Abstract
Background
Healthcare workers (HCWs) fighting against the COVID-19 pandemic are under incredible pressure, which puts them at risk of developing mental health problems. This study aimed to determine the prevalence of depression, anxiety, and stress among HCWs responding to COVID-19 and its associated factors.
Methods
A multi-country cross-sectional study was conducted during July–August 2020 among HCWs responding to COVID-19 in nine Eastern Mediterranean Region (EMR) countries. Data were collected using an online questionnaire administered using KoBo Toolbox. Mental problems were assessed using the Depression, Anxiety, and Stress Scale (DASS-21).
Results
A total of 1448 HCWs from nine EMR countries participated in this study. About 51.2% were male and 52.7% aged ≤ 30 years. Of all HCWs, 57.5% had depression, 42.0% had stress, and 59.1% had anxiety. Considering the severity, 19.2%, 16.1%, 26.6% of patients had severe to extremely severe depression, stress, and anxiety, respectively. Depression, stress, anxiety, and distress scores were significantly associated with participants’ residency, having children, preexisting psychiatric illness, and being isolated for COVID-19. Furthermore, females, those working in a teaching hospital, and specialists had significantly higher depression and stress scores. Married status, current smoking, diabetes mellitus, having a friend who died with COVID-19, and high COVID-19 worry scores were significantly associated with higher distress scores.
Conclusions
Mental problems were prevalent among HCWs responding to COVID-19 in EMR. Therefore, special interventions to promote mental well-being among HCWs responding to COVID-19 need to be immediately implemented.
Keywords: died, stressanxiety, associated factors, COVID-19, depression, stress
Introduction
The world is passing through and is being challenged by the emergence of a novel Severe Acute Respiratory Syndrome Coronavirus (SARS-Cov-2).1 The 2019 Corona Virus Disease (COVID-19) has been declared an international public health emergency on 30 January 2020, by the World Health Organization (WHO).2 As of 5 February 2021, 105.74 million cases of COVID-19 have been reported worldwide, including 2.3 million deaths.3 In the Eastern Mediterranean Region (EMR), 5.7 million confirmed cases and 135 438 deaths have been reported as of 3 February 2021.3
The COVID-19 pandemic is now a major global health threat and severely affecting mental health worldwide.4 Although the mental health impact of COVID-19 has been well documented by the media, the mental health care needs of those suffering from this crisis have been relatively neglected.5 Healthcare workers (HCWs) is the most vulnerable group and at high risk for COVID-19.6 The Centers for Disease Control and Prevention (CDC) reported 342 859 cases and 1177 deaths among health care personnel as of 4 January 2021.7 Moreover, information released by the international council of nurses (ICN), stated that up to 6 May 2020, nearly 90 000 HCWs have been affected, and more than 260 nurses have died.8
COVID-19 pandemic has been associated with a considerable level of stress and anxiety among HCWs who face exhaustion, difficult triage decisions, separation from families, stigma, fear of being infected, fear of infecting their beloved ones, and pain of losing patients and colleagues.9 The balance between professional duty, altruism, and personal fear for oneself and others can often cause conflict and dissonance in many HCWs.10
Despite the significant stress that HCWs face daily during the COVID-19 pandemic, data on the impact of the COVID-19 pandemic on the mental health status of HCWs in the Eastern Mediterranean Region (EMR) are scarce. Therefore, this multi-country study aimed to determine the prevalence of depression, anxiety, and stress and assess preventive behaviors among HCWs responding to COVID-19 in the EMR countries. Moreover, this study aimed to determine the factors associated with these mental health illnesses. The findings of this study are expected to help in planning interventions that protect HCWs’ capacity to carry out their duties in responding to COVID-19 as well as maintain their mental health well-being.
Methods
Study design
A multi-country cross-sectional study was conducted between 15 July 2020, and 30 August 2020, among HCWs responding to COVID-19 in nine different countries in the EMR. The study involved various HCWs including physicians, nurses, pharmacists, radiologists, radiology technicians, and laboratory technicians working at teaching, public and private hospitals of the selected countries.
Questionnaires and data collection
Data were collected using an online questionnaire. The study questionnaire was developed in English based on the previous surveys11 and translated into Arabic language using forward and backward translation procedure. The questionnaire was administered using KoBo Toolbox. Data collection involved the identification of survey anchors for participants’ recruitment online and survey administration. In each country, two to three hospitals assigned to manage and treat patients with COVID-19 in that country were selected. A link to an online questionnaire was sent to all HCWs in these hospitals and study participants were encouraged to fill the online survey form in their free time.
The questionnaire included questions about socio-demographic characteristics (age, gender, nationality, marital status, education level, work status, and lifestyle), medical history, and exposure to COVID-19. The questionnaire included information on self-perceived psychological distress concerning the COVID pandemic. The Depression, Anxiety and Stress Scale- 21 Items (DASS-21) was used to measure the negative emotional states of depression, anxiety, and stress.12 It is a self-reported 21-item tool developed by the University of New South Wales, Australia to provide independent measures of depression, stress, and anxiety with recommended severity thresholds for depression, stress, and anxiety subscales. The scores in each subscale were summed and multiplied by 2 (this is because the DASS-21 is the short form of the scale). Cut-off values of > 9, > 7, and > 14 represent a positive screen of depression, anxiety, and stress, respectively. The scores of depression, anxiety, and stress were categorized into mild, moderate, severe, and extremely severe according to the scoring system in the DASS manual.12
Moreover, the COVID-19 Peritraumatic Distress Index (CPDI) was used to assess psychological distress.13 It consisted of 15 items and inquired about the frequency of anxiety, depression, specific phobias, cognitive change, avoidance and compulsive behavior, physical symptoms, and loss of social functioning in the past week. Responses to the questions were 1 = not at all, 2 = rarely, 3 = sometimes, and 4 = often. The scores were summed with a total score ranging from 15 to 60. A base count of 40 was added to the sum, according to the tool instructions, to have a standard scale score with a maximum of 100. The addition of the base allows our results to be compared to with results of previous studies. The CPDI score was then classified to obtain the levels of distress as follows: a CPDI score between 1 and 28 indicates normal levels, a CPDI score between 29 and 52 indicates mild distress and a CPDI score between 53 and 100 indicates severe distress.13
The worry from COVID-19 was assessed using a 10-item COVID-19 worry scale that assessed the worrying status on a scale ranging from 1 (not worried at all) to 10 (extremely worried). The total scale score ranges from 10 to 100. Higher scores indicate higher levels of worry from the COVID-19 outbreak.14
The study tools were pilot tested on 30 persons and necessary changes were made to improve the clarity of questions.
Data analysis
Data were exported into IBM SPSS version 24 (IBM Corp. Released 2016. IBM SPSS Statistics for Windows, Version 24.0. Armonk, NY: IBM Corp) for analysis. Data were described using frequencies and percentages. Percentages were compared using the chi-square test (χ2). Cronbach’s alpha test was used to assess the internal consistency, with satisfactory reliability corresponding to a value >0.70.15 Floor and ceiling effects of the scales were calculated. We adopted the commonly used 15% threshold for persons achieving the highest and lowest score to define a ceiling and floor effect, respectively.16 Multivariate analysis of factors associated with depression, stress, anxiety, and distress was conducted using the General Linear Model (GLM) procedure with a separate analysis for each outcome. The GLM procedure provides regression analysis and analysis of variance for one dependent variable. A P-value of less than 0.05 was considered statistically significant.
Ethical considerations
The study was approved by Ethical Committees at the Ministries of Health in the nine countries. Permissions were obtained from the hospital’s officials. Confidentiality was maintained and participation was strictly voluntary. All participants gave informed consent before answering the study questionnaires.
Results
A total of 1448 HCWs were enrolled from nine countries including Iraq (n = 381), Egypt (n = 308), Somalia (n = 212), Sudan (n = 202), Yemen (n = 160), Jordan (n = 55), Pakistan (n = 53), Afghanistan (n = 36), and Morocco (n = 41). Of all respondents, 742 (51.2%) were male, 763 (52.7%) aged ≤ 30 years old, 867 (59.9%) were married and 770 (53.2%) reported having children. A total of 940 (64.9%) of HCWs were working in Ministry of Health hospitals, 506 (34.9%) were general practitioners and 463 (32%) were nurses. Table 1 shows the HCWs’ demographic, clinical, and work-related characteristics.
Table 1.
Health care workers’ demographic, clinical, and work-related characteristics
| Characteristics | n | % |
|---|---|---|
| Gender | ||
| Male | 742 | 51.2 |
| Female | 706 | 48.8 |
| Age (year) | ||
| ≤ 30 | 763 | 52.7 |
| > 30 | 685 | 47.3 |
| Type of workplace | ||
| Teaching hospital | 332 | 22.9 |
| Ministry of Health hospital | 940 | 64.9 |
| Private hospital | 176 | 12.2 |
| Job title | ||
| Specialist | 206 | 14.2 |
| General practitioner | 506 | 34.9 |
| Nurse/Midwife | 463 | 32.0 |
| Pharmacist | 94 | 6.5 |
| Laboratory technician | 135 | 9.3 |
| Radiology technician | 44 | 3.0 |
| Marital status | ||
| Married | 867 | 59.9 |
| Single | 558 | 38.5 |
| Divorced/Widow | 23 | 1.6 |
| Having children | 770 | 53.2 |
| Cigarettes smoker | ||
| Current smoker | 158 | 10.9 |
| Ex-smoker | 65 | 4.5 |
| Non-smoker | 1225 | 84.6 |
| Hours of daily sleep | ||
| ≤ 7 | 925 | 64.3 |
| > 7 | 513 | 35.7 |
| Hours of daily exercise | ||
| < 2 | 617 | 51.1 |
| ≥ 2 | 591 | 48.9 |
| Home/living arrangement | ||
| Live alone | 203 | 14.0 |
| Live with family members | 1132 | 78.2 |
| Live in shared accommodation (other than family members) | 113 | 7.8 |
| Presence of chronic diseases | ||
| Hypertension | 163 | 11.3 |
| Hyperlipidemia | 138 | 9.6 |
| Diabetes mellitus | 103 | 7.1 |
| Asthma | 154 | 10.7 |
| Preexisting psychiatric illness | 94 | 6.5 |
| Ischemic heart disease | 76 | 5.3 |
Of all HCWs, 432 (29.8%) were infected with COVID-19, 490 (33.9%) were isolated due to COVID-19, 458 (31.6%) had family member infected with COVID-19, 127 (8.8%) had family member died of COVID-19, 1151 (79.5%) had a friend/colleague infected, and 364 (25.3%) had friend/colleague died with COVID-19.
Table 2 shows the summary statistics of depression, anxiety, stress, distress, and COVID-19 worry scales. Cronbach’s alpha was satisfactory for all scales and exceeded 0.80. Of all HCWs, 57.5% had depression, 42.0% had stress, and 59.1% had anxiety. Considering the severity, 19.2%, 16.1%, 26.6% of patients had severe to extremely severe depression, stress, and anxiety, respectively (Figure 1).
Table 2.
Summary statistics of depression, anxiety, stress, distress, and COVID-19 worry scales
| Scale | Minimum | Maximum | Mean | SD | Cronbach’s Alpha | Floor effect (%) | Ceiling effect (%) |
|---|---|---|---|---|---|---|---|
| Depression | 0.0 | 42.0 | 12.8 | 10.0 | 0.86 | 10.3 | 0.6 |
| Stress | 0.0 | 42.0 | 14.4 | 9.8 | 0.86 | 9.1 | 0.6 |
| Anxiety | 0.0 | 42.0 | 10.6 | 8.8 | 0.82 | 12.8 | 0.3 |
| Distress | 55.0 | 100.0 | 72.9 | 9.3 | 0.87 | 4.1 | 0.1 |
| Worry from COVID-19 | 10.0 | 90.0 | 55.3 | 20.1 | 0.89 | 1.1 | 2.7 |
Fig. 1 .
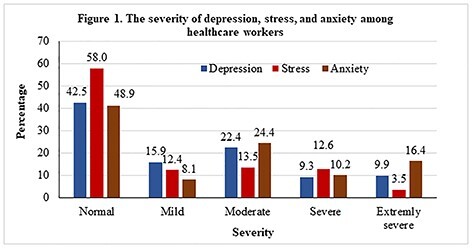
The severity of depression, stress, and anxiety among healthcare workers.
Table 3 shows a multivariate analysis of factors associated with depression, anxiety, and stress scores. There were significant variations in the three scales’ scores between HCWs according to the country. HCWs in Egypt, Iraq, and Sudan had the highest depression, anxiety, and stress scores compared to those in other countries. Females had significantly higher depression and stress scores than males. HCWs working in private hospitals had relatively lower depression and stress scores compared to those working in the Ministry of Health and teaching hospitals. Specialists and general practitioners had the highest stress scores when compared to other HCWs. HCWs with children had significantly higher depression and stress scores than those without children. Having a preexisting psychiatric illness, have been isolated due to COVID-19, having a friend/colleague infected with COVID-19, and increased COVID-19 worry score were significantly associated with higher depression, stress, and anxiety scores.
Table 3.
Factors associated with depression, stress, and anxiety scales scores in the multivariate analysis
| Depression | Stress | Anxiety | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Mean | SD | P-value | Mean | SD | P-value | Mean | SD | P-value |
| Country | <0.001 | <0.001 | <0.001 | ||||||
| Afghanistan | 9.7 | 7.8 | 10.4 | 6.5 | 9.4 | 7.6 | |||
| Egypt | 17.0 | 10.1 | 18.2 | 9.4 | 14.4 | 9.0 | |||
| Iraq | 14.3 | 10.3 | 16.2 | 10.3 | 10.7 | 8.8 | |||
| Jordan | 9.9 | 8.7 | 11.6 | 8.7 | 5.3 | 5.7 | |||
| Morocco | 9.6 | 7.7 | 14.6 | 8.4 | 8.4 | 8.2 | |||
| Pakistan | 8.3 | 9.2 | 10.3 | 10.2 | 7.7 | 8.9 | |||
| Somalia | 9.3 | 8.9 | 10.2 | 8.3 | 9.3 | 8.7 | |||
| Sudan | 13.9 | 9.8 | 15.0 | 9.3 | 11.4 | 8.2 | |||
| Yemen | 8.2 | 7.5 | 10.8 | 8.3 | 7.4 | 7.8 | |||
| Gender | 0.007 | 0.002 | 0.321 | ||||||
| Male | 11.6 | 9.8 | 13.0 | 9.4 | 9.3 | 8.4 | |||
| Female | 14.0 | 10.1 | 15.8 | 9.9 | 11.9 | 9.0 | |||
| Type of workplace | 0.023 | 0.002 | 0.321 | ||||||
| Teaching/Academic hospital | 12.9 | 10.2 | 15.3 | 9.7 | 10.0 | 8.2 | |||
| Ministry of Health hospital | 13.1 | 10.1 | 14.6 | 9.9 | 11.0 | 9.0 | |||
| Private hospital | 10.9 | 9.2 | 11.4 | 8.8 | 9.4 | 8.5 | |||
| Job title | 0.187 | 0.002 | 0.604 | ||||||
| Specialist | 13.0 | 9.8 | 16.1 | 9.3 | 10.1 | 8.2 | |||
| General practitioner | 13.5 | 10.6 | 15.2 | 10.4 | 10.5 | 9.1 | |||
| Nurse/Midwife | 12.4 | 9.9 | 13.5 | 9.5 | 11.1 | 9.0 | |||
| Pharmacist | 11.6 | 10.1 | 12.7 | 10.1 | 9.6 | 9.1 | |||
| Laboratory technician | 12.8 | 8.2 | 14.2 | 8.5 | 10.8 | 7.4 | |||
| Radiology technician | 10.5 | 9.6 | 11.7 | 8.9 | 9.7 | 9.6 | |||
| Having children | <0.001 | 0.010 | 0.051 | ||||||
| Yes | 13.0 | 10.3 | 14.6 | 9.5 | 10.4 | 8.5 | |||
| No | 12.6 | 9.8 | 14.2 | 10.1 | 10.8 | 9.1 | |||
| Diagnosed with preexisting psychiatric illness | <0.001 | 0.001 | 0.001 | ||||||
| Yes | 16.6 | 10.5 | 18.3 | 9.9 | 14.8 | 9.4 | |||
| No | 12.5 | 9.9 | 14.1 | 9.7 | 10.3 | 8.7 | |||
| Have been isolated due to COVID-19 | <0.001 | <0.001 | <0.001 | ||||||
| Yes | 14.0 | 10.0 | 16.0 | 9.8 | 12.6 | 9.1 | |||
| No | 12.1 | 10.0 | 13.6 | 9.7 | 9.5 | 8.5 | |||
| Have friend/colleague infected with COVID-19 | <0.001 | 0.003 | 0.001 | ||||||
| Yes | 13.5 | 10.1 | 15.3 | 9.7 | 11.1 | 8.8 | |||
| No | 9.9 | 9.4 | 11.1 | 9.2 | 8.5 | 8.4 | |||
| Worry from COVID-19 score (Quartiles) | <0.001 | <0.001 | <0.001 | ||||||
| ≤ 43 | 9.0 | 8.0 | 9.7 | 8.1 | 7.7 | 7.1 | |||
| 44–56 | 12.5 | 9.3 | 14.0 | 8.4 | 10.2 | 8.2 | |||
| 57–71 | 13.2 | 9.1 | 15.4 | 8.9 | 10.8 | 8.2 | |||
| ≥ 72 | 16.4 | 11.9 | 18.7 | 11.2 | 13.7 | 10.4 | |||
Table 4 shows the multivariate analysis of factors associated with the distress scale score. Distress score among HCWs varied significantly according to the country. Jordan’s HCWs had the highest distress score. Radiology technicians had the highest distress score. Female gender, being married, ex-smoking, diabetes, having a friend/colleague died with COVID-19, and higher COVID-19 worry score were significantly associated with higher distress score.
Table 4.
Factors associated with distress scale scores in the multivariate analysis
| Variable | Mean | SD | P-value |
|---|---|---|---|
| Country | <0.001 | ||
| Afghanistan | 72.6 | 6.8 | |
| Egypt | 75.5 | 8.6 | |
| Iraq | 74.3 | 8.4 | |
| Jordan | 77.5 | 8.7 | |
| Morocco | 74.1 | 9.6 | |
| Pakistan | 67.1 | 10.1 | |
| Somalia | 70.2 | 9.0 | |
| Sudan | 70.9 | 10.1 | |
| Yemen | 70.4 | 9.3 | |
| Gender | 0.001 | ||
| Male | 71.7 | 9.2 | |
| Female | 74.1 | 9.2 | |
| Type of healthcare worker | <0.001 | ||
| Specialist | 73.1 | 9.0 | |
| General practitioner | 72.7 | 9.5 | |
| Nurse/Midwife | 72.0 | 9.2 | |
| Pharmacist | 73.3 | 10.7 | |
| Laboratory technician | 74.5 | 8.5 | |
| Radiology technician | 76.2 | 6.6 | |
| Marital status | 0.003 | ||
| Married | 73.6 | 9.1 | |
| Single | 71.9 | 9.5 | |
| Divorced/Widow | 67.0 | 9.9 | |
| Cigarettes Smoker | 0.008 | ||
| Current Smoker | 70.3 | 9.3 | |
| Ex-smoker | 75.8 | 8.4 | |
| Non-smoker | 73.0 | 9.3 | |
| Diagnosed with diabetes mellitus | 0.012 | ||
| Yes | 73.9 | 9.0 | |
| No | 72.8 | 9.3 | |
| Have friend/colleague died with COVID-19 | <0.001 | ||
| Yes | 75.1 | 8.6 | |
| No | 72.0 | 9.4 | |
| Worry from COVID-19 score (Quartiles) | <0.001 | ||
| ≤ 43 | 68.7 | 8.9 | |
| 44–56 | 72.6 | 8.3 | |
| 57–71 | 73.7 | 8.5 | |
| ≥ 72 | 76.4 | 9.8 |
Discussion
Main finding of this study
Almost half of health care workers responding to the spread of COVID-19 in the EMR experienced depression, anxiety, and stress. The depression, anxiety, and stress scores varied significantly according to country of HCWs, gender, type of workplace, job title, having children, preexisting psychiatric illness being isolated due to COVID-19, having friend/colleague infected with COVID-19, and worry from COVID-19 score.
What is already known on this topic
HCWs are at an increased risk of adverse psychological health outcomes during the COVID-19 outbreak. Reasons for this include long working hours, risk of infection, and shortages of protective equipment, loneliness, physical fatigue, and separation from families.17 There are many studies done in the past reported that HCWs especially those working in emergency units, intensive care units, and infectious disease wards are at higher risk of developing adverse psychiatric impact.18–20 Data on the factors associated with depression, anxiety, and stress among HCWs in the EMR are scarce.
What this study adds
Significant proportions of HCWs responding to the spread of COVID-19 in the EMR countries experienced moderate to severe mental health impact. Overall, DASS-21 scores among health care workers were higher than those reported in previous studies in China and Singapore.21,22 This could be attributed to decreased mental preparedness and an increase in case fatality rate in the region. Reasons for this may include reduced accessibility to formal psychological support, less first-hand medical information on the outbreak, and less intensive training on personal protective equipment and infection control measures.
Our finding showed the mean scores of depression, stress, and anxiety were higher among participants from Egypt and Iraq. This might be attributed to the increased number of COVID-19 cases and deaths during the study period.
The current study showed that females had slightly higher stress, depression, and distress scores than males. Similarly, recent studies in China and Italy that assessed psychological distress post the COVID-19 outbreak found that females were more likely to develop psychological distress, while males were less susceptible to post-traumatic distress in responding to stressful outbreaks.4,13 This finding could be attributed to gender differences in the hormonal response to stress.23 More research is needed to explain gender differences in the mental health impact of COVID-19 among HCWs.
This study revealed that participants who were working in Ministry of Health hospitals and Teaching/Academic hospitals were more likely to report severe symptoms of stress and depression compared to participants who were working in private hospitals. A similar result was previously reported among HCWs in China.21This finding in the EMR may be explained by the higher workload and higher number of COVID-19 treated in the Ministry of health and academic hospitals.
Specialists and general practitioners had the highest stress scores when compared to other HCWs. This finding is explained by their closer contact with patients with COVID-19. In contrast, other studies in Singapore and China reported that nurses were more affected by mental health problems.11,21
HCWs who reported having children had higher depression, stress, and anxiety scores, and married HCWs had higher distress score. Fear of transmitting the infection to family members might explain this association. Similar findings were reported in a previous study.24 On the other hand, a Singapore study found that single doctors are at higher risk than married nurses to develop psychiatric symptoms.25
Worrying about family members and friends and fear of being infected are major stressors among HCWs.26 In our study, mental problems were significantly higher among HCWs isolated due to COVID-19, having friend/colleague infected, and who had a higher COVID-19 related worry score. These findings are consistent with the findings of other studies including studies conducted in China and Saudi Arabia.20,27–29
In conclusion, mental problems were prevalent among HCWs responding to COVID-19 in EMR. Therefore, special interventions to promote mental well-being among HCWs responding to COVID-19 need to be immediately implemented.
Limitations of this study
Our study has many limitations. One limitation is that this study has relied on self-reported data collected via an online questionnaire. Thus, only those who had access to the internet had received the link to the online questionnaire and this might affect the representativeness of the sample.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Acknowledgement
The authors would like to acknowledge the Global Health Development (GHD) for supporting the research.
Yasser Ghaleb
Faris Lami
Mohannad Al Nsour
Hiba Abdulrahman Rashak
Sahar Samy
Yousef S. Khader
Abdulwahed Al Serouri
Hala BahaaEldin
Salma Afifi
Maisa Elfadul
Aamer Ikram
Hashaam Akhtar
Ahmed Mohamud Hussein
Abdelaziz Barkia
Huda Hakim
Hana Ahmad Taha
Yasser Hijjo
Ehab Kamal
Abdirizak Yusuf Ahmed
Fazalur Rahman
Khwaja Mir Islam
Moshtaq Hassan Hussein
Shahd Raid Ramzi
Contributor Information
Yasser Ghaleb, Ministry of Public Health and Population, Yemen Field Epidemiology Training Program, Sana’a, Yemen.
Faris Lami, Department of Community and Family Medicine, University of Baghdad, Baghdad, Iraq.
Mohannad Al Nsour, Global Health Development (GHD), The Eastern Mediterranean Public Health Network (EMPHNET), Amman, Jordan.
Hiba Abdulrahman Rashak, Directorate of Public Health, Ministry of Health, Baghdad, Iraq.
Sahar Samy, Ministry of Health and Population, Cairo, Egypt.
Yousef S Khader, Professor of Epidemiology, Medical Education and Biostatistics, Department of Public Health, Jordan University of Science & Technology, Irbid 22110, Jordan.
Abdulwahed Al Serouri, Ministry of Public Health and Population, Yemen Field Epidemiology Training Program, Sana’a, Yemen.
Hala BahaaEldin, Ministry of Health and Population, Cairo, Egypt.
Salma Afifi, Ministry of Health and Population, Cairo, Egypt.
Maisa Elfadul, Public Health Institute, Federal Ministry of Health, Department of Research, Khartoum, Sudan.
Aamer Ikram, National Institute of Health, Islamabad, Pakistan.
Hashaam Akhtar, Yusra Institute of Pharmaceutical Sciences, Yusra Medical and Dental Collage, Islamabad, Pakistan.
Ahmed Mohamud Hussein, Somali International University, Somal.
Abdelaziz Barkia, Epidemic Diseases Service, Ministry of Health, Rabat, Morocco.
Huda Hakim, Department of Community Medicine, Al-Majmaah University, AL-Majmaah, Kingdom of Saudi Arabia.
Hana Ahmad Taha, Health Protection and Promotion, Global Health Development (GHD), Eastern Mediterranean Public Health Network, Amman, Jordan.
Yasser Hijjo, Clinical Pharmacy, Public and Tropical Health Programs, University of Medical Sciences & Technology, Khartoum, Sudan.
Ehab Kamal, Ministry of Health and Population, Cairo, Egypt.
Abdirizak Yusuf Ahmed, Demartino Hospital, Somalia.
Fazalur Rahman, Medical Unit 1 Benazir Bhutto Hospital, Rawalpindi Medical University, Rawalpindi, Pakistan.
Khwaja Mir Islam, Afghanistan Field Epidemiology Training Program, Global Health Development (GHD), Afghanistan.
Moshtaq Hassan Hussein, Directorate of Public Health, Ministry of Health, Baghdad, Iraq.
Shahd Raid Ramzi, Al-Rusafa Health Directorate, Public Health Department, Ministry of Health, Baghdad, Iraq.
Conflict of interest
The author(s) declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
References
- 1. Jones DS. History in a crisis - lessons for covid-19. N Engl J Med 2020;382(18):1681–3. [DOI] [PubMed] [Google Scholar]
- 2. Lai CC, Shih TP, Ko WC et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int J Antimicrob Agents 2020;55(3):105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. WHO . COVID-19 Weekly Epidemiological Update, 27 December 2020. Available at https://www.who.int/publications/m/item/weekly-epidemiological-update---29-december-2020
- 4. Moccia L, Janiri D, Pepe M et al. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav Immun 2020;87:75–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Xiang YT, Yang Y, Li W et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 2020;7(3):228–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Alrubaiee GG, Al-Qalah TAH, Al-Aawar MSA. Knowledge, attitudes, anxiety, and preventive behaviors towards COVID-19 among health care providers in Yemen: an online cross-sectional survey. BMC Public Health 2020;20(1):1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. CDC . Cases & Deaths among Healthcare Personnel, Updated: Jan. Available at: https://covid.cdc.gov/covid-data-tracker/#health-care-personnel
- 8. The International Council . ICN calls for data on healthcare worker infection rates and deaths. 6 May 2020. https://www.icn.ch/news/icn-calls-data-healthcare-worker-infection-rates-and-deaths
- 9. Regly E. Italian doctors’ fatalities reach tragic levels as they fight COVID-19 in overburdened hospitals. The Globe and Mail 2020. https://www.theglobeandmail.com/world/article-italian-doctors-fatalities-reach-tragic-levels-as-they-fight-covid-1/. [Google Scholar]
- 10. Ho CS, Chee CY, Ho RC. Mental Health Strategies to Combat the Psychological Impact of COVID-19 Beyond Paranoia and Panic. Ann Acad Med Singap 2020;49(3):155–60. [PubMed] [Google Scholar]
- 11. Tay BYQ, Chew NWS, Lee GKH et al. 2020. Psychological impact of the COVID.19 pandemic on health care workers in Singapore. Ann Intern Med 2020;173(4):317–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lovibond, S.H. & Lovibond, P.F. (1995). Manual for the Depression Anxiety Stress Scales. (2nd. Ed.) Sydney: Psychology Foundation. ISBN 7334-1423-0. [Google Scholar]
- 13. Qiu J, Shen B, Zhao M et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr 2020;33(2):e100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Conway, L. G. III, Woodard, S. R., & Zubrod, A. (2020). Social Psychological Measurements of COVID-19: Coronavirus Perceived Threat, Government Response, Impacts, and Experiences Questionnaires. PsyArXiv. doi: 10.31234/osf.io/z2x9a. https://psyarxiv.com/z2x9a/. [DOI] [Google Scholar]
- 15. Cronbach LJ, Shavelson, R. J. (Ed.). My Current Thoughts on Coefficient Alpha and Successor Procedures. Educ Psychol Meas 2004;64(3):391–418. [Google Scholar]
- 16. Terwee CB, Bot SD, de Boer MR et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007;60(1):34–42. [DOI] [PubMed] [Google Scholar]
- 17. Kang L, Li Y, Hu S et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020;7(3):e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Naushad VA, Bierens JJ, Nishan KP et al. A Systematic Review of the Impact of Disaster on the Mental Health of Medical Responders. Prehosp Disaster Med 2019;34(6):632–43. [DOI] [PubMed] [Google Scholar]
- 19. Spoorthy MS, Pratapa SK, Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J Psychiatr 2020;51:102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lai J, Ma S, Wang Y et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open 2020;3(3):e203976–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Que J, Le Shi JD, Liu J et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. Gen Psychiatr 2020;33(3):e100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tan BY, Chew NW, Lee GK et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med 2020;173(4):317–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sareen J, Erickson J, Medved MI et al. Risk factors for post-injury mental health problems. Depress Anxiety 2013;30(4):321–7. [DOI] [PubMed] [Google Scholar]
- 24. Chew NWS, Lee GKH, Tan BYQ et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun 2020;88:559–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chan AO, Huak CY. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med (Lond) 2004;54(3):190–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brooks SK, Webster RK, Smith LE et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395(10227):912–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Al-Hanawi MK, Mwale ML, Alshareef N et al. Psychological Distress Amongst Health Workers and the General Public During the COVID-19 Pandemic in Saudi Arabia. Risk Manag Healthc Policy 2020;13:733–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Shechter A, Diaz F, Moise N et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry 2020;66:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Balkhi F, Nasir A, Zehra A, Riaz R. Psychological and behavioral response to the coronavirus (covid-19) pandemic. Cureus 2020;12(5):e7923. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.


