Abstract
Background:
The oral squamous cell carcinoma (OSCC) often affects elderly aged adults, who had long-term tobacco exposure. In the recent past decade, there is an increasing incidence of OSCC in younger individuals, who had less tobacco association.
Aim:
The aim of this study is to examine the risk factors and to assess and compare the clinicopathological features and prognosis of OSCC in young patients with the older group patients.
Materials and Methods:
We included studies that addressed the OSCC involving young patients during the period between 2014 and 2019. Initially, we found 679 articles; after refined evaluation, 92 works had their titles matching to the present work. After extraction of case reports, reviews, and studies with un-matched objectives or inadequate data, we have chosen only 24 presentations matching to the abstract. The statistical analysis performed by Chi-square tests using SPSS 20.0 version for windows.
Results:
Of the total OSCC, 10% of patients belonged to the younger age group, and 90% were the older aged group. Both the groups showed male gender predominance and tongue as the predominant site of involvement. The younger patients tend to have significantly reduced tobacco exposure. The highly reported tumors were advanced staged and moderately differentiated tumors in both groups. There was a statistically evident high recurrence reported in the younger group. The overall survival seems to be similar for both groups.
Conclusion:
The identification of the potential risk factors, along with unique molecular mechanisms, and biological behavior of the disease is mandatory to control the incidence of OSCC in young adults.
Keywords: Oral cancer, oral squamous cell carcinoma, younger adults
Introduction
Oral cancer is a chief public health concern with the incidence of approximately 350,000 cases annually worldwide.[1] Histologically, over 90% of oral cancers are squamous cell carcinomas.[2] Oral squamous cell carcinoma (OSCC) usually affects patients in the sixth to eighth decades of life and reported with a male predilection. The rising trend of the development of OSCC in younger patients is observed in recent literature worldwide. The estimation of the increased incidence of the disease in young patients was 5%–16.5%.[3]
Materials and Methods
Database searches
Step 1: Electronic search identification
We searched the electronic databases, which include PubMed, Scopus, and Medline, for previously published articles that addressed the OSCC involving young patients between 2014 and 2019. We selected works only in English, using the following keywords, “oral squamous cell carcinoma,” “young patients,” and “patients under 45 years.”
Step 2: Screening for relevance
We identified the articles that discussed OSCC in young patients. We shortlisted the titles and abstracts of all the collected materials for the screening of relevance and duplication.
Step 3: The articles excluded for the following reasons
Articles with unmatched objective and abstract
Being case reports; literature reviews; systematic reviews.
Step 4: We retrieved full-text articles for the selected papers
We independently assessed all the presentations against the following essential criteria selection bias, missing data, specification of data, selective reporting of analyses or outcomes, imprecision (e.g., small sample size), incomplete outcome data or attrition bias, baseline confounding, other measures of quality (e.g., ethics approval, funding, and conflicts of interest statement) and limitations. After assessing all the elements, we have considered the articles for eligibility criteria. We have excluded the works with inadequate data, which limits the comparison between groups.
Step 5: We included the studies if they met the following inclusion criteria
Studies reported OSCC incidence data in young age group
Papers revealed clinical and histopathological characteristics of OSCC involving young patients and old patients
Studies expressed follow up details
Papers provided sufficient data to allow comparison of younger and older age groups.
From the methodology used, we retrieved 679 articles. After search refinement, 580 articles had unmatched titles with seven duplicated data reports. After extraction of these articles, 92 articles had their titles relevant to our work. We excluded the articles with un-matched objectives (n = 37), systematic reviews (n = 2), reviews (n = 9), and case reports (n = 5). We recovered full-text articles for the 39 articles with matching objectives. In the refined evaluation, we excepted the articles had not provided adequate data for the older age group (n = 15). Therefore, we included only 24 articles matching the abstract of the present work [Figure 1].
Figure 1.
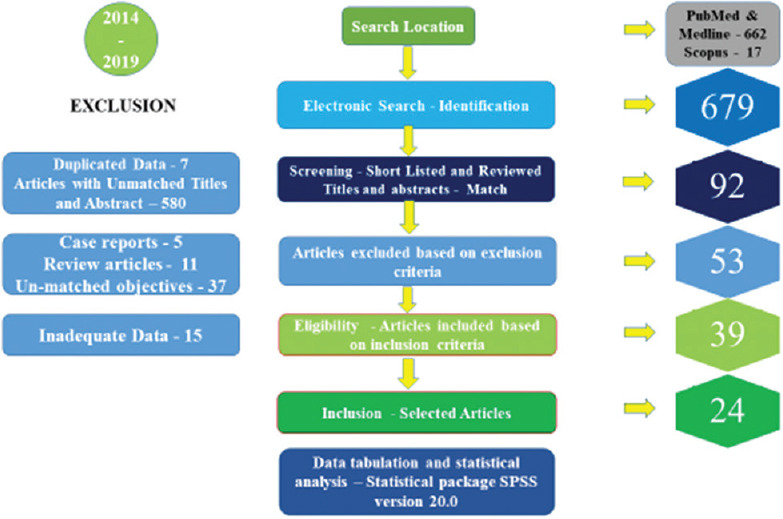
Diagram of the study selection
Data extraction
The extracted data from full-text articles were, author, country, publication year, age groups, sample size, sex, sites, tobacco exposure, TNM staging, histopathological grading, recurrence, and (2–5 years) overall survival rate. We tabulated all the collected data separately for the younger and older group patients in a specified format. The statistical analysis performed by Chi-square tests using SPSS 20.0 version for windows (IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp).
Results
The analysis of the preceding, published case series reveals several notable differences in their methodology. These studies often utilized different age thresholds for defining “young.” Age distribution of patients in the presented articles varied, individuals considered young, were those aged ≤30 years (0.8%),[3] ≤40 years (90%),[4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20] and ≤45 years (6.7%).[21,22,23,24,25] The majority of the studies (nearly 17 studies) classified individuals under 40 years as young. One research denoted aged <50 years as the young group (2.5%).[26]
We tabulated the available data regarding clinical and histopathological grading for the younger and older group patients distinctly in a specified format [Tables 1 and 2].
Table 1.
Clinical and histopathological grade for the younger group
| Authors | Total OSCC (n) | Young cases (n) | Male/female (n) | Site -tongue (n) | Other sites (n) | Tobacco users (n) | HPG WD (n) | HPG MD (n) | HPG PD (n) |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al.[3] | 263 | 36 | 17/19 | 36 | 0 | 3 | - | - | 6 |
| Fang et al.[4] | 176 | 15 | 6/9 | 15 | 0 | 5 | 6 | 4 | 5 |
| Khammissa et al.[5] | 537 | 36 | 21/11 | 11 | 25 | - | 3 | 30 | 3 |
| Troeltzsch et al.[6] | 45 | 11 | 6/5 | 7 | 4 | 1 | 0 | 10 | 1 |
| Sun et al.[7] | 430 | 31 | 19/12 | 15 | 16 | 14 | 14 | 8 | 9 |
| Naz et al.[8] | 87 | 19 | - | 5 | 14 | - | 4 | 13 | 1 |
| Komolmalai et al.[9] | 874 | 36 | 23/13 | 27 | 9 | 23 | 18 | 11 | 5 |
| Frare et al.[10] | 28 | 14 | 12/2 | 11 | 3 | 10 | 3 | 10 | 1 |
| Blanchard et al.[11] | 100 | 50 | 39/11 | 50 | 0 | 27 | 40 | 9 | 1 |
| Jeon et al.[12] | 117 | 23 | 15/8 | 23 | 0 | 12 | 10 | 6 | 6 |
| Kapila et al.[13] | 40 | 21 | 18/3 | - | - | 13 | 1 | 13 | 7 |
| Mahmood et al.[14] | 115 | 40 | 33/7 | 7 | 33 | - | 5 | 24 | 11 |
| Mukdad et al.[15] | 16423 | 1232 | 706/526 | 1232 | 0 | - | 308 | 588 | 203 |
| Xu et al.[16] | 2782 | 174 | 109/65 | 120 | 54 | 68 | 60 | 88 | 12 |
| Costa et al.[17] | 60 | 21 | 14/7 | 11 | 10 | 17 | 13 | 3 | 5 |
| Oliver et al.[18] | 22930 | 2266 | 1211/1055 | 2266 | 0 | - | 384 | 823 | 256 |
| Teixeira et al.[19] | 57 | 17 | 14/3 | 10 | 7 | 14 | 4 | 12 | 1 |
| Zhang et al.[20] | 206 | 103 | 53/50 | 53 | 50 | 10 | 47 | 43 | 13 |
| Goepfert et al.[21] | 54 | 18 | 0/18 | 18 | 0 | 9 | 6 | 7 | 5 |
| Cariati et al.[22] | 133 | 33 | 18/15 | 18 | 15 | 16 | 13 | 17 | 3 |
| Abdulla et al.[23] | 420 | 86 | 53/33 | 25 | 59 | 67 | 30 | 40 | 4 |
| Farquhar et al.[24] | 397 | 117 | 58/59 | 117 | 0 | 56 | - | - | - |
| Choi et al.[25] | 189 | 51 | 26/25 | 51 | 0 | 21 | 18 | 21 | 12 |
| Campbell et al.[26] | 395 | 113 | 67/46 | 113 | 0 | 61 | 25 | 64 | 13 |
NS: Not specified; -: Data not available; HPG: Histopathological grade; WD: Well differentiated; MD: Moderately differentiated; PD: Poorly differentiated
Table 2.
Clinical and histopathological grade details for the older group
| Authors | Old cases (n) | Male (n) | Female (n) | Site -tongue (n) | Other site total (n) | Tobacco users (n) | HPG WD (n) | HPG MD (n) | HPG PD (n) |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al.[3] | 227 | 117 | 110 | 227 | 0 | 85 | - | - | 13 |
| Fang et al.[4] | 161 | 113 | 48 | 161 | 0 | 109 | 85 | 36 | 40 |
| Khammissa et al.[5] | 501 | 352 | 112 | 187 | 314 | - | 29 | 398 | 74 |
| Troeltzsch et al.[6] | 34 | 23 | 11 | 4 | 30 | 11 | 2 | 27 | 5 |
| Sun et al.[7] | 399 | 277 | 122 | 161 | 238 | 252 | 204 | 104 | 91 |
| Naz et al.[8] | 68 | - | - | 17 | 51 | - | 20 | 36 | 12 |
| Komalmalai et al.[9] | 838 | 494 | 344 | 309 | 529 | 502 | 487 | 235 | 62 |
| Frare et al.[10] | 14 | 11 | 3 | 9 | 5 | 8 | 2 | 11 | 1 |
| Blanchard et al.[11] | 50 | 39 | 11 | 50 | 0 | 46 | 40 | 9 | 1 |
| Jeon et al.[12] | 94 | 51 | 43 | 94 | 0 | 41 | 59 | 27 | 5 |
| Kapila et al.[13] | 19 | 14 | 5 | - | - | 11 | 3 | 12 | 4 |
| Mahmood et al.[14] | 75 | 49 | 26 | 13 | 62 | - | 12 | 56 | 7 |
| Mukdad et al.[15] | 15191 | 8895 | 6296 | 15191 | 0 | - | 3823 | 7123 | 2186 |
| Xu et al.[16] | 2608 | 2379 | 229 | 1039 | 1568 | 1060 | 1126 | 1240 | 124 |
| Costa et al.[17] | 39 | 30 | 9 | 22 | 17 | 31 | 23 | 14 | 2 |
| Oliver et al.[18] | 20664 | 12502 | 8162 | 20664 | 0 | - | 366 | 850 | 248 |
| Teixeira et al.[19] | 40 | 35 | 5 | 14 | 26 | 36 | 13 | 23 | 4 |
| Zhang et al.[20] | 103 | 53 | 50 | 53 | 50 | 10 | 40 | 52 | 11 |
| Goepfert et al.[21] | 36 | 25 | 11 | 36 | 0 | 20 | 11 | 18 | 7 |
| Cariati et al.[22] | 100 | 66 | 34 | 35 | 65 | 87 | 8 | 66 | 26 |
| Abdulla et al.[23] | 334 | 213 | 109 | 42 | 258 | 220 | 128 | 130 | 18 |
| Farquhar et al.[24] | 280 | 169 | 110 | 280 | 0 | 192 | - | - | - |
| Choi et al.[25] | 138 | 87 | 51 | 138 | 0 | 48 | 71 | 54 | 13 |
| Campbell et al.[26] | 282 | 171 | 111 | 282 | 0 | 192 | 58 | 166 | 33 |
NS: Not specified; -: Data not available; HPG: Histopathological grade; WD: Well differentiated; MD: Moderately differentiated; PD: Poorly differentiated
The TNM staging of the tumors, along with the follow-up details for the selected group, was also presented separately [Tables 3 and 4].
Table 3.
Clinical stage and patient’s follow-up details for the younger group
| Authors | Young cases (n) | Stage I + II (n) | Stage III + IV (n) | Stage NS (n) | Recurrences (n) | Recurrence NS (n) | Overall survival (n) | Overall survival NS (n) |
|---|---|---|---|---|---|---|---|---|
| Zhang et al.[3] | 36 | 17 | 17 | 2 | 12 | 0 | 1 | 24 |
| Fang et al.[4] | 15 | - | - | 15 | 10 | 0 | 10 | 0 |
| Sun et al.[7] | 31 | - | - | 31 | 17 | 0 | 22 | 0 |
| Komalmalai et al.[9] | 36 | 14 | 14 | 8 | - | 36 | 20 | 0 |
| Frare et al.[10] | 14 | 9 | 5 | 0 | 8 | 0 | 7 | 0 |
| Blanchard et al.[11] | 50 | 29 | 21 | 0 | 16 | 0 | 39 | 0 |
| Jeon et al.[12] | 23 | 9 | 14 | 0 | 13 | 0 | 10 | 0 |
| Mahmood et al.[14] | 40 | 2 | 38 | 0 | - | 40 | - | 40 |
| Mukdad et al.[15] | 1232 | 316 | 191 | 725 | - | 1232 | 875 | 0 |
| Xu et al.[16] | 174 | - | - | 174 | 49 | 14 | 130 | 14 |
| Costa et al.[17] | 21 | 3 | 18 | 0 | - | 21 | - | 21 |
| Oliver et al.[18] | 2266 | 1225 | 515 | 526 | - | 2266 | 1804 | 0 |
| Teixeira et al.[19] | 17 | 3 | 6 | 8 | - | 17 | - | 17 |
| Zhang et al.[20] | 103 | 66 | 37 | 0 | 18 | 0 | 88 | 0 |
| Goepfert et al.[21] | 18 | 9 | 9 | 0 | 7 | 0 | 13 | 0 |
| Cariati et al.[22] | 33 | - | - | 33 | - | 33 | 16 | 0 |
| Abdulla et al.[23] | 86 | 5 | 32 | 49 | - | 86 | - | 86 |
| Farquhar et al.[24] | 117 | - | - | 117 | 24 | 61 | 48 | 61 |
| Choi et al.[25] | 51 | - | - | 51 | 20 | 0 | 31 | 0 |
| Campbell et al.[26] | 113 | 66 | 36 | 11 | 40 | 11 | 86 | 0 |
NS: Not specified; -: Data not available
Table 4.
Clinical stage and patient’s follow-up details for the older group
| Authors | Old cases (n) | Stage I + II (n) | Stage III + IV (n) | Stage NS (n) | Recurrences (n) | Recurrence NS (n) | Overall survival (n) | Over survival NS (n) |
|---|---|---|---|---|---|---|---|---|
| Zhang et al.[3] | 227 | 142 | 75 | 10 | 88 | 0 | 21 | 139 |
| Fang et al.[4] | 161 | - | - | 161 | 70 | 0 | 117 | 0 |
| Sun et al.[7] | 399 | - | - | 399 | 186 | 0 | 285 | 0 |
| Komalmalai et al.[9] | 838 | 252 | 411 | 175 | - | 838 | 231 | 0 |
| Frare et al.[10] | 14 | 9 | 5 | 0 | 2 | 0 | 7 | 0 |
| Blanchard et al.[11] | 50 | 29 | 21 | 0 | 17 | 0 | 27 | 0 |
| Jeon et al.[12] | 94 | 57 | 37 | 0 | 24 | 0 | 66 | 0 |
| Mahmood et al.[14] | 75 | 8 | 67 | 0 | - | 75 | - | 75 |
| Mukdad et al.[15] | 15191 | 4215 | 2244 | 8732 | - | 15191 | 7747 | 0 |
| Xu et al.[16] | 2608 | - | - | 2608 | 1009 | 286 | 1663 | 286 |
| Costa et al.[17] | 39 | 11 | 28 | 0 | - | 39 | - | 39 |
| Oliver et al.[18] | 20664 | 11529 | 4342 | 4793 | - | 20664 | 14361 | 0 |
| Teixeira et al.[19] | 40 | 4 | 25 | 11 | - | 40 | - | 40 |
| Zhang et al.[20] | 103 | 66 | 37 | 0 | 34 | 0 | 73 | 0 |
| Goepfert et al.[21] | 36 | 19 | 17 | 0 | 9 | 0 | 26 | 0 |
| Cariati et al.[22] | 100 | - | - | 100 | - | 100 | 62 | 0 |
| Abdulla et al.[23] | 334 | 18 | 164 | 152 | - | 334 | - | 334 |
| Farquhar et al.[24] | 280 | - | - | 280 | 8 | 224 | 47 | 224 |
| Choi et al.[25] | 138 | - | - | 138 | 43 | 0 | 72 | 0 |
| Campbell et al.[26] | 282 | 169 | 91 | 22 | 96 | 22 | 200 | 0 |
NS: Not specified; -: Data not available
As for the sample size consideration, the young group displayed between 11 and 2266 patients, whereas the older group presented with 14–20664 patients.
Regarding the country of study, China carried out five works,[3,4,7,16,20] followed by the United States (four works),[15,21,24,26] Brazil (three works),[10,17,19] Pakistan, India, and Korea (two works).[8,12,13,14,23,25] The remaining works were single reported studies in various countries.[5,6,9,11,18,22]
The prevalence of oral cancer in young and old
Out of published series comparing OSCC in young and old group patients, a total record of OSCC was 46,858, during the period between 2014 and 2019. Of the total OSCC, 42295 (90.3%) were older age group, and 4563 (9.7%) patients belonged to the younger age group.
Gender distribution of oral cancer in young and old group patients
The present work showed that there were 2538 (56%) male and 2002 (44%) female patients in the younger group. The observed male-to-female ratio was 1.5:1 in the younger group. In the older age group, there were 26165 (62%) male and 16012 (38%) female patients. The detected male-to-female ratio was 1.7:1 in the older group. Gender details were not known for 23 younger and 118 older patients. Although both the groups showed male predominance, a higher number of female patients were recorded in the younger group (44%) when compared to the older group (38%). The gender distribution was not statistically significant between the selected groups (P > 0.05).
Site distribution for oral cancer in young and old group patients
Ten studies used only lesions in the tongue (TSCC) as inclusion criteria. One of the articles had not mentioned the site specification details.[13] Both the groups showed tongue as the predominant site of involvement than the other sites. The average percentage of the tongue lesions was 72% in the young group, while it was 64% in the older group. The exact location was not known for 23 younger and 54 older group patients. Though the trend line for tongue carcinoma showed a higher level in the younger group when compared to the older group, no statistically significant difference was observed in tumor location (P > 0.05) [Graph 1].
Graph 1.
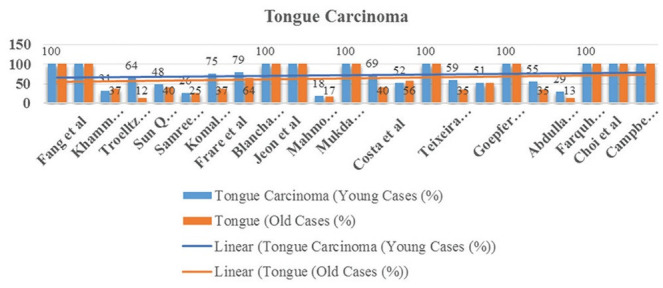
Tongue carcinomas in younger and older groups
Risk factor assessment
Traditional habit history was not known for 3601 younger and 36,598 older patients. An average of 48% of patients had tobacco exposure in the younger group, while it was 59% in the older group. The proportion of tobacco exposure was less in young patients. The difference was statistically significant in the present study (P < 0.05) [Graph 2].
Graph 2.
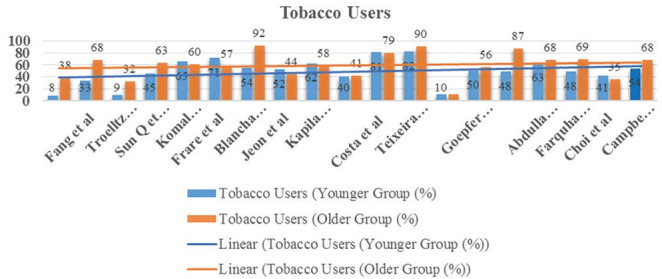
Tobacco users in younger and older groups
Clinical stage
The clinical-stage at diagnosis in accord with the UICC TNM system was unavailable for 40% (n = 1837) and 43% (n = 18203) of younger and older patients, respectively. Both groups showed the predominance of advanced-stage tumors (Stage III + IV) at the time of presentation. There was an average of 54%, and 52% of advanced tumors and 46% and 48% of early-stage tumors reported in the younger and older group, respectively. In the present study, there was no statistically significant difference in the clinical-stage distribution of the selected groups (P > 0.05) [Graph 3].
Graph 3.
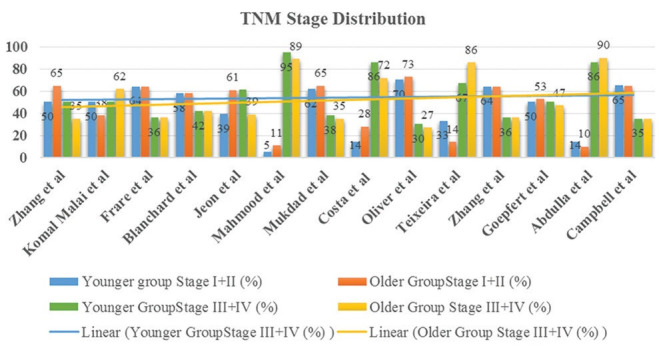
TNM stage distribution in younger and older groups
Histopathological grade distribution
The majority of the patients had moderately differentiated tumors, which was followed by well-differentiated tumors in both groups. None of the studies had found the poorly differentiated tumor predominance. The histopathological grading details were unknown for 25% (n = 1124) of younger patients and 52% (n = 22011) of older group patients. The younger group showed an average of 50% moderately differentiated tumors, 33% well-differentiated, and 17% poorly-differentiated tumors. The older group reported with 51% of moderately differentiated tumors, 36% of well-differentiated tumors, and 13% of poorly differentiated tumors. The younger patients tend to have a higher number of poorly differentiated tumors compared to the older group. The histopathological grade distribution difference was not statistically significant in the selected age groups (P > 0.05) [Graph 4].
Graph 4.
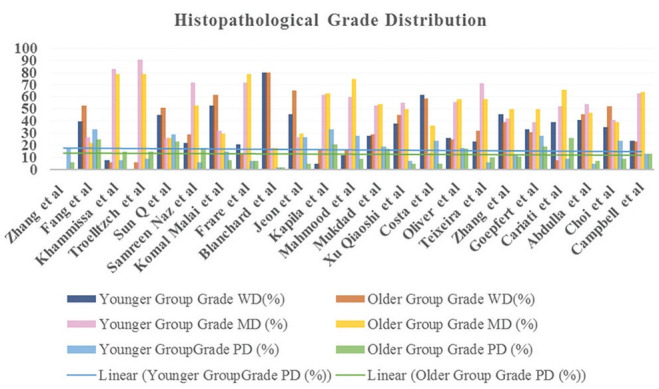
Histopathological grade distribution in younger and older groups
Recurrence
The average recurrence was 42% for the younger group, while the older group patients experienced 32% of recurrence. The data regarding recurrence after the treatment was unavailable for 86% (n = 3904) and 91% (n = 38435) of younger patients and older patients, respectively. The recurrence percentage was higher in the younger group compared to the older group. There was a significant age-specific difference in the recurrence rate (P < 0.05) [Graph 5].
Graph 5.
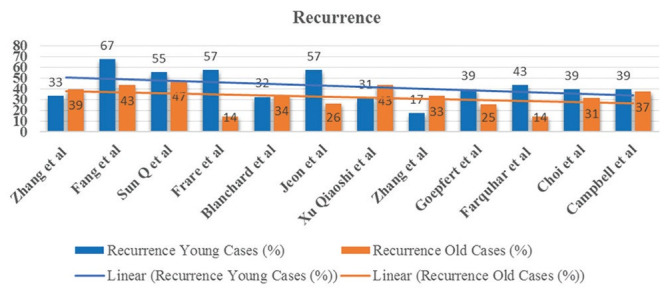
Recurrences in younger and older group
Overall survival
The average percentage of two to five years overall survival for the younger group was 65%, while it was 62% for the older group. The data regarding the survival period after the therapy was unavailable for 8% (n = 350) and 4% (n = 1759) of younger and older patients, respectively. There was no evidence of a significant association between overall survival and selected age groups (P > 0.05) [Graph 6].
Graph 6.
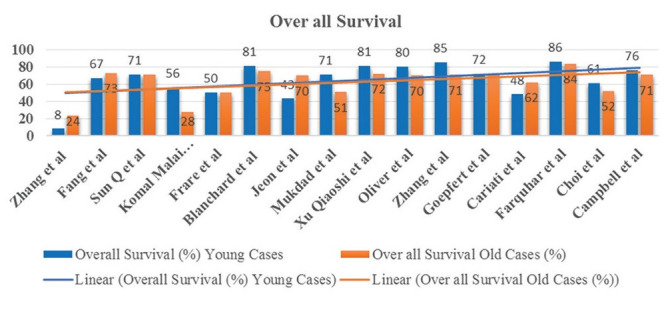
Overall survival in younger and older groups
The younger group hazard ratio with a 95% confidence interval with reference to the older age group was available in only six of the published studies. The available data showed a lower risk for the younger group [Graph 7].
Graph 7.
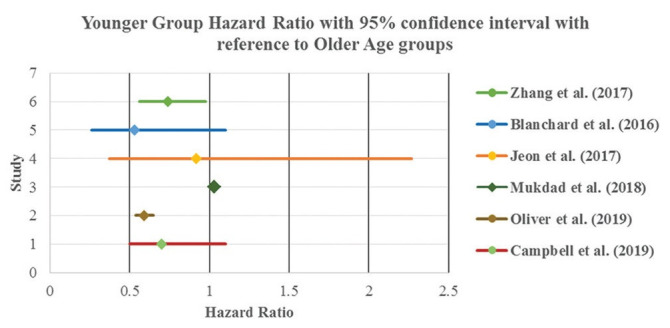
Age as a prognostic factor for overall survival
Discussion
Recent literature showed a rising worldwide incidence of OSCC in individuals younger than 40 years.[3] The evidence displayed that many younger patients have a different etiological association for the progression of cancer. There is no consensus, and controversy still exists, especially oral cancer in young nontobacco users, whether the different etiology results in characteristic clinical and progressive behavior or as similar to for older patients.[23] Hence, the present work had an objective to conduct a comparative analysis on the clinicopathological aspects and the prognosis of OSCC in young patients with the older group patients to provide more in-depth knowledge of the disease at the younger population.
There was inevitable heterogeneity in cut off age employed to classify individuals as young in the selected studies, and it restricts comparative analysis between groups. However, the majority of the studies arbitrarily considered individuals under 40 as young (90%) as the unique group of OSCC.[4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20]
In attention to gender distribution, one article had not provided the details.[8] In general, OSCC occurs more frequently in males belonging to the older age group. The present work corroborates with the literature in 23 of the published studies of OSCC in the older age group and nearly 19 of the published studies in the younger group in male gender predominance.[5,6,7,9,10,11,12,13,14,15,16,17,18,19,20,22,23,25,26]
The young women reported with a higher incidence in three studies.[3,4,24] One study group only comprised of female patients.[21] The attributed difference in gender predilection toward female patients could be due to other etiological factors, such as passive smoking and the presence of various cultural or behavioral characteristics in the diverse group of different populations.[27]
Analysis based on localization revealed nearly nine studies found tongue lesions about 48%–79% amongst the intraoral SCC, especially in younger individuals.[6,7,9,10,16,17,19,20,22] In the young population, the next most frequent site predilection is gingiva[7] or buccal mucosa.[23] One study depicted that the floor of the mouth representing the second-most affected region in the young group.[22] On the contrary, OSCC of the floor of the mouth occurred significantly less frequently (6%) in the younger group in one presentation.[5] The older group showed tongue as the predominant site of involvement in three studies.[10,17,20] Ten of the selected studies included only TSCC patients.[3,4,11,12,15,18,21,24,25,26]
Although the individual reports stated different opinions regarding site predilection, the present work showed tongue as the predominant site of involvement than the other sites in both groups. The discrepancy in results about the anatomical site may happen due to the cut off age, site selection criteria, sample size selection in the studied population. The trend line for tongue carcinoma showed an elevated level in the younger group, but there was no statistically significant difference in tumor location in the selected groups (P > 0.05).
Concerning the relationship with harmful habits, nineteen investigations demonstrated an association between tobacco use and OSCC, of which 13 presentations showed >50% of positive association with tobacco use in the older group.[4,7,9,10,11,13,17,19,21,22,23,24,26] One of the previous works also supported the fact, i.e., nearly 70% were tobacco users in the older group affected by SCC.[27]
Many studies had observed that OSCC in the younger cohort had significantly less association with tobacco.[3,4,6,7,16,20,21,22,24,25] One of the previous studies expressed the fact that the absence of these traditional risk factors among young tongue carcinoma patients had been noted globally in many countries, such as the US, UK, KSA, China, India, and Brazil. The study also stated that >50% of the patients were nonsmokers and nondrinkers in the younger group patients.[27] Only three presentations displayed 70%–80% of younger patients had a history of tobacco exposure.[10,17,19] One study pointed out that the occurrence of OSCC equally distributed between tobacco users and nonusers of the younger group.[21] Besides, authors had also found that the female cohort of younger patients was significantly abstain from the use of tobacco.[3,4,24,25] The remaining five works did not assess the parameter related to harmful habits in both groups.[5,8,14,15,18]
In a few studies, there was smokeless tobacco use predominance reported in the pathogenesis of OSCC in the younger group.[13,26] The other presentation depicted that increased consumption of pan when compared to betel nut usage in the younger cohort of the South Indian population.[23]
In the present study, an average of 48% of younger patients and 59% of older patients had tobacco exposure for carcinogenesis. The traditional risk factor association was less in young patients; the difference was statistically significant in the present study (P < 0.05).
Other influencing factors such as chromosomal fragility, and DNA ploidy abnormalities frequently alter the genetic sensitivity to environmental carcinogens, should also be considered especially in nonsmoking young patients with oral cancer.[13]
There was also a significant familial risk association (20%) in the development of early-onset OSCC. The diagnosed cancer in younger group mandates for considerable attention on genetic expression profiling, and pan-genome studies to explore the pathogenesis responsible for the onset of complex disease at an earlier age.[14]
One of the previous studies had reported that human papillomavirus (HPV) infection was also a significant risk factor for OSCC, especially in a young population.[28] Only limited archival information are available on HPV status, since many hospitals do not perform assays to assess HPV infection on a routine basis. Few authors did not identify HPV colonization as an age-related risk factor for OSCC in young patients.[6,26] Additional studies are required to confirm HPV influence in OSCC of younger adults.
To concise, OSCC in the younger population showed a complex etiological association. The other factors, such as syndromes, Fanconi anemia, trauma, sharp teeth, stress, hormone/immune modulation, environmental carcinogens, malnutrition, lifestyle, and dietary patterns, should also be considered in the younger population.[27]
UICC TNM is an international system for clinical staging of cancer that measures three parameters such as, tumor size (T), presence of metastasis in cervical lymph nodes (N), presence, or absence of distance metastasis (M). Literature shows conflicting reports regarding features such as nodal and distant metastasis. Nearly ten works had not discussed the clinical stages of the tumor at the time of presentation.[4,5,6,7,8,13,16,22,24,25] Three presentations stating that there was an equal distribution of early and advanced stage tumors in the younger group.[3,9,21] Three articles highlighted the observation of a similar distribution pattern of early and advanced stage tumors in both groups.[11,20,26] Three studies depicted that young cancer patients had a higher rate of nodal metastasis when compared to the older group.[12,13,22] Conversely, the younger group patients showed a decreased rate of metastasis in two presentations.[4,7]
In the analyzed studies, advanced stage tumors (stage III and stage IV) were the most frequent presentation in both young and old group of patients, with an average percentage of 54% and 52%, respectively. The little rise of advanced tumors in the young group may be due to delay in consultation or late diagnosis since the expectation of OSCC was not as much in nonsmoker of the younger group in general. However, the clinical-stage distribution difference was not statistically significant in the selected groups (P > 0.05).
The malignant tumor grading system proposed by the World Health Organization (2005) evaluates the degree of cellular differentiation, grouping tumors into well, moderately, and poorly differentiated. It is unknown whether the degree of tumor differentiation could signify a prognostic marker for young patients or not.[22] In the present study, out of the 24 articles, two had not presented data about the differentiation of the lesion.[3,24] Fourteen of the remaining works reported that the majority of the patients had moderately differentiated tumors in both groups.[5,6,8,10,13,14,15,16,18,19,21,22,23,26] Conversely, six reports depicted that the majority of the tumors were well-differentiated in both groups.[4,7,9,11,12,17] Irrespective of the age groups, none of the studies had found the poorly differentiated tumor predominance. However, many authors had found younger patients tend to have a more proportion of poorly differentiated tumors.[3,4,7,9,12,17,21,25] The previous statement was conflicted by five reports, which specified that there was a nearly equal distribution of poorly differentiated tumors in both groups.[10,11,18,20,26]
The pathological comparison depicted that an average of 50%–51% of the tumors was moderately differentiated. The next frequently presented tumors were well differentiated in both groups. There was no significant difference in histopathological grade distribution in the studied groups (P > 0.05).
OSCC in young patients displayed a different pattern of recurrence and biological behavior.[13] Twelve articles had not specified the recurrence data.[3,4,7,10,11,12,16,20,21,24,25,26] Nearly eight studies experienced a higher recurrence rate in the younger group.[4,7,10,12,21,24,25,26] Two presentations depicted that the young patients tended to higher death rate due to increased recurrences.[3,4] On the contrary, the remaining four presentations stated a higher recurrence rate observed in the older group.[3,11,16,20]
The present work showed an average of 42% of recurrence in the younger group, while the older group patients experienced 32% of recurrence. The recurrence percentage was higher in the younger group, and there was a significant age-specific difference in the recurrence rate (P < 0.05). The elevated recurrence rate in younger adults could be attributable due to unidentified or complexed etiology.
Regarding overall survival percentage, 2–5 years overall survival rate was not mentioned in sixteen of the reported presentations.[3,4,7,9,10,11,12,15,16,18,20,21,22,24,25,26] Despite the increased recurrence, there was no significant difference in overall survival between young and older patients in four of the presentations.[7,10,21,24] Four studies pointed out that reduced overall survival in the younger group.[3,4,12,22] On the contrary, few other reports had depicted that the overall survival and prognosis among the young was better than that of old patients.[9,11,15,16,18,20,25,26] The present work showed an average percentage of overall survival was 65% for the younger group, while it was 62% for the older group. There was a milder improvement in the overall survival of younger patients attributed due to reduced tobacco exposure and better palliative care over recent years. The difference in overall survival was nonsignificant in the specified groups (P > 0.05).
Inferences
There is still no consensus, especially as to the etiopathogenesis of cancer in non– tobacco users, a subset of young patients. The present study showed an elevated recurrence rate in younger adults. The overall survival percentage seems to be similar for both the group of patients, despite the young patients, displayed reduced history of tobacco exposure and presented with enhanced immunity when compared to older group patients.
Limitations
The review is limited because of a few smaller sample size presentations and the various inherent biases of a retrospective study, because the data from many of the selected articles had taken from histopathological records of a single hospital. Due to the lack of availability of archives, there were missing pieces of information that had limited the valid comparison. Few studies had not separated the effects of two associated exposures (e.g., smoking and alcohol consumption) and selected a specific site for comparison. The confounders such as baseline functional status and underlying comorbidities had not addressed due to missing data in retrospective records, which could be a causative factor affecting the survival of the patients in both the groups. Finally, there was heterogeneity in the age group selection criteria and length of follow-up duration, due to a lack of uniformly annotated presentation in retrospective records. These limitations should be given further consideration in future studies.
Despite such limitations, we have acted appropriately to minimize bias due to heterogeneity, missing data, and confounders. We presented the aggregate knowledge from the selected articles with P value to control multiple factors and reduce sources of error and bias as much as possible. We are moderately confident in the precision and consistency of the summary of findings. The present work is valuable in providing insight into the clinical, histological, and general outcomes of oral carcinomas occurring in young patients. Since the current knowledge regarding the characteristics of SCC in young people is limited, the findings of the present work will serve as add on to the existing literature.
The present study emphasizes the need for multicenter prospective studies with restriction of age limit and a complete systematic and methodical presentation of patient data using electronic databases for meaningful comparison of OSCC between young and older individuals.
Conclusion
The expected increase in the incidence of OSCC in the younger group may become a significant public health concern shortly if the current trend persists. Further research in this field, will be of higher value to unveil the differences in risk factors, genetic influence, unique molecular pathogenesis, and predictable biomarkers of prognosis of the disease in the younger population.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I sincerely thank Mr. Syed Imran Maktoum, Director, Kalbani Group, for his support towards this present article.
References
- 1.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 2.Sloan P, Gale N, Hunter K, Lingen M, Nylander K, Reibel J, et al. Tumours of the oral cavity and mobile tongue: Malignant surface epithelial tumors: Squamous cell carcinoma. In: El-Naggar AK, Chan JKC, Grandis JR, Takata T, Slootweg PJ, editors. WHO Classification of Head and Neck Tumours. 4th ed. Lyon, France: IARC Press; 2017. pp. 108–9. [Google Scholar]
- 3.Zhang YY, Wang DC, Su JZ, Jia LF, Peng X, Yu GY. Clinicopathological characteristics and outcomes of squamous cell carcinoma of the tongue in different age groups. Head Neck. 2017;39:2276–82. doi: 10.1002/hed.24898. [DOI] [PubMed] [Google Scholar]
- 4.Fang QG, Shi S, Liu FY, Sun CF. Tongue squamous cell carcinoma as a possible distinct entity in patients under 40 years old. Oncol Lett. 2014;7:2099–102. doi: 10.3892/ol.2014.2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Khammissa RA, Meer S, Lemmer J, Feller L. Oral squamous cell carcinoma in a South African sample: Race/ethnicity, age, gender, and degree of histopathological differentiation. J Cancer Res Ther. 2014;10:908–14. doi: 10.4103/0973-1482.138100. [DOI] [PubMed] [Google Scholar]
- 6.Troeltzsch M, Knösel T, Eichinger C, Probst F, Troeltzsch M, Woodlock T, et al. Clinicopathologic features of oral squamous cell carcinoma: Do they vary in different age groups? J Oral Maxillofac Surg. 2014;72:1291–300. doi: 10.1016/j.joms.2014.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Sun Q, Fang Q, Guo S. A comparison of oral squamous cell carcinoma between young and old patients in a single medical center in China. Int J Clin Exp Med. 2015;8:12418–23. [PMC free article] [PubMed] [Google Scholar]
- 8.Naz S, Salah K, Khurshid A, Hashmi AA, Faridi N. Head and neck squamous cell carcinoma-Comparative evaluation of pathological parameters in young and old patients. Asian Pac J Cancer Prev. 2015;16:4061–3. doi: 10.7314/apjcp.2015.16.9.4061. [DOI] [PubMed] [Google Scholar]
- 9.Komolmalai N, Chuachamsai S, Tantiwipawin S, Dejsuvan S, Buhngamongkol P, Wongvised C, et al. Ten-year analysis of oral cancer focusing on young people in northern Thailand. J Oral Sci. 2015;57:327–34. doi: 10.2334/josnusd.57.327. [DOI] [PubMed] [Google Scholar]
- 10.Frare JC, Sawazaki-Calone I, Ayroza-Rangel AL, Bueno AG, de Morais CF, Nagai HM, et al. Histopathological grading systems analysis of oral squamous cell carcinomas of young patients. Med Oral Patol Oral Cir Bucal. 2016;21:e285–98. doi: 10.4317/medoral.20953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blanchard P, Belkhir F, Temam S, El Khoury C, De Felice F, Casiraghi O, et al. Outcomes and prognostic factors for squamous cell carcinoma of the oral tongue in young adults: A single-institution case-matched analysis. Eur Arch Otorhinolaryngol. 2017;274:1683–90. doi: 10.1007/s00405-016-4419-1. [DOI] [PubMed] [Google Scholar]
- 12.Jeon JH, Kim MG, Park JY, Lee JH, Kim MJ, Myoung H, et al. Analysis of the outcome of young age tongue squamous cell carcinoma. Maxillofac Plast Reconstr Surg. 2017;39:41. doi: 10.1186/s40902-017-0139-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kapila SN, Natarajan S, Boaz K. A comparison of clinicopathological differences in oral squamous cell carcinoma in patients below and above 40 years of age. J Clin Diagn Res. 2017;11:ZC46–50. doi: 10.7860/JCDR/2017/27828.10600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahmood N, Hanif M, Ahmed A, Jamal Q, Saqib, Khan A. Impact of age at diagnosis on clinicopathological outcomes of oral squamous cell carcinoma patients. Pak J Med Sci. 2018;34:595–9. doi: 10.12669/pjms.343.14086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mukdad L, Heineman TE, Alonso J, Badran KW, Kuan EC, St John MA. Oral tongue squamous cell carcinoma survival as stratified by age and sex: A surveillance, epidemiology, and end results analysis. Laryngoscope. 2019;129:2076–81. doi: 10.1002/lary.27720. [DOI] [PubMed] [Google Scholar]
- 16.Xu QS, Wang C, Li B, Li JZ, Mao MH, Qin LZ, et al. Prognostic value of pathologic grade for patients with oral squamous cell carcinoma. Oral Dis. 2018;24:335–46. doi: 10.1111/odi.12727. [DOI] [PubMed] [Google Scholar]
- 17.Costa V, Kowalski LP, Coutinho-Camillo CM, Begnami MD, Calsavara VF, Neves JI, et al. EGFR amplification and expression in oral squamous cell carcinoma in young adults. Int J Oral Maxillofac Surg. 2018;47:817–23. doi: 10.1016/j.ijom.2018.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Oliver JR, Wu SP, Chang CM, Roden DF, Wang B, Hu KS, et al. Survival of oral tongue squamous cell carcinoma in young adults. Head Neck. 2019;41:2960–8. doi: 10.1002/hed.25772. [DOI] [PubMed] [Google Scholar]
- 19.Teixeira LR, Almeida LY, Silva RN, Mesquita AT, Colturato CB, Silveira HA, et al. Young and elderly oral squamous cell carcinoma patients present similar angiogenic profile and predominance of M2 macrophages: Comparative immunohistochemical study. Head Neck. 2019;41:4111–20. doi: 10.1002/hed.25954. [DOI] [PubMed] [Google Scholar]
- 20.Zhang B, Du W, Gan K, Fang Q, Zhang X. Significance of the neutrophil-to-lymphocyte ratio in young patients with oral squamous cell carcinoma. Cancer Manag Res. 2019;11:7597–603. doi: 10.2147/CMAR.S211847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goepfert RP, Kezirian EJ, Wang SJ. Oral tongue squamous cell carcinoma in young women: A matched comparison-Do outcome justify treatment intensity? ISRN Otolaryngol. 2014;2014:1–6. doi: 10.1155/2014/529395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cariati P, Cabello-Serrano A, Perez-de Perceval-Tara M, Monsalve-Iglesias F, Martínez-Lara I. Oral and oropharyngeal squamous cell carcinoma in young adults: A retrospective study in Granada University Hospital. Med Oral Patol Oral Cir Bucal. 2017;22:e679–e685. doi: 10.4317/medoral.21755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Abdulla R, Adyanthaya S, Kini P, Mohanty V, D'Souza N, Subbannayya Y. Clinicopathological analysis of oral squamous cell carcinoma among the younger age group in coastal Karnataka, India: A retrospective study. J Oral Maxillofac Pathol. 2018;22:180–7. doi: 10.4103/jomfp.JOMFP_16_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Farquhar DR, Tanner AM, Masood MM, Patel SR, Hackman TG, Olshan AF, et al. Oral tongue carcinoma among young patients: An analysis of risk factors and survival. Oral Oncol. 2018;84:7–11. doi: 10.1016/j.oraloncology.2018.06.014. [DOI] [PubMed] [Google Scholar]
- 25.Choi G, Song JS, Choi SH, Nam SY, Kim SY, Roh JL, et al. Comparison of Squamous Cell Carcinoma of the Tongue between Young and Old Patients. J Pathol Transl Med. 2019;53:369–77. doi: 10.4132/jptm.2019.09.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Campbell BR, Sanders CB, Netterville JL, Sinard RJ, Rohde SL, Langerman A, et al. Early onset oral tongue squamous cell carcinoma: Associated factors and patient outcomes. Head Neck. 2019;41:1952–60. doi: 10.1002/hed.25650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mohideen K, Krithika C, Jeddy N, Bharathi R, Thayumanavan B, Sankari SL. Meta-analysis on risk factors of squamous cell carcinoma of the tongue in young adults. J Oral Maxillofac Pathol. 2019;23:450–7. doi: 10.4103/jomfp.JOMFP_118_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martinez RC, Sathasivam HP, Cosway B, Paleri V, Fellows S, Adams J, et al. Clinicopathological features of squamous cell carcinoma of the oral cavity and oropharynx in young patients. Br J Oral Maxillofac Surg. 2018;56:332–7. doi: 10.1016/j.bjoms.2018.03.011. [DOI] [PubMed] [Google Scholar]


