Abstract
Background
Intensive care unit (ICU) patients age 90 years or older represent a growing subgroup and place a huge financial burden on health care resources despite the benefit being unclear. This leads to ethical problems. The present investigation assessed the differences in outcome between nonagenarian and octogenarian ICU patients.
Methods
We included 7900 acutely admitted older critically ill patients from two large, multinational studies. The primary outcome was 30-day-mortality, and the secondary outcome was ICU-mortality. Baseline characteristics consisted of frailty assessed by the Clinical Frailty Scale (CFS), ICU-management, and outcomes were compared between octogenarian (80–89.9 years) and nonagenarian (> 90 years) patients. We used multilevel logistic regression to evaluate differences between octogenarians and nonagenarians.
Results
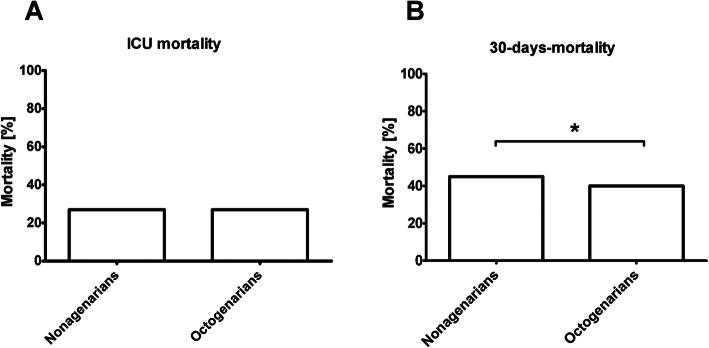
The nonagenarians were 10% of the entire cohort. They experienced a higher percentage of frailty (58% vs 42%; p < 0.001), but lower SOFA scores at admission (6 + 5 vs. 7 + 6; p < 0.001). ICU-management strategies were different. Octogenarians required higher rates of organ support and nonagenarians received higher rates of life-sustaining treatment limitations (40% vs. 33%; p < 0.001). ICU mortality was comparable (27% vs. 27%; p = 0.973) but a higher 30-day-mortality (45% vs. 40%; p = 0.029) was seen in the nonagenarians. After multivariable adjustment nonagenarians had no significantly increased risk for 30-day-mortality (aOR 1.25 (95% CI 0.90–1.74; p = 0.19)).
Conclusion
After adjustment for confounders, nonagenarians demonstrated no higher 30-day mortality than octogenarian patients. In this study, being age 90 years or more is no particular risk factor for an adverse outcome. This should be considered– together with illness severity and pre-existing functional capacity - to effectively guide triage decisions.
Trial registration
NCT03134807 and NCT03370692.
Keywords: Octogenarians, Nonagenarians, Frailty, Intensive care medicine, Outcome
Introduction
The proportion of older patients has increased significantly over time. In 2030, there will be more than 30 million people over the age of 90 (nonagenarians) in 35 industrialised countries [1]. Consequently, health care providers nowadays perform medical procedures on very old patients (from surgery to oncological therapies), which were previously considered unfeasible because of age or age-related deterioration in physical and mental performance [2]. Similarly, the rate of older patients (> 80 years) in intensive care units (ICU) is increasing [3–6]. Today, older patients utilise a disproportionate amount of health care resources compared to their relative proportion of the total population [3, 7].
In particular, the extent to which “old age” per se is a risk factor and the extent to which different groups of old patients differ from one another regarding the prognosis is the subject of continuing debate. Older patients suffer worse outcomes than younger patients undergoing intensive care [8, 9], but some studies failed to establish age as an independent predictor of mortality in older ICU patients [10, 11]. However, most prognostic studies demonstrated an almost linear relationship between chronological age and mortality after the age of 40 [12]. In this respect, patients ageing 80 years and more represent a particular challenge to intensive care medicine [13, 14]. Still, there are no large studies that further differentiate this group of very old ICU patients and it is unclear if being a nonagenarian is a risk factor for adverse outcomes. We hypothesize that critically ill nonagenarians have an elevated 30-day mortality compared to octogenarians. To address this hypothesis, we performed a retrospective cohort study comprised of two large, multinational prospective observational cohorts [13–15]. This post-hoc analysis combined data from the VIP-1 and VIP-2 studies to compare octo- and nonagenarians regarding 30-day mortality (primary outcome) and ICU mortality (secondary outcome), the distribution of risk factors, and the intensive care management [13–15].
Methods
Study subjects
The very old intensive care patients (VIP) studies, VIP1 and VIP2, were prospective, multi-centre studies, registered on ClinicalTrials.gov (ID: NTC03134807, NCT03370692). Both studies included very old intensive care patients (VIPs), defined as patients admitted to an ICU and aged 80 years or older. The main results from these studies have been published previously [13, 14, 16, 17]. In summary, for both studies, each participating ICU could include either consecutive patients admitted over a six-month period or the first 20 consecutive patients fulfilling the inclusion criteria (all patients aged 80 years or older). The data collection for VIP1 took place between October 2016 and February 2017 and between May 2018 to May 2019 for VIP2. Both studies used similar inclusion criteria as described elsewhere [13]. Informed consent was obtained from study participants. Local ethical committees might have waived the need of informed consent.
In this post-hoc analysis of these two studies, all patients admitted acutely (non-electively) with complete data on age, gender, clinical frailty score (CFS), sequential organ failure assessment (SOFA) score, and ICU mortality were included. For this study, the elective patients included in VIP1 were excluded as their outcomes differ significantly compared with those admitted acutely, as previously shown [18]. The primary endpoint of this study was ICU-mortality, and the secondary endpoint was 30-day-mortality.
Scales, scores, and limitations in life-sustaining therapy
The SOFA score was recorded on admission; it could be calculated manually or using an online calculator. Frailty was assessed by the clinical frailty scale (CFS). The CSF distinguishes nine classes of frailty from very fit (CFS 1) to terminally ill (CFS 9). The respective visual and simple description for this assessment tool was used with permission [19–21].
The Katz Activities of Daily Living (Katz ADL) scale is a widely used graded instrument to assess disability in chronically ill or older patients. It evaluates six primary and psychosocial functions: bathing, dressing, going to the toilet, transferring, feeding, and continence. The patient receives 1 point for every independent and 0 for every dependent activity (6 = independent patient, 0 = very dependent patient). For the patients in the VIP2 trial, disability was defined by Katz ADL score ≤ 4.
For cognitive decline, VIP2 utilised the Short form of Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE). IQCODE is a questionnaire, completed by carers, with 16 questions about cognitive decline over the past 10 years. For each question, 1 to 5 points can be assigned. An average of 3 points per question is considered “normal”. A cumulative IQCODE of ≥3.5 is regarded as “cognitive decline” [19–21].
The burden of co-morbidity was assessed using the co-morbidity and polypharmacy score (CPS) [22]. The CPS calculates the total number of chronic diagnoses and drugs taken. Standard ICU procedures were also documented.
In addition, limitations of therapy, such as withholding or withdrawing treatment, were recorded. Withholding life-sustaining therapy (e.g. mechanical ventilation, renal replacement therapy, cardiopulmonary resuscitation) was defined as not performing a measure that was indicated; withdrawing was defined as stopping any kind of life-sustaining therapy. All these decisions were at the discretion of the treating physicians and documented according to international recommendations. VIP2 recorded the exact date of treatment limitation, but VIP1 did not give specific details. Thus, the present analysis used withholding or withdrawing treatment as binary information at any time during the ICU-stay.
Statistical analysis
Post-hoc power calculations using the 7110 octogenarians and 790 nonagenarians, primary outcome event rates of 40% versus 45%, and an alpha of 0.05, the power of the study to detect differences in 30-day mortality is 77%. Continuous data points are expressed as median ± interquartile range. Differences between independent groups were calculated using the Mann Whitney U-test. Categorical data are expressed as numbers (percentage). The chi-square test was applied to calculate differences between groups. Sensitivity analysis, analysing only patients with SOFA scores below the 75th percentile SOFA score of 10 (i.e. all patients with SOFA < 10) was performed. Univariable and multivariable logistic regression analysis was performed to assess associations with treatment limitations and mortality. Odds ratios (OR) and adjusted odds ratios (aOR) with respective 95% confidence intervals (CI) were calculated. Two sequential random effects, multilevel logistic regression models were used to evaluate the impact of being a nonagenarian on ICU- and 30-days- mortality. All patients with valid data on ICU-mortality were included. First, a baseline model with being nonagenarian as a fixed effect and ICU as random effect (model-1) was fitted. Second, to model-1, patient characteristics (SOFA, CFS, sex) (model-2) were added to the model. Adjusted odds ratios (aOR) with respective 95% confidence intervals (CI) were calculated. Sensitivity analysis, analysing only patients with and without any treatment limitation was performed. All tests were two-sided, and a p-value of < 0.05 was considered statistically significant. SPSS version 23.0 (IBM, USA) and MedCalc Statistical Software version 19.1.3 (MedCalc Software bv, Ostend, Belgium; https://www.medcalc.org; 2019) were used for all statistical analyses.
Results
Study population
This study included 7900 patients. 10% of the patients were nonagenarians. Table 1 displays the baseline characteristics of nonagenarians versus octogenarians. Nonagenarians were predominantly female (57% versus 46%, p < 0.001), evidenced higher rates of frailty (58% vs 42%; p < 0.001), disability (44% vs. 26%; p < 0.001) and cognitive decline (50% vs. 31%; p < 0.001) but lower SOFA scores at admission (6 + 5 vs. 7 + 6; p < 0.001). Specific ICU-treatment strategies were used, with octogenarians receiving higher rates of organ support (renal replacement therapy, mechanical ventilation, vasoactive drugs), while for nonagenarians there were higher rates of treatment limitation (40% vs. 33%; p < 0.001; Table 1). After discharge from the ICU, most patients had a treatment limitation; 1053 octogenarians (55% of all octogenarians leaving the ICU alive) and 182 (85%) nonagenarians left the ICU with treatment limitations in place.
Table 1.
Baseline characteristics in the total cohort, nonagenarians versus octogenarians
| nonagenarians | octogenarians | p-value | |
|---|---|---|---|
| n = 790 | n = 7110 | ||
| Male sex n (%) | 339 (43%) | 3812 (54%) | < 0.001 |
| Age | |||
| median (±IQR) | 91 (90–93) | 83 (81–86) | < 0.001 |
| Frailty Score - CFS | |||
| median (±IQR) | 5 (4–6) | 4 (3–6) | < 0.001 |
| Frailty (CFS > 4) n (%) | 454 (58) | 2962 (42) | < 0.001 |
| ADL | |||
| median (±IQR) | 5 (3–6) | 6 (4–6) | < 0.001 |
| Disability (ADL ≤4) | 151 (44) | 805 (26) | < 0.001 |
| IQCODE | |||
| median (±IQR) | 3.5 (3–4) | 3.2 (3–4) | < 0.001 |
| Cognitive Decline (IQCODE ≥3.5) | 149 (50) | 812 (31) | < 0.001 |
| SOFA score | 6 (4–9) | 7 (4–10) | < 0.001 |
| median (±IQR) | |||
| ICU length of stay (hours) | |||
| median (±IQR) | 84 (24–117) | 54 (37–186) | < 0.001 |
| Treatment withdrawn and/or withheld (%) | 312 (40) | 2302 (33) | < 0.001 |
| NIV n (%) | 168 (21) | 1794 (23) | 0.03 |
| Intubation n (%) | 324 (41) | 3685 (52) | < 0.001 |
| Renal replacement therapy n (%) | 33 (4) | 816 (12) | < 0.001 |
| Vasoactive drugs n (%) | 414 (52) | 4179 (59) | 0.002 |
| Admission diagnosis n (%) | < 0.001 | ||
| Respiratory failure | 155 (20) | 1745 (23) | |
| Circulatory failure | 136 (17) | 968 (14) | |
| Combined circulatory & respiratory failure | 104 (13) | 825 (12) | |
| Sepsis | 74 (9) | 966 (14) | |
| Multitrauma w/o Head Injury | 23 (3) | 128 (2) | |
| Trauma with Head Injury | 18 (2) | 124 (2) | |
| Head Injury | 29 (4) | 166 (2) | |
| Intoxication | 1 (< 1) | 36 (< 1) | |
| Cerebral Injury (Non-Traumatic) | 38 (5) | 469 (7) | |
| Emergency Surgery | 91 (12) | 817 (12) | |
| Other | 91 (12) | 866 (12) | |
CFS Clinical Frailty Scale, SOFA Sequential Organ Failure Assessment, ADL Activity of Daily Life measured with the Katz index, IQCODE Informant Questionnaire on COgnitive Decline in the Elderly, ICU Intensive Care Unit, NIV Non-Invasive Ventilation, SD Standard Deviation
Survival analysis in the total cohort
The overall ICU mortality was 27% (N = 2134 of 7900 patients), the 30-day-mortality was 39% (N = 3080 of 7555 patients). Compared to the octogenarians the nonagenarians had a similar ICU mortality (27% vs. 27%; p = 0.973), but a higher 30-day-mortality (45% vs. 40%; p = 0.029, Fig. 1). Nonagenarians showed a significantly longer length of ICU-stay (84 h versus 54 h, p < 0.001).
Fig. 1.
Comparison of 30-day and ICU-mortality. A: ICU-mortality [%], B: 30-day-mortality [%]. * = p < 0.05
Comparison of nonagenarians versus octogenarians in the multilevel logistic regression models
After the adjustment for the ICU cluster as a random effect (model-1), nonagenarians had an increased risk for withholding life-sustaining therapy (aOR 1.54 (95% CI 1.22–1.94; p = < 0.001)), but not for withdrawal (aOR 1.03 (95% CI 0.77–1.39; p = 0,82)). Nonagenarians received significantly less mechanical ventilation, renal replacement therapy and vasoactive drugs. There was no difference between both age groups regarding the use of mechanical ventilation, vasopressors, and ICU-mortality, but an increased risk for 30-day-mortality (aOR 1.39 (95% CI 1.13–1.72); p = 0.002). After adding patient-specific confounders (model-2), nonagenarians demonstrated no significant risks compared to octogenarians (Table 2)
Table 2.
Associations of primary exposure (being nonagenarian) with mortality and management strategies in a multilevel logistic regression model
| octogenarians | nonagenarians | p-value | model-1 | model-2 | |
|---|---|---|---|---|---|
| Treatment withheld | 27% (1945) | 35% (279) | < 0.001 |
aOR 1.54 (95% CI 1.22–1.94; p = < 0.001) |
aOR 0.95 (95% CI 0.67–1.36; p = 0.79) |
| Treatment withdrawn | 14% (1026) | 13% (102) | 0.24 |
aOR 1.03 (95% CI 0.77–1.39; p = 0.82) |
aOR 0.73 (95% CI 0.48–1.10; p = 0.13) |
| NIV | 25% (1794) | 21% (168) | 0.014 |
aOR 0.79 (95% CI 0.61–1.03; p = 0.08) |
aOR 0.85 (95% CI 0.59–1.22; p = 0.36) |
| Mechanical Ventilation | 52% (3685) | 41% (324) | < 0.001 |
aOR 0.72 (95% CI 0.56–0.93; p = 0.01) |
aOR 1.26 (95% CI 0.85–1.87; p = 0.26) |
| RRT | 11% (816) | 4% (33) | < 0.001 |
aOR 0.32 (95% CI 0.19–0.53; p = < 0.001) |
aOR 0.55 (95% CI 0.28–1.08; p = 0.08) |
| Vasoactive drugs | 59% (4179) | 52% (414) | < 0.001 |
aOR 0.74 (95% CI 0.58–0.95; p = 0.017) |
aOR 0.90 (95% CI 0.60–1.35; p = 0.62) |
| 30d Mortality | 40% (2743) | 44% (337) | 0.029 |
aOR 1.39 (95% CI 1.13–1.72); p = 0.002) |
aOR 1.25 (95% CI 0.90–1.74; p = 0.19) |
| ICU-Mortality | 27% (1921) | 27% (213) | 0.97 |
aOR 1.10 (95% CI 0.87–1.40); p = 0.43) |
aOR 0.91 (95% CI 0.63–1.32; p = 0.63) |
NIV Non-Invasive Ventilation, RRT renal replacement therapy, ICU Intensive Care Unit, aOR Adjusted Odds Ratio, 95% CI 95% Confidence Interval
Model 1 - ICU cluster (the patient’s individual ICU) as random effect
Model 2 - Model 1 plus patient level (SOFA, CFS, age, sex)
Discussion
This study examines the largest multi-centre prospectively recruited group of intensive care patients of 90 years and older published to date. Nonagenarians differ in their baseline risk distribution, management, and clinical outcomes from octogenarians. Nonagenarians had higher rates of frailty, cognitive impairment, and disability. However, when compared with octogenarians, nonagenarians had a lower illness severity and required less organ support. After adjustment for relevant confounders, the 30-day mortality did not differ between both groups.
Our results are in line with other studies looking at older ICU patients: Fuchs et al. evaluated a cohort of more than 7000 surgical and medical ICU patients and found age, especially above 75 years, to be an independent risk factor for mortality [9, 23]. In a large retrospective analysis of 1,807,531 patients admitted to an ICU between 1997 and 2016, Jones et al. reported increased mortality in patients older than 84 years, although they had a similar illness severity at ICU admission compared to younger patients [23]. Conversely, in a study evaluating 5882 patients after cardiac arrest, age alone was only a weak predictor of mortality [24]. In a recent study by Roedl et al., a survival rate of 46% with a good neurological outcome was reported for nonagenarians after cardiac arrest [11]. Recently, Druwé et al. performed a subgroup analysis on out-of-hospital cardiac arrests with a special interest in the resuscitation attempts in octogenarians: Most physicians considered cardiopulmonary resuscitation to be appropriate even in older patients with poor outcome perspectives [25]. Furthermore, in another study by Becker et al., the ICU mortality of nonagenarians was low at 30% and, importantly, the one-year survival was 50%, indicating outcomes “better than expected” in nonagenarians [26]. Of note, the study by Becker et al. was a single-centre study, and the number of patients who received vasoactive drugs was lower when compared to the patients in our multi-centre study. Therefore, we propose the higher mortality rates reported in the present study may be more representative of a “real-world scenario”.
Demoule et al. performed a matched case-control study in 36 nonagenarians admitted to an ICU. They were matched according to sex with 72 controls: ICU admissions chosen from the 20- to 69-year age range. They found no differences in the reason for admission, but nonagenarians suffered significantly less from pre-existing co-morbidities. Advanced life-support interventions were used equally. ICU and intra-hospital mortality, as well as the length of stay, did not differ significantly between nonagenarians and the control group [27]. Despite differences in the absolute length of stay, the trend of a shorter length of stay for older (nonagenarian) intensive care patients is consistent with previous studies [28].
Interestingly, being a nonagenarian was independently associated with the decision for withholding life-sustaining therapy, but not for withdrawing it. After adjustment for patient characteristics, nonagenarians evidenced no particular risk for treatment limitations compared to octogenarians. These findings contradict the usual expectation that physicians in general tend to be more reluctant to provide organ support to nonagenarians compared to similarly sick octogenarians. In nonagenarians, ICU re-triage should be emphasised: after an initial intensive care treatment for up to 48 h, patients should be critically evaluated in cooperation with their family and/ or carers and discharged to a normal ward for best-supportive care if further intensive care seems unethical, unjustified, or unlikely to improve outcomes. However, modern intensive care medicine is not limited to life-sustaining measures. Even beyond invasive ventilation, renal replacement therapy or cardiopulmonary resuscitation, intensive care medicine can provide valuable treatment for the patient, which might be intensified palliative therapy. Based on our data, being a nonagenarian does not represent a particular risk factor for adverse outcomes. Application of ICU re-triage could help to reduce the economic burden of ICU care in very old patients, in addition to unethical intensive care and distress caused to health care providers.
Mortality was similar between octogenarians and nonagenarians at ICU discharge and after 30 days. The long-term outcomes of the VIP2 study are awaited and will answer the question of whether this effect remains stable further over time.
An important limitation is, that we have no information about pre-ICU triage decisions, although this might be an important factor for the differences in disease illness scores and frailty between nonagenarians and octogenarians. Furthermore, this study only provides detailed information up to ICU-discharge and there was a significant rise in mortality during the 30 days after ICU-discharge, but we do not have detailed data on decisions made and developments during this period. Another limitation is that no a priori sample size calculation was made to detect a difference in the mortality between nonagenarians and octogenarians. Our post-hoc power calculation shows that the present study is likely underpowered for the primary outcome, and thus the reporting results that are at a higher risk of false positive results. However, this was counterbalanced by using a multilevel model to adjust for relevant confounders.
Conclusion
Nonagenarian ICU patients demonstrated higher rates of frailty but had less acute organ dysfunction than octogenarians. After adjustment for multiple relevant confounders, nonagenarians did not suffer from worse outcomes compared to octogenarian ICU patients. Rather than being a nonagenarian, the severity of illness, functional capacity – and of course the patients’ will - should guide triage decisions.
Acknowledgements
VIP-2-STUDY GROUP:
| Hospital | City | ICU | Name |
Austria
| Medical University Innsbruck | Innsbruck | Division of Intensive Care and Emergency Medicine, Department of Internal Medicine | Michael Joannidis |
| Medical University Graz | Graz | Allgemeine Medizin Intensivstation | Philipp Eller |
| Medical University of Innsbruck | Innsbruck | Department of Neurology, Neurocritical Care Unit | Raimund Helbok |
| Hospital of St. John of God | Wienna | ICU B5 | René Schmutz |
Belgium
| AZ Maria Middelares Ghent | Ghent | Department of Intensive Care | Joke Nollet |
| OLVrouw Hospital Aalst | Aalst | Department of Intensive Care | Nikolaas de Neve |
| AZ Sint-Lucas | Ghent | Department of Intensive Care | Pieter De Buysscher |
| Ghent University Hospital | Ghent | Department of Intensive Care | Sandra Oeyen |
| AZ Sint-Blasius | Dendermonde | Department of Intensive Care | Walter Swinnen |
Croatia
| Clinical Hospital Centre Split | Split | Institute for Intensive Medicine | Marijana Mikačić |
Denmark
| Bispebjerg Hospital | Copenhagen | Intensiv Terapi Afsnit | Anders Bastiansen |
| Regionshospitalet Randers | Randers | ITA | Andreas Husted |
| Sygehus Lillebælt, Kolding Sygehus | Kolding | Bedøvelse og Intensiv | Bård E. S. Dahle |
| Aarhus University Hospital | Aarhus | Intensive Care East | Christine Cramer |
| Viborg Regional Hospital | Viborg | Department of Anaesthesiology and Intensive Care | Christoffer Sølling |
| Nordsjællands Hospital, University of Copenhagen | Hillerød | Department of Anaesthesiology and Intensive Care | Dorthe Ørsnes |
| Regions Hospital Herning | Herning | Intensiv Herning | Jakob Edelberg Thomsen |
| Vejle | Vejle | A710 Vejle | Jonas Juul Pedersen |
| Regionshospital Nordjylland Hjørring | Hjørring | Intensiv | Mathilde Hummelmose Enevoldsen |
| Aarhus University Hospital | Aarhus | Intensive Care North | Thomas Elkmann |
England
| Yeovil District Hospital | Yeovil | Intensive Care Unit | Agnieszka Kubisz-Pudelko |
| Peterborough City Hospital | Petersborough | Critical Care Unit | Alan Pope |
| Queen Elizabeth Hospital | Critical Care Queen Elizabeth Hospital | Amy Collins | |
| Croydon University Hospital | Croydon | Croydon University Hospital ITU | Ashok S. Raj |
| Royal Devon & Exeter NHS Foundation Trust | Exeter | Intensive Care Unit | Carole Boulanger |
| South Tyneside District Hospital | South Shields | ITU | Christian Frey |
| Maidstone | Maidstone | Intensive Care/High Dependency | Ciaran Hart |
| University Hospital Southampton | Southampton | General Intensive Care Unit | Clare Bolger |
| St George’s University Hospitals NHS Foundation trust | London | Cardiothoracic Intensive Care Unit (CTICU) | Dominic Spray |
| Norfolk and Norwich University Hospital | Norwich | Critical care complex | Georgina Randell |
| Royal Free Hospital NHS Foundation Trust | London | ICU 4 | Helder Filipe |
| Royal Liverpool University Hospital | Liverpool | Intensive care | Ingeborg D Welters |
| Royal Hampshire County Hospital | Winchester | ICU | Irina Grecu |
| St George’s University Hospitals NHS Foundation trust | London | Acute Dependency Unit | Jane Evans |
| Blackpool Victoria Hospital | Blackpool | General Critical Care Unit | Jason Cupitt |
| Worthing Hospital | Worthing | ICU | Jenny Lord |
| James Cook University Hospital | Midlesbrough | ICU 2 and 2 | Jeremy Henning |
| Tunbridge Wells Hospital | Pembury | Intensive care unit | Joanne Jones |
| St George’s University Hospitals NHS Foundation trust | London | Neuro Intensive Care | Jonathan Ball |
| James Paget University Hospital | Norfolk | ICU/HDU | Julie North |
| Royal Papworth Hospital NHS Foundation Trust | Cambridge | ICU | Kiran Salaunkey |
| Royal Sussex County Hospital | Brighton | Level 7 | Laura Ortiz-Ruiz De Gordoa |
| Salisbury | Salisbury | Radnor | Louise Bell |
| Royal Bolton Hospital | Bolton | Royal Bolton CRITICAL CARE | Madhu Balasubramaniam |
| Chelsea and Westminster Hospital | London | Adult Intensive Care Unit | Marcela Vizcaychipi |
| Countess of Chester Hospital | Chester | Intensive Care Unit | Maria Faulkner |
| Hampshire Hospitals Foundation Trust | Basingstoke | Basingstoke and North Hampshire Hospital | McDonald Mupudzi |
| Hinchingbrooke Hospital | Huntingdon | Critical Care | Megan Lea-Hagerty |
| Russells Hall Hospital | Dudley | Intensive Care Unit Russells Hall | Michael Reay |
| Royal Cornwall Hospital Trust | Cornwall | Critical Care Unit | Michael Spivey |
| Northern Devon Healthcare NHS Trust | Barnstaple | North Devon District Hospital | Nicholas Love |
| Chesterfield Royal Hospital | Chesterfield | Intensive Care Unit | Nick Spittle Nick Spittle |
| Royal Bournemouth Hospital | Bournemouth | Bournemouth Critical Care Unit | Nigel White |
| Dorset County | Dorchester | ICU DCH | Patricia Williams |
| Surrey and Sussex Healthcare NHS Trust | Redhill | East Surrey Hospital | Patrick Morgan |
| Darent Valley | Dartford | ICU | Phillipa Wakefield |
| Royal Surrey County Hospital | Guildford | Royal Surrey | Rachel Savine |
| Wirral University Teaching Hospital | Birkenhead | Critical care | Reni Jacob |
| Musgrove Park Hospital | Taunton | Critical care Unit | Richard Innes |
| Kent and Canterbury Hospital | Canterbury | K&C ITU | Ritoo Kapoor |
| West Suffolk NHS Foundation Trust | Bury St Edmunds | Critical Care | Sally Humphreys |
| QAH | Portsmouth | Dept Critical Care QAH (DCCQ) | Steve Rose |
| Whiston Hospital | Liverpool | Ward 4E | Susan Dowling |
| St George’s University Hospitals NHS Foundation trust | London | General Intensive care | Susannah Leaver |
| North Tees University Hospital | Stockton on Tees | Critical Care Unit | Tarkeshwari Mane |
| Bradford Teaching Hospitals NHS Foundation Trust | Bradford | Bradford Royal Infirmary | Tom Lawton |
| Medway Maritime Hospital | Medway | Adult Intensive Care Unit | Vongayi Ogbeide |
| University Hospital Lewisham | Lewisham | ICU/HDU Lewisham | Waqas Khaliq |
| St Richards Hospital | Chichester | Itchenor | Yolanda Baird |
France
| CH Francois Mitterand | Pau | Reanimation polyvalente | Antoine Romen |
| Hôpital Privé Claude Galien | Quincy sous Sénart | Polyvalente | Arnaud Galbois |
| Saint Antoine | Paris | Medecine Intensive Reanimation | Bertrand Guidet |
| Germon and Gauthier | Béthune | Médecine Intensive Réanimation | Christophe Vinsonneau |
| Hôpital Ambroise Paré | Boulogne Billancourt | Medecine Intensive Reanimation | Cyril Charron |
| CH Dr. Schaffner | Lens | Reanimation polyvalente | Didier Thevenin |
| Hopital Européen Georges Pompidou | Paris | Médecine Intensive Réanimation | Emmanuel Guerot |
| CHU de Besançon | Besançon | Département de Anesthésie Réanimation Chirurgicale | Guillaume Besch |
| Hôpital Cochin | Paris | Médecine Intensive Réanimation | Guillaume Savary |
| Victor Dupouy | Argenteuil | Service de Réanimation Polyvalente et USC | Hervé Mentec |
| Centre Hospitalier Général | Cambrai | Réanimation polyvalente | Jean-Luc Chagnon |
| Dieppe General Hospital | Dieppe | Médecine Intensive Réanimation | Jean-Philippe Rigaud |
| CHU Dijon Bourgogne | Dijon | Medecine intensive-Réanimation | Jean-Pierre Quenot |
| CH Bigorre | Tarbes | service de réanimation polyvalente | Jeremy Castanera |
| CH de Charleville-Mézières | Charleville-Mezieres | Medecine Intensive Reanimation | Jérémy Rosman |
| CHU Amiens | Amiens | Reanimaiton medicale | Julien Maizel |
| Groupe Hospitalier Paris Saint Joseph | Paris | Réanimation polyvalente | Kelly Tiercelet |
| CHU de Besançon | Besancon | Réanimation Médicale | Lucie Vettoretti |
| CH DAX | Dax | Réanimation polyvalente | Maud Mousset Hovaere |
| Louis Mourier | Colombes | Réanimation médico-chirurgicale | Messika Messika |
| Tenon | Paris | Service de Réanimation Médico Chirurgicale | Michel Djibré |
| Groupe Hospitalier Sud Ile de France | Melun | Département de médecine intensive | Nathalie Rolin |
| Clinique Du Millenaire | Montpellier | Reanimation Chirurugicale II et III | Philippe Burtin |
| Marne La Vallee | Jossigny | Reanimation Polyvalente | Pierre Garcon |
| CHU Lille | Lille | Critical Care Center | Saad Nseir |
| CHU de Caen | Caen | Service de Réanimation Médicale | Xavier Valette |
Germany
| Klinikum rechts der Isar TU München | München | Toxikologische Intensivstation | Christian Rabe |
| University Hospital Ulm | Ulm | Anesthesiologic Intensive Care Department | Eberhard Barth |
| Katholisches Krankenhaus St. Johann Nepomuk | Erfurt | Klinik für Innere Medizin II/ Kardiologie und Internistische Intensivmedizin | Henning Ebelt |
| Klinikum rechts der Isar, School of Medicine, Technical University of Munich | München | Intensivstation IS2/L2a | Kristina Fuest |
| Jena University Hospital, Department of Internal Medicine I | Jena | Internistische Intensivstation | Marcus Franz |
| West German Heart and Vascular Center Essen (WHGZ) | Essen | INTK | Michael Horacek |
| Universitätsmedizin der Johannes Gutenberg-Universität Mainz | Mainz | Anästhesie-Intensivstation | Michael Schuster |
| University Hospital Frankfurt | Frankfurt am Main | Department of Anaesthesiology, Intensive Care Medicine and Pain Therapy | Patrick Meybohm |
| University Hospital Düsseldorf | Düsseldorf | MI1/2 | Raphael Romano Bruno |
| Robert-Bosch-Krankenhaus | Stuttgart | 1D | Sebastian Allgäuer |
| Heidelberg University Hospital | Heidelberg | Station 13 IOPIS | Simon Dubler |
| Klinikum rechts der Isar, School of Medicine, Technical University of Munich | München | Intensivstation IS1 / M2b | Stefan J Schaller |
| University Hospital Leipzig | Leipzig | Department of Anesthesiology and Intensive Care Medicine | Stefan Schering |
| St Vincenz Hospital | Limburg/Lahn | Intensive care unit | Stephan Steiner |
| Hannover Medical School | Hannover | 44 | Thorben Dieck |
| Universitätsklinikum Knappschaftskrankenhaus Bochum | Bochum | Operative IBA | Tim Rahmel |
| Universitätsklinikum Schleswig-Holstein | Lübeck | IKI 12a | Tobias Graf |
Greece
| Asklepieio Voulas | Athens | ICU | Anastasia Koutsikou |
| Xanthi General Hospital | Xanthi | Xanthi ICU | Aristeidis Vakalos |
| Sismanoglio - Amallia Fleming G. H | Marousi - Athens Attika | Sismanoglio | Bogdan Raitsiou |
| General Hospital Agios Pavlos | Thessaloniki | ICU Agios Pavlos | Elli Niki Flioni |
| General Hospital of Larissa | Larissa | General ICU | Evangelia Neou |
| Lamia General Hospita | Lamia | Lamia ICU | Fotios Tsimpoukas |
| University Hospital of Ioannina | Ioannina | Intensive Care Unit | Georgios Papathanakos |
| General Hospital of Athens Korgialeneio Mbenakeio Red Cross | Athens | ICU | Giorgos Marinakis |
| General Hospital of Eleusis Thriassio | Eleusis | ICU Latsio | Ioannis Koutsodimitropoulos |
| KONSTANTOPOULEION GEN. HOSPITAL | Athens | General ICU | Kounougeri Aikaterini |
| Sotiria Hospital | Athens | ICU 1st Department of Pulmonary Medicine Athens Medical School, National and Kapodistrian University of Athens | Nikoletta Rovina |
| General Hospital of Patra | Achaia | ICU | Stylliani Kourelea |
| G Gennimatas Hospital of Thessaloniki | Thessaloniki | ICU G GENNIMATAS | Polychronis Tasioudis |
| Agioi Anargiroi Hospital | Athens | General ICU | Vasiiios Zidianakis |
| Theagenio | Theassaloniki | Meth Theagenio | Vryza Konstantinia |
| University General Hospital Ahepa | Thessaloniki | Metha | Zoi Aidoni |
Ireland
| Mater Misericordiae University Hospital | Dublin | Department of Critical Care Medicine | Brian Marsh |
|---|---|---|---|
| University Hospital Limerick | Limerick | UHL ICU | Catherine Motherway |
| University Hospital Galway | Galway | General ICU | Chris Read |
| St James’s Hospital | Dublin | ICU | Ignacio Martin-Loeches |
Italy
| Arnas Ospedale Civico De Christina Benfratelli | Palermo | Terapia Intensiva Polivalente Con Trauma Center | Andrea Neville Cracchiolo |
| Istituto Ortopedico Rizzoli | Bologna | TIPO | Aristide Morigi |
| San Giuseppe | Empoli | Terapia Intensiva | Italo Calamai |
| Humanitas Reseach Hospital | Milan | General ICU | Stefania Brusa |
Libya
| Al-Zawia University Hospital | Al-Zawia | ICU | Ahmed Elhadi |
| Alkhums Hospital | Alkhums | ICU | Ahmed Tarek |
| Elkhadra Hospital | Tripoli | ICU | Ala Khaled |
| Abo Selim Trauma Hospital | Tripoli | ICU | Hazem Ahmed |
| Tripoli Medical Center | Tripoli | CCU | Wesal Ali Belkhair |
Netherland
| Medisch Spectrum Twente | Enschede | Intensive Care Center | Alexander D. Cornet |
| Erasmus Medical Center | Rotterdam | ICU adults | Diederik Gommers |
| UMC Utrecht | Utrecht | ICU departement | Dylan de Lange |
| Albert Schweitzer Ziekenhuis | Dordrecht | ICU asz | Eva van Boven |
| Isala Hospital | Zwolle | Intensive Care | Jasper Haringman |
| Diakonessenhuis Utrecht | Utrecht | Intensive care | Lenneke Haas |
| Haga Ziekenhuis | The Hague | ICU | Lettie van den Berg |
| Canisius Wilhelmina Ziekenhuis | Nijmegen | C38 | Oscar Hoiting |
| Jeroen Bosch Ziekenhuis | Den Bosch | IC JBZ | Peter de Jager |
| Medical Centre Leeuwarden | Leeuwarden | Department of Intensive Care | Rik T. Gerritsen |
| Zuyderland Medical Center | Heerlen | Zuyderland Heerlen | Tom Dormans |
| University Medical Center Groningen | Groningen | Department of Critical Care | Willem Dieperink |
Norway
| Førde Central Hospital | Førde | Department of Emergency Medicine and Inensive Care | Alena Breidablik Alena Breidablik |
|---|---|---|---|
| Kongsberg | Kongsberg | Intensivavdelingen | Anita Slapgard |
| Sykehuset Østfold | Grålum | Intensiv | Anne-Karin Rime |
| Sykehuset Telemark | Skien | Intensiv Skien | Bente Jannestad |
| Haukeland University Hospital | Bergen | General ICU | Britt Sjøbøe |
| Ålesund | Ålesund | Medisinsk intensiv | Eva Rice |
| Ålesund hospital | Ålesund | Dept. Anesthesia and Intensive Care, Surgical ICU | Finn H. Andersen |
| Kristiansund sykehus Helse Møre og Romsdal HF | Kristiansund N | Intensiv Kristiansund | Hans Frank Strietzel |
| Namsos Sykehus | Namsos | Intensivavdeling | Jan Peter Jensen |
| Haukeland University Hospital | Bergen | Medisinsk intensiv og overvåkning (MIO) | Jørund Langørgen |
| Oslo University Hospital | Oslo | Intensive Care section Ullevaal | Kirsti Tøien |
| Stavanger University Hospital | Stavanger | Department of Intensive Care | Kristian Strand |
| Haugesund sjukehus | Haugesund | Intensivavdelingen | Michael Hahn |
| St Olavs University Hospital | Oslo | Hovedintensiv | Pål Klepstad |
Poland
| Szpital Wojewódzki w Bełchatowie | Bełchatów | Oddział Intensywnej Terapii | Aleksandra Biernacka |
|---|---|---|---|
| Heliodor Swiecicki Clinical Hospital at the Karol Marcinkowski Medical University in Poznan | Poznań | Anaesthesiology intensive care and pain treatment Department | Anna Kluzik |
| University Hospital in Zielona Góra | Zielona Góra | Clinical Department od Anesthesiology and Intensiv Care | Bartosz Kudlinski |
| Regional Teaching Hospital | Bielsko-Biała | Department of Anaesthesiology and Intensive Care | Dariusz Maciejewski |
| St. John Grande Hospital | Kraków | Oddział Anestezjologii i Intensywnej Terapii | Dorota Studzińska |
| The John Paul II Hospital | Krakow | Department of Anesthesiology and Intensive Care | Hubert Hymczak |
| Uniwersyteckie Centrum Kliniczne w Gdańsku | Gdańsk | Klinika Anestezjologii i Intensywnej Terapii | Jan Stefaniak |
| Pomeranian Medical University | Szczecin | Department of Anesthesiology and Intensive Care | Joanna Solek-Pastuszka |
| University Hospital in Cracow | Kraków | Anaesthesiology and Intensive Care Unit No.1 | Joanna Zorska |
| Regionalne Centrum Zdrowia w Lubinie | Lubin | Oddział Anestezjologii i Intensywnej Terapii | Katarzyna Cwyl |
| University Clinical Center Katowice | Katowice | Department of Anaesthesiology and Intensive Care - School of Medicine in Katowice, Medical University of Silesia | Lukasz J. Krzych |
| Teching Hospital No 2 | Szczecin | Department Anaesthesiology Intensive Therapy and Acute Poisoning | Maciej Zukowski |
| 4th Military Hospital in Wrocław | Wrocław | Anesthesia and Intensive Care Unit | Małgorzata Lipińska-Gediga |
| Centrum Chorób Płuc | Łódź | Oddział Anestezjologii i Intensywnej Terapii | Marek Pietruszko |
| The Dr. Wł. Biegański Regional Specialist Hospital in Łódź | Łódź | Department of Anaesthesiology and Intensive Therapy - Centre for Artificial Extracorporeal Kidney and Liver Support | Mariusz Piechota |
| Central Clinical Hospital CKD - University Medical College in Lodz | Lodz | Anaesthesia and Intensive Care Clinic | Marta Serwa |
| First Independent Teaching Hospital No. 1 | Lublin | II Department of Anesthesiology and Intensive Care | Miroslaw Czuczwar |
| Krakowski Szpital Specjalistyczny im. Jana Pawła II | Kraków | Thoracic Anaesthesia and Respiratory ICU | Mirosław Ziętkiewicz |
| Wroclaw Medical University | Wroclaw | Department of Anesthesiology and Intensve Therapy | Natalia Kozera |
| Szpital św.Anny W Miechowie | Miechów | Oddział Anestezjologii i Intensywnej Terapii | Paweł Nasiłowski |
| University Hospital in Krakow | Krakow | ICU Skawinska | Paweł Sendur |
| Infant Jesus Teaching Hospital | Warsaw | I Department of Anaesthesiology and Intensive Care | Paweł Zatorski |
| Regional Hospital in Bialystok | Bialystok | Department of Anaesthesiology and Intensive Care | Piotr Galkin |
| Opole University Hospital | Opole | Department of Anesthesiology and Intensive Care | Ryszard Gawda |
| University Hospital in Bialystok | Bialystok | Department of Anaesthesiology and Intensive Therapy | Urszula Kościuczuk |
| Dr Antoni Jurasz University Hospital in Bydgoszcz | Bydgoszcz | Department of Anesthesia and Critical Care | Waldemar Cyrankiewicz |
| Saint Lucas Hospital, Konskie | Konskie | Intensive Care Department | Wojciech Gola |
Portugal.
| Centro Hospitalar do Porto | Oporto | Serviço de Cuidados Intensivos 1 | Alexandre Fernandes Pinto |
|---|---|---|---|
| Hospital S. José, CHULC EPE | Lisboa | UCI Neurocríticos e Trauma | Ana Margarida Fernandes |
| Hospital São Francisco Xavier | Lisbon | Unidade Cuidados Intensivos Polivalente | Ana Rita Santos |
| Hospital da Luz | Lisboa | UCI Hospital da Luz | Cristina Sousa |
| Hospital de Viseu | Viseu | UCIP | Inês Barros |
| Hospital Professor Doutor Fernando Fonseca EPE | Amadora | Serviço de Medicina Intensiva SMI | Isabel Amorim Ferreira |
| Hospital Garcia de Orta - HGO | Almada | Serviço de Medicina Intensiva | Jacobo Bacariza Blanco |
| Hospital São Bernardo - CH Setúbal | Setúbal | Serviço de Cuidados Intensivos | João Teles Carvalho |
| Centro Hospitalar de Trás Montes e Alto Douro | Vila Real | Serviço de Medicina Intensiva | Jose Maia |
| Lusiadas Lisboa | Lisboa | UCI- Lusiadas | Nuno Candeias |
| CHMT-Abrantes | Abrantes | SMI | Nuno Catorze |
Russia.
| Privolzhskiy District Medical Center | Nizhniy Novgorod | Department of Anesthesiology and Intensive Care | Vladislav Belskiy |
Spain.
| Hospital De Bellvitge | Barcelona | UCI | Africa Lores |
|---|---|---|---|
| Hospital General Universitario de Albacete | Albacete | UCI Polivalente | Angela Prado Mira |
| Hospital Clinic of Barcelona | Barcelona | Respiratory Intensive Care Unit | Catia Cilloniz |
| Hospital Universitario Río Hortega | Valladolid | UVI Polivalente y Coronaria | David Perez-Torres |
| Universitario La Paz | Madrid | Surgical ICU | Emilio Maseda |
| General Universitario de Castellón | Castellón | Servicio de Medicina Intensiva | Enver Rodriguez |
| Hospital Universitario Río Hortega | Valladolid | UVI Neurocríticos Trauma y Quemados | Estefania Prol-Silva |
| Hospital de Tortosa Verge de la Cinta | Tortosa | Servei de Medicina Intensiva | Gaspar Eixarch |
| Parc Taulí | Sabadell | Parc Taulí | Gemma Gomà |
| Clínico Universitario de Valencia | Valencia | Surgical Intensive Care Unit | Gerardo Aguilar |
| Hospital Universitario de Torrejon | Torrejon de Ardoz, Madrid | Intensive Care UNit | Gonzalo Navarro Velasco |
| Hospital General de Catalunya | Barcelona | HGC | Marián Irazábal Jaimes |
| Hospital Universitario Sagrado Corazon | Barcelona | Intensive Care Unit | Mercedes Ibarz Villamayor |
| Hospital reina Sofía | Murcia | Reina Sofía | Noemí Llamas Fernández |
| Complejo Hospitalario de Segovia | Segovia | ICU Segovia | Patricia Jimeno Cubero |
| Universitario de Getafe | Getafe | Intensive Care and Burn Unit | Sonia López-Cuenca |
| Germans Trias i Pujol Hospital | Badalona | General ICU | Teresa Tomasa |
| Centralsjukhuset i Karlstad | Karlstad | IVA | Anders Sjöqvist |
Sweden.
| Umeå University | Umeå | Department of Surgical and Perioperative Sciences, Anestesiology and Intensive Care Medicine | Camilla Brorsson |
|---|---|---|---|
| Vrinnevisjukhuset | Norrköping | IVA Norrköping | Fredrik Schiöler |
| Sundsvall Hospital | Sundsvall | Sundsvall ICU | Henrik Westberg |
| Blekingesjukhuset | Karlskrona | Intensivvårdsavdelning 31 | Jessica Nauska |
| Alingsås Lasarett | Alingsås | Intensivvårdsavdelningen | Joakim Sivik |
| Västervikssjukhus | Västervik | IVA Västervikssjukhus | Johan Berkius |
| Sahlgrenska University Hospital/ Område 3/ Mölndals sjukhus | Göteborg | IVA avd 227 | Karin Kleiven Thiringer |
| Linköping University Hospital | Linköping | ICU Linköping | Lina De Geer |
| Linköping University Hospital | Linköping | Cardiothoracic Intensive Care Unit | Sten Walther |
Switzerland.
| Hopitaux Universitaires de Genève | Geneva | Adult Intensive Care Unit | Filippo Boroli |
|---|---|---|---|
| University of Bern Inselspital | Bern | Department of Intensive Care Medicine | Joerg C. Schefold |
| Fribourg Hospital | Fribourg | Intensive Care Unit | Leila Hergafi |
| Centre Hospitalier Universitaire Vaudois | Lausanne | Service de médecine intensive adulte | Philippe Eckert |
Turkey.
| Ordu University Training and Research Hospital | Ordu | General ICU | Ismail Yıldız |
Ukraine.
| Dnipro Mechnikov Regional Clinical Hospital | Dnipro | Intensive Care Unit of Polytrauma | Ihor Yovenko |
|---|---|---|---|
| European Wellness Academy, Luhansk Regional Clinical Hospital | Luhansk | ICU 1 | Yuriy Nalapko |
| European Wellness Academy, Luhansk Regional Clinical Hospital | Luhansk | ICU 2 | Yuriy Nalapko |
Wales.
| Glan Clwyd Hospital | Bodelwyddan | Critical Care | Richard Pugh |
Financial disclosure statement
No (industry) sponsorship has been received for this investigator-initiated study.
Authors’ contributions
BW, RRB and CJ analysed the data and wrote the first draft of the manuscript. HF and BG and DL contributed to statistical analysis and improved the paper. MK and AB and AM and FA and AA and SF and MC and SC and LF and ML and JM and BM and RM SO and CÖ and BP and IS and WS and AV and XW and SL and CB and SW and JS and MJ and YN and ME JF and TZ gave guidance and improved the paper. All authors read and approved the final manuscript.
Authors’ information
N/A
Funding
This study was endorsed by the ESICM. Free support for running the electronic database and was granted from the dep. of Epidemiology, University of Aarhus, Denmark. Financial support for creation of the e-CRF and maintenance of the database was possible from a grant (open project support) by Western Health region in Norway) 2018 who also funded the participating Norwegian ICUs. DRC Ile de France and URC Est helped conducting VIP2 in France. Open Access funding enabled and organized by Projekt DEAL.
Availability of data and materials
The anonymised data can be requested from the authors if required. The datasets analysed during the current study are not publicly available due to the different local institutional and/or licensing committees but are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The primary competent ethics committee was the Ethics Committee of the University of Bergen, Norway. A study protocol was provided to participating centres. Every participating centre obtained ethics approval according to local legislation. A copy of the ethics approval was sent to the study coordinator before start of the study. Institutional research ethic board approval was obtained from each study site. This was a prerequisite for participation in the study. All methods were carried out in accordance with relevant guidelines and regulations. All experimental protocols were approved by the local institutional and/or licensing committees. Written informed consent was obtained of all included subjects, except for patients from VIP2 of sites where study inclusion was explicitly granted without written informed consent. The inclusion of deceased patients was strictly in accordance with the requirements of the local competent ethics committees. In most cases, the consent of the patient or the legal guardian was mandatory (see above). The studies conducted were observational studies. No examinations (e.g. blood sampling) or tissue sampling took place.
Consent for publication
The manuscript does not contain any individual person’s data in any form.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Raphael Romano Bruno and Bernhard Wernly contributed equally to this work.
Contributor Information
Raphael Romano Bruno, Email: raphael.bruno@med.uni-duesseldorf.de.
Bernhard Wernly, Email: bernhard@wernly.at.
Malte Kelm, Email: malte.kelm@med.uni-duesseldorf.de.
Ariane Boumendil, Email: ariane.boumendil@gmail.com.
Alessandro Morandi, Email: morandi.alessandro@gmail.com.
Finn H. Andersen, Email: finn.andersen@ntnu.no
Antonio Artigas, Email: aartigas@tauli.cat.
Stefano Finazzi, Email: stefano.finazzi@marionegri.it.
Maurizio Cecconi, Email: Maurizio.cecconi@humanitas.it.
Steffen Christensen, Email: steffen.christensen@auh.rm.dk.
Loredana Faraldi, Email: loredana.faraldi@ospedaleniguarda.it.
Michael Lichtenauer, Email: m.lichtenauer@salk.at.
Johanna M. Muessig, Email: johanna.muessig@med.uni-duesseldorf.de
Brian Marsh, Email: bmarsh@mater.ie.
Rui Moreno, Email: r.moreno@mail.telepac.pt.
Sandra Oeyen, Email: Sandra.Oeyen@UGent.be.
Christina Agvald Öhman, Email: christina.agvald-ohman@sll.se.
Bernardo Bollen Pinto, Email: bernardo.bollenpinto@hcuge.ch.
Ivo W. Soliman, Email: i.w.soliman@umcutrecht.nl
Wojciech Szczeklik, Email: wojciech.szczeklik@uj.edu.pl.
Andreas Valentin, Email: Andreas.Valentin@ks-klinikum.at.
Ximena Watson, Email: ugm2xw@doctors.org.uk.
Susannah Leaver, Email: susannahleaver@nhs.net.
Carole Boulanger, Email: carole.boulanger@nhs.net.
Sten Walther, Email: sten.walther@telia.com.
Joerg C. Schefold, Email: joerg.schefold@insel.ch
Michael Joannidis, Email: Michael.joannidis@i-med.ac.at.
Yuriy Nalapko, Email: nalapko@ukr.net.
Muhammed Elhadi, Email: muhammed.elhadi.uot@gmail.com.
Jesper Fjølner, Email: jespfjoe@rm.dk.
Tilemachos Zafeiridis, Email: tilemachos@hotmail.com.
Dylan W. De Lange, Email: d.w.delange@umcutrecht.nl
Bertrand Guidet, Email: bertrand.guidet@aphp.fr.
Hans Flaatten, Email: hans.flaatten@uib.no.
Christian Jung, Email: Christian.Jung@med.uni-duesseldorf.de.
on behalf of the VIP2 study group, Email: contact@vipstudy.org.
on behalf of the VIP2 study group:
Michael Joannidis, Philipp Eller, Raimund Helbok, René Schmutz, Joke Nollet, Nikolaas de Neve, Pieter De Buysscher, Sandra Oeyen, Walter Swinnen, Marijana Mikačić, Anders Bastiansen, Andreas Husted, Bård E. S. Dahle, Christine Cramer, Christoffer Sølling, Dorthe Ørsnes, Jakob Edelberg Thomsen, Jonas Juul Pedersen, Mathilde Hummelmose Enevoldsen, Thomas Elkmann, Agnieszka Kubisz-Pudelko, Alan Pope, Amy Collins, Ashok S. Raj, Carole Boulanger, Christian Frey, Ciaran Hart, Clare Bolger, Dominic Spray, Georgina Randell, Helder Filipe, Ingeborg D. Welters, Irina Grecu, Jane Evans, Jason Cupitt, Jenny Lord, Jeremy Henning, Joanne Jones, Jonathan Ball, Julie North, Kiran Salaunkey, Laura Ortiz-Ruiz De Gordoa, Louise Bell, Madhu Balasubramaniam, Marcela Vizcaychipi, Maria Faulkner, Mc Donald Mupudzi, Megan Lea-Hagerty, Michael Reay, Michael Spivey, Nicholas Love, Nick Spittle Nick Spittle, Nigel White, Patricia Williams, Patrick Morgan, Phillipa Wakefield, Rachel Savine, Reni Jacob, Richard Innes, Ritoo Kapoor, Sally Humphreys, Steve Rose, Susan Dowling, Susannah Leaver, Tarkeshwari Mane, Tom Lawton, Vongayi Ogbeide, Waqas Khaliq, Yolanda Baird, Antoine Romen, Arnaud Galbois, Bertrand Guidet, Christophe Vinsonneau, Cyril Charron, Didier Thevenin, Emmanuel Guerot, Guillaume Besch, Guillaume Savary, Hervé Mentec, Jean-Luc Chagnon, Jean-Philippe Rigaud, Jean-Pierre Quenot, Jeremy Castanera, Jérémy Rosman, Julien Maizel, Kelly Tiercelet, Lucie Vettoretti, Maud Mousset Hovaere, Messika Messika, Michel Djibré, Nathalie Rolin, Philippe Burtin, Pierre Garcon, Saad Nseir, Xavier Valette, Christian Rabe, Eberhard Barth, Henning Ebelt, Kristina Fuest, Marcus Franz, Michael Horacek, Michael Schuster, Patrick Meybohm, Raphael Romano Bruno, Sebastian Allgäuer, Simon Dubler, Stefan J. Schaller, Stefan Schering, Stephan Steiner, Thorben Dieck, Tim Rahmel, Tobias Graf, Anastasia Koutsikou, Aristeidis Vakalos, Bogdan Raitsiou, Elli Niki Flioni, Evangelia Neou, Fotios Tsimpoukas, Georgios Papathanakos, Giorgos Marinakis, Ioannis Koutsodimitropoulos, Kounougeri Aikaterini, Nikoletta Rovina, Stylliani Kourelea, Polychronis Tasioudis, Vasiiios Zidianakis, Vryza Konstantinia, Zoi Aidoni, Brian Marsh, Catherine Motherway, Chris Read, Ignacio Martin-Loeches, Andrea Neville Cracchiolo, Aristide Morigi, Italo Calamai, Stefania Brusa, Ahmed Elhadi, Ahmed Tarek, Ala Khaled, Hazem Ahmed, Wesal Ali Belkhair, Alexander D. Cornet, Diederik Gommers, Dylan W. De Lange, Eva van Boven, Jasper Haringman, Lenneke Haas, Lettie van den Berg, Oscar Hoiting, Peter de Jager, Rik T. Gerritsen, Tom Dormans, Willem Dieperink, Alena Breidablik Alena Breidablik, Anita Slapgard, Anne-Karin Rime, Bente Jannestad, Britt Sjøbøe, Eva Rice, Finn H. Andersen, Hans Frank Strietzel, Jan Peter Jensen, Jørund Langørgen, Kirsti Tøien, Kristian Strand, Michael Hahn, Pål Klepstad, Aleksandra Biernacka, Anna Kluzik, Bartosz Kudlinski, Dariusz Maciejewski, Dorota Studzińska, Hubert Hymczak, Jan Stefaniak, Joanna Solek-Pastuszka, Joanna Zorska, Katarzyna Cwyl, Lukasz J. Krzych, Maciej Zukowski, Małgorzata Lipińska-Gediga, Marek Pietruszko, Mariusz Piechota, Marta Serwa, Miroslaw Czuczwar, Mirosław Ziętkiewicz, Natalia Kozera, Paweł Nasiłowski, Paweł Sendur, Paweł Zatorski, Piotr Galkin, Ryszard Gawda, Urszula Kościuczuk, Waldemar Cyrankiewicz, Wojciech Gola, Alexandre Fernandes Pinto, Ana Margarida Fernandes, Ana Rita Santos, Cristina Sousa, Inês Barros, Isabel Amorim Ferreira, Jacobo Bacariza Blanco, João Teles Carvalho, Jose Maia, Nuno Candeias, Nuno Catorze, Vladislav Belskiy, Africa Lores, Angela Prado Mira, Catia Cilloniz, David Perez-Torres, Emilio Maseda, Enver Rodriguez, Estefania Prol-Silva, Gaspar Eixarch, Gemma Gomà, Gerardo Aguilar, Gonzalo Navarro Velasco, Marián Irazábal Jaimes, Mercedes Ibarz Villamayor, Noemí Llamas Fernández, Patricia Jimeno Cubero, Sonia López-Cuenca, Teresa Tomasa, Anders Sjöqvist, Camilla Brorsson, Fredrik Schiöler, Henrik Westberg, Jessica Nauska, Joakim Sivik, Johan Berkius, Karin Kleiven Thiringer, Lina De Geer, Sten Walther, Filippo Boroli, Joerg C. Schefold, Leila Hergafi, Philippe Eckert, Ismail Yıldız, Ihor Yovenko, Yuriy Nalapko, and Richard Pugh
References
- 1.Kontis V, Bennett JE, Mathers CD, Li G, Foreman K, Ezzati M. Future life expectancy in 35 industrialised countries: projections with a Bayesian model ensemble. Lancet. 2017;389(10076):1323–1335. doi: 10.1016/S0140-6736(16)32381-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arenal JJ, de Teresa G, Tinoco C, Toledano M, Said A. Abdominal surgery in nonagenarians: short-term results. Surg Today. 2007;37(12):1064–1067. doi: 10.1007/s00595-007-3537-1. [DOI] [PubMed] [Google Scholar]
- 3.Boumendil A, Somme D, Garrouste-Orgeas M, Guidet B. Should elderly patients be admitted to the intensive care unit? Intensive Care Med. 2007;33(7):1252. doi: 10.1007/s00134-007-0621-3. [DOI] [PubMed] [Google Scholar]
- 4.Guidet B, de Lange DW, Flaatten H. Should this elderly patient be admitted to the ICU? Intensive Care Med. 2018;44(11):1926–1928. doi: 10.1007/s00134-018-5054-7. [DOI] [PubMed] [Google Scholar]
- 5.Flaatten H, Garrouste-Orgeas M. The very old ICU patient: a never-ending story. Intensive Care Med. 2015;41(11):1996–1998. doi: 10.1007/s00134-015-4052-2. [DOI] [PubMed] [Google Scholar]
- 6.Guidet B, Leblanc G, Simon T, Woimant M, Quenot JP, Ganansia O, Maignan M, Yordanov Y, Delerme S, Doumenc B, Fartoukh M, Charestan P, Trognon P, Galichon B, Javaud N, Patzak A, Garrouste-Orgeas M, Thomas C, Azerad S, Pateron D, Boumendil A, for the ICE-CUB 2 Study Network Effect of systematic intensive care unit triage on long-term mortality among critically ill elderly patients in France: a randomized clinical trial. JAMA. 2017;318(15):1450–1459. doi: 10.1001/jama.2017.13889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chin-Yee N, D'Egidio G, Thavorn K, Heyland D, Kyeremanteng K. Cost analysis of the very elderly admitted to intensive care units. Crit Care. 2017;21(1):109. doi: 10.1186/s13054-017-1689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ihra GC, Lehberger J, Hochrieser H, Bauer P, Schmutz R, Metnitz B, Metnitz PGH. Development of demographics and outcome of very old critically ill patients admitted to intensive care units. Intensive Care Med. 2012;38(4):620–626. doi: 10.1007/s00134-012-2474-7. [DOI] [PubMed] [Google Scholar]
- 9.Fuchs L, Chronaki CE, Park S, Novack V, Baumfeld Y, Scott D, McLennan S, Talmor D, Celi L. ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med. 2012;38(10):1654–1661. doi: 10.1007/s00134-012-2629-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Somme D, Maillet JM, Gisselbrecht M, Novara A, Ract C, Fagon JY. Critically ill old and the oldest-old patients in intensive care: short- and long-term outcomes. Intensive Care Med. 2003;29(12):2137–2143. doi: 10.1007/s00134-003-1929-2. [DOI] [PubMed] [Google Scholar]
- 11.Roedl K, Jarczak D, Becker S, Fuhrmann V, Kluge S, Muller J. Long-term neurological outcomes in patients aged over 90 years who are admitted to the intensive care unit following cardiac arrest. Resuscitation. 2018;132:6–12. doi: 10.1016/j.resuscitation.2018.08.020. [DOI] [PubMed] [Google Scholar]
- 12.Le Gall JR, Neumann A, Hemery F, Bleriot JP, Fulgencio JP, Garrigues B, et al. Mortality prediction using SAPS II: an update for French intensive care units. Crit Care. 2005;9(6):R645–R652. doi: 10.1186/cc3821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guidet B, de Lange DW, Boumendil A, Leaver S, Watson X, Boulanger C, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2019;132:6–12. [DOI] [PMC free article] [PubMed]
- 14.Flaatten H, De Lange DW, Morandi A, Andersen FH, Artigas A, Bertolini G, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (>/= 80 years) Intensive Care Med. 2017;43(12):1820–1828. doi: 10.1007/s00134-017-4940-8. [DOI] [PubMed] [Google Scholar]
- 15.D'Agostino RB., Jr Propensity scores in cardiovascular research. Circulation. 2007;115(17):2340–2343. doi: 10.1161/CIRCULATIONAHA.105.594952. [DOI] [PubMed] [Google Scholar]
- 16.Guidet B, Flaatten H, Boumendil A, Morandi A, Andersen FH, Artigas A, et al. Withholding or withdrawing of life-sustaining therapy in older adults (>/= 80 years) admitted to the intensive care unit. Intensive Care Med. 2018;44(7):1027–1038. doi: 10.1007/s00134-018-5196-7. [DOI] [PubMed] [Google Scholar]
- 17.Muessig JM, Nia AM, Masyuk M, Lauten A, Sacher AL, Brenner T, Franz M, Bloos F, Ebelt H, Schaller SJ, Fuest K, Rabe C, Dieck T, Steiner S, Graf T, Jánosi RA, Meybohm P, Simon P, Utzolino S, Rahmel T, Barth E, Schuster M, Kelm M, Jung C. Clinical frailty scale (CFS) reliably stratifies octogenarians in German ICUs: a multicentre prospective cohort study. BMC Geriatr. 2018;18(1):162. doi: 10.1186/s12877-018-0847-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jung C, Wernly B, Muessig JM, Kelm M, Boumendil A, Morandi A, Andersen FH, Artigas A, Bertolini G, Cecconi M, Christensen S, Faraldi L, Fjølner J, Lichtenauer M, Bruno RR, Marsh B, Moreno R, Oeyen S, Öhman CA, Pinto BB, Soliman IW, Szczeklik W, Valentin A, Watson X, Zafeiridis T, de Lange DW, Guidet B, Flaatten H, VIP1 study group. Electronic address: hans.flaatten@uib.no. A comparison of very old patients admitted to intensive care unit after acute versus elective surgery or intervention. J Crit Care. 2019;52:141–148. doi: 10.1016/j.jcrc.2019.04.020. [DOI] [PubMed] [Google Scholar]
- 19.Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173(5):489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jorm AF, Jacomb PA. The informant questionnaire on cognitive decline in the elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol Med. 1989;19(4):1015–1022. doi: 10.1017/S0033291700005742. [DOI] [PubMed] [Google Scholar]
- 21.Katz S. Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc. 1983;31(12):721–727. doi: 10.1111/j.1532-5415.1983.tb03391.x. [DOI] [PubMed] [Google Scholar]
- 22.Evans DC, Cook CH, Christy JM, Murphy CV, Gerlach AT, Eiferman D, Lindsey DE, Whitmill ML, Papadimos TJ, Beery PR, II, Steinberg SM, Stawicki SPA. Comorbidity-polypharmacy scoring facilitates outcome prediction in older trauma patients. J Am Geriatr Soc. 2012;60(8):1465–1470. doi: 10.1111/j.1532-5415.2012.04075.x. [DOI] [PubMed] [Google Scholar]
- 23.Jones A, Toft-Petersen AP, Shankar-Hari M, Harrison DA, Rowan KM. Demographic Shifts, Case Mix, Activity, and Outcome for Elderly Patients Admitted to Adult General ICUs in the United Kingdom, Wales, and Northern Ireland. Crit Care Med. 2020;48(4):466–474. doi: 10.1097/CCM.0000000000004211. [DOI] [PubMed] [Google Scholar]
- 24.Kim C, Becker L, Eisenberg MS. Out-of-hospital cardiac arrest in octogenarians and nonagenarians. Arch Intern Med. 2000;160(22):3439–3443. doi: 10.1001/archinte.160.22.3439. [DOI] [PubMed] [Google Scholar]
- 25.Druwe P, Benoit DD, Monsieurs KG, Gagg J, Nakahara S, Alpert EA, et al. Cardiopulmonary resuscitation in adults over 80: outcome and the perception of appropriateness by clinicians. J Am Geriatr Soc. 2020;68(1):39–45. doi: 10.1111/jgs.16270. [DOI] [PubMed] [Google Scholar]
- 26.Becker S, Muller J, de Heer G, Braune S, Fuhrmann V, Kluge S. Clinical characteristics and outcome of very elderly patients >/=90 years in intensive care: a retrospective observational study. Ann Intensive Care. 2015;5(1):53. doi: 10.1186/s13613-015-0097-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Demoule A, Cracco C, Lefort Y, Ray P, Derenne JP, Similowski T. Patients aged 90 years or older in the intensive care unit. J Gerontol A Biol Sci Med Sci. 2005;60(1):129–132. doi: 10.1093/gerona/60.1.129. [DOI] [PubMed] [Google Scholar]
- 28.Boumendil A, Aegerter P, Guidet B, Network CU-R. Treatment intensity and outcome of patients aged 80 and older in intensive care units: a multicenter matched-cohort study. J Am Geriatr Soc. 2005;53(1):88–93. doi: 10.1111/j.1532-5415.2005.53016.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The anonymised data can be requested from the authors if required. The datasets analysed during the current study are not publicly available due to the different local institutional and/or licensing committees but are available from the corresponding author on reasonable request.