Abstract
Introduction: The aim of this study was to compare the number of the Pediatric Emergency Department (PED) visits for young allergic patients with respiratory or cutaneous symptoms during the first wave of the coronavirus disease 19 (COVID-19) pandemic in 2020 with the same period in 2019, evaluating the percentage of positive cases to Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2). We carried out a retrospective analysis using data from young patients who visited the PED with cutaneous or respiratory symptoms in the period from 20th February to 12th May of the years 2020 and 2019. Data on allergy and COVID-19 nasal swab were also collected. We observed eleven (28.2%) PED visits for allergic patients with respiratory or cutaneous symptoms for the period from 20th February to 12th May of the year 2020 and ninety-three (31.8%) PED visits for the same time frame of the year 2019 (p=0.645). Only a two-month-old child out of 39 patients with non-allergic respiratory or cutaneous symptoms resulted positive for SARS-CoV-2. Specifically, we found for all the PED visits: 21 (7.2%) in 2019 vs 2 (5.1%) in 2020 for patients with urticaria/angioedema or atopic dermatitis (p=0.634); 3 (1.0%) in 2019 vs 3 (7.7%) in 2020 for patients with anaphylaxis (p=0.003); 19 (6.5%) in 2019 vs 2 (5.1%) in 2020 for those with asthma (p=0.740); 11(3.8%) in 2019 vs 1(2.6%) in 2020 for those with lower respiratory diseases, excluding asthma (p=0.706); 39(13.4%) in 2019 vs 3 (7.7%) in 2020 for those with upper respiratory diseases (URDs) (p=0.318). We also showed a substantial decrease (~80%) in all PED visits compared with the same time frame in 2019 (absolute number 263 vs 1,211, respectively). Among all the PED visits a significant reduction was mostly found for URDs [155 (12.8%) in 2019 vs 17 (6.5%) in 2020; p=0.045)]. The total number of PED visits for allergic patients with respiratory or cutaneous symptoms dropped precipitously in 2020. It is very tricky to estimate whether it was a protective action of allergy or the fear of contagion or the lockdown or a reduction in air pollution that kept children with allergy from visiting the PED. Further studies are needed to better understand the impact of underlying allergies on COVID-19 susceptibility and disease severity.
Key words: COVID-19, children, allergic diseases
Dear Editor,
The first wave of the Coronavirus disease 19 (COVID-19) pandemic has had a remarkable impact on health-care visits, with enormous implications for children with chronic disorders, such as asthma. Asthma is the most frequent chronic disease in childhood and one of the major causes of hospitalization among those younger than 15 years of age [1]. Severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) attacks primarily the lungs [2] as other common respiratory viruses, and there were concerns regarding the effects on children and adolescents with asthma and allergic diseases until a short time ago [3]. Indeed, asthma was listed as a potential risk factor for severe COVID-19 illness according to the Center for Disease Control (CDC) [4]. It is known that subjects with underlying pathological conditions, such as hypertension, obesity, diabetes mellitus and cerebrovascular disease, more easily developed severe COVID-19 disease [5]. In contrast, the number of asthma exacerbations was reduced during the first year of COVID-19 pandemic, as well as the health-care utilization, although the high worldwide prevalence of asthma (13.2-13.7% in the 13–14-year age group; 11.1-11.6% in the 6–7-year age group) [6]. National lockdowns are important interventions that have an effect not only on COVID-19 diffusion but also on all infectious diseases. Social distancing countermeasures, stay-at home orders and school closures might have modified the epidemiology of the other viral infections that commonly trigger the asthma exacerbations requiring acute care [7]. Furthermore, DeLaroche et al. [8] showed that the ED visit percentages across 27 pediatric hospitals decreased by 45.7% during the pandemic and the largest decrease was for respiratory diseases (70.0%), such as acute otitis media and upper respiratory infections, as well as for chronic conditions, including asthma. Haddadin et al. [9] showed a 50% decrement in all pediatric Emergency Department (ED) visits at a regional children’s hospital during the COVID-19 pandemic compared to the same time periods in the 2 previous years. In addition, during the last months several studies have supported the hypothesis according to which asthma and allergy could be “protective factors” against COVID-19 [10,11]. Licari et al. [10] confirmed a reduction in the frequency and severity of COVID-19 in pediatric patients admitted to two hub hospitals in the North of Italy, in addition to a decreased presence of allergic comorbidities. These latter authors hypothesized that allergic patients having a serum eosinophilia could be less affected from COVID-19 [10], confirming the important role of eosinophils in the immune response against SARSCoV- 2 [11]. Jackson et al. [11] referred a potential mechanism which could explain the lower frequency of COVID-19 in allergic children. Indeed, they showed a reduced angiotensin-converting enzyme-2 (ACE2) gene expression in airway cells in patients with allergy regardless of asthma, and thus a decreased susceptibility to infection [12]. Several studies have shown the presence of eosinopenia in COVID-19 patients [13,14]. Our research hypothesis arose from the clinical observation of a substantial decrease of the medical consults for allergic and asthmatic outpatients during the first wave of COVID-19 pandemic despite its starting in the “spring allergy season”. Therefore, we conducted a retrospective analysis of the hard copy archive of the Pediatric Emergency Department (PED) to evaluate trends of the visits for allergic patients with respiratory or cutaneous symptoms during the first wave of pandemic (specifically from 20th February to 12th May 2020) compared to the same time frame in 2019.We also investigated the frequency of the positivity to SARS-CoV-2 amongst them. The patients’ data were collected by using Hospital Information System {SISWeb ((https://cup.asl2abruzzo.it/ asl2alpi/login.aspx)}https://cup.asl2abruzzo.it/asl2alpi/login.aspx) . We included patients with lower respiratory diseases (LRDs) (wheezing and asthma, bronchitis, bronchiolitis and pneumonia), upper respiratory diseases (URDs) (rhinitis, pharyngotonsillitis and laryngospasm) and cutaneous diseases [urticaria and/or angioedema, atopic dermatitis (AD) and contact dermatitis]. Flowchart of the study is shown in Figure 1.
During emergency visits the pediatrician collected the medical history of a previous physician asthma-diagnosis and the presence of allergy evaluated by parent-reported positive Immunoglobulin(Ig)E dosage or by skin prick test. The sociodemographic and clinical characteristics of the study population are shown in Table 1.
Table 1.
Socio-demographic and clinical characteristics of the study population.
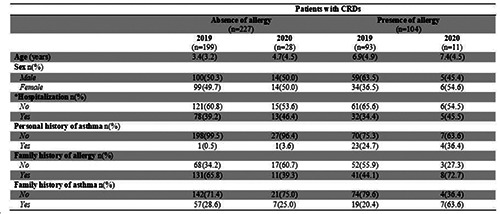
Data are absolute numbers (percentages) or media (standard deviation). N. numbers; CRDs: cutaneous or respiratory diseases; *number of patients who were hospitalized after the entering to emergency room.
We found ninety-three (31.8%) PED visits for allergic patients with respiratory or cutaneous symptoms for the period from 20th February to 12th May of the years 2019 and a total of 11 (28.2%) during the first wave of COVID-19 pandemic (p=0.645). Noteworthy, the only COVID-19 positive patient (2 months of age) was not allergic or asthmatic, and presented a mild clinical course. Among all the PED visits for allergic patients with respiratory or cutaneous symptoms, specifically we also showed: 21 (7.2%) in 2019 versus 2 (5.1%) in 2020 for patients with urticaria/angioedema or atopic dermatitis (p=0.634); 3 (1.0%) in 2019 versus 3 (7.7%) in 2020 for patients with anaphylaxis (p=0.003); 19(6.5%) in 2019 versus 2(5.1%) in 2020 for those with asthma (p=0.740); 11 (3.8%) in 2019 versus 1 (2.6%) in 2020 for those with LRDs, excluding asthma (p=0.706); 39 (13.4%) in 2019 versus 3 (7.7%) in 2020 for those with URDs (p=0.318). All PED visits for cutaneous or respiratory symptoms were decreased of 24.1% in 2020 to 14.8% in 2019 (<0.001). Moreover, a reduction, albeit not statistically significant, was found for patients with asthma [39(3.2%) in 2019 vs 3(1.1%) in 2020; p=0.066]. The data are shown in Figure 2 and Figure 3, and in Table S1 and in Table S2.
As regards to the link between asthma and COVID-19 the current understanding is still unclear. Theoretically, it seems that preexisting asthma has a potential influence on SARS-CoV-2 susceptibility. However, in a systematic review by Castro Rodriguez et al. [15], the scientific evidence on the role of asthma as a potential risk factor for COVID-19 severity in children was scarce. In Wuhan, China, Zhang et al. [14] reported that on 140 COVID-19 patients 11.4% was hypersensitive to certain drugs and 1.4% presented urticaria, but no patient had asthma or other allergic diseases. In a very recent review, the authors summarized that probably in adults the comorbidities which increased the susceptibility for SARS-CoV-2, such as asthma and obesity, did not appear to be as such in children [16]. Hurst et al. [17] evaluated changes in healthcare utilization for children and adolescents with asthma before and after the onset of the COVID-19 pandemic. These latter authors found that the overall healthcare utilization decreased in all settings and asthma outcomes for the children and adolescents were improved during the first year of the pandemic; they speculated that it was partially due a reduced spread of the common viral triggers of asthma. A retrospective analysis of data from 18,912 pediatric patients with asthma treated in a large healthcare network in California found reductions of 68-90% in asthma-related hospitalizations and ED visits during the first 6 months of the pandemic compared to percentages from 2017 to 2019 [18]. Another retrospective study including 1,054 children with asthma and 505 non - asthmatic children in the multinational Pediatric Asthma in asthma- Real Life (PeARL) cohort identified decreased asthma-related hospitalizations and ED visits [19].
In our opinion, a few crucial questions remain about the low frequency of COVID-19 in patients with allergic disorders and asthma: could this diversity be related to a more allergic asthma phenotype in children than adults? Could the mechanisms underlying the comorbidities which influence the susceptibility to SARSCoV- 2 and COVID-19 severity in children be different? Could a Th2 skewed cytokine production be the main explanation for a lower susceptibility to SARS-CoV2 in allergic and asthmatic children? The modulation of ACE2 expression by type 2 inflammatory processes, as well as the predominance of some specific type 2 cytokines might provide potential protective effects against COVID-19 [20]. In the Urban Environment and Childhood Asthma study the authors found that allergic sensitization was inversely related to ACE2 expression in the nasal epithelium regardless of asthma status [21]; ACE2 expression was also significantly inversely associated with type 2 biomarkers including the number of positive allergen-specific IgE tests, total IgE, fractional exhaled nitric oxide and nasal epithelial interleukin(IL)13 expression. The modulation of ACE2 expression by type 2 inflammatory processes suggests the need to comprehensively evaluate the role of type 2 immune regulation in COVID-19 pathogenesis. In addition, we experienced a reduction in Telehealth visits for allergic and asthmatic medical consults, suggesting that the decline of the allergic symptoms was likely not only related to the reluctance to seek pediatric care during the first wave of COVID-19 pandemic, but also maybe to a real protection of the allergy to SARS-CoV-2 in children. Unfortunately, we cannot prove that link because of our study design (absence of any biological contribution). On the other hand, our findings also support that there may be negative unintended consequences deriving from the execution of public health measures that disrupt normal social interactions.
Figure 1.
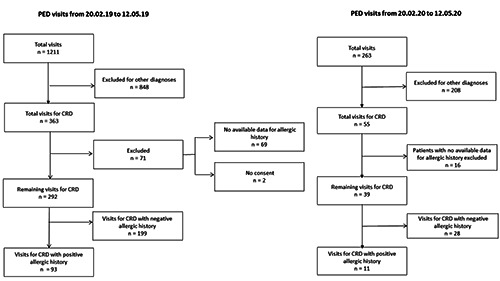
Flow-chart of the study. The figure shows the total number of charts reviewed in 83 days period (20th February-12th May) of the years 2019 and 2020. It evidences the number of children excluded in the initial analysis due to the exclusion criteria, and the number of patients excluded in a second analysis, due to the absence of consent (n=2 for 2019 year) and no available data for allergic history (n=69 for year 2019 and n=16 for year 2020). The total number included in the final analysis is also shown (n=93 for year 2019 and n=11 for year 2020). PED, pediatric emergency department; CRD, cutaneous and respiratory diseases.
Regarding food allergies, we found an increase in children with food anaphylaxis (from 1.0% to 7.7%; p<0.003) during the national lockdown, this was probably due to the difficulty of finding specialist allergy products due to high demand in shops or low income caused from the pandemic itself, or for the increased time spent at home.
We also highlighted in the period from February 20th to May 12th 2020, a substantial decline (~80%) in all PED visits compared with the same period of time in 2019 (absolute number 263 vs 1,211, respectively). Furthermore, there was a significant difference in PED visits for patients who presented at least one of the pathologies among urticaria/AD, anaphylaxis, URDs, LRDs or asthma during the COVID-19 pandemic compared with the same period in 2019 (p=<0.001). Specifically, a significant reduction of the PED visits for URDs remained after adjustment for pairwise comparisons [155 (12.8%) in 2019 vs 17 (6.5%) in 2020; p=0.045). The data are shown in Figure 3 and in Table S2 (supporting information). Similarly to our findings, Lazzerini et al. [22] showed substantial decreases, from 88% to 73%, in PED visits in the period March 1–27, 2020, compared with the same period in 2019 and 2018 in five Italian hospitals. Ciacchini et al [23] also demonstrated a 76% reduction in the number of admissions with an evident decrement during March 2020 to the corresponding time frame of the previous year. During the national lockdown in Italy the closure of all schools and sports activities yielded lower percentages of acute infections among children than usual. Indeed, we also found a substantial decrease of the PED visits for patients with URDs or LRDs, from 20.6% to 10.7% (p=<0.001), during the first wave of COVID-19 pandemic. Cozzi et al. [24] also experienced an important drop in respiratory infections, such as fever, respiratory distress, cough, sore throat and earache due to the effect of lockdown. Pines et al. [25] showed that certain types of pediatric visits were more impacted; in particular, URDs, otitis media, and symptoms of nausea and vomiting, had sharper and more persistent declines. Finally, we also hypothesized that this substantial decrease in number of PED visits for patients with allergic respiratory and cutaneous diseases likely could also be due to a dramatic reduction in air pollution as a consequence of this unprecedented quarantine [26]. Hassoun et al. [27] also experienced lower rates of allergic reactions, such as asthma, allergic rashes, or angioedema caused by a limited environmental allergen exposure. Indeed, Dutheil et al. [28] showed how the overall air quality was improved due to the lockdown and blocked transportation activities among many countries of the world.
The strengths of our study are the inclusion of almost the first entire quarantine period and acute visits to PED for allergic or respiratory emergency or life-threatening acute events which are mandatory even during pandemics rather than the outpatient visits; indeed, visits for mild-to-moderate disease in well-controlled patients could be transitioned to a digital medicine service. Furthermore, we considered not only the absolute numbers but also the percentage of the visits and compared them with the same period in 2019. The limitations included the retrospective study design, the definition of allergy based on parent-reported positive diagnostic tests and the absence of any biological contribution. Furthermore, our data refer to a single PED, thus limiting the scope of our findings. However, to investigate the effects of lockdown on our clinical setting it is also important to better comprehend what can be expected when such measures are adopted. This could also help us to plan for a future outbreak.
Figure 2.
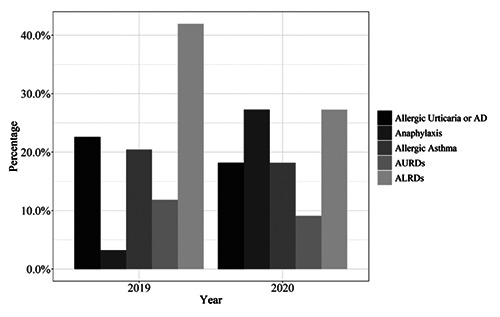
Histogram showing the percentages of the total number of allergic patients who visited the Pediatric Emergency Department for respiratory and cutaneous symptoms during the first wave of COVID-19 pandemic compared with the same period in 2019. AD, atopic dermatitis; AURDs, allergic upper respiratory diseases; ALRDs, allergic lower respiratory diseases.
Figure 3.
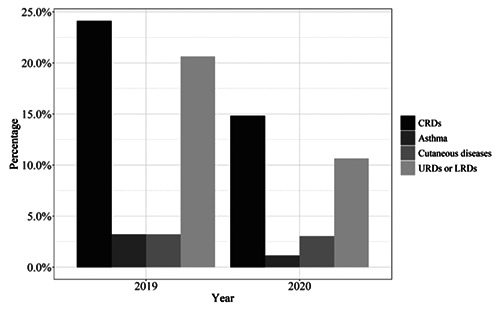
Histogram showing the percentages of the total number of the patients who visited the Pediatric Emergency Department for respiratory or cutaneous diseases, asthma only, cutaneous diseases only, and for upper and lower respiratory diseases only during the first wave of COVID-19 pandemic compared with the same period in 2019. The chart shows the total number of the patients who visited the Pediatric Emergency Department for respiratory or cutaneous diseases, for asthma only, for cutaneous disease only, and finally for respiratory tract diseases only (indicated as the sum of upper or lower respiratory diseases), independently from the presence of allergy; CRDs, cutaneous or respiratory diseases; URDs, upper respiratory diseases; LRDs, lower respiratory diseases.
It is very intriguing to explore whether the allergy is really responsible of providing certain protective effects against COVID- 19 mostly for the hypothesis to find potential biological drugs enhancing the type 2 immune response and inducing resistance to SARS-CoV-2. However, it is very tricky to estimate if the protective role of the allergy or the fear of contagion or the lockdown or a reduction in air pollution that kept children with allergic diseases from visiting PED. Surely, further clinical and basic studies are needed to explore the relationship of COVID-19 with asthma and other allergic diseases. However, a close examination of trends in PED visits during the COVID-19 pandemic should be a priority for both physicians and public health officials.
Acknowledgements
The authors would like to thank the investigators and patients at the investigative sites for their support of this study and all the nurses of the Department of Pediatrics, University of Chieti, in particular Romina Capuzzi and Cecilia Finamore for their daily support in clinical research and care of children. We thank Prof. Simon Cunningham for his help in reviewing the English language content. We also are very grateful to Dr. Maria Stella Cantini for her important support to the project.
Funding Statement
Funding: No funds, grants, or other support was received.
References
- 1.World Health Organization. Asthma. 2006. Accessed on: 7 March 2007. Available from: http://www.who.int/mediacentre/factsheets/fs307/en/index.html [Google Scholar]
- 2.Attanasi M, Pasini S, Caronni A, Pellegrino GM, Faverio P, Di Pillo S, et al. Inpatient care during the COVID-19 pandemic: A survey of Italian physicians. Respiration 2020;99:667-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shaker MS, Oppenheimer J, Grayson M, Stukus D, Hartog N, Hsieh EWY, et al. COVID-19: pandemic contingency planning for the allergy and immunology clinic. J Allergy Clin Immunol Pract 2020;8:1477-88.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention [Internet]. People who are at higher risk for severe illness. Updated July 30, 2020. Available from: www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medicalconditions.html [PubMed] [Google Scholar]
- 5.Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pearce N, Aït-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax 2007;62:758-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Angoulvant F, Ouldali N, Yang DD, Filser M, Gaidos V, Rybak A, et al. COVID-19 pandemic: impact caused by school closure and national lockdown on pediatric visits and admissions for viral and non-viral infections, a time series analysis. Clin Infect Dis 2021;72:319-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.DeLaroche AM, Rodean J, Aronson PL, Fleegler EW, Florin TA, Goyal M, et al. Pediatric emergency department visits at US children's hospitals during the COVID-19 pandemic. Pediatrics 2021;147:e2020039628. [DOI] [PubMed] [Google Scholar]
- 9.Haddadin Z, Blozinski A, Fernandez K, Vittetoe K, Greeno AL, Halasa NB, Lovvorn HN III. Changes in pediatric emergency department visits during the COVID-19 pandemic. Hosp Pediatr 2021;11:e57-e60. [DOI] [PubMed] [Google Scholar]
- 10.Licari A, Votto M, Brambilla I, Castagnoli R, Piccotti E, Olcese R, et al. Allergy and asthma in children and adolescents during the COVID outbreak: What we know and how we could prevent allergy and asthma flares. Allergy 2020;75:2402-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jackson DJ, Busse WW, Bacharier LB, Kattan M, O’Connor GT, Wood RA, et al. Association of respiratory allergy, asthma and expression of the SARS-CoV-2 receptor, ACE2. J Allergy Clin Immunol 2020;146:203-6.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindsley AW, Schwartz JT, Rothenberg ME. Eosinophil responses during COVID-19 infections and coronavirus vaccination. J Allergy Clin Immunol 2020;146:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qin C, Zhou L, Hu Z, Zhang S, Yang S, Tao Y, et al. Dysregulation of immune response in patients with Coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis 2020;71:762-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang JJ, Dong X, Cao YY, Yuan YD, Yang YB, Yan YQ, et al. Clinical characteristics of 140 patients infected with SARSCoV- 2 in Wuhan, China. Allergy 2020;75:1730-41. [DOI] [PubMed] [Google Scholar]
- 15.Castro-Rodriguez JA, Forno E. Asthma and COVID-19 in children - a systematic review and call for data. Pediatr Pulmonol 2020;55:2412-2418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boechat JL, Wandalsen GF, Kuschnir FC, Delgado L. COVID- 19 and pediatric asthma: Clinical and management challenges. Int J Environ Res Public Health 2021;18:1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hurst JH, Zhao C, Fitzpatrick NS, Goldstein BA, Lang JE. Reduced pediatric urgent asthma utilization and exacerbations during COVID-19 pandemic. Pediatr Pulmonol 2021. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guijon OL, Morphew T, Consulting M, Ehwerhemuepha L, Galant SP. Evaluating the impact of COVID-19 on asthma morbidity: a comprehensive analysis of potential influencing factors. Ann Allergy Asthma Immunol 2021;127:91-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Papadopoulos NG, Mathioudakis AG, Custovic A, Deschildre A, Phipatanakul W, Wong G, et al. Childhood asthma outcomes during the COVID- 19 pandemic: findings from the:1765 PeARL multinational cohort. Allergy 2021;76:1765-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brake SJ, Barnsley K, Lu W, Mc Alinden KD, Eapen MS, Sohal SS. Smoking upregulates angiotensin-converting enzyme-2 receptor: A potential adhesion site for novel Coronavirus SARS-CoV-2 (Covid-19). J Clin Med 2020;9:841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bacharier LB, Beigelman A, Calatroni A, Jackson DJ, Gergen PJ, O'Connor GT, et al. Longitudinal phenotypes of respiratory health in a high-risk urban birth cohort. Am J Respir Crit Care Med 2019;199:71-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19 (2020). Lancet Child Adolesc Health 4:e10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ciacchini B, Tonioli F, Marciano C, Faticato MG, Borali E, Pini Prato A, et al. Reluctance to seek pediatric care during the COVID-19 pandemic and the risks of delayed diagnosis. Ital J Pediatr 2020;46:87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cozzi G, Zanchi C, Giangreco M, Rabach I, Calligaris L, Giorgi R, et al. The impact of the COVID-19 lockdown in Italy on a pediatric emergency setting. Acta Paediatr 2020;109:2157-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pines JM, Zocchi MS, Black BS, Carlson JN, Celedon P, Moghtaderi A, et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med 2021;41:201-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bao R, Zhang A. Does lockdown reduce air pollution? Evidence from 44 cities in northern China. Sci Total Environ 2020;731:139052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hassoun A, Pugh S, Merced I, Sharma M. The power of social isolation on pediatric emergency visits during COVID-19 lockdown. Acta Paediatr 2020;109:2425-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dutheil F, Baker JS, Navel V. COVID-19 as a factor influencing air pollution? Environ Pollut 2020;263:114466. [DOI] [PMC free article] [PubMed] [Google Scholar]


