Abstract
Introduction:
Aerosols and droplets contaminated with bacteria and blood are produced during ultrasonic scaling. Measures to control aerosol contamination in dental clinics are recommended by the Centers for Disease Control and Prevention. This study aimed to evaluate the efficacy of preprocedural boric acid (BA) mouthrinse in reducing bacterial contamination in dental aerosols generated during ultrasonic scaling.
Materials and Methods:
This was a randomised clinical trial in 90 systemically healthy subjects (25-55 yrs) diagnosed with chronic periodontitis who were allocated into three groups of 30 subjects each to receive, Group A - 0.12% chlorhexidine (CHX), Group B - 0.75% BA and Group C-water, as a preprocedural rinse for 1 min. The aerosol generated while performing ultrasonic scaling for 30 min was collected at three locations on blood agar plates. Incubation of the blood agar plates at 37°C for next 48 h for aerobic culture was performed and subsequently colony-forming units (CFUs) were counted.
Results:
CFUs in Group A were significantly reduced compared with Group B (P < 0.001). When we compare CFUs in all the three groups, CFUs in Groups A and B were statistically significantly reduced compared with Group C (P < 0.001). Furthermore, it was also observed that the assistant's chest area had lowest CFUs whereas patient's chest area had highest.
Conclusion:
This study recommends routine use of preprocedural mouthrinse as a measure to reduce bacterial aerosols generated during ultrasonic scaling and that 0.12% CHX gluconate is more effective than 0.75% BA mouthwash in reducing CFUs count.
Keywords: Aerosol contamination, boric acid, chlorhexidine, infection control dentistry preprocedural rinse, mouthwash, ultrasonic scaling
Introduction
Proper infection control protocol maintenance is a prime concern in dentistry. Patients and dental professionals in the working area are vulnerable to cross infections and it can result in vicious cycle. Aerosols are any air suspended particles which can be either classified as liquid or solid generated by human, animal, instruments, or machine.[1] When the aerosols consist of particles having any kind of organisms, it is termed as bioaerosols and they differ in characteristics depending on humidity, air flow, and temperatures.[2] Aerosols consisting small particles are termed as droplet nuclei which are <5μm and >5μm are designated as droplets. These particles can remain suspended in air for long hours and has capacity to transport over long distances, contaminating any surfaces that comes in contact with them.[1] The droplet needs special consideration as they have the ability to contaminate surfaces over a wide range of 1 meter (3ft) penetrating deep into the alveoli and serves as source of infection in dental practice.[3,4] Aerosols are reported to be associated with various systemic infections namely respiratory, skin, ophthalmic infections, tuberculosis, and hepatitis B.[5]
Ultrasonic scaling produces a large amount of aerosols and is considered as one of the aerosol generating procedures that can lead to cross infections, disease transmission, and respiratory disease.[6] Accordingly to the Centers for Disease Control and Prevention (CDC) use Rubber dam placement, air evacuation having high velocity air, proper ventilated rooms for escape of aerosols are methods to reduce blood borne microorganism resulting from aerosols contamination during patient treatment.[7]
Unfortunately, methods to minimize the formation of droplets and aerosols during ultrasonic scaling procedures are limited. The most frequent recommendation for reducing aerosols produced by an ultrasonic sealer is the concurrent use of a high volume evacuator during scaling procedure.[8] Recently, use of preprocedural mouthrinse as a method of reducing aerosol contamination has gained popularity. Efficacy of various mouthrinses such as herbal rinse, aloevera rinse, povidine iodine, and chlorhexidine (CHX) rinse is studied.[9,10]
CHX is an antimicrobial rinse which has broad spectrum antimicrobial activity and 8–12 h of substantivity. However,when CHX is used as mouthrinse side effects such as teeth, restorations and mucosal staining, mucosal dryness and soreness, alteration in taste sensation and enhancement in supragingival calculus formation can be seen.[11] In developing countries, where many dental hospitals and clinics have limited resources and constraints in use of additional equipments like high velocity air evacuation and trained dental assistants; use preprocedural rinse seems easy and economical basis in reduction of aerosols contamination.
This leads to investigation/use of mouthrinses which will have high potency, economical, pleasant taste, and availability. However, the urge for a better antimicrobial rinse with few side effects which can be used as a preprocedural rinse remains a potential field of research in dental community.
Boron is a bioactive trace element, found naturally as boric acid (BA) and borate. Fruits, vegetables (potato and avocado), legumes, nuts, eggs, milk, wine, and dried foods are considered as rich sources of boron.[12] Boron has antibacterial and anti-inflammatory activity and contains AN0128, a boron-containing compound. It has antimicrobial activity against anaerobic microbes such as Prevotella intermedia, Porphyromonas gingivalis, Eubacterium nodatum, and Treponema denticola.[13] An animal study in rats showed reduced levels of inflammatory infiltrate and subsequent alveolar bone loss by daily topical application of AN0128 (1%) in experimentally ligature induced periodontitis.[13] Sağlam et al. studied effects of BA irrigation in addition to scaling and root planing (SRP) and found significant reduction in pocket depth (PD) and clinical attachment loss for moderate pockets.[14]
Therefore, boron could have a possible role in prevention of aerosol contamination during ultrasonic scaling. To date, no study has been conducted demonstrating the effect of BA as preprocedural rinse in reducing aerosol contamination. The present study was designed to determine the role of BA mouthrinse as a preprocedural rinse in reducing bacterial contamination in dental aerosols generated during ultrasonic scaling.
Materials and Methods
Study participants
This randomized single-center trial was conducted at the Department of Periodontology from March 2016 to August 2016. This study got approval by the Institutional Ethics Committee and registered at CTRI/2017/10/010189. Initially, a pilot study with the same protocol was performed for sample size estimation. Written Informed consent was taken from all the participants. Systemically healthy individuals (25 to 55 years) male or female diagnosed with moderate chronic periodontitis having least 20 natural teeth with a mean Plaque index(PI) score of 2.0 - 3.0[15], probing pocket depth (PPD) ≥4 mm in four or more sites [Table 1] were included.
Table 1.
Baseline demographic characteristics of each group
| Patient | Group A (0.12% CHX) Mean±SD |
Group B (0.75% BA) | Group C (water) | P |
|---|---|---|---|---|
| Age (years) | 36.36±7.02 | 38.34±4.5 | 37.45±6.23 | NS |
| Males/females | 13/17 | 10/20 | 12/16 | NS |
| Number of teeth | 27.88±1.47 | 27.35±1.47 | 27.77±1.78 | NS |
| PI | 2.6±0.06 | 2.75±0.27 | 2.81±0.29 | NS |
CHX: Chlorhexidine; BA: Boric acid; SD: Standard deviation; PI: Plaque index
Subjects with respiratory infection, smokers, Pregnant / Lactating women, administration of any mouth rinses or oral irrigation, any systemic or topical antimicrobial drug intake in last 6 months, hypersensitivity to chlorhexidine gluconate or boric acid and other formula ingredients were excluded from the study.
Exclusion criteria where subjects with respiratory infection, smokers, pregnant/lactating women, administration of any mouthrinses or oral irrigation, any systemic or topical antimicrobial drug intake in the last 6 months, hypersensitivity to CHX gluconate or BA, and other formula ingredients.
Boric acid mouthrinse preparation
Sağlam et al. used 12% stock solution of BA and other diluents (6%, 3%, 1.5%, 0.75%, 0.375%, 0.1875%, and 0.09375%) were obtained from stock solution.[14] Based on this study in vitro cytotoxicity results, 0.75% BA solution was used for subgingival irrigation. Based on this study, 0.75% BA formulation was prepared at JSS College of Pharmacy, Mysuru. 2% stock solution was prepared from BA (12 g BA/100 ml distilled water) (64,271, Merck, Darmstandt, Germany). 1/16 dilutions were prepared from this solution. All these processes were carried out in laminar flow cabin. Solutions were sterilized by filters with a sieve size of 0.22 μm. The pH of the prepared BA solution was 4.9.
Clinical procedure
The entire study was conducted in a single special clinic where fumigation facility was available. Ethyl alcohol (70%) was used to disinfect the operatory surfaces. Blood agar plate was positioned on patient dental chair area for 30 min before the procedure to check for environmental contamination. The procedure on the patients commenced only after the operator was assured that there is no environmental contamination seen on the agar plate. The subjects were allocated randomly into three groups as mentioned below.
Group A (CHX) – 0.12% CHX (Periogard®, Colgate-Palmolive)
Group B (BA) – 0.75% BA
Group C (control group)–Water.
Single sitting ultrasonic scaling with saliva ejector for 20 min duration was performed in randomly selected quadrant using computerized randomization (GraphPad). Each subject was instructed to maintain asepsis' and was allowed to enter the operatory area with head caps and autoclaved gowns. Subjects were instructed to rinse for 1 min with 15 ml of 0.12% CHX, 10 ml BA, or 10 ml water just 15 min prior to the treatment procedure. Any discomfort, taste alteration, burning sensation, and adverse effects were noted during the intraoperative procedure and posttreatment. 0.12% of CHX was chosen as preprocedural rinse due to its potent antimicrobial activity.
Blood agar plates were used to culture airborne bacteria which were placed in 3 positions. The position of the agar plates were decided based on previous study.[16] Mouth of the patients was considered as a reference point and 12 inches fixed distance of the plates were maintained in regard to this reference point [Figure 1]. Patients' chest, operators' chest, and dental assistants' chest were the three locations for positioning the agar plates. The agar plates were fixed on the position using tapes and three-color coding was used to conceal the allocated groups.
Figure 1.

Position of agar plates
Microbial analysis
Since the study protocol involved triple masking, the operator, microbiologist, and the patients were unaware of allocated groups. The blood agar plates were transferred to the Microbiology Department of JSS Medical College and Hospital for incubation at 37°C for next 48 h, and colony-forming units (CFUs) were counted [Figures 2–4].
Figure 2.
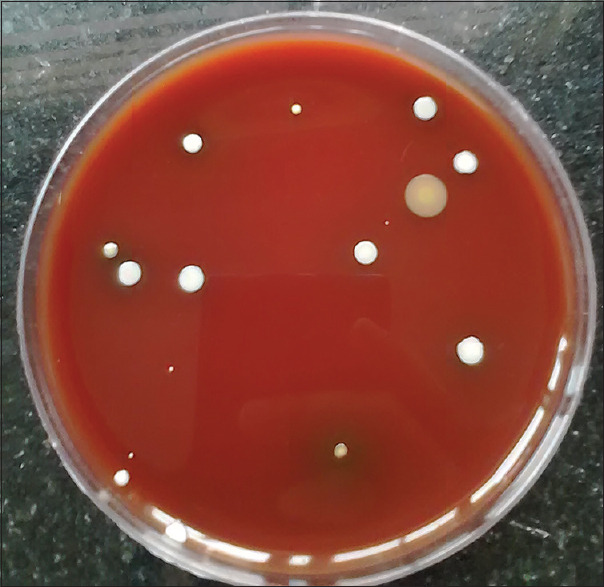
Microbial colonies formed on an agar plate after using chlorhexidine mouthrinse
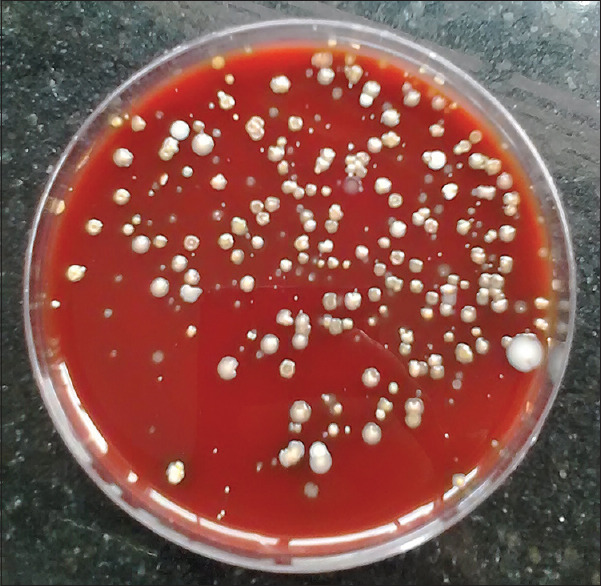
Figure 4.

Microbial colonies formed on an agar plate after using water
Figure 3.
Microbial colonies formed on an agar plate after using boric acid mouthrinse
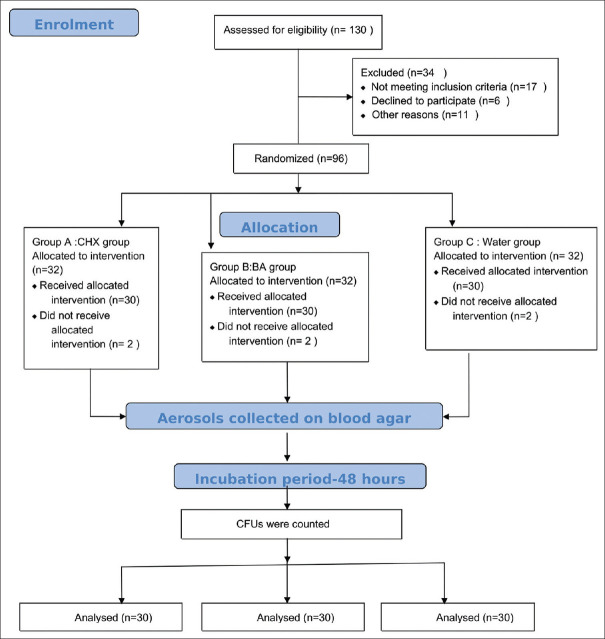
The sample size was determined from a previous related study[17] and adjusted based on results of the pilot study, where in each group, 10 subjects were enrolled. Volunteers who participated in the pilot study were excluded from the main study. The minimum number of 26 subjects per group was required to achieve 80% power and a 5% significance level. To compensate for an estimated 20% drop out of subjects, 32 subjects with periodontitis in each group were recruited. During the course of study due to 2 drop outs in each group, the sample size was adjusted to 30 in each group. The patients were randomly allotted using computer-generated random sequence table (GraphPad) to one of the three groups by one examiner (Avinash BS) while the treatment was performed by another examiner (S Nisha) unknown of the pre rinse used before scaling [Figure 5].
Figure 5.
Consort flowchart
Statistical analysis
Descriptive analysis included mean and standard deviation of age, number of teeth, and PI of each group [Table 1]. Comparison of CFUs among the three groups at all the three locations was done using analysis of variance (ANOVA) [Table 2]. The mean difference between Groups 1 and 2 was done using independent t-test [Table 3]. Statistical significance at P < 0.05 was considered. All the statistical analysis was done using Statistical Package for the Social Sciences (SPSS) software (SPSS for Windows, version 16.0, SPSS Inc., Chicago, IL, USA).
Table 2.
Colony-forming units (mean±standard deviation) in relation to treatment and location
| Location of agar plate | 0.12% CHX | 0.75% BA mouthrinse | Water |
|---|---|---|---|
| Doctor’s chest area | 23.2±2.4 | 49.8±3.90 | 79.1±8.5 |
| Assistant’s chest area | 12.06±1.81 | 20.09±4.16 | 34.13±5.35 |
| Patient’s chest area | 80.10±4.11 | 170.3±3.65 | 298.83±11.65 |
CHX: Chlorhexidine; BA: Boric acid; SD: Standard deviation
Table 3.
Comparison of colony-forming units between the three groups (n=30 in each group) at all three locations
| Location and rinse | Mean±SD | F | P |
|---|---|---|---|
| Doctor’s chest area | |||
| CHX | 23.2±2.4 | 745.627 | <0.001 |
| BA | 49.8±3.9 | ||
| Water | 79.1±8.5 | ||
| Patient’s chest area | |||
| CHX | 80.10±4.11 | 225.169 | <0.001 |
| BA | 170±3.65 | ||
| Water | 298.83±11.65 | ||
| Assistant’s chest area | |||
| CHX | 12.06±1.81 | 6543.55 | <0.001 |
| BA | 20.06±4.61 | ||
| Water | 34.13±5.35 |
Statistically significant at P<0.05. CHX: Chlorhexidine; BA: Boric acid; SD: Standard deviation
Results
A total of 130 subjects with moderate chronic periodontitis were initially assessed for participation in the study, 37 did not meet the inclusion criteria, and 96 subjects randomized into three groups, 6 lost to follow-up, so 30 subjects were finally allotted in each group [Figure 4].
A total of 90 subjects with moderate chronic periodontitis participated in this study. The mean age of the subjects was 37 years with average number of teeth 27. The mean PI score was 2.6 [Table 1]. In all the three groups, the mean CFUs at three locations are presented in Table 2 and its graphical representation is given in Figure 6. Maximum CFUs reduction was seen in Group A (CHX) at all the three locations. However, both Group A (CHX) and Group B (BA) were effective in CFUs reduction when compared with the control Group C (water). It was also observed that the assistant's chest area had lowest CFUs whereas patient's chest area had highest.
Figure 6.
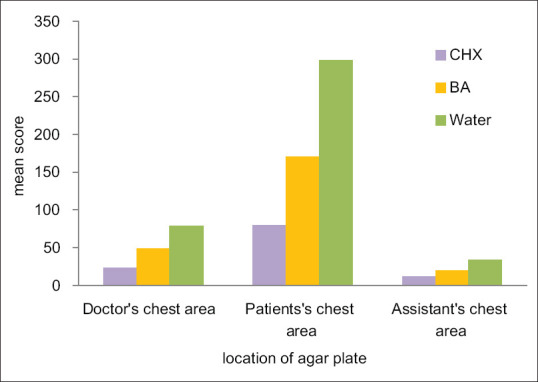
Mean CFUs for three groups at three locations
The mean difference among the three groups (ANOVA test) showed statistical significant difference (P < 0.001) at all the three locations [Table 3]. Comparison of mean differences between Groups A and B showed statistical significant reduction in CFUs in CHX group when compared with BA group (P < 0.001) [Table 4].
Table 4.
Comparison of colony-forming units between the chlorhexidine and boric acid groups (n=30 each) at all three locations
| Location and rinse | Mean±SD | t-test | P |
|---|---|---|---|
| Doctor’s chest area | |||
| CHX | 22.00±6.52 | 31.46 | <0.001 |
| BA | 54.75±18.86 | ||
| Patient’s chest area | |||
| CHX | 79.75±26.22 | 89.85 | <0.001 |
| BA | 182.50±62.28 | ||
| Assistant’s chest area | |||
| CHX | 10.00±4.54 | 10.69 | <0.001 |
| BA | 19.25±6.34 |
Significant at P<0.05. CHX: Chlorhexidine; BA: Boric acid; SD: Standard deviation
Thus, reduction of CFU's on agar plates for observed better in CHX group when compared with BA and water when used as a preprocedural mouthrinse.
Discussion
There lies a significant risk of infection transmission when we work with dental procedures involving aerosols generation. Infected patient's body fluids, contaminated surfaces, infectious particles like aerosols have potential to enter respiratory passages and they should be considered as greatest threat to infection. These particles have the ability to stay airborne or to become reairborne as a dust particle.
A recent study on effects of CHX preprocedural rinse on bacteremia showed gingivitis and periodontitis induced by ultrasonic scaling and discrete effect on total bacterial load.[18] As many of the procedures generating aerosols are basic dental treatment and cannot be avoided, every effort should be made to minimize the chance of cross-infection. It should be the responsibility of dental team to use protective measures like high-volume evacuators, air cleaning systems, use of ultraviolet (UV), UV chambers, and preprocedural rinsing as methods to minimize airborne infections.
Irrespective of the methods used, they target either removal of contaminated material from the treatment area once it becomes airborne using devices or removal of airborne contamination before it leaves the immediate operative area. Use of combination approach might be beneficial in infection control as no single approach or device can minimize the risk of infection and it is difficult to exactly quantify the exact infection risk represented by aerosolized material.
In the present study, we evaluated the efficacy of BA as preprocedural rinse in reducing aerosol contamination and found statistical significant difference when compared with water but not with CHX. We hypothesized that BA would reduce the aerosol generated during ultrasonic scaling when compared to CHX and water. The rationale behind such hypothesis was based on antimicrobial efficacy of BA when used as subgingival irrigation, in local drug therapy, its inhibitory effect on alveolar bone loss.[14,19,20] A study by Cuadra et al. demonstrated antimicrobial property of BA by dependency of autoinducer-2 detection among commensal oral streptococci on pH and BA. BA 1 mM addition enhanced the bioluminescence and allowed better binding and detection of streptococci strains.[21]
Direct comparison of clinical efficacy of BA mouthrinse with other studies was not possible as no studies till date have reported the use of 0.75% BA mouthrinse as preprocedural rinse in reducing aerosol contamination.
Sağlam et al. evaluated effects of BA irrigation in adjunct to nonsurgical periodontal therapy and showed whole mouth bleeding on probing, probing depth and clinical attachment reduction was more favorable in BA group compared to CHX.[14] However, no significant differences between the groups were seen in terms of microbiologic parameters. In the present study, fewer CFUs developed in CHX group as compared with BA group, this might be due to the lack of standardisation of rinse dosage, use of more concentrated solution might have an effect on its antimicrobial property and CFUs count. Future research should be focused on exploring substantivity property of BA and its efficacy against various microbes.
Irrespective of the efficacy of CHX or BA as preprocedural rinse, this study gives an idea that preprocedural rinse is crucial and should be considered as a daily protocol before ultrasonic scaling as a method of infection control. This can be concluded as both the mouthrinses had statistical significant results in reducing CFUs compared to water which was used as control.
Kanoriya et al. demonstrated the use of locally delivered 0.75% BA gel in chronic periodontitis patients and observed reduction in PPD and increased clinical attachment levels suggesting antibacterial and regenerative potential of BA.[19] Another study used 0.75% BA gel in Grade II furcation defects and showed significant improvement in clinical parameters suggesting its anti-inflammatory property.[22] These studies give us an idea of the antimicrobial, anti-inflammatory properties of BA and its potential use in the field of periodontology.
Müller et al. investigated the antibacterial effects and cytotoxicity of oral rinses and observed that oral rinses are heterogeneous with regard to their antimicrobial and cytotoxic activities in vitro.[23] CHX at low concentrations have potent antimicrobial property, favors eukaryotic cell viability, and inhibits growth of prokaryotic bacteria. Similar study with different concentration of BA mouthrinse will helps us to better understand its antimicrobial efficacy.
The limitations of the study are the method of sampling, position and distance of agar plates placement, selective medium to grow microorganisms and its culturing method. As several study showed different number of agar plate positioned at different locations. The results obtained cannot be generalized. The spread of aerosol is heterogeneous and air quantification, sampling time, distance, and location should be taken into consideration while interpretation of the results. Only aerobic bacterial growth was seen as viruses, and anaerobic bacteria are specific microorganisms requiring selective sampling and culturing methods. Further research should concentrate preprocedural rinsing with shorter duration and various volumes of pre rinse.
Conclusion
Irrespective of the efficacy of CHX or BA as preprocedural rinse, the study gives an idea that preprocedural rinse is crucial and should be considered as a daily protocol before ultrasonic scaling as a method of infection control. This can be concluded as both the mouthrinses had statistical significant results in reducing CFUs compared to water which was used as control in the present study. Furthermore, BA though less potent than 0.12% CHX, still it can be preferred in case of patients allergic to CHX, who wants to avoid alcohol-based, artificial preservatives and colors. Measures to reduce aerosol contamination should be strictly practice in dental offices, particularly in multichair clinics and also specially in hospital-based setup, where quiet a number of dental chairs are simultaneously used for ultrasonic scaling and a larger population of dental practitioner, students, and patients are at risk of infection. infection. Practising infection control at undergraduate level should be stressed on standard dental practice as such measures will minimise risk of infection.
Financial support and sponsorship
This research was financially supported by JSS Academy of higher education and Research University, Mysuru, Karnataka (No.REG/DIR(R)/URG/5 4/2011-12/7279/9). The funding source had no influence in design; collection, analysis and interpretation of data; writing and submission of the report; and in the decision to submit the article for publication.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Professor Dr. Deepika Pawar Chandrashekara Rao, Department of Periodontology for her constant guidance and support throughout this research work and Interns posted in Department of Periodontology for their assistance during the clinical procedure.
References
- 1.ASHRAE. ASHRAE Position Document on Airbone Infectious Diseases. Atlanta, Georgia: ASHRAE; 2014. [Google Scholar]
- 2.Szymanska J. Dental bioaerosol as an occupational hazard in a dentist's workplace. Ann Agric Environ Med. 2007;14:203–7. [PubMed] [Google Scholar]
- 3.Barker J, Jones MV. The potential spread of infection caused by aerosol contamination of surfaces after flushing a domestic toilet. J Appl Microbiol. 2005;99:339–47. doi: 10.1111/j.1365-2672.2005.02610.x. [DOI] [PubMed] [Google Scholar]
- 4.Seto WH, Conly JM, Pessoa-Silva CL, Malik M, Eremin S. Infection prevention and control measures for acute respiratory infections in healthcare settings: East Mediterr Health J. 2013;19(Suppl 1):S39–47. [PubMed] [Google Scholar]
- 5.Laheij AM, Kistler JO, Belibasakis GN, Valimaa H, de Soet JJ. European Oral Microbiology W. Healthcare associated viral and bacterial infections in dentistry. J Oral Microbiol. 2012;4:1–4. doi: 10.3402/jom.v4i0.17659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldman HS, Hartman KS. Infectious diseases. Their disease, our unease: Infectious diseases and dental practice. Va Dent J. 1986;63:10–9. [PubMed] [Google Scholar]
- 7.CDC. Recommended infection-control practices for dentistry. Morb Mortal Wkly Rep Recomm Rep. 1993;41:1–12. [PubMed] [Google Scholar]
- 8.Bently CD, Burkhart NW, Crawford JJ. Evaluating spatter and aerosol contamination during dental procedures. J Am Dent Assoc. 1994;125:579–84. doi: 10.14219/jada.archive.1994.0093. [DOI] [PubMed] [Google Scholar]
- 9.Paul B, Baiju RM, Raseena NB, Godfrey PS, Shanimole PI. Effect of Aloe vera as a preprocedural rinse in reducing aerosol contamination during ultrasonic scaling. J Indian Soc Periodontol. 2020;24:37–41. doi: 10.4103/jisp.jisp_188_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haffajee AD, Yaskell T, Socransky SS. Antimicrobial effectiveness of an herbal mouthrinse compared with an essential oil and a chlorhexidine mouthrinse. J Am Dent Assoc. 2008;139:606–11. doi: 10.14219/jada.archive.2008.0222. [DOI] [PubMed] [Google Scholar]
- 11.Varoni E, Tarce M, Lodi G, Carrassi A. Chlorhexidine (CHX) in dentistry: State of the art. Minerva Stomatol. 2012;61:399–419. [PubMed] [Google Scholar]
- 12.Nielsen FH. Is boron nutritionally relevant? Nutr Rev. 2008;66:183e91. doi: 10.1111/j.1753-4887.2008.00023.x. [DOI] [PubMed] [Google Scholar]
- 13.Luan Q, Desta T, Chehab L, Sanders VJ, Plattner J, Graves DT. Inhibition of experimental periodontitis by a topical boron-based antimicrobial. J Dent Res. 2008;87:148–52. doi: 10.1177/154405910808700208. [DOI] [PubMed] [Google Scholar]
- 14.Sağlam M, Arslan U, Buket Bozkurt Ş, Hakki SS. Boric acid irrigation as an adjunct to mechanical periodontal therapy in patients with chronic periodontitis: A randomized clinical trial. J Periodontol. 2013;84:1297–308. doi: 10.1902/jop.2012.120467. [DOI] [PubMed] [Google Scholar]
- 15.Silness J, Loee H. Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand. 1963;21:533–51. doi: 10.3109/00016356309011240. [DOI] [PubMed] [Google Scholar]
- 16.Kaur R, Singh I, Vandana KL, Desai R. Effect of chlorhexidine, povidone iodine, and ozone on microorganisms in dental aerosols: Randomized double-blind clinical trial. Indian J Dent Res. 2014;25:160–5. doi: 10.4103/0970-9290.135910. [DOI] [PubMed] [Google Scholar]
- 17.Gupta G, Mitra D, Ashok KP, Gupta A, Soni S, Ahmed S, et al. Efficacy of preprocedural mouth rinsing in reducing aerosol contamination produced by ultrasonic scaler: A pilot study. J Periodontol. 2014;85:562–8. doi: 10.1902/jop.2013.120616. [DOI] [PubMed] [Google Scholar]
- 18.Balejo RDP, Cortelli JR, Costa FO, Cyrino RM, Aquino DR, Cogo-Muller K, et al. Effects of chlorhexidine preprocedural rinse on bacteremia in periodontal patients: A randomized clinical trial. J Appl Oral Sci. 2017;25:586–95. doi: 10.1590/1678-7757-2017-0112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kanoriya D, Singhal S, Garg V, Pradeep AR, Garg S, Kumar A. Clinical efficacy of subgingivally-delivered 0.75% boric acid gel as an adjunct to mechanotherapy in chronic periodontitis: A randomized, controlled clinical trial. J Invest Clin Dent. 2017;9:e12271. doi: 10.1111/jicd.12271. [DOI] [PubMed] [Google Scholar]
- 20.Sağlam M, Hatipoğlu M, Köseoğlu S, Esen HH, Kelebek S. Boric acid inhibits alveolar bone loss in rats by affecting RANKL and osteoprotegerin expression. J Periodontal Res. 2014;49:472–9. doi: 10.1111/jre.12126. [DOI] [PubMed] [Google Scholar]
- 21.Cuadra GA, Frantellizzi AJ, Kimberly M, Gaesser KM, Tammariello SP, Ahmed A. Autoinducer-2 detection among commensal oral streptococci is dependent on pH and boric acid. J Microbiol. 2016;54:492–502. doi: 10.1007/s12275-016-5507-z. [DOI] [PubMed] [Google Scholar]
- 22.Singhal S, Pradeep AR, Kanoriya D, Garg S, Garg V. Boric acid gel as local drug delivery in the treatment of class II furcation defects in chronic periodontitis: A randomized, controlled clinical trial. J Invest Clin Dent. 2017;9:e12279. doi: 10.1111/jicd.12279. [DOI] [PubMed] [Google Scholar]
- 23.Müller HD, Eick S, Moritz A, Lussi A, Gruber R. Cytotoxicity and antimicrobial activity of oral rinses in vitro. BioMed Res Int. 2017;2017:4019723. doi: 10.1155/2017/4019723. [DOI] [PMC free article] [PubMed] [Google Scholar]