Abstract
Purpose
The purpose of this study was to determine whether direct arthroscopic control of femoral buttons can prevent improper deployment and soft tissue interposition in anterior cruciate ligament (ACL) reconstruction.
Methods
A retrospective analysis of prospectively collected data from the SANTI study group database was performed. All patients who underwent ACL reconstruction using suspensive femoral fixation between 01/01/2017 and 31/12/2019 were included. Patient assessment included demographics, sports metrics, reoperations performed and femoral button-related specific complications such as iliotibial band (ITB) irritation and/or septic arthritis. Proper deployment of the button and soft tissue interposition were assessed on postoperative radiographs.
Results
A total of 307 patients underwent ACL reconstruction using adjustable femoral button fixation and were analyzed after a mean follow-up of 35.2 ± 11.0 months (14.3–50.2). The mean age was 39.5 ± 10.9-years old (range 13.3–70.6). Postoperative radiographs showed a correctly deployed femoral button without soft tissue interposition for all patients. No septic arthritis was reported. Nine patients (2.9%) suffered from lateral pain related to ITB irritation due to the button. Five of them had their symptoms resolve during rehabilitation. Ultrasound-guided corticosteroid infiltration was necessary for four patients after an average delay of 14.5 ± 4.8 months (11.7–21.7). Three patients were then symptom-free, but one required surgical removal of the implant 27.5 months after the surgery. Regarding unrelated femoral button complications, 15 patients (4.9%) underwent secondary arthroscopic procedures, including meniscectomy (1.6%), surgery for cyclops syndrome (2.6%) and revision ACLR (0.7%).
Conclusion
Arthroscopic confirmation of femoral button deployment prevents soft tissue interposition without specific complications.
Level of evidence
Level IV.
Keywords: ACL, ACL reconstruction, Femoral button, Button deployment, Tissue interposition, Ilio-tibial Band Irritation
Introduction
Graft fixation during anterior cruciate ligament reconstruction (ACLR) is a hotly debated topic [1, 2]. Since the study by Kurosaka et al.[3] in 1987, several hundred studies based mainly on in vitro biomechanical experiments have been devoted to this subject [1]. Given the lack of clinical studies demonstrating the superiority of one method over another, no gold standard has been recommended to date. Easy and fast to use while providing excellent clinical outcomes, suspensive femoral fixation has become a popular technique over the last fifteen years [4–7].
Anterior cruciate ligament (ACL) graft fixation using a femoral button presents specific complications, such as improper deployment of the implant [8, 9], widening of the tunnel [10–12], and iliotibial band (ITB) irritation [13, 14]. Occurring in 15–25.2% of cases, soft tissue interposition is, however, the most frequent complication [9, 15–17]. A degradation of postoperative clinical scores is also directly related to implant migration over time [15, 18]. As suggested by Mae et al.[15], this could decrease femoral fixation quality and alter graft integration. The increased rate of graft rupture in cases of ACL reconstruction with a femoral button compared to other fixation modes, as reported by the Danish and Norwegian registries, could then be explained [4, 6].
Various techniques have been described to prevent these complications, such as intraoperative fluoroscopy or accessory approaches allowing direct visualization of the implant [9, 19]. Although effective, these methods are time consuming and either irradiating or invasive. Intra-articular positioning of the femoral tunnel exit point, made possible with outside-in drilling, allows direct arthroscopic visualization of the femoral button in the lateral glutter [20, 21]. The purpose of this study was to determine whether soft tissue interposition and improper button deployment can be prevented using direct arthroscopic control. The hypothesis was that direct arthroscopic visualization of femoral button deployment decreases specific complications related to femoral fixation during ACLR.
Materials and methods
Institutional Review Board approval (COS-RGDS-2021-01-004) was granted for this study, and all participants gave valid consent to participate. A retrospective analysis of prospectively collected data from the SANTI study group database was performed. All patients who underwent arthroscopic ACLR (primary or revision) or ACL repairs performed by a single surgeon (BSC) from 01/01/2017 to 31/12/2019 were assessed for eligibility. The diagnosis of ACL tears was based on magnetic resonance imaging (MRI) and a complete clinical examination. Surgical management was decided upon when the patient's subjective instability restricted him in his sports or daily activities. From this group, all patients whose ACL graft was fixed to the femur using suspensive fixation (TightRope®, Arthrex, Naples, Florida) were identified and included. Patients who underwent ACL repairs or major concomitant surgery (e.g., multiligament reconstructions) were excluded.
Data extraction
Demographic data (age, sex, weight, height and body mass index (BMI)) and the characteristics of the index surgical procedures (whether a LEAP or associated high tibial osteotomy was performed or meniscal and chondral lesions were observed during arthroscopy) were extracted from the SANTI study group database. Preoperative sports practice was reported, and sports levels were evaluated by the Tegner activity scale.
Knee radiographs were systematically performed postoperatively. Each radiograph was analyzed by a trained orthopedic surgeon who attested to the correct deployment of the button on the lateral side of the femur. The distance between the cortex and the implant was measured on frontal radiographs. If the latter distance was less than one millimeter, soft tissue interposition was considered nonexistent [15].
Data regarding subsequent arthroscopy and its indications were provided. Any postoperative complications that did not require surgical management were also indicated, as was the resulting treatment. Potentially femoral button-related complications were given particular attention: lateral knee pain (requiring corticosteroid infiltration or not), surgical removal of the implant, and septic arthritis.
Surgical technique
All ACLRs were performed according to the Single-AnteroMedial Bundle Biological Augmentation (SAMBBA) technique described previously [20]. The semitendinosus (ST) was harvested using an open-ended tendon stripper and then quadrupled. The tibial insertion was preserved to improve fixation and vascularity [22]. An outside-in femoral guide was used, and its exit point was positioned intraarticularly under arthroscopic control. A 20-mm femoral bone socket was created using a FlipCutter II (Arthrex, Naples, Florida) according to the graft diameter [23]. Soft tissues were shaved along the lateral end of the femoral tunnel. The ACL graft was passed from the tibia to the femur. The arthroscope was introduced into the lateral gutter, allowing direct visualization of the button deployment (Fig. 1). The graft was secured on the femoral side with the TightRope® tensioning device (Arthrex, Naples, Florida) and then fixed on the tibial side at 30° of flexion using a bioabsorbable screw (Arthrex, Naples, Florida). The button sutures were cut flush with the implant under arthroscopic control without additional safety knots.
Fig. 1.

Arthroscopic confirmation of correct Button deployment in the lateral gutter. Process of flipping the TightRope button on the lateral cortex of the femur under arthroscopic visualization in the right knee. While the arthroscope is in the lateral gutter, the blue suture is tensioned to pull the graft into the joint. a The button is visualized while exiting the tunnel. b, c A probe is used to help seat the button. (Reprinted with permission from Arthroscopy Techniques)
For patients who underwent an additional lateral extra-articular procedure (LEAP), a modified deep Lemaire procedure [24] or independent reconstruction of the anterolateral ligament using the gracilis tendon was performed.
Rehabilitation
Weight bearing was allowed in the immediate postoperative period and while protected by crutches until the fourth week. Mobilization of the knee was brace free, except in the presence of meniscal repairs; weight bearing was progressive. Early rehabilitation focused on the restoration of full extension. Open-chain muscle strengthening was contraindicated until 3 months postoperatively. Cycling was allowed at one month, running at three months, nonpivoting sports at 4 months, pivoting noncontact sports at 6 months and pivoting contact sports at 8 to 9 months.
Follow-up
Postoperative follow-up was undertaken either by a sport physician or the senior surgeon at 3 and 6 weeks and then at 3, 6, 12 and 24 months. Anteroposterior side-to-side laxity (Rolimeter®, Aircast, Europe) and pivot shift examinations were performed at each consultation, and the occurrence of femoral button-related lateral pain was assessed. If the patient’s pain did not improve through functional rehabilitation, echo-guided corticosteroid infiltration was performed around the implant by a trained radiologist. In case of failure, surgical removal of the button was then proposed.
Statistical analysis
Descriptive statistics were calculated to characterize demographics, surgical characteristics, and radiographs analysis, including proper button deployment and soft tissue interposition. Additional descriptive statistics were obtained regarding postoperative complications, stratified by their potential connection to the femoral button. Quantitative variables are expressed as the mean values, standard deviation, and range. For qualitative variables, the number of observations and the percentage are presented.
Results
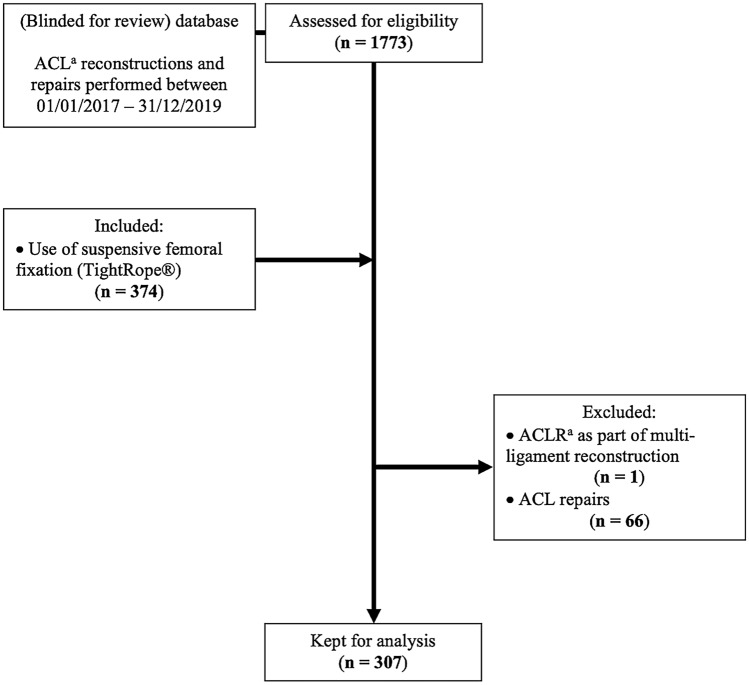
A total of 1773 ACLRs and ACL repairs were performed by the same senior surgeon between 01/01/2017 and 12/31/2019. Among these, 374 grafts were fixed to the femur using suspensive fixation (TightRope®, Arthrex, Naples, Florida). One patient was excluded because of concomitant multiligament reconstruction. Sixty-six ACL repairs were also excluded. Therefore, the results of 307 ACLRs performed according to the SAMBBA technique on 302 patients were retained for analysis. The study flow chart is shown in Fig. 2.
Fig. 2.
Study flow chart. Study flow chart in line with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement [40]. aACL anterior cruciate ligament, ACLR anterior cruciate ligament reconstruction
The demographics of the study population are presented in Table 1. The mean age was 39.5 ± 10.9-years old (13.3–70.6), with a mean follow-up of 35.2 ± 11.0 months (14.3–50.2). A majority of patients were involved in pivoting or pivoting-contact sports (n = 239, 77.9%) before surgery, with a mean Tegner activity scale score of 6.0 ± 1.2 (3–9). The surgical characteristics are presented in Table 2. Twenty-six patients (8.5%) had a concomitant lateral extra-articular procedure (LEAP), either modified Lemaire (n = 14, 4.6%) or anterolateral ligament reconstruction (ALLR, n = 12, 3.9%). Meniscal lesions were identified and treated in 143 patients (46.5%), most of which involved the medial meniscus (n = 103, 33.5%).
Table 1.
Demographics of the study population and sport practice metrics
| SAMBBA n = 307 | |
|---|---|
| Sex n (%) | |
| Male | 181 (59.0) |
| Female | 126 (41.0) |
|
Age mean ± SD (range), y |
39.5 ± 10.9 (13.3–70.6) |
|
BMIa mean ± SD (range), kg/m2 |
24.5 ± 3.6 (16.6–36.8) |
| Side n (%) | |
| Left | 153 (49.8) |
| Right | 154 (50.2) |
|
Delay accident—ACLRa mean ± SD (range), month |
12.5 ± 38.1 (0.2–329.6) |
|
Preoperative side-to-side laxity (Rolimeter®) mean ± SD (range), mm |
6.0 ± 1.6 (4–14) |
| Preoperative sport practice n (%) | |
| Pivoting | 105 (34.2) |
| Pivoting–contact | 134 (43.7) |
| Non-pivoting | 68 (22.1) |
|
Preoperative Tegner activity scale score mean ± SD (range) |
6.0 ± 1.2 (3–9) |
|
Follow-up mean ± SD (range), month |
35.2 ± 11.0 (14.3–50.2) |
aBMI body mass index, ACLR anterior cruciate ligament reconstruction. SAMBBA single-anteromedial bundle biological augmentation
Table 2.
Surgical characteristics
| SAMBBA n = 307 | |
|---|---|
| Indication n (%) | |
| Primary ACLRa | 302 (98.4) |
| Revision ACLRa | 5 (1.6) |
| LEAPa n (%) | |
| Modified lemaire | 14 (4.6) |
| ALLRa | 12 (3.9) |
| Associated high tibial osteotomy n (%) | |
| Medial opening | 1 (0.3) |
| Anterior closing | 1 (0.3) |
|
Native ACL remnant preservation mean ± SD (range), % |
48.3 ± 27.4 (0–90) |
| Meniscal tears n (%) | |
| Total | 143 (46.5) |
| Medial meniscus (MM) | 79 (25.7) |
| Lateral meniscus (LM) | 40 (13.0) |
| MM + LM | 24 (7.8) |
| Cartilaginous lesions, ICRSa grading, n (%) | |
| MCa | |
| 1–2 | 13 (4.2) |
| 3–4 | 7 (2.3) |
| LCa | |
| 1–2 | 2 (0.6) |
| 3–4 | 2 (0.6) |
| FPCa | |
| 1–2 | 17 (5.5) |
| 3–4 | 4 (1.3) |
|
Tourniquet time mean ± SD (range), min |
30.2 ± 8.2 (0–81) |
aACLR anterior cruciate ligament reconstruction, LEAP lateral extra-articular procedure, allr antero-lateral ligament reconstruction, ICRS International Cartilage Repair Society, MC medial compartment, LC lateral compartment, FPC femoro-patellar compartment, SAMBBA single-anteromedial bundle biological augmentation
The mean side-to-side laxity (Rolimeter®, Aircast, Europe) was 0.51 ± 0.89 mm (– 4 to 3). Postoperative radiographs showed a correctly deployed femoral button without soft tissue interposition in all patients (Fig. 3). Regarding potentially button-related complications, nine patients (2.9%) suffered from lateral pain related to ITB irritation (Table 3). Five of them had their symptoms resolve during rehabilitation. Ultrasound-guided corticosteroid infiltration was necessary for four patients after an average delay of 14.5 months. Three patients were then symptom free. Nevertheless, one 45-year-old female patient, a sports education teacher, had persistent pain. She underwent ACLR in January 2019 following a work-related accident and experienced ITB irritation during follow-up. Corticosteroid infiltration was performed in January 2020. Due to ineffective medical treatment, surgical removal of the femoral implant was scheduled in March 2020 but could not be performed until May 2021, 27.5 months after surgery, due to the coronavirus disease 2019 (COVID-19) pandemic. Regarding other complications, 15 patients (4.9%) underwent secondary arthroscopic procedures, including meniscectomy (1.6%), surgery for cyclops syndrome (2.6%) and revision ACLR (0.7%) (Table 4).
Fig. 3.
Frontal, lateral and Schuss view radiographs following ACLR according to the SAMBBA technique. Female, 47-years old. Frontal, lateral and Schuss view radiographs at the nine-month follow-up (right knee). Correct deployment of the femoral button on the lateral cortex was verified on all radiographs. No soft tissue interposition was noticed
Table 3.
Potentially femoral button-related complications
| SAMBBA n = 307 | |
|---|---|
| Femoral button-related lateral pain n (%) | 9 (2.9) |
| Lateral corticosteroid infiltration n (%) | 4 (1.3) |
|
Delay ACLRa—infiltration mean ± SD (range), month |
14.52 ± 4.80 (11.73–21.70) |
| Femoral button removal n (%) | 1 (0.3) |
| Septic arthritis n (%) | 0 |
SAMBBA single-anteromedial bundle biological augmentation
aAnterior cruciate ligament reconstruction
Table 4.
Reoperations performed after ACLR (all reoperations were performed arthroscopically)
| SAMBBA n = 307 | |
|---|---|
| Secondary arthroscopy: total n (%) | 15 (4.9) |
| Meniscectomy n (%) | |
| Medial meniscus | 4 (1.3) |
| Lateral meniscus | 1 (0.3) |
|
Surgery for cyclops syndrome n (%) |
8 (2.6) |
|
Revision ACLRa n (%) |
2 (0.7) |
SAMBBA single-anteromedial bundle biological augmentation
aAnterior cruciate ligament reconstruction
Discussion
The main finding of this study was that intra-articular positioning of the femoral button in ACLR, allowing direct arthroscopic visualization of the implant, prevented improper deployment and soft tissue interposition. Preventing these complications was not achieved at the expense of other complications. No septic arthritis was reported in our cohort. Only 9 patients (2.9%) experienced lateral knee pain related to ITB irritation, and one (0.3%) required implant removal. Our initial hypothesis, is therefore, validated.
Suspensory femoral fixation has become increasingly attractive to surgeons over the last fifteen years [4–7, 25]. Pitfalls have, however, been reported, one of the most criticized being postoperative widening of the tunnels [10–12, 26, 27]. No study has yet demonstrated an unfavorable clinical impact on either subjective scores or objective stability [10, 11, 26, 27]. The hypothesis that this phenomenon is related to the distance between the graft and its fixation was questioned by Choi et al. as no correlation was found between the adjustable femoral button loop length and tunnel widening [28]. Ma et al. even reported greater widening when bioabsorbable interference screws were used [29]. Finally, Pioger et al. showed no influence of tunnel widening on the surgical management of revision ACLR [30]. Single-stage management has always been possible using an outside-in femoral guide, and excellent clinical outcomes have thus been obtained independently of preoperative tunnel position and width. This potential complication of the femoral button should not then call its use into question.
Other complications have been reported, such as improper deployment of the button in the femoral tunnel or its intra-articular migration over time [8, 31, 32]. These complications were mentioned in case reports and had no clinical consequences. More detrimental from a functional point of view, ITB irritation related to the implant has been reported [13, 14]. Both Taketomi et al. and Kawaguchi et al. performed surgical removal of femoral buttons in all patients with disabling lateral pain. [13, 14] Implant positioning too close to the lateral epicondyle or soft tissue interposition were identified as potential risk factors. In the present study, the use of an outside-in femoral guide allowed us to set the button distant from the epicondyle, and systematic shaving of soft tissues along the lateral end of the femoral tunnel limited the interposition of soft tissue beneath the implant. Moreover, no additional safety knot was performed on the button, thus limiting its volume beneath the ITB. We nevertheless, observed nine patients with ITB irritation (2.9%), but only one required removal of the material (0.3%).
The most frequent specific femoral button complication is soft tissue interposition, which is reported in 15 to 24.2% of patients [9, 15–17]. Mae et al. demonstrated a direct correlation with implant migration over time, however, this had no adverse clinical repercussions [15, 33]. Nevertheless, Gürpinar et al. pointed out that an interposition of soft tissues exceeding 3 mm increased the risk of implant migration and significantly decreased postoperative clinical scores [18]. These findings are, however, open to discussion, as they were based on the results of eight patients out of a cohort of 156. Positioning of the button posterior and distal to the epicondyle has also been identified as a risk factor for migration [33]. Given their frequency and potential clinical impact, any means of preventing these complications is welcome.
Intraoperative fluoroscopic control of the femoral button is the most frequently reported solution in the literature [9, 34, 35]. In the event of soft tissue interposition or improper deployment, a new attempt to correctly flip the implant can be attempted after the interposed tissue is bypassed [9]. A larger lateral surgical approach could also be performed over the guide pin to obtain direct visual control of the button [34]. Some authors have used this approach as an accessory arthroscopic portal, allowing its size to be limited while keeping the implant deployment visualized [19, 35]. Mistovitch et al. suggested using this portal routinely without prior fluoroscopic control [19]. According to Kang and Lee, using an outside-in femoral guide would allow the button to be easily found through this portal, in contrast with the transtibial or inside-out procedure [36].
These techniques are efficient and can limit potential complications related to the femoral button [9, 19, 34, 35]. However, intraoperative fluoroscopy is irradiating for both the patient and the surgeon and requires the involvement of trained personnel [37, 38]. Moreover, the use of an additional surgical approach is invasive and could increase the risk of sepsis. Both increase the overall surgical time. Checking the correct deployment of the implant by manual testing alone would prevent these pitfalls, but O'Brien et al. demonstrated the poor reliability of manual testing, with only 74.5% of femoral buttons having correct positioning [9]. Another option would be to check for proper passage of the button through the femoral tunnel under intra-articular arthroscopic control. Nag and Gupta proposed pushing the implant through the tunnel using a guide pin under visual control until a loss of resistance occurred, indicating the passage of the femoral cortex [39]. However, this technique does not allow direct visualization of button deployment.
The present technique allows for this through direct arthroscopic control in the lateral gutter. It also prevents soft tissue interposition by systematic shaving of tissues along the lateral end of the femoral tunnel. Easy to handle and reproducible, it is both a nonirradiating and noninvasive solution. The main concern, although rare (nine patients, 2.9%), was ITB irritation related to the implant. Most symptomatic patients (eight out of nine, 88.9%) were successfully treated with medical treatment consisting of well-managed rehabilitation and ultrasound-guided corticosteroid infiltration in patients where symptoms persisted. Only one patient (0.3%) required surgical removal of the implant, providing immediate relief of pain.
The retrospective design is the main limitation of the present study. However, a large sample size was obtained, and this is, to our knowledge, the largest cohort on the subject in the literature. Second, all data were collected from the SANTI study group database. Complications managed in other institutions were therefore not taken into account. However, all patients involved in the present study were followed up for at least 14.27 months after ACLR. The most feared complications, namely, septic arthritis and ITB irritation, would have occurred before this time. This also explains why a minimum of one year of follow-up seemed sufficient to us. Finally, the present study did not include a control group. The objective of this study was to demonstrate the reliability of intra-articular positioning of the femoral button. Therefore, comparison with another technique did not seem relevant, as only complications of this specific device were being examined.
Conclusions
Arthroscopic confirmation of femoral button deployment prevents soft tissue interposition without specific complications. This technique is reproducible, non-irradiating and non-invasive.
Funding
This article has no funding.
Declarations
Conflict of interest
BSC and MT are Arthrex consultants. SG, AF and AC received a fellowship grant during the time this article was written.
Ethical approval
Institutional Review Board Approval: COS-RGDS-2021-01-004-SONNERYCOTTET-B.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Järvinen TLN, Alami GB, Karlsson J. Anterior cruciate ligament graft fixation—a myth busted? Arthrosc J Arthrosc Relat Surg. 2010;26:681–684. doi: 10.1016/j.arthro.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 2.Lubowitz JH, Guttmann D, Järvinen TLN, Kousa P, Kannus P, Järvinen M, Noyes FR, Stannard JP. Letters to the Editor. Am J Sports Med. 2003;31:811–814. doi: 10.1177/03635465030310053101. [DOI] [Google Scholar]
- 3.Kurosaka M, Yoshiya S, Andrish JT. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15:225–229. doi: 10.1177/036354658701500306. [DOI] [PubMed] [Google Scholar]
- 4.Eysturoy NH, Nissen KA, Nielsen T, Lind M. the influence of graft fixation methods on revision rates after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2018;46:524–530. doi: 10.1177/0363546517748924. [DOI] [PubMed] [Google Scholar]
- 5.Lubowitz JH, Ahmad CS, Amhad CH, Anderson K. All-inside anterior cruciate ligament graft-link technique: second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717–727. doi: 10.1016/j.arthro.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Persson A, Kjellsen AB, Fjeldsgaard K, Engebretsen L, Espehaug B, Fevang JM. Registry data highlight increased revision rates for endobutton/biosure HA in ACL reconstruction with hamstring tendon autograft: a nationwide cohort study from the Norwegian Knee Ligament Registry, 2004–2013. Am J Sports Med. 2015;43:2182–2188. doi: 10.1177/0363546515584757. [DOI] [PubMed] [Google Scholar]
- 7.Schurz M, Tiefenboeck TM, Winnisch M, Syre S, Plachel F, Steiner G, Hajdu S, Hofbauer M. Clinical and functional outcome of all-inside anterior cruciate ligament reconstruction at a minimum of 2 years’ follow-up. Arthroscopy. 2016;32:332–337. doi: 10.1016/j.arthro.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 8.Karaoglu S, Halici M, Baktir A. An unidentified pitfall of Endobutton use: case report. Knee Surg Sports Traumatol Arthrosc. 2002;10:247–249. doi: 10.1007/s00167-002-0287-x. [DOI] [PubMed] [Google Scholar]
- 9.O’Brien DF, Fones L, Stoj V, Edgar C, Coyner K, Arciero RA. Confirming proper button deployment of suspensory fixation during ACL reconstruction. Orthop J Sports Med. 2021;9:2325967120974349. doi: 10.1177/2325967120974349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baumfeld JA, Diduch DR, Rubino LJ, Hart JA, Miller MD, Barr MS, Hart JM. Tunnel widening following anterior cruciate ligament reconstruction using hamstring autograft: a comparison between double cross-pin and suspensory graft fixation. Knee Surg Sports Traumatol Arthrosc. 2008;16:1108–1113. doi: 10.1007/s00167-008-0606-y. [DOI] [PubMed] [Google Scholar]
- 11.Fauno P, Kaalund S. Tunnel widening after hamstring anterior cruciate ligament reconstruction is influenced by the type of graft fixation used: a prospective randomized study. Arthroscopy. 2005;21:1337–1341. doi: 10.1016/j.arthro.2005.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Sabat D, Kundu K, Arora S, Kumar V. Tunnel widening after anterior cruciate ligament reconstruction: a prospective randomized computed tomography-based study comparing 2 different femoral fixation methods for hamstring graft. Arthroscopy. 2011;27:776–783. doi: 10.1016/j.arthro.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 13.Kawaguchi K, Kuribayashi S, Nakayama S, Nakazato K, Fukubayashi T, Okinaga S. Lateral knee pain after outside-in anatomic double-bundle anterior cruciate ligament reconstruction using the tightrope RT. Knee Surg Relat Res. 2016;28:83–87. doi: 10.5792/ksrr.2016.28.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Taketomi S, Inui H, Hirota J, Nakamura K, Sanada T, Masuda H, Tanaka S, Nakagawa T. Iliotibial band irritation caused by the EndoButton after anatomic double-bundle anterior cruciate ligament reconstruction: report of two cases. Knee. 2013;20:291–294. doi: 10.1016/j.knee.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Mae T, Kuroda S, Matsumoto N, Yoneda M, Nakata K, Yoshikawa H, Shino K. Migration of EndoButton after anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:1528–1535. doi: 10.1016/j.arthro.2011.06.024. [DOI] [PubMed] [Google Scholar]
- 16.Simonian PT, Behr CT, Stechschulte DJ, Wickiewicz TL, Warren RF. Potential pitfall of the EndoButton. Arthroscopy. 1998;14:66–69. doi: 10.1016/S0749-8063(98)70122-7. [DOI] [PubMed] [Google Scholar]
- 17.Taketomi S, Inui H, Nakamura K, Yamagami R, Tahara K, Sanada T, Masuda H, Tanaka S, Nakagawa T. Secure fixation of femoral bone plug with a suspensory button in anatomical anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Joints. 2015;3:102–108. doi: 10.11138/jts/2015.3.3.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gürpınar T, Polat B, Eren M, Çarkçı E, Özyalvaç ON, Erdoğan S. The effect of soft tissue interposition of the Endobutton on clinical results and on its postoperative migration after single-bundle anterior cruciate ligament reconstruction. Knee. 2020;27:1980–1987. doi: 10.1016/j.knee.2020.10.008. [DOI] [PubMed] [Google Scholar]
- 19.Mistovich RJ, O’Toole POJ, Ganley TJ. Pediatric anterior cruciate ligament femoral fixation: the trans-iliotibial band endoscopic portal for direct visualization of ideal button placement. Arthrosc Tech. 2014;3:e335–338. doi: 10.1016/j.eats.2014.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sonnery-Cottet B, Freychet B, Murphy CG, Pupim BHB, Thaunat M. Anterior cruciate ligament reconstruction and preservation: the single-anteromedial bundle biological augmentation (SAMBBA) technique. Arthrosc Tech. 2014;3:e689–693. doi: 10.1016/j.eats.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sonnery-Cottet B, Rezende FC, Martins Neto A, Fayard JM, Thaunat M, Kader DF. Arthroscopically confirmed femoral button deployment. Arthrosc Tech. 2014;3:e309–312. doi: 10.1016/j.eats.2014.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papachristou G, Nikolaou V, Efstathopoulos N, Sourlas J, Lazarettos J, Frangia K, Papalois A. ACL reconstruction with semitendinosus tendon autograft without detachment of its tibial insertion: a histologic study in a rabbit model. Knee Surg Sports Traumatol Arthrosc. 2007;15:1175–1180. doi: 10.1007/s00167-007-0374-0. [DOI] [PubMed] [Google Scholar]
- 23.Kim S-G, Kurosawa H, Sakuraba K, Ikeda H, Takazawa S, Takazawa Y. Development and application of an inside-to-out drill bit for anterior cruciate ligament reconstruction. Arthroscopy. 2005;21:1012. doi: 10.1016/j.arthro.2005.05.032. [DOI] [PubMed] [Google Scholar]
- 24.Jesani S, Getgood A. Modified lemaire lateral extra-articular tenodesis augmentation of anterior cruciate ligament reconstruction. JBJS Essent Surg Tech. 2019;9(4):e41.1. doi: 10.2106/JBJS.ST.19.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim HS, Seon JK, Jo AR. Current trends in anterior cruciate ligament reconstruction. Knee Surg Relat Res. 2013;25:165–173. doi: 10.5792/ksrr.2013.25.4.165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kong C-G, In Y, Kim G-H, Ahn C-Y. Cross pins versus endobutton femoral fixation in hamstring anterior cruciate ligament reconstruction: minimum 4-year follow-up. Knee Surg Relat Res. 2012;24:34–39. doi: 10.5792/ksrr.2012.24.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Saccomanno MF, Shin JJ, Mascarenhas R, Haro M, Verma NN, Cole BJ, Bach BR. Clinical and functional outcomes after anterior cruciate ligament reconstruction using cortical button fixation versus transfemoral suspensory fixation: a systematic review of randomized controlled trials. Arthroscopy. 2014;30:1491–1498. doi: 10.1016/j.arthro.2014.05.028. [DOI] [PubMed] [Google Scholar]
- 28.Choi N-H, Oh J-S, Jung S-H, Victoroff BN. Correlation between endobutton loop length and tunnel widening after hamstring anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:101–106. doi: 10.1177/0363546512466384. [DOI] [PubMed] [Google Scholar]
- 29.Ma CB, Francis K, Towers J, Irrgang J, Fu FH, Harner CH. Hamstring anterior cruciate ligament reconstruction: a comparison of bioabsorbable interference screw and endobutton-post fixation. Arthroscopy. 2004;20:122–128. doi: 10.1016/j.arthro.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 30.Pioger C, Saithna A, Rayes J, Haidar IM, Fradin T, Ngbilo C, Vieira TD, Cavaignac E, Sonnery-Cottet B. Influence of preoperative tunnel widening on the outcomes of a single stage-only approach to every revision anterior cruciate ligament reconstruction: an analysis of 409 consecutive patients from the SANTI study group. Am J Sports Med. 2021;49(6):1431–1440. doi: 10.1177/0363546521996389. [DOI] [PubMed] [Google Scholar]
- 31.Muneta T, Yagishita K, Kurihara Y, Sekiya I. Intra-articular detachment of the Endobutton more than 18 months after anterior cruciate ligament reconstruction. Arthroscopy. 1999;15:775–778. doi: 10.1016/S0749-8063(99)70013-7. [DOI] [PubMed] [Google Scholar]
- 32.Yanmiş I, Tunay S, Oğuz E, Yildiz C, Ozkan H, Kirdemir V. Dropping of an EndoButton into the knee joint 2 years after anterior cruciate ligament repair using proximal fixation methods. Arthroscopy. 2004;20:641–643. doi: 10.1016/j.arthro.2004.03.016. [DOI] [PubMed] [Google Scholar]
- 33.Uchida R, Mae T, Matsumoto N, Kuroda S, Toritsuka Y, Shino K. The effect of cortical button location on its post-operative migration in anatomical double-bundle anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2014;22:1047–1054. doi: 10.1007/s00167-013-2458-3. [DOI] [PubMed] [Google Scholar]
- 34.Balldin BC, Nuelle CW, DeBerardino TM. Is intraoperative fluoroscopy necessary to confirm device position for femoral-sided cortical suspensory fixation during anterior cruciate ligament reconstruction? J Knee Surg. 2020;33:265–269. doi: 10.1055/s-0039-1678523. [DOI] [PubMed] [Google Scholar]
- 35.Ohnishi Y, Chang A, Utsunomiya H, Suzuki H, Nakamura E, Sakai A, Uchida S. Arthroscopic technique to reduce suture button migration during anterior cruciate ligament reconstruction procedure. Arthrosc Tech. 2017;6:e1927–e1931. doi: 10.1016/j.eats.2017.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kang SG, Lee YS. Arthroscopic control for safe and secure seating of suspensory devices for femoral fixation in anterior cruciate ligament reconstruction using three different techniques. Knee Surg Relat Res. 2017;29:33–38. doi: 10.5792/ksrr.16.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hayda RA, Hsu RY, DePasse JM, Gil JA. Radiation exposure and health risks for orthopaedic surgeons. J Am Acad Orthop Surg. 2018;26:268–277. doi: 10.5435/JAAOS-D-16-00342. [DOI] [PubMed] [Google Scholar]
- 38.Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005;13:69–76. doi: 10.5435/00124635-200501000-00009. [DOI] [PubMed] [Google Scholar]
- 39.Nag HL, Gupta H. Seating of tightrope RT button under direct arthroscopic visualization in anterior cruciate ligament reconstruction to prevent potential complications. Arthrosc Tech. 2012;1:e83–85. doi: 10.1016/j.eats.2012.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Initiative STROBE. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]