Abstract
Background.
Targeted naloxone distribution to potential overdose bystanders increases the timeliness of overdose response and reduces mortality. Little is known, however, about the patterns of decision-making among overdose lay responders. This study explored heuristic decision-making among laypersons equipped with an emergency response smartphone app.
Methods.
UnityPhilly, a smartphone app that connects lay responders equipped with naloxone to overdose victims, was piloted in Philadelphia from March 2019 to February 2020. Participants used the app to signal overdose alerts to peer app users and emergency medical services, or respond to alerts by arriving at overdose emergency sites. This study utilised in-depth interviews, background information, and app use data from a sample of 18 participants with varying histories of opioid use and levels of app use activity.
Results.
The sample included 8 people who used opioids non-medically in the past 30 days and 10 people reporting no opioid misuse. Three prevailing, not mutually exclusive, heuristics were identified. The heuristic of unconditional signalling (“Always signal for help or backup”) was used by 7 people who valued external assistance and used the app as a replacement for a 911 call; this group had the highest number of signalled alerts and on-scene appearances. Nine people, who expressed confidence in their ability to address an overdose themselves, followed a heuristic of conditional signalling (“Rescue, but only signal if necessary”); these participants had the highest frequency of prior naloxone administrations. Eleven participants used the heuristic of conditional responding (“Assess if I can make a difference”), addressing an alert if they carried naloxone, were nearby, or received a signal before dark hours.
Conclusion.
The deployment of specific heuristics was influenced by prior naloxone use and situational factors. Success of overdose prevention interventions assisted by digital technologies may depend on the involvement of people with diverse overdose rescue backgrounds.
Keywords: opioid overdose, naloxone, lay responders, smartphone app, heuristics
Introduction
The U.S. drug overdose crisis has contributed to 72,707 deaths provisionally reported in 2019 (Ahmad, Rossen, & Sutton, 2020), an almost 8% increase compared to 2018 when 67,367 people died of overdose (Hedegaard, Miniño, & Warner, 2020). In the first 6 months of 2019, more than 80% of overdose deaths involved opioids alone (especially fentanyl or fentanyl analogues) or mixed with stimulants, as indicated by data from 24 states and the District of Columbia (O’Donnell, Gladden, Mattson, Hunter, & Davis, 2020). Targeted distribution of naloxone, an opioid antagonist, to lay first responders has been recognized as an evidence-based overdose prevention intervention (Carroll, Green, & Noonan, 2018). Such programs were found to reduce overdose mortality (Walley et al, 2013), increase the likelihood of naloxone use for overdose emergency (Clark, Wilder, & Winstanley, 2014), and to be cost-effective (Townsend et al, 2020). A 2019 survey among U.S. syringe service programs implementing overdose education and naloxone distribution reported that during the previous 12 months, 237 organisations distributed naloxone to 230,506 laypersons with the average rate of 3 doses distributed per person (Lambdin et al, 2020).
Understanding factors that influence rescue behaviours of overdose lay responders, especially those with active drug use, is necessary to increase the impact of community-based overdose prevention interventions. Overall, research has documented that altruism and mutual aid have been a driving force behind many helping behaviours of people who use drugs (Friedman et al., 2015), including overdose reversals (Bathje, Pillersdorf, Kacere, & Bigg, 2020). Particularly, in regard to dialling 911 during an overdose, studies found that fear of the police (Koester et al, 2017; Latimore & Bergstein, 2017; Wagner, 2019), lack of trust in medical staff (Koester et al, 2017), feeling competent to reverse an overdose without medical help (Koester et al, 2017; Neale et al., 2019), and responding in a group of bystanders (Tobin, Davey, & Latkin, 2005) reduced the chances of a 911 call. In contrast, knowledge of Good Samaritan Laws (Jakubowski, Kunins, Huxley-Reicher, & Siegler, 2018), seeking professional help to prevent a repeated overdose (Neale et al. 2019), and the inability to reverse an overdose with naloxone (Ataiants et al, 2020) increased the willingness to dial 911.
A separate line of qualitative research examined the complexity of decision-making in situations involving peer naloxone use. On one hand, once equipped with naloxone, lay responders were found to be empowered by their new role of overdose rescuers and capable of making effective decisions in overdose emergency situations (Bardwell, Fleming, Collins, Boyd, & McNeil, 2019; Faulkner-Gurstein, 2017; Neale et al., 2019; Wagner et al., 2014). On the other hand, studies suggested that victims’ adverse physiological or emotional reactions to naloxone, sometimes related to naloxone-induced acute withdrawal, contributed to laypersons’ hesitancy and even avoidance to use this life-saving medication and engage in overdose emergency assistance overall (Neale et al, 2019; Parkin et al., 2020).
Overdose interventions facilitated by mobile digital technologies, such as smartphone apps, represent a particularly promising area of research, especially given the importance of digital health interventions during the COVID-19 global pandemic (Mahmood, Hasan, Carras, & Labrique, 2020). Developing and testing a specialised smartphone app to respond to an overdose is an emergent area of research (Marcu Aizen, Roth, Lankenau, & Schwartz, 2019; Schwartz et al., 2020), and has shown that bystanders can initiate alerts with an app and layperson responders can subsequently deliver naloxone to an overdose event. In addition, research on app-based interventions for other medical emergencies, such as cardiac arrest or anaphylaxis, have demonstrated that laypersons connected through an emergency response app can often respond to a medical crisis faster than emergency medical services (EMS) (Caputo et al., 2017) and provide life-saving measures such as cardiopulmonary resuscitation (CPR) and defibrillation (Andelius et al., 2020). However, certain factors may affect a layperson’s decision to intervene in a medical emergency situation in the context of using an app. Those barriers include spatial characteristics, such as distance to an emergency location (Brooks et al., 2016) or the combination of an unfamiliar location plus darkness (Yablowitz, Dölle, Schwartz, & Worm, 2019), as well as behavioural factors, such as the “bystander effect” (Latané& Darley, 1970) or diffusion of responsibility (Yablowitz et al., 2019), including the belief that professional first responders will arrive at an emergency location first (Brooks, Simmons, Worthington, Bobrow, & Morrison, 2016).
Responding to an overdose involves several factors that impact decision-making, including time pressure, uncertainty, and high stakes situation (Neale et al., 2019; Parkin et al., 2021; Wagner et al., 2014), similar to other medical emergencies, such as cardiac arrest (Mausz, Snobelen, & Tavares, 2018). Studies have shown that in situations of stressful uncertainty, analytical reasoning is often replaced by an intuitive, simplified, and effort-saving heuristic (Kahneman, 2003; Yu, 2016) defined as “a strategy that ignores part of the information, with the goal of making decisions more quickly, frugally, and/or accurately than more complex methods” (Gigerenzer & Gaissmaier, 2011, p. 454). In other words, a heuristic approach to decision-making focuses on simple rules of information processing (Suter, Pachur, & Hertwig, 2013) that rely on effort reduction (Shah & Oppenheimer, 2008).
As heuristic decisions assume a trade-off between effort and accuracy, they have been linked to biases and suboptimal judgements and, correspondingly, opposed to rational decision-making (Kahneman 2003). Yet, under certain conditions, relying on partial information (i.e., heuristic decisions) can lead to higher predictability than applying multivariate statistical models, thus establishing the effect of a “less-is-more” (Gigerenzer & Gaissmaier, 2011). This effect holds because heuristics represent ecologically (versus logically) rational decisions adapted to the structure of the environment (Todd & Gigerenzer, 2000).
Given the gap in the understanding of patterns of decision-making among overdose lay responders, this study explored the heuristics of overdose response among persons with and without active non-medical opioid use who were equipped with an emergency response smartphone app. The study aimed to answer two questions: First, what heuristics do people employ when using a specialised smartphone app to respond to an overdose emergency? Second, are people who follow the same heuristics also similar in other ways, including their patterns of app use, prior experience with naloxone, or active opioid use?
Methods
Setting
Data for this analysis was collected in Philadelphia, Pennsylvania as part of a feasibility study which piloted UnityPhilly, a smartphone app that connects layperson first responders with people experiencing overdose (Schwartz et al. 2020). In 2018 (the latest year for which complete U.S. data are available), the rate of drug-related overdose deaths in Philadelphia was 70.0 per 100,000 residents (DEA Philadelphia Division, 2019), which is more than triple the national average rate of 20.7 per 100,000 (Hedegaard, Miniño, & Warner, 2020). The vast majority (93%) of all opioid deaths in Philadelphia in 2019 were attributed to the presence of fentanyl or fentanyl analogue (Department of Public Health, City of Philadelphia, 2020).
The study was conducted in the Kensington neighbourhood of Northeast Philadelphia. Kensington is home to a large number of people dependent on opioids and other drugs, who often lack stable housing. Kensington is also the epicentre of Philadelphia’s opioid overdose crisis. According to the Philadelphia Department of Public Health (2019), in 2019, the highest number of overdose deaths in Philadelphia occurred in the zip codes of Kensington or adjacent areas.
Naloxone is increasingly available in Kensington due to governmental responses to the ongoing opioid crisis. Between July 2017 and April 2020, the city of Philadelphia distributed nearly 150 thousand doses of naloxone to law enforcement agencies and community-based organisations (Department of Public Health, city of Philadelphia, 2020), including Prevention Point Philadelphia (PPP), the city’s largest harm reduction organisation which is located in Kensington.
UnityPhilly app
UnityPhilly is a smartphone app that facilitates overdose emergency response among lay first responders based upon the Emergency Response Community (ERC) concept (Marcu et al., 2019; Schwartz, Bellou, Garcia-Castrillo, Muraro, & Papadopoulos, 2016). The app was proposed in 2018 by the study team that included researchers from Drexel University (Philadelphia, PA) and Bar-Ilan University (Ramat-Gan, Israel) and developed in collaboration with Verint/NowForce, which also helped customize and support the app. The study team piloted the app in Philadelphia between March 2019 and February 2020 (Schwartz et al. 2020). The app can be used to signal an overdose SOS alert by a person witnessing an overdose. The alert triggers an SOS push notification on the phones of other UnityPhilly app users who are within a 15-minute estimated-time-of-arrival from the location. Alerted individuals can then use the app to indicate that they are either on their way to assist with the overdose, or they are declining to respond to this incident, or provide no response. Irrespective of laypersons’ response, a semi-automated phone call to Philadelphia 9–1-1 dispatch is initiated after pressing the SOS button, and the app user is connected to a live emergency services dispatcher. The app includes other features, such as navigation to the overdose incident, and options for communicating with the signaller, including a “Push-To-Talk” button for a walkie-talkie type of communication. Detailed information about UnityPhilly can be found in a prior publication from the larger study (Schwartz et al., 2020).
The larger study
From October 2018 to January 2020, 112 people were recruited into an observational cohort to examine use of the UnityPhilly app to respond to opioid overdoses. Participants were recruited from different parts of Kensington, including the PPP main office, PPP shelter, PPP-operated suboxone treatment bus, and from adjacent areas, using both targeted and chain referral sampling. Inclusion criteria included: the possession of an Android or iPhone smartphone with a data plan; the agreement to install UnityPhilly and have the app track the participants’ locations; the agreement to carry naloxone; as well as living, working, or spending a significant portion of time in one of four Kensington zip codes. Participants were screened in recruitment locations or by phone, and if all four criteria were satisfied, invited to undergo baseline procedures in the study’s Kensington office. The baseline procedures involved: written consent, registration of demographic and contact information, completing a baseline survey, and undertaking UnityPhilly app training and overdose prevention training. The baseline survey collected sociodemographic, drug use, overdose, and naloxone use characteristics. At the end of the baseline procedures, each participant received an overdose prevention kit, including two spray devices, each containing 4 mg of intranasal naloxone.
For data tracking purposes, enrolled participants were categorized into two groups: “people who use opioids” (PWUO) if they used opioids non-medically, including illicit or prescription opioids, at least once in the past 30 days prior to baseline and “people reporting no opioid misuse” (“non-users”) at baseline. Overall, the larger study enrolled 57 people who use opioids and 55 people reporting no opioid misuse.
During 12 months of the observation period, from March 1, 2019 to February 29, 2020, two types of short surveys were sent by text and email. Regular monthly surveys were sent to all participants of the larger study to monitor changes in drug use and capture recent personal and witnessed overdose experiences. Follow-up surveys were sent to participants who signalled or responded to app-initiated overdose alerts to clarify details about incidents. App activity data, including SOS alerts and on-scene arrivals, were recorded and stored on the system server. The participants were compensated in cash, totalling $25 for baseline procedures and $5 for each short survey completed.
The study protocol was approved by Drexel University Institutional Review Board and registered with ClinicalTrials.gov (NCT03305497).
The present study
a). Sampling and data collection
The present study is based on one-time qualitative interviews with a subsample of the larger study at the end of the observation period. Utilizing maximum variation sampling (Palinkas et al., 2015), 20 people were selected from the total sample of 112 participants to capture the diversity of app-facilitated overdose response by people with different gender identity, baseline opioid use status, and app use activity level. Qualitative participants were initially contacted via a phone call, text message or in-person when they visited the research office in Kensington.
Interviews were conducted between the end of January 2020 and mid-March 2020 by the research team consisting of the first author and four research assistants. Eighteen interviews took place in the research office in Kensington and the last two interviews were held by phone since the end of the qualitative part of the study coincided with the start of the COVID-19 epidemic. Interviews ranged in length from 17 to 55 minutes. The interview guide was developed to elicit participants’ detailed perspectives on use of the app and based upon our prior qualitative work in the areas of opioid overdose and mobile health technologies (Ataiants et al., 2020; Marcu et al., 2019). The following domains were included in the interview guide: motivation for participation in the study; feedback on UnityPhilly training and overdose prevention training; experience of using the app as a signaller and SOS responder; reasons for not using the app; overall feedback on the app and its specific features; and recommendations for future use of the app. Participants were compensated $25 in cash for participating in a qualitative interview.
b). Analysis
This analysis utilized quantitative and qualitative data from three sources: interview transcripts, baseline survey, and app activity data. In-depth qualitative interviews were used to identify heuristics, while baseline and app use data were used to compare heuristic groups.
Qualitative interviews were recorded on a digital recorder, uploaded as digital files, and transcribed by a transcription agency. Transcripts were uploaded into Dedoose, version 8.3.35 (2020), a web application for qualitative and mixed-methods research. Qualitative analysis involved three steps. First, all interviews were coded deductively by the first author. The list of codes replicated the overarching domains in the qualitative interview guide, including motivations for participation in the study, feedback on UnityPhilly training, the experience of signalling or addressing UnityPhilly alerts, etc. An “App use heuristics” code was added to the predefined list of codes since the theme of decision-making for UnityPhilly use emerged during the early stage of conducting qualitative interviews. Following deductive coding, interview excerpts under the “App use heuristics” code were exported into a Word document and divided into two types of decision-making: by signallers and responders. The next step was to identify heuristics, assign them initial names, and use heuristics to categorize interviewee decision-making behaviours. Three co-authors working on the shared version of the Word document engaged in this step, focusing on common motivations for signalling or addressing app alerts. Decision-making processes were examined as well, such as whether participants relied on past experiences versus situational cues, or whether decisions were reached based on one good reason versus considering several relevant cues. This procedure included further reading of the excerpts and the entire transcripts in some cases. Finally, heuristics’ names and participant assignments to categories were further refined, and any outstanding analytical disagreements were discussed and resolved collaboratively, initially, by the three co-authors and then, by all co-authors.
Of the 20 participants recruited into the qualitative sample, two were not assigned to any heuristics and were excluded from the analysis. One participant spent a significant amount of time outside of the geographical parameters of Kensington during the study and therefore, had few opportunities to respond to or decline app signals. The other participant did not reveal any decision-making for addressing app alerts during the interview, which may have been linked to the fact that her use of the app was constrained by daytime employment responsibilities. As a result, 18 participants were included in the analytical sample for this report.
To understand whether each heuristic group was homogeneous on demographics, overdose history, and app use levels, quantitative data from the baseline survey and app use activity log were stratified by heuristic groups using IBM SPSS Statistics version 25. Percentages were calculated for categorical variables: opioid use status at baseline, gender identity, history of personal overdose (categorized into “never”, 1–2, and >2 lifetime opioid overdoses), and history of witnessed overdose (categorized into “never”, 1–20, and >20 lifetime witnessed opioid overdoses). Medians and interquartile ranges (IQR) were computed for count variables, including frequency of giving naloxone at baseline, as well as frequency of SOS signals and arriving to an overdose scene during the observation period.
Results
Baseline demographics, lifetime overdose, and UnityPhilly use profiles
The sample included 10 women and 8 men. The average age was 42.4 years, ranging from 30 to 55 years of age. The majority (61% or 11 people) were Non-Hispanic White, 4 persons (22%) identified as Hispanic/Latino of any racial group, and 3 persons (17%) identified as non-Hispanic Black. At baseline, 10 participants reported no opioid misuse and 8 people used opioids non-medically within past 30 days. Compared to the total sample (see Schwartz et al., 2020), the present sample was, on average, 3 years older and had a higher proportion of women (56% vs. 51%), people reporting no opioid misuse (56% vs. 49%), and non-White people (39% vs. 26%). Among people who used opioids, only one out of eight interviewees (13%) was a racial minority (Hispanic of mixed race) compared to 15 of 57 (26%) participants in the total sample.
Half of the qualitative sample (n=9) experienced a lifetime opioid overdose, including all people who used opioids and one person who reported no opioid misuse. Overall, only 2 people (11%), both of them reporting no opioid misuse, never witnessed an overdose prior to entry into the study. One-third of the sample witnessed more than 20 opioid overdoses in their lifetime. The majority of participants (13 of 18) reported that they carried naloxone all of the time or most of the time.
The number of app alerts sent ranged from 0 to 30, with the median of 3. The frequency of on-scene arrivals, including those who never received an alert, ranged from 0 to 11, with the median of 1. Selected participant baseline and app use characteristics stratified by heuristics are presented in Table 1.
Table 1.
Participant characteristics by heuristics of UnityPhilly use
| Characteristic | Total (N=18) | Signaling | Responding | |||||
|---|---|---|---|---|---|---|---|---|
| Unconditional: Always call for help or backup (n=7) | Conditional: Rescue, but only signal if necessary (n=9) | Conditional: Assess if I can make a difference (n=11) | ||||||
| N | % | n | % | n | % | n | % | |
| Gender | ||||||||
| Women | 10 | 55.6 | 4 | 57.1 | 5 | 55.6 | 4 | 36.4 |
| Men | 8 | 44.4 | 3 | 42.9 | 4 | 44.4 | 7 | 63.6 |
| Opioid use status at baseline: | ||||||||
| People who use opioids | 8 | 44.4 | 4 | 57.1 | 4 | 44.4 | 6 | 54.5 |
| People reporting no opioid misuse | 10 | 55.6 | 3 | 42.9 | 5 | 55.6 | 5 | 45.5 |
| Lifetime number of personal opioid overdoses at baseline | ||||||||
| 0 | 9 | 50.0 | 3 | 42.9 | 5 | 55.6 | 5 | 45.5 |
| 1–2 | 3 | 16.7 | 2 | 28.6 | 0 | 0 | 3 | 27.3 |
| >2 | 6 | 33.3 | 2 | 28.6 | 4 | 44.4 | 3 | 27.3 |
| Lifetime number of witnessed opioid overdoses at baseline | ||||||||
| 0 | 2 | 11.1 | 2 | 28.6 | 0 | 0 | 1 | 9.0 |
| 1–20 | 10 | 55.6 | 4 | 57.1 | 5 | 55.6 | 5 | 45.5 |
| >20 | 6 | 33.3 | 1 | 14.3 | 4 | 44.4 | 5 | 45.5 |
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | |
| Frequency of giving naloxone at baseline | 6.50 | 2.25 – 41.75 | 4.0 | 0–7.0 | 20.0 | 4.0–55.0 | 8.0 | 0–50.0 |
| App use activity: | ||||||||
| Frequency of SOS signals | 3.0 | 0–8.50 | 10.0 | 7.0–26.0 | 2.0 | 0–3.0 | 3.0 | 0–10.0 |
| Frequency of on-scene arrivals | 1.0 | 0–3.0 | 2.0 | 0–3.0 | 0 | 0–5.50 | 1.0 | 0–3.0 |
Notes:
IQR=interquartile range;
Across rows, numbers reported for heuristic groups do not add up to numbers reported for the total sample as the heuristic groups are not mutually exclusive.
Across columns, percentages may not add up to 100 due to rounding.
Heuristics of UnityPhilly use
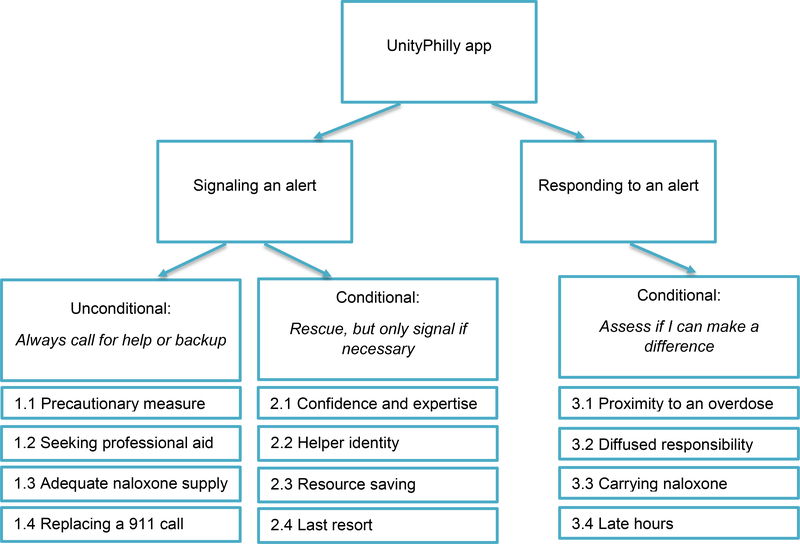
Three prevailing, not mutually exclusive, heuristics for UnityPhilly use emerged across the 18 participants: unconditional signalling (“Always signal for help or backup”); conditional signalling (“Rescue, but only signal if necessary”); and conditional responding (“Assess if I can make a difference”). Half of the sample (n=9) applied one heuristic and the other half used two heuristics, one for signalling and one for responding. A number of different motivators or justifications were given by interviewees for the use of each heuristic, summarized in Figure 1.
Figure 1.
Heuristics and sub-motivations among UnityPhilly participants
1). Heuristic of unconditional signalling: Always signal for help or backup
Did I signal it when I had Narcan on me? Yeah. Absolutely. Why wouldn’t I? Just to do it. (Male, 35 y.o., PWUO)
Seeking professional help in case of a suspected overdose, regardless of carrying naloxone, is a standard recommendation of any overdose prevention training and the American Heart Association (Naumar et al., 2016). Seven participants, including four women and three men, explicitly applied the heuristic of unconditional signalling - to “always signal for help or backup”. Signallers included four people who used opioids, all of whom had experienced at least one personal overdose and administered naloxone at least 4 times at baseline, and three people reporting no opioid misuse who had never overdosed or administered naloxone by the start of the study. This group had the highest median of alerts (10) and on-scene arrivals (2) among three heuristic groups (see Table 1).
Signallers commonly described carrying naloxone on a frequent basis and most of them administered naloxone at the last witnessed overdose. Yet, because of acute stress caused by an emergency, especially when witnessing overdoses of people in their close social network, participants signalled with the app as a precautionary measure to increase a victim’s chances of survival.
I used the app to call the ambulance. And they came, and … […]. If I remember right, he went with the ambulance. So, I administered a Narcan nasal, and the ambulance came, and he revived, he came around, and they took him to the hospital. (Female, 30 y.o., PWUO)
[Interviewer] You hit her with the Narcan, and you still used the app to call? [Respondent] Yeah.[…] Because that she […] turned blue. She turned -- She was completely done. (Female, 33 y.o., PWUO).
Sentiments expressed by several signallers specifically invoked the concept of professional medical help - “you still want medical attention” - that was valued higher than laypersons’ assistance. One person argued that sending an alert to contact Emergency Medical Services, which the UnityPhilly app automatically placed, was crucial to address a potential return of an opioid overdose that may occur after the effects of naloxone wear off.
Yeah, just in case, sure I would [signal SOS]. I’m not no doctor or nothing. […] I’ll give it [naloxone] to them, and you know what I mean? He’ll start coming around - I’m still calling somebody because you never know. Cause when you mess around with that dope and whatever, you can still [overdose] after you come up out of it, you know what I mean? So, you know, I just called somebody or let somebody else know. (Male, 55 y.o., non-user)
In some instances, the app was utilized as a resource for getting additional naloxone rather than peer-based or professional support; that line of thinking was propelled by fear that possessing an insufficient quantity of naloxone would not result in a successful reversal:
Who knows if I needed another … another hit of it [naloxone].[…] Because usually a lot of them [overdose victims] need two [doses]. You know? [...] A lot of them need two, and the nasals [intranasal naloxone] is only good for one (Male, 35 y.o., PWUO).
Two participants who used opioids at baseline reflected on how signalling app alerts had become a new overdose emergency response. One of them revealed that soon after joining the project, she witnessed an overdose of her friend and would have forgotten about the app had another friend not reminded her. While she was under tremendous stress, she did not recall that the app generated an EMS call, so she dialled 911 immediately after sending an app alert to ensure some professional help was underway. Gradually, however, signalling the app has become a new routine:
When somebody’s overdosing, you like panic. You know? And I know that like more recently, like it’s in my forefront to call, like to hit that app. (Female, 35 y.o., PWUO).
The other respondent who indicated that signalling an app alert had become an ingrained response reported that after her mother fatally overdosed two years ago, she instituted a number of safety measures around her own drug use. Those included always carrying naloxone, not using drugs alone or outside, and not using drugs simultaneously with her partner who frequently overdosed. Using the app to signal an overdose was added to this list as a replacement for a 911 call.
Additionally, two people who reported no opioid misuse described instances when they signalled with the app because they were unable to physically approach an overdose victim. One saw a victim from the window of her home, but could not leave because she was babysitting her grandchildren. The other worked in a Kensington-based store and was frequently informed about nearby overdoses; he could not leave his workplace when he had customers, but sent app alerts. In essence, they used the app to report an overdose event the same way they would have called 911.
Overall, ensuring a victim’s survival was a driving force behind the heuristic of unconditional signalling even while possessing naloxone. Signallers still administered naloxone on their own, but valued additional assistance from EMS or other app users, as well as obtaining the adequate supply of naloxone. Using UnityPhilly to signal an overdose was a supplement or substitute for making a traditional 911 call.
2). Heuristic of conditional signalling: Rescue, but only signal if necessary
The app is kind of maybe the farthest thing from my mind when I administer Narcan. (Male, 40 y.o., non-user)
Half of the participants followed a divergent heuristic of conditional signalling – to “rescue, but only signal if necessary” – so as to send an alert only when they were unable to rescue a victim on their own. Participants in this group, five women and four men, had the highest median of baseline naloxone administrations (20 times) among the three heuristic groups. The group was represented by four people with active opioid use and five people reporting no opioid misuse, four of whom worked in organisations providing services for people who use drugs. The group signalled the app a median of 2 times. The median of on-scene arrivals in this group was 0, however, among 4 participants practicing this heuristic, the number of arrivals ranged 3 to 9.
Most participants in this group believed they were “prepared” to respond to an overdose on their own, especially when they were equipped with naloxone. Sometimes their accounts about witnessed overdoses described the stress from the urgency of saving a human life, but they did not feel that they had lost control of the emergency situation.
I usually always have Narcan on me. So, if I – if someone’s overdosing, I’m already there, so there’s no real reason to text [signal] somebody. You know what I mean? Because I have probably ten boxes of Narcan, so, I mean, every time – a lot of times they put it right in with my [suboxone] prescription so I don’t even realise, and when I pick it up it’s already in the bag. So, I have so much of it, and I have a bunch in my pocketbook. So, I’m always prepared. (Female, 48 y.o., PWUO)
Moreover, some participants in this group felt they were equally as competent as medical professionals in addressing overdoses and complained that EMS did not fully appreciate their rescuing abilities:
Occasionally I would come across other [UnityPhilly] responders on the scene. So that was pretty interesting. And it was interesting to see that it wasn’t EMS. Because it’s a different vibe when EMS is on the scene. It’s just like, it becomes a territorial thing with EMS, like “Oh, I’ve got this, I’m a professional,” when we’re all professionals. (Female, 41 y.o., non-user)
Importantly, some participants in this group who had aided in overdose emergencies for many years assumed the identity of a “helper” (e.g., responder) and contrasted it with a signaller for help. Those participants reflected on their past experience of not calling 911 in an attempt to save time – the most valuable resource in overdose emergency situations:
I’ve been doing it for years and calling somebody for help is not in my thought. My thought is to help the person who’s overdosing. Give them rescue breaths. If anybody is around, I tell them to call 911 for me. I’m not concerned about my phone at all, and if I call 911 myself and they want you to stay on the line, I say “yeah, yeah” and stick it in my pocket. I don’t hang up on them, but I don’t have no time for them. I’m worried about the person. (Female, 54 y.o., non-user)
In addition to saving time, saving public resources was another motivation involved in practicing the heuristic of conditional responding. A very experienced overdose rescuer framed her reluctance to signal with the app as a gain for the community, because such a behaviour reduces the volume of unnecessary 911 calls.
If I have it [naloxone], it would be a waste of manpower to do it, because now you’re tying up an already overwhelmed community by, you know, whether overdoses or gunshots or violence and all that stuff, that EMS already responds to. (Female, 41 y.o., non-user)
Yet, several participants in this group talked about the occasional experience of signalling alerts to request help as a last resort. For example, one participant noticed an overdose incident from the window of his car. Since he did not have time to stay, he briefly stopped to give naloxone to the victim and then signalled an alert to summon UnityPhilly and EMS responders before leaving the scene. Another participant described two cases when he signalled with the app; in one case, he sent an alert after he exhausted other measures, such as administering naloxone and CPR, to revive an overdose victim. In the other case, he encountered a person who had already died of an overdose, so the participant used the app to request an ambulance to pick up the body.
Overall, participants in this group evinced a confident “helping” identity that in many cases stemmed from skills and prior experience administering naloxone and successfully responding to overdose situations. Signalling the app to request help was largely perceived as a practice reserved for inexperienced overdose rescuers or utilized as a last resort when the other viable strategies were exhausted.
3). Heuristic of conditional response: Assess if I can make a difference
As long as I’m not in the middle of doing something, and it’s close by, I’m going to respond. You know what I mean? Especially when I have Narcan, there’s no reason not to. (Female, 30 y.o., PWUO)
While the first two heuristics focused on signalling alerts, a third decision-making heuristic was used to decide when to respond to an overdose alert. Eleven participants, seven men and four women, applied a heuristic of conditioned response – to “assess if I can make a difference.” The group included 6 people who use opioids and 5 reporting no opioid misuse, and together they administered naloxone the median of 8 times by baseline (Table 1). Among 11 participants in this group, 4 people were also part of the conditional signalling heuristic (“Always signal for help or backup”) and 5 people were assigned to the unconditional signalling heuristic (“Rescue, but only signal if necessary”).
Participants identified proximity to the overdose location as an important determinant of their decision to respond to an app-generated alert. Since the study recruited people familiar with the Kensington area, a majority of the participants were able to determine a distance to an overdose location even without a map (“As soon as I see the address, I know where it is”).
Participants shared their understanding of a reasonable distance as not exceeding a mile or several blocks. One participant talked about how he received an alert in the middle of the night when buses run once per hour and decided against responding as it would have taken him 30 minutes to walk to an overdose scene. Another participant reflected on his inability to address distant alerts as a disappointing experience:
Because I want to help, but sometimes they’re [overdose incidents] just too far. [...]It didn’t bother me, but, yeah, it would’ve been nice, because when you hear the notification, and you look and you see there’s no way, it’s kind of makes you feel a little bit bad. Because I’ve had the app for a year, and probably 75 percent of them [alerts] were too far away. (Male, 44 y.o., non-user)
A number of participants explained their resistance to walking a long distance to an overdose site by the high likelihood of a faster response from emergency services or other bystanders. Non-response to app alerts was framed as saving time rather than disregard for a human life or avoiding physical distress from prolonged walking.
You get a call or a message like six blocks down the street, that something is happening… I think, you know, any, even the best-intentioned person is probably going to, you know, say, “Hey, at six blocks, by the time I get there, something should have already been done…I’m hoping someone else is going to respond,” you know?. (Male, 40 y.o., non-user)
Notably, the belief that any overdose that did not happen in close range would be handled by others was based on the perception of Kensington as a community saturated with naloxone (“usually there’s always somebody that has Narcan”). One participant supported this argument by reporting that naloxone is no longer sold in the underground economy.
I know like before people used to sell it, but now it’s in such abundance that like nobody buys it. […] Seriously. Because they used to sell them for like five apiece, and now like everybody has it, so nobody buys it. (Female, 35 y.o., PWUO)
Participants also talked about the preponderance of overdoses happening on the streets in the Kensington neighbourhood, meaning that overdose victims were visible and therefore, most likely provided timely assistance.
I haven’t heard of somebody dying from an overdose out here – I mean, I hope I’m not wrong – in a while. Because everybody’s got Narcan, everybody’s trained and know what to do. You don’t really see people dying from overdoses anymore, unless it’s like they’re doing it inside where they can’t be reached, or nobody knows. (Male, 35 y.o., PWUO)
Participants also described how the presence of other bystanders at an overdose site sometimes altered their decision to respond to an alert. In one case, a participant was so close to the incident that when he received an SOS signal, he was able to observe other bystanders already helping the victim and decided not to go. Another participant said that she was using the push-to-talk feature to communicate with a signaller, and as soon as she learned that an ambulance had arrived on scene, she turned around.
Possessing naloxone was another factor influencing the decision to respond to an app alert. Interestingly, the same participants who followed the heuristic of unconditional signalling (i.e., “always signal”) had reservations about unconditionally responding to alerts. One participant had difficulty recalling the details of the most recent responded overdose, but indicated that naloxone and proximity to an overdose scene could be two decisive factors:
I can’t remember if I had to give that person more Narcan because they didn’t have enough. That’s probably what it was, though. I probably had Narcan on me, and that’s probably why I went over there. Because most likely I was down around this area. That’s probably why I responded to it. (Female, 30 y.o., PWUO)
Responding to an overdose at night was described as a concern by two participants, both of whom were women. Notably, their family members (son and sister, respectively) were also enrolled in the study and they jointly responded to some late-night overdose alerts together. Otherwise, an alert received during evening hours was deemed as too risky to respond:
There were a lot of times that I did get a few [alerts], but they were all at night […]. It’s two stops down and nine minutes from my house to the El [the elevated subway line in Kensington]. So, I would have to walk nine minutes, get on the El and then come down here. And I mean I would have done it if I had my son with me or something. But most of the times he’s already out here […]. If it was in the daytime, I don’t mind. I – like I’m walking, I’m there, but like at nighttime I just… And it does eat me up inside because I want to be able to respond, you know, like you want to be able to help. (Female, 49 y.o., PWUO)
In sum, participants in this group discussed how their decisions about addressing app-generated overdose alerts were guided by their perceived ability to make a difference - constrained by one or more factors, such as distance, the presence of other bystanders, possession of naloxone, and responding during the late hours. The decisions were grounded in the larger context of the Kensington neighbourhood as an environment with the high concentration of trained overdose rescuers. Therefore, non-response to alerts was often framed as inability to make a meaningful contribution to an overdose rescue or concerns around personal safety, rather than inaction potentially leading to a loss of human life.
Other factors contributing to app use or non-use
In addition to heuristics outlining different approaches to signalling or responding using the UnityPhilly app, participants also described factors that objectively limited their ability to signal or respond. For instance, employed persons frequently reflected on their inability to leave a work post to address alerts. Two women reported that they never understood the technical aspects of how to respond to an overdose signal on the app. Some participants also complained about the poor quality of their phones as a barrier to proper response.
Additionally, interviews demonstrated that not using the app for all or most of overdoses encountered did not indicate a broader reluctance to respond to overdoses outside the study. Participants who professionally worked with people who used drugs stated that they were overwhelmed with daily overdose rescues at their workplace and therefore often did not have an opportunity to address app-related emergencies. In some cases, SOS signals were addressed without the app. For example, in one case, a participant simply walked to the incident that she could see across the street. In another case, a participant recognized a place from the address sent by the app and decided to walk to the emergency site without indicating she was on her way to help. Some participants never responded to app-generated signals, but reversed overdoses encountered on the streets during the study period. Finally, some participants responded with and without the app:
…And not just through the app. I actually live at [busy intersection in Kensington] – and it’s right there. I’ve saved people’s lives every morning practically, every morning for two weeks straight in a row. Every time I’m coming out to get in my car to go, there was somebody there that I had to administer Narcan. People in my building. You know what I mean? And it feels good. You know? Because I watch people just walk on by them like they don’t even exist, and that’s somebody’s daughter, mother, sister, aunt. Whatever. It’s a human. I can’t just do that. (Female, 48 y.o., non-user)
Discussion
This is the first study that identified heuristic decision-making in overdose emergency situations among people equipped with an overdose smartphone app. The study revealed three prevailing heuristics for overdose app use: unconditional signalling (“Always signal for help or backup”), conditional signalling (“Rescue, but only signal if necessary”), and conditional responding (“Assess if I can make a difference”). The study also suggests that among other factors, self-efficacy with naloxone administration and a helper identity may contribute to the use of certain heuristics and that different combinations of heuristics may explain app use profiles. The results indicate that success of overdose prevention interventions assisted by digital technologies may depend on the involvement of people with diverse overdose rescue backgrounds.
We identified two prevailing heuristics of requesting help via the app. The heuristic of unconditional signalling (“Always signal for help or backup”) was utilized by a group that included a mix of naïve naloxone users, as well as people who used opioids and had some prior naloxone use experience. While naïve naloxone users might be expected to signal “just in case,” unconditional signalling by some participants with active opioid use was surprising. This is contrary to not only previous research documenting that avoiding contact with the police has been a major deterrent to overdose-related 911 calls in this group (Koester 2017; Latimore & Bergstein 2017; Wagner, 2019), but also our formative research indicating that people who use drugs preferred to avoid interactions with authorities while responding to an overdose via the app (Marcu et al., 2019). Perhaps, participants in the study were aware that they had installed an app that tracked their location and may have been less concerned about police than people not enrolled in the study. Alternatively, participants utilizing the heuristic of unconditional signalling could be particularly sensitised to the seriousness of overdose, given rapid progression of overdoses involving fentanyl (Somerville et al., 2017), the major contributor to drug deaths in Philadelphia. Additionally, as risk environments for people who use drugs are racialized (Collins, Boyd, Cooper, & McNeil, 2019; Cooper et al., 2016; Friedman et al., 2021), it is also plausible that punitive policing as a deterrent for app use did not surface as a theme due to few racial minority participants and the absence of Black people among interviewees who use opioids.
In contrast, participants who employed the heuristic of conditional signalling (“Rescue, but only signal if necessary”) were confident in their ability to address an overdose and generally bypassed signalling to save time for actual rescue. This group, which was comprised of participants with substantial prior experience of naloxone use, emphasized their expertise and desire to act as helpers – essentially already having transitioned to the role of rescuer among trained lay responders, which has been previously described (Bathje et al., 2019; Wagner et al, 2014). Importantly, people who utilized any signalling heuristic (unconditional or conditional) acted as “responders” when administering naloxone to overdose victims. Yet, they differed on self-efficacy to manage an overdose, which was illustrated by opposing sub-motivations when comparing the two groups: using the app as a precautionary measure versus confidence and expertise, or seeking professional help versus assuming the helper’s identity. More research is needed to understand whether high self-efficacy for overdose management among “helpers” creates overconfidence sometimes leading to unexpected adverse outcomes.
Whereas using the app to signal overdose alerts added another tool for lay overdose responders, responding to alerts via the app created a new reality in which participants were prompted to address overdoses they did not originally encounter in person. Due to distance to an overdose scene or lack of visibility of an overdose, participants who received app signals may not have felt the same time and social pressure had they encountered an overdose in person. As a result, a subgroup of participants developed a utilitarian heuristic of conditional response to app alerts (“Assess if I can make a difference”). Of note, while signalling-related heuristics were grounded in past overdose rescue experiences, the heuristic for alert responding was determined by situational cues and participants’ perception of the local overdose scene as a neighbourhood with a high concentration of bystanders carrying naloxone (i.e., ecologically rational decision-making). In this respect, an app alert had the best chances for a response when it was not too late, the participant was nearby, equipped with naloxone, not occupied with work or other tasks, and generally confident that no other respondents were on site. In a similar vein, Brooks and colleagues (2016) found that non-response to a cardiac arrest response app was related to a number of reasons, including remoteness of an emergency location (31%), and belief that professional responders will arrive first (12%). Likewise, Yablowitz et al. (2019) reported that allergy response app users had lower willingness to respond to alerts that were marked by the interaction of an unfamiliar place and night time.
The finding that actual or perceived presence of other lay or professional first responders discouraged app users from showing up at an overdose scene improves our understanding of bystander intervention. Our formative research revealed perceived drawbacks of encountering other lay responders, such as loss of control or agreement about how to handle the situation (Marcu et al., 2019). This finding potentially manifests a new variation of a bystander effect in an app-mediated overdose response environment, a phenomenon also noted in other studies of app-assisted bystander interventions (Brooks et al., 2016; Yablowitz et al., 2019). Interestingly, the bystander effect among overdose witnesses is under-researched, and only one study reported that the presence of four or more bystanders significantly decreased the likelihood of calling 911 among overdose witnesses with current or past drug use (Tobin et al., 2005).
Contrary to our expectations, participants did not report concerns about the app tracking their location and potentially sharing that data with law enforcement. On one hand, agreeing to uploading an app that included location tracking was a study inclusion criterion. On the other hand, our formative research revealed that Kensington residents were more concerned with others potentially misusing information revealed by the app (e.g., location of overdose victims who could then be robbed) than excessive control by law enforcement (Marcu et al., 2019). Additional research is warranted to evaluate privacy and safety of app users, especially structurally vulnerable participants, such as people who use drugs.
The study has important implications for future app-mediated overdose prevention interventions. It revealed that app users tended to employ the opposing heuristics for signalling and responding (e.g., either conditional or unconditional) and therefore “specialised” in either signalling or responding. Such a dynamic represents an apparent variant of a two-sided market, when two sets of agents (signallers and responders) interact using an intermediary (UnityPhilly app) and create an “outcome” (i.e., overdose reversal) for the other type of agents (overdose victims) (Rysman, 2009). Hence, overdose prevention interventions facilitated by emergency response apps need to target people with diverse drug use and overdose rescue backgrounds to assure adequate representations of those who are willing to signal and respond. Additionally, future interventions should be developed by testing perceived benefits and drawbacks of app use among different sub-groups. For example, to increase the participants’ sensitisation to app alerts, an estimated-time-of-arrival radius should be adjusted to the common perception of a reasonable distance to an emergency location. Even if tightening the radius will decrease the number of potential app responders, such a measure may alleviate the “bystander effect” when fewer available participants will feel greater pressure and responsibility to show up. The study also highlighted the continuing need to scale-up community distribution of naloxone since experience with and confidence in the antidote played an important role in each heuristic. In addition, while women’s gender did not seem to have an impact on unconditional or conditional signalling, a lower percentage of women than men utilized the heuristic of conditional responding. Future research is needed to elucidate whether women may have fewer concerns than men while responding to app-initiated overdose alerts.
Our study also underscored potential problems related to the uptake of smartphone-based interventions in low-resource communities. Findings revealed that not only heuristics, but also a digital divide, including the complexity of app navigation or poor access to quality smartphones, affected app utilization. Moreover, while this study recruited people who owned smartphones and agreed to maintain data plan, prior research indicated that only a fraction of vulnerable populations, including people who use drugs (Tsang, Papamihali, Crabtree, & Buxton, 2019) or people without stable housing (McInnes, Li, & Hogan, 2013) have access to smartphones or the Internet. While distribution of smartphones may be a desirable, but yet currently unfeasible task, this study highlighted the need for a refresher training and easy-to-use app interface to increase app uptake across communities with low digital capital. At the same time, it is important to distinguish between non-use of the app and unwillingness to help in overdose emergency situations. Our data demonstrate that some participants engaged in overdose rescues without app use, for reasons including not only technology malfunctioning, but also the lack of resources to respond to app alerts, or preference for habitual (non-app) responses to an overdose.
The results should be interpreted in light of several limitations. Our qualitative sample was modest in size. While participants were relatively diverse in terms of gender (women/men), active opioid use, and prior naloxone use experience, people of colour were underrepresented compared to the larger study sample, as well as the neighbourhood where the study was conducted. While we achieved thematic saturation in key research questions, we recognize that additional research is needed to understand, for example, how racialized experiences, such as discriminatory policing practices, may contribute to decisions concerning app use. Such experiences should be addressed in the design of future studies. Further, the results may not be extrapolated to other settings due to specific characteristics of the Kensington neighbourhood, such as the predominance of outdoor-based overdoses, a high concentration of bystanders carrying naloxone, as well as a high proportion of participants with unstable access to smartphones. We believe that these characteristics could contribute to the “conditional” types of heuristics and that our results may not translate to settings with more discreet drug use where a higher proportion of app users may signal or respond to overdose alerts unconditionally. In addition, the interview guide did not specifically ask about decision-making during signalling or receiving alerts that could have brought richer detail about heuristics. Finally, recall bias and social desirability bias could influence the interviewees’ responses. Still, qualitative data were checked against digital records and discrepancies were addressed at the analysis stage and in the interviews themselves.
In conclusion, this study identified patterns of quick and intuitive decision-making in the form of heuristics, and surrounding sub-motivations in an app-assisted overdose prevention intervention. Findings indicated that the use of specific heuristics was influenced by prior naloxone use experience and situational factors rather than active opioid use since all three heuristics included both people who use opioids and people reporting no opioid misuse. Further research is needed to examine whether the same set of heuristics (unconditional and conditional signalling and conditional responding) can be extended to other settings and groups, including areas with the lower prevalence of outdoor-based overdoses, lower access to naloxone, among people more stable access to smartphones, as well as people with negative encounters with police. Overall, the study demonstrates that recognizing patterns of decision-making among lay overdose responders may help design more nuanced and potentially more effective overdose prevention interventions assisted by mobile technologies.
Acknowledgements
The authors would like to thank the participants for sharing their overdose rescue experiences. The authors would also like to acknowledge the contributions of Michael Khalemsky, Catalina Correa, Rebecca Hosey, Breanne Baez, Caleb Kindle-Parrish, Mariah Menanno, Sarah Miller, Chloe Bernardin, and Joseph Giordano.
Funding
This work was supported by the National Institute on Drug Abuse of the National Institutes of Health (grant number 5R34DA044758). The content is solely the responsibility of the authors and does not reflect the official views of the National Institutes of Health.
Footnotes
Conflict of interest
All authors [Ataiants, Reed, Schwartz, Roth, Marcu, Lankenau] declare no conflicts of interest.
Ethical approval
The study was approved by Drexel University IRB (protocol 1705005398) and registered with ClinicalTrials.gov (NCT03305497).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ahmad FB, Rossen LM, Sutton P. Provisional drug overdose death counts. National Center for Health Statistics. 2020. https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm [Google Scholar]
- Andelius L, Hansen CM, Lippert FK, Karlsson L, Torp-Pedersen C, Ersbøll AK, … & Folke F (2020). Smartphone activation of citizen responders to facilitate defibrillation in out-ofhospital cardiac arrest. Journal of the American College of Cardiology, 76(1), 43–53. [DOI] [PubMed] [Google Scholar]
- Ataiants J, Mazzella S, Roth AM, Sell RL, Robinson LF, & Lankenau SE (2020). Overdose response among trained and untrained women with a history of illicit drug use: a mixed-methods examination. Drugs: Education, Prevention and Policy, 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardwell G, Fleming T, Collins AB, Boyd J, & McNeil R (2019). Addressing intersecting housing and overdose crises in Vancouver, Canada: opportunities and challenges from a tenant-led overdose response intervention in single room occupancy hotels. Journal of Urban Health, 96(1), 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bathje GJ, Pillersdorf D, Kacere L, & Bigg D (2020). Helping behaviour among people who use drugs: Altruism and mutual aid in a harm reduction program. Journal of Community & Applied Social Psychology, 30(2), 119–131. [Google Scholar]
- Bowles JM, & Lankenau SE (2019). “I Gotta Go wWith Modern Technology, So I’m Gonna Give’em the Narcan”: The Diffusion of Innovations and an Opioid Overdose Prevention Program. Qualitative Health Research, 29(3), 345–356. [DOI] [PubMed] [Google Scholar]
- Brooks SC, Simmons G, Worthington H, Bobrow BJ, & Morrison LJ (2016). The PulsePoint Respond mobile device application to crowdsource basic life support for patients with out-of-hospital cardiac arrest: challenges for optimal implementation. Resuscitation, 98, 20–26. [DOI] [PubMed] [Google Scholar]
- Bui TX, & Sebastian I (2011). Beyond rationality: information design for supporting emergent groups in emergency response. In Supporting real time decision-making (pp. 159–179). Springer, Boston, MA. [Google Scholar]
- Caputo ML, Muschietti S, Burkart R, Benvenuti C, Conte G, Regoli F, … & Auricchio A (2017). Lay persons alerted by mobile application system initiate earlier cardio-pulmonary resuscitation: A comparison with SMS-based system notification. Resuscitation, 114, 73–78. [DOI] [PubMed] [Google Scholar]
- Carroll JJ, Green TC, & Noonan RK (2018). Evidence-based strategies for preventing opioid overdose: what’s working in the United States: an introduction for public heath, law enforcement, local organizations, and others striving to serve their community. National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. http://www.cdc.gov/drugoverdose/pdf/pubs/2018-evidence-based-strategies.pdf [Google Scholar]
- Clark AK, Wilder CM, & Winstanley EL (2014). A systematic review of community opioid overdose prevention and naloxone distribution programs. Journal of Addiction Medicine, 8(3), 153–163. [DOI] [PubMed] [Google Scholar]
- Collins AB, Boyd J, Cooper HL, & McNeil R (2019). The intersectional risk environment of people who use drugs. Social Science & Medicine, 234, 112384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HL, Linton S, Kelley ME, Ross Z, Wolfe ME, Chen YT, … & National HIV Behavioral Surveillance Study Group. (2016). Racialized risk environments in a large sample of people who inject drugs in the United States. International Journal of Drug Policy, 27, 43–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DEA [Drug Enforcement Administration] Philadelphia Division (September 2019). Drug-Related Overdose Deaths in Pennsylvania, 2018. DEA Bulletin. DEA-PHL-BUL-132–19. https://www.dea.gov/sites/default/files/2019-10/PRB%20FINAL%20--%20BUL-132-19%20Drug-Related%20Overdose%20Deaths%20in%20Pennsylvania%2C%202018.pdf
- Department of Public Health, City of Philadelphia (August 2020). Opioid Misuse and Overdose Report, Philadelphia, PA, 2019. https://www.phila.gov/media/20200702105030/Substance-Abuse-Data-Report-07.01.20.pdf [Google Scholar]
- Dedoose Version 8.3.35, web application for managing, analyzing, and presenting qualitative and mixed method research data (2020). Los Angeles, CA: SocioCultural Research Consultants, LLC; www.dedoose.com [Google Scholar]
- Faulkner-Gurstein R (2017). The social logic of naloxone: peer administration, harm reduction, and the transformation of social policy. Social Science & Medicine, 180, 20–27. [DOI] [PubMed] [Google Scholar]
- Friedman J, Syvertsen JL, Bourgois P, Bui A, Beletsky L, & Pollini R (2021). Intersectional structural vulnerability to abusive policing among people who inject drugs: a mixed methods assessment in California’s Central Valley. International Journal of Drug Policy, 87, 102981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman SR, Pouget ER, Sandoval M, Jones Y, Nikolopoulos GK, & Mateu-Gelabert P (2015). Measuring altruistic and solidaristic orientations toward others among people Who inject drugs. Journal of Addictive Diseases, 34(2–3), 248–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gigerenzer G, & Gaissmaier W (2011). Heuristic decision making. Annual review of psychology, 62, 451–482. [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Miniño AM, & Warner M (2020). Drug overdose deaths in the United States, 1999–2018. NCHS Data Brief, no 356. Hyattsville, MD: National Center for Health Statistics. 2020. https://www.cdc.gov/nchs/data/databriefs/db356-h.pdf [Google Scholar]
- Jakubowski A, Kunins HV, Huxley-Reicher Z, & Siegler A (2018). Knowledge of the 911 Good Samaritan Law and 911-calling behavior of overdose witnesses. Substance Abuse, 39(2), 233–238. [DOI] [PubMed] [Google Scholar]
- Kahneman D (2003). Maps of bounded rationality: Psychology for behavioral economics. American Economic Review, 93(5), 1449–1475. [Google Scholar]
- Kahneman D, & Tversky A (1979). Prospect Theory: An Analysis of Decision under Risk. Econometrica, 47(2), 263–291. [Google Scholar]
- Koester S, Mueller SR, Raville L, Langegger S, & Binswanger IA (2017). Why are some people who have received overdose education and naloxone reticent to call Emergency Medical Services in the event of overdose?. International Journal of Drug Policy, 48, 115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambdin BH, Bluthenthal RN, Wenger LD, Wheeler E, Garner B, Lakosky P, & Kral AH (2020). Overdose Education and Naloxone Distribution Within Syringe Service Programs—United States, 2019. Morbidity and Mortality Weekly Report, 69(33), 1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Latane B, & Darley JM (1970). The unresponsive bystander: Why doesn’t he help? New York, NY: Appleton-Century-Croft. [Google Scholar]
- Latimore AD, & Bergstein RS (2017). “Caught with a body” yet protected by law? Calling 911 for opioid overdose in the context of the Good Samaritan Law. International Journal of Drug Policy, 50, 82–89. [DOI] [PubMed] [Google Scholar]
- Mahmood S, Hasan K, Carras MC, & Labrique A (2020). Global Preparedness Against COVID-19: We Must Leverage the Power of Digital Health. JMIR Public Health and Surveillance, 6(2), e18980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcu G, Aizen R, Roth AM, Lankenau S, & Schwartz DG (2019). Acceptability of smartphone applications for facilitating layperson naloxone administration during opioid overdoses. Jamia Open; published online Dec 4. DOI: 10.1093/jamiaopen/ooz068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausz J, Snobelen P, & Tavares W (2018). “Please. Don’t. Die.” A Grounded Theory Study of Bystander Cardiopulmonary Resuscitation. Circulation: Cardiovascular Quality and Outcomes, 11(2), e004035. [DOI] [PubMed] [Google Scholar]
- McInnes DK, Li AE, & Hogan TP (2013). Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons’ access to and use of information technologies. American Journal of Public Health, 103(S2), e11–e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neale J, Brown C, Campbell AN, Jones JD, Metz VE, Strang J, & Comer SD (2019). How competent are people who use opioids at responding to overdoses? Qualitative analyses of actions and decisions taken during overdose emergencies. Addiction, 114(4), 708–718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, … & Kleinman ME (2015). Part 1: executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation, 132(18_suppl_2), S315–S367. [DOI] [PubMed] [Google Scholar]
- O’Donnell J, Gladden RM, Mattson CL, Hunter CT, & Davis NL (2020). Vital Signs: Characteristics of Drug Overdose Deaths Involving Opioids and Stimulants — 24 States and the District of Columbia, January–June 2019. Morbidity and Mortality Weekly Report, 69, 1189–1197. DOI: 10.15585/mmwr.mm6935a1external icon. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health and Mental Health Services Research, 42(5), 533–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parkin S, Neale J, Brown C, Campbell AN, Castillo F, Jones JD, … & Comer SD (2020). Opioid overdose reversals using naloxone in New York City by people who use opioids: Implications for public health and overdose harm reduction approaches from a qualitative study. International Journal of Drug Policy, 79, 102751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Philadelphia Department of Public Health (May 2020). Unintentional Drug Overdose Fatalities in Philadelphia, 2019. CHART 5(4). https://www.phila.gov/media/20200511105852/CHART-v5e4.pdf [Google Scholar]
- Rysman M (2009). The economics of two-sided markets. Journal of Economic Perspectives, 23(3), 125–43. [Google Scholar]
- Schwartz DG, Ataiants J, Roth A, Marcu G, Yahav I, Cocchiaro B, Khalemsky M, & Lankenau S (2020). Layperson reversal of opioid overdose supported by smartphone alert: A prospective observational cohort study. EClinicalMedicine, 25, doi: 10.1016/j.eclinm.2020.100474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz D, Bellou A, Garcia-Castrillo L, Muraro A, & Papadopoulos N (2016). Exploring mHealth participation for emergency response communities. Australasian Journal of Information Systems, Special Section on “Participatory Health Information Systems: Theory and Applications”, Forthcoming. [Google Scholar]
- Shah AK, & Oppenheimer DM (2008). Heuristics made easy: an effort-reduction framework. Psychol. Bull. 137, 207–222. [DOI] [PubMed] [Google Scholar]
- Somerville NJ, O’Donnell J, Gladden RM, Zibbell JE, Green TC, Younkin M, … & Walley AY (2017). Characteristics of fentanyl overdose—Massachusetts, 2014–2016. MMWR. Morbidity and mortality weekly report, 66(14), 382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter R, Pachur T, & Hertwig R (2013). How does prospect theory reflect heuristics’ probability sensitivity in risky choice?. In CogSci 2013: 35th Annual Conference of the Cognitive Science Society (pp. 1408–1413). Cognitive Science Society. [Google Scholar]
- Tobin KE, Davey MA, & Latkin CA (2005). Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction, 100(3), 397–404. [DOI] [PubMed] [Google Scholar]
- Todd PM, & Gigerenzer G (2000). Précis of” Simple heuristics that make us smart”. Behavioral and brain sciences, 23(5), 727–741. [DOI] [PubMed] [Google Scholar]
- Townsend T, Blostein F, Doan T, Madson-Olson S, Galecki P, & Hutton DW (2020). Cost-effectiveness analysis of alternative naloxone distribution strategies: First responder and lay distribution in the United States. International Journal of Drug Policy, 75, 102536. [DOI] [PubMed] [Google Scholar]
- Tsang VWL, Papamihali K, Crabtree A, & Buxton JA (2019). Acceptability of technological solutions for overdose monitoring: perspectives of people who use drugs. Substance Abuse, 1–10. [DOI] [PubMed] [Google Scholar]
- Tversky A, & Kahneman D (1981). The framing of decisions and the psychology of choice. Science, 211(4481), 453–458. doi: 10.1126/science.7455683 [DOI] [PubMed] [Google Scholar]
- Wagner KD, Davidson PJ, Iverson E, Washburn R, Burke E, Kral AH, … & Lankenau SE (2014). “I felt like a superhero”: The experience of responding to drug overdose among individuals trained in overdose prevention. International Journal of Drug Policy, 25(1), 157–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner KD, Harding RW, Kelley R, Labus B, Verdugo SR, Copulsky E, … & Davidson PJ (2019). Post-overdose interventions triggered by calling 911: Centering the perspectives of people who use drugs (PWUDs). PLoS One, 14(10), e0223823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, … & Ozonoff A (2013). Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ, 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yablowitz MG, Dölle S, Schwartz DG, & Worm M (2019). Proximity-Based Emergency Response Communities for Patients With Allergies Who Are at Risk of Anaphylaxis: Clustering Analysis and Scenario-Based Survey Study. JMIR mHealth and uHealth, 7(8), e13414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu R (2016). Stress potentiates decision biases: A stress induced deliberation-to-intuition (SIDI) model. Neurobiology of Stress, 3, 83–95. [DOI] [PMC free article] [PubMed] [Google Scholar]