Abstract
Cumulative studies have shown that metabolic reprogramming is a hallmark of malignant tumors. The emergence of technological advances, such as omics studies, has strongly contributed to the knowledge of cancer metabolism. Cervical cancer is among the most common cancers in women worldwide. Because cervical cancer is a virus-associated cancer and can exist in a precancerous state for years, investigations targeting the metabolic phenotypes of cervical cancer will enhance our understanding of the interference of viruses on host cells and the progression of cervical carcinogenesis. The purpose of this review was to illustrate metabolic perturbations in cervical cancer, the role that human papillomavirus (HPV) plays in remodeling cervical cell metabolism and recent approaches toward application of metabolomics in cervical disease research. Cervical cancer displays typical cancer metabolic profiles, including glycolytic switching, high lactate levels, lipid accumulation and abnormal kynurenine/tryptophan levels. HPV, at least in part, contributes to these alterations. Furthermore, emerging metabolomics data provide global information on the metabolic traits of cervical diseases and may aid in the discovery of biomarkers for diagnosis and therapy.
Keywords: Cervical cancer, HPV, p53, Metabolomics, Warburg effect
Introduction
Cervical cancer is the fourth most common cancer worldwide, and more than 500,000 new cases of cervical cancer are diagnosed annually with the number of deaths reaching 300,000 every year [1]. Human papillomavirus (HPV) infection is detected in 90% of cervical cancers. High-risk HPV (HR-HPV) is capable of inducing anogenital cancer. Of all the HR-HPV types, HPV16 (50–60%) and HPV18 (20%) are predominately found in cervical cancer cases [2]. A small fraction of individuals who develop persistent infection for over 2 years may develop squamous precursor lesions, which are divided into stage cervical intraepithelial neoplasia (CIN) 1–3 or low-grade/high-grade squamous intraepithelial lesions (LSILs/HSILs) [3]. A minority of high-grade lesions transform into invasive cancer if no intervention occurs [4].
Cervical cancer mainly metastasizes via lymphatic vessels and direct extension. Radical hysterectomy, radiotherapy and cisplatin-based chemotherapy are primary treatment options, yet specific schemes should be carefully considered according to cancer stage [5]. However, more than 30% of patients are radioresistant, and the recurrence of early-stage cervical cancer may be greater than 5% within 4.5 years [6, 7]. However, the current standard-of-care radiation therapy for locally advanced cervical cancer has not been improved for more than 30 years, and clinical outcomes have stagnated. Thus, the development of new treatment strategies is needed to enhance the therapeutic outcome [8, 9]. Several recent studies have indicated that metabolic reprogramming may effectively support cervical cancer therapy by increasing chemo- and radiosensitivity [10].
As early as the 1920s, Otto Warburg first observed that glucose consumption and lactate production in tumors are higher than those in normal tissues. This phenomenon is named the “Warburg effect”, which describes a metabolic feature of cancer in that cancer cells tend to gain energy by glycolysis instead of oxidative phosphorylation, even in the presence of oxygen. Currently, with an increasing number of studies expanding our understanding of cancer-associated metabolic alterations, reprogramming of metabolism has been considered a hallmark of cancer. In their elegant review in 2015, Pavlova and Thompson organized cancer-associated metabolic changes into six hallmarks [11]. Most cancers display several of these hallmarks, but different cancer types and even subtypes of certain cancers show variant metabolic phenotypes. An increasing number of studies are focusing on the metabolic traits of cervical cancer cells, providing novel indications for diagnosis and treatment.
In this literature review, we present recent advances in high-throughput technology to assess the metabolic characteristics of cervical cancer and related diseases. We then discuss metabolic changes and their impact on malignancy in cervical cancer as well as the potential mechanisms behind the alterations.
Metabolic alterations in cancers: to survive and thrive
An essential issue for cancer cells is to overcome environmental restriction and sustain rapid proliferation. Consequently, cancer cells rewire their metabolism to meet the need to survive and thrive. An increasing number of studies have described and explored the metabolic adaptations of cancer cells. Here, we summarize some of the most studied hallmarks of tumorigenesis-associated metabolic reprogramming.
Active aerobic glycolysis, namely, the “Warburg effect”, is commonly observed in cancers [12] and may be a strategy to gain advantages in the case of limited energy resources. At the same time, glycolytic intermediates support other biosynthesis processes, such as de novo serine synthesis and de novo lipid synthesis [13]. Moreover, the Warburg effect rebuilds the tumor microenvironment to facilitate cancer growth and immune evasion. Secreted lactate contributes to anti-inflammatory M2 tumor-associated macrophage polarization and inhibits tumor surveillance by T cells and natural killer (NK) cells [14, 15].
Lipid metabolism is markedly altered in rapidly proliferating cells. In cancer cells, fatty acids (FAs) are utilized in large part to synthesize sphingolipids and glycerophospholipids to produce cell membrane and signaling molecules. While most normal cells prefer exogenous FA for biosynthesis, de novo FA synthesis is greatly increased in cancer cells [16]. Blocking FA synthesis has been verified to be effective in limiting cancer growth in experimental animal models and may be a potential strategy in future clinical applications [17, 18]. In addition, some cancer cells exhibit increased fatty acid oxidation (FAO, also known as β-oxidation) activity, and FAs are mainly catabolized by FAO. FAO is required for the maintenance and chemoresistance of cancer stem cells, and it prevents detached cancer cells from anoikis, thus improving metastasis [19, 20].
Alterations in amino acids are increasingly being recognized. In mammalian cells, glutamine metabolism provides carbon for the biosynthesis of amino acids and FAs, and it provides nitrogen for nucleotide synthesis. Glutamine also functions in numerous biological processes, including bioenergetics, antioxidative defense mechanisms and cell signaling regulation [21]. Many types of cancer cells show increased consumption and dependence on glutamine, and some cancer-promoting pathways boost glutamine metabolism. For example, MYC upregulation increases glutamine metabolism enzymes and transporters; protein kinase Cζ (PKCζ) loss stimulates glutamine metabolism [22].
In addition to the features mentioned above, other features, including active nucleotide metabolism and other complex metabolic alterations, are also widely observed in cancers. In general, cancer cells promote biosynthesis pathways to produce cellular components and utilize multiple energy sources.
Current status of metabolomics in cervical disease research: potential tool for identifying diagnostic markers and therapeutic targets
Metabolomics is a field of omics science that has followed genomics, transcriptomics and proteomics. Metabolomics aims to analyze the metabolic profile of cells, body fluids or tissues, enabling the identification of diverse metabolites and exploration of intrinsic biological mechanisms. High-throughput, high-resolution and high-sensitivity technology has been extensively used in various areas, including human science, animal science, drug discovery, microbiology, plant biology, food chemistry and environmental science [23, 24]. Based on analytical chemistry techniques, the 3 leading platforms of metabolomics are nuclear magnetic resonance (NMR), gas chromatography mass spectrometry (GC–MS) and liquid chromatography mass spectrometry (LC–MS) [25]. Several studies have utilized metabolomics as a tool to investigate cervical HPV-related diseases, ranging from infection to lesion to invasive cancer. These descriptive studies have demonstrated evident metabolic alterations during the cervical malignancy process, indicating the significance of exploring the phenotypes, mechanism and impact of cervical cancer metabolic traits. The results are summarized in Table 1.
Table 1.
Metabolomic analyses in cervical lesions and cervical cancer
| Year | Group and sample size | Sample origin | Method | Major findings | References |
|---|---|---|---|---|---|
| 2008 | 5 normal cervix, 45 CIN, 23 cervical cancer | Biopsy specimens | HR-MAS MRS | 1. Choline and phosphocholine increased in cancer compared with high-grade CIN tissue 2. Phosphoethanolamine was increased in cancer compared with normal tissue 3. Alanine and creatine were reduced in normal tissue from cancer patients compared with normal tissue from non-cancer patients 4. Choline was increased in CIN tissue from cancer patients compared with CIN tissue from non-cancer patients 5. Choline-containing metabolites increased from pre-invasive to invasive cervical cancer | [22] |
| 2017 | Training set: 70 cervical cancer, 80 normal control; testing set: 66 cervical cancer, 69 normal control | Plasma | LC–MS | 1. 55 metabolites were down-regulated in cervical cancer patients while 7 metabolites were up-regulated 2. Bilirubin, LysoPC(17:0), n-oleoyl threonine, 12-hydroxydodecanoic acid and tetracosahexaenoic acid can be biomarkers for cervical cancer diagnosis | [23] |
| 2018 | 40 normal cervix, 40 HSIL | Cervical cytologic specimens | LC–MS | 2 ceramides and 1 sphingosine metabolite are unique signatures for HSIL, and occurred independently of HPV status | [24] |
| 2018 | 42 negative for intraepithelial lesion or malignancy (NILM), 34 SIL | Plasma | Electrospray ionization coupled to Q Exactive Orbitrap MS (lipidomics) | Prostaglandins, phospholipids, sphingolipids, Tetranor-PGFM and hydroperoxide lipid are distinct lipids to identify NILM and SIL | [25] |
| 2019 | 69 normal, 55 CIN1, 42 CIN2/3, 60 cervical cancer | Plasma | LC–MS | 1. AMP, aspartate, glutamate, hypoxanthine, lactate, proline, and pyroglutamate were discriminated between CINs and cervical cancer versus normal 2. The seven metabolites combined with positive HPV status were correlated with substantial risk of cancer progression | [26] |
| 2019 | 18 healthy HPV−, 11 healthy HPV+, 12 LSIL, 27 HSIL, 10 cervical cancer | Cervicovaginal lavages and vaginal swabs | LC–MS | 1. Three-hydroxybutyrate, eicosenoate, and oleate/vaccenate discriminated between cancer patients versus healthy 2. ICC group had an enrichment of amino acid metabolites in comparison to other groups that were HPV positive (healthy HPV+, LSIL, and HSIL) 3. Lipid, xenobiotics, and carbohydrate super-pathways metabolites enriched in the ICC group compared to other groups | [27] |
| 2019 | 13 HPV-negative, 26 HPV-positive (including 14 HR-HPV) | Self-collected mid-vaginal swabs | LC–MS | HPV+ women had higher biogenic amine and phospholipid concentrations compared with HPV– women after adjustment for vaginal microbiota Community State Type and cigarette smoking | [28] |
| 2021 | 66 healthy controls, 55 CIN1, 44 CIN 2/3, 60 cervical cancer | Plasma | Ultraperformance liquid chromatography/quadrupole time-of-flight MS (UPLC-QTOF-MS, lipidomics) | The levels of most diglyceride and FFA species were higher, while the levels of most phosphatidylcholine and phosphatidylethanolamine species were lower in the patients with CIN 2/3 and cervical cancer than in the healthy controls and the patients with CIN1 | [31] |
Summary of the design and findings of studies that applied metabolomics to investigate metabolic features in cervical diseases (HPV infection, cervical lesions and cervical cancer). The studies are listed in chronological order
The specific metabolites included in Major findings are shown in bold texts
Similar to other types of studies on cancer, many metabolomics studies focus on differences between cancer and normal tissues. Yang et al. tested plasma samples from cervical cancer patients and normal controls with LC–MS-based untargeted metabolomics. In cervical cancer patients, Yang and colleagues reported that 55 metabolites were downregulated and that 7 metabolites were upregulated, and they suggested that the combination of bilirubin, lysophosphatidylcholine (17:0) (lysoPC(17:0)), n-oleoyl threonine, 12-hydroxydodecanoic acid and tetracosahexaenoic acid are satisfactory candidate biomarkers for cervical cancer diagnosis [26]. Ilhan and colleagues collected cervicovaginal lavages from HPV-negative controls, HPV-positive controls and women with cervical dysplasia or cancer, and they reported that cervical cancer exhibits an abundance of metabolites in lipid, xenobiotic and carbohydrate pathways in comparison to other groups. Ilhan et al. indicated that oleate/vaccenate, eicosenoate and 3-hydroxybutyrate are good indicators to discriminate cervical cancer patients from healthy controls [27].
The total course from HPV infection to invasive cervical cancer can take up to 20 years. Early diagnosis and clinical intervention of HSILs is of great importance because HSILs are identified as precancerous lesions. Using LC–MS analysis of cervical cytologic specimens, Porcari and colleagues identified 3 unique metabolites classifying HSIL and normal cervix independent of HPV status, including a sphingosine metabolite and two ceramides [28].
Because cervical cancer is often a virus-related disease, metabolic alterations might be attributed to both HPV infection and cancer progression. The HPV infection impact has also been studied using metabolomics. Analysis of samples from self-collected mid-vaginal swabs has indicated that HPV+ women have higher biogenic amine and phospholipid concentrations than HPV− women [29].
Using lipidomics, a subfield of metabolomics, Neves et al. demonstrated that 5 types of lipids, including prostaglandins, phospholipids, sphingolipids, tetranor-prostaglandin F and its metabolite (dihydroketoprostaglandin; tetranor-PGFM), as well as hydroperoxide contribute to the distinction of blood plasma samples from individuals who have no intraepithelial lesions or malignancies from those who have squamous intraepithelial lesions. The diversity of plasma lipids in healthy individuals and cervical dysplasia indicates metabolic modulation in cervical malignancy progression [30]. In a lipidomics study profiling the global lipids of plasma, Nam et al. showed that phosphatidylcholine, phosphatidylethanolamine, diglyceride and free FAs are major lipid classes with significant differences in patients with CIN2/3 and cervical cancer compared to healthy controls and patients with CIN1 [31]. However, these studies did not determine the same specific metabolites to identify cervical lesion progression. Although the findings of metabolomics are comparable to wet-lab studies, it is difficult to target a specific metabolite of cervical cancer through the articles we summarized in this research. However, discrepancies in these studies might be due to diversities in instruments, algorithms, classifications of metabolites and grouping methods of patients.
The design of a metabolomics study is based on the purpose of research. Using high-resolution magic angle spinning magnetic resonance spectroscopy (HR-MAS MRS), Silva et al. showed increased choline and phosphocholine in cervical cancer tissue compared to high-grade CIN tissue, and they reported that the evels of alanine and creatine are lower in normal tissue from cancer patients than in normal tissue from healthy individuals [32]. Because this study used in situ tissue and covered the entire process from a normal state to dysplasia and to cancer, it helped to investigate the transition from preinvasive to invasive disease. However, Khan and colleagues used LC–MS to study plasma samples from CIN patients, cervical cancer patients and normal controls, and they reported that the top 7 metabolites differing among the normal, CIN and cancer groups are adenosine monophosphate (AMP), aspartate, glutamine, hypoxanthine, lactate, proline and pyroglutamate. These combined 7 metabolites reveal satisfactory diagnostic value with an area under the curve (AUC) of 0.83 between the normal and cervical cancer groups, indicating that high levels of targeted metabolites with positive HPV status show a significant risk for the development of CIN2/3 and cervical cancer [33]. Due to the thorough AUC analysis and combination with HPV status, the study by Khan and colleagues is valuable for identifying biomarkers of cervical cancer.
Current metabolomics studies in cervical diseases are restricted to descriptive research of clinical samples, and few experiments are performed in these studies to confirm the transformation of metabolites and enzymes. Nevertheless, high-throughput technology would be beneficial to identify nonmainstream, alternative metabolic features in cervical diseases and inspire in-depth molecular mechanism research.
HPV plays a role in metabolic regulation: how viruses contribute to carcinogenesis
HPV is a double-stranded DNA virus, and the genome of HPV is divided into 8 open reading frames (ORFs), coding viral early genes E1, E2, E4, E5, E6 and E7 as well as late genes L1 and L2 [34, 35].
Viruses depend on the availability of host metabolic constituents to replicate and accomplish their life cycles. Therefore, viruses evolve to manipulate metabolism in infected host cells for better adaptation [36]. Evidence from high-throughput technologies supports that HPV infection is implicated in cell metabolism modulation. Zheng and colleagues investigated the global circRNA expression profiles in E7-transfected Ca Ski cells using bioinformatics analysis; GO enrichment analysis showed that the upregulated circRNAs are enriched in “oxidative phosphorylation” but that the downregulated circRNAs are enriched in “polyamine metabolic process”, “regulation of protein catabolic process” and “neutral amino acid transport”; while Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis indicated that the upregulated circRNAs are enriched in “FA metabolism” but that the downregulated circRNAs are enriched in “arginine and proline metabolism”, “glutathione metabolism” and “central carbon metabolism in cancer” [37]. In 3-dimensional organotypic raft cultures of cervical tissues, Kang and colleagues performed a GO enrichment analysis, revealing that early HPV16 infection-induced downregulated genes are enriched in “sphingolipid biosynthetic process” and “unsaturated FA metabolic process” [38]. In this section, we will introduce verified and speculated mechanisms of how HPV promotes metabolic reprogramming in cervical epithelial cells (Table 2).
Table 2.
Association between HPV and metabolic alterations
| HPV viral protein | Direct target | Secondary target | Enzyme | Metabolic process |
|---|---|---|---|---|
| E6 | c-MYC | HK2 | Glycolysis | |
| miR-143-3p | HK2 | Glycolysis | ||
| p53 | miR-34a | LDHA | Lactate | |
| Glycolysis | ||||
| SREBP1C | Lipogenic | |||
| Lpin1, MCD, CPT1 | FAO | |||
| miRNA-107, PANK1 | FASN, SCD1, CPT1α | Lipid metabolism | ||
| SLC7A3 | Arginine uptake | |||
| GLS2 | Glutamine metabolism | |||
| E7 | miR-143-3p | HK2 | Glycolysis | |
| Rb1 | GLUT1, HK2, PKM2 | Glycolysis | ||
| E2F1 | GLUT2, GCK, PDK4, FBP, PKLR | Glycolysis | ||
| ACACA FASN, CHREBP, SREBP1C, CKB, | Lipogenic | |||
| PI3K/Akt/mTOR | PFK1, GLUT | Glycolysis |
Summary of the mechanisms by which HPV regulates metabolism. The responsible HPV viral proteins, their targets, the modified enzymes and corresponding metabolic processes are listed
HPV remodels glucose metabolism
Glycolytic flux is the best-described metabolic alteration induced by HPV infection. HPV E6 O-GlcNAcylates and stabilizes c-MYC [39], which enhances the transcription of hexokinase 2 (HK2), the rate-limiting enzyme responsible for the first step in glycolysis [39, 40]. Furthermore, E6/E7 induces downregulation of the HK2-inhibitory microRNA, miR-143-3p, thereby promoting glycolysis [41]. E6 inactivates p53, which directly suppresses miR-34a expression. Reduction of miR-34a promotes the Warburg effect and elevates the level of lactate dehydrogenase A (LDHA), which is responsible for the processing of pyruvate to lactate [42, 43]. Thus, lactate production is increased in both the intracellular and conditioned media of HPV-positive cells [44]. In addition, amplification of the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) signaling cascade is frequent in HPV-induced cancers [45]. Akt-dependent changes are closely associated with aerobic glycolysis. Hyperactivation of Akt upregulates the expression and membrane translocation of glucose transporters, reverses forkhead box O (FoxO)-induced glycolytic gene suppression and activates key glycolytic enzymes, such as phosphofructokinase 1 (PFK1) [46].
The E6 and E7 viral proteins potentially impact host cell metabolism
The E6 and E7 oncogenes in HR-HPV types are closely related to malignant transformation of host cells. E6 and E7 interact with the p53 and pRb tumor suppressors, respectively. As a result, p53 is degraded, thus blocking its proapoptotic effect. pRb disassociates from and consequently activates the E2 factor (E2F) transcription factor, which upregulates cell cycle-related genes. Thus, hyperactivated E6 and E7 drive infected cervical cells into S phase, leading to uncontrolled cell proliferation [47, 48]. Consistent expression of E6 and E7 is required for cervical cancer cell malignant phenotype maintenance.
The metabolic modulations by HPV infection may also be driven by E6- and E7-induced inhibition of p53 and Rb activity. p53 is a well-established tumor suppressor and lipogenic inhibitor that inhibits sterol-regulatory element binding protein 1c (SREBP1C) [49]. Activated p53 directly induces transcription of FA metabolism regulator lipid phosphate phosphohydrolase 1 (Lpin1) and malonyl-CoA decarboxylase (MCD), which catalyzes the degradation of malonyl-CoA to acetyl-CoA and enhances carnitine palmitoyltransferase 1 (CPT1). As a result, p53 increases long-chain FA uptake by the mitochondria, thereby promoting FAO [50, 51]. p53 also binds to the promoter of pantothenate kinase 1 (PANK1) to increase the expression of PANK1 and its intronic miRNA-107. PANK1 and miRNA-107 enhance lipid metabolism by upregulating key enzymes involved in lipid metabolism, including fatty acid synthase (FASN), stearoyl-CoA desaturase 1 (SCD1) and CPT1α [52]. In contrast, p53 deficiency facilitates lipid accumulation [53]. Therefore, perturbation of p53 might rebuild lipid homeostasis in HPV-infected cells. Moreover, p53 modulates intracellular amino acid levels. p53 activation leads to transcriptional upregulation of arginine transporter human cationic amino acid transporter 3 (SLC7A3) to promote arginine uptake [54]. Glutaminase 2 (GLS2), encoding a key enzyme in the conversion of glutamine to glutamate, is also a target gene of p53. Elevated GLS2 increases glutamate and α-ketoglutarate, which, in turn, enhances mitochondrial respiration and adenosine triphosphate (ATP) generation [55, 56].
Conroy reported that in Kras-driven lung tumors, loss of Rb1 increases the expression of the following key glycolytic enzymes: glucose transporter 1 (GLUT1), HK2 and pyruvate kinase type M2 (PKM2). The loss of Rb1 enhances glycolytic metabolism without altering mitochondrial pyruvate oxidation but has no significant effect on tricarboxylic acid (TCA) anaplerosis or utilization of alternative nutrient sources, including lactate and glutamine [57]. However, whether the pRb/E2F1 axis participates in this process is unclear. E2F1 acts as a transcription factor and associates with promoters of several lipogenic or glycolytic genes, such as FASN, carbohydrate response element binding protein (CHREBP), SREBF1C, creatine kinase B (CKB), PDK4 and fructose-2,6-bisphosphatase (FBP). E2F1 also indirectly regulates other metabolism-related genes, such as GLUT2, glucokinase (GCK), pyruvate kinase L/R (PKLR) and acetyl-CoA carboxylase (ACC1). Therefore, in terms of lipid metabolism, Rb inactivation and successful E2F1 induction prompt de novo lipid synthesis and facilitate lipid accumulation. In contrast, E2F1 promotes glycolytic metabolism, representing a metabolic switch from oxidative to glycolytic metabolism that responds to stressful conditions [58–62]. However, the mechanism by which HPV regulates glucose, glutamine and lipid metabolism via p53 and E2F1 should be confirmed in cervical epithelial cells and cervical tissue specimens.
The metabolic changes induced by HPV, including activated glycolysis, elevated amino acid uptake and de novo lipid synthesis, are consistent with the findings in various cancers. These similarities highlight the solid connection between HPV and malignant transformation of cervical cancer.
Metabolic features in cervical cancer and carcinogenesis effects: highly associated with malignant phenotypes
Glycolysis
In a previous investigation involving 134 nondiabetic patients with cervical cancer (IIB–IVA), measurement of nonfasting plasma glucose levels before starting chemotherapy or radiation indicated that patients with higher glucose levels over 102 mg/dL have a shorter overall survival and progression-free interval compared to their counterparts. This study indicated that glucose level is associated with poor prognosis of cervical cancer, implying a potential interrelationship between cervical cancer and glucose metabolism [63].
As glucose cannot spread freely through the lipid bilayer cell membrane, GLUTs mediate the intake of glucose, and GLUT1 is a leading carrier for glucose in many cancers [64]. The intensity of GLUT1 in low-grade cervical dysplasia is similar to that in normal tissues but is significantly greater in invasive cancer and increases with cancer progression. The overexpression of GLUT1 may be a late phenomenon in cellular transformation [65, 66]. Regarding cervical cancer, higher GLUT1 expression is positively related to higher tumor stage and pelvic lymph node metastasis. Higher expression of GLUT1 is an independent prognostic factor for the overall survival of HPV16-positive patients, and HPV16-positive patients overexpressing GLUT1 have lower immune cell scores of CD8+ T cells, B cells and Th1 cells [67]. GLUT1 expression correlates with HPV infection [68]. Several pathways may contribute to the regulation of GLUT1 in cervical cancer. PKM2, which converts phosphoenolpyruvate (PEP) and adenosine diphosphate (ADP) to pyruvate to produce ATP, is a rate-limiting enzyme of glycolysis. PKM2 is abundant in radioresistant patients and is increased after radiotherapy [69]. PKM2 enhances glycolysis and upregulates the expression of GLUT1 [70]. Another mechanism is that programmed cell death ligand 1 (PD-L1) directly binds to integrin β4 (ITGB4), activates the AKT/GSK3β signaling pathway and consequently promotes snail homolog 1 (SNAI1) expression. SNAI1, which is a transcription factor, negatively regulates sirtuin 3 (SIRT3) by inhibiting its promoter activity. SIRT3 plays an important role in the regulation of glucose metabolism by upregulating GLUT1 and GLUT4 as well as the glycolytic enzymes, HK2 and LDHA, ultimately promoting glucose uptake and glycolysis [71].
6-Phosphofructo-2-kinase/fructose-2,6-biphosphatase 3 enzyme (PFKFB3) and FBP are two glycolysis regulators upregulated in chemoresistant cervical cancer cells, and they increase glycolytic levels (exhibiting high glucose uptake, high ATP levels and low oxygen consumption rates) in cervical cancer cells [72]. Phosphatidylinositol 3-kinase p110 a (PIK3CA) E542K and E545K mutants are common in cervical cancer. Mutants also activate the AKT/GSK3β signaling pathway to promote the expression and nuclear accumulation of β-catenin, subsequently suppressing SIRT3 to stimulate glycolysis [73].
Inhibition of glycolysis impairs cervical cancer cell proliferation, indicating the vital role of glycolysis in cervical cancer development [39]. Abnormal glucose metabolism also contributes to chemoresistance. Active glycolysis activates hypoxia inducible factor-1α (HIF-1α), mediates autophagy and reduces chemosensitivity [74].
Lactate
The miR-34a/LDHA axis facilitates cervical cancer cell proliferation and invasion [43]. The plasma lactate concentration is lowest in individuals without cervical lesions and increases according to cervical lesion grades, reaching a maximum in cervical cancer. Lactate produced by cervical cancer cells stimulates the secretion of interleukin-6 (IL-6) and IL-10 as well as upregulates HIF-1α expression and decreases p65 NF-κB activity in tumor-associated macrophages, contributing to a procancerous M2 macrophage phenotype. Modulated macrophages are less potent in T cell activation, promoting a protumoral microenvironment [75]. Lactate inhibits histone deacetylases (HDACs) and induces histone H3 and H4 hyperacetylation as well as decreases chromatin compactness to create a DNA repair-proficient environment. Furthermore, lactate induces the expression of genes involved in DNA repair, such as the homologous recombination-related gene, Nijmengen breakage syndrome 1 (NBS1), and the nonhomologous end joining (NHEJ) genes, DNA ligase 4 (LIG4) and aprataxin (APTX), while enhancing the activation and nuclear accumulation of DNA-dependent protein kinase (DNA-PKcs), a key enzyme involved in NHEJ. Multiple mechanisms cooperate in DNA repair and improve cell viability after chemotherapy [76].
Lipids
Lipid metabolism is altered in cervical cancer. Cumulative evidence indicates that lipid droplets gradually increase in noncancerous cervical tissue, preinvasive dysplastic cervical epithelium and invasive cervical cancer [77, 78]. Moreover, chemoresistant cervical cancer cells contain more lipid droplets than chemosensitive cells [72]. Regulation of lipid enzymes is involved in this process. Long noncoding RNA LNMICC is increased in cervical cancer with lymph metastasis and poor prognosis. LNMICC activates FA metabolism by upregulating several key FA metabolic enzymes, including FASN, ACC1, ACOX1, CPT1α and FABP5, which consequently upregulates intracellular triglycerides and phospholipids [71].
Lipids comprise nearly 50% of the cell membrane. Distinct membrane lipid composition in cervical cancer cells may be an indication of altered lipid metabolism. Compared to their nonmalignant counterparts, cervical cancer cells undergo a loss of cell membrane rigidity due to the following changes: the level of sphingomyelin 16:0 decreases; the proportion of phospholipids with shorter fatty acyl chain lengths increases; and FAs are more desaturated [79]. The changes in lipid compositions facilitate cell signaling, and a less rigid membrane may help cancer cells move the vascular wall forward to promote migration [80, 81]. The adjustment in membrane lipids may be attributed to HPV because HPV 16 E5 increases the synthesis rate of phosphatidylcholine and phosphatidylserine but diminishes the synthesis rate of phosphatidylglycerol in keratinocytes [82]. Some lipids regulate the cell membrane to facilitate their own uptake, which indirectly promotes cancer malignancy. Oleic acid elevates the membrane expression of CD36, a FA transporter, and induces Srs kinase, activating the downstream ERK1/2 pathway to promote cervical cancer cell proliferation and invasion in a CD36-dependent manner [62].
Amino acids
GLS, which catalyzes the conversion of glutamine to glutamate, is positively related to glutamine metabolism. GLS2 is enhanced in radioresistant cervical cancer and produces antioxidants, including glutathione (GSH), NADH and NADPH, to suppress reactive oxygen species (ROS) levels in response to radiation [83]. Similarly, in chemoresistant cervical cancer, loss of miR-497 leads to upregulation of transketolase, resulting in increased glucose uptake and GSH generation, which reduces ROS and chemosensitivity [84].
In mammals, tryptophan is used for protein and indole synthesis. Indoleamine 2,3-dioxygenase (IDO) is the rate-limiting enzyme that catalyzes tryptophan degradation in the kynurenine pathway and acts as an immune checkpoint. In the tumor microenvironment, IDO exhausts tryptophan to produce kynurenine and its derivatives, which are toxic to T cells. As a result, the T cell immune response is suppressed, leading to tumor microenvironment immunologic tolerance [85, 86]. Regardless of HPV infection status, normal cervical squamous epithelial cells have low IDO expression, but in women with SIL or cervical cancer, the percentage of IDO-positive cervical epithelial cells or leukocytes in their cervical tissue increases [87]. Ferns and colleagues demonstrated that cervical cancer patients with tumor bulks greater than 4 cm or lymph node metastatic spread have lower plasma tryptophan levels; these researchers reported that higher kynurenine and 3-hydroxykynurenine concentrations are positively correlated with advanced FIGO stage and lymph node metastases, and they suggested that a high kynurenine/tryptophan ratio is related to poor disease-specific survival [88]. However, cervical tissue samples from the same cohort revealed no difference in survival outcome between IDO-positive and IDO-negative patients. Compared to patients with patchy IDO expression, patients with marginal tumor IDO expression at the interface with the stroma have improved disease-free survival and disease-specific survival [89]. In addition, IDO-positive tumor-infiltrating immune cells are related to fewer lymph node metastases. Different sampling tissues (plasma and cervical tissue) may account for the divergence between these two studies. Hence, tryptophan metabolic traits may differ between blood and tumors (Fig. 1, Table 3).
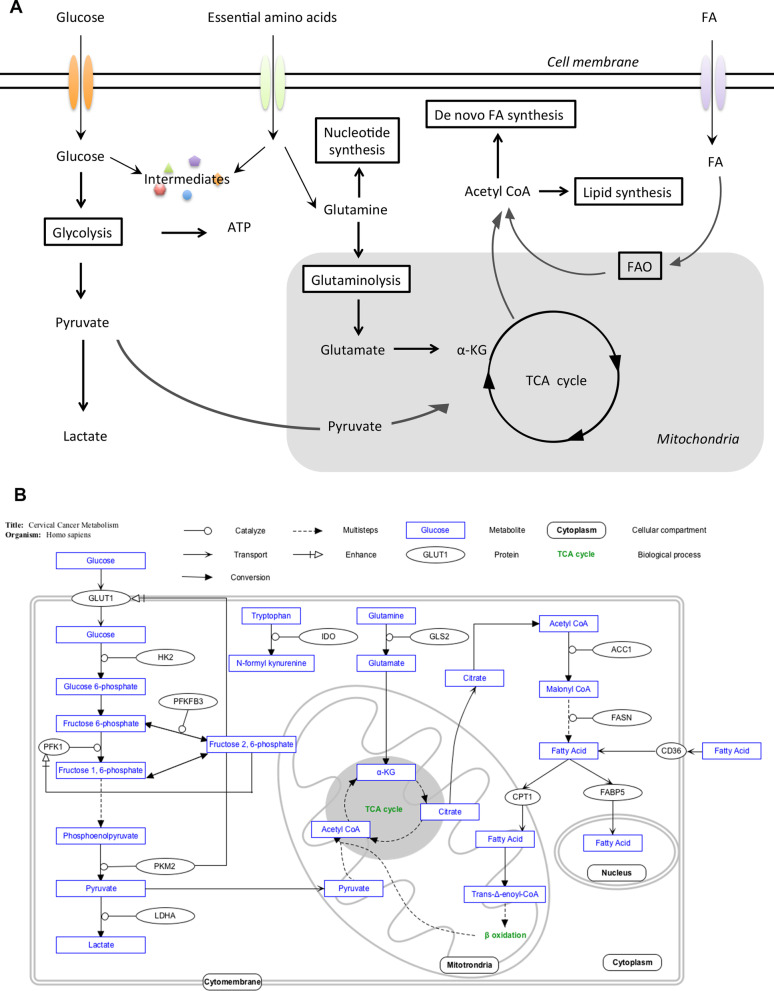
Fig. 1.
Metabolic regulation in cancer and cervical cancer. A Various cancers share several metabolic features in common. Here, we briefly illustrate typical characteristics of cancer metabolism. Generally, the uptake of glucose, amino acids and FAs is increased. Glycolysis is the leading energy source and consequently increases lactate production. Intermediates of glycolysis and glutamine metabolism are used for various biosynthesis pathways. De novo synthesis of FA is increased, and the generated FAs are further utilized in signal transduction, cellular component constitution and FAO. B Glycolysis, FA metabolism and amino acid metabolism are the most affected pathways in cervical cancer. The enzymes and transporters in the figure are all enhanced in cervical cancer or positively related to tumor aggressiveness. The figure was generated using PathVisio 3.0.0+ [102]
Table 3.
Metabolites, enzymes and transporters involved in cervical cancer and their related phenotypes
| Metabolic pathway | Specific factors involved | Related phenotypes | |
|---|---|---|---|
| Glycometabolism | Metabolites | Lactate | Pro-cancerous M2 macrophage, DNA repair after chemotherapy |
| Enzymes | LDHA | Proliferation, invasion | |
| PKM2 | Radioresistant | ||
| Lipid metabolism | Metabolites | Membrane compositions | Migration |
| Oleic acid | Proliferation, invasion | ||
| Transporters | CD36 | ||
| Amino acid metabolism | Metabolites | Kynurenine | Immunologic tolerance, metastasis |
Several specific metabolites, enzymes and transporters have been confirmed in experimental studies to be related to cancerous phenotypes in cervical cancer. Metabolic alterations are relevant to various malignant biological properties of cancer, including increased proliferation, distant metastasis and immune escape
Targeting metabolism in cervical cancer therapy: theoretically possible but requires clinical verification
Because metabolic reprogramming is crucial for cancer malignancy, targeting cancer metabolism might be a competent strategy to support conventional cancer therapy. Glucose metabolism modulators are the most widely studied, and related drug discovery has made significant progress. Several TCA regulators have been applied to clinical practice. Enasidenib (IDHIFA; AG-221), an IDH2 inhibitor, was approved by the US Food and Drug Administration (FDA) in 2017 for the treatment of adult patients with mutant IDH2 relapsed or refractory acute myeloid leukemia (R/R AML) [90]. The IDH1 inhibitor, ivosidenib (TIBSOVO, AG-120), was approved by the FDA in 2018 to treat mutant-IDH1 R/R AML. In a multicenter, randomized, double-blind, placebo-controlled, phase 3 study by ClarIDHy, ivosidenib also significantly improved the progression-free survival of advanced IDH1-mutant cholangiocarcinoma patients without severe intolerance [91]. Several drugs with other metabolic regulator capacities have been involved in clinical trials. After favorable safety results in a phase 1 study cohort, the GLS1 inhibitor, CB-839, has been combined with cabozantinib in the CANTATA study, an ongoing international, randomized, double-blind, multicenter study, to evaluate its efficacy in inhibiting metastatic renal cell carcinoma [92]. In the open-label phase 1/2 study, ECHO-202/KEYNOTE-037, epacadostat, an IDO1 selective inhibitor, and the PD-1 inhibitor, pembrolizumab, have been well tolerated and associated with promising responses in nonsmall cell lung cancer (NSCLC) and melanoma patients [93, 94]. However, a further phase 3 trial demonstrated that the combination of epacadostat and pembrolizumab is not superior to the combination of placebo and pembrolizumab in improving survival outcomes in patients with unresectable or metastatic melanoma [95]. Phase 3 clinical trials in other cancers are still ongoing [96]. The uncertainty of the results of the usefulness of metabolic regulation in cancer therapy strategies may be due to the following reasons: cultured cells have difficulty completely simulating cancer metabolism in the tumor microenvironment; there are compensation pathways for metabolic inhibition; and there is metabolic heterogeneity in cancer cells although cancer cells are metabolically distinct from adjacent normal counterparts [97, 98].
Some studies have illustrated potent metabolic targets for cervical cancer treatment. Caffeic acid downregulates GLS and malic enzyme 1 (ME1), which suppresses pyruvate dehydrogenase kinase (PDK) activity, thereby disturbing the TCA cycle. Caffeic acid also impairs de novo synthesis of unsaturated FA. Metformin inhibits glycolytic enzymes, including GLUT1, GLUT3, HK2, PFKFB4, PKM and LDH. The combined application of caffeic acid and metformin disrupts energetic homeostasis, restrains proliferation and promotes apoptosis in cervical cancer cells. Moreover, caffeic acid and metformin increases the sensitivity to cisplatin chemotherapy [99, 100]. Inhibition of glycolysis, glutathione metabolism or thioredoxin metabolism radiosensitizes cervical cancer cell lines and xenografts [101]. These results indicate that metabolic intervention may be a prospective adjuvant treatment to support anti-cervical cancer therapy. Because the related studies are mainly confined to in vitro and animal experiments, further investigation should be performed to determine whether metabolic adjuvants have potential in clinical application.
Conclusions
Metabolic adaption is a recognized feature of cancer. Many cancer types share the following similar metabolic traits: glycolysis is active even in oxygen-rich environments; de novo FA synthesis and FAO are increased; and glutamine consumption greatly increases. However, metabolic heterogeneity occurs in different cancer types. Cervical cancer remains a major threat to women’s health. High-throughput omics technology has been applied to analyze biopsy tissue, cytological specimens or vaginal lavage fluid, revealing metabolic divergence between normal cervical tissues and lesions, between uninfected and HPV-infected cells or between benign tissues and tumors. Metabolomics may contribute to further mechanistic investigation and precise cervical cancer diagnosis. In addition to metabolic phenotypes, the initiation of cervical cancer metabolic alterations has been investigated in a number of studies. Because persistent HR-HPV infection is the key to cervical epithelial cell transformation, the role of HPV viral proteins in metabolic modulation has been investigated. Many studies have demonstrated that HPV is related to remodeling of glucose metabolism and that it may also participate in lipid and glutamine regulation. Metabolic alterations benefit cervical cancer growth and several processes, including chemoresistance, radioresistance, invasion and immune escape.
Nevertheless, unresolved questions remain in this field. The utility of metabolomics opens a new field to discover potential biomarkers for cervical cancer and cervical lesion diagnosis. However, some changes revealed by metabolomics are not yet well understood. It may be worthwhile to explore why these alterations occur and how the altered metabolites affect cervical cancer progression. Previous studies on cervical cancer metabolism have suggested that metabolism may be a target for cervical cancer therapy. Although progress has been achieved using in vitro and animal experiments, evidence from clinical studies is still lacking. Future mechanistic studies and rigorously designed clinical studies will move the field forward.
Acknowledgements
Not applicable.
Abbreviations
- HPV
Human papillomavirus
- HR-HPV
High-risk HPV
- CIN
Cervical intraepithelial neoplasia
- LSIL
Low-grade squamous intraepithelial lesion
- HSIL
High-grade squamous intraepithelial lesion
- NK
Natural killer
- FA
Fatty acid
- FAO
Fatty acid oxidation
- PKCζ
Protein kinase Cζ
- NMR
Nuclear magnetic resonance
- GC–MS
Gas chromatography mass spectrometry
- LC–MS
Liquid chromatography mass spectrometry
- lysoPC
Lysophosphatidylcholine
- PGFM
Prostaglandin F and its metabolite
- HR-MAS MRS
High-resolution magic angle spinning magnetic resonance spectroscopy
- AMP
Adenosine monophosphate
- AUC
Area under curve
- ORF
Open reading frame
- KEGG
Kyoto Encyclopedia of Genes and Genomes
- HK2
Hexokinase 2
- LDHA
Lactate dehydrogenase A
- PI3K
Phosphatidylinositol 3-kinase
- mTOR
Mammalian target of rapamycin
- FoxO
Orkhead box O
- PFK1
Phosphofructokinase 1
- SREBP1C
Sterol-regulatory element binding protein 1c
- Lpin1
Lipid phosphate phosphohydrolase 1
- MCD
Malonyl-CoA decarboxylase
- CPT1
Carnitine palmitoyltransferase 1
- PANK1
Pantothenate kinase 1
- FASN
Fatty acid synthase
- SCD1
Stearoyl-CoA desaturase 1
- SLC7A3
Arginine transporter human cationic amino acid transporter 3
- GLS2
Glutaminase 2
- GLUT1
Glucose transporters 1
- PKM2
Pyruvate kinase type M2
- TCA
Tricarboxylic acid
- E2F
E2 factor
- CHREBP
Carbohydrate response element binding protein
- CKB
Creatine kinase B
- FBP
Fructose-2, 6-bisphosphatase
- GCK
Glucokinase
- PKLR
Pyruvate kinase L/R
- ACC1
Acetyl-CoA carboxylase
- ATP
Adenosine triphosphate
- PEP
Phosphoenolpyruvate
- PD-L1
Programmed cell death ligand 1
- ITGB4
Integrin β4
- SNAI1
Snail homolog 1
- SIRT3
Sirtuin 3
- PFKFB3
6-Phosphofructo-2-kinase/fructose-2, 6-biphosphatase 3 enzyme
- PIK3CA
Phosphatidylinositol 3-kinase p110 a
- HIF-1α
Hypoxia inducible factor-1 α
- IL-6
Interleukin-6
- HDAC
Histone deacetylase
- NBS1
Nijmengen breakage syndrome 1
- NHEJ
Non-homologous end joining
- LIG4
DNA ligase 4
- APTX
Aprataxin
- DNA-PKcs
DNA-dependent protein kinase
- ROS
Reactive oxygen species
- IDO
Indoleamine 2,3-dioxygenase
- NSCLC
Non-small cell lung cancer
- ME1
Malic enzyme 1
- PDK
Pyruvate dehydrogenase kinase
Authors' contributions
Li and Sui designed the research; Li conducted the library search and wrote the manuscript; Sui participated in editing of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by Shanghai Science & Technology committee research project (Project No. 18411963600).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have declared that no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cohen PA, Jhingran A, Oaknin A, et al. Cervical cancer. Lancet. 2019;393(10167):169–182. doi: 10.1016/S0140-6736(18)32470-X. [DOI] [PubMed] [Google Scholar]
- 2.Steenbergen RD, Snijders PJ, Heideman DA, et al. Clinical implications of (epi)genetic changes in HPV-induced cervical precancerous lesions. Nat Rev Cancer. 2014;14(6):395–405. doi: 10.1038/nrc3728. [DOI] [PubMed] [Google Scholar]
- 3.Darragh TM, Colgan TJ, Thomas Cox J, et al. The Lower Anogenital Squamous Terminology Standardization project for HPV-associated lesions: background and consensus recommendations from the College of American Pathologists and the American Society for Colposcopy and Cervical Pathology. Int J Gynecol Pathol. 2013;32(1):76–115. doi: 10.1097/PGP.0b013e31826916c7. [DOI] [PubMed] [Google Scholar]
- 4.Schiffman M, Doorbar J, Wentzensen N, et al. Carcinogenic human papillomavirus infection. Nat Rev Dis Primers. 2016;2:16086. doi: 10.1038/nrdp.2016.86. [DOI] [PubMed] [Google Scholar]
- 5.Federico C, Sun J, Muz B, et al. Localized delivery of cisplatin to cervical cancer improves its therapeutic efficacy and minimizes its side-effect profile. Int J Radiat Oncol Biol Phys. 2021;109(5):1483–1494. doi: 10.1016/j.ijrobp.2020.11.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez PT, Frumovitz M, Pareja R, et al. Minimally invasive versus abdominal radical hysterectomy for cervical cancer. N Engl J Med. 2018;379(20):1895–1904. doi: 10.1056/NEJMoa1806395. [DOI] [PubMed] [Google Scholar]
- 7.Mabuchi S, Matsumoto Y, Kawano M, et al. Uterine cervical cancer displaying tumor-related leukocytosis: a distinct clinical entity with radioresistant feature. J Natl Cancer Inst. 2014;106(7):dju147. doi: 10.1093/jnci/dju147. [DOI] [PubMed] [Google Scholar]
- 8.Singh SV, Ajay AK, Mohammad N, et al. Proteasomal inhibition sensitizes cervical cancer cells to mitomycin C-induced bystander effect: the role of tumor microenvironment. Cell Death Dis. 2015;6(10):e1934. doi: 10.1038/cddis.2015.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Floberg JM, Zhang J, Muhammad N, et al. Standardized uptake value for 18F-Fluorodeoxyglucose is a marker of inflammatory state and immune infiltrate in cervical cancer. Clin Cancer Res. 2021;27:4245–4255. doi: 10.1158/1078-0432.CCR-20-4450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rashmi R, Jayachandran K, Zhang J, et al. Glutaminase inhibitors induce thiol-mediated oxidative stress and radiosensitization in treatment-resistant cervical cancers. Mol Cancer Ther. 2020;19(12):2465–2475. doi: 10.1158/1535-7163.MCT-20-0271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pavlova NN, Thompson CB. The emerging hallmarks of cancer metabolism. Cell Metab. 2016;23(1):27–47. doi: 10.1016/j.cmet.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martinez-Outschoorn UE, Peiris-Pages M, Pestell RG, et al. Cancer metabolism: a therapeutic perspective. Nat Rev Clin Oncol. 2017;14(2):113. doi: 10.1038/nrclinonc.2017.1. [DOI] [PubMed] [Google Scholar]
- 13.Liberti MV, Locasale JW. The Warburg effect: how does it benefit cancer cells? Trends Biochem Sci. 2016;41(3):211–218. doi: 10.1016/j.tibs.2015.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Colegio OR, Chu NQ, Szabo AL, et al. Functional polarization of tumour-associated macrophages by tumour-derived lactic acid. Nature. 2014;513(7519):559–563. doi: 10.1038/nature13490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brand A, Singer K, Koehl GE, et al. LDHA-associated lactic acid production blunts tumor immunosurveillance by T and NK cells. Cell Metab. 2016;24(5):657–671. doi: 10.1016/j.cmet.2016.08.011. [DOI] [PubMed] [Google Scholar]
- 16.Currie E, Schulze A, Zechner R, et al. Cellular fatty acid metabolism and cancer. Cell Metab. 2013;18(2):153–161. doi: 10.1016/j.cmet.2013.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guri Y, Colombi M, Dazert E, et al. mTORC2 promotes tumorigenesis via lipid synthesis. Cancer Cell. 2017;32(6):807–823.e12. doi: 10.1016/j.ccell.2017.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Heuer TS, Ventura R, Lai J, et al. Abstract 4743: Preclinical studies characterize tumor type sensitivity to FASN inhibition and the mechanism and efficacy of novel drug combinations with TVB-2640. Cancer Res. 2016;76(14 Supplement):4743. [Google Scholar]
- 19.Carracedo A, Cantley LC, Pandolfi PP. Cancer metabolism: fatty acid oxidation in the limelight. Nat Rev Cancer. 2013;13(4):227–232. doi: 10.1038/nrc3483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang T, Fahrmann JF, Lee H, et al. JAK/STAT3-regulated fatty acid beta-oxidation is critical for breast cancer stem cell self-renewal and chemoresistance. Cell Metab. 2018;27(6):1357. doi: 10.1016/j.cmet.2018.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang J, Pavlova NN, Thompson CB. Cancer cell metabolism: the essential role of the nonessential amino acid, glutamine. EMBO J. 2017;36(10):1302–1315. doi: 10.15252/embj.201696151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altman BJ, Stine ZE, Dang CV. From Krebs to clinic: glutamine metabolism to cancer therapy. Nat Rev Cancer. 2016;16(11):749. doi: 10.1038/nrc.2016.114. [DOI] [PubMed] [Google Scholar]
- 23.Wishart DS. Emerging applications of metabolomics in drug discovery and precision medicine. Nat Rev Drug Discov. 2016;15(7):473–484. doi: 10.1038/nrd.2016.32. [DOI] [PubMed] [Google Scholar]
- 24.Newgard CB. Metabolomics and metabolic diseases: where do we stand? Cell Metab. 2017;25(1):43–56. doi: 10.1016/j.cmet.2016.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Theodoridis GA, Gika HG, Want EJ, et al. Liquid chromatography–mass spectrometry based global metabolite profiling: a review. Anal Chim Acta. 2012;711:7–16. doi: 10.1016/j.aca.2011.09.042. [DOI] [PubMed] [Google Scholar]
- 26.Yang K, Xia B, Wang W, et al. A comprehensive analysis of metabolomics and transcriptomics in cervical cancer. Sci Rep. 2017;7:43353. doi: 10.1038/srep43353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ilhan ZE, Laniewski P, Thomas N, et al. Deciphering the complex interplay between microbiota, HPV, inflammation and cancer through cervicovaginal metabolic profiling. EBioMedicine. 2019;44:675–690. doi: 10.1016/j.ebiom.2019.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Porcari AM, Negrao F, Tripodi GL, et al. Molecular signatures of high-grade cervical lesions. Front Oncol. 2018;8:99. doi: 10.3389/fonc.2018.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Borgogna JC, Shardell MD, Santori EK, et al. The vaginal metabolome and microbiota of cervical HPV-positive and HPV-negative women: a cross-sectional analysis. BJOG. 2020;127(2):182–192. doi: 10.1111/1471-0528.15981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Neves ACO, Morais CLM, Mendes TPP, et al. Mass spectrometry and multivariate analysis to classify cervical intraepithelial neoplasia from blood plasma: an untargeted lipidomic study. Sci Rep. 2018;8(1):3954. doi: 10.1038/s41598-018-22317-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nam M, Seo SS, Jung S, et al. Comparable plasma lipid changes in patients with high-grade cervical intraepithelial neoplasia and patients with cervical cancer. J Proteome Res. 2021;20(1):740–750. doi: 10.1021/acs.jproteome.0c00640. [DOI] [PubMed] [Google Scholar]
- 32.De Silva SS, Payne GS, Thomas V, et al. Investigation of metabolite changes in the transition from pre-invasive to invasive cervical cancer measured using (1)H and (31)P magic angle spinning MRS of intact tissue. NMR Biomed. 2009;22(2):191–198. doi: 10.1002/nbm.1302. [DOI] [PubMed] [Google Scholar]
- 33.Khan I, Nam M, Kwon M, et al. LC/MS-based polar metabolite profiling identified unique biomarker signatures for cervical cancer and cervical intraepithelial neoplasia using global and targeted metabolomics. Cancers (Basel) 2019;11(4):511. doi: 10.3390/cancers11040511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.zur Hausen H. Papillomaviruses and cancer: from basic studies to clinical application. Nat Rev Cancer. 2002;2(5):342–350. doi: 10.1038/nrc798. [DOI] [PubMed] [Google Scholar]
- 35.Doorbar J, Quint W, Banks L, et al. The biology and life-cycle of human papillomaviruses. Vaccine. 2012;30(Suppl 5):F55–70. doi: 10.1016/j.vaccine.2012.06.083. [DOI] [PubMed] [Google Scholar]
- 36.Levy P, Bartosch B. Metabolic reprogramming: a hallmark of viral oncogenesis. Oncogene. 2016;35(32):4155–4164. doi: 10.1038/onc.2015.479. [DOI] [PubMed] [Google Scholar]
- 37.Zheng SR, Zhang HR, Zhang ZF, et al. Human papillomavirus 16 E7 oncoprotein alters the expression profiles of circular RNAs in Caski cells. J Cancer. 2018;9(20):3755–3764. doi: 10.7150/jca.24253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang SD, Chatterjee S, Alam S, et al. Effect of productive human papillomavirus 16 infection on global gene expression in cervical epithelium. J Virol. 2018;92(20):e01261–e1318. doi: 10.1128/JVI.01261-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zeng Q, Zhao RX, Chen J, et al. O-linked GlcNAcylation elevated by HPV E6 mediates viral oncogenesis. Proc Natl Acad Sci U S A. 2016;113(33):9333–9338. doi: 10.1073/pnas.1606801113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zeng Q, Chen J, Li Y, et al. LKB1 inhibits HPV-associated cancer progression by targeting cellular metabolism. Oncogene. 2017;36(9):1245–1255. doi: 10.1038/onc.2016.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hoppe-Seyler K, Honegger A, Bossler F, et al. Viral E6/E7 oncogene and cellular hexokinase 2 expression in HPV-positive cancer cell lines. Oncotarget. 2017;8(63):106342–106351. doi: 10.18632/oncotarget.22463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Misso G, Di Martino MT, De Rosa G, et al. Mir-34: a new weapon against cancer? Mol Ther Nucleic Acids. 2014;3:e194. doi: 10.1038/mtna.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang R, Su J, Xue SL, et al. HPV E6/p53 mediated down-regulation of miR-34a inhibits Warburg effect through targeting LDHA in cervical cancer. Am J Cancer Res. 2016;6(2):312–320. [PMC free article] [PubMed] [Google Scholar]
- 44.Kindt N, Descamps G, Lechien JR, et al. Involvement of HPV infection in the release of macrophage migration inhibitory factor in head and neck squamous cell carcinoma. J Clin Med. 2019;8(1):75. doi: 10.3390/jcm8010075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhang L, Wu J, Ling MT, et al. The role of the PI3K/Akt/mTOR signalling pathway in human cancers induced by infection with human papillomaviruses. Mol Cancer. 2015;14:87. doi: 10.1186/s12943-015-0361-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Robey RB, Hay N. Is Akt the "Warburg kinase"?-Akt-energy metabolism interactions and oncogenesis. Semin Cancer Biol. 2009;19(1):25–31. doi: 10.1016/j.semcancer.2008.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moody CA, Laimins LA. Human papillomavirus oncoproteins: pathways to transformation. Nat Rev Cancer. 2010;10(8):550–560. doi: 10.1038/nrc2886. [DOI] [PubMed] [Google Scholar]
- 48.Martinez-Zapien D, Ruiz FX, Poirson J, et al. Structure of the E6/E6AP/p53 complex required for HPV-mediated degradation of p53. Nature. 2016;529(7587):541–545. doi: 10.1038/nature16481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wu H, Ng R, Chen X, et al. MicroRNA-21 is a potential link between non-alcoholic fatty liver disease and hepatocellular carcinoma via modulation of the HBP1-p53-Srebp1c pathway. Gut. 2016;65(11):1850–1860. doi: 10.1136/gutjnl-2014-308430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Assaily W, Rubinger DA, Wheaton K, et al. ROS-mediated p53 induction of Lpin1 regulates fatty acid oxidation in response to nutritional stress. Mol Cell. 2011;44(3):491–501. doi: 10.1016/j.molcel.2011.08.038. [DOI] [PubMed] [Google Scholar]
- 51.Liu Y, He Y, Jin A, et al. Ribosomal protein-Mdm2-p53 pathway coordinates nutrient stress with lipid metabolism by regulating MCD and promoting fatty acid oxidation. Proc Natl Acad Sci U S A. 2014;111(23):E2414–E2422. doi: 10.1073/pnas.1315605111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang L, Zhang B, Wang X, et al. P53/PANK1/miR-107 signalling pathway spans the gap between metabolic reprogramming and insulin resistance induced by high-fat diet. J Cell Mol Med. 2020;24(6):3611–3624. doi: 10.1111/jcmm.15053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Wang X, Zhao X, Gao X, et al. A new role of p53 in regulating lipid metabolism. J Mol Cell Biol. 2013;5(2):147–150. doi: 10.1093/jmcb/mjs064. [DOI] [PubMed] [Google Scholar]
- 54.Lowman XH, Hanse EA, Yang Y, et al. p53 promotes cancer cell adaptation to glutamine deprivation by upregulating Slc7a3 to increase arginine uptake. Cell Rep. 2019;26(11):3051–60.e4. doi: 10.1016/j.celrep.2019.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Suzuki S, Tanaka T, Poyurovsky MV, et al. Phosphate-activated glutaminase (GLS2), a p53-inducible regulator of glutamine metabolism and reactive oxygen species. Proc Natl Acad Sci U S A. 2010;107(16):7461–7466. doi: 10.1073/pnas.1002459107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hu W, Zhang C, Wu R, et al. Glutaminase 2, a novel p53 target gene regulating energy metabolism and antioxidant function. Proc Natl Acad Sci U S A. 2010;107(16):7455–7460. doi: 10.1073/pnas.1001006107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Conroy LR, Dougherty S, Kruer T, et al. Loss of Rb1 enhances glycolytic metabolism in Kras-driven lung tumors in vivo. Cancers (Basel). 2020;12(1):237. doi: 10.3390/cancers12010237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Denechaud PD, Lopez-Mejia IC, Giralt A, et al. E2F1 mediates sustained lipogenesis and contributes to hepatic steatosis. J Clin Investig. 2016;126(1):137–150. doi: 10.1172/JCI81542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bhatia B, Hsieh M, Kenney AM, et al. Mitogenic Sonic hedgehog signaling drives E2F1-dependent lipogenesis in progenitor cells and medulloblastoma. Oncogene. 2011;30(4):410–422. doi: 10.1038/onc.2010.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Murata K, Fang C, Terao C, et al. Hypoxia-sensitive COMMD1 integrates signaling and cellular metabolism in human macrophages and suppresses osteoclastogenesis. Immunity. 2017;47(1):66–79.e5. doi: 10.1016/j.immuni.2017.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blanchet E, Annicotte JS, Lagarrigue S, et al. E2F transcription factor-1 regulates oxidative metabolism. Nat Cell Biol. 2011;13(9):1146–1152. doi: 10.1038/ncb2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xu S, Tao J, Yang L, et al. E2F1 suppresses oxidative metabolism and endothelial differentiation of bone marrow progenitor cells. Circ Res. 2018;122(5):701–711. doi: 10.1161/CIRCRESAHA.117.311814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lee YY, Choi CH, Kim CJ, et al. Glucose as a prognostic factor in non-diabetic women with locally advanced cervical cancer (IIB-IVA) Gynecol Oncol. 2010;116(3):459–463. doi: 10.1016/j.ygyno.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 64.Barron CC, Bilan PJ, Tsakiridis T, et al. Facilitative glucose transporters: implications for cancer detection, prognosis and treatment. Metabolism. 2016;65(2):124–139. doi: 10.1016/j.metabol.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 65.Mendez LE, Manci N, Cantuaria G, et al. Expression of glucose transporter-1 in cervical cancer and its precursors. Gynecol Oncol. 2002;86(2):138–143. doi: 10.1006/gyno.2002.6745. [DOI] [PubMed] [Google Scholar]
- 66.Kim BW, Cho H, Chung JY, et al. Prognostic assessment of hypoxia and metabolic markers in cervical cancer using automated digital image analysis of immunohistochemistry. J Transl Med. 2013;11:185. doi: 10.1186/1479-5876-11-185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kim BH, Chang JH. Differential effect of GLUT1 overexpression on survival and tumor immune microenvironment of human papilloma virus type 16-positive and -negative cervical cancer. Sci Rep. 2019;9(1):13301. doi: 10.1038/s41598-019-49928-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Samama B, Benardais K, Lipsker D, et al. GLUT1 expression in human papillomavirus-positive anogenital lesions. J Eur Acad Dermatol Venereol. 2020;34(4):873–875. doi: 10.1111/jdv.16102. [DOI] [PubMed] [Google Scholar]
- 69.Lin Y, Zhai H, Ouyang Y, et al. Knockdown of PKM2 enhances radiosensitivity of cervical cancer cells. Cancer Cell Int. 2019;19:129. doi: 10.1186/s12935-019-0845-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wang CH, Shyu RY, Wu CC, et al. Tazarotene-induced Gene 1 interacts with DNAJC8 and regulates glycolysis in cervical cancer cells. Mol Cells. 2018;41(6):562–574. doi: 10.14348/molcells.2018.2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Shang C, Wang W, Liao Y, et al. LNMICC promotes nodal metastasis of cervical cancer by reprogramming fatty acid metabolism. Cancer Res. 2018;78(4):877–890. doi: 10.1158/0008-5472.CAN-17-2356. [DOI] [PubMed] [Google Scholar]
- 72.Mondal S, Roy D, Sarkar Bhattacharya S, et al. Therapeutic targeting of PFKFB3 with a novel glycolytic inhibitor PFK158 promotes lipophagy and chemosensitivity in gynecologic cancers. Int J Cancer. 2019;144(1):178–189. doi: 10.1002/ijc.31868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Jiang W, He T, Liu S, et al. The PIK3CA E542K and E545K mutations promote glycolysis and proliferation via induction of the beta-catenin/SIRT3 signaling pathway in cervical cancer. J Hematol Oncol. 2018;11(1):139. doi: 10.1186/s13045-018-0674-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Peng X, Gong F, Chen Y, et al. Autophagy promotes paclitaxel resistance of cervical cancer cells: involvement of Warburg effect activated hypoxia-induced factor 1-alpha-mediated signaling. Cell Death Dis. 2014;5:e1367. doi: 10.1038/cddis.2014.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Stone SC, Rossetti RAM, Alvarez KLF, et al. Lactate secreted by cervical cancer cells modulates macrophage phenotype. J Leukoc Biol. 2019;105(5):1041–1054. doi: 10.1002/JLB.3A0718-274RR. [DOI] [PubMed] [Google Scholar]
- 76.Wagner W, Ciszewski WM, Kania KD. l- and d-lactate enhance DNA repair and modulate the resistance of cervical carcinoma cells to anticancer drugs via histone deacetylase inhibition and hydroxycarboxylic acid receptor 1 activation. Cell Commun Signal. 2015;13:36. doi: 10.1186/s12964-015-0114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Zietkowski D, deSouza NM, Davidson RL, et al. Characterisation of mobile lipid resonances in tissue biopsies from patients with cervical cancer and correlation with cytoplasmic lipid droplets. NMR Biomed. 2013;26(9):1096–1102. doi: 10.1002/nbm.2923. [DOI] [PubMed] [Google Scholar]
- 78.Sharma A, Jha AK, Mishra S, et al. Imaging and quantitative detection of lipid droplets by yellow fluorescent probes in liver sections of plasmodium infected mice and third stage human cervical cancer tissues. Bioconjug Chem. 2018;29(11):3606–3613. doi: 10.1021/acs.bioconjchem.8b00552. [DOI] [PubMed] [Google Scholar]
- 79.Händel C, Schmidt BUS, Schiller J, et al. Cell membrane softening in human breast and cervical cancer cells. New J Phys. 2015;17:083008. [Google Scholar]
- 80.Friedl P, Alexander S. Cancer invasion and the microenvironment: plasticity and reciprocity. Cell. 2011;147(5):992–1009. doi: 10.1016/j.cell.2011.11.016. [DOI] [PubMed] [Google Scholar]
- 81.Braig S, Schmidt BUS, Stoiber K, et al. Pharmacological targeting of membrane rigidity: implications on cancer cell migration and invasion. N J Phys. 2015;17(8):083007. [Google Scholar]
- 82.Bravo IG, Crusius K, Alonso A. The E5 protein of the human papillomavirus type 16 modulates composition and dynamics of membrane lipids in keratinocytes. Arch Virol. 2005;150(2):231–246. doi: 10.1007/s00705-004-0420-x. [DOI] [PubMed] [Google Scholar]
- 83.Xiang L, Xie G, Liu C, et al. Knock-down of glutaminase 2 expression decreases glutathione, NADH, and sensitizes cervical cancer to ionizing radiation. Biochim Biophys Acta. 2013;1833(12):2996–3005. doi: 10.1016/j.bbamcr.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 84.Yang H, Wu XL, Wu KH, et al. MicroRNA-497 regulates cisplatin chemosensitivity of cervical cancer by targeting transketolase. Am J Cancer Res. 2016;6(11):2690–2699. [PMC free article] [PubMed] [Google Scholar]
- 85.Lemos H, Huang L, Prendergast GC, et al. Immune control by amino acid catabolism during tumorigenesis and therapy. Nat Rev Cancer. 2019;19(3):162–175. doi: 10.1038/s41568-019-0106-z. [DOI] [PubMed] [Google Scholar]
- 86.Munn DH, Mellor AL. IDO in the tumor microenvironment: inflammation, counter-regulation, and tolerance. Trends Immunol. 2016;37(3):193–207. doi: 10.1016/j.it.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Venancio PA, Consolaro MEL, Derchain SF, et al. Indoleamine 2,3-dioxygenase and tryptophan 2,3-dioxygenase expression in HPV infection, SILs, and cervical cancer. Cancer Cytopathol. 2019;127(9):586–597. doi: 10.1002/cncy.22172. [DOI] [PubMed] [Google Scholar]
- 88.Ferns DM, Kema IP, Buist MR, et al. Indoleamine-2,3-dioxygenase (IDO) metabolic activity is detrimental for cervical cancer patient survival. Oncoimmunology. 2015;4(2):e981457. doi: 10.4161/2162402X.2014.981457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Heeren AM, van Dijk I, Berry D, et al. Indoleamine 2,3-dioxygenase expression pattern in the tumor microenvironment predicts clinical outcome in early stage cervical cancer. Front Immunol. 2018;9:1598. doi: 10.3389/fimmu.2018.01598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Stein EM, Dinardo CD, Fathi AT, et al. Molecular remission and response patterns in patients with mutant- IDH2 acute myeloid leukemia treated with enasidenib. Blood. 2019;133(7):676–687. doi: 10.1182/blood-2018-08-869008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Abou-Alfa GK, Macarulla T, Javle MM, et al. Ivosidenib in IDH1-mutant, chemotherapy-refractory cholangiocarcinoma (ClarIDHy): a multicentre, randomised, double-blind, placebo-controlled, phase 3 study. Lancet Oncol. 2020;21(6):796–807. doi: 10.1016/S1470-2045(20)30157-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Tannir N, Agarwal N, Dawson N, et al. Abstract: CANTATA: randomized, international, double-blind study of CB-839 plus cabozantinib versus cabozantinib plus placebo in patients with metastatic renal cell carcinoma. J Clin Oncol. 2019;37(7):TPS682. [Google Scholar]
- 93.Mitchell TC, Hamid O, Smith DC, et al. Epacadostat plus pembrolizumab in patients with advanced solid tumors: phase I results from a multicenter, open-label phase I/II trial (ECHO-202/KEYNOTE-037) J Clin Oncol. 2018;36:3223–3230. doi: 10.1200/JCO.2018.78.9602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Villaruz L, Schneider B, Bauer T, et al. OA05.02 epacadostat plus pembrolizumab in patients with non-small cell lung cancer: phase 1/2 results from ECHO-202/KEYNOTE-037. J Thorac Oncol. 2018;13(10):S330. [Google Scholar]
- 95.Long GV, Dummer R, Hamid O, et al. Epacadostat plus pembrolizumab versus placebo plus pembrolizumab in patients with unresectable or metastatic melanoma (ECHO-301/KEYNOTE-252): a phase 3, randomised, double-blind study. Lancet Oncol. 2019;20(8):1083–1097. doi: 10.1016/S1470-2045(19)30274-8. [DOI] [PubMed] [Google Scholar]
- 96.Cohen E, Rischin D, Pfister D, et al. Abstract: A phase 3, randomized, open-label study of epacadostat plus pembrolizumab, pembrolizumab monotherapy, and the EXTREME regimen as first-line treatment for recurrent/metastatic head and neck squamous cell carcinoma (R/M SCCHN): ECHO-304/KEYNOTE-669. J Clin Oncol. 2018;36(15):TPS6090. [Google Scholar]
- 97.Hensley CT, Faubert B, Yuan Q, et al. Metabolic heterogeneity in human lung tumors. Cell. 2016;164(4):681–694. doi: 10.1016/j.cell.2015.12.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Davidson SM, Papagiannakopoulos T, Olenchock BA, et al. Environment impacts the metabolic dependencies of Ras-driven non-small cell lung cancer. Cell Metab. 2016;23(3):517–528. doi: 10.1016/j.cmet.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tyszka-Czochara M, Bukowska-Strakova K, Kocemba-Pilarczyk KA, et al. Caffeic acid targets AMPK signaling and regulates tricarboxylic acid cycle anaplerosis while metformin downregulates HIF-1alpha-induced glycolytic enzymes in human cervical squamous cell carcinoma lines. Nutrients. 2018;10(7):841. doi: 10.3390/nu10070841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Tyszka-Czochara M, Bukowska-Strakova K, Majka M. Metformin and caffeic acid regulate metabolic reprogramming in human cervical carcinoma SiHa/HTB-35 cells and augment anticancer activity of Cisplatin via cell cycle regulation. Food Chem Toxicol. 2017;106(Pt A):260–272. doi: 10.1016/j.fct.2017.05.065. [DOI] [PubMed] [Google Scholar]
- 101.Rashmi R, Huang X, Floberg JM, et al. Radioresistant cervical cancers are sensitive to inhibition of glycolysis and redox metabolism. Cancer Res. 2018;78(6):1392–1403. doi: 10.1158/0008-5472.CAN-17-2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Kutmon M, van Iersel MP, Bohler A, et al. PathVisio 3: an extendable pathway analysis toolbox. PLoS Comput Biol. 2015;11(2):e1004085. doi: 10.1371/journal.pcbi.1004085. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.