Abstract
Discharge counseling by pharmacists reduces adverse medication events, emergency department visits, and readmissions. Studies indicate that pharmacy students in advanced pharmacy practice experiences (APPE) can deliver effective medication-related activities. An open label randomized controlled trial was conducted in adults discharged on warfarin, insulin, or both. Pharmacy students performed medication reconciliation, structured medication counseling, and follow-up calls 72-hours post-discharge. The usual care arm received traditional education. The primary outcome was the 30-day readmission rate post-discharge. Ninety-eight patients on high-risk medications were randomized to intervention (n = 51) or usual care (n = 47). The 30-day hospital readmission rate was lower in the intervention group (8/51, 15% vs. 11/47, 23%); (p = 0.48). There was no statistical difference in the time to first unplanned health care use (hazard ratio = 0.49 (95 %CI, 0.19–1.24), or the time-to-first clinic visit post-discharge (p = 0.94) between the two arms. Students identified 26 drug-related problems during reconciliation. Patients in the intervention arm reported high satisfaction with the service (mean 3.94; SD 0.11). Involving APPE students in the transition of care activities presents an excellent opportunity to minimize pharmacists' workload while maintaining patient care services.
Keywords: Transitions of care, Discharge counseling, Pharmacy Students, Medication Reconciliation, Medication counseling, Post-discharge follow up, Drug-related problems
1. Introduction
The transition of care is defined as “a set of actions designed to ensure the coordination and continuity of health care as patients transfer between different locations or different levels of care in the same location” (Coleman 2003). The level of complexity varies among patients from simple transitions from the hospital to the home to transitions involving multiple healthcare settings (Oikonomou 2019). In addition to the various care settings, within and between each setting, many critical levels of coordination and communication exist. A single miscommunication or mistake can lead to a fatal error. Excessive medication errors during transitions of care occur primarily due to medication discrepancies and nearly 40% of these errors could possibly lead to moderate to severe clinical outcomes (Rozich et al., 2004, Cornish et al., 2005). During this critical process, patients are at high risk of 30-day readmission and adverse medication events. Forster et al. reported that 19% of patients discharged from a tertiary hospital to their homes experienced adverse events (Forster 2003). Furthermore, Jencks et al. analyzed Medicare claims data covering 15 months and 30-day readmission rates were calculated as high as 20% (Jencks 2009). Notably, researchers at Centers for Disease Control and Prevention and Emory University demonstrated that hospitalizations related to the “high-risk medications”, warfarin and insulin, were 33.3% and 13.9%, respectively among the elderly population (Budnitz 2011).
There are many factors that potentially contribute toward higher risk for care transition errors and/or miscommunication. Black and Duval reported that complicated patient cases and suboptimal communication, patient education, and patient follow up were the most common factors in Diabetes discharge planning during transitions of care (Black 2019). Furthermore, poor handoff communication between the hospital and the receiving care center (outpatient provider, home care, caregiver, or patient), inadequate provider patient assessment prior to discharge, poor discharge planning, and a lack of multidisciplinary coordination may also contribute to adverse events and lead to poor patient outcomes (Gheorghiade 2013).
Pharmacists play a pivotal role within a collaborating TOC healthcare team. Different models exist for integrating pharmacist service into TOC programs (Rochester-Eyeguokan 2016). A typical model involves the pharmacist conducting medication reconciliation, delivering patient-centered education, and resolving medication access issues during care transitions (Stroud 2019). Such a model also involved pharmacist performing follow-up services to ensure patients adherence to their medication regimens without adverse outcomes upon returning to their homes. In a meta-analysis, pharmacist-led medication reconciliation programs reduced 67% of adverse event-related hospital visits, 28% of emergency department visits, and 19% of hospital readmissions (Mekonnen 2016). A prospective randomized longitudinal study by Phatak et al. recorded a statistically significant difference in emergency department visits and readmission favoring pharmacist involvement in the TOC for high-risk patients (Phatak 2016).
Despite considerable evidence indicating the successes of TOC services, many barriers hinder the implementation of TOC programs. Limited staff resources, the need for additional support, and lack of a standardized discharge order times are among some of these barriers (Scott 2017). An alternative solution to overcome these challenges is by involving various pharmacy providers (residents, interns, students or pharmacy technicians). Pharmacy interns in the advanced pharmacy practice experience (APPE) program can assist during their internship year while practicing their knowledge and skills learned during the theoretical and introductory practical pharmacy courses. Several studies have demonstrated that APPE students can deliver effective medication-related education at levels comparable to certified pharmacists (Dalal et al., 2010, Lai et al., 2011, Dang et al., 2012, Dang et al., 2012, Shiyanbola et al., 2012, Hayes and Hutchison, 2013, Stebbins et al., 2013, Szkiladz et al., 2013, Vanderwielen et al., 2014, Adams et al., 2015, Beggs and Karst, 2016, Church et al., 2016, Albano 2018, Hertig et al., 2017, Rogers et al., 2017, Plakogiannis et al., 2019, O'Reilly et al., 2020).
Although published literature has demonstrated that pharmacist interventions in TOC programs have been successful, to our knowledge, there have not been any studies assessing the impact of a student-led TOC program specifically involving high-risk medications. This pilot project aimed to evaluate student-led TOC interventions on several outcome measures, including 30-day hospital readmission rates and relevant disease-state metrics. We hypothesized that patients enrolled in this program would have a lower hospital readmission rate and better clinical outcomes than those who are not. The objectives were to determine whether a student-led TOC program for patients discharged with high-risk medications, warfarin and/or insulin, reduces the rate of unplanned healthcare utilization at 30 days.
2. Methods
2.1. Study design and setting
A randomized controlled study was conducted in an academic medical center (King Saud Khalid University Hospital (KKUH). KKUH is a tertiary teaching hospital that primarily serves the employees of King Saud University and their dependents; however, a portion of the hospital’s patrons are Saudi nationals not affiliated with the university. The majority of patients are native Arabic speakers. The study period ran from October 2016 to April 2017. Participants were randomly assigned to either the standard of care or intervention groups and were followed for 30-days after discharge. King Saud University Institutional Review Board approved the study (Project number E-16–1957). The study was guided by the Consolidated Standards of Reporting Trials (CONSORT) checklist (Boutron 2017)
2.2. Participants and enrollment
Patients aged 18 years and older, discharged on either insulin, warfarin, or both, and were eligible for outpatient follow-up at KKUH were recruited. The following patients were excluded: patients diagnosed with a psychiatric disorder; patients with dementia; pregnant patients; patients with short life expectancy (<6 months); patients unable to self-manage their medications; patients who were discharged to a location other than their place of residence; patients who were discharged on pass; patients who were admitted for fewer than two days (e.g. receiving chemotherapy cycles or dialysis); patients without access to a telephone, and those discharged within 3 h of the receipt of the discharge order. During the study period, all insulin or warfarin orders were identified through the Cerner Millennium-based electronic health record, the Electronic System for Integrated Health Information. The insulin and warfarin orders were screened to identify eligible patients by two pharmacy interns.
2.3. Randomization and allocation
Patients were randomly assigned to standard of care or intervention groups using sequentially numbered, opaque sealed envelopes. The randomization sequence was generated by a member of the research team (HK) who did not have any direct clinical contact with the patients. The envelopes were placed in a secure locker and the key was only accessible to two members of the research team (AA and GB). Before opening the envelope, patient's file number was recorded on the envelope, and group assignment was then allocated.
2.4. Standard of care
At the time of the study, there were no clearly established discharge counselling services. At a minimum, patients with diabetes were often seen by a health educator and/or a dietitian to receive advice on their insulin regimen and/or diet. Some specialized units such as cardiology wards occasionally benefited from having clinical pharmacists who provided discharge counselling, however, staff workload and time constraints did not allow the delivery of discharge counselling to every patient.
2.5. Intervention
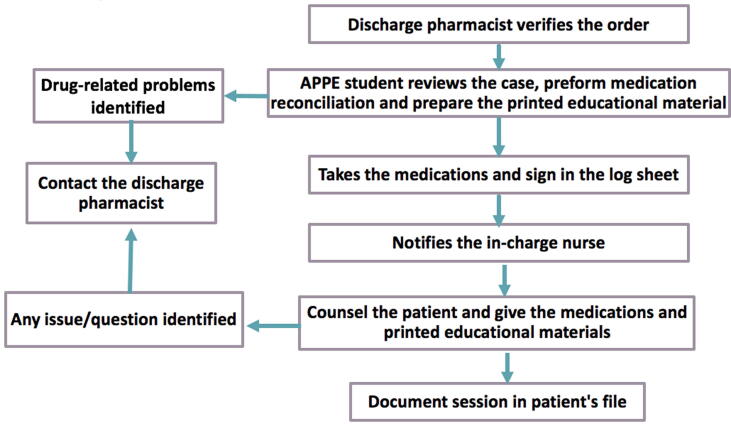
APPE pharmacy interns in their last professional year were involved in delivering student-led TOC interventions which consisted of four phases: medication reconciliation at the time of discharge before entering the patient room, a patient interview and counselling, a 72-hour follow-up phone call, and a 30-day follow-up phone call.
During medication reconciliation student interns compared patients' discharge medications to those documented on their admission medication lists. In case of discrepancies, students contacted the discharge pharmacist to initiate communication with the attending physician before patient discharge.
Under the supervision of two clinical pharmacists (GB and IS), who are members of the research team, the students then delivered structured, personalized discharge counselling on warfarin, insulin or both in the Arabic language to the patient and/or the caregiver. Students used the teach-back method to ensure each patient understood the instructions. At the end of the counselling session, the student provided the patient with printed educational materials from the hospital outpatient clinics about insulin and/or warfarin and an updated list of the patient's medications that was reviewed and approved by the pharmacist.
Following discharge, student interns conducted follow-up phone calls at 72-hour post-discharge to all intervention group patients. During the phone call, students assessed the patient's understanding of medication use, proper medication use, problems with accessing their medications, the effectiveness of therapy, and the presence of any potential adverse effects. Students also asked about any scheduled post-discharge appointments with their primary care provider or anticoagulation clinic. Based on the patient's individual needs, the students facilitated interventions by collaborating with the patient's physician and the attending clinical pharmacist to resolve any identified drug related problems (DRPs). Students contacted each patient 30 days after the initial follow-up call to ascertain study outcomes, i.e. rate of readmission, emergency department visits and utilization of any other health care services within the hospital, and patient satisfaction with the provided service. All phone calls were scripted and approved by the research team to ensure uniformity of questions asked and data collected (Appendix A: Scripted calls for the 72 hrs (A-1) and 30 days follow up (A-2).
2.6. Students' preparation and the delivery of the discharge counseling:
All students were required to complete reading assignments and attend a half-day training workshop to ensure a sufficient competency level. The workshop covered interviewing techniques, insulin types and administration technique, and medication-specific educational material. Student readiness was assessed against a competency checklist and an objective assessment exam with a required passing score of 100%. Students used an iPad preloaded with visual PowerPoint presentation on insulin and warfarin to ensure consistent delivery of critical counselling information for all patients and across participating students. The counseling covered the following: name and strength of the medication, the indication of the drug, expected benefits of treatment, expected duration of treatment, how much and how often to take the medication, possible medication, or dietary interactions, what to do in case of a missed dose, when to seek medical attention, any possible side effects and how to manage, storage recommendations and special monitoring requirements and dose adjustment (when appropriate).
2.7. Data collection
Data was collected from the electronic hospital records, the patient interview, and follow-up phone calls for participants in the intervention group between October 2016 and May 2017. For control participants, data was collected only from the electronic hospital record. The research team developed a data collection sheet to capture relevant information, including patient demographics, contact information, medical status, medications, type of interventions during the reconciliation, outcome measures, and the time spent on counseling and follow up encounters.
2.8. Outcomes
The primary outcome of this study was the readmission rate within thirty days of discharge. Secondary outcomes included time to first unplanned health care utilization, time to the first outpatient clinic visit, disease-specific parameters (glycosylated hemoglobin (HbA1C) and International normalization ratio (INR)), and the number and type of medication-related problems identified during the reconciliation stage. Additionally, in the intervention group, students assessed patient satisfaction with the service using a validated 20-item questionnaire known as the Patient Satisfaction with Pharmacist Services Questionnaire (PSPS.Q.20) (Sakharkar 2015).
2.9. Statistical analysis
2.9.1. Sample size calculation
The study used independent cases and controls where one control was assigned per case. Existing evidence indicated that the readmission rate among controls (usual care) was 0.3. If the true relative risk of readmission for intervention subjects compared to usual care was 0.6, the minimum sample size necessary to capture a medium effect size with a power of 0.80 and α of 0.05 was 214 intervention and 214 control subjects. However, due to study logistics, we opted for a pilot study design.
2.9.2. Data analysis
The participants were described using descriptive statistics. Chi-squared or Fisher exact tests were used to compare categorical data, and the Student t-test was used to compare continuous data. Independent Students t-test was also used to test the differences in index HbA1C and follow-up HbA1C, percentage INR test in range and percentage days within therapeutic range among the independent groups (control vs intervention). The Kaplan–Meier survival analysis and the Cox proportional-hazards model were employed to investigate the free survival of readmissions in both groups. The crude associations of survival between the two groups were evaluated with the Kaplan–Meier analysis. The Cox proportional-hazards model was used to estimate the hazard ratios (HR) and 95% confidence intervals (CI). For all statistical analysis, results were assumed to be significant when p was < 0.05. The tests were conducted using R software, version 4.0.3.
3. Results
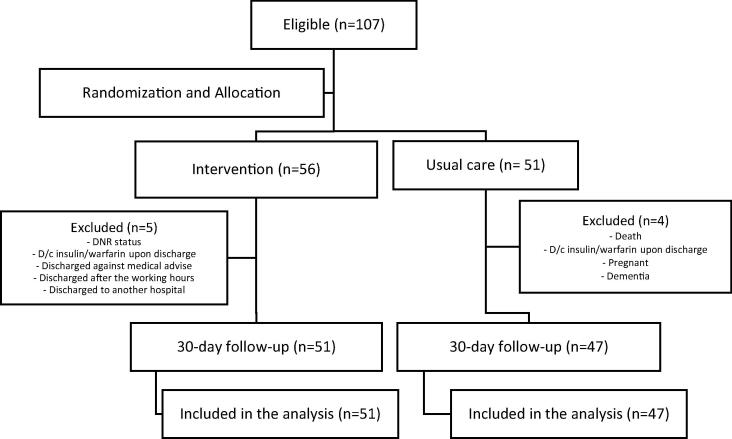
During the study period, 107-patients were discharged with the medications of interest (Fig. 1). After randomization, 56 patients were allocated to the intervention arm, and 51 were allocated to the control arm. Nine patients were excluded after randomization for the following reasons: death, do not resuscitate (DNR) status, discontinuation of insulin or warfarin upon discharge, discharge against medical advice, discharged after the working hours, discharged to another hospital, pregnancy, and dementia. A total of 98 patients (usual care = 47 and intervention = 51) were included in the study, and the final analysis. Participant baseline characteristics were similar between the two groups (Table 1). The mean (SD) age was 52.92 (15.9) for the intervention arm and 53.83 (15.41) for the control arm. Most patients were Saudi national and were females. The length of stay, acuity of admission, comorbidities, and previous 6-months emergency visits (LACE index) was similar between the two groups (p = 0.78). Per hospital practice, 74% of patients in the standard of care group received usual care discharge education, while 61% of patients in the intervention group received such education. In the intervention group, the mean time spent on discharge counselling sessions varied according to the medication involved; warfarin (23.89 ± 7.59 min), insulin (27.89 ± 8.92 min) and both drugs (34 ± 21.70 min) (Table 2). At the end of the counselling session, the percentage of information recall for insulin, warfarin, or both, was 79.62 ± 25.38, 77.29 ± 23.19 and 71.42 ± 18.89, respectively. In addition to counselling patients on insulin and warfarin, students performed counselling on other discharge medications (mean (SD) = 5.27 ± 3.83 drugs). The mean time to the 72-hr follow-up calls in the intervention group was 4.94 (2.4) days, and the mean (SD) time spent on these was 5 ± 1.0 min.
Fig. 1.
Participants Flowchart.
Table 1.
Participants Baseline Characteristics.
|
Control N = 47 |
Intervention N = 51 |
P-value | |
|---|---|---|---|
| Age, mean (SD) | 53.83 (15.41) | 52.92 (15.9) | 0.78 |
| Saudi National | 46 (98%) | 50 (98%) | |
| Gender (n,%) | 0.93 | ||
| Male | 18 (38%) | 21 (41%) | |
| Female | 29 (62%) | 30 (59%) | |
| Education Status (n,%) | 0.42 | ||
| Illiterate | 7 (15%) | 13 (25%) | |
| Primary or middle school | 15 (32%) | 16 (31%) | |
| High school | 12 (26%) | 10 (20%) | |
| University and above | 11 (23%) | 12 (24%) | |
| Missing | 2 (4.3) | 0 (0.0) | |
| Marital status (n,%) | 0.49 | ||
| Single | 6 (13%) | 8 (16%) | |
| Married | 26 (55%) | 38 (75%) | |
| Other | 3 (6%) | 5 (10%) | |
| Smoking Status (n,%) | 0.74 | ||
| Currently Smoker | 5 (11%) | 6 (12%) | |
| Non-smoker | 40 (85%) | 41 (80%) | |
| Ex-smoker | 2 (4%) | 4 (8%) | |
| LACE Index* n,% | 0.78 | ||
| Low risk | 2 (4%) | 1 (2%) | |
| Moderate risk | 15 (32%) | 17 (33%) | |
| High risk | 17 (36%) | 22 (43%) | |
| Very high risk | 13 (28%) | 11 (22%) | |
| Baseline HgA1c (%), mean (SD) | 9.14 (2.17) | 9.42 (2.61) | 0.59 |
| Baseline INR, mean (SD) | 1.64 (0.88) | 1.59 (0.68) | 0.77 |
| No. of Medications upon discharge mean (SD) | 9.32 (4.14) | 8.39 (3.53) | 0.24 |
| High risk medication (n,%) | 0.66 | ||
| Insulin | 30 (64%) | 31 (61%) | 0.77 |
| Warfarin | 13 (28%) | 17 (33%) | |
| Both | 4 (9%) | 3 (6%) | |
| Discharge Education as per standard of care in the hospital (n,%) | 47 (74%) | 51 (61%) | 0.08 |
| Diabetic educator | 12 (26%) | 14 (27%) | |
| Health educator | 3 (6%) | 8 (16%) | |
| Nurse education | 13 (28%) | 6 (12%) | |
| More than one type of education | 7 (15%) | 3 (6%) | |
| Not discharge education provided | 12 (26%) | 20 (39%) |
SD = Standard deviation; INR = international normalizing ratio; HgA1C = hemoglobin A1c
Chi-squared or Fisher exact tests were used to compare categorical data, and the Student t-test was used to compare continuous data
Table 2.
Summary of the Discharge Counseling Sessions in the Intervention Group.
| Discharged on Insulin (N = 31) | Discharged on warfarin (N = 17) | Discharged on both (N = 3) | |
|---|---|---|---|
| Mean time for the counseling session (in minutes) | 27.89 ± 8.92 | 23.89 ± 7.59 | 34 ± 21.70 |
| Mean time for the 72-hr follow-up phone call (in minutes) | 5.81 ± 2.57 | 4.44 ± 0.96 | 5 ± 1.0 |
| Score of percentage of information recall at the end of counseling session (mean, SD) | 79.62 ± 25.38 | 77.29 ± 23.19 | 71.42 ± 18.89 |
| Number of other medications counseled on (mean, SD) | 5.27 ± 3.83 | ||
3.1. Primary outcome
Eight patients in the intervention and 11 patients in the standard of care arms were readmitted within 30 days post-discharge. There was no difference in this primary outcome between the intervention (8/51;15%) and the standard of care groups (11/47; 23%), p = 0.48 (Table 3).
Table 3.
Effect of Student-Led TOC program on 30-day readmission rate, post-discharge clinic visits and clinical parameters.
| Usual careN = 47 | InterventionN = 51 | p-value* | |
|---|---|---|---|
| Primary Outcome | |||
| Readmission rate within 30 days | 11 (23%) | 8 (15%) | 0.48 |
| Secondary Outcomes | |||
| Time to 1st unplanned HC utilization post discharge | |||
| Pos-discharge clinic visits (n,%) | 0.94 | ||
|
25 (76%) | 27 (84%) | |
|
14 (88%) | 18 (90%) | |
| Time to First Clinic visit post discharge (days, mean (SD) | 17.90 (18.98) | 16.23 (15.99) | 0.67 |
|
17 (28) | 17 (25) | |
|
4.5 (5.75) | 7 (12.5) | |
| HgA1C on follow-up (mean, SD) | 8.92 (1.98) | 9.26 (2.13) | 0.53 |
| Percentage INR test in range (mean, SD) | 45.21 (28.07) | 28.09 (29.77) | 0.09 |
| Percentage days within therapeutic range (mean, SD) | 45.89 (33.32) | 37.45 (34.49) | 0.46 |
Chi-squared or Fisher exact tests were used to compare categorical data, and the Student t-test was used to compare continuous data. HbA1C: Hemoglobin A1c. INR: International Standardized ratio. SD = standard deviation.
3.2. Secondary outcomes
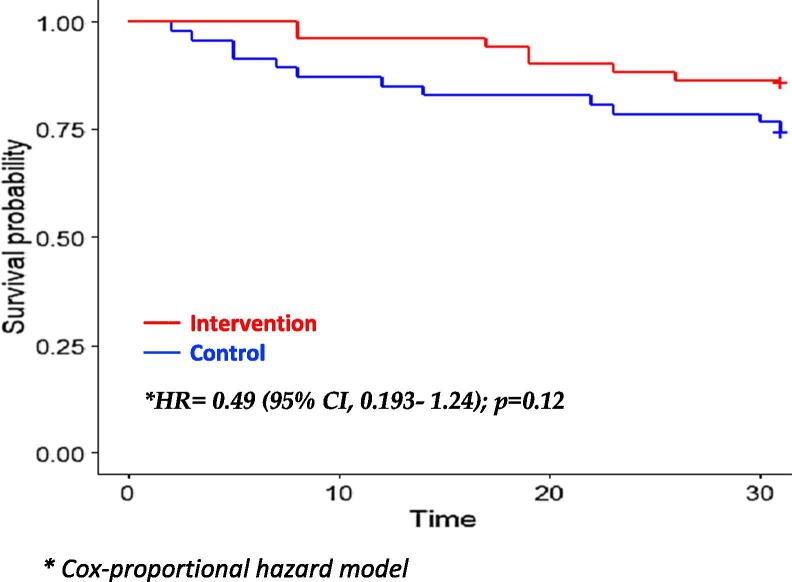
The mean time (in days) to the first unplanned health care utilization was not statistically significant; the hazard ratio was 0.49 (95% CI, 0.19–1.24); p = 0.12 (Fig. 2). The time-to-first clinic visit post-discharge was earlier in the intervention group; however, this was not statistically significant (16.23 ± 15.99 days vs. 17.9 ± 18.95 days; p = 0.94) (Table 3). Also, the impact of the student-led intervention did not reflect on any significant improvement in INR or HbA1C at follow up (p = 0.088 and p = 0.525 respectively) between the two groups. Students identified 26 DRPs during the reconciliation with most DRPs related to indication (n = 10), drug dosage regimen (n = 8) and miscellaneous DRP related to missed medications(n = 5) and additional lab before discharge (n = 3) (Table 4). Patients in the intervention arm reported high satisfaction with the service on the PSPS.Q.20 survey (mean 3.94[SD 0.11]).
Fig. 2.
Survival curve to first unplanned healthcare utilization*
Table 4.
Drug-related problems identified during medication reconciliation by students.
| Drug-related Problem | Frequency (Total = 26) |
|---|---|
| Indication DRPs (n = 10) | Total = 10 |
|
4 |
|
4 |
|
2 |
| Drug Dosage Regimen DRPs (n = 8) | |
|
2 |
|
1 |
|
1 |
|
3 |
|
1 |
| Other Miscellaneous DRPs (n = 8) | |
|
5 |
|
3 |
4. Discussion
This pilot randomized controlled trial evaluated two aspects of implementing a student-led TOC program. The first aspect investigated the impact on unplanned health care utilization within 30 days following hospital discharge. Although the 30-day readmission rate was lower in the intervention group (15%) than the standard of care group (23%), this difference was not statistically significant, as with the time for the first unplanned visit; however, the hazard ratio confidence interval did not rule out a potential clinical benefit of the intervention. This preliminary non statistically significant result can be attributed to the pilot study design and the short study duration (over seven months) to detect significance. In particular, the impact on improvement on clinical parameters (TTR and HbA1C) was not ascertained due to the short follow up period of these outcomes (Suen et al., 2020). Additionally, we found a non-significant difference in education and counseling as per hospital practice between the two groups; we associated such observation to the physical presence of students on the ward, which may have influenced the nurses' behavior to perform more discharge counseling for patients not visited by the APPE students (nurse education in the control group = 28% vs. 12% in the intervention arm). Correspondingly, fewer patients in the intervention group received any type of per hospital practice education compared to the standard of care group (26% vs. 39%). In the present pilot study, APPE students identified additional DRPs and discrepancies during discharge reconciliation (n = 26), which is an expected finding that agrees with the literature. A systematic review and meta-analysis demonstrated a significant reduction in medication discrepancies (RR 0·34; 95% CI: 0·23-0·50) in pharmacy-led medication reconciliation programs compared to usual care with a consequent reduction in medication-related events (Mekonnen 2016).
Moreover, although we did not assess patient medication adherence, the level of knowledge recalled by patients at the 72-hr phone call was satisfactory (>70%). The PSQSP survey results clearly showed patient satisfaction with the pharmacy services resulting in a mean score of 3.94 out of 4. Both high recall rate and satisfaction with care may boost patient’s adherence to their medications (Gu et al., 2008, Stroud et al., 2019). Furthermore, Stroud et al. demonstrated the importance of follow up phone call on improving patient adherence in pharmacist-led TOC program (Stroud 2019). In a study by Mills et al., patients with heart failure received verbal and written medication education by pharmacy students, and the impact on 30-day all-cause readmission rate and satisfaction with service at one week post-discharge was compared with historical patients who received medication education by nurses (Mills 2019). The study showed no difference in satisfaction between the two groups because the program was stopped early due to logistic constraints and a high rate of unanswered calls. In the present study, all patients in the intervention group responded to the satisfaction survey, which was delivered 30 days post-discharge and patients were highly satisfied with care provided. However, we did not assess patient satisfaction among the control group.
The second aspect of this pilot study is to assess the feasibility of utilizing APPE pharmacy students in performing transition of care activities, hence improve and sustain pharmacy patient care services. Several literature and organizations voiced concern about resources limitation when extending pharmacy services, especially for clinical activities such as medication reconciliation, the transition of care, patient education, care coordination (Hume et al., 2012, Couture et al., 2016, Scott et al., 2017) Abundance of studies described successful experiences in employing Pharmacy extenders such as residents, APPE and IPPE students and pharmacy technicians to deliver discrete functions that match their level of knowledge and training (Dalal et al., 2010, Dang et al., 2012, Hayes and Hutchison, 2013, Stebbins et al., 2013, Szkiladz et al., 2013, Adams et al., 2015, Beggs and Karst, 2016, Church et al., 2016, Albano 2017, Hertig et al., 2017, Rogers et al., 2017, Vavra et al., 2018, Plakogiannis et al., 2019, O'Reilly et al., 2020, Suen et al., 2020). Indeed, students in this study were able to implement a simple and structured transition of care program at no excess cost while ensuring such service is offered to patients at high risk of readmission. Vavra et al., described a pilot student-operated TOC that demonstrated APPE students ability to be highly engaged in broadening clinical pharmacy services (Vavra 2018). The study described a TOC pilot service that required APPE students to perform, under preceptor supervision, a checklist of activities that included medication reconciliation on admission, during the hospital stay, and upon discharge, assess adherence, provide discharge counseling, and prepare care document for the primary care provider. Study findings highlighted the multiple benefits to students, patients, pharmacy services and the hospital. Kelsh et al., described a 3-step TOC service led by student pharmacists and covered activities during the inpatient stay, upon discharge, and at follow-up (Kelsh 2021). The study concluded that appropriately trained APPE students are well-positioned to deliver TOC activities and contribute effectively to address medication concerns and provide education. Likewise, in the present study, APPE students were able to implement structured TOC activities, although the checklist of list activities is slightly different in our model that included medication reconciliation upon discharge, resolving DRP, discharge counseling, patient education, and follow up phone call. The program demonstrated the feasibility of utilizing APPE students to operate the service hence reducing the load on pharmacists, improving and optimizing patient care and potentially propose cost savings to the hospital. Mos importantly, exposing students to TOC activities during APPE offer them real-world experience helping reinforce the didactic aspects of the curriculum, expand their own learning, and boost their confidence and engagement in such activities in the future. (Lancaster et al., 2013, Taylor et al., 2019, Blakely and Ekong, 2021).
Ensuring APPE students’ preparedness and competency to deliver high-quality TOC is important. Therefore, in the present study a formal training was provided to students before they embark on providing TOC program. Dunkley et al, described a REWARD training program to prepare APPE students to deliver medication education targeting four classes of high-risk medications (anticoagulants, inhalers, insulin, and naloxone) (Dunkley 2020). The REWARD system included six distinct steps, which incorporated student self-directed and pharmacist-facilitated learning (Read handbook, Electronic learning, Workshop, Assessment, Review of checklist, Direct observation, and Sign-off). Successful completion was measured when students achieved a 100% on medication education criteria checklist. Similarly, APPE students in this pilot study underwent a half-day workshop that covered interviewing techniques, insulin types and administration technique, and medication-specific educational material. Student readiness was assessed against a competency checklist and an objective assessment exam with a required passing score of 100%. Although we did not have a Sign-off step that focuses on the logistics, we provided a flowchart for our student to follow from the point of identifying the patient until providing the final education to the patient.
Our study has several strengths. Firstly, the study was a randomized controlled trial with a structured intervention. Secondly, the intervention implemented was of high fidelity and included pre-discharge elements (medication reconciliation and discharge counseling) with a post-discharge intervention that consisted of a follow-up phone call that provided additional support for the patients in the post-discharge period. Thirdly, the active participation of students in patient education provided an opportunity for the students to improve the initiation of pharmacy TOC services at the hospital. As demonstrated by this study, involving pharmacy student interns is a feasible and viable option to improve the infrastructure in care delivery (Fig. 3).
Fig. 3.
Student-Led Transition of Care Program Process.
The limitations of this study include a small sample size; therefore, a more extended study with sufficient sample size and duration is recommended. The TOC program was conducted in a single academic medical center, and the results may not be generalizable beyond this setting. There were a limited number of students involved due to time restraints and may have impeded the progress of the program and additional recruitment of patients. Finally, the lack of confirmation of healthcare utilization of healthcare services from outside KKUH in the usual care group may have led to an underestimation of their 30-day readmission rates.
5. Conclusion
Integrating APPE students in TOC activities is feasible and provided an excellent opportunity to reduce pharmacists' workload, maintain patient care services, improve patient satisfaction while providing learning opportunities for students. Pharmacy programs, especially those affiliated with a teaching hospital, may consider offering a required TOC rotation during the APPE; this will help alleviate time conflicts with other rotational activities and ensure service coverage throughout the internship year. In addition, future studies should emphasize TOC in an interprofessional health care approach.
Funding
The authors extend their appreciation to the Deanship of Scientific Research at King Saud University for funding this work through research group no (RG-1441-367).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Ghada Bawazeer, Email: gbawazeer@ksu.edu.sa.
Ibrahim Sales, Email: isales@ksu.edu.sa.
Mohammad H. Aljawadi, Email: maljawadi@ksu.edu.sa.
Haya M. Almalag, Email: halmalaq@ksu.edu.sa.
Hadeel Alkofide, Email: halkofide@ksu.edu.sa.
Fakhr Alayoubi, Email: fayoubi@ksu.edu.sa.
Appendix A.
Appendix A-1. Scripted follow-up call at 72 h (intervention group only)
| 1. What medications are you currently taking? |
| 2. Explain to me when and how you should take your medications (mention the name of the drug: warfarin or insulin)? |
| 3. Have you missed any doses of your medications? |
| 4. How do you feel since taking your medications? |
| 5. Are you having any unwanted effects from your medications? (specifically mention bleeding for warfarin and hypoglycemia for insulin) |
| 6. What questions do you have about your medications? |
| 7. Has anything changed with your health or medications since we last met? |
| 8. What date/when is your appointment with your primary care doctor? |
| 9. What other questions do you have? |
Appendix A-2. Scripted follow-up call 30-days post-discharge (for both intervention and control)
| 1. How have you been since your discharge? |
| 2. Can you tell if you had to go to ER or got admitted during this past month? |
| 3. If yes, ask: what was your main complaint for seeking healthcare? If hospitalized, ask about the length of stay in days. |
| 4. Where did you receive the unplanned care? (KKUH, or other facilities) |
| 5. Were there any changes to your medications? Document the changes. |
| 6. Have you seen your care provider in the outpatient clinic? |
References
- Adams R.P., Barton G., Bhattacharya D., Grassby P.F., Holland R., Howe A., Norris N., Shepstone L., Wright D.J. Supervised pharmacy student-led medication review in primary care for patients with type 2 diabetes: a randomised controlled pilot study. BMJ Open. 2015;5(11) doi: 10.1136/bmjopen-2015-009246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albano M.E., Bostwick J.R., Ward K.M., Fluent T., Choe H.M. Discrepancies Identified Through a Telephone-Based, Student-Led Initiative for Medication Reconciliation in Ambulatory Psychiatry. Journal of Pharmacy Practice. 2018;31(3):304–311. doi: 10.1177/0897190017715391. [DOI] [PubMed] [Google Scholar]
- Beggs A.E., Karst A.C. Effectiveness of Pharmacy Student-Led Health Education in Adults Experiencing Homelessness. J Health Care Poor Underserved. 2016;27(3):954–960. doi: 10.1353/hpu.2016.0125. [DOI] [PubMed] [Google Scholar]
- Black R.L., Duval C. Diabetes Discharge Planning and Transitions of Care: A Focused Review. Curr Diabetes Rev. 2019;15(2):111–117. doi: 10.2174/1573399814666180711120830. [DOI] [PubMed] [Google Scholar]
- Blakely M.L., Ekong G. Student pharmacists' perspectives on training, readiness, and confidence to provide transition of care services. Curr Pharm Teach Learn. 2021;13(5):526–529. doi: 10.1016/j.cptl.2021.01.011. [DOI] [PubMed] [Google Scholar]
- Boutron, I., Altman, D. G., Moher, D., Schulz, K. F., Ravaud, P., and Consort NPT Group, 2017. “CONSORT Statement for Randomized Trials of Nonpharmacologic Treatments: A 2017 Update and a CONSORT Extension for Nonpharmacologic Trial Abstracts.” Ann Intern Med 167 (1), 40. [DOI] [PubMed]
- Budnitz D.S., Lovegrove M.C., Shehab N., Richards C.L. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002–2012. doi: 10.1056/NEJMsa1103053. [DOI] [PubMed] [Google Scholar]
- Church D., Johnson S., Raman-Wilms L., Schneider E., Waite N., Pearson Sharpe J. A literature review of the impact of pharmacy students in immunization initiatives. Can Pharm J (Ott) 2016;149(3):153–165. doi: 10.1177/1715163516641133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman E.A., Boult C. Improving the quality of transitional care for persons with complex care needs. J Am Geriatr Soc. 2003;51(4):556–557. doi: 10.1046/j.1532-5415.2003.51186.x. [DOI] [PubMed] [Google Scholar]
- Cornish P.L., Knowles S.R., Marchesano R., Tam V., Shadowitz S., Juurlink D.N., Etchells E.E. Unintended medication discrepancies at the time of hospital admission. Arch Intern Med. 2005;165(4):424–429. doi: 10.1001/archinte.165.4.424. [DOI] [PubMed] [Google Scholar]
- Couture M., Sasseville M., Gascon V. Facilitators and barriers to implementing transitional care managers within a public health care system. Journal of gerontological social work. 2016;59(4):364–377. doi: 10.1080/01634372.2016.1218988. [DOI] [PubMed] [Google Scholar]
- Dalal K., McCall K.L., Fike D.S., Horton N., Allen A. Pharmacy students provide care comparable to pharmacists in an outpatient anticoagulation setting. Am J Pharm Educ. 2010;74(8):139. doi: 10.5688/aj7408139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dang C.J., Dudley J.E., Truong H.A., Boyle C.J., Layson-Wolf C. Planning and implementation of a student-led immunization clinic. Am J Pharm Educ. 2012;76(5):78. doi: 10.5688/ajpe76578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkley K.A., Evelyn D., Timmons V., Feller T.T. Implementation of a medication education training program for student pharmacists employed within an academic medical center. Am J Health Syst Pharm. 2020;77(3):206–213. doi: 10.1093/ajhp/zxz309. [DOI] [PubMed] [Google Scholar]
- Forster A.J., Murff H.J., Peterson J.F., Gandhi T.K., Bates D.W. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- Gheorghiade M., Vaduganathan M., Fonarow G.C., Bonow R.O. Rehospitalization for heart failure: problems and perspectives. J Am Coll Cardiol. 2013;61(4):391–403. doi: 10.1016/j.jacc.2012.09.038. [DOI] [PubMed] [Google Scholar]
- Gu N.Y., Gai Y., Hay J.W. The effect of patient satisfaction with pharmacist consultation on medication adherence: an instrumental variable approach. Pharm Pract (Granada) 2008;6(4):201–210. doi: 10.4321/s1886-36552008000400006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes C., Hutchison L.C. Development and evaluation of a student-led Medicare Part D Planning Clinic. Consult Pharm. 2013;28(4):237–242. doi: 10.4140/TCP.n.2013.237. [DOI] [PubMed] [Google Scholar]
- Hertig R., Ackerman R., Zagar B., Tart S. Pharmacy student involvement in a transition of care program. Curr Pharm Teach Learn. 2017;9(5):841–847. doi: 10.1016/j.cptl.2017.06.004. [DOI] [PubMed] [Google Scholar]
- Hume A.L., Kirwin J., Bieber H.L., Couchenour R.L., Hall D.L., Kennedy A.K., LaPointe N.M.A., Burkhardt C.D.O., Schilli K., Seaton T., Trujillo J., Wiggins B. Improving care transitions: current practice and future opportunities for pharmacists. Pharmacotherapy, The Journal of Human Pharmacology and Drug Therapy. 2012;32(11):e326–e337. doi: 10.1002/phar.1215. [DOI] [PubMed] [Google Scholar]
- Jencks S.F., Williams M.V., Coleman E.A. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- Kelsh, S., de Voest, M., and Stout, M., 2021. “Improving 30-day readmissions: Student pharmacists' role in transitions of care.” J Am Pharm Assoc (2003) 61 (4): e233-e236. [DOI] [PubMed]
- Lai C.J., Smith A.R., Stebbins M.R., Cutler T.W., Lipton H.L. Promoting interprofessional collaboration: pharmacy students teaching current and future prescribers about Medicare Part D. J Manag Care Pharm. 2011;17(6):439–448. doi: 10.18553/jmcp.2011.17.6.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lancaster J.W., Douglass M.A., Gonyeau M.J., Wong A., Woolley A.B., Divall M.V. Providers' perceptions of student pharmacists on inpatient general medicine practice experiences. Am J Pharm Educ. 2013;77(2):26. doi: 10.5688/ajpe77226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekonnen A.B., McLachlan A.J., Brien J.E. Pharmacy-led medication reconciliation programmes at hospital transitions: a systematic review and meta-analysis. J Clin Pharm Ther. 2016;41(2):128–144. doi: 10.1111/jcpt.12364. [DOI] [PubMed] [Google Scholar]
- Mills A.A., Rodeffer K.M., Quick S.L. Impact of Heart Failure Transitions of Care Program: A Prospective Study of Heart Failure Education and Patient Satisfaction. Hospital Pharmacy. 2021;56(4):252–258. doi: 10.1177/0018578719889020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly, E. A., Kuszmaul, A. K., Carter, A. M., Kreft, K. N., and Spencer, C. A., 2020. “Impact of a transitions of care pilot service established by pharmacy residents within an academic medical center.” J Am Pharm Assoc (2003) 60 (1), 87-92 e82. [DOI] [PubMed]
- Oikonomou E., Chatburn E., Higham H., Murray J., Lawton R., Vincent C. Developing a measure to assess the quality of care transitions for older people. BMC Health Serv Res. 2019;19(1):505. doi: 10.1186/s12913-019-4306-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phatak A., Prusi R., Ward B., Hansen L.O., Williams M.V., Vetter E., Chapman N., Postelnick M. Impact of pharmacist involvement in the transitional care of high-risk patients through medication reconciliation, medication education, and postdischarge call-backs (IPITCH Study) J Hosp Med. 2016;11(1):39–44. doi: 10.1002/jhm.2493. [DOI] [PubMed] [Google Scholar]
- Plakogiannis R., Mola A., Sinha S., Stefanidis A., Oh H., Katz S. Impact of Pharmacy Student-Driven Postdischarge Telephone Calls on Heart Failure Hospital Readmission Rates: A Pilot Program. Hosp Pharm. 2019;54(2):100–104. doi: 10.1177/0018578718769243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochester-Eyeguokan C.D., Pincus K.J., Patel R.S., Reitz S.J. The Current Landscape of Transitions of Care Practice Models: A Scoping Review. Pharmacotherapy. 2016;36(1):117–133. doi: 10.1002/phar.1685. [DOI] [PubMed] [Google Scholar]
- Rogers J., Pai V., Merandi J., Catt C., Cole J., Yarosz S., Wehr A., Durkin K., Kaczor C. Impact of a pharmacy student-driven medication delivery service at hospital discharge. Am J Health Syst Pharm. 2017;74(5 Supplement 1):S24–S29. doi: 10.2146/ajhp150613. [DOI] [PubMed] [Google Scholar]
- Rozich J.D., Howard R.J., Justeson J.M., Macken P.D., Lindsay M.E., Resar R.K. Standardization as a mechanism to improve safety in health care. Jt Comm J Qual Saf. 2004;30(1):5–14. doi: 10.1016/s1549-3741(04)30001-8. [DOI] [PubMed] [Google Scholar]
- Sakharkar P., Bounthavong M., Hirsch J.D., Morello C.M., Chen T.C., Law A.V. Development and validation of PSPSQ 2.0 measuring patient satisfaction with pharmacist services. Res Social Adm Pharm. 2015;11(4):487–498. doi: 10.1016/j.sapharm.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Scott A.M., Li J., Oyewole-Eletu S., Nguyen H.Q., Gass B., Hirschman K.B., Mitchell S., Hudson S.M., Williams M.V. Understanding Facilitators and Barriers to Care Transitions: Insights from Project ACHIEVE Site Visits. The Joint Commission Journal on Quality and Patient Safety. 2017;43(9):433–447. doi: 10.1016/j.jcjq.2017.02.012. [DOI] [PubMed] [Google Scholar]
- Shiyanbola O.O., Lammers C., Randall B., Richards A. Evaluation of a student-led interprofessional innovative health promotion model for an underserved population with diabetes: a pilot project. J Interprof Care. 2012;26(5):376–382. doi: 10.3109/13561820.2012.685117. [DOI] [PubMed] [Google Scholar]
- Stebbins M.R., Frear M.E., Cutler T.W., Lightwood J.M., Fingado A.R., Lai C.J., Lipton H.L. Pharmacy students teaching prescribers strategies to lower prescription drug costs for underserved patients. J Manag Care Pharm. 2013;19(7):534–541. doi: 10.18553/jmcp.2013.19.7.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud A., Adunlin G., Skelley J.W. Impact of a Pharmacy-Led Transition of Care Service on Post-Discharge Medication Adherence. Pharmacy (Basel) 2019;7(128):2–8. doi: 10.3390/pharmacy7030128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suen J., Attrill S., Thomas J.M., Smale M., Delaney C.L., Miller M.D. Effect of student-led health interventions on patient outcomes for those with cardiovascular disease or cardiovascular disease risk factors: a systematic review. BMC Cardiovascular Disorders. 2020;20(1):332. doi: 10.1186/s12872-020-01602-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szkiladz A., Carey K., Ackerbauer K., Heelon M., Friderici J., Kopcza K. Impact of pharmacy student and resident-led discharge counseling on heart failure patients. J Pharm Pract. 2013;26(6):574–579. doi: 10.1177/0897190013491768. [DOI] [PubMed] [Google Scholar]
- Taylor H., Englin E.F., Gubbins P.O. Development, implementation and perceived benefits of student pharmacist learning experiences in transitions of care. Currents in Pharmacy Teaching and Learning. 2019;11(10):1041–1048. doi: 10.1016/j.cptl.2019.06.011. [DOI] [PubMed] [Google Scholar]
- Vanderwielen L.M., Vanderbilt A.A., Dumke E.K., Do E.K., Isringhausen K.T., Wright M.S., Enurah A.S., Mayer S.D., Bradner M. Improving public health through student-led interprofessional extracurricular education and collaboration: a conceptual framework. J Multidiscip Healthc. 2014;7:105–110. doi: 10.2147/JMDH.S52019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavra K., Paluzzi M., de Voest M., Raguckas S., Slot M. Preliminary findings from a student pharmacist operated transitions of care pilot service. Currents in Pharmacy Teaching and Learning. 2018;10(1):78–84. doi: 10.1016/j.cptl.2017.09.018. [DOI] [PubMed] [Google Scholar]