Abstract
The human coronavirus disease-2019 (COVID-19) caused by SARS-CoV-2 is now a global pandemic. Personal hygiene such as hand-washing, the use of personal protective equipment, and social distancing via local and national lockdowns are used to reduce the risk of transmission of SARS-CoV-2. COVID-19 and the associated lockdowns may have significant impacts on environmental quality and ergonomics. However, limited studies exists on the impacts of COVID-19 and the associated lockdowns on environmental quality and ergonomics in low-income settings. Therefore, the present study investigated the impacts of the COVID-19 outbreak on socioeconomics, ergonomics and environment (water quality, air quality and noise) in Uttarakhand, India. Approximately 55% of respondents experienced headaches, and the other common health-related issue was back pain, with 45% of respondents having problems with their backs. Water and air quality significantly improved during the lockdown relative to the pre-lockdown period, but was observed to return to their previous characteristics afterwards. Lockdowns significant increased the concentration of indoor air pollutants while noise pollution levels significantly declined. In summary, lockdowns have adverse impacts on ergonomics, resulting in work-related human health risks. The impacts of lockdowns on environmental quality are mixed: temporary improvements on water and air quality, and noise reduction were observed, but indoor air quality deteriorated. Therefore, during lockdowns there is a need to minimize the adverse environmental and ergonomic impacts of lockdowns while simultaneously enhancing the beneficial impacts.
Keywords: Air quality, Coronavirus, Ergonomics, Human health, Water quality
Graphical Abstract
Nomenclature
- WHO
World Health Organization
- CDC
Centers for Disease Control and Prevention
- PM
Particulate matter
- BOD
Biochemical oxygen demand
- COD
Chemical Oxygen Demand
- DO
Dissolved Oxygen
- TWA
Time weighted Average
- TDS
Total Dissolved Solids
- MPN
Most Probable Number
- CPCB
Central Pollution Control Board
- VOCs
Volatile organic compounds
- IAQ
Indoor Air Quality
1. Introduction
In the later part of the year 2019, there was an outbreak of the human coronavirus disease 2019 (COVID-19) which originated from Wuhan, China; one of the most densely populated cities with a population of more than eleven million [1], [2] . Twenty-seven (27) cases of pneumonia of unknown etiology were initially reported in Wuhan, and the patients showed common symptoms of fever, dry cough, and dyspnea. All the cases were related to the Huanan Seafood market of Wuhan city which trades in live animals including bats, fish, and snakes [3], [4]. It was declared as pandemic by WHO on 11 March 2020 with total confirmed cases of 9720 including 213 fatalities till 31 January in China [5], [6]. Through numerous studies conducted it was found that bats are the probable source which leads to the spread of this infectious virus [7]. Coronaviruses are a group of enveloped, widely varied, ribonucleic acid (RNA) viruses with a single molecule of linear positive-sense and single-stranded [8], [9].
Infected individuals had respiratory disorder (ranging from mild to severe) but patients showing mild symptoms did not require any special medical attention. Severe cases required special care due to more severe respiratory problems which may finally lead to fatality [10], [11]. In four to five days symptoms may occur or the person could be complete asymptomatic. The appearance of the symptoms totally depends upon the individual immunity which includes fever, throat problem, loss of smell and taste, difficulty in breathing, rashes on skin [12], [13], [14]. Elderly people above seventy years are more prone to get affected as well as those having a medical history of diabetes, heart disease, and respiratory disorders [15], [16], [17]. As of 8 January 2021, India has reported 10.4 million total cases in which 10 million had recovered and 150 thousand people have lost their life due to the ongoing pandemic. Two vaccines have been approved for emergency use only and other vaccine trials are going on which are a sign of positive outcomes [18]. The virus is primarily transmitted by droplets that are produced when a person having the disease exhales, coughs or sneezes, and these droplets (diameter is > 5–10 micrometer) tend to stay in the air for 3 h and are capable of reaching a distance of up to 10 m [19], [20]. There are high chances of getting infected by coming closer to the vicinity of an infected person or touching the mouth, nose, or eyes after touching a contaminated surface [21], [22], [23]. The studies describing the pathophysiological behavior of COVID-19 have considerable doubt about its spread mechanism [24], [25]. The present information is primarily derived from related coronaviruses spread by respiratory formative from human-to-human [26], [27].
When a patient is symptomatic, viruses are typically the most infectious. However, evidence is indicating that transmission among humans can occur during the asymptomatic incubation time, estimated to be 2–10 days [28], [29]. Various international bodies like the World Health Organization (WHO) and Center for Disease Control and Prevention (CDC) released several advisory guidelines to decrease the spread rate [30]. They suggest restricting travel to high-risk areas, and interaction with symptomatic people, and stopping the intake of meat from regions with a confirmed outbreak of COVID-19 [31]. Frequent hand washing, use of sanitizer and use of face masks are strongly recommended [32], [33], [34]. Countries like Japan and India use applications like ‘Bebot’ and ‘Arogya setu’ which provides the current status of the disease, preventive measures to stop the spread, and a symptom checker as well [35], [36], [37]. To avoid a deteriorating pandemic situation, the Indian government took stringent public health measures such as the stay-at-home directive or national lockdown. In certain nations, this has restricted their operations, minimized road traffic, and forced flights to a stand-still [38], [39].
The first confirmed case of COVID-19 in India was identified in Kerala, on 30 January 2020, when a university student from Wuhan returned to the state [40], [41]. There was a rising number of cases in India, hence, lockdown was implemented throughout the country starting from 25 March till 31 May 2020 (Lockdown from Phase 1 to phase 4). Depending on the conditions, the lockdown continued until 30 June 2020 in various parts [42], [43], [44]. The lockdown helped to bring the daily case tally to 6.3% from 11.8%, but the government could not impose lockdown for a long time as it had a negative effect on the economy. A feasible alternative was to quarantine extremely sensitive areas so that only those infected by the virus remain in that zone to avoid further spread [45].
Studies show that there was a positive impact on the environment due to the implementation of lockdown which helps in reducing various greenhouse gases and helps in improving the water quality [46], [47] . It has been found that air pollution reduces to 50% in Barcelona during the lockdown phase [48]. During the lockdown, China's carbon emissions fell by 25% which is 1 million tons when compared to the last year data of the same period [49]. In the month of March, there was a decrease in PM2.5 in the United States, United Arab Emirates, Spain, and Italy which was due to complete shutdown [50]. In Delhi, compared to the pre-lockdown period, PM10 and PM2.5 concentrations decreased by half. Air quality has improved up to 60% in industrial and transportation areas whereas it was reported that on the second and fourth day of the lockdown, air quality improved by around 40–50% [51]. Similarly, Vembanad lake in India shows an improvement in water quality as particulate matter concentration declined by approximately 16% [52]. Water pollution in Venice, Italy [53], [54]was reduced as a result of the shutdown, and the city's water canals became more transparent than before [55].
Following the outbreak of COVID-19 pandemic, people have lived through different phases of lockdowns, and the majority of them started to work from home. Working from home has its own challenges such as working without proper workstations. In addition, long working hours associated with working from home may result in work-related health risks such as musculoskeletal disorders, and prolonged exposure to adverse indoor pollution. Lockdowns may also have significant impacts on various aspects of environmental quality. Existing literature documenting the impacts of COVID-19 and lockdowns is limited to environmental quality focusing mainly on one aspect such as water or air quality. Other studies investigated the impacts of COVID-19 and lockdowns on socio-economics.
To date, very limited comparative studies have investigated the impacts of COVID-19 lockdowns on socio-economics, ergonomics and environmental quality relative to pre- and post-lockdown periods. Moreover, integrative studies assessments the impacts of lockdowns on ergonomics, socioeconomic status and environmental quality in a single investigation are still lacking. Integrative studies encompassing socio-economics, ergonomics and various aspects of environmental quality provide a more comprehensive understanding of the impacts of lockdowns. Therefore, the objective of the present study is to investigate the impacts of COVID-19 lockdowns on the integrated aspects of socio-economic, ergonomic and environmental (water quality, air quality and noise) in Uttarakhand, India.
2. Methodology
2.1. Area of study
In the current article, socio-economic and ergonomic assessments of conditions of people working from home have been carried out for a group of 200 randomly selected people from various locations of Dehradun (Clement town, Prem Nagar, Raipur, Vasant Vihar, Patel Nagar) through a questionnaire. Assessment of water, ambient and indoor air quality has been carried out for Uttarakhand state of India before, during and after the lockdown phase of COVID-19. Uttarakhand state lies between 28°44’ & 31°28’ N Latitude and 77°35’ & 81°01’ E longitude, with a total geographical area of 53,483 km2. The state comprises of two region Garhwal and Kumaon. The state capital is Dehradun, situated at an altitude of 640 m above mean sea level [56] flowchart summarizing the research methodology is presented as Fig. 1.
Fig. 1.
A flowchart summarizing the research methodology.
2.2. Socio-economic and ergonomic assessments
The study relies upon the primary data collected randomly from 200 people from the Dehradun district in the state of Uttarakhand, India. Socio-economic assessment was carried out for these 200 respondents and information for general awareness regarding COVID-19 was collected from the same respondents. The ergonomic assessment was carried out for the respondents working from home during the ongoing pandemic, and to determine the ill health effects and comparison of major health issues for various age groups. All the data were collected through a well-structured questionnaire comprising 35 questions. Details of correspondents age, social status, marital status, education, nature of family, general awareness about Covid-19, their mode of work, number of working hours per day, and other questions related to the ill-health effects were included in the questionnaire in order to obtain the required details for carrying out the assessment. The questionnaire has been developed by considering Occupational Safety and Health Administration (USA) & National Occupational Safety and Health (OSH-India) guidelines.
2.3. Location and time periods
The impact of lockdown on water, air, noise, and indoor air quality for selected two regions of Uttarakhand (Garhwal and Kumaon) was done for four time periods: (i) January 2020 to March 2020 (Pre-lockdown), (ii) April 2020 to June 2020 (During Lockdown), (iii) July 2020 to September 2020 (Post-lockdown), and (iv) October 2020 to December 2020 (Post-lockdown).
2.4. Water quality assessment
The water quality was determined for total 8 water bodies which are river Ganga at HarkiPauri, Haridwar, Yamuna at Dakpathar, Dehradun, Mandakini at Rudraprayag, Alaknanda and Bhagirathi at Devprayag before their confluence in the Garhwal region and Naini lake, Bhimtal lake in Nainital of Kumaon region. For each water body, samples were taken at downstream end of the 3 selected locations. The instruments and methods used for sampling and assessment of water quality parameters are mentioned in Table 1.
Table 1.
Instruments/methods used for water quality assessment.
| Water quality Parameters assessed | Instruments/Method used | Indian standard Code |
|---|---|---|
|
Titrimetric analysis in Laboratory | IS 3025 (P-20) (1983) |
|
Titrimetric analysis in Laboratory | IS 3025(P-23) 1983 |
|
Gravimetric analysis | IS 3025(P-16) 1984 |
|
Colony Counter | IS:1622 1981 R-2003 |
|
BOD incubator (model no. SONAR 8450) | IS 3025 (P-21) |
|
COD digestion unit from Wealtech Corp. (model no. HB1) | IS 3025 (P-58) |
|
Winkler method (Titrimetric analysis) | IS 3025 (P-38) |
|
Digital pH meter (Thermo fisher star A11) | IS 3025 (P-11) 1983 |
2.5. Ambient air quality assessment
The ambient air quality assessment was determined at Garhwal and Kumaon region of Uttarakhand. At 6 different locations which are Dehradun, Rishikesh, Haridwar, Haldwani, Kashipur and Rudrapur. The sampling was done for a period of 24 h and at each location 3 samples were collected at breathing height (1.5–2.0 m). The instruments and methods used for sampling and assessment of ambient air quality parameters are mentioned in Table 2.
Table 2.
Instruments/methods used for Ambient air quality assessment.
| Ambient air quality Parameters assessed | Instruments/Method used | Indian standard Code |
|---|---|---|
|
PM2.5/ PM10 sampler (model Ecotech AAS 127) | IS 5182 (P-24): 2019 |
|
PM2.5/ PM10 sampler (model Ecotech AAS 127) | IS 5182 (P-23): 2004 |
|
Respirable Dust sampler + UV Spectroscopy (UV 1900i/Shimadzu) | IS 5182 (P-2): 2001 |
|
Respirable Dust sampler + UV Spectroscopy (UV 1900i/Shimadzu) | IS 5182 (P-6): 2006 |
2.6. Indoor air quality assessment
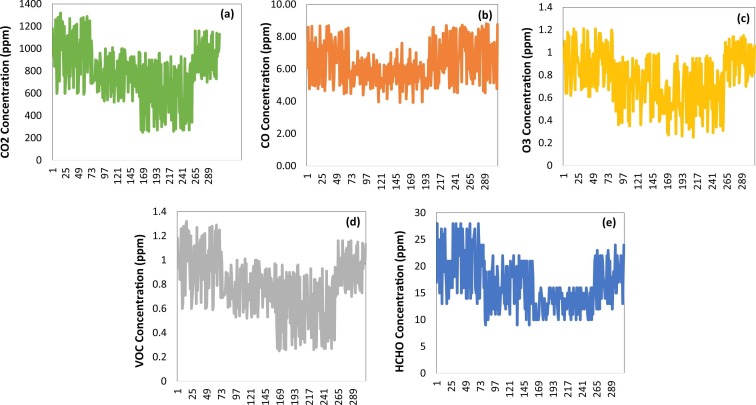
Sampling was done from a period of 21st February to 28th December (310 days,60 households were selected for indoor air monitoring and they were selected on the basis of ventilation area available within the house. CO2, CO, O3, VOC (Volatile Organic Compounds) and formaldehyde levels were measured for an indoor setting with 10–15% ventilation area (natural ventilation). Indoor air sampling was done for a period of 4-h (2 h in morning and 2 h in evening) throughout the sampling period. Residents were present during the measurement at the sampling location. The instruments and methods used for sampling and assessment of indoor air quality parameters are mentioned in Table 3.
Table 3.
Instruments/methods used for Ambient air quality assessment.
| Indoor air quality Parameters assessed | Instruments/Method used |
|---|---|
|
HSETIN HT-1000 |
|
Extech CO250 |
|
Trotec BQ16 |
|
OZ001 by Forensics |
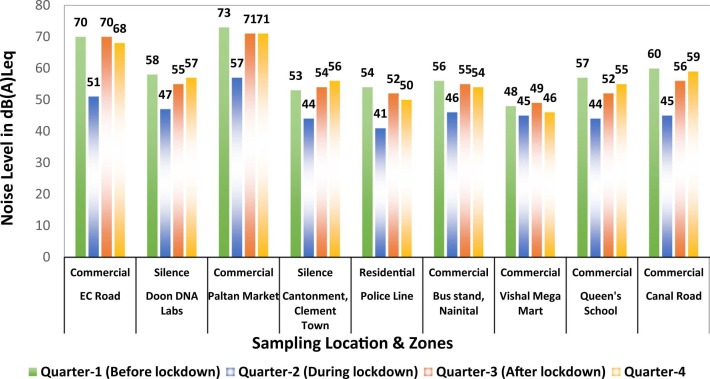
2.7. Ambient noise pollution assessment
The noise levels for various zones i.e., industrial, commercial, residential and silence were measured using a digital noise level meter from Instrumex with a measurement range of 30–130 dB. Eight hours’ time-weighted average sound level (TWA) was measured from 9:00 am to 5:00 pm at 9 locations across the state.
3. Results and discussion
3.1. Socio-economic assessment
The assessment gives clear data regarding the age group in which 78 respondents were in majority (age group in between 26 and 35) whereas much of the respondents also belongs to other younger community ( Fig. 2: a and b). Individuals from nuclear families were 108 and the one from joint family were 31 (Fig. 2: c). Marital and educational status gives a picture that the majority of people were married and having senior secondary education (Fig. 2: d and e). The assessment of 200 respondents provides with the data that 133 knows about health hazard due to COVID-19, 104 people focus on precautionary measures, 141 people do not have the proper knowledge to use the protective equipment and 156 people were not using Aarogya Setu application this application is to spread awareness of COVID–19 and to connect essential COVID–19-related health services to the people of India, results are shown in Fig. 3.
Fig. 2.
Socio-Economic Assessment: (a) age group; (b) social status; (c) marital status; (d) education; and (e) nature of family.
Fig. 3.
Awareness about Covid-19.
After estimating and evaluating socioeconomic status it is clear that the impact of the pandemic on individual life is different [57] . The various parameter such as age group, education, nature of family, population density plays a significant role while doing a socioeconomic assessment. Moreover, it has a disastrous impact on the lower-income group of society, social distancing is a worldwide strategy adopted that has ensured that it is possible to contain COVID-19 [58], [59]. A highly populated area ensures that social distancing in the urban sector is quite difficult.
3.2. Hazards and effects of improper ergonomic conditions
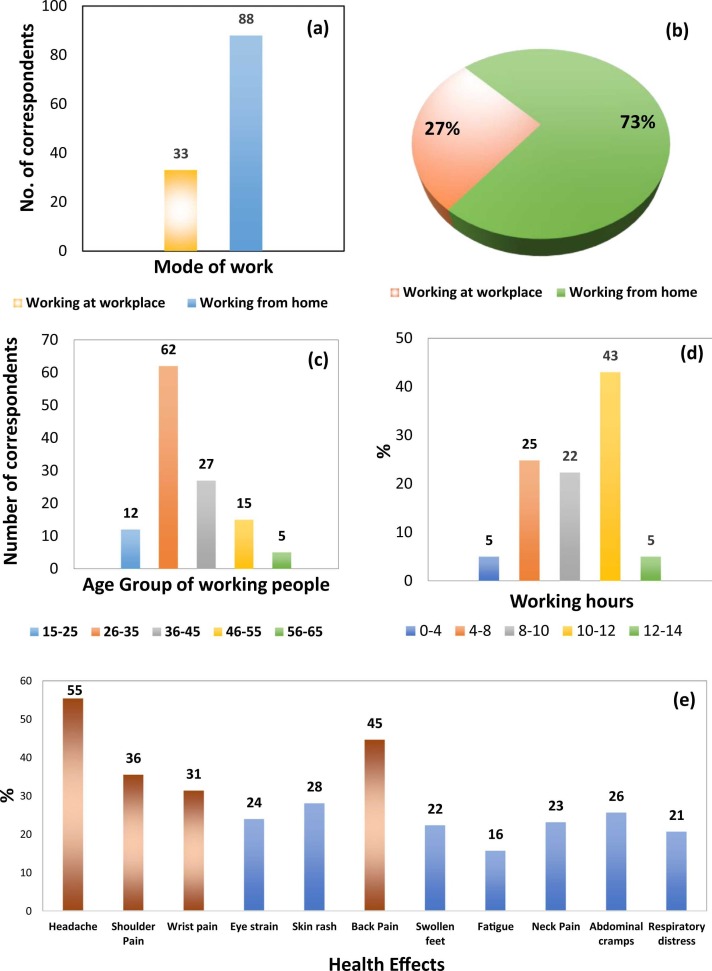
51% of people were from the age group of 26–35 ( Fig. 4: c). About 73% of the people were working from home and 50% of the individuals were working for over 10 h instead of the normal 8 h (Fig. 4: b and d). As a result, most of them were having ill-health and headache, back pain and shoulder pain was found to be common in all age groups (Fig. 4: e). People over the age of 35 were having multiple ill health effects where headache and back pain were more prominent ( Fig. 5).
Fig. 4.
Assessment of Ergonomic conditions and ill-health effects: (a) mode of work; (b) percentage of model of work; (c) age; (d) working hours; and (e) ill health effects.
Fig. 5.
Comparison of major health issues for different age groups.
Ergonomics is the improvement of interaction between worker and the machine, making the interaction more suitable for the human body. The interface should be designed in a way that does not cause any strain on muscles or any joint [60]. Amidst this pandemic, there has been a shift in large numbers of working personnel to work in a home arrangement setting [61], [62]. Along with this shift of workforce working from homes various musculoskeletal disorders like shoulder pain, neck pain, wrist pain, eye strain, swollen feel and headache are associated with people working continuously on computers [63], [64]. Most modern work organization are equipped with workstations designed by considering ergonomic factors [65], [66].
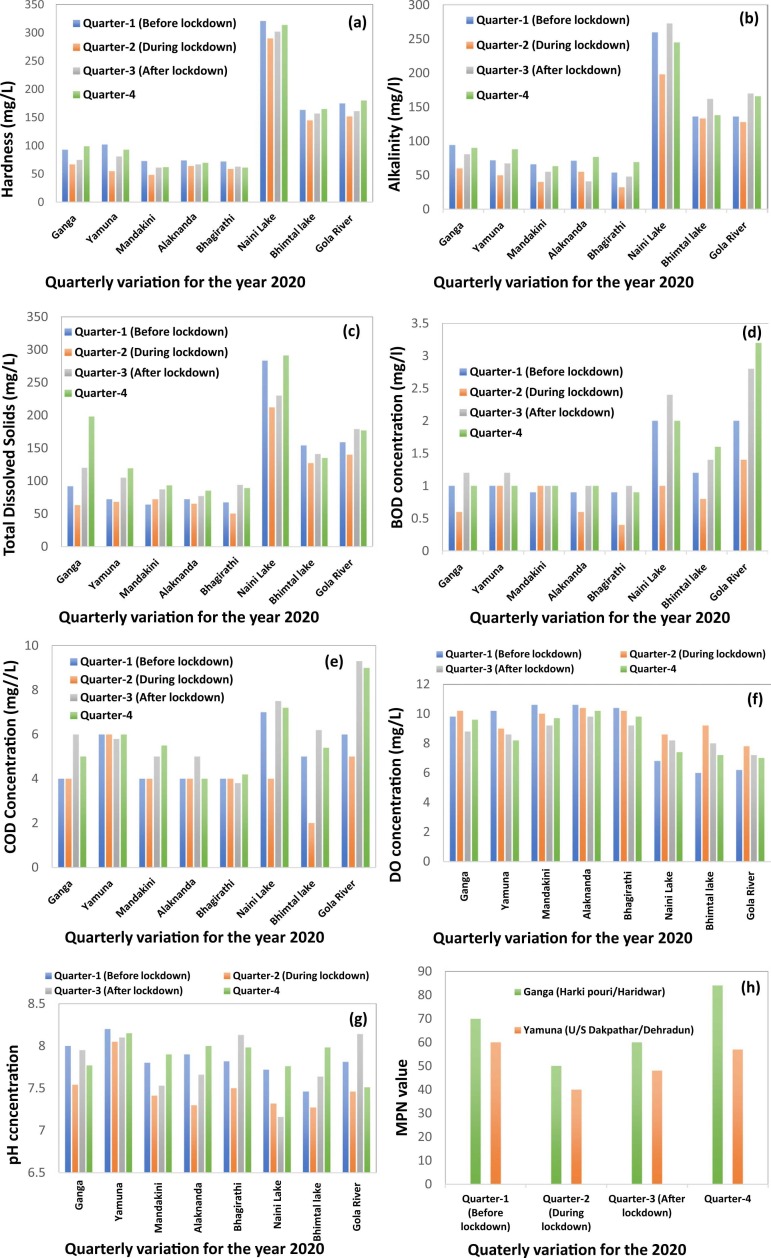
3.3. Water quality of major water bodies of Uttarakhand
The results of water quality assessment for the rivers Ganga at HarkiPauri, Haridwar, Yamuna at Dakpathar, Dehradun, Mandakini at Rudraprayag, Alaknanda and Bhagirathi at Devprayag before their confluence of Garhwal region and Naini lake, Bhimtal lake in Nainital of Kumaon region are depicted in Fig. 4. During the lockdown, the hardness levels for all the water bodies were reduced, the mean and SD for Ganga and Yamuna during lockdown i.e., quarter-2 was observed to be 67 ± 8.88 mg/L and 55 ± 6.05 mg/L, respectively but these levels started to increase once again after the lockdown was lifted in the quarter-3 ( Fig. 6: a). The results for alkalinity are depicted in Fig. 6: b. The variation in the levels of alkalinity reveals that the levels declined during the lockdown, the mean and SD for Ganga and Yamuna during the lockdown was observed to be 60 ± 7.59 mg/L and 50 ± 6.89 mg/L, respectively. However, the levels began to rise in the third and fourth quarters. Total Dissolved Solids (TDS) levels are shown in Fig. 6: c. A decline in TDS concentrations can be observed for the lockdown period. After the monsoon period i.e., quarter-3 there was a significant increase in the TDS concentrations. The total coliform index of Ganga and Yamuna was reduced to 50 MPN/100 ml, 40 MPN/100 ml respectively during the lockdown period (Fig. 6: d). The results for BOD, COD and Dissolved Oxygen (DO) are depicted in the Fig. 6: d–f, respectively. pH of Ganga, Yamuna, Mandakni, Alaknanda before the lockdown was 8, 8.2, 7.8, 7.9 respectively before lockdown which reduced to 7.54, 8.05, 7.41, 7.3 respectively during lockdown (Fig. 6: g). Hardness, alkalinity, TDS, total coliform MPN and pH have improved for all these water bodies across the state during the lockdown imposed due to COVID-19. The reason for improved water quality is reduced human activities and lesser discharge of industrial effluents into these water bodies.
Fig. 6.
Assessment of Water Quality parameters: (a) Hardness (mg/L); (b) Alkalinity (mg/L); (c) Total Dissolved Solids (mg/L); (d) BOD (mg/l); (e) COD (mg//L); (f) Dissolved Oxygen (mg/L); (g) pH of major streams of Uttarakhand; and (h) MPN for Ganga & Yamuna.
It is necessary and crucial to test the water before it is used for drinking, domestic purposes, or industrial and agricultural use. The choice of monitoring parameters depends on the purpose of use and what quality of water is needed. For testing the physical properties like temperature, pH, color, TDS, odor etc., physical tests must be performed [67], [68]. On the other hand, chemical testing is done to measure properties like hardness, alkalinity, BOD, COD and DO etc. Hasadsri and Maleewong [69]. For assessment of water quality, these parameters should be measured and monitored regularly [70]. pH determines water’s corrosive behavior, and water is more corrosive when the pH is on the lower scale, alkalinity and conductivity of water depend upon its pH [71], [72]. The toxicity of various substances in water is affected by pH, hardness, and alkalinity. Water with high alkalinity is not fit for industrial use as it causes operating problems in boilers [73]. DO is one of the most critical parameters. Its relationship with the water body provides details like bacterial activity, availability of nutrients, in the water body, stratification. During summers, the DO increases because of increased temperature and bright sunlight [74]. BOD is a measure of contamination of organic matter in water and is the quantity of dissolved oxygen needed for the biochemical decomposition of organic compounds and the oxidation of certain inorganic materials. (e.g., iron, sulfites) [75]. COD is measured to know the dissolved oxygen which is needed for the chemical oxidation of organic matter. COD and BOD are prime indicators of the environmental health of a water body [76]. The hardness of rivers varies from one season to another, it is higher in the rainy season and lower during winters. For Himalayan River calcium ions are the major contributor to total hardness [77], [78].
The water quality of rivers degrades because of anthropogenic activities such as industrial effluents, sewage discharge and surface runoff [79], [80]. Less human and industrial activity during the lockdown phase has shown improvement in the water quality of major rivers in Uttarakhand. Many of these rivers like Ganga and Yamuna are associated with religious activities [81]. Every year, millions of people from all over the country visit them for performing religious activities. Ganga river at Rishikesh is also famous for river rafting and other water sports [82], [83]. The major contamination points for river Ganga are located along the downstream of Haridwar [84].
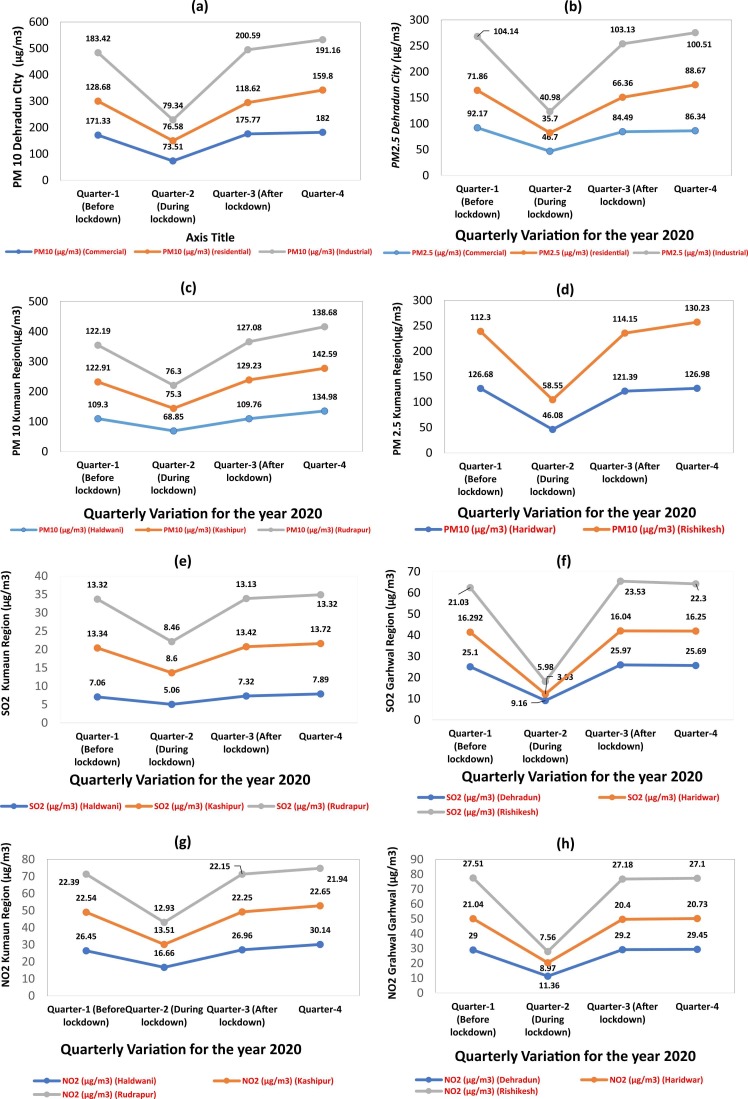
3.4. Ambient air quality of Uttarakhand
The results for ambient air quality assessment of Garhwal and Kumaon region of Uttarakhand are shown in Fig. 7. During the 2nd quarter i.e., lockdown phase, a significant reduction in the concentration levels of pollutants like PM10, PM2.5, SO2, NO2 was observed which began to rise again in third and fourth quarter. The concentration of these pollutants was under the prescribed limits as suggested by National Ambient Air Quality Standards (NAAQS for PM2.5 = 60 μg m−3, PM10 = 100 μg m−3, SO2 = 80 μg m−3, NO2 = 80 μg m−3 based on 24-h average).
Fig. 7.
Assessment of Ambient air quality: (a) PM10 Dehradun City; (b) PM2.5 Dehradun City; (c) PM10 Kumaon Region; (d) PM10 Rishikesh & Haridwar; (e) SO2 Kumaon Region; (f) SO2 Garhwal Region; (g) NO2 Kumaon Region; (h) NO2 Garhwal Region.
Air pollution is one of the serious issues which the entire world is facing especially for the countries who are in their developing phase. After liberalization in 1990, India has seen economic growth, rapid urbanization, industrialization, and huge infrastructure development [85]. At the same time, India's level of air pollution has risen to significant health risk and source of substantial premature mortality. According to a survey in India, around 1 million people lost their lives in the year 2015 due to poor air quality with the particulate matter as a major source. In recent years, cities of India are among the top twenty most contaminated cities in the world and did not meet the environmental air quality criteria given by Central Pollution Control Board-India (CPCB) and WHO [86], [87]. Emission from vehicle and industries are the major source for contributing the particulate matter [88], [89] . A study was conducted to analyze the ambient air quality for Mumbai and Delhi and it was found that there was a substantial decrease in the emission of NO2, PM10 and NO2 was recorded during the lockdown time [90]. As the lockdown was implemented most of the activities and vehicular movement was restricted to a considerable extent helping the air quality to improve [91], [92]. However, through various measures, if the air quality could be improved it would help in decreasing the number of cases of asthma, heart problems, respiratory disorder etc. Samet et al. [93].
3.5. Indoor air quality during COVID-19 lockdown phase
The results for indoor air quality assessment are depicted in Fig. 8. During the lockdown phase increase in concentration levels of these pollutants was observed, also seasonal variation can be observed for volatile organic compounds (VOCs) and HCHO (Fig. 8: d and e). Results were similar to a study performed by A. Kumar in 2014, the VOC levels in the winter season were higher than summer season [94].
Fig. 8.
Assessment of Indoor air quality: (a) CO2 (10–15% ventilation); (b) CO (10–15% ventilation); (c) Ozone (10–15% ventilation); (d) VOC (10–15% ventilation); and (e) HCHO (10–15% ventilation).
An average human being spends most of the time indoors (ranging from 85% to 90%), the understanding ambient environment is important, the indoor environment is majorly polluted from indoor pollutants like humans and combustion processes in the kitchen or living room. Cattaneo et al. [95]. There has been growing awareness about the adverse health effects of poor Indoor air quality (IAQ) in the last two decades, researchers across the globe are performing numerous studies to assess the IAQ. During the distinct phases of lockdown due to the pandemic, people spent all their time indoors, which might have a possibility to increase indoor air pollution having an adverse impact on human health [96]. Indoor air contaminant originates from a wide variety of sources. They are generated during various human activities and infiltration from outside increases the level of pollutant concentration [97]. The concentration of pollutants depends on the air confined in an indoor environment, the rate of release or removal of pollutants and the rate at which it is removed, the air exchange rate with outside air [98]. VOCs such as benzene, toluene, xylenes, and formaldehyde are commonly released indoor air pollutant. Several indoor air contaminants are human carcinogen and have various other adverse effects on human health such as eyes, skin irritation and a wide variety of respiratory diseases can be associated with these indoor contaminants. Bravi et al. [99] . Households with biomass fuel burning and charcoal burning have elevated levels of PM10 and carbon monoxide than those where clean fuels are used [100]. Various respiratory disorders such as asthma, chronic obstructive pulmonary disease etc. are caused by the smoke of biomass fuel [101], [102] .
3.6. Ambient noise pollution assessment
The results for ambient noise before the lockdown period ranges from 46 to 73 dB(A) and during the lockdown phase, it was reduced to 41–57 dB(A), shown in Fig. 8. The standard value of different zones is given by CPCB in Table 4 The noise level observed from Dehradun region i.e., from EC road, Doon DNA labs, Paltan market, Clement town, Police line were 51 dB, 47 dB, 57 dB, 44 dB, 41 dB respectively during lockdown phase, whereas data observed from Kumaon region i.e., Bus stand (Nainital), Vishal mega mart (Haldwani), Queens School Haldwani, Canal Road (Haldwani) were 46 dB, 45 dB, 44 dB and 45 dB respectively during lockdown phase. The study clearly illustrates that noise level was reduced during lockdown when compared with pre lockdown data ( Fig. 9) As per WHO noise pollution is ranked among the top three hazardous pollutions. There are many adverse effects when a person is exposed to either short term or long-term range resulting in high blood pressure, depression, hormonal disturbance, anxiety etc. Lai and Huang [103]. Through the study, it is clear that a 5 dB rise in roadside noise will increase the risk of hypertension by 3.4% [104]. Road traffic is one of the key sources of noise emission and the WHO estimates that around 40% of the population of Europe is subjected to a noisy environment [105], [106]. Globally it was estimated that there was a reduction in the level of noise up to 35–68% during the lockdown period [107]. Noise pollution also affects marine life as various human activities such as the use of radar, boats etc. creates a lot of disturbance in the aquatic ecosystem (coral reefs) [108]. Most of the underwater noise resulting from human activity is estimated to be of lower Hertz [109]. The lockdown also impacted the aquatic environment because of COVID-19, all water transport movement was stopped which significantly helps to decrease the number of emissions generated by human activities.
Table 4.
Ambient noise standard values according to CPCB, India.
| Zone category | Limit in dB (A) Leq |
|
|---|---|---|
| Day time | Night time | |
| Industrial | 75 | 65 |
| Commercial | 65 | 55 |
| Residential | 55 | 45 |
| Silence | 50 | 40 |
Fig. 9.
Assessment of noise pollution.
4. Conclusions
The present paper investigated the impacts of the COVID-19 lockdowns on socioeconomics, ergonomics, and environment (water quality, air quality and noise) in Uttarakhand, India. The key findings and conclusion were as follows:
-
•
The results showed that 33% of respondents were unaware of the health hazards of COVID-19, despite various information provided by the government. Approximately 47% of individuals were not taking the right precautionary measures such as using masks, and face shields properly.
-
•
With the shift of workforce working from homes due to the pandemic, people were working for long hours without any adequate workstations which lead to various musculoskeletal disorders in individuals of all age groups. Approximately 55% of the respondents experienced work-related health effects such as headache while 45% of respondents were having back pain. Therefore, to reduce the increasing cases of musculoskeletal disorders, there is need for raise awareness on the human health risks, improve occupation health procedures and policies, and provide appropriate work stations.
-
•
The lockdown had a positive impact on water and air quality due to reduced tourist activities in Uttarakhand, but the effects were temporary.
-
•
The concentrations of indoor air pollutants were higher during the lockdown phase due to increased indoor activities, but declined in the post-lockdown period.
-
•
Lockdowns significantly reduced the ambient noise levels relative to the pre-pandemic period.
Overall, the present study provides a comprehensive and integrative understanding of the impacts of lockdowns on socio-economics, ergonomics, and environmental quality. This information can be used to developed strategies and policies to safeguard the environment and human health. Therefore, during lockdowns there is a need to minimize the adverse environmental and ergonomic impacts of lockdowns while simultaneously enhancing the beneficial impacts. Further research should focus on developing and pilot testing various control methods for the mitigation of the negative impacts of COVID-19 lockdowns.
CRediT authorship contribution statement
Abhishek Nandan: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Visualization, Validation, Project administration. N.A. Siddiqui: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Visualization, Validation, Project administration. Chandrakant Singh: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Visualization, Validation, Project administration. Ashish Aeri: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Visualization, Validation, Project administration. Willis Gwenzi: Writing – original draft, Writing – review & editing, Visualization, Validation. Joshua O. Ighalo: Writing – original draft, Writing – review & editing, Visualization, Validation. Patrícia de Carvalho Nagliate: Writing – original draft, Writing – review & editing, Visualization, Validation. Lucas Meili: Writing – original draft, Writing – review & editing, Visualization, Validation. Pardeep Singh: Writing – original draft, Writing – review & editing, Visualization, Validation. Nhamo Chaukura: Writing – original draft, Writing – review & editing, Visualization, Validation. Selvasembian Rangabhashiyam: Conceptualization, Methodology, Investigation, Writing – original draft, Writing – review & editing, Supervision, Validation, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Teik Thye Lim
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.jece.2021.106595.
Appendix A. Supplementary material
Supplementary material
.
References
- 1.Hui D.S., I Azhar E., Madani T.A., Ntoumi F., Kock R., Dar O., Ippolito G., Mchugh T.D., Memish Z.A., Drosten C., Zumla A., Petersen E. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan, China. Int. J. Infect. Dis. 2020;vol. 91:264–266. doi: 10.1016/j.ijid.2020.01.009. 2020/02/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hasnain M., Pasha M.F., Ghani I. Combined measures to control the COVID-19 pandemic in Wuhan, Hubei, China: a narrative review. J. Biosaf. Biosecur. 2020;vol. 2(2):51–57. doi: 10.1016/j.jobb.2020.10.001. 2020/12/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu H., Stratton C.W., Tang Y.W. Vol. 92. 2020. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle; p. 401. (J. Med. Virol.). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mizumoto K., Kagaya K., Chowell G. Effect of a wet market on coronavirus disease (COVID-19) transmission dynamics in China, 2019–2020. Int. J. Infect. Dis. 2020;vol. 97:96–101. doi: 10.1016/j.ijid.2020.05.091. 2020/08/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cucinotta D., Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Med.: Atenei Parm. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fu H., Wang H., Xi X., Boonyasiri A., Wang Y., Hinsley W., Fraser K.J., McCabe R., Olivera Mesa D., Skarp J., Ledda A., Dewé T., Dighe A., Winskill P., van Elsland S.L., Ainslie K., Baguelin M., Bhatt S., Boyd O., Brazeau N.F., Cattarino L., Charles G., Coupland H., Cucunuba Z.M., Cuomo-Dannenburg G., Donnelly C.A., Dorigatti I., Eales O.D., FitzJohn R.G., Flaxman S., Gaythorpe K., Ghani A.C., Green W.D., Hamlet A., Hauck K., Haw D.J., Jeffrey B., Laydon D.J., Lees J.A., Mellan T., Mishra S., Nedjati-Gilani G., Nouvellet P., Okell L., Parag K.V., Ragonnet-Cronin M., Riley S., Schmit N., Thompson H.A., Unwin H.T., Verity R., Vollmer M., Volz E., Walker P., Walters C.E., Watson O.J., Whittaker C., Whittles L.K., Imai N., Bhatia S., Ferguson N.M. Database of epidemic trends and control measures during the first wave of COVID-19 in mainland China. Int. J. Infect. Dis. 2021;vol. 102:463–471. doi: 10.1016/j.ijid.2020.10.075. 2021/01/01/ 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Banerjee A., Kulcsar K., Misra V., Frieman M., Mossman K.J.V. Bats and coronaviruses. Viruses. 2019;vol. 11(1):41. doi: 10.3390/v11010041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paraskevis D., Kostaki E.G., Magiorkinis G., Panayiotakopoulos G., Sourvinos G., Tsiodras S. Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event. Infect., Genet. Evol. 2020;vol. 79 doi: 10.1016/j.meegid.2020.104212. 2020/04/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zumla A., Chan J.F., Azhar E.I., Hui D.S., Yuen K.Y. Coronaviruses—drug discovery and therapeutic options. Nat. Rev. Drug Discov. 2016;15(5):327–347. doi: 10.1038/nrd.2015.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Englisch C.N., Tschernig T., Flockerzi F., Meier C., Bohle R.M. Lesions in the lungs of fatal corona virus disease Covid-19. Ann. Anat. – Anat. Anz. 2021;vol. 234 doi: 10.1016/j.aanat.2020.151657. 2021/03/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hushmandi K., et al. A review of medications used to control and improve the signs and symptoms of COVID-19 patients. Eur. J. Pharmacol. 2020;vol. 887 doi: 10.1016/j.ejphar.2020.173568. 2020/11/15/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohammadi A., Esmaeilzadeh E., Li Y., Bosch R.J., Li J.Z. SARS-CoV-2 detection in different respiratory sites: a systematic review and meta-analysis. EBioMedicine. 2020;vol. 59 doi: 10.1016/j.ebiom.2020.102903. 2020/09/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carfì A., Bernabei R., Landi F. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603–605. doi: 10.1001/jama.2020.12603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Larsen J.R., Martin M.R., Martin J.D., Kuhn P., Hicks J.B. Modeling the onset of symptoms of COVID-19. Front. Public Health. 2020;8:473. doi: 10.3389/fpubh.2020.00473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li N., Zhu L., Sun L., Shao G. The effects of novel coronavirus (SARS-CoV-2) infection on cardiovascular diseases and cardiopulmonary injuries. Stem Cell Res. 2021;vol. 51 doi: 10.1016/j.scr.2021.102168. 2021/03/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Visca D., Ong C., Tiberi S., Centis R., D’Ambrosio L., Chen B., Mueller J., Mueller P., Duarte R., Dalcolmo M., Sotgiu G., Migliori G.B., Goletti D. Tuberculosis and COVID-19 interaction: a review of biological, clinical and public health effects. Pulmonology. 2021;27:151–165. doi: 10.1016/j.pulmoe.2020.12.012. 2021/01/22/2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Assaad S., Avrillon V., Fournier M.L., Mastroianni B., Russias B., Swalduz A., Cassier P., Eberst L., Steineur M.P., Kazes M., Perol M., Michallet A.S., Rey P., Erena-Penet A.S., Morel A., Brahmi M., Dufresne A., Tredan O., Chvetzoff G., Fayette J., de la Fouchardiere C., Ray-Coquard I., Bachelot T., Saintigny P., Tabutin M., Dupré A., Nicolas-Virelizier E., Belhabri A., Roux P.E., Fuhrmann C., Pilleul F., Basle A., Bouhamama A., Galvez C., Herr A.L., Gautier J., Chabaud S., Zrounba P., Perol D., Blay J.Y. High mortality rate in cancer patients with symptoms of COVID-19 with or without detectable SARS-COV-2 on RT-PCR. Eur. J. Cancer. 2020;vol. 135:251–259. doi: 10.1016/j.ejca.2020.05.028. 2020/08/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Livingston G., Rostamipour H., Gallagher P., Kalafatis C., Shastri A., Huzzey L., Liu K., Sommerlad A., Marston L. Prevalence, management, and outcomes of SARS-CoV-2 infections in older people and those with dementia in mental health wards in London, UK: a retrospective observational study. Lancet Psychiatry. 2020;vol. 7(12):1054–1063. doi: 10.1016/S2215-0366(20)30434-X. 2020/12/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chakraborty S., Mallajosyula V., Tato C.M., Tan G.S., Wang T.T. SARS-CoV-2 vaccines in advanced clinical trials: where do we stand? Adv. Drug Deliv. Rev. 2021 doi: 10.1016/j.addr.2021.01.014. 2021/01/20/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Noorimotlagh Z., Jaafarzadeh N., Martínez S.S., Mirzaee S.A. A systematic review of possible airborne transmission of the COVID-19 virus (SARS-CoV-2) in the indoor air environment. Environ. Res. 2021;vol. 193 doi: 10.1016/j.envres.2020.110612. 2021/02/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lima A.A., Nunes I.C.M., da Silva Duarte J.L., Meili L., de Carvalho Nagliate P., dos Santos Almeida A.G.C. Characteristics of SARS-CoV-2 aerosol dispersion in indoor air: scoping review. Res., Soc. Dev. 2021;10(4) [Google Scholar]
- 22.Bloise I., Gómez-Arroyo B., García-Rodríguez J. Detection of SARS-CoV-2 on high-touch surfaces in a clinical microbiology laboratory. J. Hosp. Infect. 2020;vol. 105(4):784–786. doi: 10.1016/j.jhin.2020.05.017. 2020/08/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization, Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations: scientific brief, 27 March 2020, World Health Organization, 2020.
- 24.Wiwanitkit V. Atypical modes of COVID-19 transmission: how likely are they? Epidemiol. Health. 2020;42:42. doi: 10.4178/epih.e2020059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Han Y., Yang H. The transmission and diagnosis of 2019 novel coronavirus infection disease (COVID-19): a Chinese perspective. J. Med. Virol. 2020;92(6):639–644. doi: 10.1002/jmv.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsu C.-Y., Lai C.-C., Yeh Y.-P., Chang-Chuan C., Chen H.-H. Progression from pneumonia to ARDS as a predictor for fatal COVID-19. J. Infect. Public Health. 2021 doi: 10.1016/j.jiph.2020.12.026. 2020/12/30/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McCullough P.A., Kelly R.J., Ruocco G., Lerma E., Tumlin J., Wheelan K.R., Katz N., Lepor N.E., Vijay K., Carter H., Singh B., McCullough S.P., Bhambi B.K., Palazzuoli A., De Ferrari G.M., Milligan G.P., Safder T., Tecson K.M., Wang D.D., McKinnon J.E., O’Neill W.W., Zervos M., Risch H.A. Pathophysiological basis and rationale for early outpatient treatment of SARS-CoV-2 (COVID-19) infection. Am. J. Med. 2021;vol. 134(1):16–22. doi: 10.1016/j.amjmed.2020.07.003. 2021/01/01/ 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garcia M., Lipskiy N., Tyson J., Watkins R., Esser E.S., Kinley T. Centers for Disease Control and Prevention 2019 novel coronavirus disease (COVID-19) information management: addressing national health-care and public health needs for standardized data definitions and codified vocabulary for data exchange. J. Am. Med. Inform. Assoc. 2020;27(9):1476–1487. doi: 10.1093/jamia/ocaa141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bilal M., Munir H., Nazir M.S., Iqbal H.M.N. Persistence, transmission, and infectivity of SARS-CoV-2 in inanimate environments. Case Stud. Chem. Environ. Eng. 2020;vol. 2 doi: 10.1016/j.cscee.2020.100047. 2020/09/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C., Zimmer T., Thiel V., Janke C., Guggemos W., Seilmaier M. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu Z., Chu R., Gong L., Su B., Wu J. The assessment of transmission efficiency and latent infection period in asymptomatic carriers of SARS-CoV-2 infection. Int. J. Infect. Dis. 2020;vol. 99:325–327. doi: 10.1016/j.ijid.2020.06.036. 2020/10/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sohrabi C., Alsafi Z., O’neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tang S., et al. Aerosol transmission of SARS-CoV-2? Evidence, prevention and control. Environ. Int. 2020;vol. 144 doi: 10.1016/j.envint.2020.106039. 2020/11/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gray D.J., Kurscheid J., Mationg M.L., Williams G.M., Gordon C., Kelly M., Wangdi K., McManus D.P. Health-education to prevent COVID-19 in schoolchildren: a call to action. Infect. Dis. Poverty. 2020;9(1):1–3. doi: 10.1186/s40249-020-00695-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee E., Chen Y.Y., McDonald M., O’Neill E. Dynamic response systems of healthcare mask production to COVID-19: a case study of Korea. Systems. 2020;8(2):18. [Google Scholar]
- 36.Thomson E., Bullied A. Production of ethanol-based hand sanitizer in breweries during the COVID-19 crisis. MBAA TQ. 2020;57(1):47–52. [Google Scholar]
- 37.Varsavsky T., Graham M.S., Canas L.S., Ganesh S., Capdevila Pujol J., Sudre C.H., Murray B., Modat M., Jorge Cardoso M., Astley C.M., Drew D.A., Nguyen L.H., Fall T., Gomez M.F., Franks P.W., Chan A.T., Davies R., Wolf J., Steves C.J., Spector T.D., Ourselin S. Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study. Lancet Public Health. 2021;vol. 6(1):e21–e29. doi: 10.1016/S2468-2667(20)30269-3. 2021/01/01/ 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.K. Baskaran, P. Baskaran, V. Rajaram, N. Kumaratharan, IoT Based COVID Preventive System for Work Environment, in: 2020 Fourth International Conference on I-SMAC (IoT in Social, Mobile, Analytics and Cloud)(I-SMAC), IEEE, 2020, pp. 65–71.
- 39.Singh R., Kaushik S., Badal R., Sahoo S.J.J. o A., Medicine H. Ayurveda and its medicinal plants: halting the surge of Covid-19. 2020;vol. 6(2):90–99. [Google Scholar]
- 40.Sarkar K., Khajanchi S., Nieto J.J. Modeling and forecasting the COVID-19 pandemic in India. Chaos, Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sun X., Wandelt S., Zhang A. How did COVID-19 impact air transportation? A first peek through the lens of complex networks. J. Air Transp. Manag. 2020;vol. 89 doi: 10.1016/j.jairtraman.2020.101928. 2020/10/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tiwari A. Modelling and analysis of COVID-19 epidemic in India. J. Saf. Sci. Resil. 2020;vol. 1(2):135–140. 2020/12/01/ 2020. [Google Scholar]
- 43.Andrews M.A., Areekal B., Rajesh K.R., Krishnan J., Suryakala R., Krishnan B., Muraly C.P., Santhosh P.V. First confirmed case of COVID-19 infection in India: a case report. Indian J. Med. Res. 2020;151(5):490–492. doi: 10.4103/ijmr.IJMR_2131_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta M., Mohanta S.S., Rao A., Parameswaran G.G., Agarwal M., Arora M., Mazumder A., Lohiya A., Behera P., Bansal A., Kumar R., Meena V.P., Tiwari P., Mohan A., Bhatnagar S. Transmission dynamics of the COVID-19 epidemic in India and modeling optimal lockdown exit strategies. Int. J. Infect. Dis. 2021;vol. 103:579–589. doi: 10.1016/j.ijid.2020.11.206. 2021/02/01/ 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumar S. Effect of meteorological parameters on spread of COVID-19 in India and air quality during lockdown. Sci. Total Environ. 2020;745 doi: 10.1016/j.scitotenv.2020.141021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Singh J., Tyagi B. Transformation of air quality over a coastal tropical station Chennai during COVID-19 lockdown in India. Aerosol Air Qual. Res. 2021;21 [Google Scholar]
- 47.Arora P., Kumar H., Panigrahi B.K. Prediction and analysis of COVID-19 positive cases using deep learning models: a descriptive case study of India. Chaos, Solitons Fractals. 2020;139 doi: 10.1016/j.chaos.2020.110017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Camargo-Caicedo Y., Mantilla-Romo L.C., Bolaño-Ortiz T.R.J.A.S. Emissions reduction of greenhouse gases, ozone precursors, aerosols and acidifying gases from road transportation during the COVID-19 lockdown in Colombia. 2021;vol. 11(4):1458. [Google Scholar]
- 49.Shakil M.H., Munim Z.H., Tasnia M., Sarowar S. COVID-19 and the environment: a critical review and research agenda. Sci. Total Environ. 2020 doi: 10.1016/j.scitotenv.2020.141022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tobías A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci. Total Environ. 2020;vol. 725 doi: 10.1016/j.scitotenv.2020.138539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang Q., Su M. A preliminary assessment of the impact of COVID-19 on environment–A case study of China. Sci. Total Environ. 2020;vol. 728 doi: 10.1016/j.scitotenv.2020.138915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chauhan A., Singh R.P. Decline in PM2. 5 concentrations over major cities around the world associated with COVID-19. Environ. Res. 2020;vol. 187 doi: 10.1016/j.envres.2020.109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mahato S., Pal S., Ghosh K.G. Effect of lockdown amid COVID-19 pandemic on air quality of the megacity Delhi, India. Sci. Total Environ. 2020;vol. 730 doi: 10.1016/j.scitotenv.2020.139086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yunus A.P., Masago Y., Hijioka Y. COVID-19 and surface water quality: improved lake water quality during the lockdown. Sci. Total Environ. 2020;vol. 731 doi: 10.1016/j.scitotenv.2020.139012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Braga F., Scarpa G.M., Brando V.E., Manfè G., Zaggia L. COVID-19 lockdown measures reveal human impact on water transparency in the Venice Lagoon. Sci. Total Environ. 2020;vol. 736 doi: 10.1016/j.scitotenv.2020.139612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kelkar U., Narula K.K., Sharma V.P., Chandna U.J.G.E.C. Vulnerability and adaptation to climate variability and water stress in Uttarakhand State, India. Glob. Environ.Change. 2008;vol. 18(4):564–574. [Google Scholar]
- 57.Uddin S., Imam T., Khushi M., Khan A., Ali M. How did socio-demographic status and personal attributes influence compliance to COVID-19 preventive behaviours during the early outbreak in Japan? Lessons for pandemic management. Personal. Individ. Differ. 2021;175 doi: 10.1016/j.paid.2021.110692. 2021/01/27/ 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kaspar K. Motivations for social distancing and app use as complementary measures to combat the COVID-19 pandemic: quantitative survey study. J. Med. Internet Res. 2020;vol. 22(8) doi: 10.2196/21613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eze P.U., Ezenkwu C.P., Etteh C.C. Community informatics for sustainable management of pandemics in developing countries: a case study of COVID-19 in Nigeria. Ethics, Med. Public Health. 2021 doi: 10.1016/j.jemep.2021.100632. 2021/01/28/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bridger R. CRC Press; 2008. Introduction to Ergonomics. [Google Scholar]
- 61.Kramer A., Kramer K.Z. Elsevier; 2020. The Potential Impact of the Covid-19 Pandemic on Occupational Status, Work from Home, and Occupational Mobility. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chang Y.-J., Nguyen T.D., Finkbeiner M., Krüger J. Adapting ergonomic assessments to social life cycle assessment. Procedia CIRP. 2016;vol. 40:91–96. 2016/01/01/ 2016. [Google Scholar]
- 63.Ren L., Qian Z., Ren L. Biomechanics of musculoskeletal system and its biomimetic implications: a review. J. Bionic Eng. 2014;vol. 11(2):159–175. 2014/04/01/ 2014. [Google Scholar]
- 64.Workineh S.A., Yamaura H. Effects of multiple working positions on user comfort: a study on multi-position ergonomic computer workstation. Procedia Manuf. 2015;vol. 3:4792–4799. 2015/01/01/ 2015. [Google Scholar]
- 65.Wahlström J.J.O.M. Ergonomics, musculoskeletal disorders and computer work. Occup. Med. 2005;vol. 55(3):168–176. doi: 10.1093/occmed/kqi083. [DOI] [PubMed] [Google Scholar]
- 66.Poochada W., Chaiklieng S. Ergonomic risk assessment among call center workers. Procedia Manuf. 2015;vol. 3:4613–4620. 2015/01/01/ 2015. [Google Scholar]
- 67.Cheng Y.L., Kim J.-G., Kim H.-B., Choi J.H., Fai Tsang Y., Baek K. Occurrence and removal of microplastics in wastewater treatment plants and drinking water purification facilities: a review. Chem. Eng. J. 2021;vol. 410 2021/04/15/ [Google Scholar]
- 68.Jiang J., Tang S., Han D., Fu G., Solomatine D., Zheng Y. A comprehensive review on the design and optimization of surface water quality monitoring networks. Environ. Model. Softw. 2020;vol. 132 2020/10/01/ [Google Scholar]
- 69.Hasadsri S., Maleewong M. Finite element method for dissolved oxygen and biochemical oxygen demand in an open channel. Procedia Environ. Sci. 2012;vol. 13:1019–1029. 2012/01/01/ 2012. [Google Scholar]
- 70.Shwetank Suhas, Chaudhary J.K. A comparative study of fuzzy logic and WQI for groundwater quality assessment. Procedia Comput. Sci. 2020;vol. 171:1194–1203. 2020/01/01/ 2020. [Google Scholar]
- 71.Gupta D., Sunita S.J., Saharan J.P. Physiochemical analysis of ground water of selected area of Kaithal city (Haryana) India. Researcher. 2009;vol. 1(2):1–5. [Google Scholar]
- 72.Gerba C.P., Pepper I.L. In: Environmental and Pollution Science. third ed. Brusseau M.L., Pepper I.L., Gerba C.P., editors. Academic Press; 2019. Chapter 24 – drinking water treatment; pp. 435–454. [Google Scholar]
- 73.McKeough P., Fagernäs L. Further evaporation and final treatment of process-water concentrates. Water Sci. Technol. 1999;vol. 40(11):25–32. 1999/01/01/ [Google Scholar]
- 74.Peralta-Maraver I., et al. The riverine bioreactor: an integrative perspective on biological decomposition of organic matter across riverine habitats. Sci. Total Environ. 2021 doi: 10.1016/j.scitotenv.2021.145494. 2021/02/01/ [DOI] [PubMed] [Google Scholar]
- 75.Montgomery H.A.C. The determination of biochemical oxygen demand by respirometric methods. Water Res. 1967;vol. 1(10):631–662. 1967/10/01/ 1967. [Google Scholar]
- 76.Wu C., Wu K.-B. Preparation of electrochemical sensor based on morphology-controlled platinum nanoparticles for determination of chemical oxygen demand. Chin. J. Anal. Chem. 2013;vol. 41(5):704–708. 2013/05/01/ 2013. [Google Scholar]
- 77.Joshi D.M., Kumar A., Agrawal N.J.R. j o c. Studies on physicochemical parameters to assess the water quality of river Ganga for drinking purpose in Haridwar district. 2009;vol. 2(1):195–203. [Google Scholar]
- 78.Bartarya S.K. Hydrochemistry and rock weathering in a sub-tropical Lesser Himalayan river basin in Kumaun, India. J. Hydrol. 1993;vol. 146:149–174. 1993/06/01/ 1993. [Google Scholar]
- 79.Alifujiang Y., Abuduwaili J., Groll M., Issanova G., Maihemuti B. Changes in intra-annual runoff and its response to climate variability and anthropogenic activity in the Lake Issyk-Kul Basin, Kyrgyzstan. CATENA. 2021;vol. 198 2021/03/01/ [Google Scholar]
- 80.Nayeb Yazdi M., Sample D.J., Scott D., Wang X., Ketabchy M. The effects of land use characteristics on urban stormwater quality and watershed pollutant loads. Sci. Total Environ. 2021 doi: 10.1016/j.scitotenv.2021.145358. 2021/01/28/ [DOI] [PubMed] [Google Scholar]
- 81.Jha P.K., Subramanian V., Sitasawad R. Chemical and sediment mass transfer in the Yamuna River — a tributary of the Ganges system. J. Hydrol. 1988;vol. 104(1):237–246. 1988/12/30/ [Google Scholar]
- 82.Anima U., Chandrakala M., Technology E. Water quality index of Ganga River water, Rishikesh, Uttarakhand, India. Int. J. Res. Appl. Sci. Eng. Technol. 2017;vol. 5(11):2876–2880. [Google Scholar]
- 83.S. Bora, Water quality analysis of river ganga: a case-study of Rishikesh-Haridwar-Garhmukteshwar Stretch (doctoral dissertation), National Institute of Technology Kurukshetra, 2016.
- 84.Trivedi R.C. Water quality of the Ganga River – an overview. Aquat. Ecosyst. Health Manag. 2010;13(4):347–351. [Google Scholar]
- 85.Siriopoulos C., Samitas A., Dimitropoulos V., Boura A., AlBlooshi D.M. In: Pollution Assessment for Sustainable Practices in Applied Sciences and Engineering. Mohamed A.-M.O., Paleologos E.K., Howari F.M., editors. Butterworth-Heinemann; 2021. Chapter 12 – health economics of air pollution; pp. 639–679. [Google Scholar]
- 86.Kota S.H., et al. Year-long simulation of gaseous and particulate air pollutants in India. 2018;vol. 180:244–255. [Google Scholar]
- 87.Singh A.A., Fatima A., Mishra A.K., Chaudhary N., Mukherjee A., Agrawal M., Agrawal S.B. Assessment of ozone toxicity among 14 Indian wheat cultivars under field conditions: growth and productivity. Environ. Monit. Assess. 2018;vol. 190(4):190. doi: 10.1007/s10661-018-6563-0. [DOI] [PubMed] [Google Scholar]
- 88.Tsai Y.I. Urban visibility and airborne PM10 aerosol in Southern Taiwan. J. Aerosol Sci. 2000;vol. 31:895–896. 2000/09/01/ 2000. [Google Scholar]
- 89.Lozhkin V., Lozhkina O., Dobromirov V. A study of air pollution by exhaust gases from cars in well courtyards of Saint Petersburg. Transp. Res. Procedia. 2018;vol. 36:453–458. 2018/01/01/ 2018. [Google Scholar]
- 90.Kumari P., Toshniwal D. Impact of lockdown measures during COVID-19 on air quality – a case study of India. Int. J. Environ. Health Res. 2020:1–8. doi: 10.1080/09603123.2020.1778646. [DOI] [PubMed] [Google Scholar]
- 91.Etchie T.O., Etchie A.T., Jauro A., Pinker R.T., Swaminathan N. Season, not lockdown, improved air quality during COVID-19 State of Emergency in Nigeria. Sci. Total Environ. 2021 doi: 10.1016/j.scitotenv.2021.145187. 2021/01/21/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Naqvi H.R., Datta M., Mutreja G., Siddiqui M.A., Naqvi D.F., Naqvi A.R. Improved air quality and associated mortalities in India under COVID-19 lockdown. Environ. Pollut. 2021;vol. 268 doi: 10.1016/j.envpol.2020.115691. 2021/01/01/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Samet J., Krewski D., environmental health P.A. Health effects associated with exposure to ambient air pollution. J. Toxicol. Environ. Health Part A. 2007;vol. 70(3–4):227–242. doi: 10.1080/15287390600884644. [DOI] [PubMed] [Google Scholar]
- 94.Kumar A., et al. Assessment of indoor air concentrations of VOCs and their associated health risks in the library of Jawaharlal Nehru University, New Delhi. Environ. Sci. Pollut Res. Int. 2014;vol. 21(3):2240–2248. doi: 10.1007/s11356-013-2150-7. [DOI] [PubMed] [Google Scholar]
- 95.Cattaneo A., et al. Environmental and biological monitoring of personal exposure to air pollutants of adult people living in a metropolitan area. Sci. Total Environ. 2021 doi: 10.1016/j.scitotenv.2020.144916. 2021/01/29/ [DOI] [PubMed] [Google Scholar]
- 96.Du W., Wang G.J.A., Research A.Q. Indoor air pollution was nonnegligible during covid-19 lockdown. Aerosol Air Qual. Res. 2020;vol. 20(9):1851–1855. [Google Scholar]
- 97.Huang W., Xie X., Qi X., Huang J., Li F. Determination of particle penetration coefficient, particle deposition rate and air infiltration rate in classrooms based on monitored indoor and outdoor concentration levels of particle and carbon dioxide. Procedia Eng. 2017;vol. 205:3123–3129. 2017/01/01/ 2017. [Google Scholar]
- 98.Ye W., Zhang X., Gao J., Cao G., Zhou X., Su X. Indoor air pollutants, ventilation rate determinants and potential control strategies in Chinese dwellings: a literature review. Sci. Total Environ. 2017;vol. 586:696–729. doi: 10.1016/j.scitotenv.2017.02.047. 2017/05/15/ 2017. [DOI] [PubMed] [Google Scholar]
- 99.Bravi L., Murmura F., Santos G. Additive manufacturing: possible problems with indoor air quality. Procedia Manuf. 2019;vol. 41:952–959. 2019/01/01/ 2019. [Google Scholar]
- 100.Zhang X., Chen B., Fan X. Different fuel types and heating approaches impact on the indoor air quality of rural houses in Northern China. Procedia Eng. 2015;vol. 121:493–500. 2015/01/01/ 2015. [Google Scholar]
- 101.Singh U., Wangia-Anderson V., Bernstein J.A. Chronic rhinitis is a high-risk comorbidity for 30-day hospital readmission of patients with asthma and chronic obstructive pulmonary disease. J. Allergy Clin. Immunol.: Pract. 2019;vol. 7(1):279–285. doi: 10.1016/j.jaip.2018.06.029. e6, 2019/01/01/ [DOI] [PubMed] [Google Scholar]
- 102.Naclerio R., Ansotegui I.J., Bousquet J., Canonica G.W., D’Amato G., Rosario N., Pawankar R., Peden D., Bergmann K.C., Bielory L., Caraballo L., Cecchi L., Cepeda S., Chong Neto H.J., Galán C., Gonzalez Diaz S.N., Idriss S., Popov T., Ramon G.D., Ridolo E., Rottem M., Songnuan W., Rouadi P. International expert consensus on the management of allergic rhinitis (AR) aggravated by air pollutants: impact of air pollution on patients with AR: Current knowledge and future strategies. World Allergy Organ. J. 2020;vol. 13(3) doi: 10.1016/j.waojou.2020.100106. 2020/03/01/ 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lai A.-J., Huang C.-Y. Effect of occupational exposure to noise on the health of factory workers. Procedia Manuf. 2019;vol. 39:942–946. 2019/01/01/ 2019. [Google Scholar]
- 104.Suthanaya P.A. Modelling road traffic noise for collector road (case study of Denpasar City) Procedia Eng. 2015;vol. 125:467–473. 2015/01/01/ 2015. [Google Scholar]
- 105.Basu B., Murphy E., Molter A., Basu A.S., Sannigrahi S., Belmonte M., Pilla F. Investigating changes in noise pollution due to the COVID-19 lockdown: the case of Dublin, Ireland. Sustain. Cities Soc. 2021;65 [Google Scholar]
- 106.Pobedin A.V., Shekhovtsov V.V., Dolotov A.A. Computational probabilistic evaluation of passenger cars noise level. Procedia Eng. 2017;vol. 206:1558–1563. 2017/01/01/ 2017. [Google Scholar]
- 107.Arora S., Bhaukhandi K.D., Mishra P.K. Coronavirus lockdown helped the environment to bounce back. Sci. Total Environ. 2020;742 doi: 10.1016/j.scitotenv.2020.140573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Williams R., Wright A.J., Ashe E., Blight L.K., Bruintjes R., Canessa R., Clark C.W., Cullis-Suzuki S., Dakin D.T., Erbe C., Hammond P.S., Merchant N.D., O’Hara P.D., Purser J., Radford A.N., Simpson S.D., Thomas L., Wale M.A. Impacts of anthropogenic noise on marine life: Publication patterns, new discoveries, and future directions in research and management. Ocean Coast. Manag. 2015;vol. 115:17–24. 2015/10/01/ 2015. [Google Scholar]
- 109.Hildebrand J.A. Anthropogenic and natural sources of ambient noise in the ocean. Mar. Ecol. Prog. Ser. 2009;395:5–20. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material