Abstract
Background:
Although the athleticism required of cheerleaders has increased, the risks of cheerleading have been less studied as compared with other sports.
Purpose:
To update our understanding of the epidemiology of cheerleading-related injuries.
Study Design:
Descriptive epidemiology study.
Methods:
We analyzed the National Electronic Injury Surveillance System (NEISS) for cheerleading-related injuries presenting to nationally representative emergency departments (EDs) in the United States from January 2010 through December 2019. Extracted data included patient age and sex, injury characteristics (diagnosis, body region injured, time of year, and location where injury occurred), and hospital disposition. Using patient narratives, we recorded the cheerleading skills, settings, and mechanisms that led to injury. NEISS sample weights were used to derive national estimates (NEs) from actual case numbers.
Results:
From 2010 to 2019, a total of 9868 athletes (NE = 350,000; 95% CI, 250,000-450,000) aged 5-25 years presented to US EDs for cheerleading injuries. The annual number of injuries decreased by 15%, from 982 (NE = 35,000; 95% CI, 27,000-44,000) to 897 (NE = 30,000; 95% CI, 18,000-42,000) (P = .048), corresponding to a 27% decline in the injury rate per 100,000 cheerleaders (P < .01). The annual number of injuries caused by performing stunts decreased by 24%, from 240 (NE = 8700; 95% CI, 6700-11,000) to 216 (NE = 6600; 95% CI, 4000-9200) (P = .01), with a 36% decline in the corresponding injury rate per 100,000 cheerleaders (P < .01). Despite these decreases, annual incidence of concussions/closed head injuries increased by 44%, from 128 (NE = 3800; 95% CI, 2900-4700) to 171 (NE = 5500; 95% CI, 3400-7700) (P = .02), and patients requiring hospital admission increased by 118%, from 18 (NE = 330; 95% CI, 250-410) to 24 (NE = 720; 95% CI, 440-1000) (P < .01). The hospital admission rate increased by 9.0% (P = .02).
Conclusion:
The number of cheerleading-related injuries presenting to US EDs decreased from 2010 to 2019. However, the incidence of concussions/closed head injuries and hospital admissions increased, suggesting that further measures are needed to improve safety for cheerleaders.
Keywords: cheerleading, closed head injury, concussion, emergency department, hospital admission
Cheerleading is one of the most popular sports in the United States, with more than 3 million participants annually. 26 The technical skills involved in cheerleading routines have continued to grow in difficulty, and the public’s awareness of the athleticism required has increased. 10,32,38 As the difficulty of the sport increases, cheerleaders have become more susceptible to injury. In 2012, approximately 37,344 pediatric cheerleading-related injuries presented to emergency departments (EDs) nationwide, corresponding to a rate of 64 injuries per 100,000 children and adolescents. 23 In addition to the high overall rate of injury, cheerleading also presents a high risk of catastrophic injury. 5,6,18,20 In fact, cheerleading injuries account for more than half of the catastrophic injuries experienced by female athletes at the high school and college levels, surpassing the rate of catastrophic injuries caused by football among male athletes. 22
Despite the indisputable risks of cheerleading, the sport receives less attention in the medical literature as compared with other sports of similar or lower risk level. 3,13,15,27 A lack of awareness of the physical demands of the sport may contribute to the limited cheerleading-related research, with multiple studies incorrectly characterizing cheerleading as a noncontact, individual (as opposed to team) sport. 19,28,31,43,46,49 Few epidemiologic studies have assessed cheerleading characteristics, 12,16,19,23,33,35 –37 with the most recent study performed analyzing data through 2012. 23 All of these studies have reported an increase in injury rates, which was speculated to relate to the sport’s increase in athleticism and a delayed implementation of safety measures. Recently, all levels of cheerleading, from elementary to collegiate and recreational to competitive, have undergone regulation changes. Many of these regulations were designed to increase safety without diminishing the athleticism of the sport and may result in changing injury patterns. 16,21
The primary purpose of our study was to assess cheerleading-related injury patterns from 2010 to 2019 in terms of athlete demographic characteristics, injury incidence annually and per 100,000 cheerleaders, injury type, body region injured, mechanism of injury, injury setting/event type, and disposition from the ED.
Methods
Data Sources
The National Electronic Injury Surveillance System (NEISS), operated by the Consumer Product Safety Commission (CPSC), is a public database of injuries that present to EDs in the United States. Information in this database is supplied by 100 hospitals, each with at least 6 beds and an ED, selected as a representative probability sample of the more than 5300 US hospitals with EDs. Each hospital has staff trained to enter injury codes, demographic data, and treatment plans for each patient. 30 Patients are deidentified and assigned CPSC codes that indicate the activity or product involved in injury. National estimates (NEs) can then be calculated by summing the number of cases presenting to each ED and using a multiplier based on hospital size and number of similar-sized hospitals across the United States. All database entries are also accompanied by a free-text narrative summarizing the patient encounter, which provides more detail for the context of injury.
For injury rates, the annual number of US cheerleaders was gathered from available Cheerleading Participation Reports produced by the Sports and Fitness Industry Administration (SFIA). 39 Participation data are reported by year and obtained via online interviews with a representative, nationwide sample. Results are then weighted to reflect the US population according to the US Census Bureau. SFIA reports have been used reliably in previous epidemiological studies to provide participation numbers for injury rate calculation. 8,17,41
Patient Cohort
This study was deemed exempt from approval by our institutional review board. Using the code 3254 (cheerleading activity, apparel, or equipment), we identified 10,097 cheerleading-related injuries that presented to NEISS EDs from 2010 to 2019. A total of 9868 cases were included in our analysis after 229 cases were excluded. Cases were excluded if the narrative indicated that injuries were from noncheerleading activities, such as gymnastics, dance, or drill/flag team participation, or that cheerleading only secondarily exacerbated a previous injury. Narratives revealing the diagnosis to be a condition in which sports participation would not influence presentation, such as appendicitis and anaphylaxis, were also excluded. The following text is an example of a narrative we included in our analysis: “12 YOF [12-year-old female] at cheerleading practice did back handspring landed awkwardly on R [right] foot dx [diagnosis] ankle sprain.” The following is an example of an excluded narrative: “11 YOF [11-year-old female] slipped and fell into a pool and injured foot then went to cheerleading and the foot pain got worse dx [diagnosis]: foot pain.” For narratives without sufficient details describing cheerleading-specific injury mechanism, setting, skill, or stunt position, cases were included and noted as “unknown” for the incomplete variables. All narrative interpretations were reviewed for accuracy by the first author (A.L.X.), who has more than 12 years of cheerleading experience.
Data Collection
Patient Characteristics
For each injury, we extracted data on patient sex and age. Age (with corresponding cheerleading level) was categorized as follows: 5-11 (elementary school level), 12-18 (middle/high school level), and 19-25 (collegiate level). The first 2 age groups also correspond to the most popular age range for all-star cheerleading (5-18 years). 44
Injury Setting
The season of injury was categorized as winter (December-February), spring (March-May), summer (June-August), or autumn (September-November). Setting where the injury occurred was categorized as school, place of sports/recreation, home, other setting (farm/ranch, street/highway, other public property, or industrial place), and unknown. From the patient narrative, we categorized cheerleading-specific settings as team practice, cheerleading camp, cheerleading competition, noncheerleading sports event (eg, football game), tryouts, “other” (including nonregulated situations in which cheerleading skills are performed, such as home), or unknown setting.
Injury Mechanism
Using the narrative for each case, we recorded 3 additional details about the cheerleading context that led to injury. First, we categorized the mechanism of injury as a fall, a collision with another athlete, a collision with an object, performing a skill incorrectly (such as landing a tumbling pass on an inverted ankle), overexertion, multiple mechanisms (involving >1 mechanism), or unknown mechanism. Second, we categorized cheerleading skills as “stunts” (including partner stunts, pyramids, and basket tosses, all of which involve 1 or more athletes supported by ≥1 other athlete), tumbling, jumps/kicks, nonspecific training (including stretching, running, and conditioning), or unknown skill. 45 Third, if the injury involved a stunt, the narrative was assessed to determine the patient’s position as a base (one who holds, lifts, or tosses another cheerleader; we also included spotters in this category, who protect the upper body of a top person [herein, “flyer”] during stunts) or a flyer (one who is supported during a stunt). 45
Injury Characteristics
Injury types were categorized as follows: concussion/closed head injury (CHI), dislocation, fracture, skin injury (laceration or avulsion), soft tissue injury (hematoma, abrasion, or contusion), sprain/strain, or other injury type. Injured body regions were categorized as head/neck (face, eye, ear, mouth, head, and neck); upper extremity (shoulder, upper and lower arm, elbow, wrist, hand, and finger); trunk (upper and lower trunk and pubic region); lower extremity (upper and lower leg, knee, ankle, foot, and toe); nonspecific region (multiple body regions involved); and unknown region. Joint involvement was also analyzed using the categories of ankle, elbow, knee, and wrist. (The NEISS coding manual does not have codes specific to shoulder and hip injuries of the joint itself.)
ED Disposition
Disposition from the ED was categorized as follows: released after evaluation with or without treatment, treated and admitted/transferred to another hospital/held for observation, left against medical advice, or dead on arrival to the ED.
Statistical Analysis
Data were analyzed using SPSS Statistics, Version 27.0 (IBM). NEs were calculated from actual case numbers using sample weights provided by the CPSC, which are based on ED size and geographic location. An estimate may be unstable if the estimated frequency is <1200, the actual sample size is <20, or the coefficient of variation is >30%. 24 All estimates reported herein are stable unless otherwise noted.
Injury rates per 100,000 cheerleaders were calculated by dividing annual national injury estimates from NEISS by annual national participation estimates from SFIA. A linear regression was performed to assess injury trends over time. Chi-square tests and calculation of relative risks (RRs) with 95% CIs were used to compare trends among age groups, cheerleading skills leading to injury, and stunt positions. P <.05 was considered significant.
Results
Demographic Characteristics
A total of 9868 cases, corresponding to a NE of 350,000 (95% CI, 250,000-450,000) patients (98% female) aged 5-25, were treated for cheerleading-related injuries in US EDs from 2010 to 2019, equating to approximately 35,000 (95% CI, 25,000-45,000) injuries per year. Mean patient age was 14 ± 3.6 years, with most patients (80%) aged 12-18 (Tables 1 and 2). When comparing data from 2010 and 2019, the proportion of patients aged 12-18 decreased significantly (from 81% to 76%; P < .01), whereas the proportions of patients in the younger and older categories increased. During the same period, the proportion of male patients increased significantly (from 1.4% to 3.4%; P < .01). Only 1598 patient narratives (16%) provided detail on all cheerleading-specific variables studied.
Table 1.
Patient and Injury Characteristics of Cheerleading-Related Injuries Among Athletes Aged 5-25 Years Treated in US EDs, NEISS (2010-2019) a
| Characteristic | No. of Cases | NE | |
|---|---|---|---|
| n (%) b | 95% CI | ||
| Study sample | 9868 | 350,000 (100) | 250,000-450,000 |
| Patient Characteristics | |||
| Age group, years c | |||
| 5-11 | 1815 | 56,000 (16) | 41,000-73,000 |
| 12-18 | 7704 | 280,000 (80) | 200,000-360,000 |
| 19-25 | 349 | 14,000 (3.9) | 10,000-17,000 |
| Sex | |||
| Female | 9644 | 340,000 (98) | 250,000-440,000 |
| Male | 224 | 7900 (2.2) | 5700-10,000 |
| Injury Characteristics | |||
| Injury type | |||
| Sprain/strain | 3731 | 130,000 (38) | 96,000-170,000 |
| Concussion/CHI | 1632 | 58,000 (16) | 42,000-74,000 |
| Fracture | 1200 | 42,000 (12) | 31,000-54,000 |
| Soft tissue | 1103 | 38,000 (11) | 28,000-49,000 |
| Skin | 236 | 8700 (2.5) | 6300-11,000 |
| Dislocation | 194 | 6700 (1.9) | 4900-8600 |
| Other | 1772 | 65,000 (18) | 47,000-83,000 |
| Body region injured | |||
| Head/neck | 3065 | 110,000 (31) | 79,000-140,000 |
| Upper extremity | 2773 | 100,000 (29) | 74,000-130,000 |
| Lower extremity | 2773 | 95,000 (27) | 69,000-120,000 |
| Trunk | 1111 | 39,000 (11) | 28,000-50,000 |
| Nonspecific | 124 | 4800 (1.4) | 3500-6100 |
| Unknown | 22 | 630 (0.18) d | 460-810 |
| Joint involvement | |||
| Ankle | 1176 | 40,000 (11) | 29,000-51,000 |
| Knee | 956 | 33,000 (9.5) | 24,000-42,000 |
| Wrist | 666 | 25,000 (7.2) | 18,000-51,000 |
| Elbow | 439 | 15,000 (4.4) | 11,000-20,000 |
| Disposition | |||
| Released from ED | 9586 | 340,000 (97) | 250,000-430,000 |
| Admitted/transferred | 228 | 8100 (2.3) | 5900-10,000 |
| Left against medical advice | 53 | 2000 (0.56) | 1400-2500 |
| Dead on arrival to ED | 1 | 4.8 (0.001) d | 3.5-6.1 |
a CHI, closed head injury; ED, emergency department; NE, national estimate; NEISS, National Electronic Injury Surveillance System.
b Percentages may not sum to 100 and estimates may not sum to 350,000 because of rounding error.
c Mean ± SD age was 14 ± 3.6 years.
d Potentially unstable estimate.
Table 2.
Further Injury Characteristics of Cheerleading-Related Injuries Among Athletes Aged 5-25 Years Treated in US EDs, NEISS 2010-2019 a
| Characteristic | No. of Cases | NE | |
|---|---|---|---|
| n (%) b | 95% CI | ||
| Cause of Injury | |||
| Mechanism | |||
| Fall | 3095 | 110,000 (31) | 80,000-140,000 |
| Collision with another athlete | 1881 | 68,000 (19) | 49,000-87,000 |
| Performing a skill incorrectly | 590 | 21,000 (5.9) | 15,000-26,000 |
| Overexertion | 336 | 12,000 (3.4) | 8600-15,000 |
| Multiple mechanisms | 301 | 10,000 (2.9) | 7400-13,000 |
| Collision with an object | 68 | 1900 (0.54) | 1400-2400 |
| Unknown | 3597 | 130,000 (37) | 94,000-160,000 |
| Skill | |||
| Stunt | 2498 | 89,000 (25) | 65,000-110,000 |
| Tumbling | 1094 | 40,000 (11) | 29,000-51,000 |
| Nonspecific training | 358 | 12,000 (3.5) | 8800-16,000 |
| Jump/kick | 218 | 7400 (2.1) | 5400-9400 |
| Unknown | 5700 | 200,000 (58) | 150,000-260,000 |
| Stunt position c | |||
| Base | 1084 | 39,000 (44) | 29,000-50,000 |
| Flyer | 970 | 34,000 (39) | 25,000-44,000 |
| Unknown | 442 | 15,000 (17) | 11,000-19,000 |
| Injury Setting | |||
| Location | |||
| Place of sports/recreation | 5075 | 180,000 (52) | 130,000-230,000 |
| School | 3096 | 110,000 (31) | 80,000-140,000 |
| Home | 111 | 3700 (1.1) | 2700-4800 |
| Other | 75 | 2800 (0.80) | 2000-3600 |
| Unknown | 1511 | 52,000 (15) | 38,000-67,000 |
| Setting | |||
| Practice | 3834 | 140,000 (39) | 98,000-170,000 |
| Cheerleading competition | 180 | 10,000 (2.9) | 7300-13,000 |
| Noncheerleading sports event | 196 | 6900 (2.0) | 5000-8800 |
| Cheerleading camp | 180 | 6500 (1.8) | 4700-8300 |
| Tryouts | 42 | 1600 (0.45) | 1100-2000 |
| Other | 56 | 1900 (0.54) | 1400-2400 |
| Unknown | 5260 | 190,000 (54) | 140,000-240,000 |
| Season d | |||
| Autumn | 4183 | 150,000 (44) | 110,000-200,000 |
| Winter | 2503 | 90,000 (25) | 65,000-110,000 |
| Spring | 1335 | 44,000 (12) | 32,000-55,000 |
| Summer | 1847 | 64,000 (18) | 46,000-82,000 |
a ED, emergency department; NE, national estimate; NEISS, National Electronic Injury Surveillance System.
b Percentages may not sum to 100 and estimates may not sum to 350,000 because of rounding error.
c For known stunt-related injuries, n = 2498.
d Autumn, September-November; winter, December-February; spring, March-May; summer, June-August.
Injury Incidence: Annually and per 100,000 Cheerleaders
From 2010 to 2019, the annual incidence of cheerleading-related injuries declined by 15%, from an estimated 35,000 (95% CI, 27,000-44,000) to 30,000 (95% CI, 18,000-42,000) (P = .048), and the rate of injury per 100,000 cheerleaders declined by 27% (P < .01). When analyzing the subset of injuries sustained when performing stunts, we found significant decreases in the annual number of injuries, from 8700 (95% CI, 6700-11,000) to 6600 (95% CI, 4000-9200) (24%; P = .01) and the rate per 100,000 cheerleaders (36%; P < .01) (Table 3).
Table 3.
Trends in Cheerleading-Related Injuries That Presented to US EDs, NEISS 2010-2019 a
| Parameter | 2010 | 2019 | Change From 2010 to 2019, % | Slope (m), n/year | P | ||
|---|---|---|---|---|---|---|---|
| No. of Cases | Estimate (95% CI) | No. of Cases | Estimate (95% CI) | ||||
| Incidence | |||||||
| Total injury | 982 | 35,000 (27,000-44,000) | 897 | 30,000 (18,000-42,000) | −15 | −730 | .048 |
| Stunt injury | 240 | 8700 (6700-11,000) | 216 | 6600 (4000-9200) | −24 | −290 | .01 |
| Concussion/CHI | 128 | 3800 (2900-4700) | 171 | 5500 (3400-7700) | 44 | 250 | .02 |
| Admission | 18 | 330 b (250-410) | 24 | 720 b (440 -1000) | 120 | 70 | <.01 |
| Rate c | |||||||
| Total injury | 1100 (840 -1300) | 800 (490-1100) | −27 | −470 | <.01 | ||
| Stunt injury | 270 (210-330) | 180 (110-250) | −36 | −12 | <.01 | ||
| Concussion/CHI | 120 (91-150) | 150 (90-210) | 24 | Nonlinear | .21 | ||
| Admission | 10 (7.8-13) | 19 (12-27) | 9.0 | 1.6 | .02 | ||
a CHI, closed head injury; ED, emergency department; NEISS, National Electronic Injury Surveillance System.
b Potentially unstable estimate.
c Rate per 100,000 cheerleaders.
Injury Setting
Most injuries occurred at a place for sports/recreation (52%); 31% occurred at school, and 1.1% occurred in homes. Injuries were most commonly sustained during cheerleading practice (39%) (Table 2). When comparing data from 2010 and 2019, we found an increase in the annual percentage of injuries occurring during practice (from 32% to 49%; P < .01). Injuries occurred most frequently during autumn (44%).
Injury Mechanism
Falls accounted for 31% of injuries, followed by collisions between 2 athletes (19%) and landing a skill incorrectly (5.9%). Regarding cheerleading skills, injuries were caused most commonly by stunts (25%), followed by tumbling (11%). Of the stunt-related injuries, 44% occurred to bases and 39% to flyers.
Stunts were more likely than other skills to result in injury to the head/neck (RR, 1.8; 95% CI, 1.8-1.9) and to cause concussion/CHI (RR, 2.1; 95% CI, 2.1-2.2). Injury patterns were also significantly different between stunt positions (base vs flyer) for all body regions and injury types (P < .01) except head/neck injuries (P = .21). Bases were more likely to sustain wrist injuries (RR, 4.8; 95% CI, 4.4-5.2), injuries to the upper extremity (RR, 1.8, 95% CI, 1.8-1.9), and sprains/strains (RR, 1.5; 95% CI, 1.5-1.6). Meanwhile, flyers were more likely to sustain ankle injuries (RR, 7.9; 95% CI, 7.1-8.8), lower-extremity injuries (RR, 3.4; 95% CI, 3.2-3.6), and concussions/CHIs (RR, 1.5; 95% CI, 1.5-1.6). Compared with other cheerleading skills, tumbling was 1.8 (95% CI, 1.8-1.8) times as likely to result in upper-extremity injury. When tumbling, risks of injuries were higher to the elbow (RR, 2.8; 95% CI, 2.7-2.9) and wrist (RR, 1.3; 95% CI, 1.3-1.4). Tumbling was also 1.9 (95% CI, 1.9-2.0) times as likely to result in fractures compared with all other skills combined. The proportion of total injuries from collisions with another athlete decreased from 19% in 2010 to 17% in 2019 (P < .01), whereas the proportion caused by performing a skill incorrectly increased from 2.4% to 8.4% (P < .01). Injuries from tumbling increased as well (7.3% to 11%; P < .01). Notably, the proportion of injuries occurring among bases versus flyers was not significantly different (P = .29).
Injury Characteristics
Injury Types
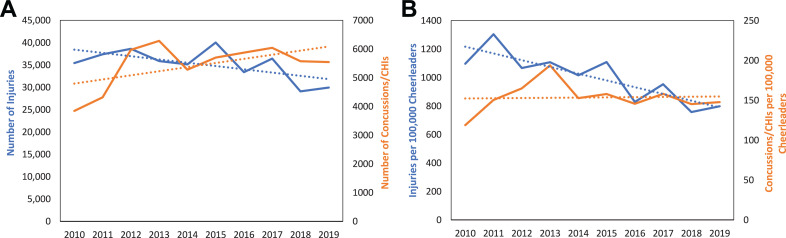
Sprains/strains accounted for 38% of all injuries, followed by concussions/CHIs (16%), fractures (12%), and soft tissue injuries (11%) (Table 1). The incidence of concussions/CHIs increased by 44% (P = .02) (Figure 1). We found no significant change in the concussion/CHI rate per 100,000 cheerleaders (P = .21). The proportion of annual injuries comprising fractures decreased from 12% in 2010 to 9.3% in 2019 (P < .01). Similarly, sprains/strains decreased from 44% to 33% (P < .01). The proportion of annual injuries occurring at places of sports/recreation, such as gymnasiums, increased from 37% in 2010 to 54% in 2019 (P < .01).
Figure 1.
Comparison of total cheerleading-related injuries versus concussions/CHI that presented to US EDs from 2010 to 2019. (A) Annual concussion/CHI numbers continued to increase despite decreasing total injury incidence from 2010 to 2019. (B) Total injury rate per 100,000 cheerleaders decreased, whereas the concussion/CHI rate remained stable during the study period. Blue line, total injury; CHI, closed head injuries; yellow line, concussion/CHI.
Distribution according to age group differed significantly for all injury types (P < .01), except skin injuries (P = .19). Patients aged 5-11 were 1.15 (95% CI, 1.1-1.2) times as likely as patients aged 12-18 and 1.3 (95% CI, 1.2-1.3) times as likely as patients aged 19-25 to be diagnosed with a concussion/CHI. Patients aged 12-18 were 1.2 (95% CI, 1.2-1.2) times as likely to sustain fractures than the other 2 age groups combined, and patients aged 19-25 were 1.1 (95% CI, 1.1-1.2) times as likely to sustain sprains/strains than the other 2 age groups combined.
Injured Body Regions
Injuries to the head/neck were the most common (31%), followed by the upper extremities (29%), lower extremities (27%), and trunk (11%). Joint injuries accounted for 32% of all injuries, with ankle injuries being the most common (11%) (Table 1). Distribution by age group differed significantly for all joint injuries and body regions (P < .01), except for trunk injuries (P = .13). Lower-extremity injuries were most common among patients aged 19-25 (31%), whereas head/neck injuries were most common among patients aged 5-11 (32%). Patients aged 19-25 were 1.2 (95% CI, 1.1-1.2) times as likely to sustain lower-extremity injuries as younger patients. Patients aged 5-11 were 1.1 (95% CI, 1.1-1.1) times as likely as patients aged 19-25 to sustain head/neck injuries. When comparing data from 2010 and 2019, we found significant increases in the percentages of head/neck injuries (28%-33%) and lower-extremity injuries (27%-31%) and a significant decrease in upper-extremity injuries (32%-25%) (P < .01 for all).
ED Disposition
Most injured cheerleaders (97%) were released from the ED after evaluation. Overall, 2.3% were admitted, kept for observation, or transferred to another medical facility, and 0.56% left against medical advice. One patient was dead on arrival to the ED in 2019 after falling from a stunt during competition. Table 4 lists cases that led to hospital admission. The annual number of patients admitted/transferred to a hospital increased significantly by 118% (P < .01), and the admission rate per 100,000 cheerleaders increased by 9.0% (P = .02) (Table 3).
Table 4.
Cheerleading-Related Injuries That Presented to US EDs and Required Hospital Admission/Transfer, NEISS 2010-2019 a
| Type of Injury | No. of Cases |
|---|---|
| Head, neck, or spine | 96 |
| Concussion/CHI | 50 |
| Skull/facial fracture | 10 |
| Vertebral fracture | 9 |
| Sprain/strain | 6 |
| Contusion | 4 |
| Unspecified pain or injury | 17 |
| Upper extremity | 87 |
| Fracture | |
| Forearm | 32 |
| Elbow | 24 |
| Humerus | 20 |
| Hand/wrist | 5 |
| Dislocation | 2 |
| Sprain/strain | 1 |
| Unspecified pain or injury | 3 |
| Lower extremity | 18 |
| Tibial/fibular fracture | 7 |
| Ankle/foot fracture | 3 |
| Femoral fracture | 2 |
| Slipped capital femoral epiphysis | 2 |
| Sprain/strain | 1 |
| Unspecified pain or injury | 3 |
| Other b | 29 |
a CHI, closed head injury; ED, emergency department; NEISS, National Electronic Injury Surveillance System.
b Other injuries were asthma, heat exhaustion, cardiac arrhythmia, rhabdomyolysis, seizures, chest pain, and syncope.
Discussion
Understanding the profile of sport injuries demanding acute care is critical for implementing safety protocols and aiding physicians in advising on sport participation. From 2010 to 2019, an estimated 350,000 athletes aged 5-25 years presented to EDs in the United States for cheerleading-related injuries. The annual number of injured athletes declined significantly by 15%, but the numbers of concussions/CHIs and hospital admissions increased significantly. The distribution of injuries also shifted to favor male patients, occur at places of sports/recreation, and result from tumbling. To our knowledge, our study is the first report a national decrease in cheerleading injuries over time.
The most recent and comprehensive analysis of NEISS data included data from 1990 to 2012. Naiyer et al 23 reported a 243% increase in cheerleading injury incidence during the 23-year period, citing a rise in the number of cheerleaders and increase in sport athleticism as primary explanations. From 2010 to 2019, cheerleading has continued to increase in the difficulty of stunts and tumbling skills being performed. The sport has also expanded, with participation rising from 3.2 million in 2010 to nearly 3.8 million in 2019. 26 Despite these trends, we found a significant 27% reduction in injury rate when accounting for the number of cheerleaders participating annually in the sport.
As the risks associated with cheerleading have become more apparent, the number of rule changes designed to increase safety for recreational, scholastic, and all-star cheerleaders of all experience levels has increased. For example, 2 recent safety regulations instituted by USA Cheer (the national governing body of cheerleading) 25 increase the number of athletes involved in tossing and catching flyers when performing inverted skills (when flyers’ feet are held above their heads) during a pyramid and require a spotter for stunts involving only 1 base. These changes were enacted in 2018, which is the year for which we found the largest decrease in injury incidence and rate. Regulations typically target stunts, likely because of evidence suggesting that basket tosses and pyramids are the skills most likely to cause injury. 4,6,9 This focus of recent regulations on stunts is consistent with our finding that the number of injuries caused by stunts declined significantly during the past decade. This explanation also aligns with the findings of Yau et al, 47 who reported a 4-fold reduction in catastrophic cheerleading injuries after the implementation of a rule prohibiting the performance of basket tosses on hard surfaces during the 2006-2007 cheerleading season. Together, these results suggest the effectiveness of national organizations’ efforts to enhance safety.
Despite the overall decrease in national injury incidence, we found a continued increase in the incidence of cheerleading-related concussions/CHIs. This finding aligns with those of previous studies, which report a high and increasing risk of concussions/CHIs as cheerleading has developed. 42,47 Our findings are consistent with previous findings of stunts as the primary skills placing athletes at risk of concussions/CHIs, 33 with flyers having a significantly higher risk than bases. The high rates of concussion/CHI may reflect increased reporting, or they may indicate that the increased regulation cannot eliminate the inherent risk associated with the sport. It is essential to note that concussion rates in other sports during the same period also increased, but increased mostly to a lesser extent than we found for cheerleading. 2,7,14,29,50 Thus, although universal factors, such as increased diagnosis and sensitivity, may partially explain our temporal trends, cheerleading-specific elements likely play a role. Moreover, the continued increase in concussions/CHIs may explain the significantly higher number of patients who were admitted or transferred after ED evaluation in 2019. Except for fractures, which decreased significantly during the study period, concussions/CHIs were the most common diagnosis requiring inpatient care. Concussions/CHIs accounted for 22% of hospital admissions between 2010 and 2019. This represents an increase since 2002-2007, when Jacobson et al 12 reported only 7 cases of CHI and no concussions requiring hospital admission (13% of total admissions) during that period. The increase we found may also reflect greater vigilance and caution of health care providers in risk stratifying head injuries, particularly in children, because the consequences of such injuries have been a featured point of sports medicine in recent years. 11
Furthermore, our findings reflect changes in the sport. A larger proportion of injuries occurred in male cheerleaders in 2019 compared with 2010, aligning with an increase in participation by boys and men. 48 From 1990 to 2012, most injuries occurred at schools. 23 From 2010 to 2019, most injuries occurred at places of sports/recreation, such as private gymnasiums, with an increase from 37% to 54%. This shift may reflect increased participation in competitive cheerleading, such as all-star programs, that require nonscholastic practice settings. This transition may be associated with a rise in attention to this type of cheerleading in the media. In contrast to common beliefs, 9,33,34 bases have a similar or higher risk of injury than flyers. This is consistent with our results, with 44% of stunting injuries occurring to bases versus 39% to flyers. The number of tumbling injuries also increased during the study period. These findings may reflect that many regulations target the safety of flyers. 1 Increasing focus on bases and tumbling skills during safety training may help further reduce injury rates.
The results of our study are limited by the information contained in the NEISS database, which may not be generalizable to a larger population given its small hospital sample size. A small proportion of entries provided data on all variables studied because narratives were often vague and did not describe the full extent of the circumstances surrounding the injury. Narratives and our interpretation of them are also prone to error, so the accuracy of cheerleading-specific variables derived from narratives may be especially limited. The lack of specificity of the narratives precluded more detailed analysis, such as distinguishing among basket tosses, pyramids, and partner stunts, or determining the type of cheerleading (recreational, scholastic, or all-star) involved. Another inherent weakness is that the NEISS database does not account for individuals who sustain multiple injuries and does not provide information that would enable control of confounding factors, such as coach certification and athlete experience. Furthermore, the NEISS data set does not include minor or chronic injuries or fatal, onsite injuries. More experienced cheerleaders have a high incidence of overuse injuries, but these injuries are typically treated in a clinic rather than an ED. 40 Thus, the numbers provided by NEISS are likely an underestimation of the true incidence of injury in cheerleaders. Finally, the SFIA participation reports cover participants aged 6 years or older, which may include athletes older than 25, and would omit those who are 5 years old. As a result, the annual injury rates presented may be under- or overestimations, but this would be true for data of all years, and the important trends reported would remain.
Our study provides an update on recent injury patterns in cheerleading and shows the progress made during the past decade regarding safety in a sport known to cause injury. Although overall annual injury numbers have decreased, the incidence of severe acute injuries continues to rise. Increased education on injury prevention is needed for coaches and athletes alike, particularly regarding concussions/CHIs. Health care providers should also be aware of the sport’s prevalent injuries and the circumstances surrounding them to better counsel these athletes. Our study suggests that cheerleading demands more attention in sports medicine, and our findings can serve as a foundation for future studies of cheerleading injury risk.
Acknowledgment
For their editorial assistance, the authors thank Jenni Weems, MS, Kerry Kennedy, BA, and Rachel Box, MS, in the Editorial Services group of the Johns Hopkins Department of Orthopaedic Surgery.
Footnotes
Final revision submitted April 21, 2021; accepted May 25, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.J.L. has received education payments from Arthrex and hospitality payments from Vericel. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by John Hopkins University (IRB00258468).
References
- 1. American Association of Cheerleading Coaches and Administrators. 2018-2019 AACCA School Cheer Safety Rules. Accessed September 24, 2020. https://www.misshsaa.com/wp-content/uploads/2018/08/2018-19-AACCA-School-Cheer-Safety-Rules.pdf
- 2. Amoo-Achampong K, Rosas S, Schmoke N, et al. Trends in sports-related concussion diagnoses in the USA: a population-based analysis using a private-payor database. Phys Sportsmed. 2017;45(3):239–244. [DOI] [PubMed] [Google Scholar]
- 3. Bagnulo A. Cheerleading injuries: a narrative review of the literature. J Can Chiropr Assoc. 2012;56(4):292–298. [PMC free article] [PubMed] [Google Scholar]
- 4. Boden BP. Direct catastrophic injury in sports. J Am Acad Orthop Surg. 2005;13(7):445–454. [DOI] [PubMed] [Google Scholar]
- 5. Boden BP, Prior C. Catastrophic spine injuries in sports. Curr Sports Med Rep. 2005;4(1):45–49. [DOI] [PubMed] [Google Scholar]
- 6. Boden BP, Tacchetti R, Mueller FO. Catastrophic cheerleading injuries. Am J Sports Med. 2003;31(6):881–888. [DOI] [PubMed] [Google Scholar]
- 7. Buzas D, Jacobson NA, Morawa LG. Concussions from 9 youth organized sports: results from NEISS hospitals over an 11-year time frame, 2002-2012. Orthop J Sports Med. 2014;2(4):2325967114528460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Buzzacott P, Schiller D, Crain J, Denoble PJ. Epidemiology of morbidity and mortality in US and Canadian recreational scuba diving. Public Health. 2018;155:62–68. [DOI] [PubMed] [Google Scholar]
- 9. Currie DW, Fields SK, Patterson MJ, Comstock RD. Cheerleading injuries in United States high schools. Pediatrics. 2016;137(1):e20152447. doi:10.1542/peds.2015-2447 [DOI] [PubMed] [Google Scholar]
- 10. Greenspan RE. Cheer shows competitive cheerleading is almost as dangerous as football. So why isn’t it officially considered a sport? Accessed February 8, 2021. https://time.com/5782136/cheer-netflix-cheerleading-dangers/
- 11. Homme JJL. Pediatric minor head injury 2.0: moving from injury exclusion to risk stratification. Emerg Med Clin North Am. 2018;36(2):287–304. [DOI] [PubMed] [Google Scholar]
- 12. Jacobson NA, Morawa LG, Bir CA. Epidemiology of cheerleading injuries presenting to NEISS hospitals from 2002 to 2007. J Trauma Acute Care Surg. 2012;72(2):521–526. [DOI] [PubMed] [Google Scholar]
- 13. Jones S, Almousa S, Gibb A, et al. Correction to: Injury incidence, prevalence and severity in high-level male youth football: a systematic review. Sports Med. 2019;49(12):1901. [DOI] [PubMed] [Google Scholar]
- 14. Kerr ZY, Chandran A, Nedimyer AK, et al. Concussion incidence and trends in 20 high school sports. Pediatrics. 2019;144(5):e20192180. [DOI] [PubMed] [Google Scholar]
- 15. Kilic O, Maas M, Verhagen E, Zwerver J, Gouttebarge V. Incidence, aetiology and prevention of musculoskeletal injuries in volleyball: a systematic review of the literature. Eur J Sport Sci. 2017;17(6):765–793. [DOI] [PubMed] [Google Scholar]
- 16. LaBella CR, Mjaanes J. Cheerleading injuries: epidemiology and recommendations for prevention. Pediatrics. 2012;130(5):966–971. [DOI] [PubMed] [Google Scholar]
- 17. Lemme NJ, Ready L, Faria M, et al. Epidemiology of boxing-related upper extremity injuries in the United States. 2018;46(4):503–508. [DOI] [PubMed] [Google Scholar]
- 18. Luckstead EF, Patel DR. Catastrophic pediatric sports injuries. Pediatr Clin North Am. 2002;49(3):581–591. [DOI] [PubMed] [Google Scholar]
- 19. McCarthy MM, Bihl JH, Frank RM, et al. Epidemiology of clavicle fractures among US high school athletes, 2008-2009 through 2016-2017. Orthop J Sports Med. 2019;7(7):2325967119861812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mueller FO. Catastrophic head injuries in high school and collegiate sports. J Athl Train. 2001;36(3):312–315. [PMC free article] [PubMed] [Google Scholar]
- 21. Mueller FO. Cheerleading injuries and safety. J Athl Train. 2009;44(6):565–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mueller FO, Cantu RC. Catastrophic Sports Injury Research. Accessed September 24, 2020. http://nccsir.unc.edu/files/2014/05/2011Allsport.pdf
- 23. Naiyer N, Chounthirath T, Smith GA. Pediatric cheerleading injuries treated in emergency departments in the United States. Clin Pediatr (Phila). 2017;56(11):985–992. [DOI] [PubMed] [Google Scholar]
- 24. National Electronic Injury Surveillance System (NEISS) Online. Explanation of NEISS Estimates Obtained Through the CPSC Web-site. Accessed September 24, 2020. https://www.cpsc.gov/cgibin/NEISSQuery/webestimates.html
- 25. National Governing Body for Sport Cheering in the United States. USA Cheer’s Position Paper on Cheer Safety & Title IX. Accessed September 24, 2020. https://www.usacheer.org/safety/positionpaper
- 26. Outdoor Foundation. 2019 Outdoor Participation Report. Accessed September 25, 2020. https://outdoorindustry.org/resource/2019-outdoor-participation-report/
- 27. Pfirrmann D, Herbst M, Ingelfinger P, Simon P, Tug S. Analysis of injury incidences in male professional adult and elite youth soccer players: a systematic review. J Athl Train. 2016;51(5):410–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pfister T, Pfister K, Hagel B, Ghali WA, Ronksley PE. The incidence of concussion in youth sports: a systematic review and meta-analysis. Br J Sports Med. 2016;50(5):292–297. [DOI] [PubMed] [Google Scholar]
- 29. Schallmo MS, Weiner JA, Hsu WK. Sport and sex-specific reporting trends in the epidemiology of concussions sustained by high school athletes. J Bone Joint Surg Am. 2017;99(15):1314–1320. [DOI] [PubMed] [Google Scholar]
- 30. Schroeder T, Ault K. The NEISS sample (design and implementation) 1997 to present. Accessed September 24, 2020. https://cpsc.gov/s3fs-public/pdfs/blk_media_2001d011-6b6.pdf
- 31. Schulz MR, Marshall SW, Mueller FO, et al. Incidence and risk factors for concussion in high school athletes, North Carolina, 1996-1999. Am J Epidemiol. 2004;160(10):937–944. [DOI] [PubMed] [Google Scholar]
- 32. Sherman E. Why don’t more people consider competitive cheerleading a sport? The rigorous activity is dominated by female athletes—and is growing in legitimacy and popularity. Accessed February 8, 2021. https://www.theatlantic.com/entertainment/archive/2017/05/why-dont-more-people-consider-competitive-cheerleading-a-sport/524940/
- 33. Shields BJ, Fernandez SA, Smith GA. Epidemiology of cheerleading stunt-related injuries in the United States. J Athl Train. 2009;44(6):586–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shields BJ, Smith GA. Cheerleading-related injuries in the United States: a prospective surveillance study. J Athl Train. 2009;44(6):567–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Shields BJ, Smith GA. Cheerleading-related injuries to children 5 to 18 years of age: United States, 1990-2002. Pediatrics. 2006;117(1):122–129. [DOI] [PubMed] [Google Scholar]
- 36. Shields BJ, Smith GA. Epidemiology of cheerleading fall-related injuries in the United States. J Athl Train. 2009;44(6):578–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shields BJ, Smith GA. Epidemiology of strain/sprain injuries among cheerleaders in the United States. Am J Emerg Med. 2011;29(9):1003–1012. [DOI] [PubMed] [Google Scholar]
- 38. Smith M. Cheerleading has changed, so should our attitudes. Accessed February 11, 2021. https://www.espn.com/espnw/news/story/_/id/6579788/cheerleading-changed-our-attitude
- 39. Sports & Fitness Industry Association. Cheerleading Participation Report 2020. Accessed September 24, 2020. https://www.sfia.org/reports/808_Cheerleading-Participation-Report-2020
- 40. Stracciolini A, Casciano R, Friedman HL, Meehan WP III, Micheli LJ. A closer look at overuse injuries in the pediatric athlete. Clin J Sport Med. 2015;25(1):30–35. [DOI] [PubMed] [Google Scholar]
- 41. Swain TA, McGwin G. Yoga-related injuries in the United States from 2001 to 2014. Orthop J Sports Med. 2016;4(11):2325967116671703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Tsushima WT, Siu AM, Ahn HJ, Chang BL, Murata NM. Incidence and risk of concussions in youth athletes: comparisons of age, sex, concussion history, sport, and football position. Arch Clin Neuropsychol. 2019;34(1):60–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Tsushima WT, Siu AM, Yamashita N, Oshiro RS, Murata NM. Comparison of neuropsychological test scores of high school athletes in high and low contact sports: a replication study. Appl Neuropsychol Child. 2018;7(1):14–20. [DOI] [PubMed] [Google Scholar]
- 44. U.S. All Star Federation. 2020-2021 USASF Cheer Age Grid. Accessed April 14, 2021. https://rules.usasfmembers.net/wp-content/uploads/2020/05/USASF_Cheer_Age-Grid_20-21.pdf
- 45. U.S. All Star Federation. USASF Glossary, 2015-16. Accessed October 27, 2020. https://usasf.net.ismmedia.com/ISM3/std-content/repos/Top/2013%20Website/Safety/docs/USASF_15-16_Cheer_Glossary.pdf
- 46. Wells EK, Chin AD, Tacke JA, Bunn JA. Risk of disordered eating among Division I female college athletes. Int J Exerc Sci. 2015;8(3):256–264. [PMC free article] [PubMed] [Google Scholar]
- 47. Yau RK, Dennis SG, Boden BP, et al. Catastrophic high school and collegiate cheerleading injuries in the United States: an examination of the 2006-2007 basket toss rule change. Sports Health. 2019;11(1):32–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Young B. More male students sign up for high school cheerleading squads. Accessed September 24, 2020. https://www.rrstar.com/article/20130130/NEWS/301309735
- 49. Young TE, Chen M. One-year concussion prevalence in Marion County, Florida high school athletes. J Chiropr Med. 2016;15(3):204–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Zuckerman SL, Kerr ZY, Yengo-Kahn A, et al. Epidemiology of sports-related concussion in NCAA athletes from 2009-2010 to 2013-2014: incidence, recurrence, and mechanisms. Am J Sports Med. 2015;43(11):2654–2662. [DOI] [PubMed] [Google Scholar]