Abstract
Both neurocognition and negative symptoms have demonstrated strong links to functional outcomes, such as work functioning, among those with severe mental illness (SMI). Prior models have suggested that reduced neurocognition 1) precedes or predicts greater negative symptoms and 2) indirectly influences functional outcomes via its impact on negative symptoms. The current study sought to also test a divergent model: whether greater negative symptoms predict reduced neurocognition and indirectly influence work functioning through their impact on neurocognition. Both models were tested using cross-sectional and prospective data spanning 20-years in a sample of 277 people with a SMI with psychotic features. Results showed that both models were supported in cross-sectional analyses. However, in prospective models predicting work functioning, only the models examining the indirect influence of negative symptoms on work functioning (7.5 to up to 20-years later) through neurocognition demonstrated significant mediation (i.e., a significant indirect effect); further, higher negative symptoms significantly predicted lower prospective neurocognition, while lower neurocognition did not significantly predict greater prospective negative symptoms. Although cross-sectional data were consistent with prior models, our prospective models offered greater support for a putative causal pathway running from negative symptoms to neurocognition—rather than the reverse—to work functioning. Findings have implications for mechanisms contributing to longitudinal work functioning and suggest that targeting negative symptoms prior to neurocognition could be more beneficial for long-term work outcomes.
Keywords: work, negative symptoms, vocational rehabilitation, neurocognition, severe mental illness, psychosis
1. Introduction
A sense of purpose and meaning is one of the main tenants of recovery from severe mental illness (SMI) (Anthony, 1993; Farkas, 2007). A primary way most people develop meaningful and productive roles in their communities is through competitive employment. However, many with SMI have difficulty obtaining work, with approximately 10–25% of those with SMI being employed despite upwards of 70% reporting a desire to work (Brantschen et al., 2014; Evensen et al., 2016; Rosenheck et al., 2006). Although supported employment and cognitive-behavioral therapy (CBT) programs can improve work-related outcomes (Kinoshita et al., 2013; Kukla et al., 2018; Lysaker et al., 2009), a number of people with SMI do not successfully obtain employment even after these programs. Therefore, enhanced understanding of the putative causal pathways contributing to work outcomes may help to improve these interventions that support this critical element of recovery among those with SMI.
Theoretical models and empirical studies emphasize the importance of neurocognition and more recently, negative symptoms, in predicting work functioning for those with SMI (McGurk and Mueser, 2004; Quinlan et al., 2014; Rosenheck et al., 2006; Tsang et al., 2010; Ventura et al., 2009). For example, a 2004 review by McGurk and Mueser found that neurocognition was significantly related to current, recent, or later work in all reviewed retrospective, cross-sectional, or prospective studies for those with SMI not in vocational rehabilitation services. A later review by Tsang et al. (2010) found that neurocognition was the most widely studied and received the most “overwhelming” empirical support as a significant predictor of work functioning. However, within the last decade, some researchers have shifted to identifying the role of negative symptoms on work outcomes. To date, studies have shown cross-sectional links between greater negative symptoms and reduced work functioning (Hunter and Barry, 2012; Shamsi et al., 2011) as well as shown that higher negative symptoms significantly predict poorer work outcomes 6 to 12-months later in those with SMI (Erickson et al., 2011; Llerena et al., 2018; Saperstein et al., 2011; Ventura et al., 2015).
Although research suggests neurocognition and negative symptoms are key cross-sectional and prospective predictors of work functioning, an important unresolved question is whether negative symptoms and neurocognition independently or jointly influence work outcomes over time. One possibility Ventura et al. (2009) demonstrated using cross-sectional data from 73 studies is that neurocognition directly influences as well as indirectly influences (i.e., partially mediates) functional outcomes through its impact on negative symptoms. This aligns with the prominent theory suggesting that lower neurocognition is an underlying causal factor influencing negative symptoms (Ventura et al., 2009). Building on this work, Meyer et al. (2014) examined this model in a sample of 167 individuals at clinically high-risk for psychosis from the North America Prodrome Longitudinal Study Phase 1 (NAPLS-1; Addington et al., 2007) and demonstrated that baseline negative symptoms partially mediated the relationship between baseline composite neurocognition and both role (e.g., school/work) and social functioning assessed at both baseline and then 12-months later. Thus, in addition to neurocognition directly impacting functional outcomes, there is some support suggesting that negative symptoms may act as a conduit through which the effects of neurocognition impact functional outcomes such as work outcomes in SMI; however, in order to more decisively test these putative causal pathways (Maxwell and Cole, 2007), additional work is needed to examine this model prospectively in those who have developed SMI.
There is also burgeoning evidence suggesting that an alternative model might explain the relationships between negative symptoms, neurocognition, and functional outcomes. Several recent studies have suggested that negative symptoms may actually precede and contribute to lower neurocognition (Fervaha et al., 2014; Foussias et al., 2015; Strauss et al., 2015). For example, Strauss et al. (2015) found that higher negative symptoms and reduced effort significantly predicted lower global neurocognition in a cross-sectional study with SMI participants, while Fervaha et al. (2014) found that the negative symptom domain of reduced motivation was significantly correlated with reduced concurrent and 6-month neurocognition. Notably, these studies align with a recent alternative cognitive model (Beck et al., 2018; Grant et al., 2019), which posits that negative symptoms may lead to reductions in neurocognitive performance. However, this model has not been tested in long-term prospective studies. Further, the functional impact of this pathway is unclear, including whether neurocognition may partially mediate the association between negative symptoms and work functioning. Identifying the strongest putative causal pathway impacting long-term work functioning could clarify which domain (e.g., negative symptoms or neurocognition) should be prioritized in treatment.
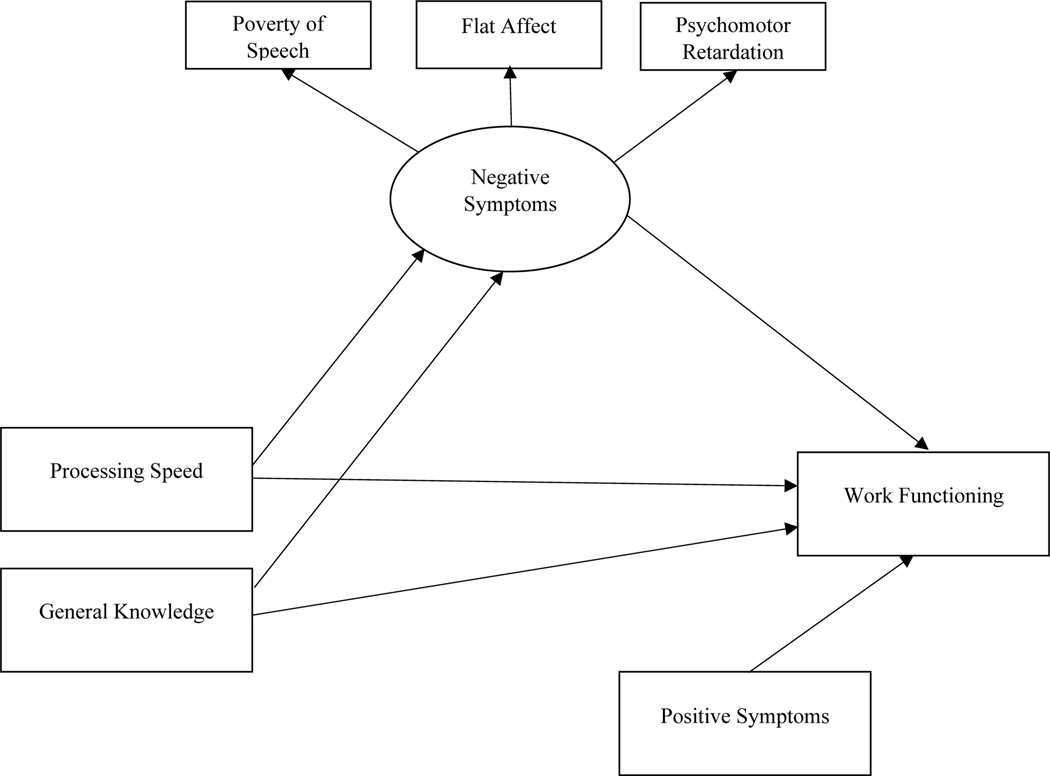
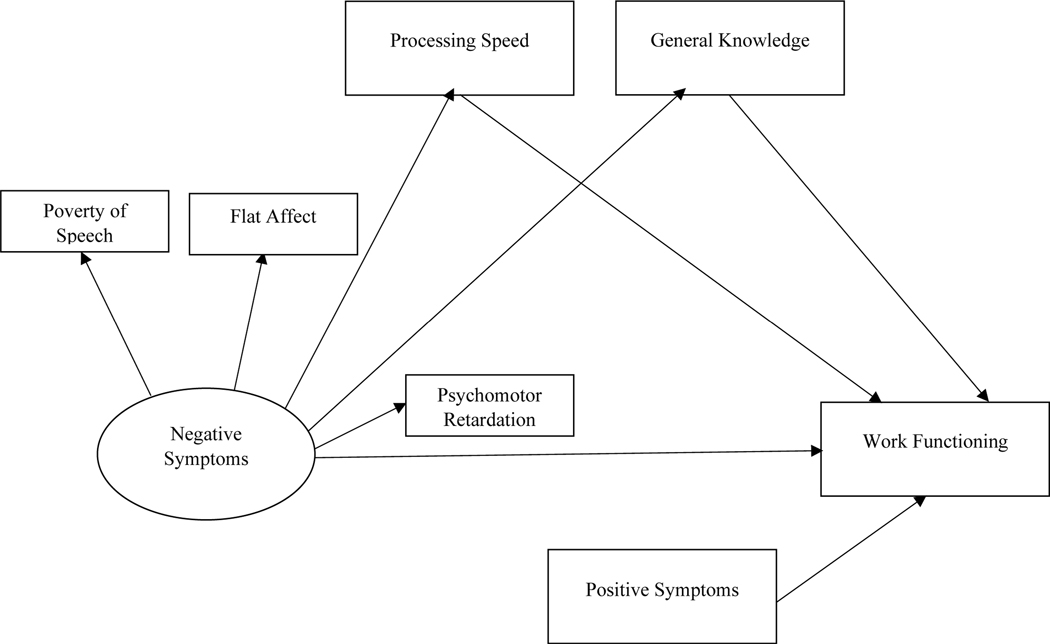
This study tested both of the aforementioned mediational models (see Figure 1, 2) to clarify the causal pathways to work outcomes using participants with SMI from the Harrow Chicago Follow-up study (Harrow et al., 2000; Harrow et al., 2014; Harrow et al., 1997), which included six follow-up assessments spanning 20 years. We first tested these models cross-sectionally in attempts to build on prior work examining negative symptoms as a partial mediator between neurocognition and community functioning in psychosis (Ventura et al., 2009) and to cross-sectionally test the model with neurocognition as a mediator between negative symptoms and work functioning. To examine the temporal order of these variables, we then examined these models using prospective data. Specifically, we examined whether the relationship between neurocognition assessed at the first follow-up (2-year) and work functioning assessed 7.5 years later was partially mediated by negative symptoms assessed at 4.5 years. We then tested whether 4.5-year neurocognition partially mediated the effects of 2-year negative symptoms on 7.5-year work functioning. If significant mediation was detected in either model, we then aimed to test whether the model remained significant when examining longer term work functioning (i.e., 10, 15, and 20-year follow-ups).
Figure 1.
Hypothesized model testing mediating effects of negative symptoms in associations between neurocognition and work functioning. For clarity, covariances and error terms are not depicted.
Figure 2.
Hypothesized model testing mediating effects of neurocognition in association between negative symptoms and work functioning. For clarity, covariances and error terms are not depicted.
2. Methods
2.1. Procedure
The Harrow Chicago Follow-up Study is a longitudinal observational research project designed to examine the course of SMI. Participants were identified during an index inpatient hospitalization and completed an initial interview within several weeks of hospitalization. Based on these interviews and hospital charts, participant diagnoses were determined using the Research Diagnostic Criteria (RDC; Spitzer et al., 1978). Negative symptoms and neurocognition were first assessed at the initial follow-up approximately two years after discharge from their index hospitalization and then during each of the five subsequent follow-ups (4.5-years, 7.5-years, 10-years, 15-years, and 20-years post-index hospitalization). For the current investigation, all participants with a SMI with psychotic features at index hospitalization were eligible to be included. The local institutional review board approved study procedures, and informed consent was obtained from all participants.
2.2. Participants
The sample consisted of 277 participants with a SMI with psychotic features at the initial follow-up (n = 128 with schizophrenia; n = 62 schizoaffective; n = 29 with psychotic depressive disorders; n = 43 with psychotic bipolar or unipolar mania; n = 15 with other psychotic disorders). At index hospitalization, participants had a mean age of 22.86 (SD = 3.95) and 12.99 (SD = 2.14) years of education. Approximately half of the participants were male (54.2%), and the majority identified as white (n = 190, 68.6%); the remaining identified as African American (n = 87, 31.4%).
2.3. Measures
2.3.1. Negative Symptoms.
Following prior studies (Herbener and Harrow, 2001, 2004; Pogue-Geile and Harrow, 1984), negative symptoms were assessed with 12 items from the Behavior Rating Schedule of the Psychiatric Assessment Interview (Carpenter et al., 1976). The interviewer-rated items included assessments of flat affect (sum of avoids looking at interviewer, expressionless face, reduced emotion, apathetic and uninterested, reduced voice inflection, and low voice items), poverty of speech (sum of long lapses prior to responses, restricted speech quantity, failure to answer questions, and slowed speech items) and psychomotor retardation (sum of slowed movements and voluntary movements reduction items). Items are rated on a 3-point scale ranging from 0 (absent) to 2 (present in marked form).
2.3.2. Positive Symptoms.
The interviewer-rated Schedule for the Affective Disorders and Schizophrenia (Endicott and Spitzer, 1978) was used to assess for positive symptoms. Hallucinations and delusions items were scored on a 3-point scale ranging from 1 (absent) to 3 (definitely present). Since positive symptoms have demonstrated modest associations with work functioning in some prior studies (McGurk and Mueser, 2004; Tsang et al., 2010), positive symptoms were included as a covariate in all mediational analyses.
2.3.3. Neurocognition.
Two subtests from the Wechsler Adult Intelligence Scale (WAIS; Wechsler, 1955) were used: 1) processing speed was assessed with the Digit Symbol-Coding subtest; 2) General knowledge was assessed by the Information subtest. The total number of correctly written symbols or questions answered correctly, respectively, were used.
2.3.4. Work Functioning.
The interviewer-rated Strauss and Carpenter (1972) outcome scale, which is rated on a 5-point (0–4) scale was used to assess working functioning (e.g., amount of past-year employment, including full-time, part-time, or partial-year).
2.4. Analyses
The mediational models were tested using structural equation modeling in AMOS 25.0 statistical software (Arbuckle, 2017). To create our mediational model, we first created a latent variable for negative symptoms consisting of the three negative symptom subscales. Manifest variables were used for work functioning, processing speed, and general knowledge. A manifest variable was used for positive symptoms, which was included as a covariate in all models. The model fit was estimated using three commonly used model fit indices (Hu and Bentler, 1999): the relative chi-square statistic (Wheaton, 1987) (p > .05 is preferred), the comparative fit index (CFI; Bentler, 1990) (>.90 is acceptable; > .95 is preferred), and the root-mean-square error of approximation (RMSEA; Steiger, 1980) (< .08 is acceptable; < .05 is preferred). Mediation was tested by examining the indirect effect of our predictor variable(s) of interest (model 1 = processing speed, general knowledge; model 2 = negative symptoms) on work functioning through our mediator(s) of interest (model 1 = negative symptoms; model 2 = processing speed, general knowledge). The significance of the indirect effect was tested using the PRODCLIN program (MacKinnon, Fritz, Williams, & Lockwood, 2007) in the RMediation web application (Tofighi and MacKinnon, 2011); significant mediation is present if the 95% confidence interval of the indirect effect does not include zero. If significant mediation was present, we distinguished between full and partial mediation by examining the direct effect (i.e., effect of predictor of interest on work functioning after accounting for the mediator of interest); partial mediation occurred if the direct effect was significant, while full mediation occurred when the direct effect was not significant (MacKinnon, Fairchild, and Fritz, 2007). We first tested each mediational model cross-sectionally using data from the 2-year follow-up, and then each model was tested with prospective data. If significant mediation (full or partial) was found in the initial prospective model, we then aimed to examine whether the model remained significant when examining longer-term work functioning (i.e., 10, 15, and 20-year follow-ups). In each mediational model, we used Full Information Maximum Likelihood estimation (FIML; Enders and Bandalos, 2001) to estimate missing data; this approach is appropriate to use even when missing data is as high as 50% (Schlomer, Bauman, & Card, 2010). Finally, for each model, we followed Cohen (1988) in categorizing the magnitude of R2 effect sizes (small = 0.1, medium = 0.3, and large = 0.5).
3. Results
Preliminary analyses. Over the course of the study, nine participants passed away and were excluded from relevant models. Further, for our main prospective model, 217 participants participated in the 4.5-year follow-up and 198 participated in the 7.5-year follow-up (see Table 1, 2, and Supplemental Table 1 for the number of participants who completed assessments at each time-point). No significant differences were observed in demographics or model variables between those that completed all follow-ups versus those that dropped out of the study at either 4.5-years or 7.5-years or any later follow-ups. Further, we also re-ran all prospective mediational models using only participants that were retained at the follow-ups examined in the model of interest, and the results were replicated; thus, we report the results using FIML below.
Table 1.
Mediation Results for Models with Negative Symptoms as Proposed Mediator Between Neurocognition and Work Functioning
| Path | β | B | SE | p-value |
|---|---|---|---|---|
| Cross-Sectional Model (n = 277) | ||||
| Indirect effect with processing speed: z = .01, SE = .01, 95% CI [.002, .03] | ||||
| Indirect effect with general knowledge: z = .01, SE = .01, 95% CI [−.01, .02] | ||||
| 2-year processing speed → 2-year work functioning | .21 | .02 | .01 | .01 |
| 2-year general knowledge → 2-year work functioning | .12 | .03 | .02 | .07 |
| 2-year negative symptoms → 2-year poverty of speecha,b | .78 | 1.00 | -- | -- |
| 2-year negative symptoms → 2-year flat affecta | .58 | 1.15 | .20 | < .001 |
| 2-year negative symptoms → 2-year psychomotor retardationa | .75 | .48 | .07 | < .001 |
| 2-year processing speed → 2-year negative symptoms | −.47 | −.03 | .01 | < .001 |
| 2-year general knowledge → 2-year negative symptoms | −.03 | −.01 | .01 | .71 |
| 2-year negative symptoms → 2-year work functioning | −.24 | −.48 | .20 | .02 |
| 2-year positive symptoms → 2-year work functioning | −.18 | −.34 | .12 | .004 |
| Prospective Model - 7.5-year work functioning (n = 277)c | ||||
| Indirect effect with processing speed: z = .002, SE = .003, 95% CI [−.002, .01] | ||||
| Indirect effect with general knowledge: z = .004, SE = .005, 95% CI [−.004, .02] | ||||
| 2-year processing speed → 7.5-year work functioning | .37 | .04 | .01 | < .001 |
| 2-year general knowledge → 7.5-year work functioning | −.002 | −.001 | .02 | .98 |
| 4.5-year negative symptoms → 4.5-year poverty of speecha,b | .98 | 1.00 | -- | -- |
| 4.5-year negative symptoms → 4.5-year flat affecta | .70 | .77 | .11 | < .001 |
| 4.5-year negative symptoms → 4.5-year psychomotor retardationa | .61 | .32 | .05 | < .001 |
| 2-year processing speed → 4.5-year negative symptoms | −.10 | −.01 | .01 | .29 |
| 2-year general knowledge → 4.5-year negative symptoms | −.10 | −.02 | .02 | .29 |
| 4.5-year negative symptoms → 7.5-year work functioning | −.14 | −.20 | .11 | .07 |
| 2-year positive symptoms → 7.5-year work functioning | −.18 | −.34 | .13 | .01 |
Loadings are for observed negative symptom subscales on the latent negative symptoms indicator
Regression weight set at 1
217 participants participated in the 4.5 year follow-up and 198 participated in the 7.5 year follow-up; FIML was used to estimate missing data.
Table 2.
Mediation Results for Models with Neurocognition as Proposed Mediator Between Negative Symptoms and Work Functioning
| Path | β | B | SE | p-value |
|---|---|---|---|---|
| Cross-Sectional Model (n = 277)_ | ||||
| Indirect effect through processing speed: z = −.26, SE = .10, 95% CI [−.48, −.08] | ||||
| Indirect effect through general knowledge: z = −.05, SE = .04, 95% CI [−.15, .02] | ||||
| 2-year negative symptoms → 2-year poverty of speecha,b | .78 | 1.00 | -- | -- |
| 2-year negative symptoms → 2-year flat affecta | .58 | 1.13 | .20 | < .001 |
| 2-year negative symptoms → 2-year psychomotor retardationa | .74 | .47 | .07 | < .001 |
| 2-year negative symptoms → 2-year work functioning | −.24 | −.48 | .20 | .02 |
| 2-year negative symptoms → 2-year processing speed | −.50 | −8.73 | 1.63 | < .001 |
| 2-year negative symptoms → 2-year general knowledge | −.23 | −1.69 | .69 | .01 |
| 2-year processing speed → 2-year work functioning | .22 | .03 | .01 | .01 |
| 2-year general knowledge → 2-year work functioning | .12 | .03 | .02 | .09 |
| 2-year positive symptoms → 2-year work functioning | −.17 | −.31 | .12 | .01 |
| Prospective Model - 7.5-year work functioning (n = 277)c | ||||
| Indirect effect through processing speed: z = −.20, SE = .09, 95% CI [−.39, −.05] | ||||
| Indirect effect through general knowledge: z = .02, SE = .05, 95% CI [−.07, .13] | ||||
| 2-year negative symptoms → 2-year poverty of speecha,b | .77 | 1.00 | -- | -- |
| 2-year negative symptoms → 2-year flat affecta | .57 | 1.14 | .20 | < .001 |
| 2-year negative symptoms → 2-year psychomotor retardationa | .76 | .49 | .08 | < .001 |
| 2-year negative symptoms → 7.5-year work functioning | −.30 | −.61 | .22 | .006 |
| 2-year negative symptoms → 4.5-year processing speed | −.37 | −6.50 | 1.88 | < .001 |
| 2-year negative symptoms → 4.5-year general knowledge | −.30 | −2.21 | .80 | .006 |
| 4.5-year processing speed → 7.5-year work functioning | .26 | .03 | .01 | .002 |
| 4.5-year general knowledge → 7.5-year work functioning | −.03 | −.01 | .02 | .71 |
| 2-year positive symptoms → 7.5-year work functioning | −.19 | −.36 | .14 | .009 |
Loadings are for observed negative symptom subscales on the latent negative symptoms indicator
Regression weight set at 1
217 participants participated in the 4.5 year follow-up and 198 participated in the 7.5 year follow-up; FIML was used to estimate missing data.
Cross-sectional models. Model fit was excellent (χ2 = 10.32, df = 9, p = .33; CFI = .99; RMSEA = .02) with 2-year negative symptoms as a possible mediator between 2-year neurocognition domains (processing speed and general knowledge) and 2-year work functioning (see Table 1 and Supplemental Figure 1 for parameter estimates). Examination of direct effects showed that lower processing speed was significantly associated with lower work functioning (β = .21, p = .01), while general knowledge was only marginally associated with work functioning (β = .12, p = .07). Greater positive symptoms were associated with lower work functioning (β = −.18, p = .004). In terms of indirect effects, lower processing speed was significantly associated with higher negative symptoms (β = −.47, p < .001), which in turn predicted lower work functioning (β = −.24, p = .02); this indirect path was significant (z = .01, SE = .01, 95% CI [.002, .03]). General knowledge did not significantly predict negative symptoms (β = −.03, p = .71); thus, 2-year negative symptoms partially mediated the influence of 2-year processing speed–but not 2-year general knowledge–on 2-year work functioning. The total model explained 27% of the variance in 2-year work functioning, a medium effect size.
Model fit was good (χ2 = 17.08, df = 10, p = .07; CFI = .97; RMSEA = .05) when 2-year neurocognition domains were tested as mediators between 2-year negative symptoms and 2-year work functioning (see Table 2 and Supplemental Figure 2 for parameter estimates). There was a significant direct effect from negative symptoms to work functioning (β = −.24, p = .02). Greater negative symptoms predicted lower processing speed (β = −.50, p < .001), which then predicted lower work functioning (β = .22, p = .01); this indirect effect was significant (z = −.26, SE = .10, 95% CI [−.48, −.08]). Higher negative symptoms also predicted lower general knowledge (β = −.23, p = .01), but general knowledge only then marginally predicted work functioning (β = .12, p = .09). Thus, 2-year processing speed (but not 2-year general knowledge) significantly and partially mediated between 2-year negative symptoms and 2-year work functioning. Two-year positive symptoms were also associated with lower 2-year work functioning (β = −.17, p = .01). This model explained 26% of the variance in 2-year work functioning (medium effect size).
Prospective models. Model fit was excellent (χ2 = 6.89, df = 9, p = .65; CFI = 1.00; RMSEA = .00) with 4.5-year negative symptoms as a potential mediator between 2-year neurocognition domains and 7.5-year work functioning (see Table 1 and Supplemental Figure 3 for parameter estimates). Similar to the cross-sectional model, the direct effect between 2-year processing speed and 7.5-year work functioning was significant (β = .37, p < .001), and the direct effect from 2-year general knowledge to 7.5-year work functioning was non-significant (β = −.002, p = .98). However, neither 2-year processing speed (β = −.10, p = .29) nor general knowledge (β = −.10, p = .29) predicted 4.5-year negative symptoms; 4.5-year negative symptoms were marginally predictive of 7.5-year work functioning (β = −.14, p = .07). Thus, there was no evidence of an indirect effect. Two-year positive symptoms were predictive of reduced 7.5 work functioning (β = −.18, p = .01). This model explained 24% of the variance in 7.5-year work functioning (medium effect size).
Model fit was excellent (χ2 = 10.96, df = 10, p = .36; CFI = .99; RMSEA = .02) with 4.5-year neurocognition domains as possible mediators between 2-year negative symptoms and 7.5-year work functioning (see Table 2 and Supplemental Figure 4 for parameter estimates). Akin to the cross-sectional model, there was a significant direct effect from 2-year negative symptoms to 7.5-year work functioning (β = −.30, p = .006). Greater 2-year negative symptoms predicted lower 4.5-year processing speed (β = −.37, p < .001), which in turn predicted lower 7.5-year work functioning (β = .26, p = .002); this indirect effect was significant (z = −.20, SE = .09, 95% CI [−.39, −.05]). Greater 2-year negative symptoms also predicted reduced 4.5-year general knowledge (β = −.30, p = .006), but general knowledge did not significantly predict work functioning (β = −.03, p = .71). Similar to the cross-sectional model, 4.5-year processing speed (and not 4.5-year general knowledge) was a significant partial mediator between 2-year negative symptoms and 7.5-year work functioning. Greater two-year positive symptoms were also associated with lower 7.5-year work functioning (β = −.19, p = .009). This model explained 26% of the variance in 7.5-year work functioning (medium effect size).
Model fit remained excellent with 4.5-year neurocognition domains as mediators between 2-year negative symptoms and 10-year, 15-year, and 20-year work functioning (See supplemental Figures 5–7 and supplemental Table 1 for fit statistics and parameter estimates). In all three models, there was a significant indirect effect of negative symptoms on work functioning through 4.5 year processing speed (10-year: z =−.37, SE = .12, 95% CI [−.63, −.15]; 15-year: z = −.21, SE = .09, 95% CI [−.41, −.06]; 20-year: z = −.21, SE = .09, 95% CI [−.42, −.06]); the indirect effect of general knowledge remained non-significant in each model. However, in contrast to the cross-sectional and 7.5-year work functioning model, there were no significant direct effects of 2-year negative symptoms on work functioning at either 10, 15, or 20-years, which is consistent with full mediation. Further, 2-year positive symptoms no longer significantly predicted 20-year work functioning but significantly predicted 10 and 15-year work functioning. The variance explained in work functioning for each model was: 21% for 10-year, 23% at 15-year, and 20% at 20-year (all medium effects).
4. Discussion
Competitive employment is a critical ingredient of recovery for many with SMI. However, extant interventions do not efficiently improve work functioning in a sizeable proportion of individuals with SMI. Prior work has demonstrated that neurocognition plays an important role in work functioning, and more recent work has shed light on how negative symptoms may also reduce work functioning. In attempts to better identify the causal pathways among negative symptoms, neurocognition, and long-term work functioning, we tested two putative causal models. Using both cross-sectional and prospective data spanning 20-years, we first tested a previously identified model suggesting that neurocognition may directly and indirectly (i.e., partially mediate) influence work outcomes through its impact on negative symptoms. We also aimed to examine a divergent model that is informed by the recent alternative cognitive model (Beck et al., 2018; Grant et al., 2019): whether greater negative symptoms predict reduced neurocognition and indirectly influence work functioning through their impact on neurocognition.
In line with the broader work functioning literature highlighting the importance of both neurocognition and negative symptoms on work functioning (Llerena et al., 2018; Tsang et al., 2010), our results supported both mediational models when these domains and work functioning were measured concurrently. Consistent with prior models (Meyer et al., 2014; Nakagami et al., 2008; Ventura et al., 2009), we observed that negative symptoms partially mediated the effects of reduced neurocognition–specifically processing speed–on lower work functioning. Notably, these findings extend these prior models by demonstrating that this cross-sectional mediation model applies to the more specific functional domain of work functioning in those who have transitioned to an SMI diagnosis. Further, in line with more recent studies that have demonstrated links between greater negative symptoms and lower neuropsychological test performance (Fervaha et al., 2014; Foussias et al., 2015; Strauss et al., 2015), we observed that reduced processing speed was also a partial mediator between greater negative symptoms and poorer work functioning. Together these models suggest that at the cross-sectional level, neurocognition and negative symptoms may have a bidirectional relationship. This is consistent with the notion that these variables have some common underlying features (Harvey et al., 2006). It may be that some domains of clinician-rated negative symptoms (e.g., reduced emotional experience or apathy) influence different elements of performance-based processing speed (e.g., relational memory or visual scanning efficiency; Bachman et al., 2010) which in turn influence other domains of negative symptoms (i.e., alogia) or vice versa. Future studies using more precise or multiple elements of processing speed may help to elucidate this relationship both cross-sectionally and prospectively. In addition, these results build on prior work that has largely been driven by the theory that reduced neurocognition causes or leads to greater negative symptoms, which in turn leads to reduced functional outcomes (Ventura et al., 2009) by also demonstrating that the reverse relationship–that greater negative symptoms predict reduced neurocognition and in turn poor functional outcomes–is also true in concurrent models.
To help clarify the temporal order of these relationships, we then examined these models prospectively. Notably, only the prospective models examining neurocognition as a mediator between negative symptoms and work functioning demonstrated significant pathways consistent with mediation. Similar to the cross-sectional model, 4.5-year processing speed—and not general knowledge—was a significant partial mediator of the effects of 2-year negative symptoms on 7.5-year work functioning; this significant indirect effect extended to 10, 15, and 20-year work functioning, suggesting that this pathway is critical to work outcomes even decades later. Alternatively, we found no evidence that 4.5-year negative symptoms significantly mediated the relationship between 2-year neurocognition–either processing speed or general knowledge–and 7.5-year work functioning. Given that prospective models offer a stronger test of mediation than cross-sectional models (Maxwell and Cole, 2007), our results provide greater support for a putative causal pathway running from negative symptoms to neurocognition—rather than the reverse—to work functioning. Notably, these prospective findings are inconsistent with the more common theory that lower neurocognition leads to greater negative symptoms and instead support the alternative cognitive model (Beck et al., 2018; Grant et al., 2019) suggesting that negative symptoms lead to poorer neurocognition.
Our prospective model findings are consistent with prior work showing negative symptoms are a significant predictor as well as cross-sectional and prospective correlate of neurocognition (Fervaha et al., 2014; Foussias et al., 2015; Strauss et al., 2015). Together, these findings suggest two possibilities. First, it is likely that negative symptoms such as apathy influence performance on processing speed tests. Second, it may be that as negative symptoms become more prolonged, they contribute to reduced engagement and participation in the community or activities of daily life, which could lead to less use of neurocognitive resources. This reduction of use of neurocognitive abilities and behavioral engagement may in turn lead to a diminution in neurocognitive abilities and in turn (Thomas et al., 2019), poorer performance at work.
In addition, we observed in both cross-sectional and prospective models that processing speed was a stronger predictor of work functioning than general knowledge. The specificity of processing speed is consistent with a prior study by Bell and Bryson (2001) who found that baseline processing speed was particularly critical to improvement in 6-month work outcomes among those in a vocational rehabilitation program. Further, the importance of processing speed aligns with meta-analytic findings showing that at the group level, people with psychosis have the lowest performance on digit symbol coding processing speed tasks relative to all other commonly used neuropsychological measures (Dickinson et al., 2007). Relatedly, we observed that in all cross-sectional and prospective mediational models, positive symptoms predicted work functioning after accounting for all other predictor variables (i.e., negative symptoms and neurocognition). Although positive symptoms have shown modest associations with work functioning in some but not all studies (McGurk and Mueser, 2004; Tsang et al., 2010), few studies have examined this relationship over more than a few years. Our findings suggest that positive symptoms can significantly influence prospective work outcomes up to fifteen years later among those with SMI.
Although a strength of this study was its longitudinal design, there were some limitations that should be noted. The length of the study precluded the use of more recent negative symptom measures such as the Clinical Assessment Interview for Negative Symptoms (Kring et al., 2013) that can more comprehensively assess some negative symptom domains (i.e., experiential negative symptoms). Similarly, while processing speed reductions have been widely implicated in SMI, future studies should examine additional domains such as working memory. Although both cross-sectional and prospective models explained 20–27% of the variance in work functioning, future studies should include additional factors that have been linked to work functioning or that might influence the tested mediational pathways (e.g., trauma history, internalized stigma, social skills, and substance use (Bell et al., 2008; McGurk et al., 2009; Tsang et al., 2010). Relatedly, a limitation is that we did not assess antipsychotic medication doses, and additional work is needed to evaluate the impact of antipsychotic medication doses and side effects on the identified temporal pathways. In addition, more work is needed to examine whether there are factors that may moderate the observed pathways, including whether there are certain subgroups (e.g., those with persistent negative symptoms) that demonstrate stronger or weaker relationships among the mediational pathways. Additionally, although this work helps to clarify the temporal order of the impact of negative symptoms and neurocognition on work functioning, future work could also examine the incremental predictive validity of each of these domains on work functioning. Lastly, the availability of employment opportunities for persons with SMI may have been more limited, especially during the earlier follow-ups, than what is currently available.
These findings have several implications for interventions targeting vocational outcomes among those with SMI. Although our results align with prior work suggesting that that cognitive remediation may be an important adjunct for vocational rehabilitation (McGurk and Wykes, 2008; Wexler and Bell, 2005), our mediational findings also suggest that incorporating interventions that target negative symptoms prior to or in conjunction with cognitive remediation could be more beneficial for long-term work outcomes. Specifically, our findings of neurocognition (i.e., processing speed) as a partial mediator between negative symptoms and work functioning 7.5 years later suggest that targeting negative symptoms with interventions such as CBT, Metacognitive Reflection and Insight Therapy, or repetitive transcranial magnetic stimulation (Grant et al., 2012; Lysaker and Klion, 2017; Shi et al., 2014) may directly as well as indirectly improve subsequent work functioning. Further, our findings suggest that targeting negative symptoms prior to neurocognition may have the greatest impact, as improving negative symptoms could improve prospective processing speed and general knowledge and in turn, prospective work functioning. Alternatively, while our findings suggest that targeting neurocognition alone may help to break down the influence of negative symptoms on 10, 15, and 20-year work functioning (i.e., where we observed full mediation), they also suggest that targeting neurocognition alone will have limited direct impact on prospective negative symptoms and may not help to alleviate the impact of negative symptoms on 7.5 year work functioning (i.e., where partial mediation was observed). Ultimately, to better enhance prospective work functioning, vocational rehabilitation programs could prioritize negative symptoms treatments or use them in conjunction with cognitive remediation that specifically targets processing speed.
Supplementary Material
References
- Addington J, Cadenhead KS, Cannon TD, Cornblatt B, McGlashan TH, Perkins DO, Seidman LJ, Tsuang M, Walker EF, Woods SW, 2007. North American Prodrome Longitudinal Study: a collaborative multisite approach to prodromal schizophrenia research. Schizophr. Bull 33 (3) 665–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anthony WA, 1993. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosoc. Rehabilitation J 16 (4) 11–23. [Google Scholar]
- Arbuckle JL, 2017. Amos (version 25.0)[computer program]. Chicago: IBM SSSS. [Google Scholar]
- Bachman P, Reichenberg A, Rice P, Woolsey M, Chaves O, Martinez D, Maples N, Velligan DI, Glahn DC, 2010. Deconstructing processing speed deficits in schizophrenia: application of a parametric digit symbol coding test. Schizophr. Res 118 (1–3) 6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Himelstein R, Bredemeier K, Silverstein SM, Grant P, 2018. What accounts for poor functioning in people with schizophrenia: a re-evaluation of the contributions of neurocognitive v. attitudinal and motivational factors. Psychol. Med 48 (16) 2776–2785. [DOI] [PubMed] [Google Scholar]
- Bell M, Tsang HW, Greig TC, Bryson GJ, 2008. Neurocognition, social cognition, perceived social discomfort, and vocational outcomes in schizophrenia. Schizophr. Bull 35 (4) 738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell MD, Bryson G, 2001. Work rehabilitation in schizophrenia: does cognitive impairment limit improvement? Schizophr. Bull 27 (2) 269–279. [DOI] [PubMed] [Google Scholar]
- Bentler PM, 1990. Comparative fit indexes in structural models. Psychological bulletin 107 (2) 238–46. [DOI] [PubMed] [Google Scholar]
- Brantschen E, Kawohl W, Rössler W, Bärtsch B, Nordt C, 2014. Supported employment–improving competitive employment for people with mental illness: The role of motivation and social network. J. Vocat. Rehabil 40 (1) 41–47. [Google Scholar]
- Carpenter WT, Sacks MH, Strauss JS, Bartko JJ, Rayner J, 1976. Evaluating signs and symptoms: Comparison of structured interview and clinical approaches. Br. J. Psychiatry 128 (4) 397–403. [DOI] [PubMed] [Google Scholar]
- Dickinson D, Ramsey ME, Gold JM, 2007. Overlooking the obvious: a meta-analytic comparison of digit symbol coding tasks and other cognitive measures in schizophrenia. Arch. Gen. Psychiatry 64 (5) 532–542. [DOI] [PubMed] [Google Scholar]
- Enders CK, Bandalos DL, 2001. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equ. Modeling 8 (3) 430–457. [Google Scholar]
- Endicott J, Spitzer RL, 1978. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch. Gen. Psychiatry 35 (7) 837–844. [DOI] [PubMed] [Google Scholar]
- Erickson M, Jaafari N, Lysaker P, 2011. Insight and negative symptoms as predictors of functioning in a work setting in patients with schizophrenia. Psychiatry Res. 189 (2) 161–165. [DOI] [PubMed] [Google Scholar]
- Evensen S, Wisloff T, Lystad JU, Bull H, Ueland T, Falkum E, 2016. Prevalence, Employment Rate, and Cost of Schizophrenia in a High-Income Welfare Society: A Population-Based Study Using Comprehensive Health and Welfare Registers. Schizophr. Bull 42 (2) 476–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkas M, 2007. The vision of recovery today: what it is and what it means for services. World Psychiatry. 6 (2) 68–74. [PMC free article] [PubMed] [Google Scholar]
- Fervaha G, Zakzanis KK, Foussias G, Graff-Guerrero A, Agid O, Remington G, 2014. Motivational deficits and cognitive test performance in schizophrenia. JAMA Psychiatry. 71 (9) 1058–1065. [DOI] [PubMed] [Google Scholar]
- Foussias G, Siddiqui I, Fervaha G, Mann S, McDonald K, Agid O, Zakzanis KK, Remington G, 2015. Motivated to do well: an examination of the relationships between motivation, effort, and cognitive performance in schizophrenia. Schizophr. Res 166 (1–3) 276–282. [DOI] [PubMed] [Google Scholar]
- Grant PM, Best MW, Beck AT, 2019. The meaning of group differences in cognitive test performance. World Psychiatry. 18 (2) 163–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant PM, Huh GA, Perivoliotis D, Stolar NM, Beck AT, 2012. Randomized trial to evaluate the efficacy of cognitive therapy for low-functioning patients with schizophrenia. Arch. Gen. Psychiatry 69 (2) 121–127. [DOI] [PubMed] [Google Scholar]
- Harrow M, Grossman LS, Herbener ES, Davies EW, 2000. Ten-year outcome: patients with schizoaffective disorders, schizophrenia, affective disorders and mood-incongruent psychotic symptoms. Br. J Psychiatry 177 421–426. [DOI] [PubMed] [Google Scholar]
- Harrow M, Jobe TH, Faull RN, 2014. Does treatment of schizophrenia with antipsychotic medications eliminate or reduce psychosis? A 20-year multi-follow-up study. Psychol. Med 44 (14) 3007–3016. [DOI] [PubMed] [Google Scholar]
- Harrow M, Sands JR, Silverstein ML, Goldberg JF, 1997. Course and outcome for schizophrenia versus other psychotic patients: a longitudinal study. Schizophr. Bull 23 (2) 287–303. [DOI] [PubMed] [Google Scholar]
- Harvey PD, Green MF, Bowie C, Loebel A, 2006. The dimensions of clinical and cognitive change in schizophrenia: evidence for independence of improvements. Psychopharmacology. 187 (3) 356–363. [DOI] [PubMed] [Google Scholar]
- Herbener ES, Harrow M, 2001. Longitudinal assessment of negative symptoms in schizophrenia/schizoaffective patients, other psychotic patients, and depressed patients. Schizophr. Bull 27 (3) 527–537. [DOI] [PubMed] [Google Scholar]
- Herbener ES, Harrow M, 2004. Are negative symptoms associated with functioning deficits in both schizophrenia and nonschizophrenia patients? A 10-year longitudinal analysis. Schizophr. Bull 30 (4) 813–825. [DOI] [PubMed] [Google Scholar]
- Hu L.t., Bentler PM, 1999. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equ. Modeling 6 (1) 1–55. [Google Scholar]
- Hunter R, Barry S, 2012. Negative symptoms and psychosocial functioning in schizophrenia: neglected but important targets for treatment. Eur. Psychiatry 27 (6) 432–436. [DOI] [PubMed] [Google Scholar]
- Kinoshita Y, Furukawa TA, Kinoshita K, Honyashiki M, Omori IM, Marshall M, Bond GR, Huxley P, Amano N, Kingdon D, 2013. Supported employment for adults with severe mental illness. Cochrane Database of Systematic Reviews (9) CD008297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP, 2013. The clinical assessment interview for negative symptoms (CAINS): final development and validation. Am. J. Psychiatry 170 (2) 165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kukla M, Strasburger AM, Salyers MP, Rollins AL, Lysaker PH, 2018. A Pilot Test of Group Based Cognitive Behavioral Therapy to Augment Vocational Services for Persons With Serious Mental Illness: Feasibility and Competitive Work Outcomes. J. Nerv. Men. Dis 206 (5) 310–315. [DOI] [PubMed] [Google Scholar]
- Llerena K, Reddy LF, Kern RS, 2018. The role of experiential and expressive negative symptoms on job obtainment and work outcome in individuals with schizophrenia. Schizophr. Res 192 148–153. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Davis LW, Bryson GJ, Bell MD, 2009. Effects of cognitive behavioral therapy on work outcomes in vocational rehabilitation for participants with schizophrenia spectrum disorders. Schizophr. Res 107 (2–3) 186–191. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Klion RE, 2017. Recovery, meaning-making, and severe mental illness: A comprehensive guide to metacognitive reflection and insight therapy. Routledge, New York. [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS 2007. Mediation analysis. Annu. Rev. Psychol 58: 593–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA, 2007. Bias in cross-sectional analyses of longitudinal mediation. Psychol. Methods 12 (1) 23–44. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, 2004. Cognitive functioning, symptoms, and work in supported employment: a review and heuristic model. Schizophr. Res 70 (2–3) 147–173. [DOI] [PubMed] [Google Scholar]
- McGurk SR, Mueser KT, DeRosa TJ, Wolfe R, 2009. Work, recovery, and comorbidity in schizophrenia: a randomized controlled trial of cognitive remediation. Schizophr. Bull 35 (2) 319–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGurk SR, Wykes T, 2008. Cognitive remediation and vocational rehabilitation. Psychiatr. Rehabil. J 31 (4) 350–359. [DOI] [PubMed] [Google Scholar]
- Meyer EC, Carrión RE, Cornblatt BA, Addington J, Cadenhead KS, Cannon TD, McGlashan TH, Perkins DO, Tsuang MT, Walker EF, 2014. The relationship of neurocognition and negative symptoms to social and role functioning over time in individuals at clinical high risk in the first phase of the North American Prodrome Longitudinal Study. Schizophr. Bull 40 (6) 1452–1461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakagami E, Xie B, Hoe M, Brekke JS, 2008. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: testing mediator and moderator effects. Schizophr. Res 105 (1–3) 95–104. [DOI] [PubMed] [Google Scholar]
- Pogue-Geile MF, Harrow M, 1984. Negative and positive symptoms in schizophrenia and depression: a followup. Schizophr. Bull 10 (3) 371–87. [DOI] [PubMed] [Google Scholar]
- Quinlan T, Roesch S, Granholm E, 2014. The role of dysfunctional attitudes in models of negative symptoms and functioning in schizophrenia. Schizophr. Res 157(1–3), 182–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenheck R, Leslie D, Keefe R, McEvoy J, Swartz M, Perkins D, Stroup S, Hsiao JK, Lieberman J, Group CSI, 2006. Barriers to employment for people with schizophrenia. Am. J. Psychiatry 163 (3) 411–417. [DOI] [PubMed] [Google Scholar]
- Saperstein AM, Fiszdon JM, Bell MD, 2011. Intrinsic motivation as a predictor of work outcome after vocational rehabilitation in schizophrenia. J. Nerv. Ment. Dis 199 (9) 672–677. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA (2010). Best practices for missing data management in counseling psychology. J Couns. Psychol 57 1–10. [DOI] [PubMed] [Google Scholar]
- Shamsi S, Lau A, Lencz T, Burdick KE, DeRosse P, Brenner R, Lindenmayer J-P, Malhotra AK, 2011. Cognitive and symptomatic predictors of functional disability in schizophrenia. Schizophr. Res 126 (1–3) 257–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi C, Yu X, Cheung EF, Shum DH, Chan RC, 2014. Revisiting the therapeutic effect of rTMS on negative symptoms in schizophrenia: a meta-analysis. Psychiatry Res. 215 (3) 505–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Endicott J, Robins E, 1978. Research diagnostic criteria: Rationale and reliability. Arch. Gen. Psychiatry 35 (6) 773–82. [DOI] [PubMed] [Google Scholar]
- Steiger JH, 1980. Statistically based tests for the number of common factors, the annual meeting of the Psychometric Society, Iowa City, IA. [Google Scholar]
- Strauss GP, Morra LF, Sullivan SK, Gold JM, 2015. The role of low cognitive effort and negative symptoms in neuropsychological impairment in schizophrenia. Neuropsychology 29 (2) 282–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauss JS, Carpenter WT, 1972. The prediction of outcome in schizophrenia: I. Characteristics of outcome. Arch. Gen. Psychiatry 27 (6) 739–746. [DOI] [PubMed] [Google Scholar]
- Thomas EC, Snethen G, McCormick B, Salzer MS, in press. An exploration of linear and curvilinear relationships between community participation and neurocognition among those with serious mental illnesses. Psychiatr. Rehabil. J [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi D, MacKinnon DP, 2011. RMediation: An R package for mediation analysis confidence intervals. Behav. Res. Methods 43 (3) 692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsang HW, Leung AY, Chung RC, Bell M, Cheung WM, 2010. Review on vocational predictors: systematic review of predictors of vocational outcomes among individuals with schizophrenia: an update since 1998. Aust. N. Z. J. Psychiatry 44 (6) 495–504. [DOI] [PubMed] [Google Scholar]
- Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH, 2009. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr. Res 113 (2–3) 189–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J, Subotnik KL, Gitlin MJ, Gretchen-Doorly D, Ered A, Villa KF, Hellemann GS, Nuechterlein KH, 2015. Negative symptoms and functioning during the first year after a recent onset of schizophrenia and 8 years later. Schizophr. Res 161 (2–3) 407–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D, 1955. Manual for the Wechsler adult intelligence scale. Psychological Corporation, Oxford, England. [Google Scholar]
- Wexler BE, Bell MD, 2005. Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophr. Bull 31 (4) 931–941. [DOI] [PubMed] [Google Scholar]
- Wheaton B, 1987. Assessment of fit in overidentified models with latent variables. Sociol. Methods Res 16 (1) 118–154. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.