Abstract
Pneumocephalus is a condition defined by air present in the intracranial space. There are several causes of pneumocephalus, however this is a case of a patient who developed pneumocephalus following a cervical epidural steroid injection. Uniquely, this patient's chief complaint was sudden onset of syncope, and respiratory arrest following the injection. The diagnosis was made by CT, and conservative treatment was used for resolution of the condition. Patients with pneumocephalus can present with a wide range of neurologic symptoms, and prompt recognition and treatment are key to preventing irreversible neurologic damage.
Keywords: Pneumocephalus, Epidural, Headache, CT Brain
Introduction
By far the most common causes of pneumocephalus are trauma, which accounts for 74% of cases, and surgery [1]. Pneumocephalus in the absence of trauma is exceedingly rare. Common causes of which are infection, valsalva maneuver, and repeated forceful sneezing [2]. Other causes have been reported including pneumococcal meningitis, CSF leaks, and pneumosinus dilatans [3,4]. CT is the gold standard in diagnosing pneumocephalus and can detect as little as 0.55 mL of intracranial gas [5]. Treatment of pneumocephalus is typically conservative and includes bed rest, fowler position, and high flow oxygen administration. In fact, pneumocephalus is spontaneously absorbed in approximately 85% of patients during the first week of developing the condition [6]. If severe features are present, then surgical intervention is indicated. Complications of pneumocephalus can be meningitis, seizures, brain abscess, and brain herniation depending on the mechanism by which pneumocephalus formed in each patient. However, prognosis is typically favorable especially when prompt recognition, and treatment are performed.
Case report
Our patient is a 94-year-old woman who came to the emergency department for evaluation of sudden syncope and respiratory arrest. The patient was at a pain clinic and received a cervical epidural steroid injection. Immediately after the injection procedure the patient became unresponsive as she began sitting up; she did not fall or hit her head. Emergency medical services were called and a supraglottic airway was placed for respiratory arrest. Rescue breathing with a bag valve mask was initiated and CPR was not performed. When she arrived at the emergency department the patient was awake and following commands. The supraglottic airway was removed at that time. She reported nausea, dizziness, and lightheadedness, and had no recollection of the event at the pain center. However, she denied shortness of breath or chest pain. She has not had any recent trauma or medical procedures except the spine injection. The physical exam of this patient was unremarkable, and her vital signs were normal and stable including an SpO2 of 99%.
The patient has a history of atrial fibrillation, multiple myeloma on monthly VELCADE infusions, and diet-controlled type 2 diabetes. She currently takes apixaban, dexamethasone with monthly VELCADE infusion, metoprolol, and tramadol. The patient has never smoked or used recreational drugs besides consuming 2 beers on the weekend. Her family history is significant for multiple myeloma in her mother and 2 sisters.
A CT of her brain was ordered which revealed scattered intracranial gas, particularly suprasellar region, and left hemisphere (Figs. 1,2, and 3). There was no evidence for a depressed skull fracture or air cell disruption. The sylvian fissures and interpeduncular cistern were all dense in appearance. The patient's fourth ventricle appeared partially effaced with some developing downward herniation of the cerebellum. The total estimated intracranial air was 5 milliliters. A differential considered in the report includes a subarachnoid hemorrhage or complex and/or proteinaceous material, perhaps in the setting of infectious and/or inflammatory processes such as meningitis. Part of the density along the sylvian fissures could be from some component of sulcal effacement giving this dense appearance, and or from the courses of the middle cerebral arteries.
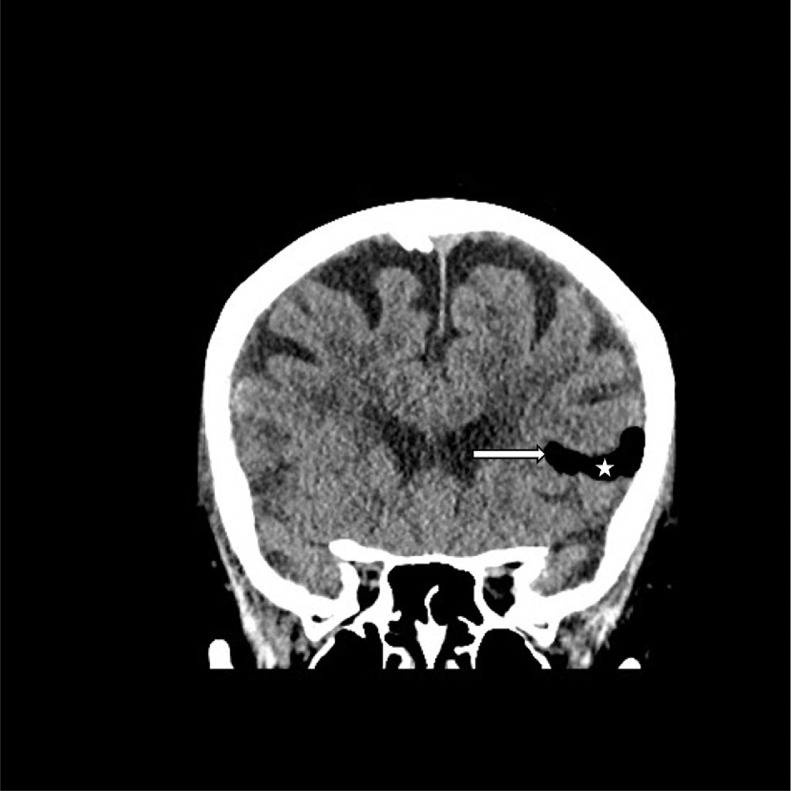
Fig. 1.
Coronal reconstruction CT showing gas (star) within the patient's left sylvian fissure (arrow).
Fig. 2.
Axial CT showing gas (star) within the suprasellar region.
Fig. 3.
Axial CT scan showing gas (star) adjacent to the left temporal lobe (arrow). The fourth ventricle (arrowheads) appears partially effaced.
An electrocardiogram demonstrated a normal sinus rhythm with a first-degree atrioventricular block which is unchanged from her previous tracings. A chest x-ray was unremarkable for acute cardiopulmonary abnormalities. Laboratory workup included a complete blood count, complete metabolic panel, coagulation and troponin studies, arterial blood gas, and COVID test. Pertinent findings were a blood glucose level of 138 and troponin level of 16 pg/mL, otherwise laboratory findings were noncontributory.
The diagnosis of iatrogenic pneumocephalus secondary to epidural steroid injection was made based on CT results and the patient's history. Neurosurgery was consulted and the decision was ultimately made to pursue conservative treatment for resolution of the pneumocephalus.
Discussion
There are many causes of respiratory arrest in elderly patients that should be considered for this patient. The most common of these are CHF (43%), pneumonia (35%), COPD exacerbation (32%), and PE (18%) [7]. In addition, a study of 902 patients showed that the causes of being ventilated in adults over the age of 70 are CHF (16%), CAP (16%), COPD (14%), and sepsis (10%) [8]. Our patient had no medical history to support these etiologies, nor medications to affect her breathing. Moreover, our patient recovered from her acute respiratory failure by the time she presented to the ED. The other etiologies listed are unlikely to present in this fashion. Granted, airway obstruction caused by a foreign body can cause respiratory arrest, and if that foreign body became dislodged, respirations may resume like this patient. Yet, no foreign body was seen on intubation insertion or removal nor the chest x-ray.
Various cases have reported that the first symptom of pneumocephalus following epidural access is a sudden and intense headache [12]. Our case was unusual given that the patient lost consciousness and went into respiratory arrest following the cervical epidural procedure. One plausible theory behind this is due to mobility of gas within the meninges which can shift rapidly as the patient changes position. This could potentially cause compression and displacement of different cerebral structures depending on where the gas settles. Presumably, the intracranial gas seen in our patient was introduced in the cervical region. Therefore, migration of gas cephalad into the intracranial space could irritate the medulla oblongata during its ascent superiorly. This mechanism could explain the patient's respiratory arrest upon sitting upright. As the gas shifted further into the cranium and away from the brainstem, the patient would theoretically regain respiratory drive which was seen as the patient arrived at the ED. Given this theory, it is not hard to argue that pneumocephalus could present with a wide range of neurologic symptoms such as respiratory arrest seen in our patient.
Pneumocephalus is often a complication of accessing the epidural space, such as for analgesia during labor, or for cervical steroid injections, as was the case for our patient [9]. This typically occurs from air being accidentally injected into the intrathecal space when the operator uses the ‘loss of resistance’ technique to identify the epidural space [10]. As the epidural needle is advanced, a small amount of constant pressure is applied to the attached syringe which is either filled with saline or air. Once the needle is advanced far enough into the epidural space, loss of resistance to the syringe plunger is felt, indicating that the needle is in the epidural space. Use of air for the loss of resistance technique has been controversial because if too much pressure is applied to the syringe as the needle enters the epidural space, excessive amounts of air or saline can be injected into the epidural space. In our patient, we suspect that the dura mater was punctured during the epidural injection with the loss of resistance technique, causing air to become trapped in the subdural space. Once the patient sat upright, the air could migrate cephalad into the cranium causing her respiratory arrest. This mechanism is not unreasonable because the incidence of accidental dural puncture during epidural injections is 1.5% [11]. Another potential mechanism for the pneumocephalus is from the respiratory support our patient received. There are reports of positive pressure ventilation resulting in pneumocephalus in literature. However, this does not explain the sudden respiratory distress our patient experienced immediately after the steroid injection procedure.
Commonly cited complications of injections are infection, bleeding at the injection site, and damage to surrounding structures. This case demonstrates the importance of considering pneumocephalus in patients who develop neurologic symptoms following epidural injections. Although there are many reported cases of epidural pain blocks causing pneumocephalus in laboring women, there are far fewer cases dedicated to steroid injections resulting in pneumocephalus. Our patient developed life threatening syncope and respiratory arrest following her epidural injection procedure. Thankfully, emergency response was able to quickly provide rescue breaths to stabilize the patient. Though the patient was diagnosed with pneumocephalus, only conservative management was needed to support the spontaneous gas absorption process.
Patient consent
Written informed consent for publication of this case was obtained from the patient and is available upon request.
Footnotes
Competing Interests: The authors have no conflicting interests.
References
- 1.Markham JW. The clinical features of pneumocephalus based upon a survey of 284 cases with report of 11 additional cases. Acta Neurochirurgica. 1967;1:1–78. doi: 10.1007/BF01401900. [DOI] [PubMed] [Google Scholar]
- 2.Pishbin E, Azarfardian N, Salarirad M, Ganjeifar B. Spontaneous nontraumatic pneumocephalus: a case report. Iran Red Crescent Med J. 2015;17:e23920. doi: 10.5812/ircmj.23920v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim HS, Kim SW, Kim SH. Spontaneous pneumocephalus caused by pneumococcal meningitis. J Korean Neurosurg Soc. 2013;53:249–251. doi: 10.3340/jkns.2013.53.4.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baba M, Tarar O, Syed A. A rare case of spontaneous pneumocephalus associated with nontraumatic cerebrospinal fluid leak. Case Rep Neurol Med. 2016;2016:1828461–1828463. doi: 10.1155/2016/1828461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Karavelioglu E, Eser O, Haktanir A. Pneumocephalus and pneumorrhachis after spinal surgery: case report and review of the literature. Neurologia medico-chirurgica. 2014;54:405–407. doi: 10.2176/nmc.cr2013-0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Penrose-Stevens A, Ibrahim A, Redfern R. Localized pneumocephalus caused by Clostridium perfringens meningitis. Br J Neurosurg. 1999;13:85–86. doi: 10.1080/02688699944285. [DOI] [PubMed] [Google Scholar]
- 7.Ray P, Birolleau S, Lefort Y, Becquemin M, Beigelman C, Isnard R. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Critical Care. 2006;10:R82. doi: 10.1186/cc4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Recovery rate and prognosis in older persons who develop acute lung injury and the acute respiratory distress syndrome.(Summaries for Patients) Ann Intern Med. 2002;136:1–42. doi: 10.7326/0003-4819-136-1-200201010-00004. [DOI] [PubMed] [Google Scholar]
- 9.Reddi S, Honchar V, Robbins MS. Pneumocephalus associated with epidural and spinal anesthesia for labor. Neurol Clin Pract. 2015;5:376–382. doi: 10.1212/CPJ.0000000000000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Saberski L, Kondamuri S, Osinubi O. Identification of the epidural space: is loss of resistance to air a safe technique? A review of the complications related to the use of air. Reg Anesth. 1997;22:3–15. doi: 10.1016/s1098-7339(06)80050-7. [DOI] [PubMed] [Google Scholar]
- 11.Choi PT, Galinski SE, Takeuchi L, Lucas S, Tamayo C, Jadad AR. PDPH is a common complication of neuraxial blockade in parturients: a meta-analysis of obstetrical studies. Can J Anaesth. 2003;50:460–469. doi: 10.1007/BF03021057. [DOI] [PubMed] [Google Scholar]
- 12.Verdun AV, Cohen SP, Williams BS, Hurley RW. Pneumocephalus after lumbar epidural steroid injection: a case report and review of the literature. A & A case reports. 2014;3:9–13. doi: 10.1213/XAA.0000000000000055. [DOI] [PubMed] [Google Scholar]