Key Points
Question
Among hospital staff who work day and night shifts, do sleep and attention metrics vary between those who work forward- vs backward-rotating shifts?
Findings
This cohort study of 144 nurses found that fast forward-rotating shifts for nurses were associated with lower levels of tiredness and sleepiness and higher levels of sustained attention compared with backward-rotating shifts.
Meaning
These findings suggest that optimization of shift rotations for nurses should be implemented to decrease the negative outcomes associated with shift work.
This cohort study examines the association of shift rotation direction with tiredness, sleepiness, and sustained attention among nurses working forward- and backward-rotating shifts.
Abstract
Importance
The association of fast backward-rotating shift work (ie, anticlockwise sequence of afternoon, morning, and night shifts) with subjective and objective measures of sleep-wake quality, daytime attention, and tiredness of health care workers has not yet been established.
Objective
To investigate the association of shift rotation direction with tiredness, sleepiness, and sustained attention among nurses working forward- and backward-rotating shifts.
Design, Setting, and Participants
Data of this cohort study were collected from nurses working at 5 midsized Italian hospitals. The nurses had either a forward-rotating schedule (ie, morning to afternoon to night) and or a backward-rotating schedule (ie, afternoon to morning to night). The data were collected from July 2017 to February 2020. Data analysis was performed from May to October 2020.
Exposures
Participants were working either forward- or backward-rotating schedules, in which the sequence of 3 shifts (morning, afternoon, and night) changed in a clockwise or anticlockwise direction.
Main Outcomes and Measures
Sleep data were collected using the Karolinska Sleepiness Scale and Pittsburgh Sleep Quality Index. Sustained attention was measured using the Psychomotor Vigilance Task. Tiredness was evaluated using the Tiredness Symptom Scale.
Results
A total of 144 nurses (mean [SE] age, 41.3 [0.8] years; 92 women [63.9%]) participated in the study; 80 nurses had forward-rotating schedules, and 64 had backward-rotating schedules. Nurses with irregular sleep-wake patterns due to night shift work had poor sleep quality (46 [57.5%] in forward-rotating schedule group; 37 [57.8%] in backward-rotating schedule group). Nurses working backward-rotating shifts exhibited significantly greater sleepiness (F1,139 = 41.23; P < .001) and cognitive slowing (ie, longer median reaction times; F1,139 = 42.12; P < .001) than those working forward rotations. Importantly, these differences were not affected by age, years of employment, and quality of sleep. Of nurses working on a backward-rotating schedule, 60 (93.8%) reported elevated sleepiness (Karolinska Sleepiness Scale score ≥7) after the night shift. The median reaction time (F1,139 = 42.12; P < .001), 10% fastest reaction time (F1,139 = 97.07; P < .001), minor lapses (F1,139 = 46.29; P < .001), and reaction time distribution (F1,139 = 60.13; P < .001) of nurses on backward-rotating schedules indicated a lower level of vigilance, which is negatively associated with neurobehavioral performance.
Conclusions and Relevance
In this study, both shift rotation models were negatively associated with health and cognitive performance. These findings suggest that forward shift rotation may be more beneficial than backward rotation for several measured performance attentional outcomes and sleepiness. Optimization of shift rotations should be implemented to decrease the combination of the negative outcomes associated with shift work and reduce the potential risk of medical errors in health care systems.
Introduction
Within the health care industry, 24-hour rotating shifts for hospital nursing staff are necessary to ensure continuity and high-quality care. Shifts vary owing to numerous factors, including the timing and length of work hours (ie, 8- or 12-hour shifts), fixed or rotating schedules, duration of rotations, and number of consecutive days of night work. A nurse’s adaptability to night shifts is often affected by the speed and direction of the shift rotation.
In the US, slow rotations are becoming more common, allowing workers to adjust their circadian rhythm gradually over a period of 2 to 4 weeks,1 whereas in Europe and Japan fast rotations (ie, changing every 3-5 days) are more common, which permits workers to maintain constant circadian rhythms.2 The direction of shift rotation (ie, clockwise [forward] or counterclockwise [backward]) also affects workers’ adaptability. In forward-rotating shift (FRS) work, morning shifts are followed by afternoon and then night shifts. In contrast, backward-rotating shifts (BRSs) consist of night shifts followed by afternoon and then morning shifts. It is commonly assumed that forward rotation is easier to adapt to physiologically because the human circadian rhythm tends to move forward, and it is more difficult to fall asleep earlier than the normal bedtime.3
Prospective studies4,5 suggest that the change from a slowly rotating backward system to a slowly rotating forward system has the greatest effect on night shift workers, in terms of improved sleep quality, decreased fatigue, and fewer attention lapses. Over the long term, these improvements are paralleled by some sleep difficulties during the morning and afternoon shifts.4,5 Moreover, studies of shift schedules comparing changes from a slow BRS to a fast FRS revealed improvements in sleep quality and sleep duration after a night shift.6,7,8 However, no evidence of change or increased sleep quality and length during the day as a result of the change to forward rotation has been provided thus far.9,10,11,12,13 Similarly, no difference in self-rated sleep,14,15,16 alertness during the shift,16 or driving performance15,17 were observed when comparing workers following forward and backward rotation schedules.
For many professions with rotating shifts, large-scale data from shift work have suggested that poor sleep quality is associated with backward rotations.18 Less is known about the possible effects of the direction of shift-work rotation among specific hospital personnel. A study19 of the effects of clockwise and counterclockwise shift-work rotation in 50 Italian nurses indicated that greater self-reported sleep disturbance and poorer work-life balance were observed among nurses working BRSs than among nurses working FRSs.
Confounding these rotating shift results19,20,21 is the structure of the data used, including variations in shift length, shift starting time and/or shift number, and shift direction. Furthermore, some studies used the same participants for both shift rotations, whereas others compared different groups or groups with small sample sizes.22 Notably, few studies used an instrument with known validity and/or reliability, and more studies included only qualitative outcome measures. Although each shift schedule has implications for health care and productivity, the preferable shift rotation direction remains unclear.23
The current study assessed whether shift rotation direction is associated with changes in both subjective and objective measures by using 2 large samples of nurses working 8-hour FRSs or BRSs. We explored the associations of tiredness and sleepiness and metric changes in vigilance performance with several participant-level factors (ie, age, sex, and years of work experience). We hypothesized that a BRS is associated with increased tiredness, sleepiness, and especially with decreased behavioral measures of sustained attention.
Methods
This study was performed in accordance with the ethical standards of the Declaration of Helsinki24 and was approved by the ethical committee of Sapienza University of Rome. Participation was anonymous and voluntary, and each participant provided written informed consent. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Participants
The data were obtained from a sample of nurses who were recruited from 5 midsized hospitals in Italy: Policlinico Umberto I (48 nurses), San Giovanni Addolorata (15 nurses), the Sant’Andrea of Rome (17 nurses), San Carlo of Potenza (50 nurses), and San Jacopo of Pistoia (14 nurses). The first 3 hospitals (Policlinico Umberto I, San Giovanni Addolorata, and Sant’Andrea) adopted FRSs, whereas the remaining 2 (San Carlo of Potenza and San Jacopo of Pistoia) adopted BRSs. The data collection started on July 2017 and ended on February 2020. The participants were categorized into 1 of 2 groups according to the direction of shift rotation. The inclusion criteria were the absence of medical and chronic disorders as assessed by a clinical interview, a roster based on the sequence of shifts described in the procedure with no change in shifts for the 3 days under investigation, and no naps during the night shift. Trainees were excluded from this study.
Measures
Pittsburgh Sleep Quality Index
An Italian version of the Pittsburgh Sleep Quality Index (PSQI) was used to evaluate the participants’ sleep quality.25 This instrument is a reliable, valid, and standardized self-rating scale designed to assess sleep quality during the previous month.25 The questionnaire shows high internal consistency (Cronbach α = 0.835) and good reliability (split-half reliability of 0.85).26 The PSQI comprises 19 items divided into 7 subscales that are rated on a 0- to 3-point Likert scale to evaluate the subjective quality of sleep, sleep latency, sleep duration, habitual sleep efficiency, sleep disorders, use of hypnotic drugs, and disorders during the day. The sum of the scores of the 7 components gives the overall score, ranging from 0 to 21, with 0 indicating the absence of difficulty and 21 indicating serious difficulties in all areas. Scores greater than 5 indicate poor sleep quality.26
Karolinska Sleepiness Scale
An Italian version of the Karolinska Sleepiness Scale (KSS)27 was used to evaluate the subjective level of sleepiness in the 5 minutes before administering the questionnaire to participants.28 The KSS is a 9-point rating scale ranging from “very alert” to “very sleepy, fighting sleep.” The KSS is a reliable and valid drowsiness indicator that correlates with objective electroencephalogram measures of sleepiness and neurobehavioral performance.27
Tiredness Symptoms Scale
An Italian version of the Tiredness Symptoms Scale (TSS)28 was used to evaluate symptoms of chronic fatigue. The TSS is a dichotomous checklist of 14 physical and emotional symptoms that the participant may experience at the time of evaluation.
Psychomotor Vigilance Task
The psychomotor vigilance task (PVT) is a well-established, computerized, simple, cued reaction time (RT) task29 that provides the most widely used metrics of sustained attention and sleep loss.30 During the PVT, participants are placed in front of a computer screen for 5 minutes and asked to click the left mouse button every time a scrolling timer appears, at irregular intervals, with a random interstimulus interval (from 2 to 100 seconds). In this manner, vigilance must be maintained throughout the 5-minute task. The dependent variables used to quantify PVT include median RT, speed (reciprocal of RT), 10% slowest RT, and 10% fastest RT. Validity and sensitivity of this 5-minute version of the PVT has been shown by independent studies.31,32,33
Procedure
Each participant was studied 3 times: after the morning, afternoon, and night shifts. The rosters were as follows: for FRS, day A was morning (7:00 am to 1:30 pm), day B was afternoon (1:30 pm to 8:00 pm), day C was night (8:00 pm to 7:00 am), day D was dismount (daytime off duty), and day E was rest. For BRS, day A was afternoon (2:00 pm to 8:00 pm), day B was morning (7:00 am to 2:00 pm), day C was night (8:00 pm to 7:00 am), day D was dismount (daytime off duty), and day E was rest.
Hence, all nurses were evaluated after their shift on 3 consecutive days (days A through C). Each testing session (maximum duration, 15 minutes) was conducted in a room without noise or environmental distractions. The nurses were asked to switch off their mobile phones during the session, and no one was allowed to enter, except for the experimenter. The task and questionnaires were administered in a fixed order as follows: KSS, TSS, and PVT. The PSQI was administered only during the first testing session.
Statistical Analysis
The following dependent variables were considered: TSS and KSS scores and measures of the PVT (median RT, speed, minor lapses [>500 milliseconds RT], major lapses [>1000 milliseconds RT], 10% slowest RT, 10% fastest RT, false starts [premature responses or response times <100 milliseconds], and response time divergence as a measure of variability [ie, dissimilarity of RT probability density functions]). Each dependent variable was analyzed using a repeated measures analysis of covariance, with independent variables of direction of shift rotation (forward or backward) and shift (morning, afternoon, or night), and covariates of PSQI scores, age, and years of work experience. Paired t tests were used for post hoc comparisons. The significance level was set at P < .05. Data were tested for normality (Kolmogorov-Smirnov test) and homoscedasticity of variance (Bartlett test). We found that PVT did not fit normal distributions (minor and major lapses, false starts, and 10% slowest RTs). Hence, to normalize the distributions, all data were log-transformed before analyses log(1+ x).
Following this main analysis, we conducted linear regression analysis for examining associations between sex and all dependent variables. Because of the number of regressions performed, we adopted a conservative approach setting the threshold for statistical significance at 2-sided α = .01 for these analyses. Statistica software version 4.1 (StatSoft) was used to conduct analyses. Data analysis was performed from May to October 2020.
Results
A total of 144 nurses (mean [SE] age, 41.3 [0.8] years; 92 women [63.9%]) were assigned to 1 of 2 groups according to the direction of shift rotation: 80 nurses (50 women) working an 8-hour fast FRS and 64 nurses (42 women) working an 8-hour fast BRS. As shown in Table 1, age, years of work experience, and sleep quality did not differ significantly between the shift rotation groups. The sex distribution did not differ between the groups (χ21 = 0.15; P = .70). Hospitals working a FRS (Policlinico Umberto I, San Giovanni Addolorata, and Sant’Andrea) did not show significant differences on behavioral measures. Similarly, the remaining hospitals (San Carlo of Potenza and San Jacopo of Pistoia) adopting a BRS were not different.
Table 1. Demographic Variables and PSQI Scores.
| Variable | Mean (SE) | t 142 a | P value | |
|---|---|---|---|---|
| Forward rotating shift (n = 80) | Backward rotating shift (n = 64) | |||
| Age, y | 40.4 (1.0) | 42.3 (1.3) | −0.89 | .37 |
| Time on the job, y | 14.9 (0.9) | 15.8 (1.4) | 0.93 | .35 |
| PSQI subscale score | ||||
| Sleep duration | 1.16 (0.07) | 1.31 (0.09) | −1.22 | .22 |
| Sleep disturbance | 1.35 (0.11) | 1.17 (0.11) | 0.91 | .36 |
| Sleep latency | 1.11 (0.09) | 0.94 (0.11) | 1.34 | .18 |
| Daytime dysfunction | 0.50 (0.10) | 0.44 (0.09) | 0.11 | .91 |
| Sleep efficiency | 1.24 (0.06) | 1.12 (0.06) | 1.45 | .15 |
| Sleep quality | 0.16 (0.07) | 0.11 (0.07) | 0.60 | .55 |
| Medication to sleep | 1.00 (0.09) | 1.12 (0.10) | −0.94 | .35 |
| Total score | 6.54 (0.35) | 6.22 (0.36) | 0.80 | .42 |
Abbreviation: PSQI, Pittsburgh Sleep Quality Index.
Data are the results of the t tests comparing the means log(1 + x) values of the 2 groups.
The baseline characteristics related to the direction of shift rotation and sleep quality of the participants are outlined in Table 1. No statistically significant differences were found in the PSQI global score or sleep problem dimensions (ie, component scores) between the BRS and FRS groups. The mean total score of both groups exceeded the proposed cutoff of 5 for poor sleepers.26 Notably, 46 nurses (57.5%) in the FRS group and 37 nurses (57.8%) in the BRS group had poor sleep quality (χ21 = 0.001; P = .97).
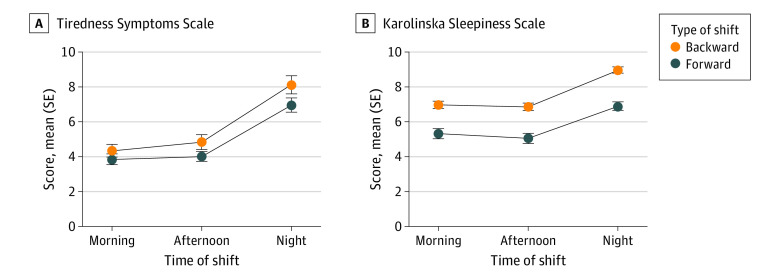
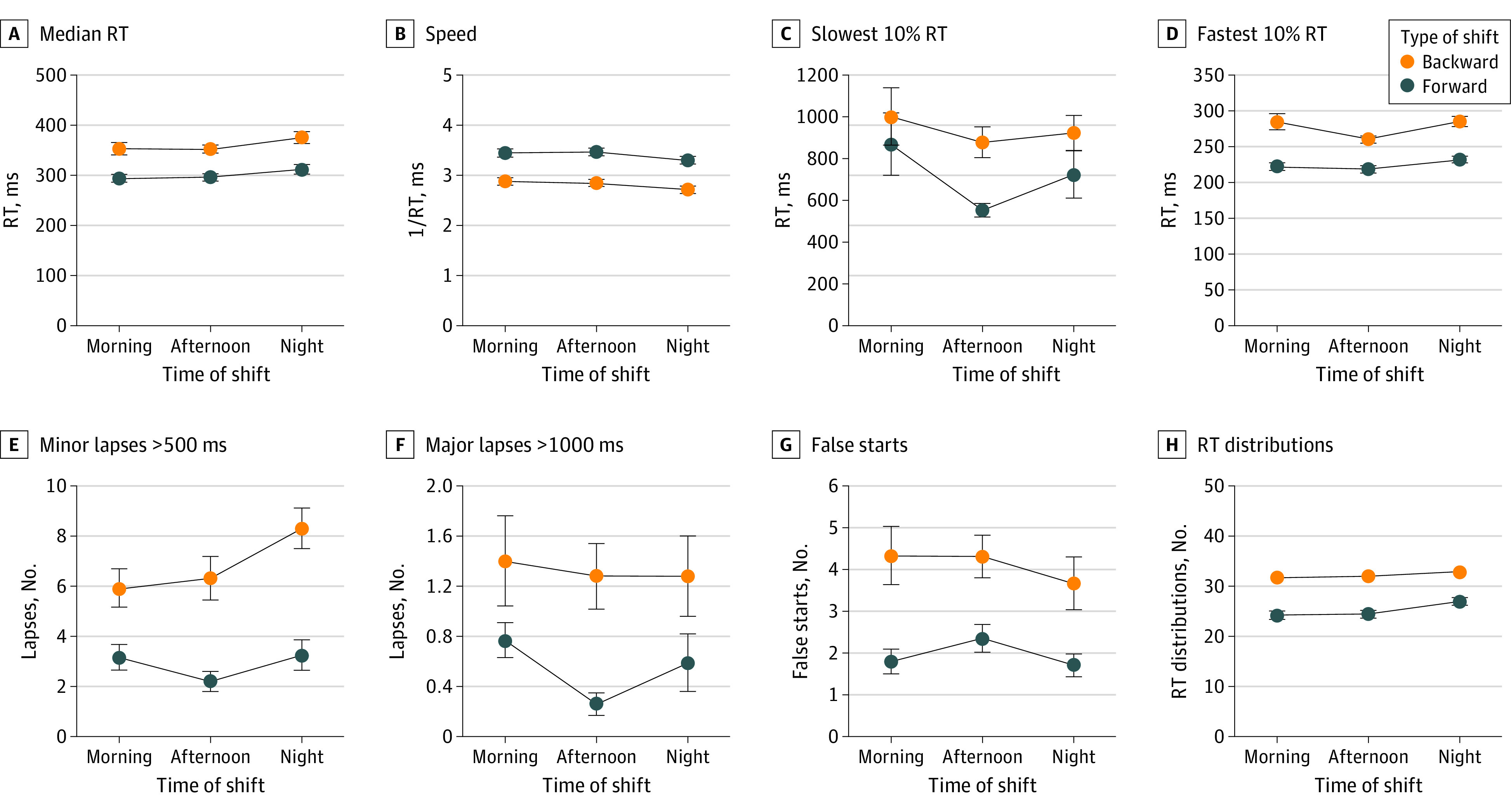
Most importantly, there were significant differences between the BRS and FRS groups for all PVT variables (Table 2). BRS nurses had significantly worse attentional performance than those in the FRS group, as shown in Figure 1. BRS also demonstrated greater subjective sleepiness, as measured by the KSS (60 nurses working a BRS [93.8%] reported a KSS score of ≥7) compared with FRS (F1,139 = 41.23; P < .001), whereas the difference for tiredness, assessed by the TSS did not reach statistical significance (Figure 2 and Table 2).
Table 2. Results of the Statistical Analyses on Tiredness, Sleepiness, and Sustained Attention.
| Variable | Forward-rotating shift (n = 80), mean (SE)a | Backward-rotating shift (n = 64), mean (SE)a | Rotation | Shift | Rotation and shift interaction | Multivariate tests within-cell regressionb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Morning | Afternoon | Night | Morning | Afternoon | Night | F 1,139 | P value | F 2,278 | P value | F 2,278 | P value | Wilks λ (Rao R9,328) | P value | |
| TSS score | 0.60 (0.03) | 0.63 (0.03) | 0.84 (0.03) | 0.65 (0.04) | 0.67 (0.04) | 0.88 (0.04) | 1.58 | .21 | 67.91 | <.001 | 0.02 | .98 | 0.76 (4.38) | <.001 |
| KSS score | 0.76 (0.02) | 0.73 (0.02) | 0.88 (0.02) | 0.89 (0.01) | 0.88 (0.01) | 0.99 (0.01) | 41.23 | <.001 | 43.29 | <.001 | 0.59 | .55 | 0.92 (1.30) | .23 |
| PVT | ||||||||||||||
| Median RT | 2.46 (0.01) | 2.47 (0.01) | 2.49 (0.01) | 2.54 (0.01) | 2.54 (0.01) | 2.57 (0.01) | 42.12 | <.001 | 7.78 | <.001 | 0.06 | .94 | 0.92 (1.17) | .31 |
| Slowest 10% | 2.80 (0.03) | 2.71 (0.02) | 2.75 (0.03) | 2.89 (0.03) | 2.86 (0.03) | 2.89 (0.03) | 13.77 | <.001 | 3.26 | .04 | 1.73 | .18 | 0.94 (0.97) | .46 |
| Fastest 10% | 2.34 (0.01) | 2.34 (0.01) | 2.36 (0.01) | 2.44 (0.01) | 2.42 (0.01) | 2.45 (0.01) | 97.07 | <.001 | 10.18 | <.001 | 1.17 | .31 | 0.96 (0.66) | .74 |
| Minor lapses | 0.45 (0.04) | 0.35 (0.04) | 0.43 (0.04) | 0.69 (0.05) | 0.73 (0.04) | 0.85 (0.04) | 46.29 | <.001 | 4.37 | .01 | 3.581 | .02 | 0.93 (1.13) | .34 |
| Major lapses | 0.18 (0.02) | 0.06 (0.02) | 0.11 (0.02) | 0.22 (0.04) | 0.23 (0.04) | 0.21 (0.04) | 6.76 | .01 | 2.79 | .06 | 4.13 | .02 | 0.92 (1.35) | .21 |
| False starts | 0.36 (0.03) | 0.41 (0.03) | 0.33 (0.03) | 0.58 (0.05) | 0.62 (0.04) | 0.47 (0.05) | 19.83 | <.001 | 6.61 | .002 | 0.96 | .38 | 0.95 (0.82) | .59 |
| RT distribution | 1.37 (0.02) | 1.39 (0.01) | 1.43 (0.01) | 1.51 (0.01) | 0.51 (0.01) | 1.53 (0.01) | 60.13 | <.001 | 8.88 | <.001 | 2.73 | .07 | 0.98 (0.24) | .99 |
| Speed | 0.64 (0.01) | 0.65 (0.01) | 0.63 (0.01) | 0.59 (0.01) | 0.58 (0.01) | 0.57 (0.01) | 56.90 | <.001 | 8.80 | <.001 | 0.28 | .75 | 0.93 (1.13) | .34 |
Abbreviations: KSS, Karolinska Sleepiness Scale; PVT, Psychomotor Vigilance Task; RT, reaction time; TSS, Tiredness Symptoms Scale.
Data are log(1 + x) values and results of the rotation (forward or backward) by shift (morning, afternoon, or night) analysis of covariance values of the dependent measures (TSS, KSS, and variables of the PVT), considering Pittsburgh Sleep Quality Index score, age, and years on the job as covariates.
Sex, Pittsburgh Sleep Quality Index scores, age, and years on the job were used as covariates.
Figure 1. Psychomotor Vigilance Task Measures.
Data are means (dots) and SEs (error bars) for median reaction time (RT), speed (1 / RT), 10% slowest RT, 10% fastest RT, minor lapses (>500 milliseconds RT), major lapses (>1000 milliseconds RT), false starts, and RT distribution for nurses working in forward and backward shifts across different rapidly rotating shifts (morning, afternoon, and night).
Figure 2. Tiredness Symptoms Scale Scores and Karolinska Sleepiness Scale Scores .
Data are mean (dots) and SE (error bars) scores, expressed as raw data, for nurses working in forward and backward shifts across different rapidly rotating shifts (morning, afternoon, and night).
Subjective tiredness and sleepiness were higher during the night shifts vs the morning shift (tiredness: F1,143 = 115.9; P < .001; sleepiness: F1,143 = 64.2; P < .001) and afternoon shift (tiredness: F1,143 = 92.0; P < .001; sleepiness: F1,143 = 76.7; P < .001) whereas the differences between morning and afternoon shifts were not significant (tiredness: F1,143 = 1.51; P = .23; sleepiness: F1,143 = 1.14; P = .29). We found that 51 nurses in the FRS group (63.7%) and 60 nurses in the BRS group (93.7%) reported very high levels of sleepiness at the end of their night shift (χ21 = 18.12; P < .001). Therefore, the night shift was associated with almost all nurses (60 of 64) working backward in a state of elevated sleepiness. Night shifts were also associated with worse performance on the PVT: median RT (F1,139 = 42.12; P < .001), 10% fastest RT (F1,139 = 97.07; P < .001), minor lapses (F1,139 = 46.29; P < .001), and RT distribution (F1,139 = 60.13; P < .001) (Table 2). Specifically, the median RT was slower during night shifts than during morning and afternoon shifts (night vs morning: F1,143 = 10.47; P = .001; night vs afternoon: F1,143 = 10.89; P < .001), whereas the differences between morning and afternoon shifts were not significant (F1,143 = 0.35; P = .56). Furthermore, minor lapses and the RT distribution were characterized by similar differences, with more lapses and greater variability during night shifts than during morning (lapses: F1,143 = 4.31; P = .04; variability: F1,143 = 16.5; P < .001) and afternoon (lapses: F1,143 = 8.63; P = .004; variability: F1,143 = 15.01; P < .001) shifts, whereas the differences between morning and afternoon shifts were not significant (lapses: F1,143 = 0.80; P = .36; variability: F1,143 = 0.14; P = .72). Conversely, the 10% fastest RT was shorter during the afternoon shift than during the morning (F1,143 = 4.42; P = .03) and night (F1,143 = 4.52; P = .02) shifts. As detailed in Table 2, the rotation × shift interaction never reached significance, except for major and minor lapses.
The multivariate effect of covariates (PSQI scores, age, and years of work experience) was not significant, excepted for tiredness (Table 2). This finding indicated that PVT measures were significantly associated with TSS scores after each shift: morning (β = 0.40; 95% CI, 0.36-0.80; P < .001), afternoon (β = 0.41; 95% CI, 0.37-0.81; P < .001), and night (β = 0.39; 95% CI, 0.32-0.76; P < .001). Concerning the control of sex, the linear regressions examining the associations with all dependent variables mostly were not significant, except 4 variables of the PVT in the morning shift of the FRS condition (eTable in the Supplement).
Discussion
This cohort study found that working fast BRSs was associated with increased sleepiness and decreased behavioral measures of sustained attention in nurses. Age, years of employment, and quality of sleep were not associated with modulating sleepiness and performance of this group. Notably, tiredness did not differ between the 2 groups.
Working schedules that conflict with the typical circadian rhythm are well-established to have negative effects. Physiologically, for a proper phase-shift in circadian alignment, shift rotation schedules should advance to allow easier adaption.3 The phenomenon is analogous to jet lag that occurs when traveling, when it is easier to adapt to traveling from east to west than from west to east, because eastward flights are associated with a phase advance of the internal clock.34
Contrary to our expectation, the 2 groups of shift workers did not differ in terms of any component of sleep quality, as measured using the PSQI. We found that 57.5% and 57.8% of the FRS and BRS groups, respectively, reported poor sleep quality (ie, score >5 on the PSQI), which is consistent with our previous studies (ie, 64%21 and 55%20) and studies in other countries (ie, 57%,35 59%,36 58%,37 68.3%,38 78%,39 and 61.9%40) and confirmed that night work is consistently associated with a high risk of sleep disruption and poor sleep quality.41,42,43,44
Conversely, the self-rated sleepiness of the BRS and FRS workers revealed a significant difference. Given that a KSS score of 7 or higher suggests a high degree of sleepiness, we found that 63.7% and 93.7% of nurses in the FRS and BRS groups, respectively, reported very high levels of sleepiness at the end of their night shift. Therefore, the night shift was associated with almost all nurses (60 of 64 nurses) working backward in a state of elevated sleepiness. Although these symptoms were elevated after the night, the BRS group also reported high sleepiness after morning and evening shifts, suggesting a stably elevated daytime sleepiness.
Another aspect of the difference between the 2 groups was that the BRS group reported higher sleepiness associated with shift rotation, which makes it more difficult to perform well.45,46 Indeed, we recorded the detrimental effects of anticlockwise rotation systems in health care on cognitive performance. The BRS groups had significantly slower speed, greater variability, more lapses and false starts, and longer lapse times than the FRS groups, with worse performance after night work than after day work. In 2016, an analysis estimated that medical errors are the third leading cause of death in the US.47 A medical error is a complex and multicausal phenomenon, in which sleepiness and impaired sustained attention are relevant components.44 Sleepiness has serious public health implications.48 Although, to our knowledge, there are no studies in a health care context, reduced sustained attention, as measured using the PVT, is associated with errors in workplaces.49,50 Therefore, strategies to reduce death from medical errors should also consider the adoption of a less disruptive shift-work schedule.44,48
Limitations
This study has limitations. It is a field study, and we did not control for some potential confounders. For example, the BRS group performed more poorly on all outcome measures even after a rest day than the FRS group, and there were significant rotation × shift interactions limited to major and minor lapses. The current design does not allow us to disentangle 3 different interpretations: (1) the BRS group was unable to recover even after a rest day, (2) possible long-lasting consequences exist for working in BRSs, and (3) a fundamental difference exists between the groups that was not primarily due to the shift rotation direction. Furthermore, these interpretations are not necessarily mutually exclusive. Along this line, controlling of circadian and homeostatic factors was not possible in the current cohort study. The duration of the night shift was 11 hours, whereas the morning shift was 6.5 hours and the afternoon shift was 6 to 6.5 hours. However, these limitations are inherent in shift work. The typical comparison of morning, afternoon, and night shifts also intrinsically confounds 3 different factors: (1) homeostatic pressure (ie, the time spent after the last sleep period), (2) circadian phase, and (3) the sequence of days in the shift (ie, in a clockwise rotation system, afternoon and night shifts are the second and the third consecutive days on duty).
Ideally, the measures of tiredness (TSS), sleepiness (KSS), and cognitive slowing (PVT) should have been collected both before and after each shift, but we did not have the opportunity to collect these data. Similarly, we were not able to collect data on the participants’ habits (eg, use of caffeine, napping, or smoking) in some hospitals. This is another limitation of our study because these factors are likely to affect sleepiness and psychomotor vigilance. In fact, the increased coffee consumption during the night shift by BRS nurses has been reported as a potential countermeasure to sleepiness.19
Conclusions
Considering the large number of different shift-work systems used worldwide, it is impossible to establish a single solution suitable for all workers. The current study compared a system consistent with circadian principles (ie, human circadian rhythms better tolerate phase delays than advances) vs a system with shorter recovery in the afternoon-morning shift sequence than in the morning-afternoon shift sequence (11 vs 24 hours), but longer recovery after the night shift (55 vs 48 hours). Our findings strongly discourage the adoption of BRS systems, favoring FRS work.
eTable. Results of the Linear Regressions for Examining Associations Between Sex and Dependent Variables
References
- 1.Kuhn G. Circadian rhythm, shift work, and emergency medicine. Ann Emerg Med. 2001;37(1):88-98. doi: 10.1067/mem.2001.111571 [DOI] [PubMed] [Google Scholar]
- 2.Lilie JK. Shift work and circadian rhythm disorders. In: Golbin AZ, Kravitz HM, Keith LG, eds. Sleep Psychiatry. Taylor & Francis. 2004:97-103. [Google Scholar]
- 3.Czeisler CA, Moore-Ede MC, Coleman RH. Rotating shift work schedules that disrupt sleep are improved by applying circadian principles. Science. 1982;217(4558):460-463. doi: 10.1126/science.7089576 [DOI] [PubMed] [Google Scholar]
- 4.Hossain JL, Reinish LW, Heslegrave RJ, et al. Subjective and objective evaluation of sleep and performance in daytime versus nighttime sleep in extended-hours shift-workers at an underground mine. J Occup Environ Med. 2004;46(3):212-226. doi: 10.1097/01.jom.0000117421.95392.31 [DOI] [PubMed] [Google Scholar]
- 5.van Amelsvoort LG, Jansen NW, Swaen GM, van den Brandt PA, Kant I. Direction of shift rotation among three-shift workers in relation to psychological health and work-family conflict. Scand J Work Environ Health. 2004;30(2):149-156. doi: 10.5271/sjweh.772 [DOI] [PubMed] [Google Scholar]
- 6.Barton J, Folkard S, Smith L, Poole CJ. Effects on health of a change from a delaying to an advancing shift system. Occup Environ Med. 1994;51(11):749-755. doi: 10.1136/oem.51.11.749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hakola T, Härmä M. Evaluation of a fast forward rotating shift schedule in the steel industry with a special focus on ageing and sleep. J Hum Ergol (Tokyo). 2001;30(1-2):315-319. [PubMed] [Google Scholar]
- 8.Harma M, Tarja H, Irja K, et al. A controlled intervention study on the effects of a very rapidly forward rotating shift system on sleep-wakefulness and well-being among young and elderly shift workers. Int J Psychophysiol. 2006;59(1):70-79. doi: 10.1016/j.ijpsycho.2005.08.005 [DOI] [PubMed] [Google Scholar]
- 9.Cruz C, Boquet A, Detwiler C, Nesthus T. Clockwise and counterclockwise rotating shifts: effects on vigilance and performance. Aviat Space Environ Med. 2003;74(6 Pt 1):606-614. [PubMed] [Google Scholar]
- 10.Cruz C, Detwiler C, Nesthus T, Boquet A. Clockwise and counterclockwise rotating shifts: effects on sleep duration, timing, and quality. Aviat Space Environ Med. 2003;74(6 Pt 1):597-605. [PubMed] [Google Scholar]
- 11.Nesthus T, Cruz C, Boquet A, Detwiler C, Holcomb K, Della Rocco P. Circadian temperature rhythms in clockwise and counter-clockwise rapidly rotating shift schedules. J Hum Ergol (Tokyo). 2001;30(1-2):245-249. [PubMed] [Google Scholar]
- 12.Orth-Gomér K. Intervention on coronary risk factors by adapting a shift work schedule to biologic rhythmicity. Psychosom Med. 1983;45(5):407-415. doi: 10.1097/00006842-198310000-00004 [DOI] [PubMed] [Google Scholar]
- 13.Boquet A, Cruz C, Nesthus T, Detwiler C, Knecht W, Holcomb K. Clockwise and counterclockwise rotating shifts: effects on temperature and neuroendocrine measures. Aviat Space Environ Med. 2004;75(10):898-904. [PubMed] [Google Scholar]
- 14.Manodpitipong A, Saetung S, Nimitphong H, et al. Night-shift work is associated with poorer glycaemic control in patients with type 2 diabetes. J Sleep Res. 2017;26(6):764-772. doi: 10.1111/jsr.12554 [DOI] [PubMed] [Google Scholar]
- 15.Kantermann T, Haubruge D, Skene DJ. The shift-work accident rate is more related to the shift type than to shift rotation. Hum Ecologic Risk Assessm. 2013;19(6):1586-1594. doi: 10.1080/10807039.2012.708263 [DOI] [Google Scholar]
- 16.Tucker P, Smith L, Macdonald I, Folkard S. Effects of direction of rotation in continuous and discontinuous 8 hour shift systems. Occup Environ Med. 2000;57(10):678-684. doi: 10.1136/oem.57.10.678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Valck E, Quanten S, Berckmans D, Cluydts R. Simulator driving performance, subjective sleepiness and salivary cortisol in a fast-forward versus a slow-backward rotating shift system. Scand J Work Environ Health. 2007;33(1):51-57. doi: 10.5271/sjweh.1064 [DOI] [PubMed] [Google Scholar]
- 18.Shon Y, Ryu S, Suh BS, et al. Comparison of sleep quality based on direction of shift rotation in electronics workers. Ann Occup Environ Med. 2016;28(1):37. doi: 10.1186/s40557-016-0122-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shiffer D, Minonzio M, Dipaola F, et al. Effects of clockwise and counterclockwise job shift work rotation on sleep and work-life balance on hospital nurses. Int J Environ Res Public Health. 2018;15(9):E2038. doi: 10.3390/ijerph15092038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Muzio M, Diella G, Di Simone E, et al. Nurses and night shifts: poor sleep quality exacerbates psychomotor performance. Front Neurosci. 2020;14:579938. doi: 10.3389/fnins.2020.579938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Muzio M, Reda F, Diella G, et al. Not only a problem of fatigue and sleepiness: changes in psychomotor performance in Italian nurses across 8-h rapidly rotating shifts. J Clin Med. 2019;8(1):E47. doi: 10.3390/jcm8010047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ganesan S, Magee M, Stone JE, et al. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci Rep. 2019;9(1):4635. doi: 10.1038/s41598-019-40914-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Driscoll TR, Grunstein RR, Rogers NL. A systematic review of the neurobehavioural and physiological effects of shiftwork systems. Sleep Med Rev. 2007;11(3):179-194. doi: 10.1016/j.smrv.2006.11.001 [DOI] [PubMed] [Google Scholar]
- 24.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 25.Curcio G, Tempesta D, Scarlata S, et al. Validity of the Italian version of the Pittsburgh Sleep Quality Index (PSQI). Neurol Sci. 2013;34(4):511-519. doi: 10.1007/s10072-012-1085-y [DOI] [PubMed] [Google Scholar]
- 26.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 27.Kaida K, Takahashi M, Akerstedt T, et al. Validation of the Karolinska Sleepiness Scale against performance and EEG variables. Clin Neurophysiol. 2006;117(7):1574-1581. doi: 10.1016/j.clinph.2006.03.011 [DOI] [PubMed] [Google Scholar]
- 28.Turco M, Corrias M, Chiaromanni F, et al. The self-morningness/eveningness (Self-ME): an extremely concise and totally subjective assessment of diurnal preference. Chronobiol Int. 2015;32(9):1192-1200. doi: 10.3109/07420528.2015.1078807 [DOI] [PubMed] [Google Scholar]
- 29.Dinges DF, Powell JW. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav Res Methods Instrum Comput. 1985;17(6):652-655. doi: 10.3758/BF03200977 [DOI] [Google Scholar]
- 30.Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci. 2008;1129:305-322. doi: 10.1196/annals.1417.002 [DOI] [PubMed] [Google Scholar]
- 31.Loh S, Lamond N, Dorrian J, Roach G, Dawson D. The validity of psychomotor vigilance tasks of less than 10-minute duration. Behav Res Methods Instrum Comput. 2004;36(2):339-346. doi: 10.3758/BF03195580 [DOI] [PubMed] [Google Scholar]
- 32.Roach GD, Dawson D, Lamond N. Can a shorter psychomotor vigilance task be used as a reasonable substitute for the ten-minute psychomotor vigilance task? Chronobiol Int. 2006;23(6):1379-1387. doi: 10.1080/07420520601067931 [DOI] [PubMed] [Google Scholar]
- 33.Alfonsi V, Palmizio R, Rubino A, et al. The association between school start time and sleep duration, sustained attention, and academic performance. Nat Sci Sleep. 2020;12:1161-1172. doi: 10.2147/NSS.S273875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waterhouse J, Reilly T, Atkinson G, Edwards B. Jet lag: trends and coping strategies. Lancet. 2007;369(9567):1117-1129. doi: 10.1016/S0140-6736(07)60529-7 [DOI] [PubMed] [Google Scholar]
- 35.Shao MF, Chou YC, Yeh MY, Tzeng WC. Sleep quality and quality of life in female shift-working nurses. J Adv Nurs. 2010;66(7):1565-1572. doi: 10.1111/j.1365-2648.2010.05300.x [DOI] [PubMed] [Google Scholar]
- 36.Hsieh ML, Li YM, Chang ET, Lai HL, Wang WH, Wang SC. Sleep disorder in Taiwanese nurses: a random sample survey. Nurs Health Sci. 2011;13(4):468-474. doi: 10.1111/j.1442-2018.2011.00641.x [DOI] [PubMed] [Google Scholar]
- 37.Lin PC, Chen CH, Pan SM, et al. Atypical work schedules are associated with poor sleep quality and mental health in Taiwan female nurses. Int Arch Occup Environ Health. 2012;85(8):877-884. doi: 10.1007/s00420-011-0730-8 [DOI] [PubMed] [Google Scholar]
- 38.De Martino MM, Abreu AC, Barbosa MF, Teixeira JE. The relationship between shift work and sleep patterns in nurses. Cien Saude Colet. 2013;18(3):763-768. doi: 10.1590/S1413-81232013000300022 [DOI] [PubMed] [Google Scholar]
- 39.McDowall K, Murphy E, Anderson K. The impact of shift work on sleep quality among nurses. Occup Med (Lond). 2017;67(8):621-625. doi: 10.1093/occmed/kqx152 [DOI] [PubMed] [Google Scholar]
- 40.Tarhan M, Aydın A, Ersoy E, Levent D. The sleep quality of nurses and its influencing factors. Euras J Pulmonol. 2018;20(2):78-84. doi: 10.4103/ejop.ejop_35_18 [DOI] [Google Scholar]
- 41.Stocker LJ, Macklon NS, Cheong YC, Bewley SJ. Influence of shift work on early reproductive outcomes: a systematic review and meta-analysis. Obstet Gynecol. 2014;124(1):99-110. doi: 10.1097/AOG.0000000000000321 [DOI] [PubMed] [Google Scholar]
- 42.Waage S, Pallesen S, Moen BE, et al. Changes in work schedule affect the prevalence of shift work disorder among Norwegian nurses: a two year follow-up study. Chronobiol Int. 2021;38(6):924-932. doi: 10.1080/07420528.2021.1896535 [DOI] [PubMed] [Google Scholar]
- 43.Pallesen S, Bjorvatn B, Magerøy N, Saksvik IB, Waage S, Moen BE. Measures to counteract the negative effects of night work. Scand J Work Environ Health. 2010;36(2):109-120. doi: 10.5271/sjweh.2886 [DOI] [PubMed] [Google Scholar]
- 44.Alfonsi V, Scarpelli S, Gorgoni M, Pazzaglia M, Giannini AM, De Gennaro L. Sleep-related problems in night shift nurses: towards an individualized interventional practice. Front Hum Neurosci. 2021;15:644570. doi: 10.3389/fnhum.2021.644570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fujiwara S. Studies on fatigue and shift work in nurses [in Japanese]. Sangyo Igaku. 1992;34(3):225-235. doi: 10.1539/joh1959.34.225 [DOI] [PubMed] [Google Scholar]
- 46.Matsumoto K, Sasagawa N, Kawamori M. Studies of fatigue of hospital nurses due to shift work: with special reference to night shifts and short off-duty [in Japanese]. Sangyo Igaku. 1978;20(2):81-93. doi: 10.1539/joh1959.20.81 [DOI] [PubMed] [Google Scholar]
- 47.Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016;353:i2139. doi: 10.1136/bmj.i2139 [DOI] [PubMed] [Google Scholar]
- 48.Chattu VK, Manzar MD, Kumary S, Burman D, Spence DW, Pandi-Perumal SR. The global problem of insufficient sleep and its serious public health implications. Healthcare (Basel). 2018;7(1):E1. doi: 10.3390/healthcare7010001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Edkins GD, Pollock CM. The influence of sustained attention on railway accidents. Accid Anal Prev. 1997;29(4):533-539. doi: 10.1016/S0001-4575(97)00033-X [DOI] [PubMed] [Google Scholar]
- 50.Basner M, Rubinstein J. Fitness for duty: a 3-minute version of the Psychomotor Vigilance Test predicts fatigue-related declines in luggage-screening performance. J Occup Environ Med. 2011;53(10):1146-1154. doi: 10.1097/JOM.0b013e31822b8356 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Results of the Linear Regressions for Examining Associations Between Sex and Dependent Variables