Abstract
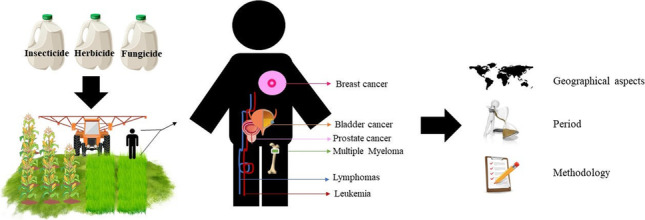
Occupational exposure to pesticides has been identified as a major trigger of the development of cancer. Pesticides can cause intoxication in the individuals who manipulate them through either inhalation, ingestion, or dermal contact. Given this, we investigated the association between the incidence of cancer and occupational exposure to pesticides through a bibliometric analysis of the studies published between 2011 and 2020, based on 62 papers selected from the Scopus database. The results indicated an exponential increase in the number of studies published over the past decade, with most of the research being conducted in the USA, France, India, and Brazil, although a further 17 nations were also involved in the research on the association between cancer and pesticides. The principal classes of pesticides investigated in relation to their role in intoxication and cancer were insecticides, herbicides, and fungicides. The types of cancer reported most frequently were multiple myeloma, bladder cancer, non-Hodgkin’s lymphoma, prostate cancer, leukemia, and breast cancer. Despite the known association between pesticides and cancer, studies are still relatively scarce in comparison with the global scale of the use of these xenobiotic substances, which is related to the increasing demand for agricultural products throughout the world.
Graphical abstract
Supplementary Information
The online version contains supplementary material available at 10.1007/s11356-021-17031-2.
Keywords: Agriculture, Cancer, DNA, Diseases, Farm workers, Health, Pesticides
Introduction
Pesticides are applied to some extent in most homes, businesses, and farms to control insects, weeds, fungi, rodents, and even microbial organisms (Langley and Mort 2012; Mostafalou and Abdollahi 2017). These products are classified according to their chemical composition and include an ample diversity of conventional pesticides, herbicides, insecticides, rodenticides, plant growth regulators, miticides, nematicides, fungicides, fumigants, and antimicrobial agents (EPA 2020). Globally, almost 3 billion tons of pesticides are deployed per annum, with a total cost of approximately 40 billion dollars (Sharma et al. 2020). Despite being essential to guarantee agricultural productivity, pesticides can have highly deleterious impacts on the environment, biodiversity, and, in particular, public health (Gil and Pla 2001; Parker et al. 2017; Vale et al. 2019; Sharma et al. 2020; Ramos et al. 2021).
Exposure to pesticides occurs primarily through inhalation and dermal contact (Cuenca et al. 2019; Godoy et al. 2019; Sharma et al. 2020; Ramos et al. 2021). Exposure to high concentrations over a short period of time can lead to acute poisoning, but may also have chronic effects, which may only become several months or even years after the original exposure (Sharma et al. 2020; Ramos et al. 2021). There are a number of occupational risk groups, ranging from the individuals employed in the industrial production of these xenobiotic substances to transporters and distributors, and, in particular, the farm workers involved in the mixing, application, and spraying of pesticides on a regular basis (Damalas and Koutroubas 2016; Ye et al. 2017; Cuenca et al. 2019; Kalliora et al. 2018).
The acute or chronic effects associated with the production, distribution, and use of pesticides may be manifested in cytotoxic disorders, genotoxic mechanisms with immunotoxicity, hormonal changes, or carcinogenesis (VoPham et al. 2017; Kapeleka et al. 2019; Saad-Hussein et al. 2019). Pesticides can induce the formation of the free radicals that cause oxidative stress, and may provoke changes in the enzymatic system that eliminates and depletes the antioxidant reservoir in the cell, causing damage to the DNA, which may result in mutations, double-strand and chromosomal breaks, and the formation of DNA adducts (Eren et al. 2016; Barrón-Cuenca et al. 2019; Marcelino et al. 2019). Organophosphorus toxicants impair the action of thyroid hormones by affecting different parts of the hypothalamus–pituitary–thyroid axis (Rashidi et al., 2020), i.e., the hormone receptors, the synthesis of the hormones, and their secretion and metabolism.
Ramos et al. (2021) also identified a number of studies which demonstrated that the toxic effects of pesticides could lead to immunostimulation or immunosuppression (Barnett and Brundage 2010; Corsini et al. 2013), although the exact mechanisms are still unclear (Noworyta-Głowacka et al. 2012; Aroonvilairat et al. 2015; Medina-Buelvas et al. 2019). The disorders known to be associated with pesticides include several types of cancer (Mostafalou and Abdollahi 2017; Calaf 2021), congenital malformations (Castillo-Cadena et al. 2017; Rocha and Grisolia 2018), problems in the reproductive system (García et al. 2017; Hu et al. 2018), depression, anxiety, Parkinson’s and Alzheimer’s diseases, and even death (Ratnasekhar et al. 2019; Sharma et al. 2020).
Given this association, it is essential to monitor the diseases that are associated with occupational exposure to pesticides, in particular, to identify both the potential risks of these substances to human health and the measures that can be taken to mitigate this problem. Although the impact of pesticides on human health is not a new question, bibliometric studies that elucidate patterns of research and, in particular, knowledge gaps, are still scarce. Given this, the present study applied a bibliometric approach to the research published on the association between cancer and the occupational exposure to pesticides over the past 10 years. We focus on the studies published between January 2011 and December 2020, in order to identify (i) which countries have produced most research on the risks associated with occupational exposure to pesticides, (ii) the types of cancer most frequently associated with occupational exposure to pesticides, (iii) the methods used to investigate this association, and (iv) the principal knowledge gaps that persist in this area of research, with the aim of providing guidelines for future studies.
Material and methods
Data and the selection of papers
The present study was based on a literature search of the Scopus® database, a trademarked product of Elsevier BV Scopus (www.elsevier.com), which was used to identify studies published recently on the association between cancer and occupational exposure to pesticides. We selected the Scopus® database for this study because it provides the most comprehensive global coverage of a multidisciplinary field (Elsevier 2014; AlRyalat et al. 2019).
We used the three search terms: “pesticide,” “farmer,” and “cancer” in our review of the period between January 2011 and December 2020, which saw a significant increase in the use of pesticides, worldwide (Sharma et al. 2019). The recent growth in the use of pesticides has led to a major increase in the number of cases of acute pesticide poisoning, which represents a significant global public health challenge, especially in the case of farm workers (Boedeker et al. 2020; Nascimento et al. 2020).
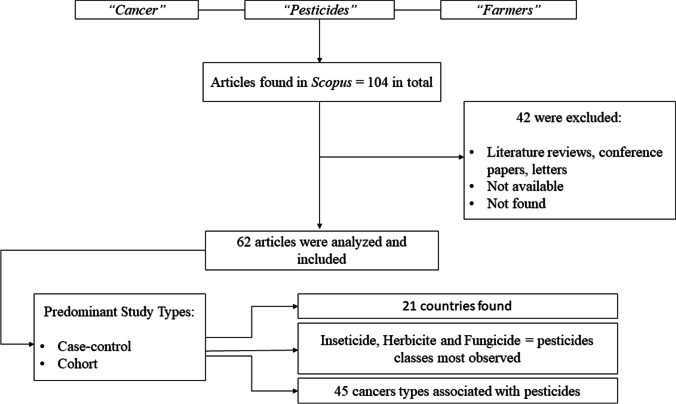
We identified a total 104 papers, but after screening, only 62 were selected for the present study (Fig. 1). The selected papers referred to studies that analyzed susceptibility to cancer related to direct exposure to pesticides or inferred carcinogenesis derived from observations of the action of pesticides in rural workers. The 42 papers excluded following screening were classified as literature reviews, letters not related directly to the study focus, and sites that could not be accessed.
Fig. 1.
Flowchart of selection, inclusion, and exclusion of the papers for bibliometrics involving occupational exposure to pesticides and cancer
Analysis of the database
For each of the papers included in the final analysis, we identified the following variables: (i) the year of the study, (ii) the country in which the study was conducted, (iii) the country of the affiliation of the first author, (iv) the year when the paper was published, (v) the type of cancer studied, (vi) the type of pesticide involved in the study (classified by group according to the chemical compound), and (vii) the principal methods used in the investigation of the cancer risk (we considered only the methods that had practical applications and that were related directly to the proposed research theme).
Data analysis
The data are presented in both absolute and relative frequencies. To analyze the distribution of the studies over the 10-year survey period, we first applied the Shapiro–Wilk test to determine the normality of the data and, as the data were not distributed normally, we applied the nonparametric X2 test. The variation in the distribution of the studies based on the type of exposure (direct, indirect, or a combination of the two) and the type of study (cohort, case–control, or transversal) was evaluated using an analysis of variance (ANOVA) with Tukey’s post hoc test for pairwise comparisons. The variation in the distribution of the different classes of pesticide among the published studies was evaluated using the Kruskal–Wallis nonparametric analysis of variance (H), followed by Dunn’s post hoc test. These variables are presented as the mean ± standard deviation (SD).
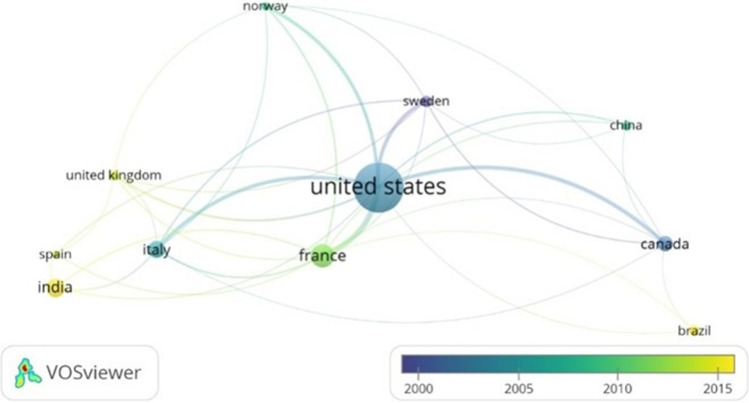
We used the VOSviewer program from the University of Leiden (http://www.vosviewer.com/) to generate a cluster plot of the scientific collaboration among countries. The QGis software (version 3.14.1) was used to plot the sites of the different studies.
Results
Geographical distribution of the recent studies of cancer and pesticides
The number of papers (N = 62) published per annum varied significantly over the course of the study decade (X2 = 27.636, d.f. = 8; p = 0.0005; Fig. 2), peaking between 2017 and 2019. It seems likely that the reduced number of studies published in 2020 was related to the COVID-19 pandemic.
Fig. 2.
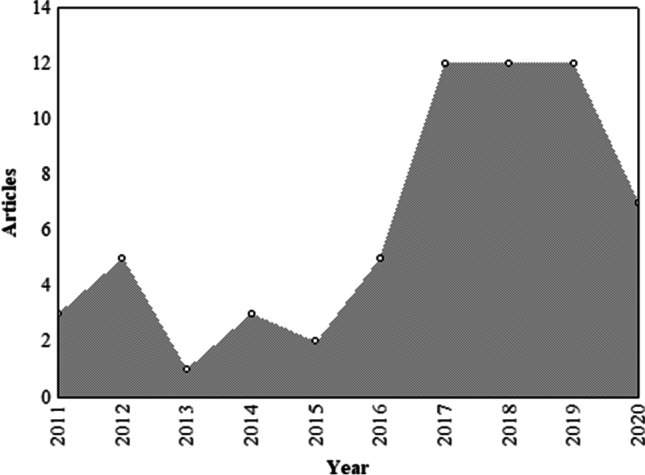
Scientific production associating cancer with occupational exposure to pesticides in rural workers from 2011 to 2020
The studies reported in the 62 papers were classified as analyses of either direct or indirect exposure to pesticides, or a combined (direct and indirect) approach. The mean number of papers published per annum using each of these three approaches varied significantly over the decade (F(2;27) = 4.5044; p = 0.02), with direct exposure studies (mean papers per annum = 3.20 ± 2.15) being significantly (p < 0.05) more frequent than either the indirect exposure (mean = 0.60 ± 1.07) or the combined approach (mean = 1.70 ± 2.36).
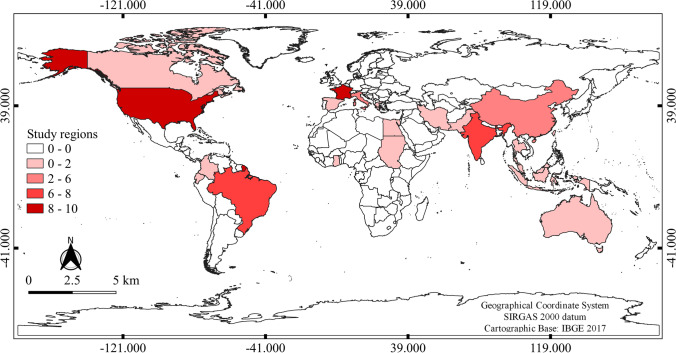
Overall, the 62 papers identified in the present study were published by authors from 21 countries. Almost one fifth (19.35%, n = 12) of these studies were conducted in the USA, followed by France (n = 9; 14.52%), India (n = 8; 12.9%; Fig. 3), and Brazil (n = 7; 11.29%). If we consider co-authorships and collaborations among countries (Fig. 4), the scientific output from the USA is even more predominant, although countries such as India, Brazil, and Spain have produced more publications in recent years.
Fig. 3.
Geographical aspects of scientific production on cancer associated with occupational exposure to pesticides
Fig. 4.
Clusters of scientific production per year involving cancer and occupational exposure to pesticides
Types of cancer and their association with pesticides
A total of 45 different types of cancer were identified in the 62 papers evaluated in the present study, of which, four were most frequent (Fig. 5). These included multiple myeloma and bladder cancer, which were each focused on in eight papers (12.9% of the total), and non-Hodgkin lymphoma (NHL) and prostate cancer, both appearing in seven papers (11.3%). The other cancers featured in between one and six studies.
Fig. 5.
Types of cancer frequently associated with occupational exposure to pesticides between 2011 and 2020
Pesticides
The three principal types of pesticide featured in the papers identified in the present study, according to the mean frequency of occurrence in the published papers, insecticides (mean papers per annum = 3.7 ± 2.26), herbicides (mean = 2.8 ± 1.81), and fungicides (mean = 1.9 ± 0.99). These types of pesticide featured significantly more often in the papers published during the study period (H = 30.2439; p < 0.05) than other pesticides, such as acaricides (mean = 0.20 ± 0.42) and nematicides (mean = 0.10 ± 0.32). The principal types of pesticide recorded during the present study are listed in Supplementary File 1. The least-studied pesticides were acaricides, rodenticides, and larvicides, and the paucity of studies on these types of compounds may reflect a knowledge gap in terms of the diversity of the available pesticides.
Principal methods used to investigate cancer risk
The application of questionnaires was a very frequent research strategy in the studies reviewed here (Table 1). This approach provides data on the lifestyle, socio-economic profile, and social context of the interviewee, and the diagnosis of these data can provide important insights into the most appropriate approach for the investigation of the study population. The other principal investigative techniques involved the collection and analysis of biological material. The most frequently used techniques were the micronucleus test (n = 5 studies; 7.9%), hematological analyses (n = 4; 6.4%), and biochemical tests (n = 4; 6.4%).
Table 1.
Main methodologies described in the selected papers to evaluate cancer and occupational exposure to pesticides
| Methodologies | Classification (types) | Number of studies N (%) |
|---|---|---|
| Qualitative methods | Questionnaire | 24 (38.7%) |
| MRADC | 2 (3.1%) | |
| Molecular biology | PCR | 2 (3.1%) |
| SNP genotyping | 2 (3.1%) | |
| Methylation profile | 3 (4.8%) | |
| Cytogenetic tests | Micronucleus test | 5 (7.9%) |
| Comet assay | 3 (4.8%) | |
| Fluorescent in situ hybridization (FISH) | 1 (1.6%) | |
| Hematological tests | Complete blood count (CBC) | 4 (6.4%) |
| Biochemical tests | Acetylcholinesterase quantification | 3 (4.8%) |
| Other biochemical tests | 4 (6.4%) | |
| Determination of pesticides residues (in saliva, blood, urine) | Spectrometry | 3 (4.8%) |
| Chromatography | 4 (6.4%) | |
| Immunological analyses | Flow cytometry | 1 (1.6%) |
| Immunofluorescence staining | 1 (1.6.%) |
MRADC medical record analysis and death certificate, PCR polymerase chain reaction, SNP single nucleotide polymorphism
Other techniques, such as the quantification of acetylcholinesterase, comet assay, and methylation profiles, while less frequent, were also applied in the studies of the association between cancer and pesticide use (Table 1). The vast majority of the studies were based on either the monitoring of cohorts (n = 24; 38.71%) or the case–control approach (n = 23; 37.1%). The other studies were based on a cross-sectional approach (n = 9; 14.52%), longitudinal monitoring (n = 3; 4.84%), and a descriptive or biomonitoring approach, each used in one (1.61%) study (Rusiecki et al. 2017; Kumar et al. 2018; Joshi et al. 2019; Shearer et al. 2019). However, no significant variation was found (F(2;27) = 1.9939, p = 0.154) in the application of the three most frequently-used approaches (cohort, case–control or cross-sectional studies) among the different years of the study period.
Discussion
The present study reviews the studies on the potential association between cancer and occupational exposure to agricultural pesticides published over the past 10 years. The USA was the most prominent source country, which is consistent with the leading role of this country in most fields of scientific knowledge (Haeffner et al. 2019). While the USA is a major scientific powerhouse responsible for an enormous output of good quality and high impact research (NSF 2018), this country has been losing ground in recent years due to the increasing of the global scientific landscape (Tollefson 2018). In recent years, countries such as China, India, and Brazil have been investing increasingly in science and technological research and are producing papers in ever-growing numbers (Klebis 2018).
The prominence of the USA in pesticide research is also consistent with the fact that this country is one of the world’s largest producers of foodstuffs and also among its principal users of pesticides (Donley 2019). Research in this field has also been driven by a large number of cohort studies in agricultural health in Iowa and North Carolina (Waggoner et al. 2011; Rusiecki et al. 2017; Shrestha et al. 2019).
Europe, India, and Brazil are also major users of agricultural pesticides, which represent a potential problem for non-target organisms, including humans (Hossard et al. 2017; Paumgartten 2020; Zheng et al. 2020). In France, the AGRICAN (Agriculture and Cancer) cohort study, which began in 2005, has provided important insight into rare diseases due to the large number of participants—more than 181,000 individuals (Tual et al. 2013; Lemarchand et al. 2016; Piel et al. 2017, 2019; Boulanger et al. 2018). One study in France showed that more than half (54.4%) of the 408 cases of occupational exposure to pesticides referred to a poison control center between 2012 and 2016 involved insecticides, while a third (33.3%) involved herbicides, and 12.2%, fungicides (Boucaud-Maitre et al. 2019; Tual et al. 2019).
Since the Green Revolution, the intensification of pesticide use in India has had significant long-term impacts on public health and the environment (Keswani et al. 2019). The Indian economy is highly agriculture-oriented, with approximately 70% of the country’s population being involved in some form of agriculture (Keswani et al. 2019). India is currently the world’s fourth largest producer of pesticides in Asia and is ranked 12th in the countries that most apply pesticides to crops, (Reddy and Wagh 2020; TAAS 2020). The dependence of this population on agricultural activities makes it especially vulnerable to occupational exposure to pesticides, especially when they are applied without adequate regulation.
In Brazil, the agrarian economy is based on the mechanized production of cash crops for export, which involves the intensive application of pesticides (Porto and Soares 2012; Rocha et al. 2019). Brazil has become a major consumer of pesticides, and in 2019, unprecedented amounts of these substances were released into the environment, as documented by the Ministry of Agriculture since 2005 (Nascimento et al. 2020; Ramos et al. 2021). Given the importance of pesticides for the Brazilian system, many international corporations have been attracted to the local market, although the unregulated use of these substances may be a widespread problem (Sant’Ana et al. 2019). Nascimento et al. (2020) recently demonstrated a positive correlation between cultivated areas and intoxication by pesticides, reflecting an emerging problem in the country, due to the ongoing expansion of agricultural frontiers.
Salerno et al. (2016) documented many cancers attributed to exposure to herbicides, including myeloma, non-melanoma skin cancer, colorectal cancer, and breast cancer. Lemarchand et al. (2017) found that the incidence of multiple myeloma was higher in male pesticide handlers, whereas that of melanoma was higher in females. Multiple myeloma, a hematopoietic malignancy of the plasma cells, is one of the most common hematological cancers in men and women (Tual et al. 2019), and it is frequently manifested in farm workers exposed occupationally to pesticides, although the causal factors are still poorly understood (Ferri et al. 2017; Packard et al. 2019). The incidence of bladder cancer has also increased substantially since the 1950s (Boada et al. 2016). Jackson et al. (2017) found that cohabitation with a farmer increased the risk of bladder cancer in married Egyptian women. Boulanger et al. (2017) further reinforced the potential relationship between bladder cancer and exposure to pesticides, with an exposure–response relationship determined by the number of years of occupational exposure, as well as a potentially greater risk in women.
However, some studies of organochlorine pesticides have found no evidence that exposure to these compounds, per se, constitutes an isolated risk factor for bladder cancer (Boada et al. 2016). These authors reinforced the role of the genes that encode xenobiotic-metabolizing enzymes in bladder cancer. Even so, other studies have shown a significant relationship between pesticides and some types of cancer.
Zakerinia et al. (2012) demonstrated that the risk of non-Hodgkin Lymphoma (NHL) and multiple myeloma was much higher in individuals exposed to insecticides in Shiraz, southern Iran, in comparison with non-exposed individuals. Occupational exposure to DDT, lindane, permethrin, diazinon, and terbufos has also been associated with NHL (Alavanja et al., 2014). Ferri et al. (2017) demonstrated that occupational exposure to the fungicide Captafol was associated significantly with the risk of NHL. Tsai et al. (2018) also identified an increase of death related to NHL from an analysis of the death certificates of Taiwanese farmers registered between 1997 and 2009.
Lemarchand et al. (2016, 2017) also found evidence that the risk of prostate cancer is increased in farmers. Band et al. (2011) demonstrated a significant association between prostate cancer and exposure to DDT, simazine, and lindane. The standardized mortality rate in workers exposed to pesticides was relatively high in the cases of melanoma, prostate, breast and lymphohematopoietic cancers, and cancers of the digestive system, kidney, and brain (Hoseini et al. 2017). A significant risk of the development of tumors in the primary central nervous system of farm workers has also been found, in particular in those that apply pesticides and cultivate peas (Piel et al. 2017). These authors also found a two to three times higher risk of tumors in the central nervous system following exposure to (dithio/thio)-carbamates in farm workers who grow vines, fruit, potatoes, and sugar beet. Jones et al. (2014) found that the risk of developing acute myeloid leukemia was higher in women living in agricultural areas than those in in urban areas.
It is important to note that, while a substantial number of papers was identified in the present review, there is in fact a relative paucity of research in this field, considering that cancer is one of the principal risks to human health, and is known to be associated with occupational exposure to pesticides, an increasing problem worldwide, in addition to its association with other comorbidities (Brust et al. 2019; Jacobsen-Pereira et al. 2020; Mongedet al. 2020). Even when convincing evidence is presented, the procedures used to confirm this association and its determining factors are often not dealt with adequately (Elebead et al. 2012; Tual et al. 2013; Jin et al. 2017; Tarar and Riaz 2019; Hutter et al. 2020). Kachuri et al. (2017) observed that exposure to pesticides may lead to an increase in hematopoietic cancers, whereas increased risks of lip cancer and melanoma may be attributed to exposure to the sun. Given this, Darcey et al. (2018) also draw attention to the risks derived from factors such as solar radiation, diesel exhaust fumes, and certain types of solvent, as observed in more than 85% of the farming population of Western Australia.
Most of the papers analyzed in the present study added further to the evidence that occupational exposure to pesticides contributes to an increased risk of the development of cancer in farmer workers. In comparison with the general population, however, these workers are also more susceptible to other factors that further reinforce the effects of specific oncological in these individuals (Salerno et al. 2014, 2016; Gunier et al. 2017; Jackson et al. 2017).
Although it is possible to establish a relationship between the pesticide concentrations in the body and the body’s response to these compounds, the scenario is complex, given that it depends on a range of factors. In general, pesticides target essential metabolic pathways (Sharma et al. 2020) and may interact with these pathways in different ways, depending on the type of compound, the dose, and the target organs, resulting in multiple effects (Hernandez et al. 2017). For example, toxicokinetic and genetic factors, as well as pesticides, may induce disturbances in the immune system and even carcinogenesis, through an increase in the production of reactive oxygen species, which contributes to an increase in DNA damage, immunotoxicity, and chromosomal aberrations (Gil and Pla 2001; Pressuti et al. 2016; Jacobsen-Pereira et al. 2020).
Humans may be exposed to pesticides through a number of different processes, including occupational activities that involve the production, transportation, delivery, and application of these substances, as well as inhabiting areas with high levels of pesticide contamination and the accumulation of residues in the food chain (Mostafalou and Abdollahi 2017). Pesticides may be available in liquid, solid, or gaseous forms, which will facilitate their absorption, through contact with the skin, inhalation, or ingestion (Ratnasekhar et al. 2019; Sharma et al. 2020).
While farm workers are usually aware that continuous exposure to pesticides may induce illness (Kannuri and Jadhav 2018), many workers or employers tend to neglect the need for personal protective equipment (PPE) and adequate training for the safe handling of pesticides (Godoy et al. 2019). This obviously contributes to any propensity for the development of cancer and means that a worker may be directly and indirectly exposed to pesticides at storage, preparation, mixing, and application, in residential areas where pesticides are used, and may have contact with exposed workers and their contaminated clothing or tools). Commercial suppliers and regulatory agencies could contribute to the mediation of these effects, by providing guidance on the handling and application of these substances (Salerno et al. 2016; Godoy et al. 2019; Ramos et al. 2021).
An additional question is the impregnation of work clothes and tools, as well as the worker’s hands, which may result in the passive transfer of pesticides to other individuals (Zakerinia et al. 2012). Amr et al. (2014) showed that women married to farm workers or who have contact with these individuals are at a greater risk of developing bladder cancer than other individuals. An increase in the number of leukemia cases has also been recorded in children of under 5 years of age, which was not linked to any maternal or intrauterine exposure to pesticides, but rather to perinatal exposure to the contaminated father (Salerno et al. 2016; Gunier et al. 2017; Jackson et al. 2017). These various factors compromise the selection of the most adequate methods for the testing and analysis of the potential link between cancer and pesticides in different populations.
For example, Cepeda et al. (2020) warn that even though the factors associated with the development of the cancer are discussed, data on cancer types and their frequency are often lacking. It is important to note here that the monitoring of exposure to xenobiotics, such as pesticides, using biomarkers like the micronucleus test, is an essential tool for the early detection and prevention of diseases such as oral cancer (Tomiazzi et al. 2018). Another factor limiting the conclusions of a toxicological or genotoxic analysis is the timing of the testing, which means that it may not always be possible to link the results with the specific components of a pesticide, which is an important question, given that the mixing of pesticides is a common practice (Hutter et al. 2020; Ramos et al. 2021). This represents an additional problem with the application of questionnaires, given that almost half of the farm workers do not know which pesticides they have been exposed to (Vindas et al. 2004).
Overall, then, the results of the present study emphasize the need to evaluate overuse of pesticides and the concomitant increase in the number of cancer cases. Future research should thus include active intervention in the correct use of pesticides by farm workers and encourage adequate training and the use of PPEs, as well as routine periodic medical examinations.
Final considerations and future perspectives
The present study analyzed the scientific production on the association between cancer and occupational exposure to agricultural pesticides over the past decade. Countries such as the USA, France, India, and Brazil have been the driving force of this research. In these studies, a number of different cancers were associated exposure to pesticides, including multiple myeloma, non-Hodgkin’s Lymphoma, leukemia, and bladder, breast, and prostate cancer.
In general, farm workers are aware of the risks of pesticide exposure, but due to a lack of adequate training on the use of personal protective equipment, many workers and their employers neglect the adoption of adequate precautions during the handling and application of pesticides. In this context, it would be important for pesticide manufacturers and their distributors, together with the personnel of local cooperatives, to contribute to the training of farm workers, as well as encouraging a reduction in the application of toxic agents, the adoption of integrated pest management approaches, and the implementation of further scientific research.
Agricultural cohort studies have focused on a range of diseases that may be associated with the exposure of farm workers to toxic substances. This association can be confirmed most effectively using questionnaires to cross-reference the data, when complemented with appropriate methods. Despite the availability of these methodological tools, and the fact that many studies have identified a relationship between cancer risk and occupational exposure to pesticides, the mechanisms involved are not described adequately, which results in a persistent knowledge gap in this field of research.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
T.M.A.P., M.B.S., and J.W. thank the Coordination for Higher Education Personnel Training (CAPES) for scholarships, while T.M.A.P. is also grateful to the Goiás State Research Foundation (FAPEG), and M.B.S. to the Brazilian Fund for Biodiversity (FUNBIO), for additional scholarships. D.M.S. is grateful to the National Council for Scientific and Technological Development (CNPq) for a research productivity grant (Process: 307652 / 2018-1).
Author contribution
T.M.A.P., F.G.R., and D. M.S. conceived the idea for the present study.
T.M.A.P., F.A.N., M.B-S, and J.W. developed the analytical methods.
T.M.A.P. wrote the manuscript with support from J.W., M.B-S, F.G.R, and D.M.S.
All the authors provided critical feedback and helped formulate the research and analysis and finalize the manuscript.
Data availability
The datasets analyzed in the present study are available from the corresponding author on reasonable request.
Declarations
Ethical approval
Not applicable.
Consent to participate
No consent to participate is required because no human participants were involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alavanja MC, Hofmann JN, Lynch CF, Hines CJ, Barry KH, Barker J, Buckman DW, Thomas K, Sandler DP, Hoppin JA, Koutros S, Andreotti G, Lubin JH, Blair A, Freeman LEB. Non-Hodgkin lymphoma risk and insecticide, fungicide and fumigant use in the agricultural health study. PLoS ONE. 2014;9:e109332. doi: 10.1371/journal.pone.0109332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AlRyalat SAS, Malkawi LW, Momani SM (2019) Comparing bibliometric analysis using PubMed, Scopus, and Web of Science databases. J Vis Exp 152. 10.3791/58494 [DOI] [PubMed]
- Amr S, Dawson R, Saleh DA, Magder LS, Mikhail NN, St George DM, Squibb K, Khaled H, Loffredo CA. Agricultural workers and urinary bladder cancer risk in Egypt. Arch Environ Occup Health. 2014;69(1):3–10. doi: 10.1080/19338244.2012.719556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aroonvilairat S, Kespichayawattana W, Sornprachum T, Chaisuriya P, Siwadune T, Ratanabanangkoon K. Effect of pesticide exposure on immunological, hematological and biochemical parameters in Thai orchid farmers— a cross-sectional study. Int J Environ Res Public Health. 2015;12:5846–5861. doi: 10.3390/ijerph120605846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Band PR, Abanto Z, Bert J, Lang B, Fang R, Gallagher RP, Le ND. Prostate cancer risk and exposure to pesticides in British Columbia farmers. Prostate. 2011;71:168–183. doi: 10.1002/pros.21232. [DOI] [PubMed] [Google Scholar]
- Barnett JB, Brundage KM (2010) Immunotoxicology of pesticides and chemotherapies. In Comprehensive Toxicology, Second Edition 5:467–487). 10.1016/B978-0-08-046884-6.00627-8
- Barrón-Cuenca J, Tirado N, Barral J, Ali I, Levi M, Stenius U, Berglund M, Dreij K. Increased levels of genotoxic damage in a Bolivian agricultural population exposed to mixtures of pesticides. Sci Total Environ. 2019;695:133942. doi: 10.1016/j.scitotenv.2019.133942. [DOI] [PubMed] [Google Scholar]
- Boada LD, Henriquez-Hernandez LA, Zumbado M, Almeida-Gonzalez M, Alvarez-Leon EE, Navarro P, Luzardo OP. Organochlorine pesticides exposure and bladder cancer: evaluation from a gene-environment perspective in a hospital-based case-control study in the Canary Islands (Spain) J Agromedicine. 2016;21:34–42. doi: 10.1080/1059924X.2015.1106374. [DOI] [PubMed] [Google Scholar]
- Boedeker W, Watts M, Clausing P. Marquez E (2020) The global distribution of acute unintentional pesticide poisoning: estimations based on a systematic review. BMC Public Health. 2020;20:1875. doi: 10.1186/s12889-020-09939-0. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Boucaud-Maitre D, Ranabourg MO, Sinno-Tellier S, Puskarczyk E, Pineau X, Kammerer M, Bloch J, Langrand J. Human exposure to banned pesticides reported to the French Poison Control Centers: 2012–2016. Environ Toxicol Pharmacol. 2019;69:51–56. doi: 10.1016/j.etap.2019.03.017. [DOI] [PubMed] [Google Scholar]
- Boulanger M, Tual S, Lemarchand C, Guizard AV, Velten M, Marcotullio E, et al. Agricultural exposure and risk of bladder cancer in the AGRIculture and CANcer cohort. Int J Hyg Environ Health. 2017;90:169–178. doi: 10.1007/s00420-016-1182-y. [DOI] [PubMed] [Google Scholar]
- Boulanger M, Tual S, Lemarchand C, Guizard AV, Delafosse P, Marcotullio E, Pons R, Piel C, Pouchieu C, Baldi I, Clin B, Lebailly P, AGRICAN group, Lung cancer risk and occupational exposures in crop farming: results from the AGRIculture and CANcer (AGRICAN) cohort. Occup Environ Med. 2018;75:776–785. doi: 10.1136/oemed-2017-104976. [DOI] [PubMed] [Google Scholar]
- Brust RS, Oliveira LPMD, Silva ACSSD, Regazzi ICR, Aguiar GSD, Knupp VMDAO. Epidemiological profile of farmworkers from the state of Rio de Janeiro. Rev Bras Enferm. 2019;72:122–128. doi: 10.1590/0034-7167-2017-0555. [DOI] [PubMed] [Google Scholar]
- Calaf GM. Role of organophosphorous pesticides and acetylcholine in breastcarcinogenesis. Seminars Cancer Biology. 2021 doi: 10.1016/j.semcancer.2021.03.016. [DOI] [PubMed] [Google Scholar]
- Castillo-Cadena J, Mejia-Sanchez F, López-Arriaga JA. Congenital malformations according to etiology in newborns from floricultural zone of Mexico state. Environ Sci Pollut Res. 2017;2:7662–7667. doi: 10.1007/s11356-017-8429-3. [DOI] [PubMed] [Google Scholar]
- Cepeda S, Forero-Castro M, Cárdenas-Nieto D, Martínez-Agüero M, Rondón-Lagos M. Chromosomal instability in farmers exposed to pesticides: high prevalence of clonal and non-clonal chromosomal alterations. Risk Manag Healthc Policy. 2020;13:97. doi: 10.2147/RMHP.S230953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corsini E, Sokooti M, Galli CL, Moretto A, Colosio C. Pesticide inducedimmunotoxicity in humans: a comprehensive review of the existing evidence. Toxicology. 2013;307:123–135. doi: 10.1016/j.tox.2012.10.009. [DOI] [PubMed] [Google Scholar]
- Cuenca JB, Tirado N, Vikström M, Lindh CH, Steinus U, Leander K, Berglund M, Dreij K. Pesticide exposure among Bolivian farmers: associations between worker protection and exposure biomarkers. J Expo Sci Environ Epidemiol. 2019;30:730–742. doi: 10.1038/s41370-019-0128-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damalas CA, Koutroubas SD. Farmers’ exposure to pesticides: toxicity types and ways of prevention. Toxics. 2016;8:1. doi: 10.3390/toxics4010001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darcey E, Carey RN, Reid A, Driscoll T, Glass DC, Benke GP, Peters S, Fritschi L (2018) Prevalence of exposure to occupational carcinogens among farmers. Rural Remote Health 18:4348. 10.22605/RRH4348 [DOI] [PubMed]
- Donley N. The USA lags behind other agricultural nations in banning harmful pesticides. Environ Health. 2019;18:44. doi: 10.1186/s12940-019-0488-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elebead FM, Hamid A, Hilmi HSM, Galal H. Mapping cancer disease using geographical information system (GIS) in Gezira State-Sudan. J Community Health. 2012;37:830–839. doi: 10.1007/s10900-011-9517-9. [DOI] [PubMed] [Google Scholar]
- Elsevier Scopus comes of age (2014) Available at: https://www.elsevier.com/about/press-releases/science-and-technology/scopus-comes-of-age. Accessed on June 15, 2021
- EPA (2020) U.S. Environmental Protection Agency. What is a pesticide? Available in: <http://www.epa.gov/pesticides/about/index.htm> Accessed on: October 21, 2020
- Eren Y, Erdogmus SF, Akyıl D, Ozkara A. Mutagenic and cytotoxic activities of benfuracarb insecticide. Cytotechnology. 2016;68:637–643. doi: 10.1007/s10616-014-9811-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferri GM, Specchia G, Mazza P, Ingravallo G, Intranuovo G, Guastadisegno CM, Congedo ML, Lagioia G, Loparco MC, Giordano A, Perrone T, Guadio F, Spinosa C, Minoia C, D’Onghia L, Strusi M, Corrado V, Cavone D, Vimercati L, Schiavulli N, Cocco P. Risk of lymphoma subtypes by occupational exposure in Southern Italy. J Occup Med Toxicol. 2017;12:31. doi: 10.1186/s12995-017-0177-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- García J, Ventura MI, Requena M, Hernández AF, Parrón T, Alarcón R. Association of reproductive disorders and male congenital anomalies with environmental exposure to endocrine active pesticides. Reprod Toxicol. 2017;71:95–100. doi: 10.1016/j.reprotox.2017.04.011. [DOI] [PubMed] [Google Scholar]
- Gil F, Pla A. Biomarkers as biological indicators of xenobiotic exposure. J Appl Toxicol. 2001;21:245–255. doi: 10.1002/jat.769. [DOI] [PubMed] [Google Scholar]
- Godoy FR, Nunes HF, Alves AA, Carvalho WF, Franco FC, Pereira RR, da Cruz AS, da Silva CC, Bastos RP, Silva DM. Increased DNA damage is not associated topolymorphisms inOGGIDNA repair gene, CYP2E1detoxification gene, and biochemical and hematologicalfindings in soybeans farmers from Central Brazil. Environ SciPollut Res. 2019;26:26553–26562. doi: 10.1007/s11356-019-05882-9. [DOI] [PubMed] [Google Scholar]
- Gunier RB, Kang A, Hammond SK, Reinier K, Lea CS, Chang JS, Does M, Scelo G, Kirsch J, Crouse V, Cooper R, Quinlan P, Metayer C. A task-based assessment of parental occupational exposure to pesticides and childhood acute lymphoblastic leukemia. Environ Res. 2017;156:57–62. doi: 10.1016/j.envres.2017.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haeffner C, Zanotto SR, Nader HB, GuimarãesJA, Contrasting high scientific production with low international collaboration and scientific impact: the Brazilian case. Scientometrics Recent Advances, Suad Kunosic and Enver Zerem, IntechOpen, 2019 doi: 10.5772/intechopen.85825. [DOI] [Google Scholar]
- Hernandez AF, Gil F, Lacasana M. Toxicological interactions of pesticide mixtures: an update. Arch Toxicol. 2017;91:3211–3223. doi: 10.1007/s00204-017-2043-5. [DOI] [PubMed] [Google Scholar]
- Hoseini M, Bahrampour A, Mirzaee M. Comparison of weibull and lognormal cure models with cox in the survival analysis of breast cancer patients in Rafsanjan. J Res Med Sci. 2017;17:369. [PubMed] [Google Scholar]
- Hossard L, Guichard L, Pelosi C, Makowski D. Lack of evidence for a decrease in synthetic pesticide use on the main arable crops in France. Sci Total Environ. 2017;575:152–161. doi: 10.1016/j.scitotenv.2016.10.008. [DOI] [PubMed] [Google Scholar]
- Hu Y, Ji L, Zhang Y, Shi R, Han W, Tse LA, Pan R, Wang Y, Ding G, Xu J, Zhang Q, Gao Y, Tian Y. Organophosphate and pyrethroid pesticide exposures measured before conception and associations with time to pregnancy in Chinese couples enrolled in the Shanghai birth cohort. Environ Health Perspect. 2018;126:077001. doi: 10.1289/EHP2987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hutter HP, Poteser M, Lemmerer K, Wallner P, Shahraki Sanavi S, Kundi M, Moshammer H, Weitensfelder L. Indicators of genotoxicity in farmers and laborers of ecological and conventional banana plantations in Ecuador. Int J Environ Res. 2020;17:1435. doi: 10.3390/ijerph17041435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson SS, St George DM, Loffredo CA, Amr S. Non-occupational exposure to agricultural work and risk of urinary bladder cancer among Egyptian women. Arch Environ Occup Health. 2017;72:166–172. doi: 10.1080/19338244.2016.1169155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen-Pereira CH, Cardoso CC, Gehlen TC, dos Santos CR, Santos-Silva MC. Immune response of Brazilian farmers exposed to multiple pesticides. Ecotox Environ Safety. 2020;202:110912. doi: 10.1016/j.ecoenv.2020.110912. [DOI] [PubMed] [Google Scholar]
- Jin J, Wang W, He R, Gong H. Valuing health risk in agriculture: a choice experiment approach to pesticide use in China. Environ Sci Pollut Res. 2017;24:17526–17533. doi: 10.1007/s11356-017-9418-2. [DOI] [PubMed] [Google Scholar]
- Jones RR, Yu CL, Nuckols JR, Cerhan JR, Airola M, Ross JA, Robien K, Ward MH. Farm residence and lymphohematopoietic cancers in the Iowa Women’s Health Study. Environ Res. 2014;133:353–361. doi: 10.1016/j.envres.2014.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi G, Joshi AG, Sontakke A, Wingkar KC, Mane D (2019) Pesticides: Deleterious Effects on Neurotransmission. Indian J. Forensic Med. Toxicol 13
- Kachuri L, Harris MA, MacLeod JS, Tjepkema M, Peters PA, Demers PA. Cancer risks in a population-based study of 70,570 agricultural workers: results from the Canadian census health and Environment cohort (CanCHEC) BMC Cancer. 2017;17:1–15. doi: 10.1186/s12885-017-3346-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalliora C, Mamoulakis C, Vasilopoulos E, Stamatiades GA, Kalafati L, Barouni R, Tsatsakis A (2018) Association of pesticide exposure with human congenital abnormalities. Toxicology and Applied Pharmacology. Academic Press Inc. 10.1016/j.taap.2018.03.025 [DOI] [PMC free article] [PubMed]
- Kannuri NK, Jadhav S. Generating toxic landscapes: impact on the well-being of cotton farmers in Telangana, India. Anthropol Med. 2018;25:121–140. doi: 10.1080/13648470.2017.1317398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapeleka JA, Sauli E, Ndakidemi PA. Pesticide exposure and genotoxic effects as measured by DNA damage and human monitoring biomarkers. Int J Environ Health Res. 2019;00:1–18. doi: 10.1080/09603123.2019.1690132. [DOI] [PubMed] [Google Scholar]
- Keswani C, Dilnashin H, Birla H, Singh SP. Regulatory barriers to Agricultural Research commercialization: a case study of biopesticides in India. Rhizosphere. 2019;11:100155. doi: 10.1016/j.rhisph.2019.100155. [DOI] [Google Scholar]
- Klebis D (2018) China é o país que produz mais artigos científicos no mundo. Brasil é o 12°. Jornal da Ciência. Available in: http://www.jornaldaciencia.org.br/china-e-o-pais-que-produz-mais-artigos-cientificos-no-mundo-brasil-e-o-12o. Accessed on March 24 2021
- Kumar P, Thakur S, Dhingra GK, Singh A, Pal MK, Harshvardhan K, Dubey RC, Maheshwari DK. Inoculation of siderophore producing rhizobacteria and their consortium for growth enhancement of wheat plant. Biocatal Agric Biotechnol. 2018;15:264–269. doi: 10.1016/j.bcab.2018.06.019. [DOI] [Google Scholar]
- Langley RL, Mort SA. Human exposures to pesticides in the United States. J Agromedicine. 2012;17:300–315. doi: 10.1080/1059924X.2012.688467. [DOI] [PubMed] [Google Scholar]
- Lemarchand C, Tual S, Levêque-Morlais N, Perrier S, Belot A, Velten M, Guizard AV, Marcotullio E, Monnereau A, Chin B, Baldi I, Lebailly P, the AGRICAN group, Cancer incidence in the AGRICAN cohort study (2005–2011) Cancer Epidemiol. 2017;49:175–185. doi: 10.1016/j.canep.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemarchand C, Tual S, Boulanger M, Levêque-Morlais N, Perrier S, Clin B, Guizard AV, Velten M, Rigaud E, Baldi I, Lebailly P (2016) Prostate cancer risk among French farmers in the AGRICAN cohort. Scand J Work Environ. Health 144–152. [DOI] [PubMed]
- Marcelino AF, Wachtel CC, Ghisi N de C (2019) Are our farm workers in danger? Genetic damage in farmers exposed to pesticides. Int J Environ Res Public Health 16. 10.3390/ijerph16030358 [DOI] [PMC free article] [PubMed]
- Medina-Buelvas D, Estrada-Muñiz E, Flores-Valadez M, Vega L. Genotoxic and immunotoxic efects of the organophosphate metabolite diethyldithiophosphate (DEDTP) in Vivo. Toxicol Appl Pharmacol. 2019;366:96–103. doi: 10.1016/j.taap.2019.01.023. [DOI] [PubMed] [Google Scholar]
- Monged MH, Hassan HB, El-Sayed SA. Spatial distribution and ecological risk assessment of natural radionuclides and trace elements in agricultural soil of northeastern Nile Valley. Egypt Water Air Soil Poll. 2020;231:1–24. doi: 10.1007/s11270-020-04678-9. [DOI] [Google Scholar]
- Mostafalou S, Abdollahi M. Pesticides: an update of human exposure and toxicity. Arch Toxicol. 2017;91:549–599. doi: 10.1007/s00204-016-1849-x. [DOI] [PubMed] [Google Scholar]
- Nascimento AF, Alves AA, Nunes HF, Miziara F, Parise MR, de Melo e Silva D Cultivated areas and rural workers’ behavior are responsible for the increase in agricultural intoxications in Brazil? Are these factors associated? Environ Sci Pollut Res. 2020;27:38064–38071. doi: 10.1007/s11356-020-09988-3. [DOI] [PubMed] [Google Scholar]
- Noworyta-Głowacka J, Bańkowski R, Siennicka J, Wiadrowska B, Beresińska M, Ludwicki JK. Influence of chlorpyrifos on the profile of subpopulation of immunoactivecell and their phagocytic activity in an experimental in vivo model. Ann Agric Environ Med. 2012;19:483–486. [PubMed] [Google Scholar]
- NSF (2018) National Science Foundation. Science and Engineering Indicators 2018. NSB-2018–1. Alexandria VA. Available in: <https://www.nsf.gov/statistics/indicators/>Accessed Accessed on March 24, 2021
- Packard E, Shahid Z, Groff A, et al. Multiple myeloma in an agricultural worker exposed to pesticides. Cureus. 2019;11(5):e4762. doi: 10.7759/cureus.4762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker AM, et al. UV/H202 advanced oxidation for abatement of organophosphorus pesticides and the effects on various toxicity screening assays. Chemosphere. 2017;182:477–482. doi: 10.1016/j.chemosphere.2017.04.150. [DOI] [PubMed] [Google Scholar]
- Paumgartten FJR (2020) Pesticides and public health in Brazil. Current Opinion in Toxicology. Elsevier B.V. 10.1016/j.cotox.2020.01.003
- Piel C, Pouchieu C, Tual S, Migault L, Lemarchand C, Carles C, Boulanger M, Gruber A, Rondeau V, Marcotullio E, Lebailly P, Baldi I, AGRICAN group, Central nervous system tumors and agricultural exposures in the prospective cohort AGRICAN. Int J Cancer. 2017;141:1771–1782. doi: 10.1002/ijc.30879. [DOI] [PubMed] [Google Scholar]
- Piel C, Pouchieu C, Carles C, Béziat B, Boulanger M, Bureau M, Busson A, Gruber A, Lecluse Y, Migault L, Renier M, Rondeau V, Schwall X, the AGRICAN group, Agricultural exposures to carbamate herbicides and fungicides and central nervous system tumour incidence in the cohort AGRICAN. Environ Int. 2019;130:104876. doi: 10.1016/j.envint.2019.05.070. [DOI] [PubMed] [Google Scholar]
- Porto FP, Soares WL. Development model, pesticides, and health: a panorama of the Brazilian agricultural reality and proposals for an innovative research agenda. Revista Brasileira De Saúde Ocupacional. 2012;37:17–50. doi: 10.1590/S0303-76572012000100004. [DOI] [Google Scholar]
- Ramos JSA, Pedroso TMA, Godoy FR, Batista RE, de Almeida FB, Francelin C, Ribeiro FLEE, Parise MR, de Melo e Silva, D, Multi-biomarker responses to pesticides in an agricultural population from Central Brazil. Sci Total Environ. 2021;754:141893–141900. doi: 10.1016/j.scitotenv.2020.141893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashidi M, Mahabadi H, Khavanin A (2020) Evaluation of the effects of chronic exposure to organophosphorus pesticides on thyroid function. Asia Pacific Journal of Medical Toxicology9:35–43. 10.22038/apjmt.2020.16385
- Ratnasekhar Ch, Singh AK, Pathak MK, Singh A, Kesavachandran CN, Bihari V, Mudiam MKR. Saliva and urine metabolic profiling reveals altered amino acid and energy metabolism in male farmers exposed to pesticides in Madhya Pradesh State, India. Chemosphere. 2019;226:636–644. doi: 10.1016/j.chemosphere.2019.03.157. [DOI] [PubMed] [Google Scholar]
- Reddy DKH, Wagh D. Association of cognitive function and depression with chronic exposure to organophosphate pesticides in the agricultural community of rural area of Wardha District. Eur J Mol Clin Med. 2020;7:2049–2056. [Google Scholar]
- Rocha GM, Grisolia CK. Why pesticides with mutagenic, carcinogenic and reproductive risks are registered in Brazil. Developing World Vioeth. 2018;19:148–154. doi: 10.1111/dewb12211. [DOI] [PubMed] [Google Scholar]
- Rocha A, Gonçalves E, Almeida E. Agricultural technology adoption and land use: evidence for Brazilian municipalities. J Land Use Sci. 2019;14:320–346. doi: 10.1080/1747423x.2019.1707312. [DOI] [Google Scholar]
- Rusiecki JA, Beane Freeman LE, Bonner MR, Alexander M, Chen L, Andreotti G, Barry KH, Moore LE, Byun HM, Kamel F, Alavanja M, Hoppin JÁ, Baccarelli A. High pesticide exposure events and DNA methylation among pesticide applicators in the agricultural health study. Environ Mol Mutagen. 2017;58:19–29. doi: 10.1002/em.22067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saad-Hussein A, Beshir S, Taha MM, Shahy EM, Shaheen W, Abdel-Shafy EA, Thabet E. Early prediction of liver carcinogenicity due to occupational exposure to pesticides. Mutat Res Genet Toxicol Environ Mutagen. 2019;838:46–53. doi: 10.1016/j.mrgentox.2018.12.004. [DOI] [PubMed] [Google Scholar]
- Salerno C, Carcagnì A, Sacco S, Palin LA, Vanhaecht K, Panella M, Guido D An Italian population-based case-control study on the association between farming and cancer: Are pesticides a plausible risk factor? Arch Environ Occup Health. 2016;71:147–156. doi: 10.1080/19338244.2015.1027808. [DOI] [PubMed] [Google Scholar]
- Salerno C, Sacco S, Panella M, Berchialla P, Vanhaecht K, Palin LA Cancer risk among farmers in the Province of Vercelli (Italy) from 2002 to 2005: an ecological study. Ann Ig. 2014;26:255–263. doi: 10.7416/ai.2014.1983. [DOI] [PubMed] [Google Scholar]
- Sant’Ana GDF, Araujo SHC, Pereira JL, Oliveira EE (2019) Apprehension of illegal pesticides, agricultural productivity and food poisoning on the Brazilian state of Mato Grosso do Sul. Reve Cien Agricolas 36:52–62. 10.22267/rcia.1936E.106
- Sharma A, Kumar V, Shahzad B, Tanveer M, Sidhu GPS, Handa N, Kohli SK, Yadav P, Bali AS, Parihar RD, Dar OI, Singh K, Jasrotia S, Bakshi P, Ramakrishnan M, Kumar S, Bhardwaj R. Thukral AK (2019) Worldwide pesticide usage and its impacts on ecosystem. SN Appl Sci. 2019;1:1446. doi: 10.1007/s42452-019-1485-1. [DOI] [Google Scholar]
- Sharma A, Shukla A, Attri K, Kumar M, Kumar P, Suttee A, Singh G, Barnwal RP, Singla N. Global trends in pesticides: a looming threat and viable alternatives. Ecotox Environ Safe. 2020;201:110812. doi: 10.1016/j.ecoenv.2020.110812. [DOI] [PubMed] [Google Scholar]
- Shearer JJ, Freeman LEB, Liu D, Andreotti G, Hamilton J, Happel J, Lynch CF, Alavanja MC, Hofmann JN. Longitudinal investigation of haematological alterations among permethrin-exposed pesticide applicators in the Biomarkers of Exposure and Effect in Agriculture study. Occup Environ Med. 2019;76:467–470. doi: 10.1136/oemed-2018-105559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrestha S, Parks CG, Keil AP, Umbach DM, Lerro CC, Lynch CF, Chen HL, Blair A, Koutros S, Hofmann JN, Freeman LEB, Sandler DP. Overall and cause- specific mortality in a cohort of farmers and their spouses. Occup Environ Med. 2019;76:632–643. doi: 10.1136/oemed-2019-105724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TAAS. (2020) (Trust for Advancement of Agricultural Sciences), SPS, (Society of Pesticide Science), IPS, (Indian Phytopathological Society), ESI, (Entomological Society of India), 2020. Stakeholders Dialogue on Current Challenges and Way Forward for Pesticides Management - A Road Map. Indian Phytopathological Society
- Tarar MA, Riaz M (2019) Effects of pesticides on male farmer’s health: a study of Muzaffar Garh. Pakistan Journal of Agricultural Sciences, vol. 56, no. 4, 1021–1030. 10.21162/PAKJAS/19.9157
- Tollefson J (2018) China declared largest source of research articles. Spring Nature. 553. 10.1038/d41586-018-00927-4
- Tomiazzi JS, Judai MA, Nai GA, Pereira DR, Antunes PA, Favareto APA. Evaluation of genotoxic effects in Brazilian agricultural workers exposed to pesticides and cigarette smoke using machine-learning algorithms. Environ Sci Pollut Res. 2018;25:1259–1269. doi: 10.1007/s11356-017-0496-y. [DOI] [PubMed] [Google Scholar]
- Tsai SS, Weng YH, Chiu YW, Yang CY. Farming and mortality rates attributed to non–Hodgkin’s lymphoma in Taiwan. J Toxicol Environ Health Part. 2018;A81:31–36. doi: 10.1080/15287394.2017.1408362. [DOI] [PubMed] [Google Scholar]
- Tual S, Clin B, Levêque-Morlais N, Raherison C, Baldi I, Lebailly P. Agricultural exposures and chronic bronchitis: findings from the AGRICAN (AGRIculture and CANcer) cohort. Ann Epidemiol. 2013;23:539–545. doi: 10.1016/j.annepidem.2013.06.005. [DOI] [PubMed] [Google Scholar]
- Tual S, Busson A, Boulanger M, Renier M, Piel C, Pouchieu C, Pons R, Perrier S, Leveque-Morlais N, Karuranga P, Lemarchand C, Marcotullio E, Guizard AV, Monnereau A, Baldi I, Lebailly P. Occupational exposure to pesticides and multiple myeloma in the AGRICAN cohort. CCC. 2019;30:1243–1250. doi: 10.1007/s10552-019-01230-x. [DOI] [PubMed] [Google Scholar]
- Vale RL, Netto AM, Toríbio LXB, Lâvor MPB, Siqueira JPS. Assessment of the gray water footprint of the pesticide mixture in a soil cultivated with sugarcane in the northern area of the State of Pernambuco, Brazil. J Clean pro. 2019;234:925–932. doi: 10.1016/j.jclepro.2019.06.282. [DOI] [Google Scholar]
- Vindas R, Ortiz F, Ramírez V, Cuenca P. Genotoxicidad de tres plaguicidas utilizados en la actividad bananera de Costa Rica. Rev Biol Trop. 2004;52:601–609. [PubMed] [Google Scholar]
- VoPham, et al. Pesticides exposures and liver cancer: a review. CCC. 2017;28:177–190. doi: 10.1007/s10552-017-0854-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waggoner JK, Kullman GJ, Henneberger PK, Umbach DM, Blair A, Alavanja MC, Kamel F, Lynch CF, Knott C, London SJ, Hines CJ, Thomas KW, Sandler DP, Lubin JH, Freeman LE, Hoppin JA. Mortality in the agricultural health study, 1993–2007. Am J Epidemiol. 2011;173:71–83. doi: 10.1093/aje/kwq323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ye M, Beach J, Martin JW, Senthilselvan A (2017) Pesticide exposures and respiratory health in general populations. Journal of Environmental Sciences (China). Chin Acad Sci. 10.1016/j.jes.2016.11.012 [DOI] [PubMed]
- Zakerinia M, Namdari M, Amirghofran S. The relationship between exposure to pesticides and the occurrence of lymphoid neoplasm. Iran Red Crescent Med J. 2012;14:337. [PMC free article] [PubMed] [Google Scholar]
- Zheng W, Luo B, Hu X (2020) The determinants of farmers’ fertilizers and pesticide use behavior in China: An explanation based on label effect. J Clean Prod 272 10.1016/j.jclepro.2020.123054
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed in the present study are available from the corresponding author on reasonable request.