Abstract
Background
The COVID-19 pandemic has led to significant mental health consequences for frontline health care workers (FHCWs). However, no known study has examined the prevalence, determinants, or correlates of posttraumatic growth (PTG) in this population.
Methods
Data were analyzed from a prospective cohort of FHCWs at an urban tertiary care hospital in New York City (NYC). Assessments were conducted during the spring 2020 pandemic peak (Wave 1) and seven months later (Wave 2). Multivariable logistic regression analyses were conducted to identify Wave 1 sociodemographic, occupational, and psychosocial factors associated with PTG at Wave 2, and the association between aspects of PTG with burnout and pandemic-related PTSD symptoms at Wave 2.
Results
A total 76.8% of FHCWs endorsed moderate or greater PTG; the most prevalent domains were increased appreciation of life (67.0%), improved relationships (48.7%), and greater personal strength (44.1%). Non-White race/ethnicity, greater levels of positive emotions, pandemic-related PTSD symptoms, dispositional gratitude, and feelings of inspiration were independently associated with PTG. At Wave 2, endorsement of spiritual growth during the pandemic was associated with 52% and 44% lower odds of screening positive for pandemic-related PTSD symptoms and burnout, respectively; greater improvement in relationships was associated with 36% lower odds of screening positive for burnout.
Limitations
Single institution study and use of self-report instruments.
Conclusions
Nearly 4-of-5 FHCWs report pandemic-related PTG, driven largely by salutogenic factors assessed during the pandemic surge. Interventions to bolster these factors may help promote PTG and mitigate risk for burnout and pandemic-related PTSD symptoms in this population.
Keywords: Posttraumatic growth, COVID-19, Health care workers, Burnout, Posttraumatic stress disorder
1. Introduction
The COVID-19 pandemic has led to significant negative mental health consequences for frontline health care workers (FHCWs; Preti et al., 2020). To date, however, no known study has examined the prevalence, determinants, or potential clinical significance of pandemic-related posttraumatic growth (PTG) in this population (Olson et al., 2020). PTG is defined as the positive psychological changes that may develop as a consequence of enduring highly challenging life circumstances (Tedeschi and Calhoun, 2004). These changes may include increased awareness and utilization of one's personal strengths, the development of deeper interpersonal relationships, identification of new possibilities for one's life, enhanced spiritual development, and greater appreciation of life.
Although PTG may be a meaningful end in and of itself, the presence of PTG does not preclude the presence of symptoms of posttraumatic stress disorder (PTSD), and the two phenomena often co-occur, with moderate PTSD symptoms generally associated with the highest levels of PTG (Garcia et al., 2017; Greenberg et al., 2021; Pietrzak et al., 2021; Tsai et al., 2015; Xu et al., 2019; Yang and Ha, 2019). While some studies have found that PTG is associated with improved functioning and resilience to subsequent traumatic events (Pietrzak et al., 2021; Boehm-Tabib and Gelkopf, 2021; Tsai et al., 2015), the relationship between PTG and adverse mental health outcomes is mixed, with some studies observing that PTG is unrelated to or positively associated with these outcomes (Hamam et al., 2021; Zoellner and Maercker, 2006). A recent study of nurses found that PTG was inversely correlated with burnout, a state of emotional, mental, and physical exhaustion related to work-related stress, and that this association was mediated by secondary traumatization and moderated by perceived meaning of work (Hamama-Raz et al., 2021). These findings underscore the potential significance of PTG when considering approaches to the management of burnout and related mental health issues in health care personnel.
In the current study, we analyzed data from a prospective cohort of FHCWs at a tertiary care hospital in New York City (NYC) to evaluate the prevalence and determinants of PTG, and its association with burnout and pandemic-related PTSD symptoms seven months following the spring 2020 pandemic surge in New York City (NYC). Based on prior work (Pietrzak et al., 2021; Hamama-Raz et al., 2021; Wu et al., 2019; Tsai et al., 2015; Tsai et al., 2016), we hypothesized that more than 50% of the sample would endorse PTG and that the prevalence of PTG would be higher among those who reported greater severity of COVID-19-related PTSD symptoms during the acute pandemic surge. We further expected that protective psychosocial characteristics (e.g., dispositional gratitude) assessed during this surge would be associated with PTG, and that greater PTG would be associated with a lower likelihood of screening positive for burnout and pandemic-related PTSD symptoms at the seven month assessment (Hamama-Raz et al., 2021).
2. Methods
2.1. Participants
Data at Wave 1 (W1) were collected between April 14th and May 11th, 2020 using an electronically administered anonymous survey to a purposively-selected sample of FHCWs working at The Mount Sinai Hospital (MSH), an urban tertiary care hospital in NYC. This period corresponded with the initial peak and downward slope of the epidemic curve at MSH, as defined by COVID-19 inpatient census data. Participants were eligible to receive a $25 gift card after survey completion, based on filling out a separate form to endorse study participation that was not linked to the study survey. Self-generating research codes were used to enable data linkage to future surveys while preserving anonymity (Yurek et al., 2008). The entire sample was re-contacted seven months later to complete a Wave 2 (W2) follow-up assessment and were eligible to receive a tablet, headphones, or a smart watch via raffle.
The eligible study population included health care workers most likely to be directly involved in the care of patients infected with COVID-19, either as a result of their standard practice or anticipated redeployment within the study period. Hospital and administrative leaders helped to identify the groups most likely to be involved in frontline care prior to procuring contact information for study invitation. The sample including attending-level physician faculty and house staff from multiple departments, patient-facing nurses and nurse practitioners, physician assistants, psychologists, social workers, hospital chaplains, and dietitians. Participants were excluded if email invitations went undelivered to addresses on file. The study was approved by the Institutional Review Board at the Icahn School of Medicine at Mount Sinai.
2.2. Assessments
The W1 survey included validated instruments to assess demographic, COVID-19-associated personal and occupational exposures, coping and psychosocial characteristics, and psychological symptoms. A full description of W1 is provided in Supplemental Table 1 and detailed elsewhere (Feingold et al., 2021). The W2 survey included validated instruments that assessed pandemic-related PTG and PTSD symptoms, and burnout, as described below.
2.3. Dependent variables
COVID-19 pandemic-related posttraumatic growth. The Posttraumatic Growth Inventory-Short Form (Cann et al., 2010) was used to assess pandemic-related PTG at W2 (α=0.92). Total scores and scores on the five subscales reflecting personal strength (α=0.86), relating to others (α=0.73), new possibilities (α=0.75), spiritual change (α=0.87), and appreciation of life (α=0.78) were computed. Instructions of the PTGI-SF were modified to index experiences associated with the COVID-19 pandemic: e.g., “Please indicate the degree to which you experienced these changes in your life as a result of the COVID-19 pandemic: I have a greater sense of closeness with others.” Given that the total and subscale scores were non-normally distributed (all Shapiro-Wilk test p values <0.0001), scores were dichotomized so that endorsements of “moderate,” “great,” or “very great” growth indicated a positive endorsement of PTG (Tsai et al., 2015; Pietrzak et al., 2021; Xu et al., 2019; Wu et al., 2019). A composite measure of “any PTG” was operationalized as endorsement of PTG in 1 or more of the 5 domains (Wu et al., 2019).
Burnout. Burnout was assessed at W2 using a slightly modified single-item Mini-Z measure, which is rated on a 5-point scale and asks participants to choose the best answer (1-5) as it relates to their work experience (Rohland et al., 2004). Response options range from “I enjoy my work. I have no symptoms of burnout” (score of 1) to “I feel completely burnt out. I am at the point where I may need to seek help” (score of 5). This item was additionally modified to include a definition of burnout, as follows: “Burnout is a long-term stress reaction characterized by depersonalization, including cynical or negative attitudes toward patients, emotional exhaustion, a feeling of decreased personal achievement and a lack of empathy for patients.” A positive screen for burnout was operationalized as a score of 3 (“I am definitely burning out and have one or more symptoms of burnout, e.g., emotional exhaustion”); 4 (“The symptoms of burnout that I am experiencing won't go away. I think about work frustrations a lot”); or 5 (“I feel completely burned out. I am at the point where I may need to seek help”). The Mini-Z has been validated against the emotional exhaustion subscale of the Maslach Burnout Inventory (MBI) with a correlation of 0.64 (p<0.001) (Rohland et al., 2004).
COVID-19 pandemic-related PTSD symptoms. The PTSD-Checklist for DSM-5 (PCL-5) (Weathers, 2013) was used to assess pandemic-related PTSD symptoms at W2 (α=0.95). Scores on the PCL-5 range from 0-80, with scores ≥33 indicative of a positive screen for PTSD, which has been calibrated against the gold-standard Clinician Administered PTSD Scale for DSM-5 that is used to diagnose PTSD (Weathers, 2013). Items were modified to index the COVID-19 pandemic: e.g., “In the past month, how much were you bothered by: repeated, disturbing and unwanted memories of your experiences related to the COVID-19 pandemic?”
2.4. Data analysis
Data analyses proceeded in three stages. First, descriptive statistics were computed to summarize the prevalence of positive endorsements of PTG in the full sample, as well as in FHCWs with and without a positive screen for pandemic-related PTSD symptoms. Second, three multivariable logistic regressions were conducted to identify: (a) W1 variables associated with PTG at W2; and (b) W2 endorsements of aspects of PTG associated with positive screens for burnout and pandemic-related PTSD symptoms at W2. These analyses adjusted for a broad range of background characteristics and risk factors (see Table 1 ). Third, for the first regression model, planned secondary analyses of multi-faceted constructs (e.g., protective psychosocial characteristics) were conducted to identify specific indicator variables from these constructs that were independently associated with PTG.
Table 1.
Demographic, occupational, and psychosocial factors associated with PTG in FHCWs.
| Bivariate association with posttraumatic growth (r) | Multivariable model predicting posttraumatic growth (R2=0.19) | |
|---|---|---|
| Demographic and occupational characteristics | ||
| Age | -0.02 | - |
| Male gender | -0.09** | 0.66 (0.41-1.07) |
| White, non-Hispanic race/ethnicity | -0.10** | 0.63 (0.41-0.96)* |
| Married/partnered | -0.07 | - |
| RN vs. other profession | 0.12** | 1.05 (0.63-1.75) |
| Supervisory role during pandemic | -0.08* | 0.74 (0.46-1.20) |
| Years in practice | 0.02 | - |
| Perceived preparedness | -0.03 | - |
| Exposures and mental health | ||
| Pre-pandemic burnout | 0.09* | 1.24 (0.78-1.98) |
| Pre-pandemic mental disorder | -0.03 | - |
| COVID-19-associated stressors (wave-1) | 0.14*** | 1.16 (0.90-1.50) |
| COVID-19-associated stressors (wave-2) | 0.08* | 1.10 (0.86-1.40) |
| Positive emotions | 0.09** | 1.03 (1.01-1.07)* |
| Negative emotions | 0.10** | 1.02 (0.98-1.06) |
| COVID-19-associated PTSD symptoms | 0.14*** | 1.13 (1.06-1.21)*** |
| Depressive symptoms | 0.17*** | 0.98 (0.90-1.06) |
| Generalized anxiety symptoms | 0.11** | 1.04 (0.95-1.13) |
| Mental health treatment during pandemic | -0.03 | - |
| Coping and support during pandemic surge | ||
| Self-sufficient coping strategies | 0.06 | - |
| Socially-supported coping strategies | -0.01 | - |
| Avoidant coping strategies | -0.05 | - |
| Positive psychological characteristics | 0.16*** | 1.34 (1.03-1.76)* |
| Perceived social support | -0.02 | - |
| Work pride and meaning | 0.17*** | 1.45 (1.11-1.88)** |
| Leadership support and value | 0.06 | - |
| Restorative behaviors during pandemic surge | ||
| Sleep hours | -0.05 | - |
| Physical exercise | -0.01 | - |
| Meditation | 0.11** | 1.08 (0.92-1.27) |
| Artistic activities | 0.10** | 1.09 (0.96-1.24) |
| Hobbies/games | 0.00 | - |
| Media consumption | -0.03 | - |
| Resources during pandemic surge | ||
| Food and supplies | 0.04 | - |
| Predeployment training and communication | 0.01 | - |
| Stress reduction and support | 0.11** | 1.24 (0.89-1.72) |
| Housing and financial support | 0.00 | - |
| Increase in PTSD symptom severity | 0.03 | - |
Note: All variables were assessed at Wave 1 with the exception of W2 COVID-19-related stressors and change in PTSD symptom severity. PTG was assessed at Wave 2.
3. Results
3.1. Response rate
Of the 6,026 presumed FHCWs, 3,360 completed the W1 survey (55.8%), of which 2,579 (76.8%) endorsed having frontline responsibilities in caring for COVID-19 patients; median completion date=04/21/20; range=04/14/20-05/11/20. A total of 787 (30.5%) FHCWs completed the follow-up assessment (median completion date=12/6/20; range=11/19/20-1/10/21). Distributions of age, sex, and profession between the full W1 and W2 samples did not differ (all χ2>1.52, all p's>0.22).
3.2. Prevalence of burnout and pandemic-related PTSD symptoms at Wave 2
At the W2 assessment, 351 FHCWs (44.6%) screened positive for burnout and 108 (13.7%) for pandemic-related PTSD symptoms.
3.3. Prevalence of PTG
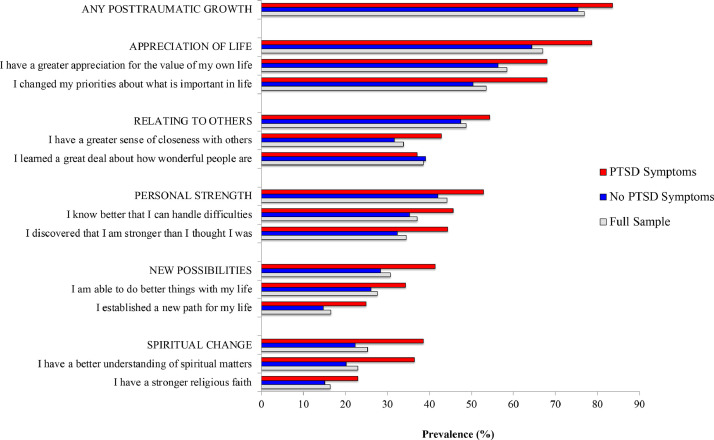
Figure 1 shows the prevalence of W2 PTG by W1 screening status for pandemic-related PTSD symptoms. In the full sample, 76.8% endorsed at least moderate levels of PTG, the most prevalent domains being greater appreciation of life (67.0%), improved relationships (48.7%), and personal strength (44.1%). FHCWs who screened positive for pandemic-related PTSD symptoms at W1 were significantly more likely than those who screened negative to endorse all aspects of PTG at W2 except “Relating to Others” and “I learned a great deal about how wonderful people are” (All χ2>3.90, all p's<0.05).
Fig. 1.
Prevalence of posttraumatic growth at Wave 2 in frontline health care workers responding to the COVID-19 pandemic.
3.4. Collinearity diagnostics
Collinearity diagnostics did not reveal the presences of multicollinearity in any of the regression models, with variance inflation factors for all independent variables <3.
3.5. Factors associated with PTG
Table 1 shows bivariate correlations and results of a multivariable analysis of W1 factors associated with W2 endorsement of PTG. In the multivariable model, non-White race/ethnicity, and higher scores on measures of positive emotions (i.e., inspiration, OR=1.24, 95%CI=1.02-1.53), pandemic-related PTSD symptoms (i.e., severity of intrusive thoughts about the pandemic, OR=1.25, 95%CI=1.02-1.53), dispositional gratitude (OR=1.35, 95%CI=1.02-1.78), and greater feelings of being inspired by role-models (OR=1.74, 95%CI=1.26-2.41) emerged as independent W1 predictors of W2 PTG.
3.6. Association between PTG and positive screens for burnout and PTSD symptoms at W2
After adjustment for all the variables shown in Table 1, endorsement of pandemic-related spiritual changes (i.e., moderate or greater perceived growth on one or both of the Spiritual Changes items of the PTGI-SF) was associated with a 44% lower odds of screening positive for burnout (OR=0.56, 95%CI=0.35-0.90) and 52% lower odds of screening positive for pandemic-related PTSD symptoms (OR=0.48, 95%CI=0.24-0.99). Greater improvement in interpersonal relationships (i.e., moderate or greater perceived growth on one or both of the Relating to Others items of the PTGI-SF) was additionally associated with 36% lower odds of screening positive for burnout (OR=0.64, 95%CI=0.43-0.97). Endorsements of all other aspects of PTG were not significantly associated with these measures (all Wald χ2<3.78, all p's>0.05).
4. Discussion
This study examined the prevalence, determinants, and potential clinical significance of COVID-19 pandemic-related PTG in FHCWs. Results revealed that, seven months following the initial pandemic surge in NYC, 77% of FHCWs reported pandemic-related PTG, particularly in the domains of appreciation of life, improved personal relationships, and increased sense of personal strength. This prevalence of PTG is consistent with the 77% observed in a recent population-based study of American and Canadian adults during the pandemic (Asmundson et al., 2021) and markedly higher than the 53% observed among trauma survivors in a recent meta-analysis (Wu et al., 2019) and in a recent study of a national cohort of U.S. military veterans during the pandemic (43.3%; Pietrzak et al., 2021).
Consistent with prior work (Tsai et al., 2015; Garcia et al., 2017; Greenberg et al., 2021; Pietrzak et al., 2021; Xu et al., 2019; Yang and Ha, 2019). PTG was more prevalent in FHCWs with greater severity of pandemic-related PTSD symptoms (e.g., intrusive thoughts) during the acute pandemic surge. This finding aligns with prior findings suggesting that the processing of traumatic memories may be a necessary impetus for PTG, as it may prompt more purposeful and reflective rumination (Tsai et al., 2015; Wu et al., 2019; Tsai et al., 2016). Indeed, some level of intrusive rumination—a core symptom of PTSD—is often required for more reflective and constructive rumination to occur, and this transition from intrusive and automatic thoughts to more organized, deliberate, and controlled reflection may help promote PTG (Garcia et al., 2017). This finding may help inform psychoeducation programs to differentiate types of rumination and foster greater hope for FHCWs who perceive distressing thoughts and emotions as problematic, rather than as potentially helpful in facilitating recovery from PTSD and related symptoms. Importantly, greater social support has been found to moderate the relationship between deliberate rumination and PTG (Xu et al., 2019), suggesting that reflective processing of traumatic memories in a supportive context may be particularly helpful in facilitating PTG.
Greater feelings of inspiration—both in general and by role models—and greater dispositional gratitude at W1 were associated with a greater likelihood of W2 PTG. These findings corroborate prior work demonstrating that the cultivation of positive emotions in the midst of stressful circumstances is linked to greater PTG (Laslo-Roth et al., 2020; Levine et al., 2009; Rodríguez-Rey and Alonso-Tapia, 2019; Tsai and Pietrzak, 2017). This finding also underscores the potential utility of health system, team-based, and individual interventions aimed at helping health care workers cultivate positive emotions in real-time during a crisis. For example, efforts at both individual and organizational levels to deliberately understand and encourage reflection as to how one has been affected by the pandemic; identify role-models who have grown through adversity; encourage viewing the pandemic as both a crisis and as an opportunity to improve on the status quo; and assess how the pandemic may have helped build connections with the broader community may help foster PTG in FHCWs (Morganstein and Flynn, 2021; Olson et al., 2020).
FHCWs who reported developing positive spiritual changes during the pandemic had 52% and 44% lower odds of screening positive for pandemic-related PTSD symptoms and burnout, respectively. Further, those who reported developed a greater pandemic-related improvement in interpersonal relationships had 36% lower odds of screening positive for burnout. Collectively, these findings are consistent with recent studies of nurses which found an inverse association between PTG and burnout (Hamama-Raz et al., 2021), and that religion/spirituality is negatively associated with burnout (Harris and Tao, 2021; Zhang et al., 2019). They also align with prior research underscoring the importance of social support on burnout risk in health care personnel (Bellanti et al., 2021; Cyr et al., 2021; Galanis et al., 2021; Ruisoto et al., 2020), and that spirituality, particularly positive spiritual coping, is associated with lower rates of PTSD and related mental health outcomes (González-Sanguino et al., 2020; Sharma et al., 2017; Smith-MacDonald et al., 2017). Given that PTG, burnout, and PTSD symptoms were both assessed cross-sectionally at W2 in the current study, it is possible that these aspects of PTG may help mitigate risk for these outcomes, that lower severity of burnout or PTSD symptoms may lead to greater PTG in these domains, or that these variables may evolve in a complex and dynamic manner. While longitudinal studies with repeated assessments of PTG and mental health outcomes are needed to disentangle these associations, results of the current study underscore the importance of examining how domains of PTG relate to mental health outcomes in FHCWs and other trauma-affected populations.
In light of data suggesting that burnout is a prevalent and disabling occupational concern that has threatened the well-being of health care workers well before COVID-19 (Dzau et al., 2020) and that PTSD symptoms may be elevated in FHCWs (Feingold et al., 2021), interventions aimed at simultaneously reducing burnout and PTSD symptoms, and fostering PTG may be helpful in promoting the mental health of FHCWs. For example, investment in workplace and clinical interventions that focus on relationship-building (e.g. peer-support and buddy programs, strengths-focused programs that foster community; Albott et al., 2020; Morganstein and Flynn, 2021) and meaning in work (Hamama-Raz et al., 2021) may help bolster resilience to pandemic-related stress and possibly PTG, though further research is needed to evaluate the effectiveness of these interventions in this population.
Limitations of this study are that it was conducted at a single institution with a relatively low W2 response rate, and that it utilized brief self-report instruments to assess psychopathology and PTG. Assessment of PTSD symptoms also did not evaluate whether occupational and personal exposures qualified as Criterion A traumas (i.e., person was exposed to death, threatened death, actual or threatened serious injury or sexual violence), which is required for a diagnosis of PTSD (Van Overmeire, 2020). Further, W2 PTG, burnout, and PTSD symptoms were assessed concurrently, so the temporal/causal associations among these variables is unclear. Longer-term follow-up studies with repeated assessments (e.g., autoregressive cross-lagged panel designs; Whealin et al., 2020) will be helpful in elucidating whether aspects of PTG may mitigate risk for these outcomes or whether aspects of PTG change as a consequence of living with these conditions. Despite these limitations, notable strengths of this study include the rapid deployment of the W1 survey in the midst of the acute phase of the initial pandemic surge, prospective cohort design, the assessment of a broad range of psychopathology and salutogenic measures, and the identification of acute-phase targets that may help facilitate PTG in FHCWs.
Given that PTG may be both constructive and illusory in nature (Asmundson et al., 2021; Zoellner and Maercker, 2006) and take months-to-years to develop, more longitudinal studies are needed to elucidate the potential role of PTG in recovering from pandemic-related distress in FHCWs. Further research is also needed to replicate these results in other samples of FHCWs; identify biopsychosocial mechanisms that may help facilitate PTG; and evaluate the efficacy of interventions aimed at targeting PTG-promoting factors in helping facilitate PTG and mitigate risk of burnout, PTSD symptoms, and related mental health outcomes in FHCWs and other trauma-exposed populations.
Contributors
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Feingold & Pietrzak.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Pietrzak.
Administrative, technical, or material support: Ripp.
Supervision: Ripp, Southwick, Pietrzak.
Funding sources
This study was supported by internal funding devoted to COVID-19-associated projects from the Icahn School of Medicine at Mount Sinai.
Preparation of this report was supported in part by the US Department of Veterans Affairs National Center for Posttraumatic Stress Disorder (Dr. Pietrzak).
Jordyn H. Feingold was grant funded by NIH TL1 grant TR001434. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval.
Declaration of Competing Interest
Feder, A: Dr. Feder is named co-inventor on an issued patent in the United States, and several issued patents outside the U.S., filed by the Icahn School of Medicine at Mount Sinai (ISMMS) for the use of ketamine as a therapy for PTSD. This intellectual property has not been licensed. Southwick, S: Dr. Southwick receives royalties for a book on resilience published by Cambridge University Press.
Acknowledgements
The authors thank all of the frontline health care workers at the Mount Sinai Hospital who participated in this study. They also acknowledge the COVID-19 Psychological Impact Study Team for their contributions to this project: Chi C. Chan, PhD; Carly A. Kaplan, BS; Halley Kaye-Kauderer, BA; Jaclyn Verity, MPH; Larissa Burka, RN; James W. Murrough, MD, PhD; and Dennis Charney, MD.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2021.09.032.
Appendix. Supplementary materials
References
- Albott C.S., Wozniak J.R., McGlinch B.P., Wall M.H., Gold B.S., Vinogradov S. Battle Buddies: Rapid Deployment of a Psychological Resilience Intervention for Health Care Workers During the COVID-19 Pandemic. Anesth. Analg. 2020;131:43–54. doi: 10.1213/ANE.0000000000004912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asmundson G.J.G., Paluszek M.M., Taylor S. Real versus illusory personal growth in response to COVID-19 pandemic stressors. J. Anxiety Disord. 2021;81 doi: 10.1016/j.janxdis.2021.102418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellanti F., Lo Buglio A., Capuano E., Dobrakowski M., Kasperczyk A., Kasperczyk S., Ventriglio A., Vendemiale G. Factors Related to Nurses’ Burnout during the First Wave of Coronavirus Disease-19 in a University Hospital in Italy. Int. J. Environ. Res. Public Health. 2021;18 doi: 10.3390/ijerph18105051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehm-Tabib E., Gelkopf M. Educational Publishing Foundation, US; 2021. Posttraumatic growth: A deceptive illusion or a coping pattern that facilitates functioning? pp. 193–201. [DOI] [PubMed] [Google Scholar]
- Cann A., Calhoun L.G., Tedeschi R.G., Taku K., Vishnevsky T., Triplett K.N., Danhauer S.C. A short form of the Posttraumatic Growth Inventory. Anxiety Stress Coping. 2010;23:127–137. doi: 10.1080/10615800903094273. [DOI] [PubMed] [Google Scholar]
- Cyr S., Marcil M.J., Marin M.F., Tardif J.C., Guay S., Guertin M.C., Rosa C., Genest C., Forest J., Lavoie P., Labrosse M., Vadeboncoeur A., Selcer S., Ducharme S., Brouillette J. Factors Associated With Burnout, Post-traumatic Stress and Anxio-Depressive Symptoms in Healthcare Workers 3 Months Into the COVID-19 Pandemic: An Observational Study. Front. Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.668278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dzau V.J., Kirch D., Nasca T. Preventing a Parallel Pandemic — A National Strategy to Protect Clinicians’ Well-Being. N. Engl. J. Med. 2020;383:513–515. doi: 10.1056/NEJMp2011027. [DOI] [PubMed] [Google Scholar]
- Feingold J.H., Peccoralo L., Chan C.C., Kaplan C.A., Kaye-Kauderer H., Charney D., Verity J., Hurtado A., Burka L., Syed S.A., Murrough J.W., Feder A., Pietrzak R.H., Ripp J. Psychological Impact of the COVID-19 Pandemic on Frontline Health Care Workers During the Pandemic Surge in New York City. Chronic Stress (Thousand Oaks) 2021;5 doi: 10.1177/2470547020977891. 2470547020977891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galanis P., Vraka I., Fragkou D., Bilali A., Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J. Adv. Nurs. 2021;77:3286–3302. doi: 10.1111/jan.14839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia F.E., Duque A., Cova F. The four faces of rumination to stressful events: A psychometric analysis. Psychol. Trauma. 2017;9:758–765. doi: 10.1037/tra0000289. [DOI] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental Health Consequences of the Coronavirus 2020 Pandemic (COVID-19) in Spain. A Longitudinal Study. Front. Psychiatry. 2020;11 doi: 10.3389/fpsyt.2020.565474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg J., Tsai J., Southwick S.M., Pietrzak R.H. Can military trauma promote psychological growth in combat veterans? Results from the national health and resilience in veterans study. J. Affect. Disord. 2021;282:732–739. doi: 10.1016/j.jad.2020.12.077. [DOI] [PubMed] [Google Scholar]
- Hamam A.A., Milo S., Mor I., Shaked E., Eliav A.S., Lahav Y. Peritraumatic reactions during the COVID-19 pandemic - The contribution of posttraumatic growth attributed to prior trauma. J. Psychiatr. Res. 2021;132:23–31. doi: 10.1016/j.jpsychires.2020.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamama-Raz Y., Hamama L., Pat-Horenczyk R., Stokar Y.N., Zilberstein T., Bron-Harlev E. Posttraumatic growth and burnout in pediatric nurses: The mediating role of secondary traumatization and the moderating role of meaning in work. Stress and Health. 2021;37:442–453. doi: 10.1002/smi.3007. [DOI] [PubMed] [Google Scholar]
- Harris S., Tao H. The Impact of US Nurses’ Personal Religious and Spiritual Beliefs on Their Mental Well-Being and Burnout: A Path Analysis. J. Relig. Health. 2021:1–20. doi: 10.1007/s10943-021-01203-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laslo-Roth R., George-Levi S., Margalit M. Social participation and posttraumatic growth: The serial mediation of hope, social support, and reappraisal. J. Commun. Psychol. 2020 doi: 10.1002/jcop.22490. [DOI] [PubMed] [Google Scholar]
- Levine S.Z., Laufer A., Stein E., Hamama-Raz Y., Solomon Z. Examining the relationship between resilience and posttraumatic growth. J. Trauma Stress. 2009;22:282–286. doi: 10.1002/jts.20409. [DOI] [PubMed] [Google Scholar]
- Morganstein J.C., Flynn B.W. Enhancing Psychological Sustainment & Promoting Resilience in Healthcare Workers During COVID-19 & Beyond: Adapting Crisis Interventions from High-Risk Occupations. J. Occup. Environ. Med. 2021 doi: 10.1097/JOM.0000000000002184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson K., Shanafelt T., Southwick S. Pandemic-Driven Posttraumatic Growth for Organizations and Individuals. JAMA. 2020;324:1829–1830. doi: 10.1001/jama.2020.20275. [DOI] [PubMed] [Google Scholar]
- Pietrzak R.H., Tsai J., Southwick S.M. Association of Symptoms of Posttraumatic Stress Disorder With Posttraumatic Psychological Growth Among US Veterans During the COVID-19 Pandemic. JAMA Netw. Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti E., Di Mattei V., Perego G., Ferrari F., Mazzetti M., Taranto P., Di Pierro R., Madeddu F., Calati R. The Psychological Impact of Epidemic and Pandemic Outbreaks on Healthcare Workers: Rapid Review of the Evidence. Curr. Psychiatry Rep. 2020;22:43. doi: 10.1007/s11920-020-01166-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Rey R., Alonso-Tapia J. Predicting Posttraumatic Growth in Mothers and Fathers of Critically Ill Children: A Longitudinal Study. J. Clin. Psychol. Med. Set. 2019;26:372–381. doi: 10.1007/s10880-018-9594-3. [DOI] [PubMed] [Google Scholar]
- Rohland B.M., Kruse G.R., Rohrer J.E. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress and Health. 2004;20:75–79. [Google Scholar]
- Ruisoto P., Ramírez M.R., García P.A., Paladines-Costa B., Vaca S.L., Clemente-Suárez V.J. Social Support Mediates the Effect of Burnout on Health in Health Care Professionals. Front. Psychol. 2020;11 doi: 10.3389/fpsyg.2020.623587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma V., Marin D.B., Koenig H.K., Feder A., Iacoviello B.M., Southwick S.M., Pietrzak R.H. Religion, spirituality, and mental health of U.S. military veterans: Results from the National Health and Resilience in Veterans Study. J. Affect. Disord. 2017;217:197–204. doi: 10.1016/j.jad.2017.03.071. [DOI] [PubMed] [Google Scholar]
- Smith-MacDonald L., Norris J.M., Raffin-Bouchal S., Sinclair S. Spirituality and Mental Well-Being in Combat Veterans: A Systematic Review. Mil. Med. 2017;182:e1920–e1940. doi: 10.7205/MILMED-D-17-00099. [DOI] [PubMed] [Google Scholar]
- Tedeschi R., Calhoun L. Target article: posttraumatic growth. Psychol. Inquiry. 2004;15:1–18. [Google Scholar]
- Tsai J., El-Gabalawy R., Sledge W.H., Southwick S.M., Pietrzak R.H. Post-traumatic growth among veterans in the USA: results from the National Health and Resilience in Veterans Study. Psychol. Med. 2015;45:165–179. doi: 10.1017/S0033291714001202. [DOI] [PubMed] [Google Scholar]
- Tsai J., Mota N.P., Southwick S.M., Pietrzak R.H. What doesn’t kill you makes you stronger: A national study of U.S. military veterans. J. Affect. Disord. 2016;189:269–271. doi: 10.1016/j.jad.2015.08.076. [DOI] [PubMed] [Google Scholar]
- Tsai J., Pietrzak R.H. Trajectories of posttraumatic growth among US military veterans: a 4-year nationally representative, prospective cohort study. Acta Psychiatr. Scand. 2017;136:483–492. doi: 10.1111/acps.12800. [DOI] [PubMed] [Google Scholar]
- Van Overmeire R. The Methodological Problem of Identifying Criterion A Traumatic Events During the COVID-19 Era: A Commentary on Karatzias et al. (2020) J. Trauma Stress. 2020;33:864–865. doi: 10.1002/jts.22594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers, F.W., Litz, B.T., Keane, T.M., Palmieri, P.A., Marx, B.P., & Schnurr, P.P., 2013. The PTSD Checklist for DSM-5 (PCL-5), www.ptsd.va.gov.
- Whealin J.M., Pitts B., Tsai J., Rivera C., Fogle B.M., Southwick S.M., Pietrzak R.H. Dynamic interplay between PTSD symptoms and posttraumatic growth in older military veterans. J. Affect. Disord. 2020;269:185–191. doi: 10.1016/j.jad.2020.03.020. [DOI] [PubMed] [Google Scholar]
- Wu X., Kaminga A.C., Dai W., Deng J., Wang Z., Pan X., Liu A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. J. Affect. Disord. 2019;243:408–415. doi: 10.1016/j.jad.2018.09.023. [DOI] [PubMed] [Google Scholar]
- Xu W., Jiang H., Zhou Y., Zhou L., Fu H. Intrusive Rumination, Deliberate Rumination, and Posttraumatic Growth Among Adolescents After a Tornado: The Role of Social Support. J. Nerv. Ment. Dis. 2019;207:152–156. doi: 10.1097/NMD.0000000000000926. [DOI] [PubMed] [Google Scholar]
- Yang S.K., Ha Y. Predicting Posttraumatic Growth among Firefighters: The Role of Deliberate Rumination and Problem-Focused Coping. Int. J. Environ. Res. Public Health. 2019;16 doi: 10.3390/ijerph16203879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurek L.A., Vasey J., Sullivan Havens D. The use of self-generated identification codes in longitudinal research. Eval. Rev. 2008;32:435–452. doi: 10.1177/0193841X08316676. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Wu X., Wan X., Hayter M., Wu J., Li S., Hu Y., Yuan Y., Liu Y., Cao C., Gong W. Relationship between burnout and intention to leave amongst clinical nurses: The role of spiritual climate. J. Nurs. Manage. 2019;27:1285–1293. doi: 10.1111/jonm.12810. [DOI] [PubMed] [Google Scholar]
- Zoellner T., Maercker A. Posttraumatic growth in clinical psychology - a critical review and introduction of a two component model. Clin. Psychol. Rev. 2006;26:626–653. doi: 10.1016/j.cpr.2006.01.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.