Abstract
In human retina, photoreceptor cell death (PCD) is a slow but conspicuous event, which continues with aging. Rods die earlier than cones, the latter continue to alter in a subtle manner until advanced aging. This review summarizes the existing information on age-related changes in photoreceptor cells, especially cones and analyses the possible associated factors. Oxidative and nitrosative stress are involved in photoreceptor alterations, which may stem from light and iron toxicity and other sources. Lipid peroxidation in macular photoreceptor outer segments and mitochondrial aberrations are prominent in aging. It is important to understand how those changes ultimately trigger PCD. The redistribution of calbindin D-28K and long/middle-wavelength-sensitive opsin in the parafoveal and perifoveal cones, anomalies in their somata and axons are strong predictors of their increasing vulnerability with aging. Signs of reduced autophagy, with autophagosomes containing organelle remnants are seen in aging photoreceptor cells. Currently, mechanisms that lead to human PCD are unknown; some observations favour apoptosis as a pathway. Since cones appear to change slowly, there is an opportunity to reverse those changes before they die. Therefore, a full understanding of how cones alter and the molecular pathways they utilize for survival must be the future research goal. Recent approaches to prevent PCD in aging and diseases are highlighted.
Subject terms: Retina, Retina
摘要
在人类视网膜中, 感光细胞死亡 (photoreceptor cell death, PCD) 是一个缓慢而显著的过程, 并随着年龄的增长而持续。视杆细胞比视锥细胞死亡发生的更早, 但后者以微妙的方式继续改变, 直到老年。这篇综述总结了光感受器与年龄相关变化的现有资料, 特别是视锥细胞, 并分析了可能的相关因素。氧化和亚硝化应激与光感受器的改变有关, 这源于光和铁的毒性以及其他来源。黄斑光感受器外节脂质过氧化和线粒体畸变在衰老过程中尤为突出。重要的是要了解这些改变最终是如何触发PCD的。随年龄增加, 钙结合蛋白D-28K和长/中波长敏感视蛋白在中心凹旁和中心凹周围的视锥细胞中重新分布, 因此视锥细胞神经元胞体和轴突异常是易受损的强预测因子。在老化的光感受器中可以看到自噬减少的迹象, 自噬小体内含有细胞器残余物。目前, 导致人类PCD的机制尚不清楚;一些研究认为其通过细胞凋亡的信号通路。由于视锥细胞变化缓慢, 所以有机会在它们死亡之前逆转这些变化。因此, 全面了解视锥细胞是如何改变的, 视锥细胞赖以生存的分子信号传导通路是未来的研究目标。另外, 我们强调了近期关于防止 PCD在衰老以及疾病中的作用。
Introduction
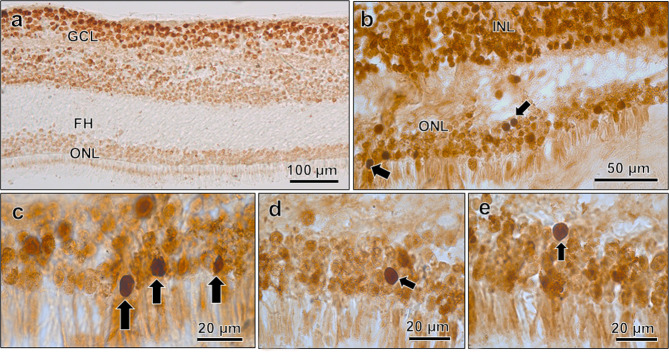
The human retina changes with aging. In fact, most constituent cell types within it are changed perceptibly, unparalleled by instances recognized elsewhere in the aging brain. The severity of retinal aging is centred on the photoreceptor cells, the rods and cones, which are inherently vulnerable [1], change slowly and ultimate die [2–8]. Photoreceptor cell death (PCD) is prominent in aging [7] and diseases such as retinitis pigmentosa (RP), and in some individuals, the initial changes in the retinal pigment epithelium (RPE) and Bruch’s membrane lead secondarily to PCD, which often culminates in the manifestation of a disease called age-related macular degeneration (AMD) in elderly population. Efforts were made therefore, to understand the ways in which photoreceptors alter with aging, since aging is considered to be a strong risk factor for AMD. Photoreceptor cells are differentiated into several parts (Fig. 1) and a defect occurring in any individual part can have a serious consequence on executing specific functions therein. Contemporary research into revealing the associated factors implies that PCD may stem from any continuing changes in the structural integrity of photoreceptors or components involved with phototransduction and energy metabolism [9]. The present review highlights the photoreceptor cell changes in aging human retina and examines the underlying factors and strategies to preserve the PRE and photoreceptor cells in aging and AMD.
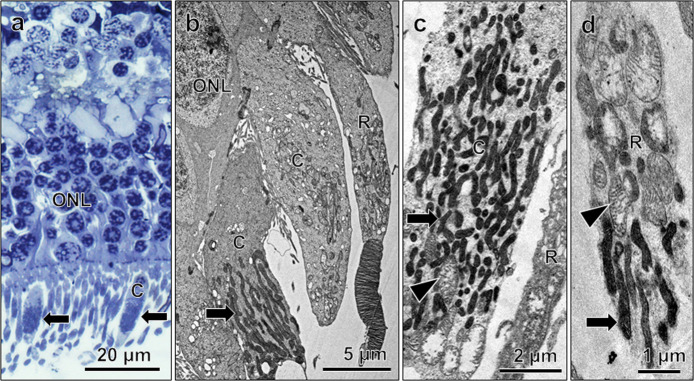
Fig. 1. Morphology of human photoreceptors.
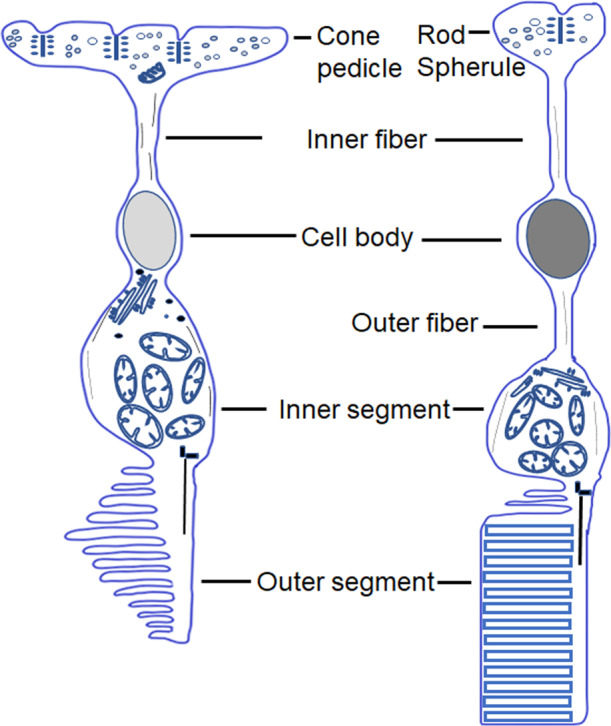
Diagram showing various parts of human cone (left) and rod (right side), as seen by TEM.
Photoreceptor outer segment damage and renewal capacity
The discs of the photoreceptor outer segments (POS) are fragile. With aging, about 20% of the rod outer segments (ROS) discs develop convolutions [10]. Likewise, in advanced aging (>80 years), the cone outer segment (COS) discs disorganize sporadically [11] (Supplementary Fig. 1). The reasons for those changes are unclear, given the presence of lutein and zeaxanthin (in ROS) therein, allowing them to scavenge the free radicals generated in phototoxicity [12, 13]. Photoreceptor cells have some potential for recovering their outer segments after light damage [14], in mice models of RP [15, 16] and other diseases [17]. In early stage of retinal degeneration, sustained delivery of ciliary neurotrophic factor (CNTF) and oncostatin M can promote POS regeneration [15–18]. However, the mechanisms of POS renewal after damage in aging and light toxicity are unknown. The renewal is dependent upon the presence of intact photoreceptor inner segments and cell bodies; it also demands a healthy RPE [19], because reduced phagocytosis of the shed discs in RPE, common in aging and diseases [20, 21], may hinder POS renewal.
Mitochondrial changes in aging photoreceptor inner segments
In photoreceptor cells, mitochondria are concentrated in their inner segments [22–25], which bestow them to be metabolically active. With aging, there are striking changes in mitochondrial morphology (Fig. 2) [24–27], and deletions in mitochondrial DNA (mtDNA) [28] in macular photoreceptors. mtDNA damage in RPE results from oxidative stress (OS) via mitochondrial generation of reactive oxygen species and free radicals [29, 30]. A similar mechanism might operate in aging photoreceptors. A decrease in the number of cytochrome C oxidase-positive photoreceptor cells [28] due to acquired mtDNA mutations, and a reduction of complex I and IV immunoreactivity in aging macular cones [25] were reported. These mitochondrial changes are likely to cause a reduced energy output in aging photoreceptors [30], driving them to rely on glycolysis. Certain glycolytic enzymes even become dysfunctional in AMD due to OS [31]. Collectively, these changes might lead to energy deficiency in photoreceptors. The interplay of mitochondrial fission and fusion in aging photoreceptors is unknown. Recent reports suggest that the photoreceptor mitochondrial damage can be ameliorated by the use of far red to near infra-red light, in a process called photobiomodulation [PBM; refs. [32, 33]; see also for references of animal studies], and improving mitochondrial function via reducing OS could be a basis for treatment in AMD [34].
Fig. 2. Mitochondrial status in human photoreceptor cells.
Light micrograph (a) and electron micrographs (b–d), showing mitochondrial features in photoreceptor cells. (a) Dark mitochondria (arrows) in cones (C) are visible in semithin section. b–d Show dark, condensed mitochondria in cone inner segments (arrows) and rod (R, arrow in d), few swollen mitochondria are seen amongst them (c, d; arrowheads). From 83-year (a, c; nasal part) and 85-year (b, d; perifoveal part)-old donor retina.
Microtubule misalignment in aging photoreceptor cells
Photoreceptor cells are directionally sensitive, being sensitive to light travelling along their longitudinal axis. Eckmiller [35] hypothesized that changes in the macular cone cytoskeleton and associated proteins could be a basis for photoreceptor misalignment and death in AMD. In aging human retina, the photoreceptor microtubules undergo misalignment and partial disorganization [36], raising to the possibility that aging photoreceptor cells may suffer from interrupted axonal transport, which may make them vulnerable to death.
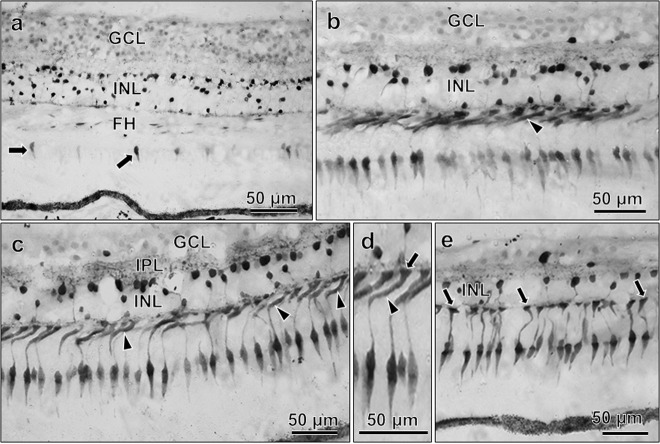
Cone axonal changes and role of calbindin D
Calbindin D is a major calcium-binding protein of human photoreceptor cells [37–39] and regulates the cytosolic calcium (Ca2+). Immunolabelling with calbindin D revealed axonal outgrowth from cones with aging [27] and in dry AMD [40]. Also, aberrant swellings were noted in perifoveal cone axons before terminating into pedicles (Fig. 3a–d), a feature that was absent in mid-peripheral retina (Fig. 3e). Because Ca2+ levels vary in different photoreceptor compartments [41], these aberrant axonal changes suggest their possible link with dysregulated Ca2+ homoeostasis in aged cones. Experimental studies reported the involvement of excessive, dysregulated Ca2+ in PCD [42].
Fig. 3. Calbindin D immunoreactivity in 94-year-old donor retina.
In the parafovea (a), immunoreactivity is weakly present in few cone inner segments (arrows). It is strong in many cones of the perifovea (b, c), where abnormal axonal swellings (arrowheads) before terminating into pedicles are seen, as shown in enlarged view in d; arrow denotes pedicle (in d). In mid-peripheral cones, the axons terminate straight into pedicles (arrows, e). In all areas, the INL shows strong immunoreactivity.
Vulnerability of long/middle-wavelength-sensitive cones with aging
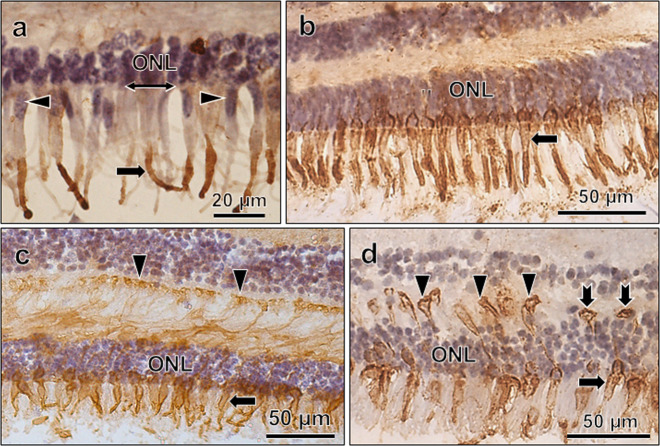
Immunoreactivity to long–middle-wavelength opsin (L/M opsin, a marker for red-green cones) showed ectopic labelling of membranes of the cone somata and swollen axons, besides the usual labelling of COS [43] (Fig. 4 and Supplementary Fig. 2). The ectopic labelling indicates L/M opsin mislocalization due to dysregulated opsin trafficking in the affected cones. The L/M cone somata align in the outermost row of the ONL [44], and with aging, many of them prolapse beyond the ONL [43] (Fig. 4a). All these data indicate that L/M cone anomalies are common in aging and also in AMD [40, 43]. The fate of other cones (e.g., S cones) in human retina is unknown. They do not appear to die in primates [45].
Fig. 4. Pattern of L/M opsin immunoreactivity in aging cones.
L/M opsin immunoreactivity in cones from parafoveal (a) and mid-peripheral retina (b–d). In (a), immunoreactivity is present in COS only (arrow), whereas in (b–d), it is also present in membranes of inner segments (arrows) and cone terminals (arrowheads; c, d). In (d), the cone pedicles lie at different levels. Two of them lie close to the ONL (notched arrows), indicating their retraction from the OPL. Counterstained with hematoxylin. In (a), note the prolapse of cone nuclei (arrowheads) outer to the OLM (right-left arrows). From 75-year- (a), 81-year- (b), 83-year- and (c) 85-year- (d) old retinas.
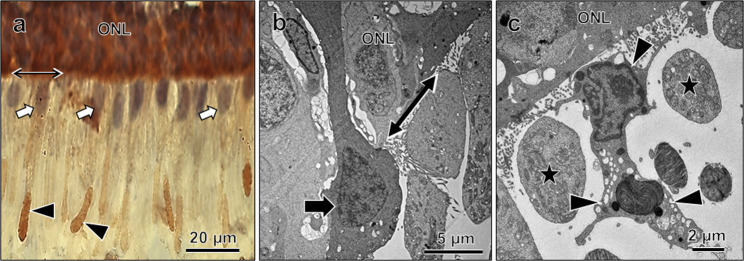
The L/M opsin+ COS was colocalized with 4-hydroxy 2-nonenal (HNE) [26], a marker of lipid peroxidation. Cones with HNE+ COS also show nuclear prolapse (Fig. 5a). This anomaly, and the fact that calbindin D is essentially present in L/M cones [44], suggests that the latter are vulnerable to calcium-mediated toxicity and lipid peroxidation and perhaps lost in advanced aging. Cones with prolapsing nuclei look dark (Fig. 5b), indicating that they may succumb to death. Wandering phagocytes are often seen in the photoreceptor layer (Fig. 5c) under such cases. In animals, cone loss is common in pigmented rats [46], and there is a differential loss of L/M cones in albino mice with aging [47].
Fig. 5. Photoreceptor nuclear prolapse.
a HNE immunoreactivity in COS (arrowheads), note their nuclei (arrows) lie outer to the OLM (right-left arrow). b Electron micrograph showing a dark cone with nuclear prolapse (arrow) outer to the OLM (right-left arrow). c A phagocyte (arrowheads) in the photoreceptor layer, the photoreceptor inner segments are cut transversely (stars). From 84-year-old donor retina.
The aging photoreceptor synaptic terminals often contain small synaptic ribbons [36, 48] (Fig. 6 and Supplementary Fig. 3a–d), swollen mitochondria (Supplementary Fig. 3b–e) and autophagosomes with organelle remnants (Fig. 6 and Supplementary Fig. 3d). There is a redistribution of presynaptic terminal proteins, e.g., vesicular glutamate transporter 1, in distal cone axons [43]. Besides, the L/M-opsin+ cone pedicles retract near the ONL (Fig. 4d). Aging rod terminals also retract into the ONL, where the rod bipolar dendrites extend for rewiring with the retracted rod terminals [49]. A similar situation is reported in AMD [50], suggesting that some aging changes are common with features seen in AMD.
Fig. 6. Electron micrograph of photoreceptor synaptic terminal.
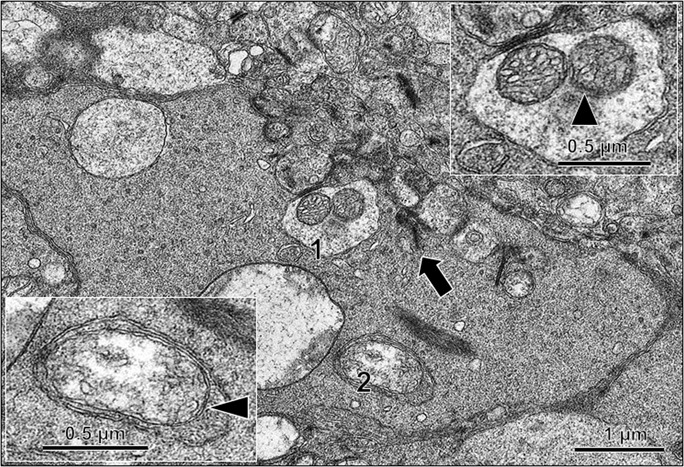
Synaptic ribbons (arrow) are small. Autophagosomes (labelled as 1 and 2) contain partially digested mitochondria (inset, arrowheads; magnified view of 1 and 2). From 84-year-old donor retina.
Pattern of PCD with normal aging
A gradual loss of photoreceptor nuclei is evident with aging [2, 4, 6, 8, 49], which is prominent in the peripheral [2], peripapillary [51] and parafoveal region [5, 6, 8]. Little is known, however, for the cone loss. In the fovea and foveola, fewer cone nuclei are present in ONL at ninth–tenth decade, comparing with that in mid-lifespan [2, 52]. Thus, cone loss may be small in early aging, which becomes prominent at advanced ages. In vivo retinal imaging in younger (22–35 years) versus older subjects (50–65 years) showed a decrease in cone packing density with age at eccentricity 1 mm or less from the foveola [53], which may be related with an age-related decrease in cone acuity. Rarely, dark and highly condensed photoreceptor nuclei, a cardinal feature of apoptosis, are noted in peripheral retina (Fig. 7a, c) and macula with aging [27]. Apoptotic nuclei are phagocytosed instantly and due to the protracted human lifespan, the features of photoreceptor cell apoptosis remain undetected. While photoreceptor nuclei are non-condensed in relatively lower ages (Fig. 7b), with progressive aging, most nuclei are in a midway, i.e. they are neither dark nor shrunken (not shown), which are the late events of apoptosis. Thus, PCD, especially of cones, seems to continue until late ages. This is evident from the appearance of space among the macular photoreceptor cells (Fig. 7d), indicating possible PCD. A major mechanism of cell death is apoptosis, which begins with DNA cleavage and is detected histochemically by terminal deoxynucleotidyl transferase dUTP nick end labelling (TUNEL), which stains nuclei with fragmented DNA. In the macula, while TUNEL staining of ganglion cell nuclei appeared earlier (Fig. 8a), it was absent in ONL of the same retina, but appeared later at ninth–tenth decade (Fig. 8b–e). Few TUNEL+ nuclei were located close to the OLM, implying that cones die in advanced aging by apoptosis. In AMD, apoptosis has been implicated in PCD [54, 55]. Light-induced PCD in animals involves the activation of caspase, a cysteine protease that plays a leading role in execution of apoptosis. Also, caspase-independent pathways (non-apoptotic) are involved in PCD [42, 56]. In AMD, RPE cell loss may occur via apoptosis, necroptosis and pyroptosis [57]. The involvement of caspases and non-apoptotic pathways in human PCD are presently unknown.
Fig. 7. Photoreceptor cell status in aging retina.
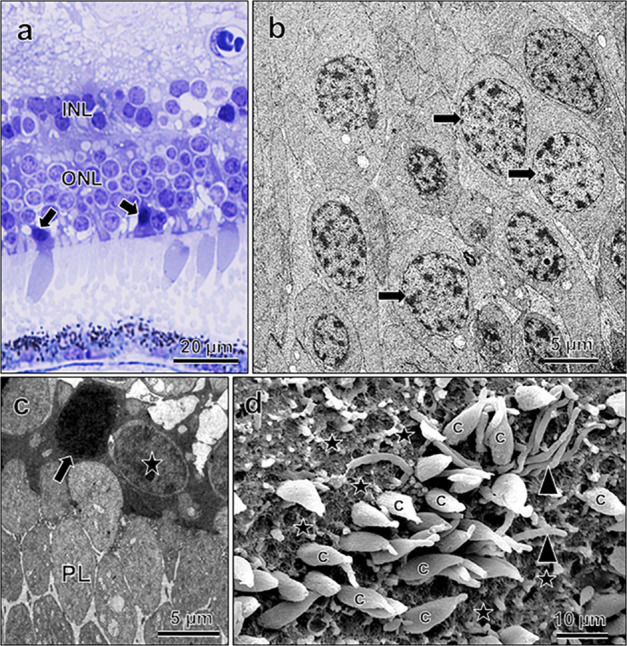
a Light micrograph showing dark, condensed cone nuclei (arrows). Electron micrographs of normal, uncondensed nuclei (b, arrows) and one condensed photoreceptor cell nucleus (c, arrow), note one normal nucleus adjacent to it (star). PL photoreceptor layer (in c). d Scanning electron micrograph of macular photoreceptor cell layer, showing empty spaces (stars), indicating loss of cones (c); note few rods (arrowheads) are present. From 89-year- (a, c; mid-periphery), 62-year- (c, macular), and 89-year- (d; parafoveal region) old retinas.
Fig. 8. Apoptosis in aging retina.
a TUNEL, showing label in macular GCL, but absent in the ONL. b–e Show TUNEL+ photoreceptor nuclei (arrows), a few of them are cone nuclei, being located close to the OLM [arrows in c, enlarged view of lower left part of b]. From 92-year-old donor retina.
By ninth decade of life, about 30% of the total rods die, when cone death is reportedly low [2]. Although signs of cone damage appear well-before the changes are extensive in rods [43], due to unknown reasons, there is an accelerated rod death, sparing the damaged cones that survive longer with aging. It is likely that the rod-derived cone viability factor (RDCVF) [58] influences cone survival in aging retina. Thus, rod loss may risk the cone survival via deprivation of RDCVF. The mRNA for RDCVF was detected in the ONL, whereas the protein product was found in ROS [59]. Assuming that RDCVF expression is an ongoing process, it is likely that changes in either of the ONL and ROS can have a harmful effect on the cones. Its potential use for cone survival in aged human retina remains to be seen.
OS as a prime factor in photoreceptor pathology
The retina has a greater oxygen demand than any other tissues. Owing to its continual exposure to light, and high membrane lipid content, it is prone to be attacked by OS [60, 61]. OS at a low level is counteracted with the efficient retinal defence system comprising antioxidant enzymes, vitamins C and E, glutathione and carotenoids [13, 61–63]. In aged rats, OS attacks the retina when the antioxidants are depleted [64]. In human retina, the activities of most antioxidant enzymes remain stable up to 86 years [63]. This suggests that other factors, e.g. glutathione, carotenoids and micronutrients (selenium) may be involved in photoreceptor vulnerability. Due to OS, lipids and proteins are modified [31, 65]. The macula is susceptible to lipid peroxidation [66], and immunoreactivity to markers of both lipid peroxidation (e.g. (HNE) and protein tyrosine nitration (nitro-tyrosine) was detected in aging human retina [27, 67]. Peroxynitrite, the major culprit in nitrosative stress, is reported to affect the cytoskeleton [68]. Thus, photoreceptor microtubule changes noted with aging [36] may have links with nitrative changes in microtubule proteins.
Drusen may influence photoreceptor cell survival
Besides OS, chronic inflammation associated with the aging retina [69] may be responsible for PCD via formation of drusen. In AMD, PCD occurs in the presence of accumulated drusen in RPE [70]. Significant changes also occur in photoreceptors overlying drusen: there is opsin redistribution in rod inner segments and axons, shortening of L/M opsin+ COS in aging macula [71], altered labelling of synaptic proteins and loss of photoreceptor nuclei impacted by drusen [48] that contain cytotoxic molecules (e.g. amyloid-β). Besides drusen, factors such as nutrients, light and iron toxicity and endogenous antioxidants are likely involved with PCD [62–64, 72].
Photoreceptor cells need protection from light and iron toxicity
Visible light in the blue spectrum is harmful to the retina and initiates PCD [56, 73–77]. PCD is induced by lipid peroxidation [76, 78], and is accompanied by changes in the inner retina [77, 79–81]. Upon reduction of light intensity, PCD subsides and functional recovery begins in the surviving neurons [77, 82]. These facts highlight that exposure to a reduced light level can delay the PCD. Retinal light injury triggers the upregulation of endogenous neuroprotectants, and can be ameliorated via intake of antioxidants, e.g. carotenoids [56, 74, 83]. Currently, it is unknown if there is a reduced synthesis of antioxidants (e.g. glutathione) with aging that may limit neuroprotection under OS. This information may be useful in future therapy to delay PCD.
Besides light, iron toxicity leads to PCD. In animals [84, 85] and in AMD [86], there is an increased retinal iron accumulation, and animal models show AMD-like phenotype upon iron accumulation [87], implying the latter to play a role in AMD pathogenesis [86–89]. Ultimately photoreceptor cells die due to iron toxicity [85, 90]. Iron chelation is suggested to have therapeutic benefits in retinal diseases involving light and iron toxicity [91].
Autophagy in photoreceptor cell survival
Autophagy is a process by which damaged organelles and macromolecules are removed via lysosomal degradation. Although operative in normal physiological conditions [92], autophagy is activated under stress, as in light-induced retinal degeneration, to remove the disorganized organelles and POS [93]. Autophagy is deceased in aging RPE due to lysosomal dysfunctions via lipofuscin accumulation and this plays a role in AMD pathogenesis [20, 94]. Photoreceptor inner segments also generate lipofuscin [25, 95, 96], and the status of autophagy in aging photoreceptor cells remains unknown. However, the presence of autophagosomes with organelle leftovers in cone inner segments [25] and synaptic terminals (present study) may hint for a reduced autophagy in aging photoreceptors, which can affect their survival. Figure 9 is a schematic showing various changes detected in human photoreceptor cells.
Fig. 9. Diagram showing various changes seen in aging photoreceptor cells.
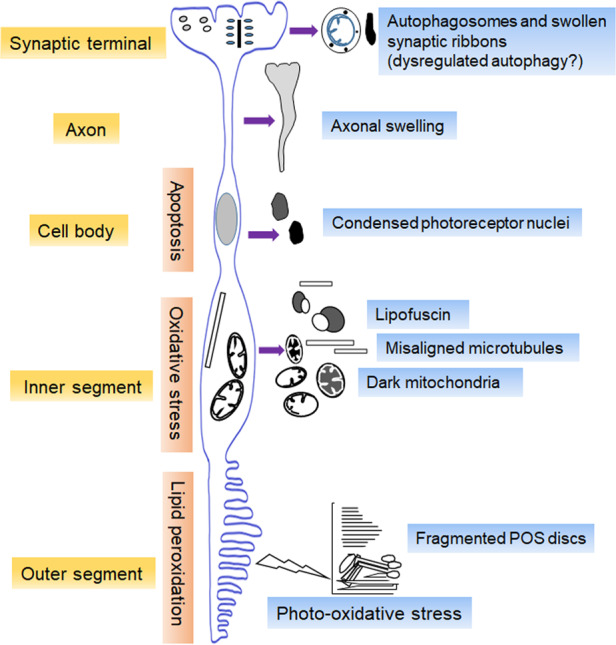
Photo-oxidative stress induces lipid peroxidation and disc fragmentation in POS. Oxidative stress in inner segments causes mitochondrial shrinkage and darkening, and mtDNA deletion. Free radicals escaped from damaged mitochondria supposedly attack the microtubules, causing their distortions and misalignment. Lipofuscin accumulation probably results from the reduced clearance of damaged inner segment organelles. Nuclear condensation and TUNEL positivity denote photoreceptor apoptosis seen sparingly (a late event for aged cones). Besides, cone distal axons show anomalous swellings before terminating into pedicles. They show mislocalized L/M opsin and presynaptic proteins. Autophagosomes with organelle remnants in synaptic terminals may indicate dysregulated autophagy. Thus, aging human photoreceptors are affected by various pathogenic mechanisms that contribute to their vulnerability. Many of those changes have been documented in eyes with AMD.
Strategies to prevent RPE and photoreceptor cell loss
Aging is a risk factor for the development of AMD. Dry AMD is characterized by accumulation of drusen in the macula, RPE atrophy and slow visual loss, which progresses over the years due to mild PCD. RPE loss and PCD become more severe in an advanced state of dry AMD, called geographic atrophy (GA). There is an accumulation of lipofuscin (containing A2E bisretinoid, a photooxidation by-product) within the RPE, resulting from visual cycle activity. This activates the complement system, especially the alternate complement pathway [97], and triggers retinal local inflammation.
There is no proper therapy for dry AMD and GA. Factors such as OS, accumulation of drusen and toxic by-products, and complement activation in RPE were chosen in drug trials [98, 99; Table 1], and while produced variable outcome, they provided rationale for future treatment plans. Drusen contain complement components and proteins (e.g. amyloid-β) related to inflammation. RPE accumulation of lipofuscin stimulates complement activation [97], and animal studies showed that light-induced rod death can be reduced by abolishing the action of the alternative complement pathway [100]. So, drugs/antibodies interfering with drusen accumulation and complement activation have been tested in clinical trials (Table 1). Antibodies against amyloid-β (RN6G and GSK 933776) reduced amyloid-β and drusen load, though no treatment benefits were found [101]. The compound GAL-101 prevents the aggregation of misfolded amyloid-β into toxic forms in vitro, and presently is in a phase 2 trial for GA treatment.
Table 1.
Clinical trials and other approaches to treat dry AMD and GA.
| Drugs/nature | Route of delivery (aim/mechanisms of action) | Sponsors | Clinical phase | Clinicaltrial.Gov identifiers (year of completion) |
|---|---|---|---|---|
| Visual cycle modulators | ||||
| Fenretinide (retinol analogue) | Oral (inhibits binding of retinol) | Sirion Therapeutics | II | NCT00429936 (2010) |
| Emixustat HCl (ACU-4429) SEATTLE | Oral (non-retinoid, inhibits RPE65, blocking conversion of retinol into 11-cis retinal) | Acucela |
II II/III |
NCT01002950 (2014) NCT01802866 (ongoing) |
| ALK-001 (a modified form of vitamin A) | Oral (forms vitamin A dimers slowly) | Alkeus Pharmaceuticals, Inc. | III | NCT03845582 (2022) |
| Suppressors of inflammation and complement activation | ||||
| RN6G |
IVI (binds and eliminates amyloid β) |
Pfizer | I |
NCT00877032 (2015) NCT01003691 (2013) |
| GSK 933776 |
IVI (binds and eliminates amyloid β) |
Glaxo Smith Kline | II | NCT01342926 (2016) |
| GAL-101 (investigational) | Oral (prevents misfolded amyloid β from aggregating into toxic forms in vitro) | Galimedix Therapeutics | II | NA |
| ARC1905 (anti-C5 Aptamer) | IVI (inhibits generation of C5a and MAC). | Ophthotech Corp | I | NCT00950638 (2012, unpublished) |
| Lampalizumab | IVI (mAb against complement factor D) | Chroma and Spectri, Genentech | III | NCT02247531 (terminated in 2018) |
|
Eculizumab (Soliris)/ the COMPLETE study |
iv (mAb against C5, inhibits its cleavage into C5a and C5b and MAC formation) | Alexion Pharmaceuticals | II | NCT00935883 (2013) |
| LFG316 (tesidolumab) | IVI (mAb against C5) | Novartis | II | NCT01527500 (2015, unpublished) |
| LG561 as a monotherapy and in combination with LFG316 | IVI (to reduce progression of GA) | Alcon Research | II | NCT02515942 (2017) |
| Pegcetacoplan (APL-2, a C3 inhibitor) | IVI (prevents C3 cleavage and cell lysis) | Apellis Pharmaceuticals | II | NCT02503332 (2018) |
| Doxycycline (ORACEA®, TOGA) | Oral (suppression of low-grade inflammation) | Paul Yates, University of Virginia | II/III | NCT01782989 (2020) |
| GEM103, full-length recombinant complement factor H protein | IVI (complement modulator; safety and tolerability of a single dose) | Gemini Therapeutics, Inc. | I | NCT04246866 (2020) |
| Zimura (anti-C5 aptamer) | IVI (to halt progression of GA) | IVERIC bio, Inc. | II/III | NCT02686658 (2020) |
| Stem cells | ||||
| CNTO 2476 (umbilical-cord-derived stem cells) | SRT (safety and response to improve visual acuity) in patients with GA | Janssen Research & Development, LLC | I/II | NCT01226628 (2017) |
| MA09-hRPE | SRT (safety and tolerability of hESC-derived RPE cells) |
Astellas Pharma Inc CHABiotech CO., Ltd |
I/II I/IIa |
NCT02463344 (2019) NCT01674829 (2020) |
| OpRegen | SRT (safety and tolerability of hESC-derived RPE cells under dose-escalation) | Lineage Cell Therapeutics, Inc. | I/IIa | NCT02286089 (2024) |
| GT005 (recombinant AAV that encodes a human complement factor I, FocuS) | SRT (increases production of the complement factor I, safety and efficacy of three doses) | Gyroscope Therapeutics | I/II | NCT03846193 (recruiting, 2025) |
| AAVCAGsCD59 | IVI (increases the expression of a soluble form of CD59, safety and efficacy of three doses) | Hemera Biosciences | I | NCT03144999 (2019) |
| iPSC-derived RPE | SRT (safety and efficacy data for future studies) | National Eye Institute (USA) | I/IIa | NCT04339764 (recruiting; 2029) |
| Antioxidants, mitochondrial enhancers and PBM | ||||
| Age-related Eye Disease Study (AREDS) 2 formulation |
Oral (AREDS formulation + lutein + zeaxanthin + docosahexaenoic acid + eicosapentaenoic acid), to reduce the risk of progression to advanced AMD Secondary goal: to test the effects of eliminating β-carotene and reducing zinc content in AREDS formulation. |
National Eye Institute (USA) | III | NCT00345176 (2012) |
| NT-501 (encapsulated human RPE-derived cells releasing CNTF) | IVI (to rescue photoreceptors) | Neurotech Pharmaceuticals | II | NCT00447954 (2011) |
| Brimonidine tartrate (α-2 adrenergic receptor agonist) | IVI (to reduce apoptosis) | Allergan | II | NCT00658619 (2013) |
| Omega-3 fatty acids (MADEOS; antioxidants) | Oral (to see therapeutic potential) | Ophthalmos Research and Education Institute, Cyprus | NA | NCT03297515 (2020) |
| Curcumin (Longvida curcumin; antioxidant) | Oral (to see impact on drusen volume) | University of Illinois at Chicago | I | NCT04590196 (recruiting; 2021) |
|
MTP-131 (Ocuvia™, ophthalmic solution) MTP-131 (elamipretide) ReCLAIM-2 study |
Topical (targets cardiolipin and preserves mitochondrial functions) Subcutaneous injection daily for 48 weeks |
Stealth BioTherapeutics Inc. |
I/II II |
NCT02314299 (2015) NCT03891875 (2022) |
| Metformin |
Oral (activates mitochondrial PGC-1α, efficacy in non-diabetic patients with GA) |
University of California, San Francisco | II | NCT02684578 (recruiting; 2021) |
| PBM |
670-nm LED light (activates cytochrome C oxidase; to increase ATP generation and improve mitochondrial function) 590, 670 and 790-nm LED light (to reduce drusen volume) |
[32, 33, 108] |
NA NA |
NA NA |
| PBM (The Valeda™ Light Delivery System, LIGHTSITE III | 590, 660 and 850-nm LED light (safety and efficacy in dry AMD) | LumiThera, Inc. | NA | NCT04065490 (2022) |
AAV adeno-associated viral vector, iv Intravenous, IVI intravitreal injection, iPSC induced pluripotent stem cell, hESC human embryonic stem cells, mAb monoclonal antibody, NA not applicable, SRT subretinal transplantation.
Lipofuscin granules are the visual cycle by-products and accumulate in the diseased RPE. Visual cycle modulators were tested if they can reduce the level of toxic by-products. Fenretinide showed some benefit, although it causes slow adaptation to dark. Emixustat hydrochloride inhibits the activity of RPE65 and reduces the buildup of 11-cis retinol and conversion into rhodopsin. Although safe, this drug was also found to be ineffective [102]. ALK-001, a modified form of vitamin A, is in phase III trial to find its efficacy in visual cycle modulation (Table 1).
Because complement activation plays a role in AMD pathogenesis, selective inhibitors of the complement cascade were tested. C5 inhibition prevents the formation of the pro-inflammatory C5a and the membrane attack complex (MAC) that initiates tissue lysis. ARC1905 (anti-C5 aptamer) and antibodies against complement factor D (lampalizumab) [103] and C5 (eculizumab and LFG316) inhibited MAC formation, though there were no benefits. LFG316 was studied in combination with CLG561 (neutralizes properdin thereby destabilizing the activities of the alternate complement pathway); however, no results were published. CD59 inhibits the formation of the MAC and gene delivery using AAVCAGsCD59 vector is found to cause an increased expression of a soluble form of CD59 in phase 1 trial that ended in 2019. Pegcetacoplan, a C3 inhibitor showed efficacy in reducing the progression of GA [104]. Trials with doxycycline and zimura (an anti-C5 aptamer) to find their efficacy in suppressing inflammation were completed in 2020.
Besides, antioxidants, neuroprotective agents, mitochondrial enhancers, stem cells and light stimulation have been used (Table 1). Earlier, oral supplement with the Age-related Eye Disease Study (AREDS) formulation (β-carotene, vitamins C and E, zinc and copper) was proven to be useful in patients with AMD [105]. The AREDS2 added lutein + zeaxanthin + docosahexaenoic acid + eicosapentaenoic acid to the original formulation, and the long-term safety profile of this formulation remains to be seen [106]. A clinical trial evaluated the therapeutic potential of omega-3 fatty acids alone in dry AMD (MADEOS). Intravitreal CNTF (produced by encapsulated human RPE-derived cells) and brimonidine tartrate showed benefit in reducing cell loss in clinical trials. MTP-131, a mitochondrial protectant was tested in phase I/II trials and showed efficacy in preventing damage, and there is an ongoing phase II trial to see its efficacy via subcutaneous injection. Two clinical trials examined the efficacy of human embryonic stem cells in regeneration of RPE in dry AMD and GA (Table 1) and the results are awaited. A third clinical trial (NCT02286089) and one with induced pluripotent stem cells are active (NCT04339764). Earlier, a trial with umbilical-cord-derived stem cells (CNTO 2376) was completed in 2017.
Recently, ocular effects of near infra-red light generated from light-emitting diodes (PBM) have been tested in aging individuals and patients with AMD. PBM stimulates cytochrome C oxidase expression and mitochondrial ATP production in photoreceptors [107], reduces drusen volume [108] and improves visual function [33]. These findings suggest that PBM can be a possible way for treating retinal changes in aging and diseases.
Future perspectives
Although it is recognized that the adult human photoreceptor cells possess a striking capacity for survival [109], they become vulnerable in the course of aging due to attack by oxidative and nitrosative stress. Lipid peroxidation can interfere with POS renewal, as HNE-modified POS membrane proteins show a reduced clearance of damaged POS [110]. So, factors interfering with POS renewal can be investigated.
As dysfunctional mitochondria accumulate due to reduced autophagy in aging and diseases, researches can provide clues as to how mitophagy can be activated in aging RPE and photoreceptor cells.
PCD is an index of retinal aging and diseases. Presently, suitable animal models for dry AMD are unavailable, so clinical trials and different approaches to reduce cell damage and loss seem rational. The fact that trials with complement inhibitors showed limited benefit tends to emphasize that many detailed steps of RPE inflammation and complement activation remain to be known. It is hoped that basic research to divulge the causes of cell death in aging and diseases along with clinical trials will guide toward an effective therapy for AMD.
Summary
What is known about this topic
Oxidative and nitrosative stress are involved in age-related photoreceptor cell alterations, which may stem from light and iron toxicity and other sources.
Lipid peroxidation in human photoreceptor outer segments and mitochondrial abnormalities in photoreceptor inner segments may drive the aging photoreceptors towards vulnerability, as in diseases.
Increasing vulnerability of the long/middle wavelength opsin positive cones with aging is evident in human retina.
There are signs of reduced autophagy in aging human photoreceptors.
What this study adds
A number of pathogenic factors influence the survival of human photoreceptor cells with aging.
Mechanisms of cone vulnerability suggest it to be a slow process, so there are opportunities to rejuvenate cones before they die.
A full understanding of the possible molecular pathways involved in cone survival must be the future research goal.
Supplementary information
Acknowledgements
The work was supported by grants from the DBT (BT/PR10195/BRB/10/589/2007), SERB (SERB-AS-27/2012) and CSIR (No. 37/1593/13/EMR-II), New Delhi, India. The eyes were procured from National Eye Bank, AIIMS via approval of Institute human Ethics Committee (No. IEC/NP-57/2010). The protocol adhered to the tenets of Helsinki Declarations. TEM work was done at SAIF-New Delhi, AIIMS.
Compliance with ethical standards
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41433-021-01602-1.
References
- 1.Luthert PJ, Chong NHV. Photoreceptor rescue. Eye. 1998;12:591–6. doi: 10.1038/eye.1998.149. [DOI] [PubMed] [Google Scholar]
- 2.Gartner S, Henkind P. Aging and degeneration of the human macula: 1. outer nuclear and photoreceptors. Br J Ophthalmol. 1981;65:23–8. doi: 10.1136/bjo.65.1.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dorey CK, Wu G, Ebenstein D, Garsd A, Weiter JJ. Cell loss in the aging retina: relationship to lipofuscin accumulation and macular degeneration. Invest Ophthalmol Vis Sci. 1989;30:1691–9. [PubMed] [Google Scholar]
- 4.Gao H, Hollyfield JG. Aging of the human retina. Invest Ophthalmol Vis Sci. 1992;33:1–17. [PubMed] [Google Scholar]
- 5.Curcio CA, Millican CL, Allen KA, Kalina RE. Ageing of the human photoreceptor mosaic: evidence for selective vulnerability of rods in central retina. Invest Ophthalmol Vis Sci. 1993;34:3278–96. [PubMed] [Google Scholar]
- 6.Panda-Jonas S, Jonas JB, Jakobczyk-Zmija M. Retinal photoreceptor density decreases with age. Ophthalmology. 1995;102:1853–59. doi: 10.1016/S0161-6420(95)30784-1. [DOI] [PubMed] [Google Scholar]
- 7.Stone J, Maslim J, Valter-Kocsi K, Mervin K, Bowers F, Chu Y, et al. Mechanisms of photoreceptor death and survival in mammalian retina. Prog Ret Eye Res. 1999;18:689–735. doi: 10.1016/S1350-9462(98)00032-9. [DOI] [PubMed] [Google Scholar]
- 8.Jackson GR, Owsley C, Curcio CA. Photoreceptor degeneration and dysfunction in aging and age-related maculopathy. Ageing Res Rev. 2002;1:381–96. doi: 10.1016/S1568-1637(02)00007-7. [DOI] [PubMed] [Google Scholar]
- 9.Pierce EA. Pathways to photoreceptor cell death in inherited retinal degenerations. Bioessays. 2001;23:605–18. doi: 10.1002/bies.1086. [DOI] [PubMed] [Google Scholar]
- 10.Marshall J, Grindle J, Ansell PL, Borwein B. Convolution in human rods: an ageing process. Br J Ophthalmol. 1979;63:181–7. doi: 10.1136/bjo.63.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nag TC, Wadhwa S. Ultrastructure of the human retina in aging and various pathological states. Micron. 2012;43:759–81. doi: 10.1016/j.micron.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 12.Sommerburg OG, Siems WG, Hurst JS. Lutein and zeaxanthin are associated with photoreceptors in the human retina. Curr Eye Res. 1999;19:491–5. doi: 10.1076/ceyr.19.6.491.5276. [DOI] [PubMed] [Google Scholar]
- 13.Rapp LM, Maple SS, Choi JH. Lutein and zeaxanthin concentrations in rod outer segment membranes from perifoveal and peripheral human retina. Invest Ophthalmol Vis Sci. 2000;41:1200–9. [PubMed] [Google Scholar]
- 14.LaVail MM, Unoki K, Yasumura D, Matthes MT, Yancopoulos GD, Steinberg RH. Multiple growth factors, cytokines, and neurotrophins rescue photoreceptors from the damaging effects of constant light. Proc Natl Acad Sci U S A. 1992;89:11249–53. doi: 10.1073/pnas.89.23.11249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Li Y, Tao W, Luo L, Huang D, Kauper K, Stabila P, et al. CNTF induces regeneration of cone outer segments in a rat model of retinal degeneration. PLoS ONE. 2010;5:e9495. doi: 10.1371/journal.pone.0009495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Xia X, Li Y, Huang D, Wang Z, Luo L, Song Y, et al. Oncostatin M protects rod and cone photoreceptors and promotes regeneration of cone outer segment in a rat model of retinal degeneration. PLoS ONE. 2011;6:e18282. doi: 10.1371/journal.pone.0018282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horton JC, Parker AB, Botelho JV, Duncan JL. Spontaneous regeneration of human photoreceptor outer segments. Sci Rep. 2015;5:12364. doi: 10.1038/srep12364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sieving PA, Caruso RC, Tao W, Coleman HR, Thompson DJS, Fullmer KR, et al. Ciliary neurotrophic factor (CNTF) for human retinal degeneration: phase I trial of CNTF delivered by encapsulated cell intraocular implants. Proc Natl Acad Sci U S A. 2006;103:3896–901. doi: 10.1073/pnas.0600236103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Young RW, Bok D. Participation of the retinal pigment epithelium in the rod outer segment renewal process. J Cell Biol. 1969;42:392–403. doi: 10.1083/jcb.42.2.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrington DA, Sinha D, Kaarniranta K. Defects in retinal pigment epithelial cell proteolysis and the pathology associated with age-related macular degeneration. Prog Ret Eye Res. 2016;51:69–89. doi: 10.1016/j.preteyeres.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Inana G, Murat C, An W, Yao X, Harris IR, Cao J. RPE phagocytic function declines in age-related macular degeneration and is rescued by human umbilical tissue derived cells. J Trans Med. 2018;16:63. doi: 10.1186/s12967-018-1434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hogan MJ, Alvarado, JA, Weddell JE. Histology of the human eye: an Atlas and Textbook. Philadelphia: Saunders; 1971.
- 23.Hoang QV, Linsenmeier RA, Chung CK, Curcio CA. Photoreceptor inner segments in monkey and human retina: mitochondrial density, optics, and regional variation. Vis Neurosci. 2002;19:395–407. doi: 10.1017/S0952523802194028. [DOI] [PubMed] [Google Scholar]
- 24.Nag TC, Wadhwa S, Chaudhury S. The occurrence of cone inclusions in the ageing human retina and their possible effect upon vision: an electron microscope study. Brain Res Bull. 2016;71:224–32. doi: 10.1016/j.brainresbull.2006.09.007. [DOI] [PubMed] [Google Scholar]
- 25.Nag TC, Wadhwa S. Immunolocalisation pattern of complex I–V in ageing human retina: correlation with mitochondrial ultrastructure. Mitochondrion. 2016;31:20–32. doi: 10.1016/j.mito.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 26.Nag TC, Kumar P, Wadhwa S. Age related distribution of 4-hydroxy 2-nonenal immunoreactivity in human retina. Exp Eye Res. 2017;165:25–35. doi: 10.1016/j.exer.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 27.Nag TC, Kathpalia P, Gorla S, Wadhwa S. Localization of nitro-tyrosine immunoreactivity in human retina. Ann Anat. 2019;223:8–18. doi: 10.1016/j.aanat.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 28.Barron MJ, Johnson MA, Andrews RM, Clarke MP, Griffiths PG, Bristow E, et al. Mitochondrial abnormalities in aging macular photoreceptors. Invest Ophthalmol Vis Sci. 2001;42:3016–22. [PubMed] [Google Scholar]
- 29.Jarrett SG, Lin H, Godley BF, Boulton ME. Mitochondrial DNA damage and its potential role in retinal degeneration. Prog Ret Eye Res. 2008;27:596–607. doi: 10.1016/j.preteyeres.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 30.Kenney MC, Atilano SR, Boyer D, Chwa M, Chak G, Chinichian S, et al. Characterization of retinal and blood mitochondrial DNA from age-related macular degeneration Patients. Invest Ophthalmol Vis Sci. 2010;51:4289–97. doi: 10.1167/iovs.09-4778. [DOI] [PubMed] [Google Scholar]
- 31.Ethen CM, Reilly C, Feng X, Olsen TW, Ferrington DA. Age-related macular degeneration and retinal protein modification by 4-hydroxy-2-nonenal. Invest Ophthalmol Vis Sci. 2007;48:3469–79. doi: 10.1167/iovs.06-1058. [DOI] [PubMed] [Google Scholar]
- 32.Sivapathasuntharam C, Sivaprasad S, Hogg C, Jeffery G. Improving mitochondrial function significantly reduces the rate of age related photoreceptor loss. Exp Eye Res. 2019;185:107691. doi: 10.1016/j.exer.2019.107691. [DOI] [PubMed] [Google Scholar]
- 33.Shinhmar H, Grewal M, Sivaprasad S, Hogg C, Chong V, Neveu M, et al. Optically improved mitochondrial function redeems aged human visual decline. J Gerontol A Biol Sci Med Sci. 2020;75:e49–52. doi: 10.1093/gerona/glaa155. [DOI] [PubMed] [Google Scholar]
- 34.Ebeling MC, Polanco JR, Qu J, Tu C, Montezuma SR, Ferrington DA. Improving retinal mitochondrial function as a treatment for age-related macular degeneration. Redox Biol. 2020;34:101552. doi: 10.1016/j.redox.2020.101552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eckmiller MS. Defective cone photoreceptor cytoskeleton, alignment, feedback, and energetics can lead to energy depletion in macular degeneration. Prog Ret Eye Res. 2004;23:495–522. doi: 10.1016/j.preteyeres.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 36.Nag TC, Kathpalia P, Wadhwa D. Microtubule alterations may destabilize photoreceptor integrity: age-related microtubule changes and pattern of expression of MAP-2, Tau and hyperphosphorylated Tau in aging human photoreceptor cells. Exp Eye Res. 2020;198:108153. doi: 10.1016/j.exer.2020.108153. [DOI] [PubMed] [Google Scholar]
- 37.Haley TL, Pochet R, Baizer L, Burton MD, Crabb JW, Parmentier M, et al. Calbindin D-28K immunoreactivity of human cone cells varies with retinal position. Vis Neurosci. 1995;12:301–7. doi: 10.1017/S0952523800007987. [DOI] [PubMed] [Google Scholar]
- 38.Nag TC, Wadhwa S. Calbindin and parvalbumin immunoreactivity in the developing and adult human retina. Dev Brain Res. 1996;93:23–32. doi: 10.1016/0165-3806(96)00011-9. [DOI] [PubMed] [Google Scholar]
- 39.Nag TC, Wadhwa S. Developmental expression of calretinin immunoreactivity in the human retina and a comparison with two other EF-hand calcium-binding proteins. Neuroscience. 1999;91:41–50. doi: 10.1016/S0306-4522(98)00654-X. [DOI] [PubMed] [Google Scholar]
- 40.Pow DV, Sullivan RK. Nuclear kinesis, neurite sprouting and abnormal axonal projections of cone photoreceptors in the aged and AMD-afflicted human retina. Exp Eye Res. 2007;84:850–7. doi: 10.1016/j.exer.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Krizaj D. Calcium stores in vertebrate photoreceptors. Adv Exp Med Biol. 2012;740:873–89. doi: 10.1007/978-94-007-2888-2_39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Doonan F, Donovan M, Cotter TG. Activation of multiple pathways during photoreceptor apoptosis in the rd mouse. Invest Ophthalmol Vis Sci. 2005;46:3530–8. doi: 10.1167/iovs.05-0248. [DOI] [PubMed] [Google Scholar]
- 43.Shelley EJ, Madigan MC, Natoli R, Penfold PL, Provis JM. Cone degeneration in aging and age-related macular degeneration. Arch Ophthalmol. 2009;127:483–92. doi: 10.1001/archophthalmol.2008.622. [DOI] [PubMed] [Google Scholar]
- 44.Chiquet C, Dkhissi-Benyahya O, Chounlamountri N, Szel A, Degrip WJ, Cooper HM. Characterization of calbindin-positive cones in primates. Neuroscience. 2002;115:1323–33. doi: 10.1016/S0306-4522(02)00327-5. [DOI] [PubMed] [Google Scholar]
- 45.Weinrich TW, Powner MB, Lynch A, Jonnal RS, Werner JS, Jeffery G. No evidence for loss of short wavelength sensitive cone photoreceptors in normal ageing of the primate retina. Sci Rep. 2017;7:46346. doi: 10.1038/srep46346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nadal-Nicolás FM, Vidal-Sanz M, Agudo-Barriuso M. The aging rat retina: from function to anatomy. Neurobiol Aging. 2018;61:146–68. doi: 10.1016/j.neurobiolaging.2017.09.021. [DOI] [PubMed] [Google Scholar]
- 47.Cunea A, Powner MB, Jeffery G. Death by color: differential cone loss in the aging mouse retina. Neurobiol Aging. 2014;35:2584–91. doi: 10.1016/j.neurobiolaging.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 48.Johnson PT, Brown MN, Pulliam BC, Anderson DH, Johnson LV. Synaptic pathology, altered gene expression, and degeneration in photoreceptors impacted by drusen. Invest Ophthalmol Vis Sci. 2005;46:4788–95. doi: 10.1167/iovs.05-0767. [DOI] [PubMed] [Google Scholar]
- 49.Eliasieh K, Liets LC, Chalupa LM. Cellular reorganization in the human retina during normal aging. Invest Ophthalmol Vis Sci. 2007;48:2824–30. doi: 10.1167/iovs.06-1228. [DOI] [PubMed] [Google Scholar]
- 50.Sullivan RK, Woldemussie E, Pow DV. Dendritic and synaptic plasticity of neurons in the human age-related macular degeneration retina. Invest Ophthalmol Vis Sci. 2007;48:2782–91. doi: 10.1167/iovs.06-1283. [DOI] [PubMed] [Google Scholar]
- 51.Curcio CA, Saunders PL, Younger PW, Malek G. Peripapillary chorioretinal atrophy: Bruch’s membrane changes and photoreceptor loss. Ophthalmology. 2000;107:334–43. doi: 10.1016/S0161-6420(99)00037-8. [DOI] [PubMed] [Google Scholar]
- 52.Feeney-Burns L, Burns RP, Gao C-L. Age-related macular changes in humans over 90 years old. Am J Ophthalmol. 1990;109:265–78. doi: 10.1016/S0002-9394(14)74549-0. [DOI] [PubMed] [Google Scholar]
- 53.Song H, Ping Chui TY, Zhong Z, Elsner AE, Burns SA. Variation of cone photoreceptor packing density with retinal eccentricity and age. Invest Ophthalmol Vis Sci. 2011;52:7376–84. doi: 10.1167/iovs.11-7199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tso MOM, Xu GZ, Li WWY. Apoptosis in human retinal degenerations. Trans Am Ophthalmol Soc. 1996;154:411–30. [PMC free article] [PubMed] [Google Scholar]
- 55.Dunaief JL, Dentchev T, Ying G-S, Milam AH. The role of apoptosis in age-related macular degeneration. Arch Ophthalmol. 2002;120:1435–42. doi: 10.1001/archopht.120.11.1435. [DOI] [PubMed] [Google Scholar]
- 56.Wenzel A, Grimm C, Samardzija M, Remé CE. Molecular mechanisms of light-induced photoreceptor apoptosis and neuroprotection for retinal degeneration. Prog Ret Eye Res. 2005;24:275–306. doi: 10.1016/j.preteyeres.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 57.Kaarniranta K, Tokarz P, Koskela A, Paterno J, Blasiak J. Autophagy regulates death of retinal pigment epithelium cells in age-related macular degeneration. Cell Biol Toxicol. 2017;33:113–28. doi: 10.1007/s10565-016-9371-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mohand-Said S, Deudon-Combe A, Hicks D, Simonutti M, Forster V, Fintz AC, et al. Normal retina releases a diffusible factor stimulating cone survival in the retinal degeneration mouse. Proc Natl Acad Sci U S A. 1998;95:8357–62. doi: 10.1073/pnas.95.14.8357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leveillard T, Mohand-Said S, Lorentz O, Hicks D, Fintz AC, Clérin E, et al. Identification and characterization of rod-derived cone viability factor. Nat Genet. 2004;36:755–9. doi: 10.1038/ng1386. [DOI] [PubMed] [Google Scholar]
- 60.Beatty S, Koh H, Phil M, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2002;45:115–34. doi: 10.1016/S0039-6257(00)00140-5. [DOI] [PubMed] [Google Scholar]
- 61.Handa JT. How does the macula protect itself from oxidative stress? Mol Asp Med. 2012;33:418–35. doi: 10.1016/j.mam.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Snodderly DM. Evidence for protection against age-related macular degeneration by carotenoids and antioxidant vitamins. Am J Clin Nutr. 1995;62:1448S–61S. doi: 10.1093/ajcn/62.6.1448S. [DOI] [PubMed] [Google Scholar]
- 63.De La Paz MA, Zhang J, Fridovich I. Antioxidant enzymes of the human retina: effect of age on enzyme activity of macula and periphery. Curr Eye Res. 1996;15:273–8. doi: 10.3109/02713689609007621. [DOI] [PubMed] [Google Scholar]
- 64.El-Sayyad HI, Khalifa SA, El-Sayyad FI, Mousa SA, Mohammed EAM. Analysis of fine structure and biochemical changes of retina during aging of Wistar albino rats. Clin Exp Ophthalmol. 2014;42:169–81. doi: 10.1111/ceo.12123. [DOI] [PubMed] [Google Scholar]
- 65.Kapphahn RJ, Giwa BM, Berg KM, Roehrich H, Feng X, Olsen TW, et al. Retinal proteins modified by 4-hydroxynonenal: identification of molecular targets. Exp Eye Res. 2006;83:165–75. doi: 10.1016/j.exer.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 66.De La Paz MA, Anderson RE. Regional and age-dependent variation in susceptibility of the human retina to lipid peroxidation. Invest Ophthalmol Vis Sci. 1992;33:3497–9. [PubMed] [Google Scholar]
- 67.Nag TC, Wadhwa S, Alladi PA, Sanyal T. Localisation of 4-hydroxy 2 nonenal immunoreactivity in ageing human retinal Müller cells. Ann Anat. 2011;193:205–10. doi: 10.1016/j.aanat.2011.02.004. [DOI] [PubMed] [Google Scholar]
- 68.Szabo C, Ischiropoulos H, Radi R. Peroxynitrite: biochemistry, pathophysiology and development of therapeutics. Nat Rev Drug Discov. 2007;6:662–80. doi: 10.1038/nrd2222. [DOI] [PubMed] [Google Scholar]
- 69.Anderson DH, Mullins RF, Hageman GS, Johnson LV. A role for local inflammation in the formation of drusen in the aging eye. Am J Ophthalmol. 2002;134:411–31. doi: 10.1016/S0002-9394(02)01624-0. [DOI] [PubMed] [Google Scholar]
- 70.Curcio CA, Medeiros NE, Millican CL. Photoreceptor loss in age-related macular degeneration. Invest Ophthalmol Vis Sci. 1996;37:1236–49. [PubMed] [Google Scholar]
- 71.Johnson PT, Lewis GP, Talaga KC, Brown MN, Kappel PJ, Fisher SK, et al. Drusen-associated degeneration in the retina. Invest Ophthalmol Vis Sci. 2003;44:4481–88. doi: 10.1167/iovs.03-0436. [DOI] [PubMed] [Google Scholar]
- 72.Hahn P, Ying GS, Beard J, Dunaief JL. Iron levels in human retina: sex difference and increase with age. Neuroreport. 2006;17:1803–6. doi: 10.1097/WNR.0b013e3280107776. [DOI] [PubMed] [Google Scholar]
- 73.Noell WK, Walker VS, Kang BS, Berman S. Retinal damage by light in rats. Invest Ophthalmol. 1966;5:450–73. [PubMed] [Google Scholar]
- 74.Organisciak DT, Vaughan DK. Retinal light damage: mechanisms and protection. Prog Ret Eye Res. 2010;29:113–34. doi: 10.1016/j.preteyeres.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jha KA, Nag TC, Kumar V, Kumar P, Kumar B, Wadhwa S, et al. Differential expression of AQP1 and AQP4 in avascular chick retina exposed to moderate light of variable photoperiods. Neurochem Res. 2015;40:2153–66. doi: 10.1007/s11064-015-1698-7. [DOI] [PubMed] [Google Scholar]
- 76.Natoli R, Jiao H, Barnett NL, Fernando N, Valter K, Provis JM, et al. A model of progressive photo-oxidative degeneration and inflammation in the pigmented C57BL/6J mouse retina. Exp Eye Res. 2016;147:114–27. doi: 10.1016/j.exer.2016.04.015. [DOI] [PubMed] [Google Scholar]
- 77.Gupta CL, Nag TC, Jha KA, Kathpalia P, Maurya M, Kumar P, et al. Changes in the inner retinal cells after intense and constant light exposure in Sprague-Dawley rats. Photochem Photobiol. 2020;96:1061–73. doi: 10.1111/php.13244. [DOI] [PubMed] [Google Scholar]
- 78.Wiegand RD, Giusto NM, Rapp LM, Anderson RE. Evidence for rod outer segment lipid peroxidation following constant illumination of the rat retina. Invest Ophthalmol Vis Sci. 1983;24:1433–35. [PubMed] [Google Scholar]
- 79.Grosche J, Härtig W, Reichenbach A. Expression of glial fibrillary acidic protein (GFAP), glutamine synthetase (GS), and Bcl-2 protooncogene protein by Müller (glial) cells in retinal light damage of rats. Neurosci Lett. 1995;185:119–22. doi: 10.1016/0304-3940(94)11239-F. [DOI] [PubMed] [Google Scholar]
- 80.Montalbán-Soler L, Alarcón-Martínez L, Jiménez-López M, Salinas-Navarro M, Galindo-Romero C, Bezerra de Sá F, et al. Retinal compensatory changes after light damage in albino mice. Mol Vis. 2012;18:675–93. [PMC free article] [PubMed] [Google Scholar]
- 81.Samardzija M, Todorova V, Gougoulakis L, Barben M, Nötzli S, Klee K, et al. Light stress affects cones and horizontal cells via rhodopsin-mediated mechanisms. Exp Eye Res. 2019;186:107719. doi: 10.1016/j.exer.2019.107719. [DOI] [PubMed] [Google Scholar]
- 82.Jozwick C, Valter K, Stone J. Reversal of functional loss in the P23H-3 rat retina by management of ambient light. Exp Eye Res. 2006;83:1074–80. doi: 10.1016/j.exer.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 83.Bernstein PS, Khachik F, Carvalho LS, Muir GJ, Zhao DY, Katz NB, et al. Identification and quantitation of carotenoids and their metabolites in the tissues of the human eye. Exp Eye Res. 2001;72:215–23. doi: 10.1006/exer.2000.0954. [DOI] [PubMed] [Google Scholar]
- 84.Hahn P, Song Y, Ying GS, He X, Beard J, Dunaief JL. Age-dependent and gender-specific changes in mouse tissue iron by strain. Exp Gerontol. 2009;44:594–600. doi: 10.1016/j.exger.2009.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kumar P, Nag TC, Jha KA, Dey SK, Kathpalia P, Maurya M, et al. Experimental oral iron administration: Histological investigations and expressions of iron handling proteins in rat retina with aging. Toxicology. 2017;392:22–31. doi: 10.1016/j.tox.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 86.Hahn P, Milam AH, Dunaief JL. Maculas affected by age-related macular degeneration contain increased chelatable iron in the retinal pigment epithelium and Bruch’s membrane. Arch Ophthalmol. 2003;121:1099–105. doi: 10.1001/archopht.121.8.1099. [DOI] [PubMed] [Google Scholar]
- 87.Gnana-Prakasam JP, Martin PM, Smith SB, Ganapathy V. Expression and function of iron-regulatory proteins in retina. IUBMB Life. 2010;62:363–70. doi: 10.1002/iub.326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Biesemeier A, Yoeruek E, Eibl O, Schraermeyer U. Iron accumulation in Bruch’s membrane and melanosomes of donor eyes with age-related macular degeneration. Exp Eye Res. 2015;137:39–49. doi: 10.1016/j.exer.2015.05.019. [DOI] [PubMed] [Google Scholar]
- 89.Picard E, Ranchon-Cole I, Jonet L, Beaumont C, Behar-Cohen F, Courtois Y, et al. Light-induced retinal degeneration correlates with changes in iron metabolism gene expression, ferritin level, and aging. Invest Ophthalmol Vis Sci. 2011;52:1261–74. doi: 10.1167/iovs.10-5705. [DOI] [PubMed] [Google Scholar]
- 90.Rogers BS, Symons RCA, Komeima K, Shen J, Xiao W, Swaim ME, et al. Differential sensitivity of cones to iron-mediated oxidative damage. Invest Ophthalmol Vis Sci. 2007;48:438–45. doi: 10.1167/iovs.06-0528. [DOI] [PubMed] [Google Scholar]
- 91.Shu W, Dunaief JL. Potential treatment of retinal diseases with iron chelators. Pharmaceuticals. 2018;11:112. doi: 10.3390/ph11040112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Remé CE. Autography in visual cells and pigment epithelium. Invest Ophthalmol Vis Sci. 1977;16:807–14. [PubMed] [Google Scholar]
- 93.Chen Y, Sawada O, Kohno H, Le YZ, Subauste C, Maeda T, et al. Autophagy protects the retina from light-induced degeneration. J Biol Chem. 2013;288:7506–18. doi: 10.1074/jbc.M112.439935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mitter SK, Song C, Qi X, Mao H, Rao H, Akin D, et al. Dysregulated autophagy in the RPE is associated with increased susceptibility to oxidative stress and AMD. Autophagy. 2014;10:1989–2005. doi: 10.4161/auto.36184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Tucker GS. Refractile bodies in the inner segments of cones in the aging human retina. Invest Ophthalmol Vis Sci. 1986;27:708–15. [PubMed] [Google Scholar]
- 96.Iwasaki M, Inomata H. Lipofuscin granules in human photoreceptor cells. Invest Ophthalmol Vis Sci. 1988;29:671–9. [PubMed] [Google Scholar]
- 97.Zhou J, Jang YP, Kim SR, Sparrow JR. Complement activation by photooxidation products of A2E, a lipofuscin constituent of the retinal pigment epithelium. Proc Natl Acad Sci U S A. 2006;103:16182–87. doi: 10.1073/pnas.0604255103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boyer DS, Rosenfield PJ. New pathways for dry AMD treatment. Several potential therapies are in clinical trials. Ret Physician. 2019;16:24–5. [Google Scholar]
- 99.Park DH, Connor KM, Lambris JD. The challenges and promise of complement therapeutics for ocular diseases. Front Immunol. 2019;10:1007. doi: 10.3389/fimmu.2019.01007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Rohrer B, Guo Y, Kunchithapautham K, Gilkeson GS. Eliminating complement factor D reduces photoreceptor susceptibility to light-induced damage. Invest Ophthalmol Vis Sci. 2007;48:5282–9. doi: 10.1167/iovs.07-0282. [DOI] [PubMed] [Google Scholar]
- 101.Rosenfeld PJ, Berger B, Reichel E, Danis RP, Gress A, Ye L, et al. A randomized phase 2 study of an anti-amyloid β monoclonal antibody in geographic atrophy secondary to age-related macular degeneration. Ophthalmol Retin. 2018;2:1028–40. doi: 10.1016/j.oret.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 102.Rosenfeld PJ, Dugel PU, Holz FG, Heier JS, Pearlman JA, Novack RL, et al. Emixustat hydrochloride for geographic atrophy secondary to age-related macular degeneration: a randomized clinical trial. Ophthalmology. 2018;125:1556–67. doi: 10.1016/j.ophtha.2018.03.059. [DOI] [PubMed] [Google Scholar]
- 103.Holz FG, Sadda SR, Busbee B, Chew EY, Mitchell P, Tufail A, et al. Efficacy and safety of lampalizumab for geographic atrophy due to age-related macular degeneration: Chroma and Spectri phase 3 randomized clinical trials. JAMA Ophthalmol. 2018;136:666–77. doi: 10.1001/jamaophthalmol.2018.1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Liao DS, Grossi FV, El Mehdi D, Gerber M, Brown DM, Heier JS, et al. Complement C3 inhibitor pegcetacoplan for geographic atrophy secondary to age-related macular degeneration: a randomized phase 2 trial. Ophthalmology. 2020;127:186–95. doi: 10.1016/j.ophtha.2019.07.011. [DOI] [PubMed] [Google Scholar]
- 105.Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001;119:1417–36. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Aronow ME, Chew EY. AREDS2: perspectives, recommendations, and unanswered questions. Curr Opin Ophthalmol. 2014;25:186–90. doi: 10.1097/ICU.0000000000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Rojas JC, Gonzalaz-Lima F. Low level light therapy of the eye and brain. Eye Brain. 2011;3:49–67. doi: 10.2147/EB.S21391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Merry GF, Munk MR, Dotson RS, Walker MG, Devenyi RG. Photobiomodulation reduces drusen volume and improves visual acuity and contrast sensitivity in dry age-related macular degeneration. Acta Ophthalmol. 2017;95:e270–7. doi: 10.1111/aos.13354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Hicks D, Forster V, Dreyfus H, Sahel J. Survival and regeneration of adult human photoreceptors in vitro. Brain Res. 1994;643:302–5. doi: 10.1016/0006-8993(94)90037-X. [DOI] [PubMed] [Google Scholar]
- 110.Kaemmerer E, Schutt F, Krohne TU, Holz FG, Kopitz J. Effects of lipid peroxidation-related protein modifications on rpe lysosomal functions and pos phagocytosis. Invest Ophthalmol Vis Sci. 2007;48:1342–47. doi: 10.1167/iovs.06-0549. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.