Abstract
Objective
This study investigates the role of age for the prospective association between physical work demands and long-term sickness absence (LTSA).
Methods
We followed 69 117 employees of the general working population (Work Environment and Health in Denmark study 2012–2018), without LTSA during the past 52 weeks preceding initial interview, for up to 2 years in the Danish Register for Evaluation of Marginalisation. Self-reported physical work demands were based on a combined ergonomic index including seven different types of exposure during the working day. Using weighted Cox regression analyses controlling for years of age, gender, survey year, education, lifestyle, depressive symptoms and psychosocial work factors, we determined the interaction of age with physical work demands for the risk of LTSA.
Results
During follow-up, 8.4% of the participants developed LTSA. Age and physical work demands interacted (p<0.01). In the fully adjusted model, very high physical work demands were associated with LTSA with HRs of 1.18 (95% CI 0.93 to 1.50), 1.57 (95% CI 1.41 to 1.75) and 2.09 (95% CI 1.81 to 2.41) for 20, 40 and 60 years old (point estimates), respectively. Results remained robust in subgroup analyses including only skilled and unskilled workers and stratified for gender.
Conclusion
The health consequences of high physical work demands increase with age. Workplaces should consider adapting physical work demands to the capacity of workers in different age groups.
Keywords: aging, sick leave, physical exertion, occupational health, workload
Key messages.
What is already known about this subject?
High physical work demands is a known risk factor for developing poor health and sickness absence.
Ageing is associated with a higher prevalence of sickness absence.
At present, little is known about the role of age for the prospective association between physical work demands and long-term sickness absence.
What are the new findings?
Our study shows that age interacts with physical work demands, that is, the health consequences of high physical work demands increase with age.
How might this impact on policy or clinical practice in the foreseeable future?
While most European countries gradually increase state pension age, policies to adapt physical work demands to the age of the worker are scarce.
Our study underscores the necessity of adapting physical work demands to the capacity of older workers.
Introduction
The age-distribution in Europe is gradually changing towards a growing proportion of elderly people above state pension age.1 This pushes the age dependency ratio towards levels that challenge existing welfare systems. European countries like Italy, Finland, Portugal, Greece, Germany, France, Sweden and Denmark, among others, have high age dependency ratios of about 1:3, meaning that for every three working-age persons there is one person above 65 years.2 This has set the scene for political reforms to increase retirement age with the basic assumption ‘we live longer, therefore we have to work longer’. In Denmark, such reforms have led to a gradually higher state pension age, diminished economic incentives for early voluntary retirement, and stringent criteria for obtaining disability pension benefits. While this makes sense from a political and economic perspective, not all workers may be able to work until a high age. Furthermore, the number of healthy life years even decreased in some European countries between 2010 and 2018.3 Thus, workplaces may need to adapt the work demands to the capabilities of workers of different ages.
High physical work demands is a well-documented risk factor for poor health and sickness absence.4–8 In Denmark and Norway, prospective cohort studies with register follow-up show that about a quarter of long-term sickness absence (LTSA) can be attributed to high physical work demands.4 7 However, age may also play an important role. From adulthood to retirement and beyond, there is gradual loss of muscle strength, muscle mass, pulmonary function, and physical function with increasing age, starting already around the age of 30–40 years and becoming more pronounced beyond the age of 50–60 years.9 10 As physical work ability depends both on physical work demands and physical capacity of the worker, the inherent age-related change of individual physical capacity can make physical work more demanding for older workers.11–13 On top of this, chronic diseases tend to emerge with age, which can accelerate the age-related loss of physical capacity.14 An imbalance between physical work demands and physical capacity of the worker can—from a theoretical point of view—push workers into sickness absence and ultimately premature exit from the labour market. Indeed, some prospective studies have reported that elderly workers are at higher risk than younger workers of poor self-rated health15 and disability pension16 from high physical work demands. However, previous studies have relied on self-reports for both predictors and outcomes, used specific job groups such as nurses, and/or small to moderate sample sizes. Thus, studies of the general working population with adequate sample sizes large enough to test for possible interactions with age are needed to thoroughly investigate whether increased age together with high physical work demands carries a stronger risk for developing poor health. LTSA based on national registers is strongly associated with measures of morbidity and mortality.17–19
The aim of this study is to investigate the impact of age on the prospective association between physical work demands and LTSA. We hypothesise that age interacts with physical work demands in the risk of developing LTSA and that the combination of higher age and higher physical work demands is associated with a higher risk of LTSA.
Methods
Study design and population
This prospective cohort with register follow-up used all four questionnaire rounds (2012, 2014, 2016, 2018) of the Work Environment and Health in Denmark study (WEHD)20 21 linked to the Danish Register for Evaluation of Marginalisation (DREAM). In summary, probability samples of employees aged 18–64 years, employed for a minimum of 35 hours per month, with an income of at least 3000 DKK (approximately €400) per month in the past 3 months were drawn from Danish registers and invited to participate in the study. Through the four rounds, a total of 228 173 invitations were sent of which 127 882 (56%) responses were received. As labour market status could change from the time of drawing the probability sample to the time of replying to the questionnaire, we included only people who confirmed on the questionnaire that they were currently employed wage earners (n=110 357). For wage earners participating in more than one round of WEHD, we included only first occasion responses (n=73 298). Finally, we included only wage earners free from LTSA during 52 weeks preceding initial interview and those replying to all seven ergonomic exposure variables (n=69 117). Reporting is in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology guidelines on cohort studies.22
Physical work demands (exposure)
For physical work demands4 23 the questions were, ‘How much of your working time do you …’ (1) walk or stand? (2) work with twisted or bent back without support from the hands and arms? (3) have the arms lifted to or above shoulder height, (4) do the same arm movements several times a minute? (eg, package work, mounting, machine feeding, carving), (5) squat or kneel when you work? (6) push or pull? and (7) lift or carry? Response options for each of the seven questions were ‘almost all the time’, ‘approx. 3/4 of the time’, ‘approx. 1/2 of the time’, ‘approx. 1/4 of the time’, ‘seldom/very little’ and ‘never’. To obtain a normalised score, these response categories were recoded to 100, 75, 50, 25, 12½ and 0, respectively. Subsequently, these seven values were averaged to give a normalised combined ergonomic index of 0–100. Finally, these were categorised as low (0–10), moderate (>10–20), high (>20–30) and very high physical work demands (>30). The lower cut-point of 10 was chosen during the process of inspecting the distribution of the mean ergonomic index in the different job groups (table 4). The majority of job groups with seated work were to be found in this category. Consequently, subsequent exposure groups were also defined in intervals of 10. The upper category was set to >30 to ensure a sufficient number of workers (statistical power) in all categories.
Table 4.
Weighted means with 95% CIs of physical work demands (ergonomic index) in different job groups
| Job group | N | Mean (95% CI) |
| Painters | 265 | 47.1 (44.0 to 50.1) |
| Bricklayers and plumbers | 716 | 43.8 (41.9 to 45.7) |
| Carpenters and woodworkers | 585 | 40.8 (39.0 to 42.5) |
| Cleaners | 1482 | 40.4 (38.9 to 41.9) |
| Food and related products industrial labourers | 687 | 39.6 (37.5 to 41.6) |
| Butchers and bakers | 194 | 39.3 (36.7 to 41.9) |
| Manufacturing labourers | 561 | 38.3 (36.1 to 40.5) |
| Hairdressers and beauticians | 83 | 37.8 (34.5 to 41.1) |
| Cashiers | 406 | 36.4 (34.1 to 38.6) |
| Food preparation assistants | 501 | 35.8 (33.9 to 37.7) |
| Mailmen | 366 | 35.0 (32.9 to 37.1) |
| Cooks and waiters | 407 | 34.9 (33.1 to 36.6) |
| Storage and transport labourers | 728 | 34.9 (33.1 to 36.6) |
| Farmers and gardeners | 399 | 34.2 (31.3 to 37.2) |
| Assemblers | 438 | 33.6 (31.2 to 35.9) |
| Construction workers | 859 | 33.0 (31.6 to 34.5) |
| Machine operators | 1724 | 32.9 (31.8 to 34.1) |
| Mechanics | 616 | 32.4 (30.8 to 34.0) |
| Smiths | 1266 | 31.7 (30.6 to 32.8) |
| Mobile plant operators and drivers | 250 | 31.0 (27.8 to 34.1) |
| Manual construction workers | 471 | 30.6 (28.9 to 32.4) |
| Travel attendants and conductors | 157 | 30.2 (27.1 to 33.4) |
| Health and personal care workers | 3435 | 30.0 (29.2 to 30.8) |
| Electricians | 797 | 29.1 (27.8 to 30.4) |
| Child care workers | 646 | 28.3 (26.9 to 29.8) |
| Teachers’ aides and pedagogical assistants | 905 | 27.3 (26.1 to 28.6) |
| Shop salespersons | 1664 | 25.8 (24.8 to 26.9) |
| Handicraft and precisions workers | 186 | 25.7 (22.2 to 29.3) |
| Building and cleaning supervisors | 608 | 25.6 (24.5 to 26.8) |
| Manual workers in healthcare | 498 | 25.5 (23.8 to 27.2) |
| Manual work without specification | 177 | 25.3 (21.4 to 29.2) |
| Truck drivers | 736 | 25.0 (23.4 to 26.5) |
| Service workers | 77 | 23.8 (19.1 to 28.5) |
| Primary school teachers and educated child care takers | 2176 | 22.6 (22.1 to 23.2) |
| Pharmaconomists and bioanalysts | 471 | 21.3 (20.1 to 22.5) |
| Fire-fighters and protective service professionals | 306 | 21.2 (19.5 to 22.9) |
| Clinic and dental assistants | 362 | 21.1 (19.2 to 22.9) |
| Freight forwarders | 1045 | 20.2 (18.8 to 21.7) |
| Nurses | 2564 | 19.6 (19.1 to 20.2) |
| Military personnel | 431 | 19.4 (17.8 to 20.9) |
| Bus, taxi and train drivers | 603 | 18.6 (16.9 to 20.3) |
| Special educators | 1173 | 18.5 (17.6 to 19.3) |
| Laboratory technician | 453 | 18.4 (17.3 to 19.4) |
| Healthcare workers without specification | 313 | 17.1 (15.6 to 18.6) |
| Teachers | 2827 | 15.6 (15.3 to 16.0) |
| Physiotherapists and occupational therapists | 671 | 15.1 (14.3 to 15.9) |
| Librarians, archivists and curators | 436 | 14.9 (13.5 to 16.4) |
| Vocational education teachers | 558 | 14.5 (13.7 to 15.3) |
| Special needs teachers | 456 | 14.2 (13.4 to 15.0) |
| Science and engineering associates | 1529 | 13.0 (12.3 to 13.8) |
| Policemen and prison guards | 415 | 12.6 (11.7 to 13.5) |
| Customer services clerks | 640 | 12.5 (11.2 to 13.7) |
| Pharmacists, dentists and veterinarians | 316 | 12.4 (11.1 to 13.7) |
| Secondary education teachers | 742 | 12.2 (11.7 to 12.8) |
| Doctors | 571 | 11.0 (10.3 to 11.7) |
| IT-technicians | 477 | 11.0 (9.9 to 12.0) |
| Office staff and secretaries | 3736 | 10.4 (9.9 to 10.8) |
| Managers | 3373 | 9.9 (9.5 to 10.4) |
| Technical draughtsmen | 278 | 9.0 (8.0 to 10.0) |
| Sales and purchasing agents | 1472 | 8.9 (8.3 to 9.4) |
| Professors and researchers at universities | 1075 | 8.5 (8.0 to 9.1) |
| Executive, medical, and legal secretaries | 1543 | 8.3 (7.9 to 8.6) |
| Journalists | 360 | 8.0 (6.9 to 9.1) |
| Accountants | 717 | 7.5 (6.7 to 8.2) |
| Social workers | 724 | 7.4 (6.9 to 8.0) |
| Accounting staff | 1294 | 7.4 (6.9 to 7.9) |
| Engineers and architects | 2131 | 7.3 (7.0 to 7.7) |
| Psychologists | 256 | 7.1 (6.1 to 8.2) |
| Scientific academics | 369 | 7.1 (6.4 to 7.8) |
| Social science academics | 482 | 7.1 (6.4 to 7.7) |
| Customs inspectors and tax officials | 427 | 6.9 (6.3 to 7.5) |
| Auditors, advisors and analysts | 2442 | 6.2 (6.0 to 6.4) |
| IT consultants | 1644 | 6.1 (5.8 to 6.4) |
| Lawyers | 887 | 5.4 (5.0 to 5.7) |
Long-term sickness absence (outcome)
Using the unique personal identification number (CPR) provided to all Danish citizens at birth and foreigners immigrating to Denmark, we linked the WEHD study to the DREAM register.18 19 This register contains weekly information about employment and sickness benefit transfers and is based on the municipalities’ actual payments. The validity is therefore considered to be high. We defined LTSA as having registered sickness absence in DREAM for a period of at least six consecutive weeks for a period of up to 2 years starting the week after the questionnaire reply. For the last round (2018) of the questionnaire replies, the follow-up period is limited to about 1½ years (ie, most recent update of the DREAM register).
Control variables
Age (continuous variable) and gender for each individual were drawn from the Central Person Register of Denmark. Year of questionnaire reply was entered as a continuous variable. Highest completed education was drawn from a national register and included 10 categories ranging from primary school to longer higher education. The psychosocial work factors were based on the Copenhagen Psychosocial Questionnaire Q) and included measures of influence at work (two items) and work-life balance (six items) that each were converted to a scale of 0–100,24 and included as continuous variables. Lifestyle included smoking status (categorical variable: daily, once in a while, ex-smoker, never), body mass index (BMI, kg/m2, continuous variable calculated from weight and height of the participants), leisure-time physical activity (continuous variable, total weekly hours of leisure physical activity). Depressive symptoms (Major Depression Inventory, scale 0–50) were included as a continuous variable.25 These control variables were chosen because they may be associated with both predictors and outcome. However, some of the variables may be potential mediators that could lead to over-adjustment. Thus, we chose to present both a minimally and fully adjusted model, as well as sensitivity/subgroup analyses.
Statistical analyses
The Cox proportional hazard model26 (Proc SurveyPhreg of SAS V.9.4.) was used to model the HR of LTSA during follow-up. Physical work demands was the exposure variable. The outcome variable was LTSA during follow-up. We used a time-to-first-event analysis and did not account for recurrent events, that is, this was not a frailty model. We censored in case of one of the following criteria: reaching the end of the follow-up period, early retirement, disability pension, statutory retirement, emigration or death. Using model-assisted weights based on information from national registers, each respondent was assigned a weight variable to make the estimates representative of workers in Denmark. We did not impute missing data as the weight variable repairs both non-response and possible deviations of the probability sample from the population. The analyses were performed as minimally and fully adjusted models. Model 1 (minimally adjusted) was adjusted for age, gender, education and year of questionnaire reply. Model 2 (fully adjusted) additionally included psychosocial work factors, lifestyle and depressive symptoms. We also performed subgroup analyses of the fully adjusted model including only skilled and unskilled workers and stratifying for gender. In all analyses, we included an interaction term between physical work demands and age to test whether the risk of LTSA from higher physical work demands depended on the age of the worker. In case of a significant interaction, the HR statement of the SurveyPhreg procedure was used to provide point estimates at the ages 20, 40 and 60 years, respectively. The reason for using point estimates, rather than an age range, is that age was included as a continuous variable in the analyses. Results are reported as HR’s with 95% CIs.
Results
Table 1 shows the descriptive baseline characteristics of the 69 117 included participants in terms of age, gender, education, lifestyle, work characteristics and depressive symptoms. The number of responses to each questionnaire item varied and BMI had most missing data (67 931 responses). In the study population free from LTSA during the last 52 weeks preceding initial interview, the weighted incidence of LTSA during follow-up was 8.4%. The average follow-up time, that is, until an event of LTSA or until censoring, was 93 weeks, corresponding to a total follow-up time of 123 661 years for the 69 117 participants.
Table 1.
Characteristics of the participants (N=69 117)
| N | % | Mean | SD | |
| Questionnaire round | ||||
| 2012 | 19 550 | 28.3 | ||
| 2014 | 15 079 | 21.8 | ||
| 2016 | 17 970 | 26.0 | ||
| 2018 | 16 518 | 23.9 | ||
| Age (years) | 69 117 | 46.0 | 10.8 | |
| Gender | ||||
| Men | 32 741 | 47.4 | ||
| Women | 36 376 | 52.6 | ||
| Highest education attained | ||||
| Less than vocational education | 12 100 | 17.6 | ||
| Vocational education | 25 437 | 37.0 | ||
| Higher education | 31 144 | 45.4 | ||
| BMI (kg/m2) | 67 931 | 25.7 | 4.4 | |
| Physical activity during leisure (hours per week) | 68 327 | 5.2 | 3.3 | |
| Smoking | ||||
| Yes, daily | 9878 | 14.5 | ||
| Yes, once in a while | 3541 | 5.2 | ||
| Ex-smoker | 19 780 | 29.0 | ||
| No, never | 35 121 | 51.4 | ||
| Physical work demands (ergonomic index 0–100) | ||||
| Mean | 69 117 | 19.0 | 16.5 | |
| Low (≤10) | 24 726 | 35.8 | ||
| Moderate (>10–20) | 19 549 | 28.3 | ||
| High (>20–30) | 10 794 | 15.6 | ||
| Very high (>30) | 14 048 | 20.3 | ||
| Psychosocial work factors (0–100) | ||||
| Work-life balance | 69 041 | 46.2 | 16.3 | |
| Influence at work | 68 995 | 78.8 | 19.0 | |
| MDI (0–50) | 68 432 | 8.0 | 7.3 | |
Values are percentage of participants or mean and SD.
BMI, body mass index; MDI, Major Depression Inventory.
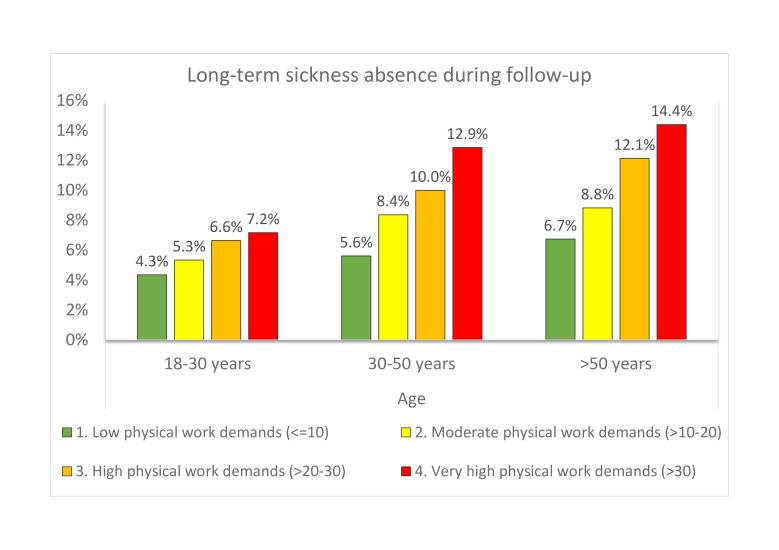
Figure 1 shows weighted incidences of LTSA during follow-up in the different subgroups of age and physical work demands. LTSA ranged from 4.3% (young workers, low physical work demands) to 14.4% (older workers, very high physical work demands).
Figure 1.
Weighted unadjusted incidence of long-term sickness absence during follow-up in different groups of age and physical work demands.
In the adjusted analyses, age and physical work demands interacted (fully adjusted model, F value=4.47, p<0.01) in the risk for LTSA during follow-up. Table 2 shows point estimates at the ages 20, 40 and 60 years for the risk of LTSA from moderate to very high physical work demands (reference: low physical work demands). In the minimally adjusted model (model 1), all levels of physical work demands at all ages were statistically significant. In the fully adjusted model (model 2), the associations were statistically significant only for 40 years old and 60 years old. The HR’s for 20 years old, 40 years old and 60 years old, respectively, were 1.18 (95% CI 0.93 to 1.50), 1.57 (95% CI 1.41 to 1.75) and 2.09 (95% CI 1.81 to 2.41) for very high physical work demands (reference: low physical work demands).
Table 2.
Weighted HRs and 95% CIs for the risk of long-term sickness absence during follow-up from moderate, high and very high physical work demands (reference: low) in workers age 20, 40 and 60 years
| Age | Physical work demands | Model 1 | Model 2 |
| HR (95% CI) | HR (95% CI) | ||
| 20 years | Low | 1 | 1 |
| Moderate | 1.29 (1.01 to 1.66) | 1.09 (0.84 to 1.41) | |
| High | 1.35 (1.03 to 1.76) | 1.09 (0.82 to 1.44) | |
| Very high | 1.73 (1.38 to 2.16) | 1.18 (0.93 to 1.50) | |
| 40 years | Low | 1 | 1 |
| Moderate | 1.39 (1.25 to 1.54) | 1.23 (1.11 to 1.37) | |
| High | 1.67 (1.49 to 1.88) | 1.41 (1.25 to 1.60) | |
| Very high | 2.14 (1.93 to 2.36) | 1.57 (1.41 to 1.75) | |
| 60 years | Low | 1 | 1 |
| Moderate | 1.49 (1.30 to 1.70) | 1.40 (1.21 to 1.61) | |
| High | 2.08 (1.79 to 2.40) | 1.84 (1.57 to 2.14) | |
| Very high | 2.64 (2.31 to 3.02) | 2.09 (1.81 to 2.41) |
Model 1: adjusted for age, gender, education and year of questionnaire reply.
Model 2: model 1+lifestyle (BMI, smoking, leisure physical activity), psychosocial work factors (work-life balance and influence at work) and depressive symptoms (MDI).
BMI, body mass index; MDI, Major Depression Inventory.
Table 3 shows that results of the fully adjusted model remained robust in subgroup analyses including only skilled and unskilled workers and stratifying for gender. For very high physical work demands (reference: low physical work demands), the HR’s were 1.00 (95% CI 0.55 to 1.82), 1.55 (95% CI 1.21 to 2.00) and 2.41 (95% CI 1.79 to 3.26) for 20 years, 40 years and 60 years men, and 1.14 (95% CI 0.77 to 1.69), 1.53 (95% CI 1.29 to 1.82) and 2.07 (95% CI 1.65 to 2.59) for 20years, 40 years and 60 years women, respectively.
Table 3.
Gender-stratified weighted HRs and 95% CIs for the risk of long-term sickness absence during follow-up from moderate, high and very high physical work demands (reference: low) in workers age 20, 40 and 60 years, including only unskilled and skilled workers
| Age | Physical work demands | Men | Women |
| HR (95% CI) | HR (95% CI) | ||
| 20 years | Low | 1 | 1 |
| Moderate | 0.86 (0.42 to 1.80) | 1.37 (0.86 to 2.20) | |
| High | 0.62 (0.31 to 1.24) | 1.19 (0.74 to 1.93) | |
| Very high | 1.00 (0.55 to 1.82) | 1.14 (0.77 to 1.69) | |
| 40 years | Low | 1 | 1 |
| Moderate | 1.06 (0.79 to 1.44) | 1.35 (1.11 to 1.65) | |
| High | 1.12 (0.84 to 1.51) | 1.43 (1.16 to 1.74) | |
| Very high | 1.55 (1.21 to 2.00) | 1.53 (1.29 to 1.82) | |
| 60 years | Low | 1 | 1 |
| Moderate | 1.31 (0.94 to 1.82) | 1.33 (1.03 to 1.71) | |
| High | 2.04 (1.48 to 2.82) | 1.70 (1.32 to 2.20) | |
| Very high | 2.41 (1.79 to 3.26) | 2.07 (1.65 to 2.59) |
Adjusted for age, gender, education, year of questionnaire reply, lifestyle (BMI, smoking, leisure physical activity), psychosocial work factors (work-life balance and influence at work) and depressive symptoms (MDI).
BMI, body mass index; MDI, Major Depression Inventory.
Table 4 shows the weighted mean physical work demands of different job groups. While job groups per se were not included as a factor in the statistical analyses, these values are presented to put the results into context. Job groups with very high physical work demands are, for example, painters, bricklayers, carpenters and cleaners. Job groups with high physical work demands are, for example, electricians, child care workers, teachers’ aides and pedagogical assistants, and shop salespersons.
Discussion
The main finding of this study is that the negative health consequences of high physical work demands depends on age of the worker. Thus, the risk for LTSA from higher physical work demands increased with increasing age of the worker. This finding remained robust in subgroup analyses including only unskilled and skilled workers and stratifying for gender.
Previous studies have found that sickness absence generally increases with age27 28 and with higher physical work demands.4 Yet, few studies have investigated the interaction between age and physical work demands. Burr and colleagues found in a smaller sample of the general working population that age and physical work demands interacted in the risk of self-rated poor health.15 However, in that study both exposure and outcome were self-rated, rendering the study vulnerable to common method bias. By contrast, only the exposure variable was self-rated in the present study, whereas the outcome was based on register data. A prospective study in a specific job group, healthcare workers in eldercare, found that age and physical exertion during work interacted in the risk of disability pension.16 However, results from that study cannot be extrapolated to the general working population. In contrast to previous studies, our study used a large sample size of the general working population and register-based outcome of LTSA. From the weighted incidences shown in figure 1, the interaction is obvious, that is, higher physical work demands was associated with higher risk of LTSA especially for the older workers. This was also clear from the Cox-regression analyses controlling for various potential confounders. In the fully adjusted analysis, the older workers (60 years) had about doubled risk of LTSA from high (HR 1.84) and very high (HR 2.09) physical work demands, while this risk was not significant for the younger workers (20 years).
There may be several explanations for the present results. First, inherent biological changes occur in the body with increasing age. Muscle strength and different measures of physical function decline gradually from the age of 30–40 years until retirement and beyond,9 10 which makes the same physical work demands relatively more demanding for the ageing worker. Second, different health-related problems tend to emerge more commonly with increasing age, and the combination of high physical work demands and poor health seems to be especially problematic.29 Third, the consequences of years of hard physical work seem to accumulate in terms of increased risk of sickness absence and disability pension.30 Together these factors may create an imbalance between physical demands of the work and physical capacity of the worker, which increases the risk of LTSA. Possible gender differences may also be expected to exist in the risk of LTSA from high physical work demands, for example, men have on average more muscle mass than women and may therefore be able to better handle high physical work demands. However, based on the overlapping CIs of the estimates for men and women (table 3) such differences were not evident.
The present study has important practical implications. First, workplaces should consider age of the worker when planning work tasks that are physically demanding. Better use of assistive devices, better planning and organisation of the work, and offering physical exercise to stay fit even at a high age may be a way forward. Some of these elements may be included in senior policies. Second, lifelong learning and further education may be necessary at the individual level to be able to change to a less physically demanding job later in life. As illustrated by table 4, job groups that require little further education can be found at the lower end of the scale, for example, bus and taxi drivers and customer services clerks. Third, a differentiated pension system taking physical work demands throughout life into account may be necessary. While the present study does not provide practical solutions, it highlights the challenges of having high physical work demands with increasing age.
Limitations
There are both strengths and limitations of the present study. The main limitation is that the exposure variable was self-reported. Thus, an inherent risk of self-report bias exists. Also, standing and walking was included in the same questionnaire item, which is not optimal from a methodological point of view as walking is generally considered healthy. The response categories only considered temporal aspects and we can therefore not conclude anything about load, for example, heavy lifting. Furthermore, we could have weighted the different ergonomic factors in the index, for example, lifting may be worse than standing/walking in terms of LTSA risk.4 However, such a weighting would require more knowledge than exists at present about the precise risk (very narrow CIs) of each ergonomic factor. In future studies, alternative methods could include job-exposure-matrices and technical measurements of physical work demands. Another option could be to use a calibration model based on objective measurements to correct self-reported exposure data.31 Nevertheless, judged by the ratings of the different job groups (table 4), the present index of physical work demands seems meaningful. Another possible bias is the healthy worker effect, that is, those who have developed the poorest health from high physical work demands may already have been pushed out of the labour market.32 Thus, the present estimates may be too conservative. There is an inherent risk of residual bias or misclassification bias in the present type of analyses including the general working population. Analyses focusing on specific occupations could therefore help strengthen the overall evidence. Similarly, our study can strengthen results from studies of specific occupations, since such results cannot be generalised to the general working population. One possible source of residual bias in analyses of the general working population may lie in lifestyle in relation to education, that is, all facets of lifestyle may not be captured equally by questionnaire replies in different educational groups. Therefore, we adjusted the analyses for level of education. Poor health is a possible source of misclassification bias, that is, those with poor health may overrate physical work demands. For this reason, we did not ask about perceived physical exertion during work, but rather about temporal aspects of ergonomic factors. Regarding the outcome variable, LTSA can have multiple causes, including underlying diseases that may be both work-related and non-work related. As we conducted an observational study, and not a randomised controlled trial, interpretation of the data needs to be done while considering strengths and limitations of the research design. A limitation of our study is that we did not have information about the specific diagnosis for the LTSA, as such information does not exist in Danish registers. LTSA in our study is thus an unspecific proxy for poor health, however, a proxy that is strongly related to serious health endpoints, such as disability and mortality.17 To reduce the possibility that existing poor health had caused both the reporting of physical demands at baseline and LTSA during follow-up, we excluded all workers with previous LTSA. Further, we controlled the analyses for a number of possible confounders, including lifestyle, psychosocial work factors and depressive symptoms. Additionally, during the revision of the present article, we performed two sensitivity analyses (not shown), (1) excluding individuals with ‘poor’ and ‘less good’ self-rated health at baseline (8.34% of the population) and (2) excluding individuals working less than 20 hours per week (1.07% of the population). These sensitivy analyses had only minimal influence on the HR estimates (second decimal changes), which increases the validity of the main findings from the pre-planned analyses.
Conclusion
In conclusion, the health consequences of high physical work demands—expressed as the risk of LTSA—increase with age. Workplaces should consider adapting physical work demands to the capacity of older workers.
Footnotes
Twitter: @larslandersen
Contributors: LLA had the idea for the project and is responsible for the study design and analyses. All coauthors provided feedback on the design and analyses. LLA drafted the manuscript and all authors have provided important intellectual feedback on the content. All authors critically reviewed and approved the final version of the manuscript.
Funding: LLA obtained a grant from the The Danish Working Environment Research Fund for this project (Arbejdsmiljøforskningsfonden, grant number 20195100758).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
The authors encourage collaboration and use of the data by other researchers. Data are stored on the secure server of Statistics Denmark, and researchers interested in using the data for scientific purposes should contact the authors.
Ethics statements
Patient consent for publication
Not required.
References
- 1. European Agency for Safety and Health at Work (EU-OSHA) . OSH management in the context of an ageing workforce - Safety and health at work, 2020. Available: https://osha.europa.eu/en/themes/osh-management-context-ageing-workforce [Accessed 7 Nov 2020].
- 2. The World Bank . Age dependency ratio, old (% of working-age population) | data, 2019. Available: https://data.worldbank.org/indicator/SP.POP.DPND.OL [Accessed 7 Nov 2020].
- 3. Eurostat . Healthy life years statistics - Statistics Explained, 2020. Available: https://ec.europa.eu/eurostat/statistics-explained/index.php/Healthy_life_years_statistics [Accessed 4 Feb 2021].
- 4. Andersen LL, Fallentin N, Thorsen SV, et al. Physical workload and risk of long-term sickness absence in the general working population and among blue-collar workers: prospective cohort study with register follow-up. Occup Environ Med 2016;73:246–53. 10.1136/oemed-2015-103314 [DOI] [PubMed] [Google Scholar]
- 5. Mayer J, Kraus T, Ochsmann E. Longitudinal evidence for the association between work-related physical exposures and neck and/or shoulder complaints: a systematic review. Int Arch Occup Environ Health 2012;85:587–603. 10.1007/s00420-011-0701-0 [DOI] [PubMed] [Google Scholar]
- 6. da Costa BR, Vieira ER. Risk factors for work-related musculoskeletal disorders: a systematic review of recent longitudinal studies. Am J Ind Med 2010;53:285–323. 10.1002/ajim.20750 [DOI] [PubMed] [Google Scholar]
- 7. Sterud T. Work-Related mechanical risk factors for long-term sick leave: a prospective study of the general working population in Norway. Eur J Public Health 2014;24:111–6. 10.1093/eurpub/ckt072 [DOI] [PubMed] [Google Scholar]
- 8. Foss L, Gravseth HM, Kristensen P, et al. The impact of workplace risk factors on long-term musculoskeletal sickness absence: a registry-based 5-year follow-up from the Oslo health study. J Occup Environ Med 2011;53:1478–82. 10.1097/JOM.0b013e3182398dec [DOI] [PubMed] [Google Scholar]
- 9. Newton RU, Hakkinen K, Hakkinen A, et al. Mixed-Methods resistance training increases power and strength of young and older men. Med Sci Sports Exerc 2002;34:1367–75. 10.1097/00005768-200208000-00020 [DOI] [PubMed] [Google Scholar]
- 10. Suetta C, Haddock B, Alcazar J, et al. The Copenhagen sarcopenia study: lean mass, strength, power, and physical function in a Danish cohort aged 20-93 years. J Cachexia Sarcopenia Muscle 2019;10:1316–29. 10.1002/jcsm.12477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ilmarinen J, Tuomi K, Klockars M. Changes in the work ability of active employees over an 11-year period. Scand J Work Environ Health 1997;23 Suppl 1:49–57. [PubMed] [Google Scholar]
- 12. Tuomi K, Ilmarinen J, Martikainen R, et al. Aging, work, life-style and work ability among Finnish municipal workers in 1981-1992. Scand J Work Environ Health 1997;23 Suppl 1:58–65. [PubMed] [Google Scholar]
- 13. van den Berg TIJ, Elders LAM, de Zwart BCH, et al. The effects of work-related and individual factors on the work ability index: a systematic review. Occup Environ Med 2009;66:211–20. 10.1136/oem.2008.039883 [DOI] [PubMed] [Google Scholar]
- 14. Prasad S, Sung B, Aggarwal BB. Age-Associated chronic diseases require age-old medicine: role of chronic inflammation. Prev Med 2012;54:S29–37. 10.1016/j.ypmed.2011.11.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Burr H, Pohrt A, Rugulies R, et al. Does age modify the association between physical work demands and deterioration of self-rated general health? Scand J Work Environ Health 2017;43:241–9. 10.5271/sjweh.3625 [DOI] [PubMed] [Google Scholar]
- 16. Andersen LL, Villadsen E, Clausen T. Influence of physical and psychosocial working conditions for the risk of disability pension among healthy female eldercare workers: prospective cohort. Scand J Public Health 2019;1403494819831821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kivimaki M, et al. Sickness absence as a global measure of health: evidence from mortality in the Whitehall II prospective cohort study. BMJ 2003;327:364. 10.1136/bmj.327.7411.364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hjollund NH, Larsen FB, Andersen JH. Register-Based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health 2007;35:497–502. 10.1080/14034940701271882 [DOI] [PubMed] [Google Scholar]
- 19. Lund T, Kivimäki M, Labriola M, et al. Using administrative sickness absence data as a marker of future disability pension: the prospective DREAM study of Danish private sector employees. Occup Environ Med 2008;65:28–31. 10.1136/oem.2006.031393 [DOI] [PubMed] [Google Scholar]
- 20. Andersen LL, Thorsen SV, Flyvholm M-A, et al. Long-Term sickness absence from combined factors related to physical work demands: prospective cohort study. Eur J Public Health 2018;28:824–9. 10.1093/eurpub/cky073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Johnsen NF, Thomsen BL, Hansen JV, et al. Job type and other socio-demographic factors associated with participation in a national, cross-sectional study of Danish employees. BMJ Open 2019;9:e027056. 10.1136/bmjopen-2018-027056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297. 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Orhede E. Nordic cooperation in research on the work environment. Scand J Work Environ Health 1994;20:65–6. 10.5271/sjweh.1426 [DOI] [PubMed] [Google Scholar]
- 24. Pejtersen JH, Kristensen TS, Borg V, et al. The second version of the Copenhagen psychosocial questionnaire. Scand J Public Health 2010;38:8–24. 10.1177/1403494809349858 [DOI] [PubMed] [Google Scholar]
- 25. Bech P, Rasmussen N-A, Olsen LR, et al. The sensitivity and specificity of the major depression inventory, using the present state examination as the index of diagnostic validity. J Affect Disord 2001;66:159–64. 10.1016/S0165-0327(00)00309-8 [DOI] [PubMed] [Google Scholar]
- 26. Cox DR. Regression models and Life-Tables. Journal of the Royal Statistical Society: Series B 1972;34:187–202. [Google Scholar]
- 27. Labriola M, Lund T, Burr H. Prospective study of physical and psychosocial risk factors for sickness absence. Occup Med 2006;56:469–74. 10.1093/occmed/kql058 [DOI] [PubMed] [Google Scholar]
- 28. Alavinia SM, van den Berg TIJ, van Duivenbooden C, et al. Impact of work-related factors, lifestyle, and work ability on sickness absence among Dutch construction workers. Scand J Work Environ Health 2009;35:325–33. 10.5271/sjweh.1340 [DOI] [PubMed] [Google Scholar]
- 29. van der Beek AJ, Kunst AE. How can we break the vicious circle between poor health and exit from paid employment? Scand J Work Environ Health 2019;45:321–3. 10.5271/sjweh.3838 [DOI] [PubMed] [Google Scholar]
- 30. Sundstrup E, Hansen Åse Marie, Mortensen EL, et al. Cumulative occupational mechanical exposures during working life and risk of sickness absence and disability pension: prospective cohort study. Scand J Work Environ Health 2017;43:415–25. 10.5271/sjweh.3663 [DOI] [PubMed] [Google Scholar]
- 31. Coenen P, Mathiassen S, van der Beek AJ, et al. Correction of bias in self-reported sitting time among office workers - a study based on compositional data analysis. Scand J Work Environ Health 2020;46:32–42. 10.5271/sjweh.3827 [DOI] [PubMed] [Google Scholar]
- 32. Andersen LL, Jensen PH, Sundstrup E. Barriers and opportunities for prolonging working life across different occupational groups: the SeniorWorkingLife study. Eur J Public Health 2020;30:241–6. 10.1093/eurpub/ckz146 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors encourage collaboration and use of the data by other researchers. Data are stored on the secure server of Statistics Denmark, and researchers interested in using the data for scientific purposes should contact the authors.