Abstract
Background
Longitudinal studies examining the impact of changes in COVID-19 pandemic-related stressors and experiences, and coping styles on the mental health trajectory of employed individuals during the lockdown are limited. The study examined the mental health trajectories of a sample of employed adults in Hamilton, Ontario during the initial lockdown and after the re-opening following the first wave in Canada. Further, this study also identified the pandemic-related stressors and coping strategies associated with changes in depressive symptoms in employed adults during the COVID-19 pandemic.
Methods
The InHamilton COVID-19 longitudinal study involved 579 employees aged 22–88 years from a large public university in an urban area of Hamilton, Ontario at baseline (April 2020). Participants were followed monthly with 6 waves of data collected between April and November 2020. A growth mixture modeling approach was used to identify distinct groups of adults who followed a similar pattern of depressive symptoms over time and to describe the longitudinal change in the outcome within and among the identified sub-groups.
Results
Our results showed two distinct trajectories of change with 66.2% of participants displaying low-consistent patterns of depressive symptoms, and 33.8% of participants displaying high-increasing depressive symptom patterns. COVID-19 pandemic-related experiences including health concerns, caregiving burden, and lack of access to resources were associated with worsening of the depressive symptom trajectories. Frequent use of dysfunctional coping strategies and less frequent use of emotion-focused coping strategies were associated with the high and increasing depressive symptom pattern.
Conclusions
The negative mental health impacts of the COVID-19 pandemic are specific to subgroups within the population and stressors may persist and worsen over time. Providing access to evidence-informed approaches that foster adaptive coping, alleviate the depressive symptoms, and promote the mental health of working adults is critical.
Keywords: Depressive symptoms, Mental health, COVID-19, Caregiving, Coping strategies, Employed adults, Growth mixture modeling
Introduction
The emergence and rapid spread of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) created a global health crisis that prompted governments around the world to implement a range of public health measures to control the spread of the infection [1]. The first lockdown began in most Canadian provinces, including Ontario, in mid-March 2020 and continued until June 2020. During this period, provincial and territorial governments implemented public health measures to mitigate the transmission of SARS-CoV-2. Examples of these measures include, but are not limited to, active surveillance for suspected cases, self-isolation and home quarantine; physical distancing and masking mandates; closure of schools and universities; closure of non-essential services, workplaces, and gathering places; international travel restrictions and closure of the Canada-U.S. border [1].
The COVID-19 pandemic has also negatively impacted the economy. Many individuals have experienced job insecurity as well as loss of employment and income, which has negatively impacted their mental health [2]. During the pandemic, the work environment has significantly changed, with one third of Canadian employees directed to work remotely from home [3]. For some individuals, remote work has enabled better integration of family and work responsibilities, and increased work efficiency and well-being in the short-term [4, 5]. However, for others, remote work introduced barriers to productivity, such as lack of interaction with colleagues, inadequate workspace, difficulty with internet speed, and limitations with accessing work-related information and devices. Such barriers have been described as a blurring of the work-home boundaries, that has been attributed to lower productivity and motivation, greater emotional exhaustion, and higher stress [6–9]. These negative effects may vary depending upon the level of support provided by an employer, the individual’s social network outside of work, types of coping strategies used, and demands of the home environment [6–9]. Studies have also reported that individuals with greater caregiving responsibilities and/or those who report feeling an added burden in terms of caring for others during disasters, including COVID-19, identify higher levels of stress and anxiety [10–12]. As those who are working remotely or otherwise continue to adhere to the physical distancing policies, it is important to examine the impact of the COVID-19 pandemic and related stressors on their respective mental health.
Studies that compared data before the pandemic with that collected during lockdowns have shown an increase in the prevalence of psychological distress, depressive symptoms, and post-traumatic stress disorder [13, 14]. However, research examining the trajectory of mental health of employees during the initial lockdown and re-opening phases of the COVID-19 pandemic is needed. Hence, it remains unclear as to whether the mental health of employed adults worsened as the lockdown continued and after the restrictions were gradually lifted, or whether the trends indicated stabilization or improvement in mental health. Longitudinal studies examining the impact of changes in COVID-19 pandemic-related stressors, experiences, and coping styles on the mental health trajectory during the lockdown are limited. The purpose of this study was to examine the mental health trajectories of employed adults during the initial lockdown and as the public health restrictions eased following the first wave in Hamilton, Ontario. This study also identified the pandemic-related stressors and coping strategies associated with depressive symptoms in working population during the COVID-19 pandemic.
Methods
Study design and participants
The InHamilton COVID-19 longitudinal study was designed to understand the impact of the COVID-19 pandemic in employed adults. A total of 3800 participants including full-time and part-time faculty and staff from McMaster University, Hamilton, Ontario, were invited to take part in the study. The study recruited 579 faculty and staff at baseline (April 2020), to be followed monthly from April to August 2020 (5 monthly questionnaires), with the exit questionnaire being administered in November 2020. Hamilton, Ontario is a city of approximately 537,000 and is part of the Greater Toronto and Hamilton Area. McMaster University is a large public university in Hamilton, with 15,900 part-time and full-time employees, and is one of city’s largest employer. Thus, the sample reflects adults working for a larger institutional employer in an urban-suburban catchment area. Participants were recruited via an e-mail sent by the university’s Human Resources department to all faculty and staff, inviting them to complete a web-based questionnaire. Participants were provided with information about the purpose of the study before obtaining their consent. At baseline, information was collected about demographic factors, COVID-19 related stressors and experiences, COVID-19 symptoms, social distancing behaviours, lifestyle behaviours, physical health conditions, impact of the COVID-19 pandemic on children, family relationships, partner conflicts, coping strategies, and mental health consequences of the pandemic. This study was approved by the Hamilton Integrated Research Ethics Board (Number 8024).
Study measures
Depressive symptoms
Screening for depressive symptoms was completed using the 10-item Center for Epidemiologic Studies Short Depression Scale (CESD-10), which assesses depressive symptoms in the past week [15]. This scale includes eight items on depressed affect and two items on positive affect. Each item includes four response categories ranging from 0 to 3: rarely or never (less than 1 day), some of the time (1–2 days), occasionally (3–4 days), and all of the time (5–7 days). Scores for each participant were summed after reversing the positive affect items and can range between 0 and 30 with higher scores indicating greater number of depressive symptoms. A score of 10 or higher is identified as clinically significant depressive symptoms [15]. The CESD-10 is shown to be reliable and valid in assessing depressive symptoms in adults, with internal consistency of 0.86, test-retest reliability of 0.85, convergent validity of 0.91, and divergent of 0.89 [16–19]. The CESD-10 was administered at baseline and at each follow-up time point.
COVID-19 experiences scale
Data on COVID-19 pandemic-related experiences and stressors were measured using a self-report questionnaire [20] where participants were asked to indicate their experiences during the past month. This questionnaire was administered at baseline and at each follow-up time point. Health-related stressors were identified by asking participants to indicate whether they were ill or if someone close to them was ill, hospitalized, or had died within the past month for COVID-19 or non-COVID-19 related reasons. Difficulties with accessing resources was identified by asking participants to indicate whether they had experienced loss of income, difficulties in accessing necessary supplies or food, and were unable to get usual healthcare and prescription medications and treatments. Caregiving experience during the pandemic was identified by asking participants to indicate whether they had spent increased time caring for young and/or school-aged children, interacting with adolescents, and caregiving for older adults, and whether they were unable to care for people who require assistance due to health condition or limitation [20, 21]. Health-related stressors, difficulties with accessing resources, and caregiving experiences were grouped as ‘yes’ if the participant indicated at least one experience in the specific category or ‘no’ if the participant did not indicate any of the experiences in the specific category.
Coping strategies
The Brief COPE, a 28-item self-reported questionnaire that examines [22]. Each item is scored on a 4-point Likert scale ranging from “I have not been doing this a lot” (0 points) to “I have been doing this a lot” (3 points). The 28 items are combined into 14 subscales: Self-distraction, active coping, denial, substance use, emotional support, use of instrumental support, behavioural disengagement, venting, positive reframing, planning, humour, acceptance, religion, and self-blame. Subscales were grouped into three coping strategies: 1) ‘problem-focused’ strategy was based on the sum of scores on the active coping, planning, and use of instrumental support subscales; 2) ‘emotion-focused’ strategy was based on the sum of scores on the positive reframing, acceptance, humour, religion, and emotional support subscales; and 3) ‘dysfunctional coping’ strategy was based on the sum of scores on the self-distraction, denial, venting, substance use, behavioural disengagement, and self-blame subscales. The score for each subscale can range from 0 to 6 with higher score indicating more frequent use of the coping style. The Brief COPE has been validated in a community sample impacted by a natural disaster with internal consistency between 0.50 and 0.90 for the individual subscales [23].
Statistical analysis
Descriptive statistics were reported at each time point. The time was coded as wave 1 (baseline) to wave 6 (exit questionnaire). The latent growth mixture model was used to estimate group-based trajectories of depressive symptoms based on the CESD-10 score [24, 25]. The growth mixture modeling approach is used to identify unobserved sub-populations of individuals who follow a similar pattern of the outcome over time and describe the longitudinal change in the outcome within and among the unobserved sub-populations. The model allows for specification of different types of terms such as linear, quadratic, and cubic terms, to characterize the pattern over time. We used the censored normal distribution (CNORM) as depressive symptom score was modeled as a continuous variable and because depressive symptom scores cluster at their minimum values. The objective of model selection was to identify and describe the distinctive patterns of the data in the most useful and parsimonious manner [25]. Model selection involved the iterative estimation of the number of trajectory groups and the shape and order of each trajectory group. Statistical criteria for selecting the best fitting model was based on the Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC) with smaller values suggestive of a good fitting model. Statistically non-significant cubic and quadratic terms were excluded from the model. In some cases, the BIC value may continue to decrease as more trajectory groups are added to the model, thus, a balance between model fit statistics and usefulness of the results were considered. Missing longitudinal data were handled in the PROC TRAJ procedure under the missing at random assumption, where patterns with missing data can borrow parameter information from patterns with more data points through the creation of a latent variable [26]. COVID-19 pandemic-related experiences were included as time-varying covariates. The following covariates assessed at baseline – coping strategies, age (less than 50, 50 and over), sex (male, female), education status (below bachelor’s degree, bachelor’s degree and above), partner status (married or living with a partner in a common-law relationship, singe), type of dwelling (house, apartment), total number of COVID-19 symptoms, and total number of chronic health conditions - were included as predictors of group trajectory membership. Total number of COVID-19 symptoms and health conditions were assessed using a self-reported questionnaire and were included in the analysis as continuous variables. Odds ratio (OR), 95% confidence intervals (95% CI), and p-values were reported, and statistical analysis was conducted using PROC TRAJ Procedure in SAS software version 9.4.
Results
Of the 579 participants recruited at baseline (wave 1), 331 participants provided information at wave two, 300 at wave three, 260 at wave four, 200 at wave five, and 131 participants who completed the exit questionnaire (wave 6). The majority of the sample was 50 years and older (56.6%), female (79.4%), had at least a bachelor’s education (72.0%), married or living with a partner in common-law (71.7%), and resided in a house rather than an apartment (82.9%). The growth-based trajectory model specifying two trajectory groups, one with a linear term and the other with a quadratic term, was identified as the best-fitting model with a BIC value of − 4863.55 and AIC value of − 4801.49. Based on the trajectories in Fig. 1, the distinct depressive symptom trajectory groups were labeled low and consistent, and high and increasing. The low and consistent depressive symptom trajectory group was comprised of 66.2% of participants, and their depressive symptoms remained consistently low during the follow-up period and below the threshold of 10 for clinical significance. The high and increasing depressive symptom trajectory group, comprising 33.8% of participants, which reflected a quadratic pattern with depressive symptoms increasing from timepoint 1 to timepoint 6.
Fig. 1.
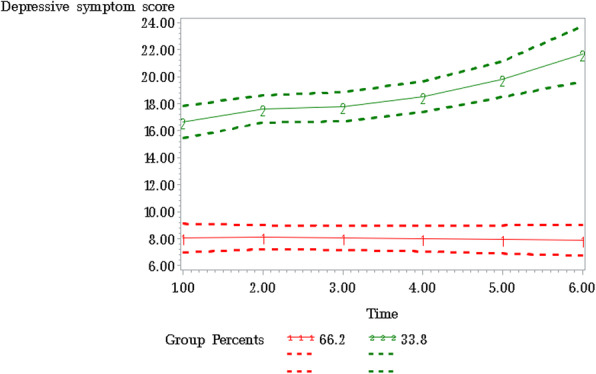
Depressive symptom trajectories (solid lines), with 95% confidence intervals (dashed lines) during the COVID-19 pandemic. Note: The dotted line indicates the threshold value (10) for clinically significant depressive symptoms
The characteristics of participants in the two depressive symptoms trajectory groups are presented in Table 1. When compared to the low and consistent depressive symptoms trajectory group, the high and increasing depressive symptoms trajectory group had a larger proportion of individuals aged 50 years and under (65.33% vs. 50.98%, p-value: 0.0037), females (85.52% vs. 76.90%, p-value: 0.0339), had lower educational attainment (i.e., below a bachelor’s degree) (31.33% vs. 22.55%, p-value: 0.0430), not married or not living with a partner in common-law (38.51% vs. 22.67%, p-value: 0.0004), resided in an apartment (25.33% vs. 13.40%, p-value: 0.0016), and had clinically significant depressive symptoms (94.00% vs. 24.51%, p-value: <.0001). Table 2 shows the depression score and COVID-19 stressors and experiences over the six time points. Overall, the average depression score at baseline was 9.63 (standard deviation (SD): 6.15) and remained relatively consistent throughout the follow-up period. At baseline, 21.93% of participants reported health-related concerns, 30.33% reported difficulties with accessing resources, and 33.20% reported spending more time in caregiving responsibilities or were unable to provide care for family members due to pandemic restrictions.
Table 1.
Distribution of demographic, health, and coping factors for the overall sample and between the two latent trajectory groups of depressive symptomsa
| Variables | Overall sample | Depression Trajectories | p-value | |
|---|---|---|---|---|
| Low and consistent | High and increasing | |||
| Age, n (%) | 0.0037 | |||
| < 50 years | 297 (56.57) | 156 (50.98) | 98 (65.33) | |
| ≥ 50 years | 228 (43.43) | 150 (49.02) | 52 (34.67) | |
| Sex, n (%) | 0.0339 | |||
| Male | 106 (20.58) | 70 (23.10) | 21 (14.48) | |
| Female | 409 (79.42) | 233 (76.90) | 124 (85.52) | |
| Education, n (%) | 0.0430 | |||
| Bachelor’s degree or above | 378 (72.00) | 237 (77.45) | 103 (68.67) | |
| Below bachelor’s degree | 147 (28.00) | 69 (22.55) | 47 (31.33) | |
| Partner status, n (%) | 0.0004 | |||
|
Married or living with a partner in common-law |
370 (71.71) | 232 (77.33) | 91 (61.49) | |
| Single | 146 (28.29) | 68 (22.67) | 57 (38.51) | |
| Type of dwelling, n (%) | 0.0016 | |||
| House | 432 (82.92) | 265 (86.60) | 112 (74.67) | |
| Apartment | 89 (17.08) | 41 (13.40) | 38 (25.33) | |
| Number of COVID-19 related symptoms, mean (SD) | 4.17 (3.24) | 3.60 (2.78) | 5.43 (3.68) | <.0001 |
| Number of chronic conditions, mean (SD) | 1.71 (1.80) | 1.75 (1.63) | 2.49 (2.03) | <.0001 |
| Coping strategy | ||||
| Problem-focused, mean (SD) | 7.29 (3.87) | 7.35 (3.79) | 7.10 (4.03) | 0.5123 |
| Emotion-focused, mean (SD) | 12.99 (4.91) | 13.51 (5.01) | 11.83 (4.45) | 0.0006 |
| Dysfunctional, mean (SD) | 7.27 (4.66) | 5.59 (3.33) | 10.78 (5.08) | <.0001 |
| Clinically significant depressive symptoms, n (%) | 225 (46.11) | 75 (24.51) | 141 (94.00) | <.0001 |
aParticipants in the low and consistent trajectory group displayed consistently low levels of depressive symptoms, while participants in the high and increasing trajectory group displayed high and accelerated increase in their depressive symptoms over time. P-value is for the comparison of characteristics between the two trajectory groups
Table 2.
Change in depression score and COVID-19 stressors and experiences for all participants over the follow-up period
| Wave 1 n = 488 |
Wave 2 n = 318 |
Wave 3 n = 294 |
Wave 4 n = 253 |
Wave 5 n = 194 |
Wave 6 n = 129 |
|
|---|---|---|---|---|---|---|
| Variables | ||||||
| Depression score, mean (SD) | 9.63 (6.15) | 9.58 (6.29) | 9.18 (6.13) | 9.04 (6.61) | 9.05 (6.84) | 9.50 (6.92) |
| Health-related stressors, n (%) | 107 (21.93) | 69 (21.70) | 62 (21.09) | 50 (19.76) | 48 (24.74) | 38 (29.46) |
| Difficulty accessing resources, n (%) | 148 (30.33) | 110 (34.59) | 68 (23.13) | 44 (17.39) | 32 (16.49) | 26 (20.16) |
| Caregiving responsibilities, n (%) | 162 (33.20) | 135 (42.45) | 114 (38.78) | 77 (30.43) | 71 (36.60) | 36 (27.91) |
aThe sample size reported for each wave is the number of participants with data available for depressive symptoms variable
Results identifying predictors of trajectory group membership (i.e., high-increasing vs. low-consistent) and time-varying covariates associated with depressive symptoms are presented in Table 3. In multivariable analysis, emotion-focused and dysfunctional coping strategies were significant predictors of trajectory group membership. Participants who were more likely to use a dysfunctional coping strategy had 1.36 (95% CI: 1.26, 1.47) times higher odds of being in the high-increasing depressive symptoms trajectory group whereas those who indicated greater use of an emotion-focused coping strategy had 0.85 (95% CI: 0.79, 0.92) times lower odds of being in this group. All three time-varying covariates (i.e., difficulties in accessing resources, caregiving stressors, and health-related stressors) significantly influenced the trajectory level of one or both groups. At a given trajectory time point, presence of difficulties in accessing resources and caregiving stressors were associated with worsening of the depressive symptoms of both the low-consistent and high-increasing trajectory groups, and presence of health-related stressors was associated with worsening of the depressive symptoms of the low-consistent trajectory group (Table 3).
Table 3.
Predictors of trajectory group membership and time-varying covariates associated with depressive symptom trajectory groups during the COVID-19 pandemic
| Predictors of group membership | ORa | 95% CI | p-value |
|---|---|---|---|
| High-increasing vs low-consistent trajectory group | |||
| Age (Ref. = ≥50) | |||
| < 50 | 1.68 | (0.88, 3.21) | 0.1112 |
| Sex (Ref. = Male) | |||
| Female | 1.57 | (0.74, 3.30) | 0.2377 |
| Education status (Ref. = Bachelor’s education or above) | |||
| Below bachelor’s education | 1.73 | (0.89, 3.38) | 0.1031 |
| Partner status (Ref. = Married or living with a partner in common-law) | |||
| Single | 1.34 | (0.67, 2.65) | 0.3994 |
| Dwelling type (Ref. = House) | |||
| Apartment | 2.08 | (0.97, 4.46) | 0.0614 |
| Number of COVID-19 related symptoms | 1.11 | (1.00, 1.22) | 0.0573 |
| Number of chronic conditions | 1.14 | (0.95, 1.36) | 0.1631 |
| Coping strategy | |||
| Problem-focused | 1.01 | (0.92, 1.11) | 0.8369 |
| Emotion-focused | 0.85 | (0.79, 0.92) | 0.0002 |
| Dysfunctional | 1.36 | (1.26, 1.47) | < 0.0001 |
| Time-varying covariates | Shift in trajectory in the presence of time-varying covariate | 95% CI | p-value |
| Health-related concerns | |||
| High-increasing group | 0.65 | (−0.27, 1.57) | 0.1635 |
| Low-consistent group | 1.36 | (0.65, 2.07) | 0.0001 |
| Difficulty in accessing resources | |||
| High-increasing group | 2.02 | (1.08, 2.96) | < 0.0001 |
| Low-consistent group | 1.48 | (0.81, 2.15) | < 0.0001 |
| Caregiving responsibilities | |||
| High-increasing group | 1.41 | (0.49, 2.33) | 0.0028 |
| Low-consistent group | 1.21 | (0.60, 1.82) | 0.0001 |
aModel was adjusted for age, sex, education status, partner status, dwelling type, number of COVID-19 related symptoms, and number of chronic conditions
Discussion
This study examined the mental health trajectories of working adults during the COVID-19 pandemic from point of initial lockdown to the gradual lifting of the public health restrictions following the first wave of the COVID-19 pandemic in Hamilton, Ontario. This study identified the pandemic-related stressors and coping strategies associated with depressive symptom trajectories. Our results showed that participants with high depressive symptoms continued to experience an increase in these symptoms even after the easing of the public health restrictions in June 2020. Use of emotion-focused and dysfunctional coping strategies were significant predictors of trajectory group membership. The COVID-19 pandemic-related stressors and experiences also had a significant influence on their respective depressive symptom trajectories.
Our results showed two distinct trajectories with a substantial one third of participants displaying high and increasing depressive symptom patterns. In comparison, a population-based, national survey conducted in the UK during the same time period identified five distinct mental health trajectories [27]. A relatively smaller sample size, a specific target population of employed adults, and differences in the timing of the implementation and lifting of the public health restrictions in our study may explain the different number of trajectories identified between the two studies.
Challenges with accessing resources, including loss of financial resources, and inability to access necessary supplies or food, healthcare, and technology, was significantly associated with depressive symptoms in both groups. Much of the evidence has focused on the impact of job insecurity, unemployment, and loss of income on the risk of anxiety and other mood disorders [28–30]. The results of the current study highlight the negative impact of the pandemic and public health measures on the mental health among individuals who are employed. When public health measures were implemented during the pandemic, many individuals reported being unable to access a range of healthcare supports including regular medical and dental services and testing, physiotherapy, massage therapy, chiropractic services, and counselling services [31]. Lack of access to these services may have led to a worsening of depressive symptoms. In fact, our results demonstrated that experiencing health-related concerns personally or living with a family member who was ill or hospitalized was a significant predictor of depression in the low-consistent group. In addition to reduced access to healthcare services, individuals who were ill or hospitalized for non-COVID-19 related health conditions may also have a fear of acquiring COVID-19, which may further contribute to stress and anxiety [32, 33]. Behavioural activation is one the core approaches for addressing depression. This approach focuses on engagement in activities that bring pleasure and mastery, as opposed to those that can lead to further depression via withdrawal (e.g., social isolation) [34]. Challenges introduced by the pandemic and the lack of access to social supports may make it difficult for individuals who experience depressive symptoms to engage in activities that can help them feel better.
The more time spent in caregiving responsibilities, including caring for young children, adolescents, and older adults as well as problems with providing such care due to pandemic-related restrictions, was a significant predictor of depressive symptoms during the initial months of the COVID-19 pandemic (April–November 2020) in both the low-consistent and high-increasing trajectory groups. Those who worked remotely and/or onsite both experienced a change in their environment, with many having to establish a new work-life routine. Working individuals have sometimes had to balance their work schedules around the needs of other family members and household chores [35]. Research has shown that many parents have experienced an increase in caregiving roles and responsibilities due to childcare and school closures during the lockdown [11]. Further, informal carers providing support to older family members are vulnerable to the consequences of the COVID-19 pandemic. They have reported mental exhaustion and increased stress levels as a result of the uncertainty of the pandemic, and the social distancing measures [36, 37]. Further, informal carers providing emotional support to family members, worrying that their older family member may acquire the infection or that they may transmit it to them, and the difficulties in meeting needs of the older adults during the pandemic have also contributed to higher mental exhaustion and stress [36, 37]. As individuals spend more time in providing support, they may have needed to alter their work or sleep schedules to concentrate on work, which in turn, may contribute to feelings of emotional exhaustion [38]. Evidence also indicates that remote working from home may be more challenging for women as they are often responsible for performing household chores, and taking care of children and supporting them with online schooling [35].
Our results showed that negative coping strategies were associated with higher and increasing levels of depressive symptoms during the COVID-19 pandemic. Compared to the low-consistent depressive symptom trajectory group, membership in the high-increasing depressive symptom trajectory group was associated with higher dysfunctional coping strategies and lower emotion-focused coping strategies. Dysfunctional coping strategies such as denial, venting, substance use, self-blame, behavioural disengagement, and self distraction have been previously shown to be significantly associated with depression, anxiety, and stress [39–41]. Research suggests that dysfunctional coping strategies may be effective in adapting to a stressor in the short-term but are ineffective over longer periods, and may lead to higher levels of stress and depressive symptoms over time [39–41]. On the contrary, positive, emotion-focused strategies have been shown to be an effective coping mechanism. Use of positive reframing, acceptance, and humour to deal with stressful situations and negative emotions in general and during the pandemic have been associated with lower stress and anxiety, and better mental health outcomes [39–41]. However, consistent with other emerging data from the COVID-19 pandemic [39], our results showed that problem-focused coping strategies such as active coping, planning, and seeking instrumental support did not predict depressive symptom trajectories. Although problem-focused coping strategies are known to be associated with mental wellbeing, individuals may seek relatively easier solutions, for example, excessive alcohol consumption, to manage stressors and problematic thoughts [39].
These results could help inform approaches to assist employed individuals working remotely during the COVID-19 pandemic. Managing the COVID-19 pandemic-related stressors and challenges requires a multidimensional approach including innovative strategies (e.g. telehealth) that provide continued access to health care while maintaining public health guidelines, unemployment insurance, access to basic needs and resources, and supportive workplace environment and policies. Employers can also develop programs that raise awareness and educate employees about effective coping skills to help manage depressive symptoms. Recommendations could include encouraging people to seek emotional support from family, friends, colleagues, or counsellors, which may help with depressive symptoms and improve mental health. In this regard, the workplace in our study has demonstrated commitment to promoting the mental health and well-being of all employees and have developed resources and implemented supports including wellness events, additional days off work in the Fall of 2020, and offered extended benefits of an Employee and Family Assistance Program. Moreover, individual departments within the University established wellness groups, developed resources for the department’s website, and offered weekly online drop-in support group to support faculty, staff, and trainees [42]. Similar approaches may also be adopted by other institutions.
Limitations
The present study has several strengths including the timing of data collection relative to the lockdown restrictions implemented in Ontario, Canada, and use of a longitudinal design to examine depressive symptom trajectories, and to identify factors associated with high and increasing depressive symptoms trajectory among working adults. However, the results of this study should be interpreted considering some limitations. First, our study had a high attrition rate over the follow-up period. Under the missing at random assumption, the PROC TRAJ procedure in SAS allows patterns with incomplete data to borrow information from patterns with more data points and thus participants with missing longitudinal data and time-varying covariates were not excluded from the analysis [26]. However, a greater proportion of individuals who had missing data for depression score had an education attainment below bachelor’s degree and were not married or in a common-law relationship compared to those who had complete data for depression score. Thus, it is possible that the shape and the number of latent trajectories identified may be influenced by the unobserved outcome of those with missing data. Second, our study lacks a pre-pandemic assessment of mental heath from this sample. Nevertheless, our results provide important information regarding the mental health of employed individuals during the initial lockdown of the COVID-19 pandemic and gradual easing of the public health restrictions. Third, our study sample included employed individuals at a single institution and had a relatively higher education attainment, thus the change in depressive symptoms observed in our study may not reflect the change in the general population. Our sample is more representative of the target population but includes a greater proportion of females than the target population. While 22–35% of our sample experienced health-related stressors, difficulties in accessing resources, and increased caregiving responsibilities, caution is warranted when generalizing the findings of this study to other segments of the population. Nevertheless, working at a university is in many ways working for other large institutional employer, as opposed to working for or owning a small business for example, and therefore, similar findings would be expected in other sectors.
Conclusions
Overall, the results of this study showed that more than one third of working adults at a large institutional employer displayed a pattern of high depressive symptoms that increased over time. COVID-19 pandemic-related stressors and experiences associated with depressive symptom trajectories included health-related concerns, financial challenges and difficulties with accessing resources, and caregiving responsibilities. Further, frequent use of dysfunctional coping strategies and less frequent use of emotion-focused coping strategies were significantly associated with the high and increasing depressive symptom group. The negative mental health impacts of the COVID-19 pandemic and related stressors may persist even after the number of infections drop and restrictions are lifted. Therefore, it is essential to promote emotion-focused strategies and programs that develop awareness, alleviate the depressive symptoms, and promote mental health of working adults.
Acknowledgements
Not applicable.
Abbreviations
- SARS-CoV-2
Severe acute respiratory syndrome coronavirus-2
- CESD-10
Center for Epidemiologic Studies Short Depression Scale
- AIC
Akaike’s Information Criterion
- BIC
Bayesian Information Criterion
- OR
Odds ratio
- 95% CI
95% confidence intervals
Authors’ contributions
DJ, AG, LG, PR participated in the design and conception of the project. DJ, AG, and PR analyzed the data. AG and PR obtained the funding. All authors have assisted with drafting the manuscript and have read and approved the final manuscript.
Funding
The InHamilton study was funded by the McMaster Institute for Research on Aging (MIRA) and the Michael G. DeGroote Institute for Pain Research and Care (IPRC) Catalyst Grant. The funding source had no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Hamilton Integrated Research Ethics Board (Number 8024). This study was carried out in accordance with the ethical guidelines and regulations of the institution. All participants provided informed consent prior to participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Government of Canada. Community-based measures to mitigate the spread of coronavirus disease (COVID-19) in Canada. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/public-health-measures-mitigate-covid-19.html 2021.
- 2.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehdi T, Morissette R. Working from home: Productivity and preferences. 2021. [Google Scholar]
- 4.Aczel B, Kovacs M, van der Lippe T, Szaszi B. Researchers working from home: benefits and challenges. PLoS One. 2021;16(3):e0249127. doi: 10.1371/journal.pone.0249127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ipsen C, van Veldhoven M, Kirchner K, Hansen JP. Six Key Advantages and Disadvantages of Working from Home in Europe during COVID-19. Int J Environ Res Public Health. 2021;18(4). 10.3390/ijerph18041826. [DOI] [PMC free article] [PubMed]
- 6.Palumbo R. Let me go to the office! An investigation into the side effects of working from home on work-life balance. Int J Public Sect Manag. 2020;33(6/7):771–790. doi: 10.1108/IJPSM-06-2020-0150. [DOI] [Google Scholar]
- 7.Eddleston KA, Mulki J. Toward understanding remote workers’ Management of Work–Family Boundaries: the complexity of workplace embeddedness. Group Org Manag. 2017;42(3):346–387. doi: 10.1177/1059601115619548. [DOI] [Google Scholar]
- 8.Oakman J, Kinsman N, Stuckey R, Graham M, Weale V. A rapid review of mental and physical health effects of working at home: how do we optimise health? BMC Public Health. 2020;20(1):1825. doi: 10.1186/s12889-020-09875-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Toniolo-Barrios M, Pitt L. Mindfulness and the challenges of working from home in times of crisis. Bus Horiz. 2021;64(2):189–197. doi: 10.1016/j.bushor.2020.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maeda M, Oe M. Mental Health Consequences and Social Issues After the Fukushima Disaster. Asia Pac J Public Health. 2017;29(2_suppl):36S–46S. doi: 10.1177/1010539516689695. [DOI] [PubMed] [Google Scholar]
- 11.Russell BS, Hutchison M, Tambling R, Tomkunas AJ, Horton AL. Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent-child relationship. Child Psychiatry Hum Dev. 2020;51(5):671–682. doi: 10.1007/s10578-020-01037-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Altieri M, Santangelo G. The psychological impact of COVID-19 pandemic and lockdown on caregivers of people with dementia. Am J Geriatr Psychiatry. 2021;29(1):27–34. doi: 10.1016/j.jagp.2020.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pierce M, Hope H, Ford T, Hatch S, Hotopf M, John A, Kontopantelis E, Webb R, Wessely S, McManus S, Abel KM. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/s2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol Med. 2020:1–10. 10.1017/s003329172000241x. [DOI] [PMC free article] [PubMed]
- 15.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. doi: 10.1016/S0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- 16.Radloff LS. The CES-D scale:a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- 17.Nguyen MT, Chan WY, Keeler C. The association between self-rated mental health status and Total health care expenditure: a cross-sectional analysis of a nationally representative sample. Medicine (Baltimore) 2015;94(35):e1410. doi: 10.1097/md.0000000000001410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 19.Miller WC, Anton HA, Townson AF. Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal Cord. 2008;46(4):287–292. doi: 10.1038/sj.sc.3102127. [DOI] [PubMed] [Google Scholar]
- 20.Khoury JE, Atkinson L, Bennett T, Jack SM, Gonzalez A. COVID-19 and mental health during pregnancy: the importance of cognitive appraisal and social support. J Affect Disord. 2021;282:1161–1169. doi: 10.1016/j.jad.2021.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonzalez A. Executive summary - Impact of the COVID-19 pandemic on Ontario Families with Children: Findings from the Initial Lockdown. 2020. https://strongfamiliesca/wp-content/uploads/2020/10/OPS-Executive-Report-EN-FINALpdf.
- 22.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 23.Carver CS. You want to measure coping but your protocol's too long: consider the brief COPE. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 24.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35(4):542–571. doi: 10.1177/0049124106292364. [DOI] [Google Scholar]
- 25.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6(1):109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 26.Dodge HH, Shen C, Ganguli M. Application of the pattern-mixture latent trajectory model in an epidemiological study with non-ignorable Missingness. J Data Sci. 2008;6(2):247–259. [PMC free article] [PubMed] [Google Scholar]
- 27.Pierce M, McManus S, Hope H, Hotopf M, Ford T, Hatch SL, John A, Kontopantelis E, Webb RT, Wessely S, Abel KM. Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry. 2021;8(7):610–619. doi: 10.1016/S2215-0366(21)00151-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Xiong J, Lipsitz O, Nasri F, Lui LMW, Gill H, Phan L, Chen-Li D, Iacobucci M, Ho R, Majeed A, McIntyre RS. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schmitz N, Holley P, Meng X, Fish L, Jedwab J. COVID-19 and depressive symptoms: a community-based study in Quebec, Canada. Can J Psychiatr. 2020;65(10):733–735. doi: 10.1177/0706743720943812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wilson JM, Lee J, Fitzgerald HN, Oosterhoff B, Sevi B, Shook NJ. Job insecurity and financial concern during the COVID-19 pandemic are associated with worse mental health. J Occup Environ Med. 2020;62(9):686–691. doi: 10.1097/jom.0000000000001962. [DOI] [PubMed] [Google Scholar]
- 31.Yang F, Dorrance K, Aitken N. The changes in health and well-being of Canadians with long-term conditions or disabilities since the start of the COVID-19 pandemic. 2020. [Google Scholar]
- 32.Alonzi S, La Torre A, Silverstein MW. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S236–S238. doi: 10.1037/tra0000840. [DOI] [PubMed] [Google Scholar]
- 33.Wessler BS, Kent DM, Konstam MA. Fear of coronavirus disease 2019-an emerging cardiac risk. JAMA Cardiol. 2020;5(9):981–982. doi: 10.1001/jamacardio.2020.2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dimidjian S, Barrera M, Jr, Martell C, Muñoz RF, Lewinsohn PM. The origins and current status of behavioral activation treatments for depression. Annu Rev Clin Psychol. 2011;7(1):1–38. doi: 10.1146/annurev-clinpsy-032210-104535. [DOI] [PubMed] [Google Scholar]
- 35.Xiao Y, Becerik-Gerber B, Lucas G, Roll SC. Impacts of working from home during COVID-19 pandemic on physical and mental well-being of office workstation users. J Occup Environ Med. 2021;63(3):181–190. doi: 10.1097/jom.0000000000002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kent EE, Ornstein KA, Dionne-Odom JN. The family caregiving crisis meets an actual pandemic. J Pain Symptom Manag. 2020;60(1):e66–e69. doi: 10.1016/j.jpainsymman.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rodrigues R, Simmons C, Schmidt AE, Steiber N. Care in times of COVID-19: the impact of the pandemic on informal caregiving in Austria. Eur J Ageing. 2021;18(2):1–11. doi: 10.1007/s10433-021-00611-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vander Elst T, Verhoogen R, Sercu M, Van den Broeck A, Baillien E, Godderis L. Not extent of telecommuting, but job characteristics as proximal predictors of work-related well-being. J Occup Environ Med. 2017;59(10):e180–e186. doi: 10.1097/jom.0000000000001132. [DOI] [PubMed] [Google Scholar]
- 39.Agha S. Mental well-being and association of the four factors coping structure model: A perspective of people living in lockdown during COVID-19. Ethics Med Public Health. 2021;16:100605. doi: 10.1016/j.jemep.2020.100605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stanisławski K. The coping Circumplex model: an integrative model of the structure of coping with stress. Front Psychol. 2019;10:694. doi: 10.3389/fpsyg.2019.00694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gurvich C, Thomas N, Thomas EH, Hudaib AR, Sood L, Fabiatos K, Sutton K, Isaacs A, Arunogiri S, Sharp G, et al. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. Int J Soc Psychiatry. 2020;20764020961790(5):540–549. doi: 10.1177/0020764020961790. [DOI] [PubMed] [Google Scholar]
- 42.Acai A, Gonzalez A, Saperson K. DPBN COVID-19 Wellness Working Group. An Iterative Approach to Promoting Departmental Wellbeing During COVID-19. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


