Abstract
Objectives
Triage is a critical component of the pandemic response. It affects morbidity, mortality and how effectively the available healthcare resources are used. In a number of nations the pandemic has sponsored the adoption of novel, online, patient-led triage systems—often referred to as COVID-19 symptom checkers. The current safety and reliability of these new automated triage systems remain unknown.
Methods
We tested six symptom checkers currently in use as triage tools at a national level against 52 cases simulating COVID-19 of various severities to determine if the symptom checkers appropriately triage time-critical cases onward to healthcare contact. We further analysed and compared each symptom checker to determine the discretionary aspects of triage decision-making that govern the automated advice generated.
Results
Of the 52 clinical presentations, the absolute rate of onward referral to any form of healthcare contact was: Singapore 100%, the USA 67%, Wales 65%, England 62%, Scotland 54% and Northern Ireland 46%. Triage decisions were broadly based on either estimates of ‘risk’ or ‘disease severity’. Risk-based symptom checkers were more reliable, with severity-based symptom checkers often triaging time-critical cases to stay home without clinical contact or follow-up.
Conclusion
The COVID-19 symptom checkers analysed here were unable to reliably discriminate between mild and severe COVID-19. Risk-based symptom checkers may hold some promise of contributing to pandemic case management, while severity-based symptom checkers—the CDC and NHS 111 versions—confer too much risk to both public and healthcare services to be deemed a viable option for COVID-19 triage.
Keywords: clinical governance, COVID-19, decision making, computer-assisted, delivery of health care
Summary.
What is already known?
Symptom checkers have been deployed at a national level in a number of countries to support the pandemic response.
There are no quality, safety or efficacy studies supporting the use of COVID-19 symptom checkers as triage tools.
What does this paper add?
The COVID-19 symptom checkers analysed here are currently in use at a national level as stand-alone triage services. They are all freely accessible to the public.
Out of the symptom checkers analysed, only the UK version (NHS 111 COVID-19 Symptom Checker) has been formally integrated into the national clinical pathway.
None of the symptom checkers analysed here could reliably distinguish between mild and severe COVID-19.
Introduction
Symptom checkers are online platforms where the public can enter details of their illness, answer set questions about their symptoms and then receive advice on what to do next. During the pandemic, many nations have deployed symptom checkers to help identify potential COVID-19 cases and provide advice to the public. Some nations have gone further, using symptom checkers in place of more typical clinical triage systems.1
Despite a number of studies highlighting the diagnostic sensitivity of various online COVID-19 symptom checkers, we could find no studies (apart from our previous analysis)2 examining the safety and reliability of online COVID-19 symptom checkers as a standalone triage tool.
The difference is stark. On the one hand, these accessible web-based questionnaires can direct potential cases toward SARS-CoV-2 testing services—answering the question: should you be tested? In such circumstances, symptom checkers act more as a prompt, conveying the national advice. On the other hand, there is another category of symptom checkers attempting to answer a much more complicated question: do you need medical help?
It is quite an ask, of an automated system. And the stakes are high. There is the unavoidable direct morbidity and mortality impact when triaging acute medical problems.3 4 There is also an operational consideration, whereby delaying treatment in time-critical conditions leads to a higher overall healthcare burden.3–6
Online COVID-19 symptom checkers may carry the potential to offset the inevitable high healthcare demands of pandemic management, allowing valuable resources to be focused on those with real clinical need. This benefit can only be realised if the symptom checker successfully triages COVID-19 pneumonia (and other serious conditions mimicking COVID-19) on to further care early enough for maximal treatment benefits to be achieved. Missing the opportunity to prevent disease progression will invariably lead to higher mortality,4 6 delayed recovery (eg, higher rates of long COVID-19)7 and a more lengthy inpatient stay.4 6 There is a very real possibility that symptom checkers, if inappropriately used, can significantly increase the healthcare burden associated with COVID-19—compromising healthcare capacity sooner than is necessary.2 5 Both at a patient level and operational level, quality and efficacy studies are essential if clinical activities are to be replaced or even augmented with such patient-led, automated clinical services.
Back in April 2020, we undertook an analysis on national symptom checkers from the UK, USA, Singapore and Japan. At that time, the results of our case-simulation study revealed a low rate of onward referral for both the UK’s ‘111 COVID-19 Symptom Checker’ and the US’s ‘CDC Coronavirus Symptom Checker’—44% and 38%, respectively. It was noted that both symptom checkers triaged simulated cases of severe COVID-19 pneumonia, bacterial pneumonia and sepsis, to stay home with no further healthcare contact.2 In short, both the US and UK symptom checkers maintained a high threshold to refer patients onward for healthcare contact.
During this previous analysis, we compared and contrasted the four symptom checkers, looking specifically for points of divergence. The most notable difference was whether known COVID-19 disease ‘risk factors’ or an estimated ‘disease severity’ were used to calculate triage disposition. Both Singapore’s and Japan’s symptom checkers focused specifically on risk factors—age, duration of symptoms, the presence of breathlessness and comorbidities—and made no attempt to quantify disease severity. We have termed these, ‘risk-based symptom checkers’. Both the US and UK symptom checkers, in April 2020, relied more on qualitative questions designed to estimate how severe a case was, and made no account of the most consistent risk factors—age, duration of symptoms or the presence of breathlessness. In addition, only moderately severe comorbidities affected the CDC symptom checker triage decision and only ‘shielding category’ comorbidities affected triage dispositions in the NHS 111 symptom checker.2 We have termed these, ‘severity-based symptom checkers’.
At the time of our initial study, the impact of the CDC symptom checker on actual case presentations to US hospitals was unknown. However, the ‘NHS 111 COVID-19 Symptom Checker’ was a known gatekeeper for UK patients with suspected or confirmed COVID-19.8–11 As such, the symptom checker’s ‘decision’ to triage cases simulating time critical urgent medical problems—severe COVID-19, bacterial pneumonia and sepsis—to remain at home was considered by the authors as unsafe. No data existed on internal or external quality assurance studies, further compounding the concerns regarding the use of the NHS 111 COVID-19 symptom checker and patient safety. These concerns were raised with NHS Digital—the body responsible for the NHS 111 symptom checker—both prior to publication and following. NHS Digital considered the concerns to be historic and not representative of the improved version of the symptom checker.12 We, therefore, undertook a repeat analysis in June 2021.
Methods
During the first week in June 2021, we undertook a follow-up analysis on national symptom checkers. In summary, we generated four distinct patient scenarios relating to COVID-19. The four scenarios included were fever with cough, comorbidity with fever and cough, immunosuppression with fever and cough, and shortness of breath with fever. We varied patient age, duration of symptoms and the severity of symptoms. In total, this generated 52 separate case simulations, including mild, moderate, severe and critical COVID-19, and COVID mimickers such as bacterial pneumonia and sepsis. Each case was applied by a single investigator (DG) to each symptom checker and the triage decision was recorded. We then calculated the total referral ratio (ie, proportion of all 52 cases that were referred for clinical contact, regardless of the level of designation—call centre, primary care provider, or emergency department). A percentage ratio was generated of total referrals made by each symptom checker. We also noted specific features of each symptom checker for comparison.
In addition to the methods as described previously, we also completed analysis of symptom checkers from Scotland,13 Wales14 and Northern Ireland,15 and thus differentiated the previously analysed NHS England symptom checker from the other three nations.
A more detailed methodology is explained by Mansab et al.2
Results
Of the four nations included in the initial analysis of April 2020, Singapore, the USA and all four nations within the UK continue to use symptom checkers as part of the national response to COVID-19. Japan was no longer using an accessible symptom checker, it being replaced by a flow chart. As such, it was excluded from further analysis.
Triage dispositions were slightly different for each symptom checker, but generally followed: stay home, or contact service provider/General Practioner (GP)/111, or go straight to emergency department/999.
The current analysis was undertaken during a relatively low prevalence time, when COVID-19 inpatient burden was relatively low (table 1).16–18
Table 1.
National inpatient healthcare burden and key population statistics. Source: World Bank and WHO
| Singapore | USA | UK | |
| Population data | |||
| Patients currently admitted to hospital per 10 000 inhabitants (rate as per April 2020) |
0.38 (2.23) |
0.21 (0.43) |
0.3 (2.29) |
| Mean national age (years) | 44.2 | 38.4 | 40.5 |
| Gross Domestic Product per capita (thousands of US dollars) | 59.8 | 63.5 | 40.3 |
| Physicians per 10 000 head of capita | 24 | 25 | 28 |
| Total case fatality rate (%) | 0.05 | 1.8 | 2.8 |
Referral ratio
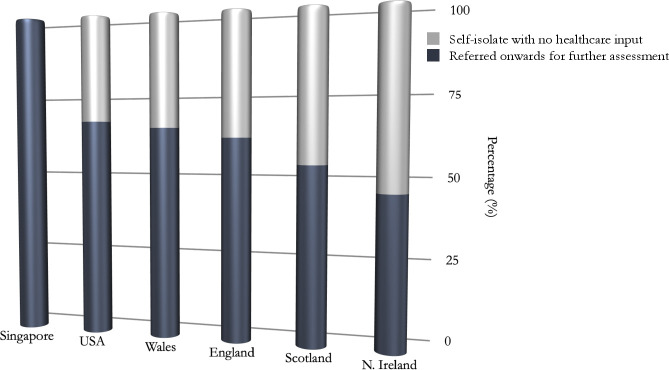
The rates of onward referral to any further healthcare contact for each national symptom checker were: Singapore 100%, the USA 67%, Wales 65%, England 62%, Scotland 54% and Northern Ireland 46% (figure 1). Previous referral rates in April 2020 were: Singapore 88%, the USA 38% and England 44%. For the triage disposition of individual case simulations, see online supplemental data.
Figure 1.
Percentage ratio of absolute onward referrals of each national symptom checker. Black represents the total percentage of cases triaged onward to further healthcare contact. Grey represents the percentage of cases triaged to remain at home with no further planned healthcare follow-up.
bmjhci-2021-100448supp001.pdf (116.2KB, pdf)
Specific features
The Singapore symptom checker currently refers all cases for a same day assessment at one of the nation’s public health clinics. It continues to refer all patients with any degree of breathing problems directly to the emergency department (scenario 4, online supplemental material).
The US (CDC) symptom checker referred twice as many cases on to clinical care than it did the year before. Notably, the advice for those referred had changed from ‘contact medical provider within 24 hours’ to ‘contact medical provider as soon as possible’. Age was also now a considered risk factor for disease severity with all patients over the age of 65 years with suspected COVID-19 being advised to contact their medical provider regardless of disease severity or other comorbidity. The CDC symptom checker continued to triage those under 65 years of age with mild to moderate shortness of breath to stay home with no further clinical contact (scenario 4, online supplemental material).
The UK symptom checkers do not account for age in the triage decision in the case simulations undertaken, except for NHS Wales. NHS Wales ‘111’ symptom checker triaged all cases over the age of 70 years onward to call ‘111’. Scotland, Northern Ireland and England continued to, for example, triage a 72 years old with cough and fever for 7 days to stay home with no healthcare contact or follow-up (scenario 1, online supplemental material).
In comparison to the year previously, the NHS England symptom checker now triaged any case with the subjective sense of shortness of breath onward to further healthcare contact (‘call 111’ for cases with self-rated mild to moderate shortness of breath, and the emergency department for severe shortness of breath). If, though, shortness of breath is a secondary symptom (ie, feeling flu-like with shortness of breath), then patients are still advised to stay home, unless self-identified as severe (table 2).
Table 2.
Summary of the national COVID-19 symptom checkers’ triage criteria
| Triage criteria | Risk-based symptom checker | Severity-based symptom checker | |
| Singapore | CDC | NHS 111 | |
| Duration of symptoms | Duration of symptoms affects triage outcomes. Patients with symptoms over 4 days are always triaged in to further care. |
Duration of symptoms does not alter triage outcomes. No length of illness leads to triage in to further healthcare contact. |
Duration of symptoms does not alter triage outcomes. No length of illness leads to triage in to further healthcare contact. |
| Age | Age affects triage outcomes. Cases over the age of 65 years are always triaged on for further healthcare contact. During times of low SARS-CoV-2 healthcare burden, age is removed as a restriction to further clinical assessment. |
Age affects triage outcomes Cases over the age of 65 years are now triaged on to further healthcare contact. |
Age has no bearing on triage advice for the NHS symptom checkers in England, Scotland and Northern Ireland. NHS Wales triages all cases over the age of 70 years to contact ‘111’. |
| Comorbidity | Comorbidity affects triage outcomes. Cases with any comorbidity are triaged on to further care. |
Comorbidity affects triage outcomes. Cases with moderately severe comorbidities are triaged on for further healthcare contact. |
Comorbidity affects triage outcomes. The type of comorbidity triggering triage on to further healthcare contact differs across the four nations.* |
| Shortness of breath | Any degree of shortness of breath is triaged straight to the emergency department. | Patients with severe breathlessness are triaged to the emergency department. Patients with mild to moderate shortness of breath are advised to stay home with no clinical follow-up. |
Patients with severe breathlessness are triaged to the emergency department. NHS England triage cases in to further care if self-rated breathlessness is mild to moderate and is the primary symptom, but not if a secondary symptom. Scotland, Northern Ireland and Wales triage all patients self-reporting breathlessness to urgent ‘111’/General Practioner. If severe, the patient is advised to call ‘999’. |
*NHS Scotland only triages cases with comorbidities that are on the shielding category list for further care. NHS Northern Ireland only triages cases with immunosuppression or conditions that have become more difficult to control since symptoms began. NHS Wales relies on shielding categories and also includes diabetes and pregnancy with heart conditions. NHS England use shielding categories and also consider immunosuppression, diabetes, heart disease, respiratory disease, kidney failure, liver disease or neurological disease.
Discussion
The WHO guidelines on triage recommend that all patients with suspected or confirmed COVID-19 are clinically triaged.19 In many countries, this proves challenging due to national policy, healthcare accessibility, healthcare resources and the level of community transmission of SARS-CoV-2. Most patients with COVID-19 do not develop complicated illness and will resolve the infection without clinical intervention. Successful clinical pathways are able to pick out the COVID-19 pneumonia reliably and, crucially, early enough for basic medical care to prevent progression of disease.
There have been noticeable improvements in the symptom checkers that were first analysed in April 2020. Notably, the overall referral rate onward to healthcare contact has increased in the USA, UK and Singapore. Other features of the symptom checkers have also been improved. Singapore has included a question on immunosuppression, although it still does not confer such patients to more urgent care. The CDC coronavirus symptom checker has now included age as a defining risk factor. Most symptom checkers have expanded the list of comorbidities affecting triage decisions. And while the seriousness of breathlessness is given variable attention by each national symptom checker, all seem to now give it more weight in triage decisions. While these changes move towards re-establishing the usual standards of care for patients with COVID-19, our results indicate that COVID-19 symptom checkers are too unreliable in discriminating mild from severe COVID-19, and, as such, are likely to confer too great a risk to public, and, if used in place of clinical triage, will only weaken the healthcare response to the pandemic.20
Specifics
Whether the CDC coronavirus symptom checker has in fact worsened outcomes for the USA or not remains unknown. It has not been formally integrated into the US healthcare system or COVID-19 clinical pathways. The fact it functions as a stand-alone patient-led triage service and is freely accessible to the public is concerning. While not formally or preferentially directed to the symptom checker, the US public can seek clinical advice from the automated service, and thereby, potentially—in the patient’s mind—negate the need to undertake actual clinical triage. Given it cannot reliably differentiate between mild and severe COVID-19, any reassurance provided is neither dependable nor evidence based. For example, the CDC coronavirus symptom checker still advises the 63 years old with a 7-day history of persistent fever and worsening cough to remain at home without contacting their healthcare service provider. In the absence of any discoverable quality and safety studies supporting its use, it would seem prudent to discontinue the use of the CDC coronavirus symptom checker until the CDC can prove its efficacy and safety, as would be the case for any diagnostic test.
Singapore remains consistent in its approach to the clinical management of COVID-19.21 All suspected cases of COVID-19 are clinically assessed by a physician and followed-up by primary care.22 This is consistent with the WHO technical guidelines and clinical recommendations for triage and management of COVID-19.19 During our previous analysis in April 2020, Singapore was suffering a surge of COVID-19 infections. The symptom checker was then set to advise the young, non-breathless patient with no comorbidities and a short duration of illness to self-isolate and contact the public health clinic if symptoms worsened or had not improved by day 4.2 This remains a compromise to normal clinical care but may have achieved a low-risk reduction in healthcare burden. Now, with SARS-CoV-2 prevalence less than in April 2020, all suspected cases are clinically assessed.
Unlike the CDC and Singapore COVID-19 symptom checkers, the NHS ‘111’ symptom checkers have a clear and critical role in the national clinical response to COVID-19.8–11 Current advice in the UK to the public (including from contact tracers) is to self-isolate if COVID-19 is suspected or confirmed and if concerned about symptoms to use NHS 111 online services or call ‘111’.23 Altogether this has generated—even during the low SARS-CoV-2 prevalence period of this analysis—around 30 000 online triages per month in England, including around 900 online triages in those 70 years old and over.24 The NHS 111 COVID-19 symptom checkers act as a gatekeeper for further clinical contact. As such, the reliability of the UK’s symptom checkers and the triage criteria set by NHS 111 is critical to COVID-19 patient outcomes and associated healthcare usage.
The NHS England symptom checker has increased the rate of onward referral since April 2020 and now refers patients with self-rated mild or moderate breathing difficulties to call ‘111’. From both a patient safety and healthcare burden perspective, this is a welcomed improvement. However, the NHS England symptom checker (and to some degree the NHS Wales symptom checker) continues to attempt to quantify disease severity with subjective questions and qualifiers likely to cause under-reporting of true disease severity, as it did previously.2 It fails to reliably identify severe COVID-19 or other time-critical COVID mimickers.
Only the NHS Wales symptom checker accounted for age in the triage decision of the cases simulated. The reason for NHS Scotland, England and Northern Ireland not accounting for age—the most reliable predictor of disease severity—remains unclear.
None of the NHS symptom checkers account for ‘silent hypoxia’ (case scenario 1, online supplemental data). Silent hypoxia is the presence of hypoxia (low blood oxygen levels) without any sensation of breathlessness. It indicates severe or critical COVID-19 pneumonia and requires immediate inpatient care. Silent hypoxia affects up to one-third of patients presenting to hospital and carries a poorer prognosis.25 26 The inability of the NHS 111 symptom checkers to identify cases suffering silent hypoxia is likely a terminal limitation to the success of such severity-based symptom checkers as viable triage tools for COVID-19.
The attempt of the NHS 111 COVID-19 symptom checker to determine if COVID-19 is present, then to assign a severity level (ie, non-severe), constitutes a diagnostic process.27 Given the NHS England symptom checker (and all UK national symptom checkers) then provide the clinical advice to ‘self-isolate’ and detailed advice on how to manage symptoms such as cough and breathlessness at home,28 it breaches the boundary between simple signposting (simply deciding who is the most appropriate next healthcare contact) and ventures into the area of diagnosis and clinical management (deciding what treatment is appropriate based on an assessment). The NHS 111 COVID-19 symptom checker should then, at the very minimum, be subject to the same quality standards as any other diagnostic test, including national regulation.
As the UK clinical COVID-19 pathway is heavily reliant on such symptom checkers, together with the subsequent diversion of patients away from actual clinical triage, the NHS 111 symptom checkers are likely to be contributing to the UK’s poor pandemic response, including the high morbidity and mortality. Also of growing concern is the impact the NHS 111 symptom checkers are likely to have on the resilience of society to tolerate background levels of SARS-CoV-2 and post-pneumonia complications (eg, long COVID-19) by delaying presentation of COVID-19 pneumonia to timely, appropriate medical care.
Given the NHS ‘111’ symptom checkers have ventured into diagnosis and, arguably, clinical management, are currently gatekeepers to further healthcare access, fail to reliably triage severe COVID-19 on to further care, fail to account for age as a risk factor (except NHS Wales) and are likely to miss COVID-19 mimickers such as bacterial pneumonia, considerable improvements are needed to render the current NHS 111 COVID-19 symptom checkers fit for purpose.
Future Direction
The use of symptom checkers as part of the national clinical care pathway for COVID-19 (and future pandemics) requires considerably more research and validation.29 Currently, none of the symptom checkers pose a viable option in replacing clinical triage, and as such, effort should focus on resourcing clinical triage services.
Data relating to the use of symptom checkers and the effects these have on future healthcare burden have not yet been analysed. At an operational level, the possibility of severity-based symptom checkers leading to an increase in healthcare burden, including an increase in high-dependency admissions, should sponsor caution and an urgent review of any care pathways depending on such forms of patient-led triage. Our analysis suggests, severity-based COVID-19 symptom checkers (such as the NHS 111 or CDC versions) are likely to increase the healthcare burden associated with the pandemic (in comparison to clinically led, remote triage).
There is the equally challenging obstacle of national versus local triage to overcome. The current NHS 111 symptom checker triages nationally using the same referral thresholds. This may have contributed to the disproportionate healthcare activity across the UK.27 Where a national symptom checker is ‘set’ to respond to critical demand in, for example, London, those using the symptom checker in an area of low demand, for example, the Lake District, will also be held to the same, compromised and rationed access to healthcare. This goes against the principles of triage, in that triage decisions must be responsive to resource availability. It is not justifiable—or logistically savvy—to ration access to healthcare preemptively or without a definitive need to.
In the short term—pending further safety studies—a ‘risk-based symptom checker’ may provide a possible low-risk solution to signposting potential COVID-19 cases, under pandemic conditions. The usual standard remains an actual clinical assessment, but where healthcare resources are insufficient for such a standard of care, an untested symptom checker that can be adjusted in response to risk and demand would be preferable to an untested symptom checker attempting to determine clinical severity from an automated algorithm. A national symptom checker may still have a role in risk stratifying, and with the benefit of postcode localisation, there may be an ability to adjust the ‘risk necessary to take’ more accurately and based on local demands. Such a national service providing local risk stratification must be dynamic and responsive to demands, be under constant data collection and review, and be viewed as a considerable compromise to usual standards of care.
Whatever future version of COVID-19 symptom checkers manifest, they must be designed with the intention of detecting progressive COVID-19 or those at risk of severe disease, not designed with the intention of preventing healthcare contact. Triage itself is not resource saving. But the effort invested in the triage process yields high returns when cases of progressive COVID-19 pneumonia are detected early enough to avoid costly, protracted and complicated admissions. Triage systems must be viewed for what they are: an opportunity to maximise the use of available resources to prevent death, avoid disability and improve healthcare resilience.
Conclusion
The use of symptom checkers to triage patients during a pandemic or major incident is novel and untested. Our case simulation study provides little reassurance for their ongoing use. Even during a period of low healthcare burden, the symptom checkers deployed by both the USA and UK maintained a high threshold for onward referral. Neither symptom checker reliably triaged treatable, time-critical cases in to healthcare contact or follow-up and were unable to consistently differentiate mild from severe COVID-19. Of further concern, age is not factored in the triage decisions of the NHS 111 symptom checkers (except NHS Wales)—an unusual practice in clinical triage and well-below national and international standards of care.
Beyond the patient safety concerns, there is no evidence that COVID-19 symptom checkers reduce the healthcare burden associated with the pandemic. Our results suggest, by delaying the presentation of time-critical cases to medical care, it is quite likely the NHS 111 symptom checkers increase the healthcare burden associated with the SARS-CoV-2 pandemic in the UK.
In the absence of any safety, efficacy or quality assurance studies to support the use of symptom checkers as triage tools, our results necessitate a recommendation for the NHS 111 symptom checker and CDC coronavirus symptom checker to be subject to further analysis prior to their ongoing use in COVID-19 clinical care pathways. The stakes of patient triage are simply too high, and the reliability of symptom checkers is simply too poor, to justify their ongoing use.
Footnotes
Contributors: All authors contributed to the conception, methodology and analysis and did final review and edit. FM undertook the majority of the write-up. DG undertook edits and contributed to the write-up and revision of the manuscript. DG is the guarantor of the study.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Morse KE, Ostberg NP, Jones VG, et al. Use characteristics and triage acuity of a digital symptom Checker in a large integrated health system: population-based descriptive study. J Med Internet Res 2020;22:e20549. 10.2196/20549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mansab F, Bhatti S, Goyal D. Performance of national COVID-19 'symptom checkers': a comparative case simulation study. BMJ Health Care Inform 2021;28:e100187. 10.1136/bmjhci-2020-100187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lim WS, Baudouin SV, George RC, et al. Bts guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax 2009;64 Suppl 3:iii1–55. 10.1136/thx.2009.121434 [DOI] [PubMed] [Google Scholar]
- 4.Phua J, Dean NC, Guo Q, et al. Severe community-acquired pneumonia: timely management measures in the first 24 hours. Crit Care 2016;20:237. 10.1186/s13054-016-1414-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Haase CB, Bearman M, Brodersen J, et al. ‘You should see a doctor’, said the robot: Reflections on a digital diagnostic device in a pandemic age. Scand J Public Health 2021;49:33–6. 10.1177/1403494820980268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6., Horby P, Lim WS, et al. , RECOVERY Collaborative Group . Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021;384:693–704. 10.1056/NEJMoa2021436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nalbandian A, Sehgal K, Gupta A, et al. Post-Acute COVID-19 syndrome. Nat Med 2021;27:601–15. 10.1038/s41591-021-01283-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.NHS England . Novel coronavirus (COVID-19) standard operating procedure - COVID Oximetry @home. Available: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/11/C0817-standard-operating-procedure-covid-oximetry-@home-v1.1-march-21.pdf [Accessed 2 May 2021].
- 9.NHS24, coronavirus (COVID-19): general advice. Available: https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/coronavirus-covid-19/coronavirus-covid-19-general-advice [Accessed 27 May 2021].
- 10.Department of Health . Northern Ireland. Covid-19 urgent and emergency care action: no more silos. Available: https://www.health-ni.gov.uk/sites/default/files/publications/health/doh-no-more-silos.pdf [Accessed 4 May 2021].
- 11.Welsh Government cabinet statement . Timely presentation of COVID-19 disease. 4 Aug 2020. Available: https://gov.wales/written-statement-timely-presentation-covid-19-disease [Accessed 3 May 2021].
- 12.BBC News . Covid online symptom checker 'may delay treatment’. Available: https://www.bbc.co.uk/news/health-56323915
- 13.NHS . NHS Inform Scotland, Self Help Guide: COVID-19, 2021. Available: https://www.nhsinform.scot/self-help-guides/self-help-guide-coronavirus-covid-19
- 14.NHS Wales . Coronavirus COVID-19 symptom Checker. Available: https://111.wales.nhs.uk/SelfAssessments/symptomcheckers/COVID19.aspx
- 15.Health and social care Northern Ireland, COVID-19 symptom Checker. Available: https://covid-19.hscni.net/symptoms/
- 16.NHS Digital . Healthcare in the UK | coronavirus in the UK (data.gov.uk). Available: https://coronavirus.data.gov.uk/details/healthcare [Accessed 14 Aug 2021].
- 17.WHO . Situation report: Singapore. Available: https://www.who.int/docs/default-source/wpro-documents/countries/singapore/singapore-situation-report/covid19_sitrep_sgp_20210606.pdf?sfvrsn=d536e556_7 [Accessed 6 Jun 2021].
- 18.John Hopkins University . COVID-19 situation Tracker. Available: https://coronavirus.jhu.edu/us-map [Accessed 14 Aug 2021].
- 19.World Health Organization . Operational considerations for case management of COVID-19 in health facility and community: interim guidance, 19 Mar 2020. World Health Organization, 2020. Available: https://apps.who.int/iris/handle/10665/331492
- 20.Christian MD. Triage. Crit Care Clin 2019;35:575–89. 10.1016/j.ccc.2019.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chotirmall SH, Wang L-F, Abisheganaden JA. Letter from Singapore: the clinical and research response to COVID-19. Respirology 2020;25:1101–2. 10.1111/resp.13929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim WH, Wong WM. COVID-19: notes from the front line, Singapore's primary health care perspective. Ann Fam Med 2020;18:259–61. 10.1370/afm.2539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.England NHS. Novel coronavirus (COVID-19) standard operating procedure - COVID Oximetry @home. Available: https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/11/C0817-standard-operating-procedure-covid-oximetry-@home-v1.1-march-21.pdf [Accessed 2 May 2021].
- 24.NHS24 . Coronavirus (COVID-19): general advice. Available: https://www.nhsinform.scot/illnesses-and-conditions/infections-and-poisoning/coronavirus-covid-19/coronavirus-covid-19-general-advice [Accessed 27 May 2021].
- 25.Brouqui P, Amrane S, Million M, et al. Asymptomatic hypoxia in COVID-19 is associated with poor outcome. Int J Infect Dis 2021;102:233–8. 10.1016/j.ijid.2020.10.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Committee on Diagnostic Error in Health Care, Board on Health Care Services, Institute of Medicine . The National Academies of Sciences, Engineering, and Medicine. In: Balogh EP, Miller BT, Ball JR, eds. Improving diagnosis in health care. Washington (DC): National Academies Press (US), 2015. [PubMed] [Google Scholar]
- 27.NHS England . How to look after yourself at home if you have coronavirus (COVID-19). Available: https://www.nhs.uk/conditions/coronavirus-covid-19/self-isolation-and-treatment/how-to-treat-symptoms-at-home/ [Accessed 4 Jun 2021].
- 28.Burn S, Propper C, Stoye G. What happened to English NHS Hospital activity during the COVID-19 pandemic? Institute for Fiscal Studies. Available: https://ifs.org.uk/publications/15432 [Accessed 13 May 2021].
- 29.Akbar S, Coiera E, Magrabi F. Safety concerns with consumer-facing mobile health applications and their consequences: a scoping review. J Am Med Inform Assoc 2020;27:330–40. 10.1093/jamia/ocz175 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjhci-2021-100448supp001.pdf (116.2KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.