Introduction
Lichen planus is a benign, chronic, mucocutaneous disorder that affects the skin, mucosae, and nails. The occurrence of nail lichen planus has been reported to be about 10% to 15%.1,2 Nail lichen planus is more common in adults than in children, and it mostly affects the fingernails rather than the toenails.3 The many nail abnormalities found in nail lichen planus depend on its pathologic location: the nail matrix or the nail bed. Dorsal pterygium is an irreversible and classic finding in nail lichen planus. The disease may lead to permanent disfigurement, which has both functional and psychological consequences. Early diagnosis and prompt treatment are also important to prevent the development of pterygium.
Nail lichen planus can sometimes be difficult to diagnose and differentiate from other nail disorders. This is especially the case in patients without other mucocutaneous findings. Systemic corticosteroids are the first-line treatment, but they have inconsistent outcomes. There are few published reports on the clinical characteristics and treatment outcomes of nail lichen planus in Asians. The aims of our study were to review the clinical characteristics of, treatment approaches to, and treatment outcomes of nail lichen planus.
Case series
This retrospective study was conducted between January 2015 and December 2019. Patients attending the Outpatient Clinic, Department of Dermatology, Faculty of Medicine, Siriraj Hospital, Bangkok, Thailand were included. Their medical charts and photographs were thoroughly reviewed.
During the study period, nail lichen planus had been diagnosed in the patients by 2 dermatologists. Differences in their diagnoses were resolved by consensus. To be included in the study, patients needed to be 18 years of age or older at the time of their initial presentation, and full medical records and photographs had to be available. We excluded patients with a diagnosis of other nail diseases, such as onychomycosis, traumatic nail abnormalities, and nail tumors. Also excluded were patients who had been given systemic drugs that might have influenced nail characteristics (such as methotrexate, acitretin, and biologic drugs) before their diagnosis of nail lichen planus. The research protocol was approved by the Siriraj Institutional Review Board (Si 573/2019).
Details were collected on the patients' baseline characteristics, duration of nail disease before diagnosis, family history of lichen planus, histopathologic results, and other mucocutaneous involvement. Also recorded were the clinical findings of the disease and its severity, treatment, and treatment outcomes. The degree of severity was categorized as mild, moderate, or severe. The features of mild nail lichen planus were nail thinning, longitudinal ridging, distal splitting <3 mm in length, onycholysis area <25%, and no subungual hyperkeratosis. The features of moderate nail lichen planus were partial fissuring, longitudinal grooves, distal splitting 3 to 5 mm in length, onycholysis area between 25% and 50%, mottled erythema of the lunula, and subungual hyperkeratosis. The features of severe nail lichen planus were complete fissuring, deep grooves, splitting >5 mm in length, onycholysis area >50%, diffuse erythema of the lunula, pterygium, and anonychia.3
The percentage of success of a treatment was categorized as follows: no improvement or worsening of nail finding; minimal improvement (≤25% reduction of nail plate abnormality); mild improvement (26% to 50% reduction); moderate improvement (51% to 75% reduction); and great improvement (76% to 99% reduction). Clinical cure was defined as 100% reduction of nail plate and nail bed abnormalities or a normal nail appearance after treatment.3
We enrolled 220 patients with lichen planus who had visited the Outpatient Clinic, Department of Dermatology, Siriraj Hospital, during the 5-year study period. Twenty-two (10%) patients had nail involvement; however, 8 of those were excluded because of incomplete data and photographs. Thus, 14 patients with nail lichen planus were enrolled.
Baseline characteristics and clinical features
The average age of the 14 patients was 53.3 ± 13.9 years, and 64.3% were women. The median duration between the onset of the nail disease and the first visit to the clinic was 42 months (range, 2 months to 30 years). The mean age at disease onset was 47.4 ± 15.4 years. Nine patients (64.3%) had isolated nail lichen planus. The remaining 5 (35.7%) had concomitant mucocutaneous involvement (2 [14.3%] had mucosal involvement only, 2 [14.3%] had cutaneous involvement only, and 1 [7.1%] had both mucosal and cutaneous involvement). In the great majority of patients (92.9%), both fingernails and toenails were affected. At baseline, 71.4% of the patients had severe nail lichen planus, and no patient had mild nail lichen planus. Two patients (14.2%) had nail symptoms, which included mild pain and difficulty handling objects.
All of the patients had nail matrix involvement. The most common nail abnormalities were melanonychia (85.7%), followed by onychorrhexis (64.3%), longitudinal ridging (53.1%), nail plate thinning (50%), trachyonychia (50%), and red lunula (50%). Dorsal pterygium was found in 42.9% of the patients at their first presentation. Nail bed involvement was observed in just over half of the patients (57.1%); it comprised onycholysis (35.7%), subungual hyperkeratosis (28.6%), and splinter hemorrhage (14.3%) (Table I, Figs 1 and 2).
Table I.
Clinical characteristics of 14 patients with nail lichen planus
| Characteristic | No. (%) of patients |
|---|---|
| Nail matrix involvement | 14 (100) |
| Melanonychia | 12 (85.7) |
| Onychorrhexis | 9 (64.3) |
| Longitudinal ridging | 8 (57.1) |
| Nail plate thinning | 7 (50) |
| Trachyonychia | 7 (50) |
| Red lunula | 7 (50) |
| Onychoschizia | 6 (42.9) |
| Dorsal pterygium | 6 (42.9) |
| Longitudinal splitting | 5 (35.7) |
| Anonychia | 4 (28.6) |
| Beau's line | 2 (14.3) |
| Onychomadesis | 2 (14.3) |
| Pitting nail | 1 (7.1) |
| Nail bed involvement | 8 (57.1) |
| Onycholysis | 5 (35.7) |
| Subungual hyperkeratosis | 4 (28.6) |
| Splinter hemorrhage | 2 (14.3) |
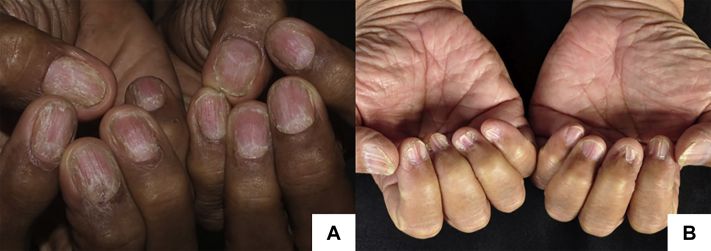
Fig 1.
The 2 most common clinical characteristics of patients with nail lichen planus. A and B, Melanonychia and onychorrhexis.
Fig 2.
Other common clinical characteristics of patients with nail lichen planus. A, Nail plate thinning and trachyonychia. B, Dorsal pterygium.
Treatment approaches and outcomes
Regarding the treatments used in this study, 78.6% of the patients received topical treatments (superpotent topical corticosteroids and topical vitamin D analogs). Two thirds of the patients (64.3%) received systemic corticosteroids, which were either oral prednisolone (average dose, 40-80 mg/wk) in a variety of regimens, or intramuscular triamcinolone acetonide (40 mg/mL monthly). During the 5-year follow-up period (median follow-up time, 38.5 months) of 12 of the 14 patients, 66.7% of the patients had shown minimal to mild improvement; the remaining 33.4% did better, showing a moderate to great improvement. Pterygium was excluded from the evaluation of improvement, because it did not respond to any treatment.
Discussion
Nail lichen planus has been reported to represent 10% to 15% of lichen planus cases.1,2 Approximately 4% of nail lichen planus cases result in permanent nail scarring.4 The present study showed that 10% of patients with lichen planus had the characteristics of nail lichen planus, which is similar to the findings of earlier investigations.1,2
At baseline, most patients were in the fifth or sixth decade of life (mean age, 53.3 years). This average was only slightly higher than that reported by Goettmann et al1 (47 years); however, their study included patients younger than 18 years. Both fingernails and toenails were affected in the vast majority (92.9%) of the cases in the present investigation, whereas toenail involvement was observed in only 53.7% of the patients in the study by Goettmann et al.1 About one third of the patients in our study had other mucocutaneous involvement. This finding is markedly different from that in the study by Goettmann et al,1 as mucocutaneous findings were not observed in any of the patients at the time of diagnosis. Importantly, diagnosis of nail lichen planus cannot be totally based on other mucocutaneous lichen planus findings, because most patients with nail lichen planus have no other mucocutaneous involvement.
There have been few published studies on the presentations of nail lichen planus in Asians. A literature review of the clinical characteristics of patients with nail lichen planus revealed that the common findings were longitudinal ridging and fissuring, nail plate thinning, and trachyonychia. Most of the patients in the present study (85.7%) had melanonychia. This finding is consistent with a study in India by Kharghoria et al,4 which reported that 88.9% of their patients had melanonychia. Multiple studies have observed that postinflammatory melanonychia is found with many inflammatory nail disorders, such as nail lichen planus, psoriatic nail, chronic paronychia, and traumatic nail.5 However, on the basis of our experience, postinflammatory melanonychia is not commonly seen with psoriatic nail in the Thai population. Traumatic nail is predominantly found with melanonychia in toenails rather than fingernails. It therefore follows that in Asian patients, the presence of melanonychia in many nails, especially fingernails, along with other common clinical characteristics of nail lichen planus, should signal the possibility of nail lichen planus. The studies of Goettmann et al1 and Żychowska et al6 described very similar levels of nail matrix and nail bed involvement. The present study found higher proportions of red lunula and trachyonychia, both of which indicate the presence of severe nail abnormalities (Table II).7,8
Table II.
Literature review of clinical characteristics, treatments, and treatment outcomes of patients with nail lichen planus
| Authors (y), country (study design) | No. of cases | Outcomes |
|
|---|---|---|---|
| Clinical characteristics | Treatment and follow-up | ||
| Tosti et al (1993), Italy2 (retrospective study) | 24 |
|
|
| Tosti et al (2001), Italy7 (retrospective study) | 15 | 15 children with nail lichen planus
Clinical characteristics
|
Treatment and follow-up
|
| Piraccini et al (2010), Italy8(retrospective study) | 105 |
|
Treatment
Follow-up
|
| Goettmann et al (2012), France1 (retrospective study) | 67 |
|
Treatment
Follow-up
|
| Żychowska et al (2020), Poland6 (retrospective study) | 21 |
|
NA |
| Kharghoria et al (2021), India4 (cross-sectional study) | 45 |
|
NA |
| Our study (2021), Thailand (retrospective study) | 14 |
|
Treatment
Follow-up
|
AD, Alternate day; IL, intralesional; IM, intramuscular; NA, not available.
Nail lichen planus is mostly recalcitrant to treatment and thus is challenging to cure. There is no currently available prospective study with long-term follow-up. Treatment outcomes are unpredictable. Intralesional or intramuscular triamcinolone acetonide should be considered as first-line therapy.3 In our study, systemic corticosteroids (oral prednisolone and intramuscular triamcinolone acetonide) yielded better treatment outcomes than topical medications alone. This result supports the conclusion of a previous study that systemic corticosteroids should be used early for the treatment of nail lichen planus, given that the disease is often aggressive and unpredictable.3 Nevertheless, the patients mostly showed only minimal to mild improvement.
The chief limitation of our study was the small number of patients due to the rarity of the disease. A longer study period is therefore needed to recruit more patients. Other limitations were the lack of dermoscopic nail findings and histopathologic results for every case.
In conclusion, given that about two thirds of patients with nail lichen planus had no concomitant mucocutaneous findings, an assessment of the clinical characteristics of the nails proved to be crucial for diagnosis. The detection of multiple melanonychia in Asians should therefore signal the possibility of nail lichen planus. In the absence of symptoms, patients may remain unaware of their nail abnormalities for extended periods, which can lead to severe and irreversible presentations. Even though systemic corticosteroids may be used, only minimal improvement is likely to be attained.
Conflicts of interest
None disclosed.
Acknowledgments
We gratefully acknowledge the professional editing of this article by Mr David Park.
Footnotes
Funding sources: None.
IRB approval status: The research protocol was approved by the Siriraj Institutional Review Board (Si 573/2019).
References
- 1.Goettmann S., Zaraa I., Moulonguet I. Nail lichen planus: epidemiological, clinical, pathological, therapeutic and prognosis study of 67 cases. J Eur Acad Dermatol Venereol. 2012;26(10):1304–1309. doi: 10.1111/j.1468-3083.2011.04288.x. [DOI] [PubMed] [Google Scholar]
- 2.Tosti A., Peluso A.M., Fanti P.A., Piraccini B.M. Nail lichen planus: clinical and pathologic study of twenty-four patients. J Am Acad Dermatol. 1993;28(5 Pt 1):724–730. doi: 10.1016/0190-9622(93)70100-8. [DOI] [PubMed] [Google Scholar]
- 3.Iorizzo M., Tosti A., Starace M. Isolated nail lichen planus: an expert consensus on treatment of the classical form. J Am Acad Dermatol. 2020;83(6):1717–1723. doi: 10.1016/j.jaad.2020.02.056. [DOI] [PubMed] [Google Scholar]
- 4.Kharghoria G., Grover C., Bhattacharya S.N., Sharma S. Histopathological evaluation of nail lichen planus: a cross-sectional study. J Cutan Pathol. 2021;48(1):11–17. doi: 10.1111/cup.13783. [DOI] [PubMed] [Google Scholar]
- 5.Tosti A., Piraccini B.M., de Farias D.C. Dealing with melanonychia. Semin Cutan Med Surg. 2009;28(1):49–54. doi: 10.1016/j.sder.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 6.Żychowska M., Żychowska M. Nail changes in lichen planus: a single-center study. J Cutan Med Surg. 2021;25(3):281–285. doi: 10.1177/1203475420982554. [DOI] [PubMed] [Google Scholar]
- 7.Tosti A., Piraccini B.M., Cambiaghi S., Jorizzo M. Nail lichen planus in children: clinical features, response to treatment, and long-term follow-up. Arch Dermatol. 2001;137(8):1027–1032. [PubMed] [Google Scholar]
- 8.Piraccini B.M., Saccani E., Starace M., Balestri R., Tosti A. Nail lichen planus: response to treatment and long term follow-up. Eur J Dermatol. 2010;20(4):489–496. doi: 10.1684/ejd.2010.0952. [DOI] [PubMed] [Google Scholar]