Abstract
Several scholars have focused on the COVID-19 case studies in Europe and USA, leaving the people in Southeast Asia with little information about the lesson learned from their own case studies. This study aims to analyses case studies through the SEIR model in three Southeast Asia countries including Singapore, Malaysia, and Indonesia. The SEIR model incorporates two types measures including social behavior and lockdowns as well as hospital preparedness. The SEIR model reveals that Malaysia, despite its relatively low testing capacity but with the application of the national lockdown, can slash the coronavirus transmission while Indonesia has still struggled to contain the COVID-19 flow owing to partial lockdowns. Singapore, at one hand, can successfully contain the coronavirus due to the national lockdowns, and the better healthcare system. With this point in mind, it is not surprising that Singapore has very low fatality rates and significantly low cases after lockdowns. Better preparedness lockdowns, and sufficient testing capacity are keys to controlling the COVID-19 flow, especially if the development of vaccines or distribution of respective vaccines is under progress.
Keywords: Coronavirus, Singapore, Malaysia, Indonesia, Southeast Asia, COVID-19, SEIR model
1. Introduction
In the past, our humankind experienced many pandemics such as Spanish flu and HIV/AIDS that led to unexpected fatalities (Roychoudhury et al., 2020). Despite our humankind experiences in the past, the COVID-19 has led to an unprecedented impact as it has severely affected almost all continents across the world, leading to multiple affected sectors such as social, economy, and health (Khairulbahri, 2021c; Roychoudhury et al., 2020).
It is not surprising that developed countries such as Germany, Italy, and Spain have faced difficulties in managing the COVID-19 flow (Wang et al., 2020). While developed countries are relatively easier in handling the COVID-19 due to their high-testing capacity and better healthcare management, developing countries such as Malaysia and Indonesia, have struggled in providing an appropriate testing capacity and accurate data (Rampal et al., 2020).
The government of Indonesia has never applied lockdowns during the COVID-19 transmission (van Empel, Mulyanto, & Wiratama, 2020). The Indonesian government argues that the best approach during the COVID-19 flow is to balance between economic and the pandemic control. In doing so, the government has never imposed national lockdowns since the first confirmed cases on March 2nd, 2020 (van Empel et al., 2020). After the government announced that two female Indonesians were positively infected by the coronavirus, the government has proposed the partial lockdowns or the large social restriction, so-called “Pembatasan Sosial Berskala Besar” (PSBB), to hamper the COVID-19 transmission (Satgas COVID-19, 2020). The government of Indonesia has also permitted the governors to apply PSBB in their own authorities if needed.
Malaysia, compared to its closest neighbor, Indonesia, has more successfully slashed the COVID-19 flow (Shah et al., 2020; Tang, 2020). Malaysia differs from Indonesia in handling the pandemic as the Malaysian government has imposed the national lockdowns while the Indonesia only have applied the partial lockdowns, so-called the large social restriction. The Malaysian first confirmed cases were on January 25th, 2020 after a woman and a kid met their male relative who was positively confirmed in Singapore (Ahmad et al., 2020). Later, owing to high infected cases, the government had imposed the first national lockdown since March 18th, 2020 until the end of May 2020 (Yusoff & Izhan, 2020).
By contrast, Singapore, an Asian developed country, has successfully slashed the COVID-19 flow and even better, Singapore has a very low Case Fatality Rate (CFR) < 0.1 % (Kayano & Nishiura, 2020). Owing to the high quality of the healthcare system, Singapore is more advanced and more successful in handling the COVID-19 flow than its neighbors (Dickens et al., 2020; Kayano & Nishiura, 2020). Due to its success, there are several scholars investigated the COVID-19 flow in Singapore. Existing studies reported some issues such as clinical analysis (Wong et al., 2020), the impacts of the containment (Lee et al., 2020, Tariq et al., 2020), and the length of stay (Sreevalsan-Nair et al., 2020, Wu et al., 2020)
Since most studies about the COVID-19 have focused on areas beyond Asia, there are limited papers dedicated to Asian case studies. Of existing Asian studies, despite their useful findings, only a few studies have focused on the Susceptible, Exposed, Infected, and Recovered (SEIR) model for Singapore, Malaysia, and Indonesia. Several studies have investigated issues such as the impacts of the pandemic on Malaysian tourism (Karim, Haque, Anis, & Ulfy, 2020), clinical analysis (Sim et al., 2020), mathematical models (Alsayed, Sadir, Kamil, & Sari, 2020; Mohd & Sulayman, 2020; Salim et al., 2020; Yusoff & Izhan, 2020), and the society preparedness (Azlan, Hamzah, Sern, Ayub, & Mohamad, 2020; Shah et al., 2020). For Indonesian cases, there are limited studies (e.g., Djalante et al., 2020; Husein, Hutabarat, Sitorus, Giawa, & Harahap, 2020) and only one study (Husein et al., 2020) discussed the epidemic model. That study (Husein et al., 2020) also did not analyse the impacts of lockdowns and social behavior in the COVID-19 transmission.
With due respect to the aforementioned studies, those studies did not separate the impacts of lockdown and social behavior. Moreover, there are very limited studies providing mechanistic models to reproduce the COVID-19 in Southeast Asian countries, especially in Malaysia and Indonesia. Those studies (e.g., Salim et al., 2020; Husein et al., 2020), for instance, discussed epidemic models based on statistical fitting which is not useful as statistical fitting models aim to fit models with observed data, lacking capability to conduct policy analysis (Holmdahl & Buckee, 2020). To the best author’s knowledge, there is no available study that develops a mechanistic SEIR model for each country. Hence, developing a mechanistic SEIR model for each country is important as another study (Holmdahl & Buckee, 2020) pointed out that mechanistic SEIR models can give users more spaces to explore possible policies.
Moreover, as disseminating information about the COVID-19 flow and its analysis is important, this study aims to develop a SEIR model for three Southeast countries including Indonesia, Singapore and Malaysia respectively. This study also investigates the roles of lockdowns and social behavior during the pandemic. For the Indonesian case study, this study also investigates the number of undetected death cases as Indonesia has a low-testing capacity. At the end, this study will compare cases in three Southeast Asian countries.
Furthermore, to the best author knowledge, there is no available study develops a mechanistic SEIR model for each country. This is important as other studies (Holmdahl & Buckee, 2020) pointed out that mechanistic SEIR model is encouraged as they can give users more spaces to explore possible policies.
2. Data and methods
Data were collected from many sources such as https://www.worldometers.info/coronavirus/ and https://coronavirus.jhu.edu (John Hopkins University’s portal for COVID-19 cases). Two available data including infected cases and death cases were collected. For each country, data from January 2020 to September 2020 were collected. Other data such as average infection and recovery time were collected from available existing studies.
This study follows other studies (Donsimoni, Glawion, Plachter, B., & Wälde, 2020; Darabi & Hosseinichimeh, 2020; Davahli, Karwowski, & Taiar, 2020; Homer & Hirsch, 2006) that developed SEIR models based on the system dynamics approach. As other studies (Ghaffarzadegan & Rahmandad, 2020; Khairulbahri, 2021a, 2021b, 2021d), this study conducts the Markov Chain Monte Carlo (MCMC) to obtain the best values for variables without defined values.
Following other studies (Khairulbahri, 2021a, 2021b), this study separates two types of measures during the pandemic including social behavior and lockdowns. They were separated as the first measure or social behavior such as physical distancing and face masking were voluntary acts during the first wave and the second measure or lockdowns are accompanied with law enforcement.
3. Results and discussion
The SEIR model for each country is displayed in Fig. 1 . As seen in Fig. 1, the SEIR model captures important dynamic patterns such as infected cases, death cases, and recovered cases. The SEIR model also highlights the roles of lockdowns, social behavior and the hospital preparedness as explained in the following paragraphs.
Fig. 1.
The SEIR model.
Compared to other existing studies (2021b, Ghaffarzadegan & Rahmandad, 2020; Khairulbahri, 2021a), this study proposes new variable so-called “the hospital preparedness”. This simplified variable aims to measure each country performance in handling infected cases, so the number of deaths is minimized. Intuitively, the higher capability of available hospital and the better healthcare systems lead to minimum death cases or low CFR. Better hospital treatment and high-skilled healthcare workers tend to minimize death cases. Eq. 1 as follows elucidates the role of the hospital treatment quality:
(1) dying rates = infected cases/infection duration*(1-the hospital treatment quality)
Other main outputs including the number of infected cases, and recoveries based on Eqs. (2), (3) as follows:
| infected rates = exposed cases / incubation time | (2) |
| recovery rates = infected cases / recovery time | (3) |
As previously mentioned, this study separates two types of measures including social behavior and lockdowns. In the model, social behavior is determined by two variables: “behavioral risk reduction” and “behavioral reduction time”. Once people do beneficial social behavior such as physical distancing, and face masks, transmission rates of the coronavirus will be minimized as seen in Eqs. 4a and 4b as follows:
| the impacts of behavioral risk reduction = IF THEN ELSE(Time> = import time + behavioral reaction time, behavioral risk reduction, 0) | (4a) |
| Transmission rate = (Ro/recovery time) *fraction of susceptible*(1-the impacts of behavioral risk reduction) | (4b) |
The second measure is lockdowns which is determined by two equations, namely, “lockdown reduction time” and "lockdown risk reduction". Please note that lockdowns are usually implemented with a delay time, so this study separates the expected and the actual impacts of lockdowns as seen in Eq. 5a and 5b respectively.
| the expected impacts of lockdown risk reduction = IF THEN ELSE(Time> = import time+"lockdown risk reduction time","lockdown risk reduction", 0) | (5a) |
| the actual impacts of lockdown risk reduction = DELAY3I ("the expected impacts of lockdown risk reduction", delaytime, "the expected impacts of lockdown risk reduction") | (5b) |
Owing to unknown parameter values, the MCMC calibration is conducted based on given ranges in Table 1 . Table 1 also provides respective supporting studies for given ranges. For Indonesia, however, estimated ranges follow existing studies from Malaysia.
Table 1.
Parameter values of the SEIR model.
| No | Names | Values | References |
|---|---|---|---|
| 1 | The first confirmed case(s) | Singapore: January 23rd, 2020 | (Tariq et al., 2020) |
| Malaysia: January 25th, 2020 | (Ahmad et al., 2020) | ||
| Indonesia: March 2nd, 2020 | (van Empel et al., 2020) | ||
| 2 | Ro (basic reproduction number) | (2−3.8) | WHO (2020) |
| 3 | Incubation time | 5 days (3−7) days | WHO (2020) |
| 4 | Infection duration (There is no available study for Indonesia, so this study assumes Indonesia has a similar infection duration and recovery time as Malaysia) | 17 (9−30) days | (Mahmud & Lim, 2020; Sim et al., 2020) |
| 5 | Recovery time | 5−15 days | (Mahmud & Lim, 2020; Sim et al., 2020) |
| 6 | Behavioral reaction time | This study sets this variable from the first confirmed cases and lockdowns. | There were campaigns of the COVID-19 threats through social media that lead to healthy behavior such as handwashing and face masks (Azlan et al., 2020; Lüdecke & von dem Knesebeck, 2020; Hoenig & Wenz, 2020) |
| The behavioral reduction time is measured between the first infection case and the beginning of the behavioral risk reduction actions. This time measurement also applies to other time measurements. | |||
| 7 | Behavioral risk reduction | This relates to individual behavior such as physical distancing and face masks. This is assumed to be between 10% and 50% | |
| 8 | Lockdown reaction time (this is measured from the first confirmed cases). | April 7th, 2020 | (Dickens et al., 2020) |
| March 18th, 2020 | (Yusoff & Izhan, 2020) | ||
| April 10th, 2020 (the first date of lockdowns) | (Satgas COVID-19, 2020) | ||
| 9 | Lockdown risk reduction | The lockdowns are very strict and enforced by law, so the efficacy is relatively high (60%–95%) | Existing studies (Dickens et al., 2020; Khairulbahri, 2021a, 2021b) pointed the beneficial impacts of lockdown |
| 10 | Fraction of asymptomatic cases | (46−62) % | Li, Pei, Chen, Song, Zhang, Yang and Shaman (2020) |
| 11 | Testing capacity (This is only additional information and not be used in the SEIR model) | Singapore: 16,000 per 1 million population | |
| Malaysia: 3500 per 1 million population | |||
| Indonesia: 200 per 1 million population (Sucahya, 2020) | |||
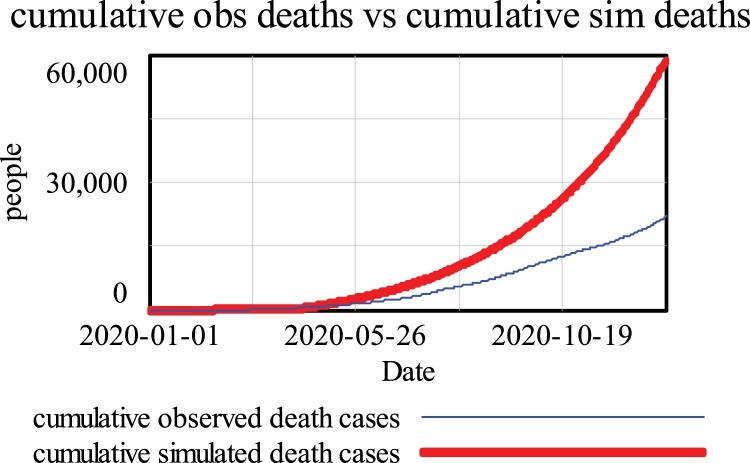
After the MCMC calibration, the best projected values for each given parameter are given in Table 2 . As seen in Fig. 2 , the SEIR model can reproduce similar patterns of death cases and infected cases for given periods. Except for Indonesia, simulated death cases were higher than observed death cases owing to undetected cases as explained in following paragraphs.
Table 2.
The best parameter values.
| No | Variables | Singapore | Malaysia | Indonesia |
|---|---|---|---|---|
| 1 | Ro (basic reproduction number) | 3.8 | 3.22 | 2.85 |
| 2 | Incubation time (days) | 3 | 5 | 5.27 |
| 3 | Infection duration (days) | 21 | 25 | 25 |
| 4 | Recovery time (days) | 5 | 5 | 5 |
| 5 | Fraction of asymptomatic cases | 10% | 25% | 60% |
| 6 | Behavioral reaction time (days) | 49 | 5 | 15 |
| 7 | Behavioral risk reduction | 11% | 10% | 16.67% |
| 8 | Lockdown risk reduction time (days) | 54 | 55 | 54 |
| 9 | Lockdown risk reduction | 65% | 71% | 55% |
| 10 | Delay time (days) | 6.57 | 6.9 | 6.8 |
| 11 | Hospital preparedness quality | 99.9% | 80% | 50% |
Fig. 2.
Simulated and observed patterns for each country Singapore (a), Malaysia (b), and Indonesia (c).
3.1. Basic reproduction number (Ro) and the efficacy of lockdown
This study finds that the Singapore’s Ro was relatively higher than that in Indonesia and Malaysia. It is probably due to high mobility in Singapore, supported by well-established public transportation. It is also shown that the efficacy of lockdown(s) in Singapore is relatively higher than that in Indonesia and Malaysia. This means that Singapore’s lockdown(s) has significantly decreased the flow of the COVID-19 than in Malaysia and Indonesia. Please note that the efficacy of lockdown(s) is represented by “lockdown risk reduction”. In case of social behavior, as shown as behavioral risk reduction, its efficacy is relatively lower than that lockdowns as well-behaved social behavior such as physical distancing and handwashing is a mitigation option once infected cases are relatively low (Piguillem & Shi, 2020).
3.2. The hospital preparedness and testing capacity
There are, however, differences in CFR and the healthcare preparedness. Indonesia has a relatively higher documented CFR (3.4%) while its counterparts, Malaysia and Singapore have lower CFRs about 0.8% and 0.1% respectively (Rampal et al., 2020). The hospital preparedness variable aims to measure how well the country capability and preparedness in handling the coronavirus flow. So, this study shows that Singapore has the highest quality of hospital preparedness about 99% while Malaysia and Indonesia have a lower quality about 80% and 35% respectively.
As the hospital preparedness leads to lower fatality rates, the hospital preparedness may include well-trained health workers, the better healthcare system, and better health facilities. So, it is not surprised if Singapore scores better in the healthcare preparedness than its counterparts.
Malaysia has a lower testing capacity than Singapore but fortunately, Malaysia can successfully slow down the COVID-19 flow and decrease fatality rates than Indonesia. A lower fatality rate and significant low infected cases than Indonesia undermines Malaysia low testing capacity. With keep this point in mind, the national lockdown or the full lockdown is an ultimate option during the pandemic, especially if there is a significant delay in vaccine distribution.
3.3. Undetected death cases and asymptomatic cases
Despite, some efforts such as the taskforce of COVID-19 and providing financial aid for affected people some have questioned about provided data by the Indonesian government. For instance, the volunteer website of the COVID-19 (www. https://kawalcovid19.id) and another study (van Empel et al., 2020) asked the government to disseminate more transparent information about cases.
As seen in Fig. 1, Indonesia has relatively similar simulated infected cases to observed infected cases. But, simulated daily death cases are relatively higher than observed daily death cases. This premise indicates a possibility of undetected death cases. Undetected death cases are a consequence of limited testing capacity and this study also informs us that an estimated of asymptomatic cases in Indonesia is about 60% of total infected cases.
It is acknowledged that providing more transparent information about cases will enhance our society awareness of the negative impacts of the COVID-19. In this regard, the Indonesian SEIR model elucidates that undetected death cases are about 75% and 150% of confirmed death cases from by May 2020 (simulated death cases are about 2800 cases and documented death cases were about 1600 cases) and by December 2020 respectively (Fig. 3). This estimate is relatively higher than that of another study (BBC, 2020) stating that undetected death cases were about 50% of confirmed death cases in the period of March-May 2020. That study (BBC, 2020) has a lower prediction as that study (BBC, 2020) was based on Jakarta area while this study is based on Indonesia at whole. Please note that Jakarta is not only Indonesia’s capital city but it also has the best hospital healthcare facilities among Indonesian provinces (Mahendradhata et al., 2017), so it is possible that percentages of undetected deaths are relatively higher outside Jakarta (Fig. 3 ).
Fig. 3.
Estimated undetected deaths in Indonesia.
Relatively higher undocumented death cases and asymptomatic cases in Indonesia underscore the importance of proper testing capacity. It is hoped that higher testing capacity and more data transparency leads to high social awareness of the vulnerability of the COVID-19 and better emergency management during the pandemic as seen in Singapore.
4. Conclusion
This study aims to investigate the COVID-19 flow in three southeast Asian countries including Singapore, Malaysia, and Indonesia. The SEIR model gives us evidence of undetected death cases and asymptomatic cases in Indonesia. Both premises, undetected death cases and asymptomatic cases, show us the importance of sufficient testing capacity. The sufficient testing capacity leads to clear pictures of the COVID-19 patterns, rising the society awareness in the vulnerability of the COVID-19.
This study also shows us that Malaysia, despite its low testing capacity compared to Singapore, can successfully slash the flow of the COVID-19 through the national lockdown. This point underlines the importance the national of lockdowns in hampering the COVID-19 flow. Furthermore, Singapore is more advanced and successful than its neighbors as Singapore has not only slashed the COVID-19 flow but also resulted in a low CFR. This point underscores the significance of well preparedness, the proper healthcare system, and the collaboration between the government and the society to handle the COVID-19 flow or other possible outbreaks in future.
The SEIR model described in this study will be a basis to investigate the impacts of vaccination on the flow of COVID-19. Thus, the effects of vaccination will be the next research.
Funding
No funding received from public, commercial or not-for-profit agencies
Competing interest
None.
Data availability
The SEIR model for each country is available on the following link: https://zenodo.org/record/4620556.
References
- Ahmad N.A., Chong Z.L., Abd Rahman S., Ghazali M.H., Nadzari E.E., Zakiman Z.…Wan Mohamed Noor W.N. First local transmission cluster of COVID-19 in Malaysia: Public health response. International Journal of Travel Medicine and Global Health. 2020;8(3):124–130. [Google Scholar]
- Alsayed A., Sadir H., Kamil R., Sari H. Prediction of epidemic peak and infected cases for COVID-19 disease in Malaysia, 2020. International Journal of Environmental Research and Public Health. 2020;17(11):4076. doi: 10.3390/ijerph17114076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azlan A.A., Hamzah M.R., Sern T.J., Ayub S.H., Mohamad E. Public knowledge, attitudes and practices towards COVID-19: A cross-sectional study in Malaysia. PLoS One. 2020;15(5) doi: 10.1371/journal.pone.0233668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC . 2020. Coronavirus: What is the true death toll of the pandemic?https://www.bbc.com/news/world-53073046 Retrieved from. [Google Scholar]
- Darabi N., Hosseinichimeh N. System dynamics modeling in health and medicine: A Systematic literature review. System Dynamics Review. 2020 [Google Scholar]
- Davahli M.R., Karwowski W., Taiar R. A system dynamics simulation applied to healthcare: A systematic review. International Journal of Environmental Research and Public Health. 2020;17(16):5741. doi: 10.3390/ijerph17165741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickens B.L., Koo J.R., Lim J.T., Park M., Quaye S., Sun H.…Cook A.R. Modelling lockdown and exit strategies for COVID-19 in Singapore. The Lancet Regional Health-Western Pacific. 2020;1 doi: 10.1016/j.lanwpc.2020.100004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djalante R., Lassa J., Setiamarga D., Sudjatma A., Indrawan M., Haryanto B.…Warsilah H. Review and analysis of current responses to COVID-19 in Indonesia: Period of January to March 2020. Progress in Disaster Science. 2020;6 doi: 10.1016/j.pdisas.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donsimoni J.R., Glawion R., Plachter B., Wälde K. Projecting the spread of COVID-19 for Germany. German Economic Review. 2020;21(2):181–216. doi: 10.1007/s10273-020-2631-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaffarzadegan N., Rahmandad H. Simulation‐based estimation of the early spread of COVID‐19 in Iran: Actual versus confirmed cases. System Dynamics Review. 2020;36(1):101–129. doi: 10.1002/sdr.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoenig K., Wenz S.E. Education, health behavior, and working conditions during the pandemic: Evidence from a German sample. European Societies. 2020:1–14. [Google Scholar]
- Holmdahl I., Buckee C. Wrong but useful—What covid-19 epidemiologic models can and cannot tell us. The New England Journal of Medicine. 2020;383(4):303–305. doi: 10.1056/NEJMp2016822. [DOI] [PubMed] [Google Scholar]
- Homer J.B., Hirsch G.B. System dynamics modeling for public health: background and opportunities. American Journal of Public Health. 2006;96(3):452–458. doi: 10.2105/AJPH.2005.062059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husein A.M., Hutabarat J.P., Sitorus J.E., Giawa T., Harahap M. Predicting the spread of the corona virus (COVID-19) in Indonesia: Approach visual data analysis and prophet forecasting. International Journal of Artificial Intelligence Research. 2020;4(2):151–161. [Google Scholar]
- Karim W., Haque A., Anis Z., Ulfy M.A. The movement control order (mco) for covid-19 crisis and its impact on tourism and hospitality sector in malaysia. International Tourism and Hospitality Journal. 2020;3(2):1–7. [Google Scholar]
- Kayano T., Nishiura H. 2020. A comparison of case fatality risk of COVID-19 between Singapore and Japan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khairulbahri M. Modeling the effect of asymptomatic cases, social distancing, and lockdowns in the first and second waves of the COVID-19 pandemic: A case study of Italy. SciMedicine Journal. 2021;3(3):265–273. [Google Scholar]
- Khairulbahri M. Understanding the first and the second waves of the COVID-19 in Germany: Is our social behavior enough to protect us from the pandemic? Walailak Journal of Science and Technology (WJST) 2021;18(15):22203–22211. [Google Scholar]
- Khairulbahri M. Multiple impacts of the COVID-19: A qualitative perspectives. International Journal of System Engineering. 2021 (in press) [Google Scholar]
- Khairulbahri M. Against the full lockdown: The COVID-19 flow in Sweden. The conference proceeding. The International System Dynamics Conference 2021; Chicago: USA; 2021. [Google Scholar]
- Lee V.J., Chiew C.J., Khong W.X. Interrupting transmission of COVID-19: Lessons from containment efforts in Singapore. Journal of Travel Medicine. 2020;27(3) doi: 10.1093/jtm/taaa039. taaa039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li R., Pei S., Chen B., Song Y., Zhang T., Yang W., Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science. 2020;368(6490):489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüdecke D., von dem Knesebeck O. Protective behavior in course of the COVID-19 outbreak—Survey results from Germany. Frontiers in Public Health. 2020;8:567. doi: 10.3389/fpubh.2020.572561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahendradhata Y., Trisnantoro L., Listyadewi S., Soewondo P., Marthias T., Harimurti P., Prawira J. 2017. The Republic of Indonesia health system review. [Google Scholar]
- Mahmud A., Lim P.Y. Applying the SEIR model in forecasting the COVID-19 trend in Malaysia: A preliminary study. medRxiv. 2020 [Google Scholar]
- Mohd M.H., Sulayman F. Unravelling the myths of R0 in controlling the dynamics of COVID-19 outbreak: A modelling perspective. Chaos, Solitons & Fractals. 2020;138 doi: 10.1016/j.chaos.2020.109943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piguillem F., Shi L. Einaudi Institute for Economics and Finance (EIEF); 2020. The optimal covid-19 quarantine and testing policies (No. 2004) [Google Scholar]
- Rampal L., Liew B.S., Choolani M., Ganasegeran K., Pramanick A., Vallibhakara S.A.…Hoe V. Battling COVID-19 pandemic waves in six South-East Asian countries: A real-time consensus review. The Medical Journal of Malaysia. 2020;75(6):613–625. [PubMed] [Google Scholar]
- Roychoudhury S., Das A., Sengupta P., Dutta S., Roychoudhury S., Choudhury A.P.…Slama P. Viral pandemics of the last four decades: Pathophysiology, health impacts and perspectives. International Journal of Environmental Research and Public Health. 2020;17(24):9411. doi: 10.3390/ijerph17249411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salim N., Chan W.H., Mansor S., Bazin N.E.N., Amaran S., Faudzi A.A.M.…Shithil S.M. COVID-19 epidemic in Malaysia: Impact of lock-down on infection dynamics. medRxiv. 2020 https://www.medrxiv.org/content/10.1101/2020.04.08.20057463v1.full-text [Google Scholar]
- Satgas COVID-19 . 2020. Satuan Tugas COVID-19 (The taskforce of COVID-19)www.satgas.co.id [Google Scholar]
- Shah A.U.M., Safri S.N.A., Thevadas R., Noordin N.K., Abd Rahman A., Sekawi Z.…Sultan M.T.H. COVID-19 outbreak in Malaysia: Actions taken by the Malaysian government. International Journal of Infectious Diseases. 2020;97:108–116. doi: 10.1016/j.ijid.2020.05.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim B.L.H., Chidambaram S.K., Wong X.C., Pathmanathan M.D., Peariasamy K.M., Hor C.P.…Goh P.P. Clinical characteristics and risk factors for severe COVID-19 infections in Malaysia: A nationwide observational study. The Lancet Regional Health-Western Pacific. 2020;4 doi: 10.1016/j.lanwpc.2020.100055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sreevalsan-Nair J., Vangimalla R.R., Ghogale P.R. Analysis and estimation of length of in-hospital stay using demographic data of COVID-19 recovered patients in Singapore. medRxiv. 2020 [Google Scholar]
- Sucahya P.K. Barriers to Covid-19 RT-PCR testing in Indonesia: A health policy perspective. Journal of Indonesian Health Policy and Administration. 2020;5(2) [Google Scholar]
- Tang K.H.D. Movement control as an effective measure against Covid-19 spread in Malaysia: An overview. Journal of Public Health. 2020:1–4. doi: 10.1007/s10389-020-01316-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tariq A., Lee Y., Roosa K., Blumberg S., Yan P., Ma S.…Chowell G. Real-time monitoring the transmission potential of COVID-19 in Singapore, March 2020. BMC Medicine. 2020;18:1–14. doi: 10.1186/s12916-020-01615-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Empel G., Mulyanto J., Wiratama B.S. Undertesting of COVID-19 in Indonesia: What has gone wrong? Journal of Global Health. 2020;10(2) doi: 10.7189/jogh.10.020306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang K., Ding L., Yan Y., Dai C., Qu M., Jiayi D.…Hao X. Modelling the initial epidemic trends of COVID-19 in Italy, Spain, Germany, and France. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0241743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. COVID-19 – A global pandemic: What do we know about SARS-CoV-2 and COVID-19?https://www.who.int/docs/default-source/coronaviruse/risk-comms-updates/update-28-covid-19-what-we-know-may-2020.pdf?sfvrsn=ed6e286c_2 [Google Scholar]
- Wong J., Goh Q.Y., Tan Z., Lie S.A., Tay Y.C., Ng S.Y.…Soh C.R. Preparing for a COVID-19 pandemic: A review of operating room outbreak response measures in a large tertiary hospital in Singapore. Canadian Journal of Anesthesia/Journal canadien d’anesthésie. 2020;67(6):732–745. doi: 10.1007/s12630-020-01620-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S., Xue L., Legido-Quigley H., Khan M., Wu H., Peng X.…Li P. Understanding factors influencing the length of hospital stay among non-severe COVID-19 patients: A retrospective cohort study in a Fangcang shelter hospital. PLoS One. 2020;15(10) doi: 10.1371/journal.pone.0240959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- www. https://kawalcovid19.id . 2020. Catatan 6 bulan Penanganan Pandemi: Buruknya Transparansi, Perparah Penanganan Pandemi.https://laporcovid19.org/2020/09/buruknya-transparansi-perparah-penanganan-pandemi/ [Google Scholar]
- Yusoff M., Izhan M. The use of system dynamics methodology in building a COVID-19 confirmed case model. Computational and Mathematical Methods in Medicine. 2020;2020 doi: 10.1155/2020/9328414. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The SEIR model for each country is available on the following link: https://zenodo.org/record/4620556.