Abstract
Aims
To investigate the incidence and presumed aetiologies of fourth cranial nerve (CN4) palsy in Korea
Methods
Using the nationally representative dataset of the Korea National Health Insurance Service–National Sample Cohort from 2006 to 2015, newly developed CN4 palsy cases confirmed by a preceding disease-free period of ≥4 years were identified. The presumed aetiology of CN4 palsy was evaluated based on comorbidities around the CN4 palsy diagnosis.
Results
Among the 1,108,292 cohort subjects, CN4 palsy newly developed in 390 patients during 10-year follow-up, and the overall incidence of CN4 palsy was 3.74 per 100,000 person-years (95% confidence interval, 3.38–4.12). The incidence of CN4 palsy showed a male preponderance in nearly all age groups, and the overall male-to-female ratio was 2.30. A bimodality by age-group was observed, with two peaks at 0–4 years and at 75–79 years. The most common presumed aetiologies were vascular (51.3%), congenital (20.0%), and idiopathic (18.5%). The incidence rate of a first peak for 0–4 years of age was 6.17 per 100,000 person-years, and cases in this group were congenital. The second peak incidence rate for 75–79 years of age was 11.81 per 100,000 person-years, and the main cause was vascular disease. Strabismus surgery was performed in 48 (12.3%) patients, most of whom (72.9%) were younger than 20 years.
Conclusion
The incidence of CN4 palsy has a male predominance in Koreans and shows bimodal peaks by age. The aetiology of CN4 palsy varies according to age-groups.
Subject terms: Ocular motility disorders, Epidemiology
Introduction
Fourth cranial nerve (CN4) palsy, also known as trochlear nerve palsy or superior oblique palsy, is one of the most common paralytic strabismus encountered in ophthalmology clinics [1]. The CN4 palsy can be caused by congenital or acquired vascular diseases, head trauma, and intracranial neoplasm [2–4]. The superior oblique muscle acts to intort, depress, and abduct the eyeball; thus, CN4 palsy may cause vertical deviation, abnormal head positioning or torsional symptoms [5]. Small deviations may be treated with observation or prisms, however, surgeries are required for larger deviations [5].
To date, CN4 palsy has been investigated mostly in tertiary referral centres, and there are various studies reporting on the aetiology, clinical features, and surgical techniques or outcomes [2, 3, 6–8]. The epidemiology of CN4 palsy in the general population has only been reported in limited studies that presented the incidence rates of CN4 palsy ranging from 2.7 to 6.3 per 100,000 person-years [9–12]. However, most of these population-based studies were performed in the United States [9, 11, 12], and the racial differences in the epidemiology of CN4 palsy remain unclear. Thus, it would be valuable to investigate the epidemiology of CN4 palsy in more detail in Asians.
In this study, we aimed to establish the epidemiology of CN4 palsy in the general Korean population, regarding its incidence, prevalence, and aetiology. To meet this need, we accessed the Korea National Health Insurance Service–National Sample Cohort (NHIS-NSC) database and analysed the nationally representative dataset of Koreans, targeting the in-care population of the NHIS system [13]. To our knowledge, this is one of the largest population-based studies on the incidence of CN4 palsy.
Methods
Dataset and study population
The NHIS of Korea has covered about 97% of the people in Korea since 1963, leaving the remaining 3% insured by the Medical Aid program [13, 14]. All claims in the NHIS have been recorded in a centralised database (National Health Information Database [NHID]), and include information regarding patient demographics, diagnostic codes, procedure types, drug prescriptions, and related costs [13, 14]. For diagnostic codes, the NHIS uses the Korean Classification of Diseases (KCD) system, which is based on the International Classification of Diseases, 10th Edition (ICD-10) [13, 14].
The NHIS-NSC database was constructed for research purposes in 2014; it consisted of ~1 million individuals observed from 2002 to 2013 [13]. In 2017, a second version of the cohort, the NHIS-NSC 2006–2015, was released with a retrospectively extended observation period from 2002 to 2005 [15]. From the target population (48,222,537 individuals in the 2006 NHID), a nationwide representative sample cohort of ~1 million participants (~2.2% of the Korean population) was randomly selected using a systematic, stratified, random sampling method with 2142 strata [15]. The strata were constructed using age (17 groups; 5-year age groups younger than 80, and 80 years or older), sex (male and female), residential area (three regions), and income level (21 types) [15].
The present study used the second version of NHIS-NSC covering the period of 2002–2015. A participation flow chart is presented in Fig. 1. During the follow-up period, the cohort was dynamically updated annually by adding a representative sample of newborns to compensate for annual disqualifications including death [15]. This retrospective cohort study was approved by the Institutional Review Board (IRB) of Hallym University Medical Center (IRB No. 2018-06-001), which waived the requirement for informed consent. The study adhered to the tenets of the Declaration of Helsinki.
Fig. 1. A flowchart of identifying newly developed fourth cranial nerve palsy.
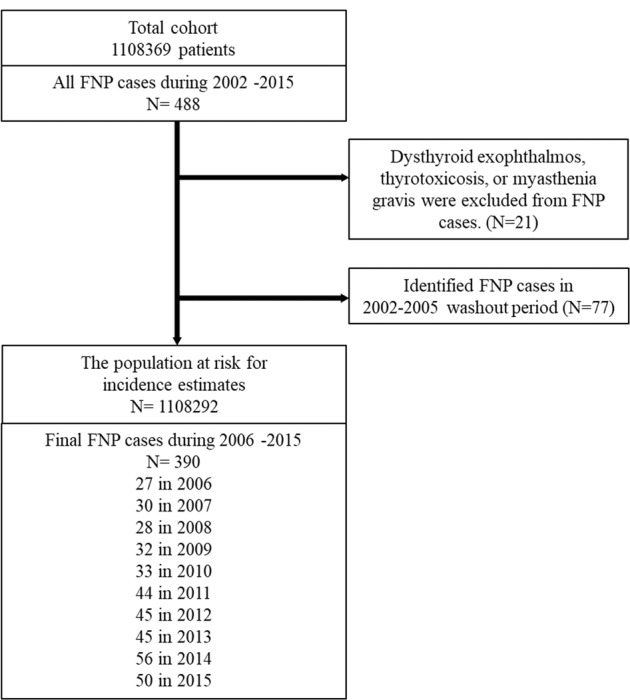
The number of subjects at each stage of the investigation is shown.
Definition of CN4 palsy cases and surgeries
Since almost all Koreans are covered by the NHIS, and the NHIS-NSC dataset is a representative sample of the NHIS database, we assumed that the prevalent cases in the population can be estimated using the cases diagnosed in the NHIS-NSC dataset. Cases of CN4 palsy were defined as claims using the KCD code for fourth cranial (trochlear) nerve palsy (H491) assigned by ophthalmologists, neurologists, or neurosurgeons. An incident of CN4 palsy was defined as the first CN4 palsy diagnosis for each subject based on the earliest diagnosis date. Among subjects diagnosed with CN4 palsy, those diagnosed with dysthyroid exophthalmos (H062), thyrotoxicosis (hyperthyroidism, E05), or myasthenia gravis (G700) at the same time were excluded in consideration of misdiagnosis. For the incidence, the year 2006 was used as the index year for the starting cohort, and subjects were identified with new CN4 palsy having a preceding 4-year disease-free washout period (2002–2005) (Fig. 1).
The incidence and prevalence of CN4 palsy were investigated by age group, sex, and the year of diagnosis. Age groups were divided by 5-year intervals. The annual incidence was calculated starting on January 1 of each year from 2006 to 2015. The annual prevalence was calculated using the total number of cases that were confirmed in a clinical practice per year and the total population qualified for NHIS-NSC in each year [16]. To estimate the annual prevalence, we defined prevalent cases as those who visited clinics at least once for each year in this study [16]. In other words, prevalent cases needed a clinical practice or a check-up once a year under the diagnosis of CN4 palsy [16]. Surgery for CN4 palsy was determined if the subject with CN4 palsy underwent strabismus surgery during the follow-up period, based on the Korean Electronic Data Interchange codes for strabismus surgeries (S5173, 5174, 5175, or 5176). The surgery code depends on simplicity and complexity, single and multiple.
Evaluation of CN4 palsy aetiologies
The aetiologies of CN4 palsy were presumed using the comorbidities for the diagnosis of CN4 palsy, because detailed medical records, including neuroimaging data of each subject, are not available in the NHIS-NSC database [17]. We investigated the aetiologies of CN4 palsy based on the principal diagnostic codes for comorbidities registered within six months before and two weeks after the CN4 palsy diagnosis. The potential CN4 palsy aetiologies considered in this study included vascular diseases, trauma, intracranial neoplasm, presumed congenital condition, and idiopathic [9].
Vascular aetiology was presumed if the patient had hypertension (I10-15), diabetes mellitus (DM; E11-14), ischaemic heart diseases (I20-25), peripheral vascular disease (I70, I73.1, I73.8, I73.9, and I79.2), or cerebrovascular disease (I60-68, G45, and G46) including vascular aneurysm (I67.1), stroke (I60, 61, 62, 63, and 64), and transient ischaemic attack (G45.8, G45.9) [18–21]. Patients with malignant neoplasm of eye and adnexa (C69), malignant neoplasm of meninges (C70), malignant neoplasm of brain (C71), malignant neoplasm of spinal cord, cranial nerves and other parts of central nervous system (C72), secondary malignant neoplasm of brain and cerebral meninges (C79.3), malignant neoplasm of nasopharynx (C11), malignant neoplasm of craniofacial bones (C41.00), benign neoplasm of meninges (D32), benign neoplasm of brain and other parts of central nervous system (D33), neoplasm of uncertain or unknown behaviour of meninges (D42), or neoplasm of uncertain or unknown behaviour of brain and central nervous system (D43) were classified into the intracranial neoplasm group [18, 19]. Traumatic aetiology was defined in subjects with fracture of skull and facial bones (S02.0, S02.1, S02.3, S02.4, S02.7, and S02.8), contusion of eyeball and orbital tissues (S05.1), and intracranial injury (S06). Others were defined in subjects with inflammatory diseases of the central nervous system (G00-G07), viral infections of the central nervous system (A81-A89), multiple sclerosis (G35), Guillain-Barré syndrome (G61.0), hydrocephalus (G91), benign intracranial hypertension (G93.2), arachnoid cyst (G93.0), and inflammation or disorders of the orbit (H05.0, H05.1, H05.8, and H05.9). Subjects younger than 20 years of age without the above-mentioned diseases were classified as congenital cases. Those aged ≥20 years without the above-mentioned diseases were classified as idiopathic.
Statistical analysis
The incidence was calculated as the number of subjects with CN4 palsy divided by the total person-time at risk during the study period. We presented incidence rates per 100,000 person-years. The 95% confidence intervals (CI) of prevalence and incidence rates were estimated using a Poisson distribution [22]. For newborn cases, the patient’s birthdate was used as the date of onset. All statistical analyses were performed using SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC, USA) and R version 3.4.3 (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Incidence of CN4 palsy
A total of 1,108,369 subjects were included between 2006 and 2015 in the cohort. As presented in Fig. 1, 488 individuals were diagnosed with CN4 palsy in 2002–2015. Of these, 21 subjects who had comorbid thyrotoxicosis (hyperthyroidism or dysthyroid exophthalmos) or myasthenia gravis were excluded from CN4 palsy cases. Seventy-seven subjects with a history of CN4 palsy in 2002–2005 were excluded to identify new cases. Among the 390 subjects with CN4 palsy in 2006–2015, 272 were males (69.7%) and 118 were females (30.3%). Of 390 subjects, 313 subjects were diagnosed by ophthalmologist and 52 subjects were diagnosed by neurologist or neurosurgeon. Twenty-five patients were diagnosed by both clinicians.
Table 1 and Fig. 2 show the incidence of CN4 palsy according to age group and sex. The estimated overall incidence of CN4 palsy was 3.74 (95% CI, 3.38–4.12) per 100,000 person-years in the entire cohort. The incidence of CN4 palsy was 5.20 (95% CI, 4.61–5.85) per 100,000 person-years for males, and 2.26 (95% CI, 1.88–2.70) per 100,000 person-years for females, respectively. A bimodal pattern by age-group was observed, with two peaks at 0–4 years and at 75–79 years. The incidence rate of the first peak in 0–4 years of age was 6.17 (95% CI, 4.22–8.65) per 100,000 person-years, and a second peak incidence rate for 75–79 years of age was 11.81 (95% CI, 7.90–16.84) per 100,000 person-years. This peak pattern was consistent in both male and female groups.
Table 1.
Incidence of fourth cranial nerve palsy in the general Korean population in 2006–2015.
| Age (years) | Total | Male | Female | MF ratio | Surgery of FNP | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Person-years | N | Incidence | 95% CI | Person-years | N | Incidence | 95% CI | Person-years | N | Incidence | 95% CI | Ratio | 95% CI | N | |
| 0–4 | 486377 | 30 | 6.17 | 4.22, 8.65 | 250844 | 20 | 7.98 | 4.97, 12.00 | 235533 | 10 | 4.25 | 2.13, 7.45 | 1.88 | 0.84, 4.49 | 12 |
| 5–9 | 535422 | 28 | 5.23 | 3.53, 7.42 | 278236 | 18 | 6.47 | 3.92, 9.94 | 257186 | 10 | 3.89 | 1.95, 6.82 | 1.66 | 0.72, 4.03 | 19 |
| 10–14 | 647123 | 14 | 2.16 | 1.22, 3.50 | 339661 | 8 | 2.36 | 1.08, 4.38 | 307461 | 6 | 1.95 | 0.78, 3.95 | 1.21 | 0.37, 4.22 | 4 |
| 15–19 | 709351 | 8 | 1.13 | 0.52, 2.10 | 374848 | 3 | 0.80 | 0.20, 2.07 | 334503 | 5 | 1.49 | 0.54, 3.21 | 0.54 | 0.08, 2.75 | 0 |
| 20–24 | 692069 | 8 | 1.16 | 0.53, 2.15 | 363697 | 6 | 1.65 | 0.65, 3.33 | 328372 | 2 | 0.61 | 0.10, 1.88 | 2.71 | 0.48, 27.44 | 2 |
| 25–29 | 746207 | 13 | 1.74 | 0.96, 2.87 | 386150 | 11 | 2.85 | 1.48, 4.88 | 360057 | 2 | 0.56 | 0.09, 1.71 | 5.13 | 1.12, 47.61 | 0 |
| 30–34 | 821952 | 8 | 0.97 | 0.44, 1.81 | 420323 | 6 | 1.43 | 0.57, 2.89 | 401629 | 2 | 0.50 | 0.08, 1.54 | 2.87 | 0.51, 29.04 | 3 |
| 35–39 | 882291 | 17 | 1.93 | 1.15, 2.99 | 449134 | 12 | 2.67 | 1.43, 4.48 | 433157 | 5 | 1.15 | 0.41, 2.48 | 2.31 | 0.76, 8.39 | 2 |
| 40–44 | 911168 | 14 | 1.54 | 0.87, 2.49 | 463984 | 9 | 1.94 | 0.93, 3.50 | 447185 | 5 | 1.12 | 0.40, 2.40 | 1.74 | 0.52, 6.59 | 0 |
| 45–49 | 889442 | 23 | 2.59 | 1.67, 3.79 | 451749 | 16 | 3.54 | 2.08, 5.57 | 437693 | 7 | 1.60 | 0.69, 3.09 | 2.22 | 0.86, 6.37 | 2 |
| 50–54 | 820412 | 30 | 3.66 | 2.50, 5.13 | 413566 | 25 | 6.05 | 3.98, 8.74 | 406846 | 5 | 1.23 | 0.44, 2.64 | 4.92 | 1.85, 16.45 | 2 |
| 55–59 | 638453 | 47 | 7.37 | 5.46, 9.68 | 317779 | 32 | 10.08 | 6.98, 13.99 | 320674 | 15 | 4.68 | 2.69, 7.46 | 2.15 | 1.13, 4.28 | 0 |
| 60–64 | 476984 | 33 | 6.92 | 4.82, 9.56 | 233295 | 26 | 11.16 | 7.40, 16.02 | 243689 | 7 | 2.87 | 1.23, 5.56 | 3.88 | 1.64, 10.59 | 1 |
| 65–69 | 403112 | 41 | 10.18 | 7.37, 13.62 | 188591 | 30 | 15.93 | 10.89, 22.33 | 214521 | 11 | 5.13 | 2.66, 8.79 | 3.11 | 1.51, 6.86 | 1 |
| 70–74 | 333292 | 34 | 10.21 | 7.15, 14.04 | 144479 | 24 | 16.64 | 10.84, 24.21 | 188812 | 10 | 5.30 | 2.66, 9.29 | 3.14 | 1.45, 7.35 | 0 |
| 75–79 | 228809 | 27 | 11.81 | 7.90, 16.84 | 87827 | 17 | 19.38 | 11.57, 30.11 | 140983 | 10 | 7.10 | 3.56, 12.45 | 2.73 | 1.18, 6.67 | 0 |
| >80 | 217850 | 15 | 6.89 | 3.96, 10.99 | 64733 | 9 | 13.92 | 6.69, 25.09 | 153118 | 6 | 3.92 | 1.56, 7.94 | 3.55 | 1.13, 12.11 | 0 |
| Overall | 10440314 | 390 | 3.74 | 3.38, 4.12 | 5227369 | 272 | 5.20 | 4.61, 5.85 | 5210731 | 118 | 2.26 | 1.88, 2.70 | 2.30 | 1.84, 2.88 | 48 |
Fig. 2. Incidence of fourth cranial nerve palsy in Koreans during 2006-2015.
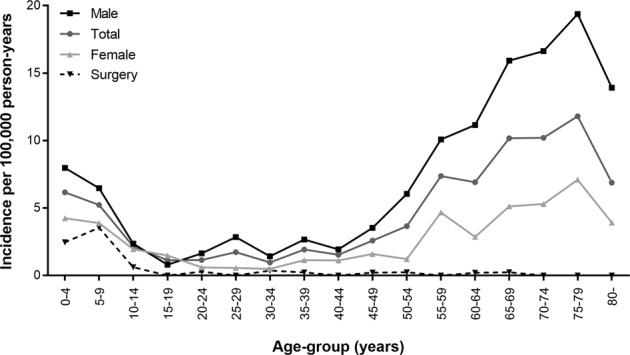
The incidence rate showed two peaks: one at 0–4 years and the other at 75–79 years.
Fig. 3 shows the male-to-female ratio of the incidence of CN4 palsy according to age groups. The incidence of CN4 palsy was higher in males than in females, and the average male-to-female incidence ratio was 2.30 (95% CI, 1.84–2.88). In children aged <20 years, the ratio was under 2, but it roamed around 3 in adults aged ≥20 years. Male preponderance was highest in the 25–29-year-old group, and was consistent throughout the cohort, except for the 15–19-year-old group.
Fig. 3. Male-to-female ratio in the incidence of fourth cranial nerve palsy in Koreans.
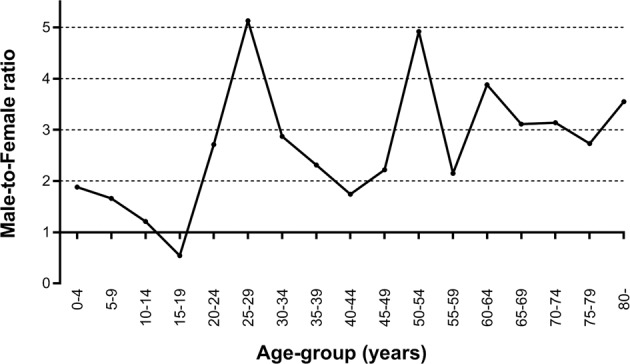
The incidence rate was higher in males than in females, except for the 15–19-year-old group.
Prevalence and surgical intervention of CN4 palsy
Table 2 presents the annual prevalence rates of CN4 palsy during the 2006–2015 period. The prevalence of CN4 palsy was 3.43 (95% CI, 2.41–4.69) per 100,000 persons in 2006, but gradually increased reaching 8.76 (95% CI, 7.87–11.60) per 100,000 persons in 2015. There was an increasing trend in the prevalence of CN4 palsy over time, and surgery for CN4 palsy was higher in the latter half of the study period. Every year, the prevalence of CN4 palsy was higher in males than in females.
Table 2.
Prevalence of fourth cranial nerve palsy in the general Korean population in 2006–2015.
| Year | Annual total population | Total | Male | Female | Surgery of FNP | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Prevalence | 95% CI | No. | Prevalence | 95% CI | No. | Prevalence | 95% CI | No. | Prevalence | 95% CI | ||
| 2006 | 1021208 | 35 | 3.43 | 2.41, 4.69 | 25 | 4.89 | 3.21, 7.06 | 10 | 1.96 | 0.98, 3.44 | 5 | 0.49 | 0.18, 1.05 |
| 2007 | 1031653 | 43 | 4.17 | 3.04, 5.54 | 32 | 6.19 | 4.28, 8.59 | 11 | 2.14 | 1.11, 3.66 | 3 | 0.29 | 0.07, 0.75 |
| 2008 | 1035089 | 40 | 3.86 | 2.79, 5.19 | 28 | 5.40 | 3.64, 7.65 | 12 | 2.32 | 1.24, 3.90 | 5 | 0.48 | 0.17, 1.04 |
| 2009 | 1038462 | 48 | 4.62 | 3.43, 6.06 | 31 | 5.96 | 4.10, 8.31 | 17 | 3.28 | 1.96, 5.10 | 3 | 0.29 | 0.07, 0.75 |
| 2010 | 1042706 | 58 | 5.56 | 4.25, 7.12 | 37 | 7.08 | 5.04, 9.62 | 21 | 4.04 | 2.55, 6.02 | 5 | 0.48 | 0.17, 1.03 |
| 2011 | 1046465 | 67 | 6.40 | 4.99, 8.06 | 50 | 9.54 | 7.13, 12.44 | 17 | 3.25 | 1.94, 5.05 | 6 | 0.57 | 0.23, 1.16 |
| 2012 | 1050743 | 72 | 6.85 | 5.39, 8.56 | 54 | 10.26 | 7.76, 13.25 | 18 | 3.43 | 2.08, 5.27 | 10 | 0.95 | 0.48, 1.67 |
| 2013 | 1053952 | 85 | 8.06 | 6.47, 9.90 | 65 | 12.32 | 9.57, 15.57 | 20 | 3.80 | 2.37, 5.71 | 10 | 0.95 | 0.48, 1.66 |
| 2014 | 1057454 | 95 | 8.98 | 7.30, 10.91 | 64 | 12.10 | 9.37, 15.31 | 31 | 5.87 | 4.04, 8.18 | 7 | 0.66 | 0.28, 1.28 |
| 2015 | 1061141 | 93 | 8.76 | 7.10, 10.67 | 64 | 12.06 | 9.34, 15.26 | 29 | 5.47 | 3.71, 7.71 | 4 | 0.38 | 0.12, 0.88 |
Of 390 subjects, 48 patients underwent surgery for CN4 palsy during the study period, and the surgical incidence for CN4 palsy was 0.46 (95% CI, 0.34–0.60) per 100,000 person-years (Table 1). Thirty-five of the 48 patients (72.9%) who underwent surgeries for CN4 palsy were younger than 20 years of age.
Presumed aetiology of CN4 palsy
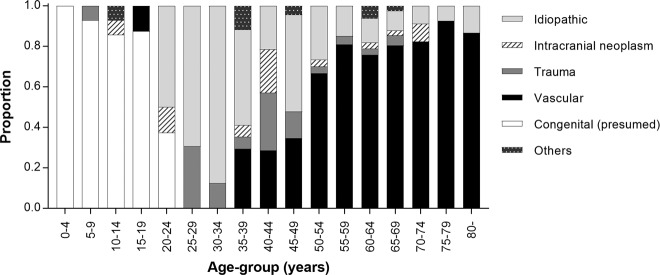
Aetiologies of CN4 palsy were evaluated in 390 subjects with CN4 palsy during 2006–2015. The most common aetiology was presumed as vascular disease (n = 200, 51.3%), followed by congenital conditions (n = 78, 20.0%), idiopathic, (n = 72, 18.5%), trauma (n = 21, 5.4%), intracranial neoplasm (n = 12, 3.1%), and others (n = 7, 1.8%). The ‘others’ group included multiple sclerosis (n = 1), benign intracranial hypertension (n = 1), hydrocephalus (n = 1), inflammation or infection of the CNS system (n = 2), and inflammation or disorder of the orbit (n = 2). The presumed aetiologies of CN4 palsy according to age group are presented in Fig. 4. The cause of the first peak in 0–4 years of age was congenital, while the main cause of a second peak was vascular disease. The proportion of vascular aetiology was rare in subjects aged <20 years, but increased according to age in adults aged ≥50 years. Of the 200 patients who had vascular disease, 28 cases had only one disease, either hypertension or diabetes. The proportion of head trauma was highest in young adults aged 25–29 years and 40–44 years (19.0% and 19.0%, respectively).
Fig. 4. Aetiologies of fourth cranial nerve palsy by age-groups in Koreans.
The aetiology varied according to the age-group.
Discussion
In this population-based cohort study, we found the incidence rate of CN4 palsy in Korea to be 3.74 per 100,000 person-years; we also found male predominance and a bimodal pattern by age-group. The most common presumed cause was cerebrovascular or cardiovascular disease, and patients with congenital CN4 palsy underwent surgery most often. In our previous study, the incidence of CN6 palsy in Korea was 4.66 per 100,000 person-years with male preponderance [23]. We found that the incidence of CN4 palsy was slightly lower than that of CN6 palsy.
To date, there have been only a few epidemiologic studies regarding the incidence of CN4 palsy [9, 11, 12, 24]. The incidence of CN4 palsy was estimated to be 6.3 per 100,000 in those with adult-onset strabismus [24] and 2.7–3.4 per 100,000 in children [11, 12]. Previous studies showed no bimodal pattern by age and included many young and middle-aged subjects [3, 7]. Dosunmu et al. reported that the overall incidence rate of CN4 palsy across all ages in the general population was 5.73 per 100,000 person-years in the United States [9], the peak presentation age was in the fourth decade of life, and the most common aetiology was of congenital origin (49%), followed by hypertension (18%) and trauma (18%) [9]. The result of that study showed a slightly higher incidence rate than our study; it also differed in terms of the peak age group and the frequency of aetiologies. Our Korean cohort showed a higher incidence of CN4 palsy in older age groups, and vascular comorbidities to be higher than in the United States.
In this study, we found the incidence of CN4 palsy to be higher in men than in women, which is consistent with previous studies [1, 3, 6, 9, 24, 25]. One suggested explanation is that head trauma is more frequent in men [9]. Ray et al. reported that the most common aetiology was trauma in men and congenital origin in women [6]. In our study, the male-to female incidence ratio was highest in the 25–29-year-old group, and the proportion of trauma aetiology was the highest in this group. However, considering the high proportion of vascular and congenital aetiologies, further explanation is needed. The male-to female ratio was 1.5-3.0 in studies on CN4 palsy caused by vascular, congenital, trauma, or idiopathic aetiologies [3, 6, 25, 26]. One possibility might be that the male sex is a risk factor for microvascular disease in Korea [27, 28].
The proportion of aetiologies for CN4 palsy have been varied across studies according to the target population and the definition of aetiologies [4, 29]. Table 3 summarises the aetiologies of CN4 palsy reported in previous major studies with greater than 70 subjects. Institution-based studies reported the most common cause to be congenital in origin, followed by trauma [1–4, 7]. A few studies found trauma to be more common than other causes [6, 29–31]. In the present study, the proportion of congenital cases (20%) may have been underestimated, because we operationally defined congenital causes only in subjects younger than 20 years of age. However, subjects with congenital CN4 palsy can be diagnosed at any age, as patients lose deviation control due to the decompensation for CN4 palsy over time in adulthood [9]. In addition, CN4 palsy associated with intracranial tumours is reported to be rare (ranging from no reported cases to 8%) [1, 6, 9, 32, 33]. Typically, intracranial tumours affect multiple cranial nerves simultaneously. In this study, we identified isolated or multiple cranial palsies involving CN4 palsy, and 3% of patients had an intracranial mass, which is similar to the results of previous studies. Idiopathic causes accounted for 19% of the cases in our study, and several other studies showed a large proportion of cases with undermined causes (4–38%) [1, 6–8, 25, 26, 30, 33].
Table 3.
Previous studies on the aetiology of fourth cranial nerve palsy.
| Country | Publication date | Studied duration | No. of cases | Aetiology (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Trauma | Tumour | Vascular | Congenital | Unknown | Other | |||||
| Rucker et al. [32, 33] | USA | 1966 | 1958–1964 | 84 | 27 | 8 | 16 | 22 | 16 | |
| Rush et al. [30] | USA | 1981 | 1966–1978 | 172 | 32 | 4 | 19 | 36 | 9 | |
| Richards et al. [8] | USA | 1992 | 1978–1988 | 578 | 29 | 5 | 18 | 32 | 16 | |
| Dosunmu et al. [9] | USA | 2018 | 1978–1992 | 74 | 18 | 1 | 24 | 49 | 4 | 1 |
| Von Noorden et al. [1] | USA | 1986 | 1973–1984 | 270 | 34 | 40 | 23 | 3 | ||
| Mansour and Reinecke [4] | Spain | 1986 | 1972–1981 | 82 | 34 | 1 | 2 | 52 | 6 | 4 |
| Keane [29] | USA | 1993 | 1970–1993 | 215 | 53 | 7 | 4 | 1 | 0 | 36 |
| Gunderson et al. [7] | USA | 2001 | 1968–1999 | 124 | 26 | 2 | 6 | 28 | 38 | |
| Mollan et al. [2] | UK | 2009 | 1999–2005 | 150 | 33 | 3 | 21 | 35 | 9 | 1 |
| Bagheri et al. [3] | Iran | 2010 | 1997–2007 | 73 | 16 | 77 | 7 | |||
| Ray et al. [6] | India | 2014 | 2001–2008 | 181 | 34 | 1 | 9 | 33 | 24 | 0 |
| Current study | Korea | 2006–2015 | 390 | 5 | 3 | 51 | 20 | 19 | 2 | |
Of note, the most common presumed cause of CN4 palsy in this study was vascular disease. Another study regarding acquired CN4 palsy in Korea also reported that vascular disease was the most common aetiology [25]. In our population-based study from 2006 to 2015, there was a greater incidence of CN4 palsy in Koreans older than 50 years of age than in those younger than 50, and there was more than 50% vascular comorbidity. We reported a presumed microvascular aetiology in 51% of CN4 palsy cases; this is higher than previously reported. The large proportion of comorbid vascular disease in CN4 palsy cases might be due to the increasingly improved detection of vascular disease or an unknown racial difference.
The form of CN4 palsy that most frequently required surgical intervention was congenital CN4 palsy, which was more common in young age groups [3, 7]. Our study showed that most of the individuals who underwent surgeries were younger than 20 years of age, and only 8.3% of those who underwent surgeries were older than 50. Although we could not evaluate the recovery rate of subjects with CN4 palsy, several studies have reported the best prognosis for recovery in the vascular group [8, 30]. Park et al. reported that vascular disease was the most common cause of acquired cranial nerve palsies, and 85.2% of patients showed complete or partial overall recovery [25]. Akagi et al. reported that eight of 14 patients with CN4 palsy caused by head trauma showed a complete recovery within 12 months [34]. These findings suggest that surgeries were more often performed for congenital cases.
There are several limitations to the present study. First, measurement errors or diagnostic issues for CN4 palsy might be present in the NHIS data, as the data were originally collected for the purpose of medical insurance claims, and not for academic research. The NHIS dataset may not be representative of the general population completely, even if it is from a random sampling method. It may not be similar according to many other characteristics that might affect the CN4 palsy data. The diagnosis of CN4 palsy depended on each physician who had examined the patient, and thus might not have been completely standardised. The prevalence and incidence of CN4 palsy could have been underestimated because the subjects who did not visit the hospitals were missed. The washout period might not be sufficient for excluding previously diagnosed cases. We could not evaluate the recovery rate or follow-up status of subjects with CN4 palsy due to unavailable medical records. Only the incidence of surgery could be assessed. To evaluate strabismus surgeries related to CN4 palsy, we investigated patients who had CN4 diagnostic codes entered close to the surgery date. However, it could not accurately confirm the surgery for CN4 palsy. Notably, the evaluation of the aetiology of CN4 palsy might be also biased. We presumed the aetiology according to the diagnostic codes associated with comorbidities because detailed medical records (i.e., neuroimaging or laboratory data) are not available in the NHIS database. However, causal relationships between the accompanying diseases and CN4 palsy remain unclear or inadequate. Moreover, the presence of a certain comorbid disease does not exclude having another true aetiology, unless a detailed systematic examination is performed. Therefore, the presumed aetiologies in our study might be biased. In addition, there was a possibility of underestimating congenital cases, because decompensated CN4 palsy over 20 years of age could not be classified as congenital cases. Lastly, we did not differentiate isolated CN4 palsy from multiple cranial nerve palsies, which could make the data less valid.
In conclusion, we found the incidence of CN4 palsy in Korea to be 3.74 per 100,000 person-years, with male predominance and a bimodal peak pattern by age. The most common presumed cause of CN4 palsy was vascular disease in the general population, and the aetiology of CN4 palsy varied according to age group. The epidemiology of CN4 palsy might help to understand the pathophysiology and build public policies for its prevention and treatment.
Summary table
What was known before:
Fourth cranial nerve palsy has been investigated mostly in tertiary referral centres, and the epidemiology of fourth cranial nerve palsy in the general population has only been reported in limited studies, mainly in the United States.
What this study adds:
Incidence of fourth cranial nerve palsy in Korea was 3.74 per 100,000 person-years, with male predominance and a bimodal peak pattern by age.
The aetiology of fourth cranial nerve palsy varied according to age-group.
Acknowledgements
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) and funded by the Korean government (MSIT) (No. NRF-2017M3A9E8033207).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.von Noorden GK, Murray E, Wong SY. Superior oblique paralysis. A review of 270 cases. Arch Ophthalmol. 1986;104:1771–6. doi: 10.1001/archopht.1986.01050240045037. [DOI] [PubMed] [Google Scholar]
- 2.Mollan SP, Edwards JH, Price A, Abbott J, Burdon MA. Aetiology and outcomes of adult superior oblique palsies: a modern series. Eye. 2009;23:640–4. doi: 10.1038/eye.2008.24. [DOI] [PubMed] [Google Scholar]
- 3.Bagheri A, Fallahi MR, Abrishami M, Salour H, Aletaha M. Clinical features and outcomes of treatment for fourth nerve palsy. J Ophthalmic Vis Res. 2010;5:27–31. [PMC free article] [PubMed] [Google Scholar]
- 4.Mansour AM, Reinecke RD. Central trochlear palsy. Surv Ophthalmol. 1986;30:279–97. doi: 10.1016/0039-6257(86)90061-5. [DOI] [PubMed] [Google Scholar]
- 5.Wang Q, Flanders M. Surgical management of unilateral superior oblique palsy: thirty years of experience. Am Orthopt J. 2016;66:79–86. doi: 10.3368/aoj.66.1.79. [DOI] [PubMed] [Google Scholar]
- 6.Ray D, Gupta A, Sachdeva V, Kekunnaya R. Superior oblique palsy: epidemiology and clinical spectrum from a tertiary eye care center in South India. Asia Pac J Ophthalmol (Philos) 2014;3:158–63. doi: 10.1097/APO.0b013e31829fbab4. [DOI] [PubMed] [Google Scholar]
- 7.Gunderson CA, Mazow ML, Avilla CW. Epidemiology of CN IV Palsies. Am Orthopt J. 2001;51:99–102. doi: 10.3368/aoj.51.1.99. [DOI] [PubMed] [Google Scholar]
- 8.Richards BW, Jones FR, Jr, Younge BR. Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear, and abducens cranial nerves. Am J Ophthalmol. 1992;113:489–96. doi: 10.1016/S0002-9394(14)74718-X. [DOI] [PubMed] [Google Scholar]
- 9.Dosunmu EO, Hatt SR, Leske DA, Hodge DO, Holmes JM. Incidence and etiology of presumed fourth cranial nerve palsy: a population-based Study. Am J Ophthalmol. 2018;185:110–4. doi: 10.1016/j.ajo.2017.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoi CP, Chen YT, Fuh JL, Yang CP, Wang SJ. Increased risk of stroke in patients with isolated third, fourth, or sixth cranial nerve palsies: a nationwide cohort study. Cerebrovasc Dis. 2016;41:273–82. doi: 10.1159/000444128. [DOI] [PubMed] [Google Scholar]
- 11.Tollefson MM, Mohney BG, Diehl NN, Burke JP. Incidence and types of childhood hypertropia: a population-based study. Ophthalmology. 2006;113:1142–5. doi: 10.1016/j.ophtha.2006.01.038. [DOI] [PubMed] [Google Scholar]
- 12.Holmes JM, Mutyala S, Maus TL, Grill R, Hodge DO, Gray DT. Pediatric third, fourth, and sixth nerve palsies: a population-based study. Am J Ophthalmol. 1999;127:388–92. doi: 10.1016/S0002-9394(98)00424-3. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017;46:e15. doi: 10.1093/ije/dyv319. [DOI] [PubMed] [Google Scholar]
- 14.Kim T, Kwon OK, Bang JS, Lee H, Kim JE, Kang HS, et al. Epidemiology of ruptured brain arteriovenous malformation: a National Cohort Study in Korea. J Neurosurg. 2018;130:1965–70. doi: 10.3171/2018.1.JNS172766. [DOI] [PubMed] [Google Scholar]
- 15.Rim TH, Yoo TK, Kwak J, Lee JS, Kim SH, Kim DW, et al. Long-term regular use of low-dose aspirin and neovascular age-related macular degeneration: National Sample Cohort 2010-2015. Ophthalmology. 2019;126:274–82. doi: 10.1016/j.ophtha.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 16.Rim TH, Kim SS, Ham DI, Yu SY, Chung EJ, Lee SC. Incidence and prevalence of uveitis in South Korea: a nationwide cohort study. Br J Ophthalmol. 2018;102:79–83. doi: 10.1136/bjophthalmol-2016-309829. [DOI] [PubMed] [Google Scholar]
- 17.Kim JY, Rim TH, Kim SS. Trends of pars plana vitrectomy rates in South Korea: a nationwide cohort study. Korean J Ophthalmol. 2017;31:446–51. doi: 10.3341/kjo.2016.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Park SJ, Yang HK, Byun SJ, Park KH, Hwang JM. Ocular motor cranial nerve palsy and increased risk of stroke in the general population. PLoS One. 2018;13:e0205428. doi: 10.1371/journal.pone.0205428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rim TH, Han J, Choi YS, Lee T, Kim SS. Stroke risk among adult patients with third, fourth or sixth cranial nerve palsy: a Nationwide Cohort Study. Acta Ophthalmol. 2017;95:e656–e61.. doi: 10.1111/aos.13488. [DOI] [PubMed] [Google Scholar]
- 20.Feinstein MJ, Bahiru E, Achenbach C, Longenecker CT, Hsue P, So-Armah K, et al. Patterns of cardiovascular mortality for HIV-infected adults in the United States: 1999 to 2013. Am J Cardiol. 2016;117:214–20. doi: 10.1016/j.amjcard.2015.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 22.Hwang S, Lim DH, Chung TY. Prevalence and incidence of keratoconus in South Korea: a nationwide population-based study. Am J Ophthalmol. 2018;192:56–64. doi: 10.1016/j.ajo.2018.04.027. [DOI] [PubMed] [Google Scholar]
- 23.Jung EH, Kim SJ, Lee JY, Cho BJ. The incidence and etiology of sixth cranial nerve palsy in Koreans: a 10-year nationwide cohort study. Sci Rep. 2019;9:18419. doi: 10.1038/s41598-019-54975-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Martinez-Thompson JM, Diehl NN, Holmes JM, Mohney BG. Incidence, types, and lifetime risk of adult-onset strabismus. Ophthalmology. 2014;121:877–82. doi: 10.1016/j.ophtha.2013.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park UC, Kim SJ, Hwang JM, Yu YS. Clinical features and natural history of acquired third, fourth, and sixth cranial nerve palsy. Eye. 2008;22:691–6. doi: 10.1038/sj.eye.6702720. [DOI] [PubMed] [Google Scholar]
- 26.Tiffin PA, MacEwen CJ, Craig EA, Clayton G. Acquired palsy of the oculomotor, trochlear and abducens nerves. Eye. 1996;10:377–84.. doi: 10.1038/eye.1996.77. [DOI] [PubMed] [Google Scholar]
- 27.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–8. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH, et al. Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens. 2006;24:1515–21. doi: 10.1097/01.hjh.0000239286.02389.0f. [DOI] [PubMed] [Google Scholar]
- 29.Keane JR. Fourth nerve palsy: historical review and study of 215 inpatients. Neurology. 1993;43:2439–43. doi: 10.1212/WNL.43.12.2439. [DOI] [PubMed] [Google Scholar]
- 30.Rush JA, Younge BR. Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1,000 cases. Arch Ophthalmol. 1981;99:76–9. doi: 10.1001/archopht.1981.03930010078006. [DOI] [PubMed] [Google Scholar]
- 31.Ellis FD, Helveston EM. Superior oblique palsy: diagnosis and classification. Int Ophthalmol Clin. 1976;16:127–35. [PubMed] [Google Scholar]
- 32.Rucker CW. Paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1958;46:787–94. doi: 10.1016/0002-9394(58)90989-9. [DOI] [PubMed] [Google Scholar]
- 33.Rucker CW. The causes of paralysis of the third, fourth and sixth cranial nerves. Am J Ophthalmol. 1966;61:1293–8. doi: 10.1016/0002-9394(66)90258-3. [DOI] [PubMed] [Google Scholar]
- 34.Akagi T, Miyamoto K, Kashii S, Yoshimura N. Cause and prognosis of neurologically isolated third, fourth, or sixth cranial nerve dysfunction in cases of oculomotor palsy. Jpn J Ophthalmol. 2008;52:32–5. doi: 10.1007/s10384-007-0489-3. [DOI] [PubMed] [Google Scholar]