Abstract
Purpose
Early COVID-19 mitigation relied on people staying home except for essential trips. The ability to stay home may differ by sociodemographic factors. We analyzed how factors related to social vulnerability impact a community's ability to stay home during a stay-at-home order.
Methods
Using generalized, linear mixed models stratified by stay-at-home order (mandatory or not mandatory), we analyzed county-level stay-at-home behavior (inferred from mobile devices) during a period when a majority of United States counties had stay-at-home orders (April 7–April 20, 2020) with the Centers for Disease Control and Prevention Social Vulnerability Index (CDC SVI).
Results
Counties with higher percentages of single-parent households, mobile homes, and persons with lower educational attainment were associated with lower stay-at-home behavior compared with counties with lower respective percentages. Counties with higher unemployment, higher percentages of limited-English-language speakers, and more multi-unit housing were associated with increases in stay-at-home behavior compared with counties with lower respective percentages. Stronger effects were found in counties with mandatory orders.
Conclusions
Sociodemographic factors impact a community's ability to stay home during COVID-19 stay-at-home orders. Communities with higher social vulnerability may have more essential workers without work-from-home options or fewer resources to stay home for extended periods, which may increase risk for COVID-19. Results are useful for tailoring messaging, COVID-19 vaccine delivery, and public health responses to future outbreaks.
Keywords: Social vulnerability, COVID-19, Population movement, Stay-at-home order, Generalized linear mixed effect model, GIS, Spatial analysis
Introduction
Social vulnerability refers to sociodemographic factors impacting a community's ability to respond to and recover from community-level stressors, such as pandemics and natural disasters [1–3]. According to the Centers for Disease Control and Prevention Social Vulnerability Index (CDC SVI), this is due to interrelated sociodemographic factors such as education, unemployment, and household composition [4,5]. Consequently, communities with higher social vulnerability experience disproportionately higher morbidity and mortality during hazardous events, such as pathogenic disease outbreaks [1].
In February 2020, community transmission of SARS-COV-2 causing COVID-19 was detected in the United States (U.S.) [6] and, as of May 2021, has resulted in over 600,000 deaths and 34 million cases nationwide [7]. There are significant disparities in COVID-19 incidence [8,9], severity [8,9], mortality [10], and testing and resource allocation [11] across demographic factors like age, race and ethnicity, and income. Understanding the role of social vulnerability relative to COVID-19 is important; evidence indicates a disproportionate burden of COVID-19 morbidity and mortality among communities experiencing higher social vulnerability [12]. Disparities in COVID-19 outcomes may be attributable to where people live and work [10], a lack of public health interventions, and barriers to physical distancing like the inability to work from home [13].
In March 2020, U.S. jurisdictions implemented stay-at-home orders to reduce virus transmission by encouraging or requiring people to stay home except for essential trips (e.g., grocery shopping, healthcare, essential jobs) [14]. However, the ability to stay home may differ by sociodemographic factors. People with lower incomes may not have work-from-home options (e.g., grocery workers), which may increase workplace-related exposure to SARS-CoV-2 [13,15]. Persons in communities with high poverty may lack resources to acquire groceries for longer durations and may need to leave home more often [13,16]. Identifying the social vulnerability factors associated with the inability to stay home could inform prioritization of resources, COVID-19 vaccine delivery [17,18], and development of future community mitigation policies.
In this study, we analyzed county-level stay-at-home behavior and CDC SVI during a two-week period when a majority of U.S. counties were under continuous COVID-19 stay-at-home orders [19]. We investigated how social vulnerability impacts a community's ability to stay home for COVID-19 mitigation and which CDC SVI characteristics were associated with stay-at-home behavior. Understanding stay-at-home behavior of persons in counties with higher social vulnerability provides important context for tailoring public health messaging for COVID-19 risk reduction behaviors (e.g., wearing masks, social distancing) outside the home. Results may inform resource allocation (e.g., vaccine prioritization) and tailored public health programs for communities at increased exposure risk for SARS-CoV-19. Findings may assist in designing equitable responses to public health emergencies and future community mitigation policies.
Methods and materials
Study population
This ecologic study analyzed county-level data for the entire U.S. (n = 3142 counties) and 2018 CDC SVI [3] while accounting for prepandemic mobile device behavior (2019 stay-at-home percentage), population density (urbanicity), and state/county stay-at-home orders. Counties with complete CDC SVI data and stay-at-home orders (mandatory and not mandatory) which were in place for the entire study period, were included in stratified analyses (n = 3119 counties).
Stay-at-home behavior
Location-based-services data from aggregated, anonymized, opted-in mobile devices (e.g., smart phones) are used as a proxy for human movement [[20], [21], [22], [23]]. Some counties were highly mobile before the pandemic and, even with large percent changes in behavior, remained high relative to other counties during periods of stay-at-home orders. We were interested in total county movement, rather than the relative change in behavior. Therefore, the percentage of devices completely-at-home (stay-at-home behavior) was assessed as the outcome of interest. Stay-at-home behavior was defined using the median percentage of devices completely at-home each day between April 7 and 20, 2020 from Cuebiq's shelter-in-place dataset (approximately 20 million active devices). Cuebiq measures shelter-in-place as the proportion of devices “completely-at-home” each day over the total number of devices seen on that day at the county-level. Cuebiq infers a device's home location using the device's most common nighttime location over a six-week period [24]. The study period (April 7–20, 2020) was selected to estimate stay-at-home behavior when a majority of U.S. counties were under continuous stay-at-home orders (mandatory and not mandatory) [19].
The CDC Social Vulnerability Index (CDC SVI)
The CDC SVI tool is a percentile-ranked metric used to identify communities that may be disproportionately burdened before, during, and after public health emergencies [1,2]. CDC SVI uses 15 U.S. census variables to rank U.S. counties from 0 to 1 (higher numbers indicating higher social vulnerability) by an overall composite rank score and by four themes representing social vulnerability: (1) Socioeconomic Status (poverty, unemployment, income, no high school diploma), (2) Household Composition and Disability (aged 65 or older, aged 17 or younger, disability, single-parent households), (3) Minority Status and Language (racial or ethnic minority group, speak English “less than well”), and (4) Housing Type and Transportation (multi-unit housing, mobile homes, crowded housing, vehicle access, group quarters). CDC SVI 2018 data for all U.S. counties were obtained from CDC/ATSDR's Geospatial Research, Analysis, and Services Program's (GRASP) publicly available database, which represent the most current sociodemographic census data available for U.S. populations [3].
Covariates
U.S. state and county stay-at-home orders
COVID-19 stay-at-home orders expressly required or recommended individuals stay home except for essential trips. Orders by U.S. county for April 7–20, 2020 were queried from CDC's database of state, territorial, and county level orders located on publicly available state and county government websites [19].
We coded counties as either with a mandatory order for all individuals or without a mandatory order for all individuals. Counties without mandatory orders include those that had mandatory orders for certain groups but not for all persons in the county, orders that advised but did not require persons to stay home, or for which no orders were found. Orders not available through publicly accessible government websites were not included [25].
Prepandemic stay-at-home behavior
Prepandemic stay-at-home behavior was included to account for a baseline level of county behavior (e.g., multiple device ownership, leaving some devices at home, or general tendency to stay home due to high county unemployment) during a non-pandemic period. Prepandemic stay-at-home behavior was defined using the median percentage of devices completely-at-home each day between April 7 and 20, 2019 from Cuebiq's shelter-in-place dataset.
Urbanicity
Urbanicity was categorized as large metropolitan (referent), medium/small metropolitan, and micropolitan/non-core, which are collapsed from the National Center for Health Statistics’ 2013 Urban-Rural Classification Scheme for Counties [26].
Analysis
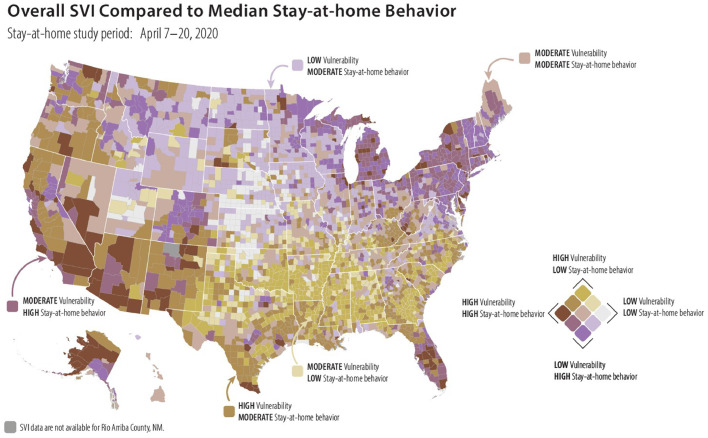
Univariate linear mixed effects models were fit to assess relationships between stay-at-home behavior for 31411 U.S. counties from April 7–20, 2020 and (1) overall CDC SVI percentile ranking, (2) each of the four CDC SVI themes by percentile ranking, and (3) each of the individual CDC SVI variables as percentages. To visualize the spatial distribution of CDC SVI and stay-at-home behavior, we mapped stay-at-home behavior during the examined period (April 7–20, 2020) with overall CDC SVI ranking for all U.S. counties (Fig. 1 ).
Fig. 1.
County-level bivariate map comparing overall 2018 CDC Social Vulnerability Index (SVI) to median stay-at-home behavior (April 7–20, 2020), United States.
Multivariate linear mixed effects models were fit to assess relationships between stay-at-home behavior for 31202 U.S. counties from April 7–20, 2020 and (1) overall CDC SVI percentile ranking, (2) all four CDC SVI themes by percentile ranking, and (3) individual CDC SVI variables as percentages. To account for typical device movement during a non-pandemic period and correlations with population density and CDC SVI variables, we controlled for prepandemic stay-at-home behavior, urbanicity, and remaining CDC SVI themes or variables in the adjusted models. An assessment of collinearities and variance inflation factors (VIF) among the individual CDC SVI variables led to the exclusion of two CDC SVI variables from the final models assessing CDC SVI variables as percentages– per capita income and percentage of persons under the age of 18. To understand how stay-at-home orders may have modified stay-at-home behavior, all final adjusted models were stratified by stay-at-home order type (mandatory order vs. no mandatory order).
All univariate and multivariate models used a Gaussian spatial correlation structure (county-level) to account for spatial autocorrelation and included “U.S. State” as a random effect. Model fit was assessed using R2. Statistical analyses were conducted in R version 4.0.0 [27]. Due to the large number of counties, significance was assessed at alpha = 0.01.
Results
During April 7–20, 2020, county-level stay-at-home behavior varied from 23.9% to 75.0% with a median of 35.6% remaining completely at home daily. Prepandemic stay-at-home behavior (April 7–20, 2019) ranged from 8.3% to 50.0% with a median of 22.8%.
Of the counties that had continuous stay-at-home orders for the study period, 71.5% had a stay-at-home order that was mandatory for all individuals (n = 2231 counties), and 28.5% did not have a known order that was mandatory for all individuals (n = 888 counties).
Higher CDC SVI percentile rank (higher social vulnerability relative to other counties) was significantly associated with lower stay-at-home behavior after adjusting for prepandemic stay-at-home behavior and urbanicity, with stronger decreases noted in counties with mandatory orders (β = -4.18, P < .01) compared to those without mandatory orders (β = -2.08, P < .01).
All four CDC SVI themes were associated with stay-at-home behavior. Lower stay-at-home behavior was found among counties with higher percentile ranks in socioeconomic status (Theme 1: β = -6.92, P < .01), household composition and disability status (Theme 2: β = -6.37, P < .01), and housing type and transportation (Theme 4: β = -0.95, P < .01). Higher percentile rank in minority status and language was associated with higher stay-at-home behavior (Theme 3: β = 3.79, P < .01). After adjusting for prepandemic stay-at-home behavior, urbanicity, and remaining CDC SVI themes, effects for themes 1, 2, and 3 were attenuated but remained significant, while the effect for theme 4 changed directionality (Table 1 ).
Table 1.
Unadjusted and adjusted linear mixed effects models* of county stay-at-home behavior† and the CDC Social Vulnerability Index (CDC SVI)‡ percentile ranking by theme, United States, April 7–April 20, 2020§
|
Unadjusted |
Adjusted¶ |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| All counties (n = 3141) |
All counties (n = 3141) |
With mandatory stay-at-home order# (n = 2231) |
Without mandatory stay-at-home order⁎⁎ (n = 888) |
||||||
| Fixed effects | Estimate†† | p-value | Estimate | p-value | Estimate | p-value | Estimate | p-value | |
| (Intercept) | – | – | 31.62 | <0.01 | 30.73 | <0.01 | 33.27 | <0.01 | |
| CDC Social Vulnerability Index | |||||||||
| Theme 1: Socioeconomic Status | -6.92 | <0.01 | -5.14 | <0.01 | -6.06 | <0.01 | -3.86 | <0.01 | |
| Theme 2: Household Composition & Disability | -6.37 | <0.01 | -3.16 | <0.01 | -3.41 | <0.01 | -2.46 | <0.01 | |
| Theme 3: Minority Status & Language | 3.79 | <0.01 | 2.99 | <0.01 | 3.75 | <0.01 | 0.96 | 0.08 | |
| Theme 4: Housing Type & Transportation | -0.95 | <0.01 | 1.90 | <0.01 | 1.75 | <0.01 | 2.06 | <0.01 | |
| Prepandemic Stay-At-Home Behavior | |||||||||
| 2019 Stay-At-Home Percentage‡‡ | – | – | 0.46 | <0.01 | 0.51 | <0.01 | 0.32 | <0.01 | |
| Urbanicity | |||||||||
| Medium & Small Metropolitan | – | – | -2.39 | <0.01 | -2.19 | <0.01 | -2.09 | <0.01 | |
| Micropolitan & Noncore | – | – | -4.21 | <0.01 | -3.76 | <0.01 | -3.93 | <0.01 | |
| Model R2 | – | – | 0.51 | – | 0.57 | – | 0.37 | – | |
Unadjusted and adjusted generalized linear mixed effects models include a Gaussian spatial correlation structure (county-level) and U.S. State as a random effect.
County stay-at-home behavior was defined as the median percentage of anonymous, aggregated mobile devices completely-at-home daily during the examined period.
Social vulnerability was assessed using the 2018 Centers for Disease Control and Prevention (CDC) Social Vulnerability Index (CDC SVI), a metric used to identify communities that may need support before, during, and after public health emergencies (https://www.atsdr.cdc.gov/placeandhealth/svi/index.html).
Examined period: April 7–April 20, 2020 selected to approximate population movement during a period when a majority of U.S. counties were under continuous stay-at-home orders (mandatory or not mandatory).
Adjusted for prepandemic 2019 stay-at-home percentage, urbanicity, and remaining CDC SVI Themes.
Mandatory orders include those counties and jurisdictions that had a state-issued or county-issued stay-at-home order for all persons for the duration of the examined period.
Counties without mandatory state-issued or county-issued orders include jurisdictions that may have had mandatory orders only for certain groups, such as persons at higher risk from COVID-19 or children, but did not extend to all persons in the county, orders which advised but did not require persons to stay home, or for which no orders were found.
A positive estimate indicates the factor listed in the first column is associated with increased stay-at-home behavior. A negative estimate indicates that the factor listed in the first column is associated with decreased stay-at-home behavior.
Prepandemic period: April 7–April 20, 2019 (used to approximate population movement before the COVID-19 pandemic).
Among counties with mandatory stay-at-home orders, each of the four CDC SVI themes were significantly associated with stay-at-home behavior after adjusting for urbanicity, prepandemic stay-at-home behavior, and remaining CDC SVI themes. Higher social vulnerability percentile rank due to socioeconomic status (Theme 1: β = -6.06, P < .01) or household composition and disability status (Theme 2: β = -3.41, P < .01) was associated with lower stay-at-home behavior. Conversely, higher social vulnerability percentile rank due to racial or ethnic minority status and language (Theme 3: β = 3.75, P < .01) or housing type and transportation (Theme 4: β = 1.75, P < .01) was associated with higher stay-at-home behavior. In counties without mandatory orders, higher percentile rank for Themes 1 and 2 was significantly associated with lower stay-at-home behavior but with weaker effects compared to counties with mandatory orders (Table 1).
Except for crowded housing, all examined CDC SVI variables were significantly associated with stay-at-home behavior in the unadjusted models. After adjustment, 8 of the examined 13 variables remained significant (Table 2 ). Among counties with mandatory stay-at-home orders, four CDC SVI individual variables were significantly associated with lower stay-at-home behavior after adjusting for urbanicity, prepandemic stay-at-home behavior, and remaining CDC SVI variables: percentage of single-parent households (β = -0.31, P < .001), percentage of adults without a high school diploma (β = -0.26, P < .01), percentage of persons with a disability (β = -0.14, P < .01), and percentage of mobile homes (β = -0.03, P < .01). Counties with higher percentages of persons who speak English less than well (β = 0.29, P < .01), multi-unit housing (β = 0.25, P < .01), unemployment (β = 0.13, P < .01), and persons in racial and ethnic minority groups (β = 0.03, P < .01) were significantly associated with increased stay-at-home behavior (Table 2). Similar but fewer significant effects were found among counties without mandatory stay-at-home orders (Table 2).
Table 2.
Unadjusted and adjusted linear mixed effects models* of county stay-at-home behavior† and the CDC Social Vulnerability Index (CDC SVI)‡ individual variables as percentages, United States, April 7–April 20, 2020§** (n=888)
|
Unadjusted |
Adjusted¶ |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All counties (n = 3141) |
All counties (n = 3141) |
With mandatory stay-at-home orders# (n = 2231) |
Without mandatory stay-at-home orders⁎⁎ (n = 888) |
||||||||||
| Fixed effects | Estimate†† | p-value | Estimate | p-value | Estimate | p-value | Estimate | p-value | |||||
| (Intercept) | – | – | 33.73 | <0.01 | 34.13 | <0.01 | 35.30 | <0.01 | |||||
| CDC Social Vulnerability Index | |||||||||||||
| Theme 1: Socioeconomic Status | |||||||||||||
| No High School Diploma | -0.30 | <0.01 | -0.27 | <0.01 | -0.26 | <0.01 | -0.30 | <0.01 | |||||
| Below Poverty | -0.13 | <0.01 | 0.03 | 0.03 | -0.02 | 0.35 | 0.09 | <0.01 | |||||
| Unemployed | -0.08 | <0.01 | 0.13 | <0.01 | 0.13 | <0.01 | 0.06 | 0.22 | |||||
| Theme 2: Household Composition & Disability | |||||||||||||
| Aged 65 or Older | -0.15 | <0.01 | 0.00 | 0.80 | 0.00 | 0.88 | 0.05 | 0.19 | |||||
| Single-Parent Households | -0.12 | <0.01 | -0.28 | <0.01 | -0.31 | <0.01 | -0.31 | <0.01 | |||||
| Living with a Disability | -0.38 | <0.01 | -0.09 | <0.01 | -0.14 | <0.01 | -0.07 | 0.08 | |||||
| Theme 3: Minority Status & Language | |||||||||||||
| Minority | 0.04 | <0.01 | 0.03 | <0.01 | 0.03 | <0.01 | 0.05 | <0.01 | |||||
| Speaks English “Less than Well” | 0.16 | <0.01 | 0.25 | <0.01 | 0.29 | <0.01 | 0.13 | 0.05 | |||||
| Theme 4: Housing Type & Transportation | |||||||||||||
| Mobile Homes | -0.20 | <0.01 | -0.03 | <0.01 | -0.03 | <0.01 | -0.01 | 0.66 | |||||
| Group Quarters | -0.05 | <0.01 | 0.01 | 0.34 | 0.02 | 0.22 | 0.02 | 0.51 | |||||
| No Household Vehicle | 0.05 | <0.01 | 0.00 | 0.98 | 0.05 | 0.02 | -0.01 | 0.78 | |||||
| Crowded Housing | -0.01 | 0.80 | 0.03 | 0.36 | -0.03 | 0.46 | 0.08 | 0.16 | |||||
| Multi-Unit Housing | 0.39 | <0.01 | 0.24 | <0.01 | 0.25 | <0.01 | 0.17 | <0.01 | |||||
| Prepandemic Stay-At-Home Behavior | |||||||||||||
| 2019 Stay-At-Home Percentage‡‡ | – | – | 0.44 | <0.01 | 0.48 | <0.01 | 0.27 | <0.01 | |||||
| Urbanicity | |||||||||||||
| Urbanicity: Med/Small | – | – | -1.95 | <0.01 | -1.70 | <0.01 | -1.92 | <0.01 | |||||
| Urbanicity: Micro/Noncore | – | – | -3.24 | <0.01 | -2.76 | <0.01 | -3.40 | <0.01 | |||||
| Model R2 | – | – | 0.63 | – | 0.69 | – | 0.48 | – | |||||
Unadjusted and adjusted generalized linear mixed effects models include a Gaussian spatial correlation structure (county-level) and U.S. State as a random effect.
County stay-at-home behavior was defined as the median percentage of anonymous, aggregated mobile devices completely-at-home daily during the examined period.
Social vulnerability was assessed using the 2018 Centers for Disease Control and Prevention (CDC) Social Vulnerability Index (CDC SVI), a metric used to identify communities that may need support before, during, and after public health emergencies (https://www.atsdr.cdc.gov/placeandhealth/svi/index.html).
Examined period: April 7–April 20, 2020 selected to approximate population movement during a period when a majority of U.S. counties were under continuous stay-at-home orders (mandatory or not mandatory).
Adjusted for prepandemic 2019 stay-at-home percentage, urbanicity, and remaining CDC SVI individual variables.
Mandatory orders include those counties and jurisdictions that had a state-issued or county-issued stay-at-home order for all persons for the duration of the examined period.
Counties without mandatory state-issued or county-issued orders include jurisdictions that may have had mandatory orders only for certain groups, such as persons at higher risk from COVID-19 or children, but did not extend to all persons in the county, orders which advised but did not require persons to stay home, or for which no orders were found.
A positive estimate indicates the factor listed in the first column is associated with increased stay-at-home behavior. A negative estimate indicates that the factor listed in the first column is associated with decreased stay-at-home behavior.
Prepandemic period: April 7–April 20, 2019 (used to approximate population movement before the COVID-19 pandemic).
Figure 1 visualizes the national spatial distribution of social vulnerability and stay-at-home behavior during April 7–20, 2020, with regional trends in both CDC SVI and stay-at-home behavior. The Southeast appeared to have higher social vulnerability and lower stay-at-home behavior, while the Northeast showed lower social vulnerability and higher stay-at-home behavior.
Discussion
This study leverages aggregated mobile device data as a novel source to understand important associations between the ability to stay home and CDC SVI during the early stages of the COVID-19 pandemic. CDC SVI had not been previously used to examine which sociodemographic factors were associated with stay-at-home behavior during COVID-19 stay-at-home orders. During periods of large-scale, uncontrolled COVID-19 transmission, stay-at-home orders were one of the most effective disease mitigation strategies available [14,28]. However, this study found that the ability to stay home differs by socioeconomic and demographic factors. After adjusting for prepandemic stay-at-home behavior and urbanicity, higher CDC SVI percentile ranking was significantly associated with lower stay-at-home behavior suggesting that persons living in counties with higher social vulnerability stayed home significantly less than persons in counties with lower social vulnerability. State and county stay-at-home orders modified these effects, with stronger effects in counties with mandatory orders and generally weaker and fewer significant associations noted in counties without mandatory orders. R2 values were higher in models stratified by mandatory order, which suggests that social vulnerability may better explain the variation in stay-at-home behavior for counties with mandatory orders compared to counties without mandatory orders.
The relationship was strong among counties with lower socioeconomic status, suggesting that there are a greater proportion of individuals with jobs requiring them to leave home. For example, counties with a higher proportion of individuals with low educational attainment may have more persons employed in essential positions without remote-work options (e.g., grocery stores, construction) and must leave home for employment [15,29,30]. People with lower socioeconomic status are less likely to have access to healthcare [31], health insurance [32], and paid sick leave [33], which could impact their ability to stay home from work when ill or when exposed to others who are ill, and could delay testing and care seeking for COVID-19. Further, these communities may require additional resources to recover economically due to higher baseline levels of unemployment and poverty.
We found important associations in stay-at-home behavior and household characteristics. Counties with higher percentages of single-parent households were associated with lower stay-at-home behavior in the adjusted models. For every ten percent increase in percentage of single parent households, stay-at-home behavior decreased by approximately 3% both in counties with and without mandatory orders. Single-parent households may require more interaction from others in the community while under stay-at-home orders to care for and educate children. Further, persons in counties with higher proportions of residents with disabilities also exhibited less stay-at-home behavior. Persons in these counties may need to leave home more often for healthcare. The true characteristics of device users are unknown, so this may reflect movement of caretakers or others in the community, rather than the residents with disabilities themselves.
Persons in counties with higher percentages of persons of racial and ethnic minority groups, with limited English language proficiency, higher percentages of baseline unemployment, and with more multi-unit housing units stayed at home more during the examined period. The increase was stronger among counties with mandatory orders and largely driven by counties with higher proportions of limited English language speakers. Persons in these counties may have been subject to inequitable enforcement of orders [34] and increased job losses from business closures [35,36] which may have increased stay-at-home behavior. Counties in Southern U.S. States with higher percentages of persons who speak English less than well may have been impacted by the U.S.-Mexico border closures to reduce movement to retail and businesses on either side of the border [37]. Stay-at-home behavior may also differ by and across racial and ethnic minority groups and should be further explored in future analyses.
Urbanicity and prepandemic behavior are confounders of these associations. Specifically, they attenuate estimates of stay-at-home behavior in expected ways. For instance, higher percentile rank in housing type and transportation (Theme 4) was associated with lower stay-at-home behavior. After adjusting for urbanicity and prepandemic behavior, the directionality reversed with higher percentile rank associated with higher stay-at-home behavior. This theme aligns with the ability to move and the conditions in which people live, such as personal vehicle access and living in multi-unit housing. However, multi-unit housing structures are more concentrated in urban areas and include residents of all income levels. CDC SVI does not distinguish between multi-unit housing in luxury apartments or affordable housing developments. Therefore, there may be unmeasured effect modification due to income and population density (urbanicity), which should be further explored.
Persons living in counties with low stay-at-home behavior and higher social vulnerability may experience increased SARS-CoV-19 exposure risk. They may be disproportionately affected by illness, business closures, and community-level consequences of the COVID-19 pandemic. These relationships may lend insight into the implementation of updated mitigation policies as jurisdictions revisit stay-at-home policies for COVID-19 or other infectious disease outbreaks. Counties that exhibited low stay-at-home behavior and higher social vulnerability were primarily concentrated in Southern and Southeastern states, which were among the first to relax stay-at-home policies in April 2020 [19]. Continuing to monitor counties with higher population movement and higher social vulnerability may contribute to improved early detection and control of COVID-19 outbreaks.
This study has limitations. These data are a sample of mobile devices used by persons of unknown demographics and are limited to the examined period, which may not be generalizable or reflect stay-at-home behavior over time. Further, using mobile devices as a proxy for population movement may not fully account for multiple device ownership, some of which may stay home while the user leaves, or communities with low device ownership. Additionally, states and counties defined activities exempt from stay-at-home orders differently, which may have impacted the ability of persons to stay home in certain communities. Future studies may review the impact of other community mitigation policies, such as bar and restaurant closures.
Conclusions
There was a relationship between county-level stay-at-home behavior and social vulnerability during the COVID-19 pandemic. In the examined period, persons in counties with higher social vulnerability stayed home less often than persons in counties with lower social vulnerability. Findings highlight the importance of understanding the socioeconomic and demographic factors that impact a community's ability to stay home during stay-at-home orders and future infectious disease outbreaks. Public health messaging should be tailored to encourage strategies to reduce COVID-19 community mitigation (e.g., wearing masks, social distancing) when leaving home. Results are useful for resource allocation (e.g., testing, vaccination) in communities with higher social vulnerability. Public health responders should consider social vulnerability and population movement when designing equitable responses to public health emergencies. Policy makers may also consider the ability for communities to stay home when developing future community mitigation policies for infectious disease outbreaks.
Acknowledgments
This activity was reviewed by the Centers for Disease Control and Prevention and was conducted consistent with applicable federal law and CDC policy (45 C.F.R. part 46, 21 C.F.R. part 56; 42 U.S.C. §241(d); 5 U.S.C. §552a; 44 U.S.C. §3501 et seq.).
The authors are grateful to Antonio Tomarchio; Brennan Lake; Cuebiq Data for Good Program; Charity Hilton; Samantha Lie-Tjauw, MBA, MPH; Jason Poovey, MS; Russell McCord, JD; GRASP Mobility Data Project Team; CDC Social Vulnerability Index Team; CDC Public Health Law Program; CDC COVID-19 Response. Proprietary data used in this study were provided to CDC/ATSDR by Cuebiq's Data for Good Program. This research was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and CDC. This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or Agency for Toxic Substances and Disease Registry.
No potential conflicts of interest were disclosed.
One county in New Mexico was excluded due to missing CDC SVI data: Rio Arriba County.
Twenty-two counties, all in the State of Texas, were excluded because the stay-at-home order was not in place for the entirety of the study period.
References
- 1.Flanagan B.E., Gregory E.W., Hallisey E.J., Heitgerd J.L., Lewis B. A social vulnerability index for disaster management. J Homel Secur Emerg Manag. 2011;8(1) doi: 10.2202/1547-7355.1792. [DOI] [Google Scholar]
- 2.Flanagan B.E., Hallisey E.J., Adams E., Lavery A. Measuring community vulnerability to natural and anthropogenic hazards: the centers for disease control and prevention's social vulnerability index. J Environ Health. 2018;80(10):34–36. [PMC free article] [PubMed] [Google Scholar]
- 3.CDC.CDC social vulnerability index 2018 database. Geospatial Research, Analysis, and Services Program (GRASP). 2018. Available from: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html [Accessed 15 May 2020].
- 4.Sherrieb K., Norris F.H., Galea S. Measuring capacities for community resilience. Soc Indic Res. 2010;99(2):227–247. doi: 10.1007/s11205-010-9576-9. [DOI] [Google Scholar]
- 5.Bergstrand K., Mayer B., Brumback B., Zhang Y. Assessing the relationship between social vulnerability and community resilience to hazards. Soc Indic Res. 2015;122(2):391–409. doi: 10.1007/s11205-014-0698-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jernigan D.B. Update: public health response to the coronavirus disease 2019 outbreak - United States, February 24, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(8):216–219. doi: 10.15585/mmwr.mm6908e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CDC . Centers for Disease Control and Prevention; Atlanta, Georgia.: 2021. COVID Data Tracker. Available from: https://covid.cdc.gov/covid-data-tracker [Accessed 15 May 2021] [Google Scholar]
- 8.Neelon B., Mutiso F., Mueller N.T., Pearce J.L., Benjamin-Neelon S.E. Spatial and temporal trends in social vulnerability and COVID-19 incidence and death rates in the United States. medRxiv. 2020.10.1101/2020.09.09.20191643. [DOI] [PMC free article] [PubMed]
- 9.Li Y., Cen X., Cai X., Temkin-Greener H. Racial and ethnic disparities in COVID-19 infections and deaths across U.S. nursing homes. J Am Geriatr Soc. 2020;68(11):2454–2461. doi: 10.1111/jgs.16847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen J.T., Krieger N. Revealing the unequal burden of COVID-19 by income, race/ethnicity, and household crowding: US county versus zip code analyses. J Public Health Manag Pract. 2021;27(1):S43–s56. doi: 10.1097/phh.0000000000001263. Suppl. [DOI] [PubMed] [Google Scholar]
- 11.Lewis N.M., Friedrichs M., Wagstaff S., Sage K., LaCross N., Bui D., et al. Disparities in COVID-19 incidence, hospitalizations, and testing, by area-level deprivation - Utah, March 3-July 9, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(38):1369–1373. doi: 10.15585/mmwr.mm6938a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dasgupta S., Bowen V.B., Leidner A., Fletcher K., Musial T., Rose C., et al. Association between social vulnerability and a county's risk for becoming a COVID-19 Hotspot - United States, June 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(42):1535–1541. doi: 10.15585/mmwr.mm6942a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jay J., Bor J., Nsoesie E.O., Lipson S.K., Jones D.K., Galea S., et al. Neighbourhood income and physical distancing during the COVID-19 pandemic in the United States. Nat Hum Behav. 2020;4(12):1294–1302. doi: 10.1038/s41562-020-00998-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CDC; 2021. Implementation of mitigation strategies for communities with local COVID-19 transmission Atlanta, Georgia. updated 2/16/2021. Available from https://www.cdc.gov/coronavirus/2019-ncov/community/community-mitigation.html [Accessed 30 July 2020] [Google Scholar]
- 15.Baker M.G., Peckham T.K., Seixas N.S. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS ONE. 2020;15(4) doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chang H.-.Y., Tang W., Hatef E., Kitchen C., Weiner J.P., Kharrazi H. Differential impact of mitigation policies and socioeconomic status on COVID-19 prevalence and social distancing in the United States. BMC Public Health. 2021;21(1):1140. doi: 10.1186/s12889-021-11149-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hughes M.M., Wang A., Grossman M.K., Pun E., Whiteman A., Deng L., et al. County-level COVID-19 vaccination coverage and social vulnerability - United States, December 14, 2020-March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(12):431–436. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barry V., Dasgupta S., Weller D.L., Kriss J.L., Cadwell B.L., Rose C., et al. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity - United States, December 14, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(22):818–824. doi: 10.15585/mmwr.mm7022e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CDC. COVID-19 community intervention and at-risk task force, monitoring and evaluation team & CDC, center for state, tribal, local, and territorial support, public health law program, state, territorial, and county COVID-19 orders and proclamations for individuals to stay home. 2021
- 20.Bourassa K.J. State-level stay-at-home orders and objectively measured movement in the united states during the COVID-19 pandemic. Psychosom Med. 2021;83(4):358–62.10.1097/psy.0000000000000905. [DOI] [PMC free article] [PubMed]
- 21.Pepe E., Bajardi P., Gauvin L., Privitera F., Lake B., Cattuto C., et al. COVID-19 outbreak response, a dataset to assess mobility changes in Italy following national lockdown. Sci Data. 2020;7(1):230. doi: 10.1038/s41597-020-00575-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hunter R.F., Garcia L., de Sa T.H., Zapata-Diomedi B., Millett C., Woodcock J., et al. Effect of COVID-19 response policies on walking behavior in US cities. Nat Commun. 2021;12(1):3652. doi: 10.1038/s41467-021-23937-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bourassa K.J., Sbarra D.A., Caspi A., Moffitt T.E. Social Distancing as a health behavior: county-level movement in the United States During the COVID-19 pandemic is associated with conventional health behaviors. Ann Behav Med. 2020;54(8):548–556. doi: 10.1093/abm/kaaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cuebiq.Shelter-in-place analysis. 2020. Available from: https://www.cuebiq.com/visitation-insights-sip-analysis/.
- 25.CDC Severe outcomes among patients with Coronavirus Disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.CDC. National Center Health Statistics, 2013 Urban-rural classification scheme for counties. Hyattsville, MD, 2013. https://www.cdc.gov/nchs/data_access/urban_rural.htm.
- 27.RStudio: Integrated Development for R. 4.0 ed. Boston, MA: R Studio Team, RStudio, PBC; 2020
- 28.Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24-April 21, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(18):551–556. doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dorn A.V., Cooney R.E., Sabin M.L. COVID-19 exacerbating inequalities in the US. Lancet. 2020;395(10232):1243–1244. doi: 10.1016/s0140-6736(20)30893-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Waltenburg M.A., Victoroff T., Rose C.E., Butterfield M., Jervis R.H., Fedak K.M., et al. Update: COVID-19 among workers in meat and poultry processing facilities - United States, April-May 2020. MMWR Morb Mortal Wkly Rep. 2020;69(27):887–892. doi: 10.15585/mmwr.mm6927e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adler N.E., Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff (Millwood) 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 32.McMaughan D.J., Oloruntoba O., Smith M.L. Socioeconomic status and access to healthcare: interrelated drivers for healthy aging. Front Public Health. 2020;8:231. doi: 10.3389/fpubh.2020.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DeRigne L., Stoddard-Dare P., Collins C., Quinn L. Paid sick leave and preventive health care service use among U.S. working adults. Prev Med. 2017;99:58–62. doi: 10.1016/j.ypmed.2017.01.020. [DOI] [PubMed] [Google Scholar]
- 34.Watts M.H., Michel K.H., Breslin J., Tobin-Tyler E. Equitable enforcement of pandemic-related public health laws: strategies for achieving racial and health justice. Am J Public Health. 2021;111(3):395–397. doi: 10.2105/ajph.2020.306112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gemelas J., Davison J., Keltner C., Ing S. Inequities in employment by race, ethnicity, and sector during COVID-19. J Racial Ethn Health Disparities. 2021 doi: 10.1007/s40615-021-00963-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Capps R.B., Jeanne; Gelatt, Julia. COVID-19 and unemployment: assessing the early fallout for immigrants and other U.S. workers. Migration Policy Institute; 2020 2020.
- 37.Rodriguez-Sanchez J.I. Rice University's Baker Institute for Public Policy; Houston, Texas: 2020. Mexican consumption and the economic impact of the coronavirus on Texas border counties. [Google Scholar]