Abstract
To determine the outcome and differences between arthroscopic hip surgery and conservative therapy in patients suffering from femoroacetabular impingement syndrome, we searched articles from PubMed, Embase, Cochrane, Web of Science and Clinicaltrials.gov using a Boolean search algorithm. Only randomized controlled trials comparing arthroscopic hip surgery and conservative therapy were included in this meta‐analysis of femoroacetabular impingement syndrome management. Two authors determined eligibility, extracted the needed data and assessed the risk of bias of eligible studies independently. Then we meta‐analyzed three articles to assess pooled estimate size (ES) and 95% confidence interval for Hip Outcome Score of activities of daily living (HOS ADL subscale), Hip Outcome Score sport (HOS sports subscale) and International Hip Outcome Tool (iHOT‐33) analyses were performed by using STATA version 14.0 MP (STATA, College Station, TX, USA) with the principal summary measures are mean between group difference, sample size, and standard deviation. We collected 52 articles in total after removing duplicates and screened by titles and abstracts. A total of three RCTs were included finally. There was definite evidence of additional benefit of arthroscopic hip surgery against conservative therapy in the field of improving quality of life (three trials, 575 participants, ES = 2.109, 95% CI: 1.373 to 2.845, I 2 = 42.8%, P = 0.000) and activity of daily living (two trials, 262 participants, ES = 9.220, 95% CI: 5.931 to 12.508, I 2 = 16.5%, P = 0.000). However, no significant difference could be seen in sports function improvement (two trials, ES = 7.562, 95% CI: −2.957 to 18.082, I 2 = 60.1%, P = 0.159). In conclusion, this meta‐analysis suggests that arthroscopic hip surgery provided essential benefit compared with conservative therapy in improving activity of daily living and quality of life.
Keywords: Arthroscopy, Conservative therapy, Femoroacetabular impingement syndrome, Meta‐analysis
A PRISMA Flow Chart of article selection process for the meta‐analysis. A total of 2483 studies were included in the study through a search of five databases, and 2480 articles were excluded by screening the abstracts and titles for duplicates, biomechanical experiments, case reports, reviews articles, and non‐comparative studies. A total of three full text articles were assessed for eligibility.

Introduction
Femoroacetabular impingement syndrome (FAIS) is a disorder of hip causing pain induced by a premature contact called impingement, between the femur and acetabulum during movement of the hip 1 . FAIS is a common cause in that young adults suffer from pain by the non‐arthritis factor 2 . FAIS is classified into cam, pincer, or mixed types. Cam morphology refers to a flattening or convexity at the femoral head neck junction, while the pincer type indicates a focal or global over‐coverage of the femoral head by the acetabulum. Mixed type indicates a combination of the previous two morphologies 3 . Hip joint, including articular cartilage, or labral cartilageor both, can be progressively damaged by FAIS. The scale of the cam deformity of the femoral head is most commonly evaluated with the radiologic alpha angle and the scale of the pincer deformity of the acetabulum is most commonly evaluated with the radiologic lateral center edge angle (LCEA) 4 . Moreover, femoroacetabular impingement may be a potential precursor to hip osteoarthritis (OA) in the young adult population 5 , 6 , 7 . Byrd et al. 8 noted that 96% of FAI teenagers participated in sports. It was significantly higher than the rate for adults. The FAI patients felt pain at anterolateral or anterior hip that radiated the groin and anterior thigh 9 , 10 . It can catastrophically affect the performance of young athletes. As a result, the current treatment strategy of FAIS is delaying the onset and progression of hip OA.
Arthroscopic hip surgery (AHS) and conservative therapy are both considered for FAIS. AHS for FAIS is an established treatment strategy, a 465% increase between 2005 and 2013 11 , and theoretical arguments have been made that the surgery for FAI may prevent the development of osteoarthritis 3 , 12 . Compared with open surgery, hip arthroscopy exhibits with the characteristics of safer and shorter recovery time 13 , 14 . Arthroscopy can correct the anatomic abnormalities causing pathologic mechanics of the hip joint and to repair any associated soft tissue damage 4 . Kunze et al. 15 even reported that FAI patients undergoing hip arthroscopy can improve sleep quality. However, it has been suggested that clinicians should be cautious in the use of surgery for FAIS and that approaches should be considered. Vovos et al. 16 and Lieberman et al. 17 reported that patients undergoing hip arthroscopy increase the risk of surgical complications in total hip arthroplasty (THA). Non‐operative treatments (conservative therapy) are also available for the therapeutic method FAIS. For instance, exercise‐based packages of conservative care delivered by a physiotherapist 1 , 18 . Patients with FAIS have altered hip muscle strength, range of motion (ROM) and gait biomechanics, and these offer potential targets for treatment through physiotherapy. However, limited articles with a high quality of evidence 19 , 20 suggested that conservative treatment was beneficial for FAI patients. Until recently, both AHS and conservative therapy can be the option for FAIS while the most suitable choice for FAIS patients is still controversial due to the limited evidence.
Therefore, we would like to assess the outcome differences between arthroscopic hip surgery and conservative therapy in patients suffered from FAIS with larger sample sizes by joint analysis of several trials performed worldwide. We planned to focus on the hip‐related quality of life and health‐related quality of life assessment to provide the most comprehensive evidence‐based treatment strategy for orthopedic doctors. For this reason, we performed this meta‐analysis of available comparative trials of arthroscopic hip surgery versus conservative therapy, to compare the outcomes of arthroscopy and conservative therapy on the management of FAIS. The objective of this study is to compare the Hip Outcome Score of activities of daily living (HOS ADL subscale), Hip Outcome Score sport (HOS sports subscale) and International Hip Outcome Tool (iHOT‐33) between arthroscopic hip surgery and conservative therapy.
Materials and Methods
This meta‐analysis followed the Preferred Reporting Items for Systematic Reviews and Meta‐analyses statement (PRISMA) under the statements for study design, data analysis and reporting of meta‐analyses of RCT that are currently available and widely adopted.
Literature Search
For trials regarding efficacy, we searched PubMed, Embase, Cochrane Central Register of Controlled Trials (CENTRAL), ClinicalTrials.gov using a Boolean search algorithm until 1 September 2019 under the following searching strategy listed in the Supplementary File. Cochrane Highly Sensitive Search Strategy for identifying randomized trials in PubMed and other sources where needed. “Femoroacetabular Impingement Syndrome” AND “arthroscopy” AND “conservative therapy” and their MeSH terms were used as the keywords for searching databases. “‘Impingement, Femoracetabular’ OR ‘Impingements, Femoracetabular’” AND “‘Arthroscopies’ OR ‘Arthroscopic Surgical Procedures’ OR ‘Arthroscopic Surgical Procedure’” AND “physiotherapy” are the free terms.
Study Selection
Two reviewers independently started and completed the initial title and abstract screening. We then retrieved full texts for the eligible studies. If a disagreement arose during the study selection process, a meeting between all authors and the supervising professor was needed to reach the agreement. The overall selection process is documented in a PRISMA flow diagram in Fig. 1.
Fig. 1.
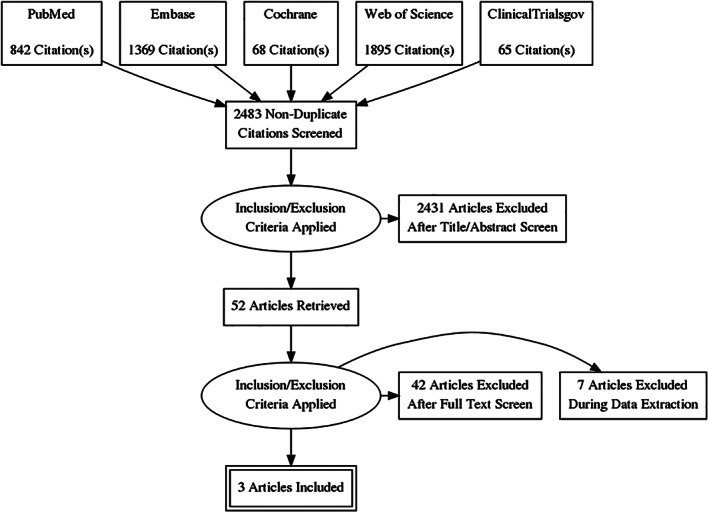
A PRISMA Flow Chart of article selection process for the meta‐analysis. A total of 2483 studies were included in the study through five databases search, and 2480 articles were excluded by screening the abstracts and titles for duplicates, biomechanical experiments, case reports, reviews articles, and non‐comparative studies. A total of three full text articles were assessed for eligibility.
Inclusion and Exclusion Criteria
We included all published randomized controlled trials comparing AHS for FAIS with conservative therapy. FAI syndrome is a motion‐related clinical disorder of the hip with a triad of symptoms, clinical signs, and imaging findings. The patients involved in this research should strictly conform to the diagnostic criteria 7 . Also, only randomized controlled trials were included in this meta‐analysis for limiting the errors and bias.
For arthroscopy, we found that the surgical strategies vary in patients with different pathology or condition of FAIS due to other complications. For example, reshaping surgery, labral surgery, or chondral surgery could be the choice of treatment for a patient but we defined all surgical strategies by arthroscopy as the AHS for FAIS. The arthroscopy for FAIS is a therapy no matter the adequate surgery method. Conservative therapy was defined as any treatments except surgery, although the administered physiotherapy or personalized treatment varied in each trial.
We excluded those who had open hip surgery for the intervention and all unfinished studies and certain types of literature, including reviews, editorial comments, letters, notes, surveys, conference abstract. Also, unpublished results and data were excluded from this meta‐analysis. The overall eligibility criteria are shown in Table 1.
TABLE 1.
Eligibility criteria applied in this meta‐analysis, including study type, participants, intervention, control intervention, and outcome
| Inclusion criteria | Exclusion criteria | |
|---|---|---|
| Study type | All randomized controlled trial |
|
| Participants | Involved patients should conform to symptoms, signs, diagnostic imaging:
|
Non‐human subjects |
| Intervention | Arthroscopic hip surgery | Open hip surgery |
| Control | Any treatment except surgery | N/A |
| Outcome |
|
Unpublished data |
Data Extraction and Quality Assessment
Two categories of data items were defined. Firstly, baseline characteristics including Gender, Age, body mass index (BMI), involved the side of hip, pathology type, and mean lateral center edge angle, which are relevant to the FAIS. Second, the Hip Outcome Score of activities of daily living (HOS ADL subscale), Hip Outcome Score sport (HOS sports subscale) and International Hip Outcome Tool (iHOT‐33) at 8 and 12 months follow‐up were included for efficacy analysis. As we know, HOS ADL is considered for activities of daily living, and it can be used as a measurement for patients' functional status 21 , while the HOS sports subscale is used for measuring sport‐related functions. Although, HOS ADL and HOS sports subscale are unidimensional, it provides adequate internal consistency, potentially responsive across the spectrum of ability, and contributed information across the spectrum of ability 22 . The International Hip Outcome Tool‐33 (iHOT‐33) is a 33‐item self‐administered outcome measure based on a Visual Analogue Scale response format designed for the young and active population with hip pathology 23 , 24 , which can reflect the hip‐related quality of life.
Two reviewers extracted the needed data from all eligible studies independently and the disagreements were solved by consensus after routine meetings in the study group. We decided to extract the data between 8 and 12 months after routine meetings because we noticed that the peak efficacy after treatment occured at this interval and no significant change could be observed at the follow‐up at two years 25 . As a result, for Palmer et al. 13 , although only baseline characteristics and 8 months follow‐up were reported, we combined 8 months follow‐up from Palmer et al. 13 with 12 months follow‐up from other articles 2 , 25 . If the relevant numeric outcome data were not reported by authors, we contacted the corresponding author or first author to obtain the related data or, extracted the numeric data from figures and graphs where available.
Risk of Bias Assessment
We aimed at minimizing reporting bias via completing a comprehensive search for eligible studies. Two authors assessed the risk of bias in included trials by using the Cochrane Collaboration's Tool 26 and assessed all the published articles including their protocols through selection bias, performance bias, attrition bias and reporting bias. If there are multiple follow‐up time points within one single trial, we assessed them individually.
Statistical Analysis
Statistical heterogeneity is analyzed within these articles with the χ2 and I 2 tests 27 . We used the following criteria for heterogeneity: I 2 > 50% for the presence of heterogeneity, and I 2 > 70% for the high heterogeneity.
If the trials used different outcome measures to evaluate the same scale, the most common outcome measure as the index and transformed other scales to mean difference (MD) and obtained the standard deviation (SD).
This meta‐analysis was performed by using STATA version 14.0 MP (STATA, College Station, TX, USA) with the principal summary measures between group difference, sample size, and standard deviation. We pooled continuous outcome data of MDs and SDs. The particular code of STATA for one group continuous variable was administered for this analysis due to the single group continuous data 28 . The fixed model was administered when I 2 < 50% while the random model was used if I 2 > 50% 29 .
Finally, MD and SD are pooled as the summary estimate 30 , 31 . Mixed‐effects regression analysis was used to assess the effects of intervention for the fixed‐effect of impingement type, sex, and baseline characteristics so that the adjusted differences between groups were treated as outcomes 2 . In the pooled trials, the raw scales were documented as MD and 95% confidence interval (CI), while SDs were needed to be pooled. Hence, we estimated the SDs from sample size and 95% CI from each trial with a specific method and formula when needed 32 , 33 , 34 .
Results
Search Results
We retrieved 842 citations from PubMed, 1369 citations from Embase, 68 citations from Cochrane, 1895 citations from Web of Science, and 65 citations from Clinicaltrials.gov. A total of 52 articles remained after the title or abstract screening. Of these, three articles were included to conduct meta‐analysis based on the inclusion and exclusion criterion, as well as meeting the data items 2 , 13 , 25 . Then we extracted data from three eligible articles and Fig. 1 demonstrated the graphical illustration of the selection process according to the suggestion of PRISMA.
Study Characteristics
Three eligible trials were included, covered an overall population of 650 patients who suffered from FAIS and received arthroscopy or conservative therapy respectively, baseline characteristics of included patients are shown in Table 2. All articles compared the effectiveness of AHS and conservative therapy via randomized controlled trials up to 1 September 2019. The enrolled patients in these trials suffered from FAIS, whereas the pathology classification, surgical method, and conservative therapy differ in each patient. Mansell et al. 25 was a single‐center (Military Health Care, MHS) designed trial comparing AHS and physiotherapy, with the patients ranging from 18 to 60 years. Acetabuloplasty, labral repair or debridement, and femoroplasty were the surgery interventions, while a supervised physical therapy was administered to the conservative group of patients. The UK FASHIoN trial 2 was a multicenter controlled trial with the criteria of age greater than 16 years. Osteoarthritis was an excluded criterion for the recruitment of patients. Reshaping surgery, labral surgery, and chondral surgery were the interventions with a package of physiotherapist‐led rehabilitation for conservative group 18 . When it comes to Palmer et al. 13 , it was a multicenter controlled trial with the age of patients ranging from 18 to 60 years. Osteochondroplasty, labral repair or debridement were the dominating surgery interventions while specific physiotherapy was for the conservative group of patients 35 . The detail study characteristics and original data used for calculations are shown in Tables 3 and 4 respectively 2 , 35 , 36 .
TABLE 2.
Baseline characteristics of patients in each trial. Three trails were selected and included in this study. Gender, age, BMI, injured hips, types of femoroacetabular impingement syndrome were embedded into the study for assessment
| Study | Male sexd | Age yeard | BMId | Right hip involvedd | Left hip involvedd | Cam typed | Mixed typed | Pincer typed | MLCEA c | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| C a | A b | C a | A b | C a | A b | C a | A b | C a | A b | C a | A b | C a | A b | C a | A b | C a | A b | |
| Mansell, 2018 | 26 (40) | 21 (40) | 30.8 (7.4) | 29.7 (7.3) | 27.47 (4.3) | 28.23 (4.4) | 19 (40) | 29 (40) | 21 (40) | 11 (40) | N/A | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Griffin, 2018 | 113 (177) | 100 (171) | 35.2 (9.4) | 35.4 (9.7) | N/A | N/A | 103 (177) | 95 (171) | 74 (177) | 75 (171) | 133 (177) | 129 (171) | 30 (177) | 29 (171) | 14 (177) | 13 (171) | 31° (5°) | 31° (5°) |
| Palmer, 2019 | 37 (110) | 38 (112) | 36.0 (9.9) | 36.4 (9.6) | 26.6 (4.8) | 25.9 (4.8) | 59 (110) | 67 (112) | 51 (110) | 45 (112) | 104 (110) | 104 (112) | 6 (110) | 7 (112) | 0 | 1 (112) | 29.2° (6.7°) | 28.5° (6.8°) |
Conservative group;
Arthroscopic hip surgery group;
Mean lateral center edge angle;
Values are presented as No of male sex (No of total participants) or Mean (SD).
TABLE 3.
Detailed characteristics among each trial. Types of randomized controlled trial, treatment strategy, sample size and the length of follow‐up were shown
| Trial | Treatment Strategy | Target sample size | Follow‐up | ||
|---|---|---|---|---|---|
| Mansell, 2018 |
|
Intervention |
|
37 |
|
| Control | Supervised physical therapy program: hip mobilization, therapeutic exercise (two 45‐min/week, 6 weeks in total). | 37 | |||
| Griffin (UK FASHIoN), 2018 |
|
Intervention |
|
171 |
|
| Control | Personalized hip therapy: assessment of pain & function & range of motion, patient education, exercise program taught in clinic & repeated at home (individualization, progression, supervision), help with pain relief. (Six to ten face to face contacts over 12–24 weeks.) | 177 | |||
| Palmer, 2019 |
|
Intervention |
|
112 |
|
| Control | Physiotherapy and activity modification: eight sessions over 5 months | 110 |
TABLE 4.
Original data used for the measurements and calculations. Group difference between intervention & control were assessed through HOS ADL subscale, HOS sports subscale, and iHOT
| Study/Trial | HOS ADL subscale | HOS sport subscalea | iHOTa |
|---|---|---|---|
| Group difference between intervention & control | Group difference between intervention & control | Group difference between intervention & control | |
| Mansell, 2018 | 4.9 (36.9) n = 74 | 0.6 (54.6) n = 74 | 5.0 (55.0) n = 74 |
| Griffin, UK FASHIoN, 2018 | N/A | N/A | 6.8 (46.9) n = 321 |
| Palmer, 2018 | 10.0 (25.0) n = 188 | 11.7 (41.20) n = 190 | 2.0 (5.1) n = 180 |
Values are presented as MD (SD) No of participants.
Risk of Bias Assessment
The assessment was demonstrated in Table 5 by the suggestion of the Cochrane Collaboration Tool 27 . For the comparisons of AHS versus conservative therapy on FAIS patients, the risk bias of all efficacy subscales was low. After assessment according to Cochrane Collaboration Tool, the selection, performance, detection, attrition and, reporting bias were low while the performance bias for all three articles was high, for the reason that the procedure between AHS and conservative therapy are incredibly different. Consequently, the blinding among interventions was impossible to administer.
TABLE 5.
Risk of bias assessment. The risk bias for included studies were assessed using the Cochrane handbook. “High risk,” “low risk,” and “unclear risk” were shown
| Bias | Judgment | Support |
|---|---|---|
| Article 1 | Mansell et al. | |
| Selection | Low | Quote: “Randomization was carried out electronically by an independent person not on the research team … All follow‐up outcome assessments were conducted by another person …” |
| Performance | High | Quote: “If patients preferred either only surgery or only rehabilitation and did not want the possibility of being randomized to the other treatment, they were not eligible to participate …” |
| Detection | Low | Quote: “All follow‐up outcome assessments were conducted by another person not involved with either treatment or aware of the initial treatment allocation.” |
| Attrition | Low | The reason of exclusion of patient was clearly stated |
| Reporting | Low | Primary outcome and secondary outcome were Hip Outcome Score (HOS) and International Hip Outcome Tool (iHOT‐33) respectively. They are widespread used in hip assessment. |
| Article 2 | Griffin et al. | |
| Selection | Low | Quote: “Participants were recruited from the specialist hip arthroscopy service at each hospital … Patients were randomly assigned with a computer‐generated minimization algorithm for center and type of impingement … Allocation concealment was ensured by used of a secure telephone randomization service hosted by Warwick Clinical Trials Unit.” |
| Performance | High | Quote: “It was not possible to mask patients or the treating clinicians to their allocation.” |
| Detection | Low | Quote: “Researchers who collected outcome assessments and analyzed the results were masked to allocation by concealment of treatment.” |
| Attrition | Low | The reason of exclusion of patient was clearly stated |
| Reporting | Low | Primary outcome and secondary outcome were Hip Outcome Score (HOS) and International Hip Outcome Tool (iHOT‐33) respectively. They are widespread used in hip assessment. |
| Article 3 | Palmer et al. | |
| Selection | Low | Quote: “A research nurse at each site performed randomization using an automated computer‐generated telephone randomization system provided by Oxford Clinical Trials Research Unit.” |
| Performance | High | Quote: “It was not possible to mask participants, or clinicians delivering the intervention.” |
| Detection | Low | Quote: “Clinicians performing follow‐up clinical assessments were blinded to the treatment group … Staff members independent of the study team carried out data entry.” |
| Attrition | Low | The reason of exclusion of patient was clearly stated |
| Reporting | Low | Primary outcome and secondary outcome were Hip Outcome Score (HOS) and International Hip Outcome Tool (iHOT‐33) respectively. They are widespread used in hip assessment. |
Clinical Outcomes
GRADE (Grading of Recommendations, Assessment, Development and Evaluation) summary of findings for outcomes for these three comparisons are shown in Table 6.
TABLE 6.
GRADE (Grading of Recommendations, Assessment, Development and Evaluation) summary of findings for the comparison of arthroscopic hip surgery versus conservative therapy. Outcome, time frame, measurement instruments and relative effects, absolute effect estimates, certainty in effect estimates (quality of evidence), and plain text summary were shown
| Absolute effect estimates | |||||
|---|---|---|---|---|---|
| Outcome, Timeframe | Measurement instruments and relative effects | Arthroscopic hip surgery | Conservative therapy | Certainty in effect estimates (quality of evidence) | Plain text summary |
| Activity of daily living, 8–12 months |
Measured by HOS ADL scaled to 0–100%. Scale: 0–100%, higher better MID: 4.9 units Based on data from 266 patients in 2 trials. |
Difference: ES 9.220 higher (95% CI 5.931 lower to 12.508 higher) | High | Arthroscopic hip surgery improves the activity of daily living compared with conservative therapy. | |
| Sports function, 8–12 months |
Measured by HOS sports scaled to 0–100 Scale: 0–100, higher better MID: 0.6 units Based on data from 264 patients in 2 trials. |
Difference: ES 7.562 higher (95% CI 2.957 lower to 18.082 higher) | High | Arthroscopic hip surgery has little or no effect on improving sports function compared with conservative care. | |
| Hip quality of life, 8–12 months |
Measured by iHOT scaled to 0–100 Scale: 0–100, higher better MID: 2.0 units Based on data from 575 patients in 3 trials. |
Difference: ES 3.501 higher (95% CI 0.068 lower to 6.934 higher) | High | Arthroscopic hip surgery improves the hip quality of life compared with conservative therapy. | |
In the analysis of iHOT score, Mansell et al. 25 , Palmer et al. 13 and UK FASHIoN 2 were pooled for the analysis. As a result, there was substantial evidence indicating that AHS is the favored choice for the situation of FAIS (three trials, 575 participants, ES = 2.109, 95% CI: 1.373 to 2.845, I 2 = 42.8%, P = 0.000) as shown in Fig. 2.
Fig. 2.
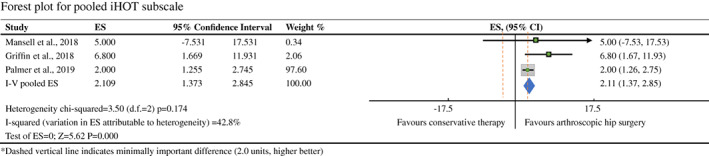
Forest plot for pooled iHOT subscale between arthroscopic hip surgery versus conservative therapy on femoroacetabular impingement syndrome. Three studies reported iHOT subscale. The heterogeneity among these studies was moderate (I 2 = 42.8%). P = 0.000, difference was statistically significant.
For HOS ADL subscale, Griffin et al. 2 , Mansell et al. 25 and Palmer et al. 13 revealed low risk of bias and were sufficiently both clinically and methodologically homogeneous (Heterogeneity chi‐squared = 1.20, P = 0.274, I 2 = 16.5%), which was allowed to be pooled for comparison of arthroscopy versus conservative care on FAIS. As a result, there was definite evidence of no significant benefit of conservative therapy at 12 months (two trials, 262 participants: ES = 9.220, 95% CI: 5.931 to 12.508, I 2 = 16.5%, P = 0.000). The detailed data is shown in Fig. 3.
Fig. 3.
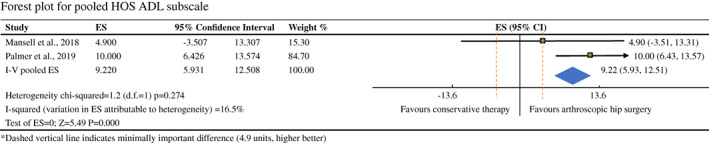
Forest plot for pooled HOS ADL subscale between arthroscopic hip surgery versus conservative therapy on femoroacetabular impingement syndrome. Two of three studies reported HOS ADL subscale. The heterogeneity among these studies was high I 2 = 16.5% represented the heterogeneity. P = 0.000, difference was statistically significant.
When it comes toHOS sports subscale analysis, however, there was no statistically significant difference between AHS and conservative therapy (two trials, 264 participants: ES = 7.562, 95% CI: −2.957 to 18.082, I 2 = 60.1%, P = 0.159) with the demonstration of detailed data Fig. 4.
Fig. 4.
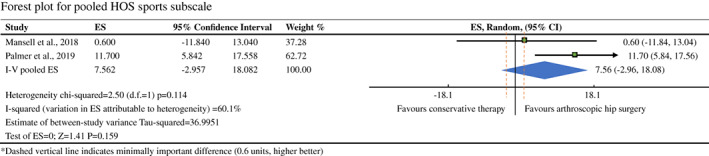
Forest plot for pooled HOS sports subscale between arthroscopic hip surgery versus conservative therapy on femoroacetabular impingement syndrome. Two of three studies reported HOS sports subscale. The heterogeneity among these studies was moderate (I 2 = 60.1%). P = 0.159, difference was not statistically significant.
Within these three trials, Mansell et al. reported the similar treatment effect between arthroscopy and conservative care while Palmer et al. and UK FASHIoN revealed that offering AHS to patient suffered from FAIS led to a better prognosis.
Discussion
In the analysis of HOS ADL subscale, AHS showed a more positive effect on daily life activity compared with conservative therapy at early follow‐up of 8 to 12 months. Also, for the concept of hip‐related quality of life, the iHOT score, AHS was the favorable option for FAIS patients. Therefore, from this meta‐anlaysis of FAIS management, offering arthroscopy for FAI patients led to better patient‐assessed function in daily life activity and improved quality of life.
Nevertheless, when it comes to sport‐related assessment, there was no statistical significance between AHS and conservative therapy. For the sake of giving comprehensive evidence to instruct clinical work, the reasons showing no significance were discussed. The required movement of the hip was lower in the assessed items in the HOS ADL and iHOT survey compared to the HOS sports subscale, while the involved range of movement counts in the situation of impingement. AHS repaired the deformity of acetabulum but conservative therapy cannot. As a result, there was a significant difference between AHS and conservative therapy. For the HOS sports scale, results of this analysis could either be because AHS or conservative therapy does not have an effect on the improvement of sports function or the scales used to measure are not sufficiently sensitive to detect the occurred changes.
More factors would be considered, such as BMI, the strength of muscle, proprioception, and rehabilitation after surgery. With this result, neither AHS nor physiotherapy could improve the sport function and, a combination of AHS and physiotherapy might be useful. Further research is needed for investigating the specific factor affecting the improvement of sports function.
Strengths and Limitations
This article is the first meta‐analysis of FAIS comparing the effectiveness of AHS and conservative therapy. As mentioned, AHS has seen a dramatical increase in North America between 2005 and 2013 11 , 37 and become a desirable option for FAIS. In spite of lack of evidence to prove the priority of AHS, leading to difficulty during the choice of treatment strategy, after this first‐published and most comprehensive meta‐analysis with three comparisons, arthroscopic surgery was concluded to be the better choice for the FAIS compared with conservative therapy. High‐quality evidence reveals that surgery versus conservative therapy confers essential benefit in the field of improving the activity of daily living and quality of life. Although just three trials were included in this meta‐analysis, they were randomized controlled trials, and two of them were multicenter trials 2 , 13 with a large sample size. Thus, our meta‐analysis provides a high‐grade evidence for the treatment option of FAIS.
However, several factors can affect the results, and they will be mentioned in this section. The conservative therapy in the three trials was not the same and they may lead to a different efficacy of the situation so that we defined the treatments except surgery as conservative care in this study. The same situation occurred in the method or eligibility criteria of surgery. The three trials in this meta‐analysis were mainly performed in America and Europe with the follow‐up of 1 to 2 years. More trials performed in different regions and centers with longer follow‐up are needed in the future.
Inferences and Implications
The exact choice for FAIS was controversial until we finished this research because there was no meta‐analysis about this topic before. We provided the highest evidence‐based proof for clinicians engaging patients with FAIS.
Policymakers, funders, and clinicians should consider these results in their policymaking, funding and clinical decisions regarding the management of patients with FAIS.
Unanswered Questions and Future Research
During the process of searching the literature, we found a protocol of Australian FASHIoN trial comparing AHS to physiotherapy care 38 and it is under the process of recruiting. It is the first trial about this topic performed in Australia, which is indispensable to draw a treatment strategy worldwide.
This meta‐analysis was designed to assess the better choice between AHS and conservative therapy, while several factors, such as complications, BMI, occupation, alcohol‐abuse, or diabetes mellitus, could lead to a different condition of the hip resulting in different outcomes. The option of treatment strategy could be changed in the above situations. Accordingly, further specific investigations targeting patients with different baseline characteristics and complications are still necessary.
Conclusion
According to this meta‐analysis, there was a strong evidence proofing AHS was the optimal choice for FAIS patients improvingthe activity of daily living and quality of life, while with the perspective of sports function, the choice should be made by comprehensive assessment of patients.
Supporting information
Appendix S1. Supporting Information
Acknowledgments
This meta‐analysis did not receive any specific grant from any funding agency.
Contributor Information
Jing‐hua Pan, Email: huajanve@foxmail.com.
Hui‐ge Hou, Email: 18620085802@126.com.
Jie‐ruo Li, Email: ilorugaie@163.com.
Data Availability Statement
All data are available in each included trials with the references and they can be found in the tables or figures of this article.
References
- 1. Kemp JL, Beasley I. International consensus on femoroacetabular impingement syndrome: the Warwick agreement—why does it matter. Br J Sports Med, 2016, 2016: 1162–1163. [DOI] [PubMed] [Google Scholar]
- 2. Griffin DR, Dickenson EJ, Wall P, et al. Hip arthroscopy versus best conservative care for the treatment of femoroacetabular impingement syndrome (UK FASHIoN): a multicentre randomised controlled trial. Lancet, 2018, 391: 2225–2235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res, 2003, 417: 112–120. 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 4. Pun S, Kumar D, Lane NE. Femoroacetabular impingement. Arthritis Rheumatol, 2015, 67: 17–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agricola R, Heijboer MP, Bierma‐Zeinstra SM, Verhaar JA, Weinans H, Waarsing JH. Cam impingement causes osteoarthritis of the hip: a nationwide prospective cohort study (CHECK). Ann Rheum Dis, 2013, 72: 918–923. [DOI] [PubMed] [Google Scholar]
- 6. Eijer H, Hogervorst T. Femoroacetabular impingement causes osteoarthritis of the hip by migration and micro‐instability of the femoral head. Med Hypotheses, 2017, 104: 93–96. [DOI] [PubMed] [Google Scholar]
- 7. Griffin DR, Dickenson EJ, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med, 2016, 50: 1169–1176. [DOI] [PubMed] [Google Scholar]
- 8. Byrd JW, Jones KS, Gwathmey FW. Arthroscopic management of femoroacetabular impingement in adolescents. Arthroscopy, 2016, 32: 1800–1806. [DOI] [PubMed] [Google Scholar]
- 9. Bedi A, Dolan M, Leunig M, Kelly BT. Static and dynamic mechanical causes of hip pain. Arthroscopy, 2011, 27: 235–251. [DOI] [PubMed] [Google Scholar]
- 10. Sink EL, Gralla J, Ryba A, Dayton M. Clinical presentation of femoroacetabular impingement in adolescents. J Pediatr Orthop, 2008, 28: 806–811. [DOI] [PubMed] [Google Scholar]
- 11. Maradit Kremers H, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty, 2017, 32: 750–755. [DOI] [PubMed] [Google Scholar]
- 12. Ganz R, Gill TJ, Gautier E, Ganz K, Krügel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br, 2001, 83: 1119–1124. [DOI] [PubMed] [Google Scholar]
- 13. Palmer A, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ, 2019, 364: 185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Matsuda DK, Carlisle JC, Arthurs SC, Wierks CH, Philippon MJ. Comparative systematic review of the open dislocation, mini‐open, and arthroscopic surgeries for femoroacetabular impingement. Arthroscopy, 2011, 27: 252–269. [DOI] [PubMed] [Google Scholar]
- 15. Kunze KN, Leong NL, Beck EC, Bush‐Joseph CA, Nho SJ. Hip arthroscopy for Femoroacetabular impingement improves sleep quality postoperatively. Arthroscopy, 2019, 35: 461–469. [DOI] [PubMed] [Google Scholar]
- 16. Vovos TJ, Lazarides AL, Ryan SP, Kildow BJ, Wellman SS, Seyler TM. Prior hip arthroscopy increases risk for perioperative total hip arthroplasty complications: a matched‐controlled study. J Arthroplasty, 2019, 34: 1707–1710. [DOI] [PubMed] [Google Scholar]
- 17. Lieberman JR. Hip arthroscopy for femoroacetabular impingement patients older than 50 years‐proceed with caution. Arthroscopy, 2019, 35: 2759–2760. [DOI] [PubMed] [Google Scholar]
- 18. Griffin D, Wall P, Realpe A, et al. UK FASHIoN: feasibility study of a randomised controlled trial of arthroscopic surgery for hip impingement compared with best conservative care. Health Technol Assess, 2016, 20: 1–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Emara K, Samir W, Motasem el H, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong), 2011, 19: 41–45. [DOI] [PubMed] [Google Scholar]
- 20. Hunt D, Prather H, Harris Hayes M, Clohisy JC. Clinical outcomes analysis of conservative and surgical treatment of patients with clinical indications of prearthritic, intra‐articular hip disorders. PM R, 2012, 4: 479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Wiener JM, Hanley RJ, Clark R, Van Nostrand JF. Measuring the activities of daily living: comparisons across national surveys. J Gerontol, 1990, 45: S229–S237. [DOI] [PubMed] [Google Scholar]
- 22. Martin RL, Kelly BT, Philippon MJ. Evidence of validity for the hip outcome score. Arthroscopy, 2006, 22: 1304–1311. [DOI] [PubMed] [Google Scholar]
- 23. Ruiz‐Ibán MA, Seijas R, Sallent A, et al. The international hip outcome Tool‐33 (iHOT‐33): multicenter validation and translation to Spanish. Health Qual Life Outcomes, 2015, 13: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Mohtadi NG, Griffin DR, Pedersen ME, et al. The development and validation of a self‐administered quality‐of‐life outcome measure for young, active patients with symptomatic hip disease: the international hip outcome tool (iHOT‐33). Arthroscopy, 2012, 28: 595–605 quiz 606‐610.e1. [DOI] [PubMed] [Google Scholar]
- 25. Mansell NS, Rhon DI, Meyer J, Slevin JM, Marchant BG. Arthroscopic surgery or physical therapy for patients with Femoroacetabular impingement syndrome: a randomized controlled trial with 2‐year follow‐up. Am J Sports Med, 2018, 46: 1306–1314. [DOI] [PubMed] [Google Scholar]
- 26. Snyder JS, Drew MR. Functional neurogenesis over the years. Behav Brain Res, 2020, 382: 112470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ, 2011, 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Siristatidis CS, Gibreel A, Basios G, Maheshwari A, Bhattacharya S. Gonadotrophin‐releasing hormone agonist protocols for pituitary suppression in assisted reproduction. Cochrane Database Syst Rev, 2015. 10.1002/14651858.cd006919.pub4. [DOI] [PMC free article] [PubMed]
- 29. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed‐effect and random‐effects models for meta‐analysis. Res Synth Methods, 2010, 1: 97–111. [DOI] [PubMed] [Google Scholar]
- 30. Guyatt GH, Thorlund K, Oxman AD, et al. GRADE guidelines: 13. Preparing summary of findings tables and evidence profiles‐continuous outcomes. J Clin Epidemiol, 2013, 66: 173–183. [DOI] [PubMed] [Google Scholar]
- 31. Thorlund K, Walter SD, Johnston BC, Furukawa TA, Guyatt GH. Pooling health‐related quality of life outcomes in meta‐analysis—a tutorial and review of methods for enhancing interpretability. Res Synth Methods, 2011, 2: 188–203. [DOI] [PubMed] [Google Scholar]
- 32. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol, 2005, 5: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol, 2014, 14: 135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Higgins JP, White IR, Anzures‐Cabrera J. Meta‐analysis of skewed data: combining results reported on log‐transformed or raw scales. Stat Med, 2008, 27: 6072–6092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Palmer AJ, Ayyar‐Gupta V, Dutton SJ, et al. Protocol for the femoroacetabular impingement trial (FAIT): a multi‐centre randomised controlled trial comparing surgical and non‐surgical management of femoroacetabular impingement. Bone Joint Res, 2014, 3: 321–327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mansell NS, Rhon DI, Marchant BG, Slevin JM, Meyer JL. Two‐year outcomes after arthroscopic surgery compared to physical therapy for femoracetabular impingement: a protocol for a randomized clinical trial. BMC Musculoskelet Disord, 2016, 17: 60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Art Ther, 2013, 29: 661–665. [DOI] [PubMed] [Google Scholar]
- 38. Murphy NJ, Eyles J, Bennell KL, et al. Protocol for a multi‐centre randomised controlled trial comparing arthroscopic hip surgery to physiotherapy‐led care for femoroacetabular impingement (FAI): the Australian FASHIoN trial. BMC Musculoskelet Disord, 2017, 18: 406. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information
Data Availability Statement
All data are available in each included trials with the references and they can be found in the tables or figures of this article.


