Introduction
Bullous pemphigoid is the most common autoimmune blistering disorder characterized by the development of autoantibodies against self-antigens at the basement membrane zone.1 The disease mainly affects elderly individuals; however, there have been reports of cases in young adults and children. Classically, bullous pemphigoid consists of intensely pruritic tense vesicles and/or bullae arising within urticarial plaques.2 In contrast, the nonbullous presentation can appear with a prodrome of pruritus with various findings, such as erythroderma, excoriations, urticarial plaques, nodules, papules, and erythematous patches without vesicles or bullae.3 A systematic review in 2017 stated that at least 20% of all pemphigoid patients did not have blisters at the time of their diagnosis.1 In this case report, we showcase an atypical manifestation of a bullous pemphigoid, interesting in that it (1) presented with and persisted as nonbullous plaques and eventual erythroderma, (2) had florid lymphadenopathy mimicking lymphoma, and (3) was steroid-resistant yet responded to dupilumab, an interleukin 4 inhibitor and novel treatment for bullous pemphigoid.
Case report
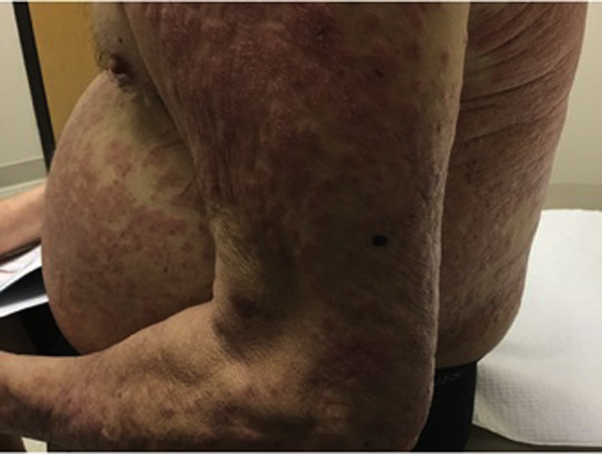
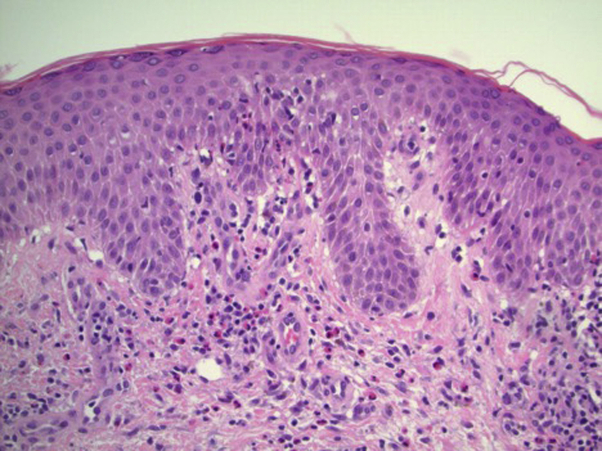
A 74-year-old man with a past medical history of diet-controlled diabetes mellitus and hypertension controlled by metoprolol presented to the office with a chief complaint of a generalized erythematous, pruritic rash, located on the bilateral upper and lower portions of the extremities, lower portion of the back, and trunk, of 4 months duration (Fig 1). He denied joint pain, fever, chills, or blisters as well as any new personal care products or medications. Biopsy of 2 lesions located on the left distal posterior upper arm and the right superior lateral lower back showed confluent parakeratosis, epidermal acanthosis with eosinophilic spongiosis, and no microscopic subepidermal splitting. A perivascular infiltrate was composed of lymphocytes and numerous eosinophils. The differential diagnosis included contact dermatitis, eczematous drug eruption, Ofuji disease, T cell lymphoma, and nonbullous pemphigoid. Medication-induced bullous pemphigoid with metoprolol, which has been associated as a trigger, was thought to be unlikely due to no temporal relationship to the onset of the patient's disease. Due to the relatively mild initial symptoms and low body surface area involvement, the patient was referred for patch testing, which revealed a positive fragrance mix determined to be not relevant based on the patient's unlikely exposure. The patient was then prescribed triamcinolone cream and 60 mg daily of systemic steroids for 2 weeks. On a follow-up appointment 4 weeks later, there was minimal improvement. Sixty milligrams of systemic steroids daily was attempted again for an additional 3 weeks. Despite the multiple systemic steroid treatments, his symptoms markedly worsened, progressing to erythroderma over the subsequent 3 months. At this time, repeat biopsy including direct immunofluorescence as well as serum BP230 antibodies was performed. Histopathologic examination again showed thin parakeratosis, mild irregular acanthosis, and eosinophilic spongiosis without subepidermal splitting (Fig 2). Direct immunofluorescence showed linear basement membrane zone deposition of IgG and C3, and enzyme-linked immunosorbent assay for BP230 was elevated at 38 U/mL (normal value, <9 U/mL), confirming the diagnosis of nonbullous pemphigoid. As the patient continued to have severe symptoms, including severe pruritus and chills refractory to high-dose prednisone, along with the clinical presentation of no bullae or mucosal involvement, a paraneoplastic trigger was considered and oncologic consultation was requested. A computed tomography scan of the chest, abdomen, and pelvis revealed florid lymphadenopathy, raising concerns for systemic lymphoma. Subsequent excisional axillary nodal biopsies fortunately showed only reactive inflammation, however, and the patient was referred back to dermatology for treatment. Due to the severity of the patient's symptoms, failure of high-dose systemic steroids, and no presence of vesicles, bullae, or mucosal involvement for a total of 5 to 6 months, the patient was placed on a loading dose of 600 mg of dupilumab via subcutaneous injection, followed by a maintenance dose of 300 mg every 2 weeks. The patient rapidly improved, with resolution of pruritus within 1 to 2 weeks and near-complete resolution of all rash and symptoms by week 4. The generalized lymphadenopathy was thought to be due to the inflammatory skin disease due to its near-complete resolution within 4 weeks. The patient has been without flares or recurrence for over a year on the same dose of dupilumab, and, to this day, has not shown any signs of vesicles or bullae.
Fig 1.
Multiple relatively well-defined erythematous, edematous papules and plaques with some areas of overlying fine scale and lichenification along with diffusely scattered erosions on the trunk, back, and bilateral upper extremities.
Fig 2.
Confluent thin parakeratosis, epidermal acanthosis with eosinophilic spongiosis, and no microscopic subepidermal splitting.
Discussion
Intense pruritus with urticarial-like plaques beneath tense bullae is the hallmark presentation of bullous pemphigoid.2 Nonbullous pemphigoid lacking the classic bullous lesions is often more difficult to diagnose, as presentation can vary from pruritus to erythematous patches and nodules to erythroderma, as seen in our case. Diagnosis consists of correlating the clinical presentation with the immunohistopathologic findings, which typically should include biopsy for hematoxylin and eosin as well as direct immunofluorescence. In addition, enzyme-linked immunosorbent assay for BP180 and 230 antibodies can be particularly helpful for confirmation in nonbullous cases, as was true in our patient. Histopathologic examination of nonbullous pemphigoid can differ from bullous pemphigoid in a few aspects. Nonbullous pemphigoid commonly will resemble that of eczema or prurigo nodularis, whereas bullous pemphigoid will more commonly present with eosinophilic spongiosis and subepidermal splitting.1 However, nonbullous pemphigoid can also present with very similar histopathologic findings as bullous pemphigoid, which lends support to performing direct immunofluorescence microscopy and immunoserology for diagnosis.1 Our particular case shows a rare presentation of nonbullous pemphigoid causing erythroderma and florid lymphadenopathy that was refractory to mainstay therapy of topical and high-potency systemic steroids. There have been recent studies that have shown success with the use of dupilumab in treatment of bullous pemphigoid that did not respond to mainstay treatment. The near-complete resolution of symptoms after administration of dupilumab in our patient provides support for it being a promising treatment for bullous pemphigoid refractory to standard therapy with high-potency steroids.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.Lamberts A., Meijer J.M., Jonkman M.F. Nonbullous pemphigoid: a systematic review. J Am Acad Dermatol. 2018;78(5):989–995.e2. doi: 10.1016/j.jaad.2017.10.035. [DOI] [PubMed] [Google Scholar]
- 2.Schmidt E., Zillikens D. Pemphigoid diseases. Lancet. 2013;381(9863):320–332. doi: 10.1016/S0140-6736(12)61140-4. [DOI] [PubMed] [Google Scholar]
- 3.Ständer S., Weisshaar E., Mettang T. Clinical classification of itch: a position paper of the international forum for the study of itch. Acta Derm Venereol. 2007;87(4):291–294. doi: 10.2340/00015555-0305. [DOI] [PubMed] [Google Scholar]