to 36.7% (p < 0.001).
Poor sleep, defined as a composite sleep index less than 3, was found in 55% (n = 114) of all respondents when assessing intra-pandemic sleep behaviors. Excluding those with poor pre-pandemic sleep (n = 79, 38%), the comparison between those who maintained good sleep behaviors during the pandemic and those who deteriorated is shown in Table 2. Participants with higher odds of developing poor sleep habits were frontline (ICU/ER) workers (OR 2.16, 95%CI 1.01–4.61) and physicians (OR 3.30, 95%CI 1.57–6.94), especially resident physicians (OR 4.29, 95%CI 1.75–10.5). There was a trend towards poor sleep for those who reported a decrease in their work responsibilities, although this did not reach statistical significance (OR 2.15, 95%CI 0.95–4.88). Interestingly, those who indicated frequent alcohol use had significantly lower odds of poor pandemic sleep (OR 0.35, 95%CI 0.14–0.89).
Table 2.
Comparing healthcare workers with good pandemic sleep to those who developed poor pandemic sleep during the first wave of COVID-19
| Good pandemic sleep health (n = 76) | Poor pandemic sleep health (n = 52) |
p | Odds ratio for poor pandemic sleep health | ||
|---|---|---|---|---|---|
| Median age, in years | 42.5 (32–54.8) | 35 (31–49.8) | 0.124 | ||
| Female sex | 58/74 (78%) | 44/50 (88%) | 0.239 | ||
| Healthcare role | Physician | 21 (28%) | 29 (56%) | 0.107 comparing all roles | |
| Registered nurse | 22 (29%) | 10 (19%) | |||
| Respiratory therapist | 2 (3%) | 0 | |||
| Administration or registration | 12 (16%) | 3 (6%) | |||
| Physician’s assistant or advanced nurse practitioner | 6 (8%) | 4 (8%) | |||
| Radiology technician (n = 2), laboratory technician (n = 2), educator (n = 1), researcher (n = 1), environmental services worker (n = 1), social worker (n = 1), registered dietician (n = 2), information technologist (n = 1), other (n = 6) | 12 (16%) | 5 (10%) | |||
| Work primarily in intensive care unit or emergency room | 19/75 (25%) | 22 (42%) | 0.044 | OR 2.16 (95%CI 1.01–4.61, p = 0.046) | |
| Physicians as proportion of group total | 21 (28%) | 29 (56%) | 0.001 | OR 3.30 (95%CI 1.57–6.94, p = 0.002) | |
| Resident physicians as proportion of group total | 9 (12%) | 19 (37%) | 0.001 | OR 4.29 (95%CI 1.75–10.5, p = 0.001) | |
| Registered nurses as proportion of group total | 22 (29%) | 10 (19%) | 0.212 | ||
| Work primarily in outpatient setting | 20 (26%) | 8 (15%) | 0.142 | ||
| Reported daily COVID exposure | 18/72 (25%) | 15/50 (30%) | 0.541 | ||
| Tested COVID-positive | 10 (13%) | 3 (6%) | 0.144* | ||
| Relationship status | Single | 13/75 (17%) | 7 (14%) | 0.984 | |
| Married | 44/75 (59%) | 31 (60%) | |||
| Dating, unmarried | 13/75 (17%) | 10 (19%) | |||
| Divorced/separated | 2/75 (3%) | 2 (4%) | |||
| Race | White | 65/74 (88%) | 48/51 (94%) | 0.482 | |
| African American | 4/74 (5%) | 1/51 (2%) | |||
| Asian | 5/74 (7%) | 2/51 (4%) | |||
| How the pandemic has changed one’s job | No change | 13 (17%) | 14 (27%) | 0.181 | |
| Increased work | 17 (22%) | 11 (21%) | 0.870 | ||
| Decreased work | 14 (18%) | 17 (33%) | 0.064 | OR 2.15 (95%CI 0.95–4.88, p = 0.067) | |
| Changed primary work location | 18 (24%) | 8 (15%) | 0.252 | ||
| Changed job type | 13 (17%) | 4 (8%) | 0.099* | ||
| Now work primarily from home | 8 (11%) | 5 (10%) | 0.867* | ||
| Furloughed | 1 (1%) | 0 | 1.000* | ||
| Have at least 1 child for whom he/she is primary caregiver | 37/72 (51%) | 19 (37%) | 0.101 | ||
| Pandemic caused a change in child care | 18/37 (49%) | 12/19 (63%) | 0.303 | ||
| Providing child care affected the ability to do his/her job | 10/37 (27%) | 7/19 (37%) | 0.449 | ||
| Sleep health before the pandemic (out of a maximum score of 5) | 3.6 (± 0.7) | 3.9 (± 0.5) | 0.004 | ||
| Sleep health during the pandemic | 3.5 (± 0.5) | 2.0 (± 0.6) | < 0.001 | ||
| Insomnia before the pandemic | 3 (4%) | 4 (8%) | 0.360 | ||
| Anxiety before the pandemic | 20 (26%) | 16 (31%) | 0.582 | ||
| Depression before the pandemic | 19 (25%) | 12 (23%) | 0.803 | ||
| Screened positive for depression during the pandemic | 17/71 (24%) | 8/51 (16%) | 0.408 | ||
| Average PSS score | 18.5 (± 4.5) | 17.8 (± 5.2) | 0.414 | ||
| PSS Score > 13 (at least moderate stress) | 69 (91%) | 46 (89%) | 0.668 | ||
| Burnout symptoms weekly | 43/75 (57%) | 30/51 (59%) | 0.868 | ||
| Drinks alcohol “Often”, “Most days,” or “Every day” | 21/59 (36%) | 8/49 (16%) | 0.024 | OR 0.35 (95%CI 0.14–0.89, p = 0.028) | |
| Reports using tobacco with any frequency | 1/61 (2%) | 5/49 (10%) | 0.087 | ||
Data are shown as frequency (column proportion) unless otherwise specified, mean (± SD) or median (IQR1–IQR3). P-values were obtained using independent t-tests, one-sided *Fisher’s exact tests, or chi-square. Unadjusted odds ratios were obtained via logistic regression using those with good pandemic sleep health as the reference group. PSS perceived stress scale
After adjusting for significant differences in the groups, the sole variable independently associated with higher odds of poor pandemic sleep was “frontline” status (aOR 2.53, 95%CI 1.07–5.99). To control for the elevated COVID exposure and positive burnout screens seen in frontline providers, a logistic regression model found the association between being an ICU/ER worker and the development of poor sleep remained independent of these factors as well (aOR 2.48, 95%CI 1.01–6.09).
No statistically significant differences were found in the stress scores or frequency of burnout symptoms or depression symptoms in those with good pandemic sleep when compared to those with poor pandemic sleep (Table 2).
Personal and professional impact of the pandemic
Table 3 describes survey items relating to respondent perceptions of the impact of COVID-19. Self-reported difficulties during the pandemic were essentially universal (98% of respondents), as were changes in job requirements (81%). Nearly one-quarter (23%) of participants screened positive for depression, with the vast majority (91%) reporting an increase in the frequency of depressive emotions during the pandemic.
Table 3.
Description of the effects of the pandemic on healthcare workers’ lives during the first wave of COVID-19
| All respondents (n = 207) | ||
|---|---|---|
| How the pandemic has changed one’s job | Increased amount of time working | 55/206 (27%) |
| Decreased amount of time working | 46/206 (22) | |
| Changed the primary work location within healthcare building(s) (e.g., reassigned from clinics to inpatient ward) | 39/206 (19%) | |
| Changed primary work responsibilities (e.g., formerly in scheduling, now screener at hospital entrance) | 24/206 (12%) | |
| Charged with working primarily from home | 23/206 (11%) | |
| Furloughed | 3/206 (2%) | |
| The pandemic has not changed my job | 40/206 (19%) | |
| Reasons why the pandemic has been difficult | Concern about self/loved ones getting sick | 177 (86%) |
| Increased emotional stressors | 165 (80%) | |
| Increased work demands | 116 (56%) | |
| Increased technology use | 65 (31%) | |
| Increased home responsibilities | 65 (31%) | |
| Financial difficulties | 43 (21%) | |
| None—it has not been personally difficult | 5 (2%) | |
| Changed living arrangement to protect vulnerable family members | 20/205 (10%) | |
| Mental health questions: | ||
| Screened positive for depression | 44/191 (23%) | |
| The frequency of the depressive symptoms changed from before the pandemic | 40/44 (91%) | |
| Burnout symptoms weekly | 101/203 (50%) | |
| Burnout symptoms daily | 19/203 (9%) | |
| Average score on the 10-item Perceived Stress Scale (PSS) | 18.6 (± 4.6) | |
| PSS > 13 (at least moderate stress) | 189 (91%) | |
| Reported changes in all 10 PSS items since onset of pandemic | 105 (51%) | |
| Having frequent nightmares | 32/116 (28%) | |
| Of the respondents with at least one child to care for at home (n = 86): | ||
| The pandemic took away or changed child care plans | 45/86 (52%) | |
| There is not another adult in the home to help with child care | 14/85 (17%) | |
| Spending more than 15 min per day on helping with your children’s schooling or educational tasks | 53/86 (62%) | |
| Providing child care has impacted your ability to do job | 26/86 (30%) | |
Data are reported as mean (± SD) or frequency (column proportion) unless otherwise specified
Half (50%) of respondents reported weekly burnout symptoms. These HCW were more likely to be residents (OR 2.99, 95%CI 1.39–6.40), frontline providers (OR 1.87, 95%CI 1.04–3.34), and/or to report pre-pandemic depression (OR 2.01, 95%CI 1.00–4.03) or anxiety (OR 1.85, 95%CI 1.00–3.34).
The mean PSS score was 18.6 (± 4.6), with 91% of respondents scoring at least 13, indicative of at least moderate stress [23]. Every respondent reported changes to at least 1 PSS item during the pandemic and half (51%) reported that all ten items worsened.
Of respondents with children (n = 86), 52% reported a loss of childcare resources during the pandemic. About one-third (30%) indicated childcare changes had a negative impact on their work. One in ten respondents had to change their primary residence during the pandemic in an attempt to insulate family members from COVID; this was associated with fourfold higher odds of weekly burnout (OR 4.372, 95%CI 1.41–13.59).
Impact of the pandemic on sleep patterns of specific providers
Of the respondents who were inpatient providers, 46% were considered frontline. Most were physicians (53%), nurses (25%), or advanced practice providers (12%) (Fig. 1). Table 4 compares the responses of frontline HCWs with those of their colleagues. Frontline providers were twice as likely to indicate poor pandemic sleep (OR 2.65, 95%CI 1.40–5.02) and weekly burnout symptoms (OR 1.87, 95%CI 1.04–3.34). Among frontline workers, physicians saw a larger change in overall sleep, translating to fivefold higher odds of ICU/ER physicians meeting criteria for poor sleep compared to frontline nurses (OR 5.73, 95%CI 1.15–28.57).
Table 4.
Comparison of frontline providers (intensive care unit and emergency room) healthcare workers to other respondents during the first wave of the COVID-19 pandemic
| Non-frontline providers n = 126 |
Frontline providers n = 77 |
p | Unadjusted odds ratio | |
|---|---|---|---|---|
| Role | Rn = 36, MD = 35, APP = 10, Support staff = 45 | MD = 41, Rn = 19, APP = 9, Support staff = 8 | 0.016 | |
| Median age, in years | 40 (31.0–53.5) | 39 (31.3–53.0) | 0.749 | |
| Female sex | 94/117 (80%) | 66 (86%) | 0.336 | |
| Reported daily COVID exposure | 24/119 (20%) | 37/75 (49%) | < 0.001 | OR 3.854 (95%CI 2.04–7.29) |
| Reported having COVID | 11 (9%) | 14 (18%) | 0.047 | OR 2.323 (95%CI 0.99–5.42) |
| Average score on the perceived stress scale (PSS) | 18.8 (± 4.0) | 17.9 (± 5.7) | 0.232 | |
| Moderate level of stress (PSS > 13) | 117 (93%) | 68 (88%) | 0.269 | |
| Sleep health before the pandemic (scale of 0 to 5) | 3.3 (± 0.9) | 3.2 (± 0.9) | 0.572 | |
| Poor sleep before the pandemic | 41/115 (36%) | 28/71 (39%) | 0.604 | |
| Sleep health during the pandemic | 2.7 (± 0.9) | 2.5 (± 0.8) | 0.120 | |
| Poor sleep during the pandemic | 59/115 (51%) | 53/72 (74%) | 0.002 | OR 2.648 (95%CI 1.40–5.02) |
| Burnout at least weekly | 55/122 (45%) | 46/76 (61%) | 0.034 | OR 1.868 (95%CI 1.04–3.34) |
| Reported depression symptoms “Fairly” or “Very Often” | 25/115 (22%) | 17/72 (24%) | 0.765 | |
| Reported depression symptoms are new during the pandemic | 14/116 (12%) | 4/73 (6%) | 0.202* |
Data are presented as mean (± standard deviation), median (IQR1–3), or frequency (column proportion, unless otherwise notated). P-values were obtained using t-tests or chi-square or *Fischer’s exact tests. Odds ratios were calculated with the non-frontline HCW as the reference group. RN registered nurse, MD physician, APP advance practice provider
COVID infection rates and risk factors
A total of 25 respondents (12%) reported testing positive for COVID-19 before the closure of the survey on June 10, 2020. Nurses had the highest infection rate (n = 11, 44%). Resident physicians were more likely to be infected than fellows or attending physicians (p = 0.033). The frequency of COVID exposure at work was not associated with reported COVID infection (p = 0.879 when comparing infection rates at all exposure levels).
Discussion
This is one of the first studies focused on multi-dimensional sleep patterns in healthcare workers in the first few months of the COVID-19 pandemic in an American epicenter. Other studies that have reported an impact on HCW sleep in the USA have focused primarily on sleep as a secondary component of overall mental health [11] or within particular provider groups, e.g., ambulatory practitioners [24], nurses [12], and surgeons [25]. Available data describing changes to various sleep dimensions (e.g., quality, regularity) are lacking. However, appreciating this granularity is essential to achieving overall sleep health as it has been shown to directly correlate with overall health in large population studies [17]. Our data suggest that the components of sleep in HCW most impacted during the beginning of this crisis were sleep efficiency and daytime energy levels.
Our results are consistent with those noted in other studies, both for poor sleep habits and for rates of positive depression and burnout screens. The reported pre- and intra-pandemic rates of poor sleep health (32% and 55%, respectively) coincide with those found in a large cohort of Chinese HCWs assessed at a similar time in their outbreak [26]. Similar to our data, pandemic-related rates of depression and burnout in HCW have been reported consistently around 50% [27, 28] and elevated stress levels have been seen in nearly three-quarters of providers [28].
Internationally, the most consistently impacted healthcare workers during COVID-19 have been females, nurses, and/or frontline providers [7, 9, 26, 28, 29]. We also found that frontline providers were largely affected by the decline in sleep. Instead of nurses, we found physicians, especially resident physicians, were more impacted than others. Trainees may be at higher risk of variations in sleep patterns due to inconsistent, shift-based schedules, relative inexperience, and a lack of autonomy, all noted to be risk factors in prior studies [14, 30]. These findings suggest that there are reproducible high-risk groups of healthcare providers that should receive interventions intended to acknowledge and improve sleep patterns during this and future crises. International studies have looked at mental health support at this time, our findings add evidence that future efforts should include sleep support as well.
Describing the impact of an ongoing public health crisis on the sleep and mental health of healthcare workers has both immediate and long-lasting importance [31, 32]. There is a well-documented interrelation between HCW stress, distress, sleep, and health. While providers with psychological stress can manifest physical symptoms mimicking COVID infection [27], superimposing poor sleep health onto emotional strain has been linked to impaired immunity and poor vaccine response [13, 30]. This explains the international finding that less sleep during the pandemic or poor baseline sleep pre-pandemic was associated with increased odds of contracting COVID-19 [15]. Unfortunately, data from previous pandemics suggest the detriment to mental health has been a long-lasting one in affected HCW. A full 2 years after the dissipation of a previous SARS outbreak, nearly one-third of HCWs still reported pandemic-related burnout [33]. Rates of post-traumatic stress disorder among HCWs after other pandemics were reportedly as high as 40% years after their conclusion [14]. The duration of any impact on provider sleep habits remains unknown and longitudinal data are sorely needed in this area.
One of the major limitations of this study was relying on self-reporting of sleep that occurred at two time points in one survey as this introduces recall bias and potential inaccuracies. In addition, we did not collect objective sleep measures to confirm subjective sleep reports. Importantly, our study design, survey distribution, and patient population are consistent with those of other pandemic studies. In fact, nearly all (88%) studies in one and 89% in another large systematic review of studies measuring pandemic-related mental health or sleep problems were cross-sectional, electronic, and utilized convenience sampling [34, 35]. One drawback to the convenience sample approach was that it led to a small sample size which did not have statistical power to analyze data from under-represented healthcare roles such as Environmental Services workers.
Conclusions
During the first wave of the COVID-19 pandemic, healthcare workers in all roles suffered from a decline in multiple aspects of their sleep. Self-reported insomnia and daytime sleepiness were the most affected. Being a resident physician or working in an ICU or ER were associated with higher odds of poor sleep health during the beginning of the COVID-19 pandemic.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We wish to thank all of our colleagues for their unwavering dedication to coming to work every day, without question.
Author contribution
ABH performed the study design, survey dissemination, IRB paperwork, data analysis, and primary manuscript preparation and revisions. RKB assisted with study design and manuscript preparation and revisions. AM assisted with study design, survey dissemination, and manuscript revisions.
Data availability
Not applicable.
Code availability
Not applicable.
Declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of the University at Buffalo and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Modified informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Amanda B. Hassinger, Email: ahassinger@upa.chob.edu, Email: albrooks@buffalo.edu
Ryan K. Breuer, Email: rbreuer@buffalo.edu
Archana Mishra, Email: amishra@buffalo.edu.
References
- 1.Zeng LN, Yang Y, Wang C, et al. Prevalence of poor sleep quality in nursing staff: a meta-analysis of observational studies. Behav Sleep Med. 2019;31:1–14. doi: 10.1080/15402002.2019.1677233. [DOI] [PubMed] [Google Scholar]
- 2.American College of Chest Physicians (2008) Most physicians sleep fewer hours than needed for peak performance, report says. ScienceDaily. www.sciencedaily.com/releases/2008/03/080304075723.htm. Retrieved October 23, 2019
- 3.West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 4.Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600–1613. doi: 10.1016/j.mayocp.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 5.West CP, Huschka MM, Novotny PJ, et al. Association of perceived medical errors with resident distress and empathy: a prospective longitudinal study. JAMA. 2006;296(9):1071–1078. doi: 10.1001/jama.296.9.1071. [DOI] [PubMed] [Google Scholar]
- 6.Shanafelt TD, Balch CM, Dyrbye L, et al. Special report: suicidal ideation among American surgeons. Arch Surg. 2011;146(1):54–62. doi: 10.1001/archsurg.2010.292. [DOI] [PubMed] [Google Scholar]
- 7.Shaukat N, Ali DM, Razzak J (2020) Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emerg Med 13(40). 10.1186/s12245-020-00299-5 [DOI] [PMC free article] [PubMed]
- 8.Wang S, Xie L, Xu Y, et al. Sleep disturbances among medical workers during the outbreak of COVID-19. Occup Med (Lond) 2020;70(5):364–369. doi: 10.1093/occmed/kqaa074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Network Open. 2020;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gupta B, Sharma V, Kumar N, Mahajan A. Anxiety and sleep disturbances among health care workers during the COVID-19 pandemic in India: cross sectional online survey. JMIR Pulic Health Surveill. 2020;6(4):e24206. doi: 10.2196/24206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jahrami H, BaHammam AS, AlGahtani H, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. 2021;25:503–511. doi: 10.1007/s11325-020-02135-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wright HM, Griffin BJ, Shoji K, et al. Pandemic-related mental health risk among front line personnel. J Psychiatr Res. 2021;137:673–680. doi: 10.1016/j.jpsychres.2020.10.045. [DOI] [PubMed] [Google Scholar]
- 13.Cruz MEM, Miyazawa M, Gozal D. Putative contributions of circadian clock and sleep in the context of SARS-CoV-2 infection. Eur Resp J. 2020;55(6):2001023. doi: 10.1183/13993003.01023-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Preti E, DiMattei V, Perego G, et al (2020) The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psych Reports 22(43). 10.1007/s11920-020-01166-z [DOI] [PMC free article] [PubMed]
- 15.Kim H, Hegde S, LaFiura C, Raghavan M, Luong E, Cheng S, Rebholz CM, Seidelmann SB (2021) COVID-19 illness in relation to sleep and burnout. BMJ Nutr Prev Health. 10.1136/bmjnph-2021-000228 [DOI] [PMC free article] [PubMed]
- 16.Buysse DJ. Sleep health: can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brindle RC, Yu L, Buysse DJ, Hall MH. Empirical derivation of cutoff values for the sleep health metric and its relationship to cardiometabolic morbidity: results from the Midlife in the United States (MIDUS) study. Sleep. 2019;42(9):zsz116. doi: 10.1093/sleep/zsz116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dalmases M, Benitez ID, Mas A, et al. Assessing sleep health in a European population: results of the Catalan Health Survey 2015. PLoS ONE. 2018;13(4):e0194495. doi: 10.1371/journal.pone.0194495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruxton OM, Lee S, Marino M, Beverly C, Almeida DM, Berkman L. Sleep health and predicted cardiometabolic risk scores in employed adults from two industries. J Clin Sleep Med. 2018;14(3):371–383. doi: 10.5664/jcsm.6980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Becker NB, Santos Martins RI, Jesus SN, Chiodelli R, Rieber MS. Sleep health assessment: a scale validation. Psychiatry Res. 2018;259:51–55. doi: 10.1016/j.psychres.2017.10.014. [DOI] [PubMed] [Google Scholar]
- 21.Furihata R, Hall MH, Stine KL, et al. An aggregate measure of sleep health is associated with prevalent and incident clinically significant depression symptoms among community-dwelling older women. Sleep. 2017;40:zsw075. doi: 10.1093/sleep/zsw075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.West CP, Dyrbye LN, Satele DV, et al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Untern Med. 2012;27(11):1445–1452. doi: 10.1007/s11606-012-2015-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 24.Conroy DA, Hadler NL, Cho E, et al. The effects of COVID-19 stay-at-home order on sleep, health, and working patterns: a survey study of United States health care workers. J Clin Sleep Med. 2021;17(2):185–191. doi: 10.5664/jcsm.8808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khusid JA, Weinstein CS, Becerra AZ, Kashani M, Robbins DJ, Fink LE, et al. Well-being and education of urology residents during the COVID-19 pandemic: results of an American national survey. Int J Clin Pract. 2020;74:1–8. doi: 10.22541/au.158981507.73370840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qi J, Xu J, Li BZ, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020;72:1–4. doi: 10.1016/j.sleep.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barello S, Palamenghi L, Graffigna G. Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 2020;290:113–129. doi: 10.1016/j.psychres.2020.113129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lai J, Ma S, Wang Y, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. 2020;3(3):e203976. doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pappa S, Ntella V, Giannakas T, et al. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systemic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Koh D. Occupational risks for COVID-19 infection. Occup Med (Lond) 2020;70(1):3–5. doi: 10.1093/occmed/kqaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lancet T. COVID-19: protecting health-care workers. Lancet. 2020;395(10228):922. doi: 10.1016/S0140-6736(20)30644-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Serrano-Ripoll MJ, Meneses-Echavez JF, Ricci-Cabello I, et al. Impact of viral epidemic outbreaks on mental health of healthcare workers: a rapid systematic review and meta-analysis. J Affect Disord. 2020 doi: 10.1016/j.jad.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Maunder RG, Lancee WJ, Balderson KE, et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg Infect Dis. 2006;12(12):1924–1932. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moitra M, Rahman M, Collins PY, Gohar F, Weaver M, Kinuthia J, Rossler W, Petersen S, Unutzer J, Saxena S, Huang KY, Lai J, Kumar M. Mental health consequences for healthcare workers during the COVID-19 pandemic: a scoping review to draw lessons for LMICs. Front Psych. 2021;12:602614. doi: 10.3389/fpsyt.2021.602614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris MA, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2021;17(2):299–313. doi: 10.5664/jcsm.8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.
Not applicable.